Virtual Reality Based Cognitive Rehabilitation in Minimally Conscious State: A Case Report with EEG Findings and Systematic Literature Review
Abstract
1. Introduction
2. Case Report
2.1. Intervention
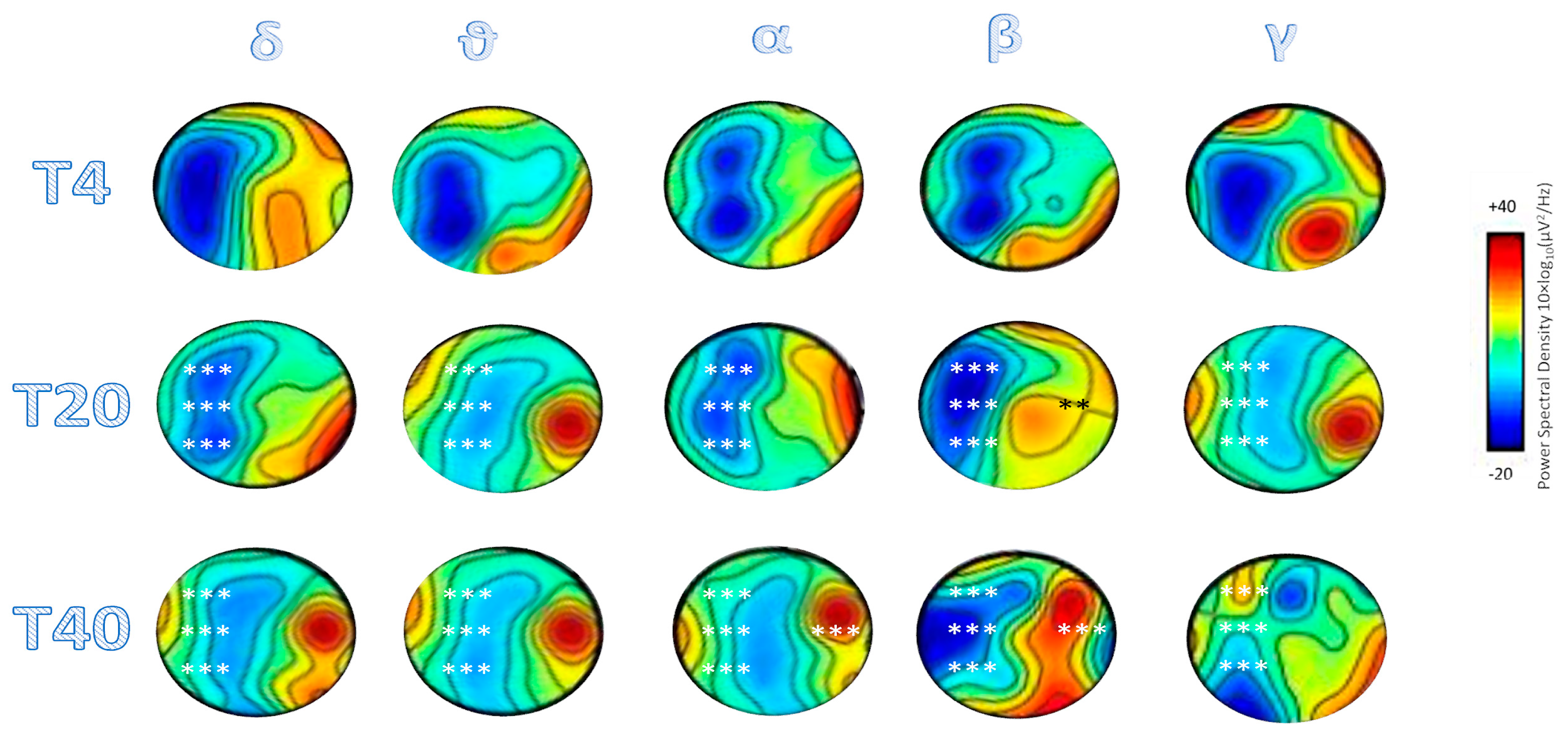
2.2. EEG Recording and Analysis
2.3. Outcomes
3. Systematic Review
3.1. Search Strategy
3.2. Data Extraction Process
3.3. Results of the Systematic Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ashwal, S.; Cranford, R.; Bernat, J.L. The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state (first of two parts). N. Engl. J. Med. 1994, 330, 1499–1508. [Google Scholar] [CrossRef]
- Giacino, J.T.; Ashwal, S.; Childs, N.; Cranford, R.; Jennett, B.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Whyte, J.; Zafonte, R.D.; et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 2002, 58, 349–353. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Milardi, D.; Cacciola, A.; Marra, A.; Digangi, G.; Casella, C.; Manuli, A.; De Luca, R.; Silvestri, R.; Bramanti, P. Moving into the wide clinical spectrum of consciousness disorders: Pearls, perils and pitfalls. Medicina 2016, 52, 11–18. [Google Scholar] [CrossRef]
- Bernat, J.L. Chronic disorders of consciousness. Lancet 2006, 367, 1181–1192. [Google Scholar] [CrossRef]
- Kalmar, K.; Giacino, J.T. The JFK Coma Recovery Scale-Revised. Neuropsychol. Rehabil. 2005, 15, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Schnakers, C.; Vanhaudenhuyse, A.; Giacino, J.; Ventura, M.; Boly, M.; Majerus, S.; Moonen, G.; Laureys, S. Diagnostic accuracy of the vegetative and minimally conscious state: Clinical consensus versus standardized neurobehavioral assessment. BMC Neurol. 2009, 9, 35. [Google Scholar] [CrossRef]
- Wannez, S.; Heine, L.; Thonnard, M.; Gosseries, O.; Laureys, S.; Coma Sci Grp, C. The repetition of behavioral assessments in diagnosis of disorders of consciousness. Ann. Neurol. 2017, 81, 883–889. [Google Scholar] [CrossRef]
- Schiff, N.D. Multimodal neuroimaging approaches to disorders of consciousness. J. Head Trauma. Rehab. 2006, 25, 388–397. [Google Scholar] [CrossRef]
- Cruse, D.; Chennu, S.; Chatelle, C.; Bekinschtein, T.A.; Fernàndez-Espejo, D.; Pickard, J.D.; Laureys, S.; Owen, A.M. Bedside detection of awareness in the vegetative state: A cohort study. Lancet 2011, 378, 2088–2094. [Google Scholar] [CrossRef]
- Fernàndez-Espejo, D.; Owen, A.M. Detecting awareness after severe brain injury. Nat. Rev. Neurosci. 2013, 14, 801–809. [Google Scholar] [CrossRef]
- Chennu, S.; Annen, J.; Wannez, S.; Thibaut, A.; Chatelle, C.; Cassol, H.; Martens, G.; Schnakers, C.; Gosseries, O.; Menon, D.; et al. Brain networks predict metabolism, diagnosis and prognosis at the bedside in disorders of consciousness. Brain 2017, 140, 2120–2132. [Google Scholar] [CrossRef] [PubMed]
- Bagnato, S.; Boccagni, C.; Sant’Angelo, A.; Fingelkurts, A.A.; Fingelkurts, A.A.; Galardi, G. Longitudinal Assessment of Clinical Signs of Recovery in Patients with Unresponsive Wakefulness Syndrome after Traumatic or Nontraumatic. Brain Inj. J. Neurotrauma 2017, 34, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, C.; Cortesi, A.; Masotti, S.; Simoncini, L.; Piperno, R. Increased behavioural responsiveness with complex stimulation in VS and MCS: Preliminary results. Brain Inj. 2012, 26, 1250–1256. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Peng, N. A design of virtual reality based coma stimulation program system. In Proceedings of the 2006 7th International Conference on Computer-Aided Industrial Design and Conceptual Design, Hangzhou, China, 17–19 November 2006; pp. 1–6. [Google Scholar] [CrossRef]
- Maggio, M.G.; Maresca, G.; De Luca, R.; Stagnitti, M.C.; Porcari, B.; Ferrera, M.C.; Galletti, F.; Casella, C.; Manuli, A.; Calabrò, R.S. The Growing Use of Virtual Reality in Cognitive Rehabilitation: Fact, Fake or Vision? A Scoping Review. J. Natl. Med. Assoc. 2019, 111, 457–463. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Leo, A.; De Luca, R.; Balletta, T.; Buda, A.; La Rosa, G.; Bramanti, A.; Bramanti, P. The role of virtual reality in improving motor performance as revealed by EEG: A randomized clinical trial. J. Neuroeng. Rehabil. 2017, 14, 53. [Google Scholar] [CrossRef]
- Bekinschtein, P.; Oomen, C.A.; Saksida, L.M.; Bussey, T.J. Effects of environmental enrichment and voluntary exercise on neurogenesis, learning and memory, and pattern separation: BDNF as a critical variable? Semin. Cell Dev. Biol. 2011, 22, 536–542. [Google Scholar] [CrossRef]
- Ansell, B.J.; Keenan, J.E. The Western Neuro Sensory Stimulation Profile: A tool for assessing slow-to-recover head-injured patients. Arch. Phys. Med. Rehabil. 1989, 70, 104–108. [Google Scholar]
- Dobkin, B.H. Functional MRI: A potential physiologic indicator for stroke rehabilitation interventions. Stroke 2003, 34, e23–e28. [Google Scholar] [CrossRef]
- Canedo, A.; Grix, M.C.; Nicoletti, J. An analysis of assessment instruments for the minimally responsive patient (MRP): Clinical observations. Brain Inj. 2002, 16, 453–461. [Google Scholar] [CrossRef]
- Tolle, P.; Reimer, M. Do we need stimulation programs as a part of nursing care for patients in “persistent vegetative state”? A conceptual analysis. Axone 2003, 25, 20–26. [Google Scholar]
- LeWinn, E.B.; Dimancescu, M.D. Environmental deprivation and enrichment in coma. Lancet 1978, 2, 156–157. [Google Scholar] [CrossRef]
- Barreca, S.; Velikonja, D.; Brown, L.; Williams, L.; Davis, L.; Sigouin, C.S. Evaluation of the effectiveness of two clinical training procedures to elicit yes/no responses from patients with a severe acquired brain injury: A randomized single-subject design. Brain Inj. 2003, 17, 1065–1075. [Google Scholar] [CrossRef] [PubMed]
- Kober, S.E.; Schweiger, D.; Witte, M.; Reichert, J.L.; Grieshofer, P.; Neuper, C.; Wood, G. Specific effects of EEG based neurofeedback training on memory functions in post-stroke victims. J. Neuroeng. Rehabil. 2015, 12, 107. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, J.; McCahill, M.P. Enabling social dimensions of learning through a persistent, unified, massively multi-user, and self-organizing virtual environment. In Proceedings Second International Conference on Creating, Connecting and Collaborating through Computing; IEEE: Piscataway, NJ, USA, 2004; pp. 166–172. [Google Scholar] [CrossRef]
- Naro, A.; Bramanti, P.; Leo, A.; Cacciola, A.; Bramanti, A.; Manuli, A.; Calabrò, R.S. Towards a method to differentiate chronic disorder of consciousness patients’ awareness: The Low-Resolution Brain Electromagnetic Tomography Analysis. J. Neurol. Sci. 2016, 368, 178–183. [Google Scholar] [CrossRef]
- Naro, A.; Leo, A.; Buda, A.; Manuli, A.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. Do you see me? The role of visual fixation in chronic disorders of consciousness differential diagnosis. Brain Res. 2016, 1653, 59–66. [Google Scholar] [CrossRef]
- Cruse, D.; Chennu, S.; Chatelle, C.; Fernández-Espejo, D.; Bekinschtein, T.A.; Pickard, J.D.; Laureys, S.; Owen, A.M. Relationship between etiology and covert cognition in the minimally conscious state. Neurology 2012, 78, 816–822. [Google Scholar] [CrossRef]
- Goldfine, A.M.; Schiff, N.D. Consciousness: Its neurobiology and the major classes of impairment. Neurol. Clin. 2011, 29, 723–737. [Google Scholar] [CrossRef]
- Gibson, R.M.; Owen, A.M.; Cruse, D. Brain-computer interfaces for patients with disorders of consciousness. Prog. Brain Res. 2016, 228, 241–291. [Google Scholar] [CrossRef]
- Maggio, M.G.; De Luca, R.; Manuli, A.; Buda, A.; Foti Cuzzola, M.; Leonardi, S.; D’Aleo, G.; Bramanti, P.; Russo, M.; Calabrò, R.S. Do patients with multiple sclerosis benefit from semi-immersive virtual reality? A randomized clinical trial on cognitive and motor outcomes. Appl. Neuropsychol. Adult 2020, 85, 7–10. [Google Scholar] [CrossRef]
- De Luca, R.; Maggio, M.G.; Maresca, G.; Latella, D.; Cannavò, A.; Sciarrone, F.; Lo Voi, E.; Accorinti, M.; Bramanti, P.; Calabrò, R.S. Improving Cognitive Function after Traumatic Brain Injury: A Clinical Trial on the Potential Use of the Semi-Immersive Virtual Reality. Behav. Neurol. 2019, 2019, 9268179. [Google Scholar] [CrossRef]
- Delorme, A.; Makeig, S. EEGLAB: An open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 2004, 134, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Makeig, S.; Bell, A.J.; Jung, T.P.; Sejnowski, T.J. Independent component analysis of electroencephalographic data. In Advances in Neural Information Processing Systems; MIT Press: Cambridge, MA, USA, 1996; pp. 145–151. [Google Scholar]
- Pfurtscheller, G.; Aranibar, A. Evaluation of event-related desynchronization (ERD) preceding and following voluntary self-paced movement. Electroencephalogr. Clin. Neurophysiol. 1979, 46, 138–146. [Google Scholar] [CrossRef]
- Makeig, S. Auditory event-related dynamics of the EEG spectrum and effects of exposure to tones. Electroencephalogr. Clin. Neurophysiol. 1993, 86, 283–293. [Google Scholar] [CrossRef]
- Graimann, B.; Huggins, J.E.; Levine, S.P.; Pfurtscheller, G. Visualization of significant ERD/ERS patterns in multichannel EEG and ECoG data. Clin. Neurophysiol. 2002, 113, 43–47. [Google Scholar] [CrossRef]
- Neuper, C.; Wörtz, M.; Pfurtscheller, G. ERD/ERS patterns reflecting sensorimotor activation and deactivation. Prog. Brain Res. 2006, 159, 211–222. [Google Scholar]
- Dubovik, S.; Ptak, R.; Aboulafia, T.; Magnin, C.; Gillabert, N.; Allet, L.; Pignat, J.M.; Schnider, A.; Guggisberg, A.G. EEG alpha band synchrony predicts cognitive and motor performance in patients with ischemic stroke. Behav. Neurol. 2013, 26, 187–189. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- De Salvo, S.; Caminiti, F.; Bonanno, L.; De Cola, M.C.; Corallo, F.; Caizzone, A.; Rifici, C.; Bramanti, P.; Marino, S. Neurophysiological assessment for evaluating residual cognition in vegetative and minimally conscious state patients: A pilot study. Funct. Neurol. 2015, 30, 237–244. [Google Scholar] [CrossRef]
- De Salvo, S.; Lo Buono, V.; Bonanno, L.; Micchia, K.; Cartella, E.; Romeo, L.; Arcadi, F.; Corallo, F.; Caminiti, F.; Bramanti, A.; et al. Role of visual P300 in cognitive assessment of subacute stroke patients: A longitudinal study. Int. J. Neurosci. 2019, 27, 1–5. [Google Scholar] [CrossRef]
- Keller, I.; Garbacenkaite, R. Neurofeedback in three patients in the state of unresponsive wakefulness. Appl. Psychophysiol. Biofeedback 2015, 40, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Naro, A.; Bramanti, A.; Leo, A.; Cacciola, A.; Manuli, A.; Bramanti, P.; Calabrò, R.S. Shedding new light on disorders of consciousness diagnosis: The dynamic functional connectivity. Cortex 2018, 103, 316–328. [Google Scholar] [CrossRef] [PubMed]
- Aricò, I.; Naro, A.; Pisani, L.R.; Leo, A.; Muscarà, N.; De Salvo, S.; Silvestri, R.; Bramanti, P.; Calabrò, R.S. Could combined sleep and pain evaluation be useful in the diagnosis of disorders of consciousness (DOC)? Preliminary findings. Brain Inj. 2016, 30, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Naro, A.; Calabrò, R.S.; Leo, A.; Russo, M.; Milardi, D.; Cannavò, A.; Manuli, A.; Buda, A.; Casella, C.; Bramanti, P.; et al. Bridging the Gap Towards Awareness Detection in Disorders of Consciousness: An Experimental Study on the Mirror Neuron System. Brain Topogr. 2018, 31, 623–639. [Google Scholar] [CrossRef]
- Cacciola, A.; Naro, A.; Milardi, D.; Bramanti, A.; Malatacca, L.; Spitaleri, M.; Leo, A.; Muscoloni, A.; Cannistraci, C.V.; Bramanti, P.; et al. Functional Brain Network Topology Discriminates between Patients with Minimally Conscious State and Unresponsive Wakefulness Syndrome. J. Clin. Med. 2019, 8, 306. [Google Scholar] [CrossRef]
- Hauger, S.L.; Olafsen, K.; Schnakers, C.; Andelic, N.; Bernhard, N.K.; Helseth, E.; Funderud, I.; Andersson, S.; Schanke, A.K.; Løvstad, M. Cognitive Event-Related Potentials during the Sub-Acute Phase of Severe Traumatic Brain Injury and Their Relationship to Outcome. J. Neurotrauma 2017, 22, 3124–3133. [Google Scholar] [CrossRef]
- Naro, A.; Chillura, A.; Portaro, S.; Bramanti, A.; De Luca, R.; Bramanti, P.; Calabrò, R.S. Novel Approaches to the Diagnosis of Chronic Disorders of Consciousness: Detecting Peripersonal Space by Using Ultrasonics. Front. Neurol. 2018, 9, 47. [Google Scholar] [CrossRef]
- Leo, A.; Naro, A.; Cannavò, A.; Pisani, L.R.; Bruno, R.; Salviera, C.; Bramanti, P.; Calabrò, R.S. Could autonomic system assessment be helpful in disorders of consciousness diagnosis? A neurophysiological study. Exp. Brain Res. 2016, 234, 2189–2199. [Google Scholar] [CrossRef]
- Keren, O.; Ben-Dror, S.; Stern, M.J.; Goldberg, G.; Groswasser, Z. Event-related potentials as an index of cognitive function during recovery from severe closed head injury. J. Head Trauma Rehabil. 1998, 13, 15–30. [Google Scholar] [CrossRef]
- Fernández-Espejo, D.; Junqué, C.; Vendrell, P.; Bernabeu, M.; Roig, T.; Bargalló, N.; Mercader, J.M. Cerebral response to speech in vegetative and minimally conscious states after traumatic brain injury. Brain Inj. 2008, 22, 882–890. [Google Scholar] [CrossRef]
- Naro, A.; Leo, A.; Manuli, A.; Cannavò, A.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. Show more How far can we go in chronic disorders of consciousness differential diagnosis? The use of neuromodulation in detecting internal and external awareness. Neuroscience 2017, 349, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Naro, A.; Leo, A.; Bruno, R.; Cannavò, A.; Buda, A.; Manuli, A.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. Reducing the rate of misdiagnosis in patients with chronic disorders of consciousness: Is there a place for audiovisual stimulation? Restor. Neurol. Neurosci. 2017, 35, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Chillura, A.; Naro, A.; Micchia, K.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. The value of midbrain morphology in predicting prognosis in chronic disorders of consciousness: A preliminary ultrasound study. J. Neurol. Sci. 2017, 380, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, R.S.; Naro, A.; Manuli, A.; Leo, A.; De Luca, R.; Lo Buono, V.; Russo, M.; Bramanti, A.; Bramanti, P. Pain perception in patients with chronic disorders of consciousness: What can limbic system tell us? Clin. Neurophysiol. 2017, 128, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Munivenkatappa, A.; Agrawal, A. Role of Thalamus in Recovery of Traumatic Brain Injury. J. Neurosci. Rural Pract. 2016, 7, S76–S79. [Google Scholar] [CrossRef]
- Naro, A.; Calabrò, R.S.; La Rosa, G.; Andronaco, V.A.; Billeri, L.; Lauria, P.; Bramanti, A.; Bramanti, P. Toward understanding the neurophysiological basis of peripersonal space: An EEG study on healthy individuals. PLoS ONE 2019, 14, e0218675. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Cimino, V.; Buda, A.; Paladina, G.; Di Lorenzo, G.; Manuli, A.; Milardi, D.; Bramanti, P.; Bramanti, A. Improving motor performance in Parkinson’s disease: A preliminary study on the promising use of the computer assisted virtual reality environment (CAREN). Neurol. Sci. 2019, 41, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; De Cola, M.C.; Latella, D.; Maresca, G.; Finocchiaro, C.; La Rosa, G.; Cimino, V.; Sorbera, C.; Bramanti, P.; De Luca, R.; et al. What About the Role of Virtual Reality in Parkinson Disease’s Cognitive Rehabilitation? Preliminary Findings from a Randomized Clinical Trial. J. Geriatr. Psychiatry Neurol. 2018, 31, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Latella, D.; Maresca, G.; Sciarrone, F.; Manuli, A.; Naro, A.; De Luca, R.; Calabrò, R.S. Virtual Reality and Cognitive Rehabilitation in People with Stroke: An Overview. J. Neurosci. Nurs. 2019, 51, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Russo, M.; Cuzzola, M.F.; Destro, M.; La Rosa, G.; Molonia, F.; Bramanti, P.; Lombardo, G.; De Luca, R.; Calabrò, R.S. Virtual reality in multiple sclerosis rehabilitation: A review on cognitive and motor outcomes. J. Clin. Neurosci. 2019, 65, 106–111. [Google Scholar] [CrossRef]
- Maresca, G.; Maggio, M.G.; Buda, A.; La Rosa, G.; Manuli, A.; Bramanti, P.; De Luca, R.; Calabrò, R.S. A novel use of virtual reality in the treatment of cognitive and motor deficit in spinal cord injury: A case report. Med. Baltim. 2018, 97, e13559. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; De Luca, R.; Molonia, F.; Porcari, B.; Destro, M.; Casella, C.; Salvati, R.; Bramanti, P.; Calabrò, R.S. Cognitive rehabilitation in patients with traumatic brain injury: A narrative review on the emerging use of virtual reality. J. Clin. Neurosci. 2019, 61, 1–4. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Portaro, S.; Le Cause, M.; De Domenico, C.; Maggio, M.G.; Ferrera, M.; Giuffrè, G.; Bramanti, A.; Calabrò, R.S. Cognitive rehabilitation using immersive virtual reality at a young age: A case report on traumatic brain injury. Appl. Neuropsychol. Child 2019, 6, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Torrisi, M.; Buda, A.; De Luca, R.; Piazzitta, D.; Cannavò, A.; Leo, A.; Milardi, D.; Manuli, A.; Calabro, R.S. Effects of robotic neurorehabilitation through lokomat plus virtual reality on cognitive function in patients with traumatic brain injury: A retrospective case-control study. Int. J. Neurosci. 2019, 2, 1–7. [Google Scholar] [CrossRef]
- Russo, M.; De Luca, R.; Naro, A.; Sciarrone, F.; Aragona, B.; Silvestri, G.; Manuli, A.; Bramanti, A.; Casella, C.; Bramanti, P.; et al. Does body shadow improve the efficacy of virtual reality-based training with BTS NIRVANA?: A pilot study. Medicine 2017, 96, e8096. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Maresca, G.; Scarcella, I.; Latella, D.; De Domenico, C.; Destro, M.; De Luca, R.; Calabro, R.S. Virtual reality-based cognitive rehabilitation in progressive supranuclear palsy. Psychogeriatrics 2019, 19, 616–618. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Russo, M.; Naro, A.; De Luca, R.; Leo, A.; Tomasello, P.; Molonia, F.; Dattola, V.; Bramanti, A.; Bramanti, P. Robotic gait training in multiple sclerosis rehabilitation: Can virtual reality make the difference? Findings from a randomized controlled trial. J. Neurol. Sci. 2017, 377, 25–30. [Google Scholar] [CrossRef]
- Levac, D.E.; Huber, M.E.; Sternad, D. Learning and transfer of complex motor skills in virtual reality: A perspective review. J. Neuroeng. Rehabil. 2019, 16, 121. [Google Scholar] [CrossRef]
- Espenhahn, S.; van Wijk, B.; Rossiter, H.E.; de Berker, A.O.; Redman, N.D.; Rondina, J.; Diedrichsen, J.; Ward, N.S. Cortical beta oscillations are associated with motor performance following visuomotor learning. Neuroimage 2019, 195, 340–353. [Google Scholar] [CrossRef]
- Schiff, N.D. Recovery of consciousness after brain injury: A mesocircuit hypothesis. Trends Neurosci. 2010, 33, 1–9. [Google Scholar] [CrossRef]
- Faugeras, F.; Rohaut, B.; Weiss, N.; Bekinschtein, T.A.; Galanaud, D.; Puybasset, L.; Bolgert, F.; Sergent, C.; Cohen, L.; Dehaene, S.; et al. Probing consciousness with event-related potentials in the vegetative state. Neurology 2011, 77, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Torrisi, M.; Piccolo, A.; De Luca, R.; Berenati, M.; Olivo, A.; Maresca, G.; Naro, A.; Calabrò, R.S. Are You There? The Growing Need to Get the Right Diagnosis in Disorder of Consciousness. J. Neurosci. Nurs. 2018, 50, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Billeri, L.; Filoni, S.; Russo, E.F.; Portaro, S.; Militi, D.; Calabrò, R.S.; Naro, A. Toward Improving Diagnostic Strategies in Chronic Disorders of Consciousness: An Overview on the (Re-) Emergent Role of Neurophysiology. Brain Sci. 2020, 10, 42. [Google Scholar] [CrossRef] [PubMed]



| Author, Year | Study’s Design | Tools | Patients | Major Findings |
|---|---|---|---|---|
| De Salvo et al., 2015 [42] | ES | Neurowave system: Visual event-related potentials (ERPs) | 11 vegetative state patients (VS) 5 Minimally Conscious State patients (MCS) | The authors found that ERPs monitoring can be useful for assessing residual cognitive function, thus guiding the optimal management at individual level. |
| De Salvo et al., 2019 [43] | ES | Neurowave system: Visual ERPs | 18 ischemic subacute stroke patients | The authors showed that the P300 ERP component could be a predictive marker for cognitive recovery of ischemic subacute stroke patients. Intensive programs of neurosensory stimulation could facilitate recovery of cognitive and attentive functions in subacute cerebrovascular disease. |
| Keller et al., 2015 [44] | ES | Neurofeedback technique (NFB) evaluated with EEG | 3 VS patients | The authors found that NFB can be used in patients in a state of insensitive insomnia. |
| Naro et al., 2018 [45] | OS | EEG | patients with chronic consciousness disorders (DoC) | The authors noted that EEG-based approaches can help differentiate patients with DoC. |
| Aricò et al., 2016 [46] | OS | EEG, including assessment of sleep structure and potential multimodal evoked recording, assessment of pain perception | 14 DoC patients | The authors stress the presence of correlations between global brain connectivity, sleep structure and pain perception, which are related to the activity of the large thalamocortical and cortico-cortical networks underlying consciousness. |
| Naro et al., 2018 [47] | ES | EEG | 14 patients with post-traumatic DoC 10 healthy controls | The authors found that mirror system evaluation can usefully be used to differentiate patients with DoC. |
| Cacciola et al., 2019 [48] | OS | EEG | 45 DoC patients | The authors show that EEG-based approaches can help understand the processes that underlie consciousness and their pathophysiology. |
| Naro et al., 2017 [27] | ES | EEG Audiovisual Stimulation | 10 healthy controls 7 MCS patients 9 UWS patients | The authors noted that the audiovisual stimulation paradigm can be used as a bed support tool to improve differential diagnosis in patients with DoC. |
| Naro et al., 2016 [26] | ES | EEG during a state of awake rest and performed a low-resolution electromagnetic brain tomography (LORETA) | DoC patient | The authors suggest that LORETA analysis may be useful in DoC differential diagnosis. |
| Hauger et al., 2017 [49] | ES | EEG ERP | 14 patients with traumatic brain injury (TBI) | The authors found that ERP can index cognitive abilities early on after TBI and cognitive P300 can provide information on residual cognition and prognosis. |
| Di Stefano et al., 2012 [13] | ES | Virtual reality | 20 DoC patients | The authors showed a difference in the patient’s response as a function of the stimulation context. A context with emotional richness and complexity of environmental stimuli can play a key role in evoking active behavior. |
| Chen and Peng, 2006 [14] | ES | Virtual reality | Coma patients | The authors suggest that a coma stimulation program that triggers the five senses of patients using VR can increase the patient’s responsiveness and improve the therapeutic process |
| Naro et al., 2018 [50] | OS | Changes in cerebral blood flow rate (CBFV) Functional transcranial Doppler (fTCD) | 21 patients with DoC (10 patients with MCS and 11 with UWS) 25 healthy controls | The authors note that fTCD can be a quick and very simple tool for differentiating patients with MCS and UWS. |
| Leo, et al., 2016 [51] | OS | Ultra-late laser evoked potentials Skin reflex | 12 MCS 10 UWS | The authors suggest that a broad spectrum electro-physiological assessment of autonomic nervous system functionality may support differential DoC diagnosis. |
| Keren et al., 1998 [52] | OS | ERPs | 60 DoC patients | The authors observed that ERP recordings can help assess the severity of the injury and as a physiological index of brain activity related to recovery from DoC. |
| Fernández-Espejo et al., 2008 [53] | OS | Functional magnetic resonance imaging | 3 VS patients 4 patients in MCS 19 healthy controls | The authors found that magnetic resonance imaging may be useful for identifying responses of brain activity, which can go unnoticed in a bed test. |
| Naro et al., 2017 [54] | ES | Repetitive transcranial magnetic stimulation | 20 patients with DoC | The authors speculate that patients with UWS who demonstrate evidence of residual default mode network and external awareness network functional correlation may be misdiagnosed. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maggio, M.G.; Naro, A.; La Rosa, G.; Cambria, A.; Lauria, P.; Billeri, L.; Latella, D.; Manuli, A.; Calabrò, R.S. Virtual Reality Based Cognitive Rehabilitation in Minimally Conscious State: A Case Report with EEG Findings and Systematic Literature Review. Brain Sci. 2020, 10, 414. https://doi.org/10.3390/brainsci10070414
Maggio MG, Naro A, La Rosa G, Cambria A, Lauria P, Billeri L, Latella D, Manuli A, Calabrò RS. Virtual Reality Based Cognitive Rehabilitation in Minimally Conscious State: A Case Report with EEG Findings and Systematic Literature Review. Brain Sciences. 2020; 10(7):414. https://doi.org/10.3390/brainsci10070414
Chicago/Turabian StyleMaggio, Maria Grazia, Antonino Naro, Gianluca La Rosa, Alice Cambria, Paola Lauria, Luana Billeri, Desiree Latella, Alfredo Manuli, and Rocco Salvatore Calabrò. 2020. "Virtual Reality Based Cognitive Rehabilitation in Minimally Conscious State: A Case Report with EEG Findings and Systematic Literature Review" Brain Sciences 10, no. 7: 414. https://doi.org/10.3390/brainsci10070414
APA StyleMaggio, M. G., Naro, A., La Rosa, G., Cambria, A., Lauria, P., Billeri, L., Latella, D., Manuli, A., & Calabrò, R. S. (2020). Virtual Reality Based Cognitive Rehabilitation in Minimally Conscious State: A Case Report with EEG Findings and Systematic Literature Review. Brain Sciences, 10(7), 414. https://doi.org/10.3390/brainsci10070414







