Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations
Abstract
1. Introduction
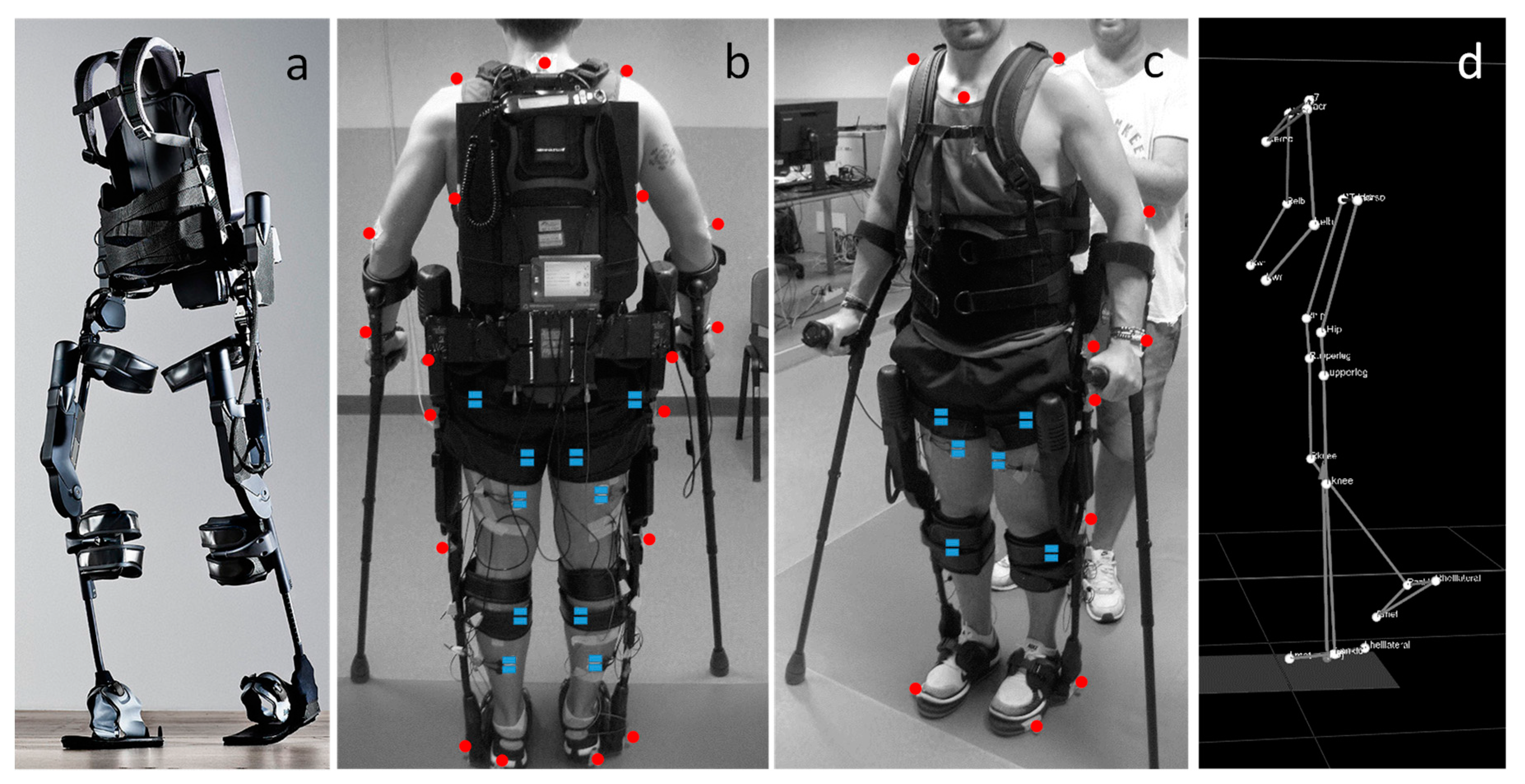
2. Materials and Methods
2.1. Participants
2.2. Apparatus: Brief Description of the Ekso Exoskeleton
- First Step: a physical therapist controls the beginning of each step by pushing a button. Usually, this modality is used in the first training session for the familiarization with the device;
- Active Step: the user controls the beginning of each step by means of an interface, placed on the crutches or on the walker, that communicate with the device.
- Pro Step: The user controls the beginning of the next step by moving his hips forward and laterally. In this case, when the device recognizes that the user is in the correct position allows the step of the contralateral leg.
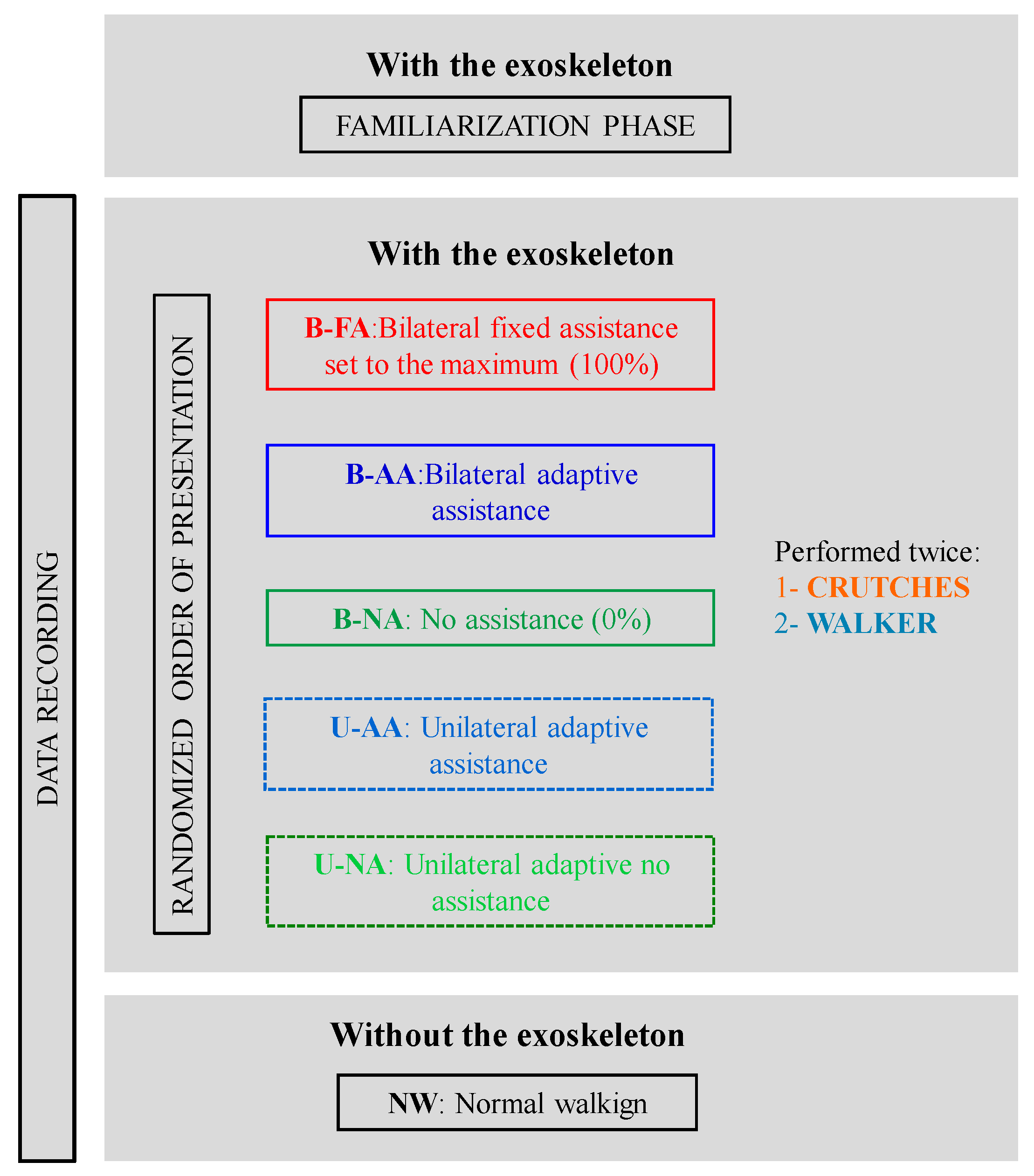
2.3. Experimental Protocol
2.4. Data Recording
2.5. Data Analysis
2.6. Statistical Analysis
3. Results
3.1. Spatio-Temporal Characteristics of the Gait
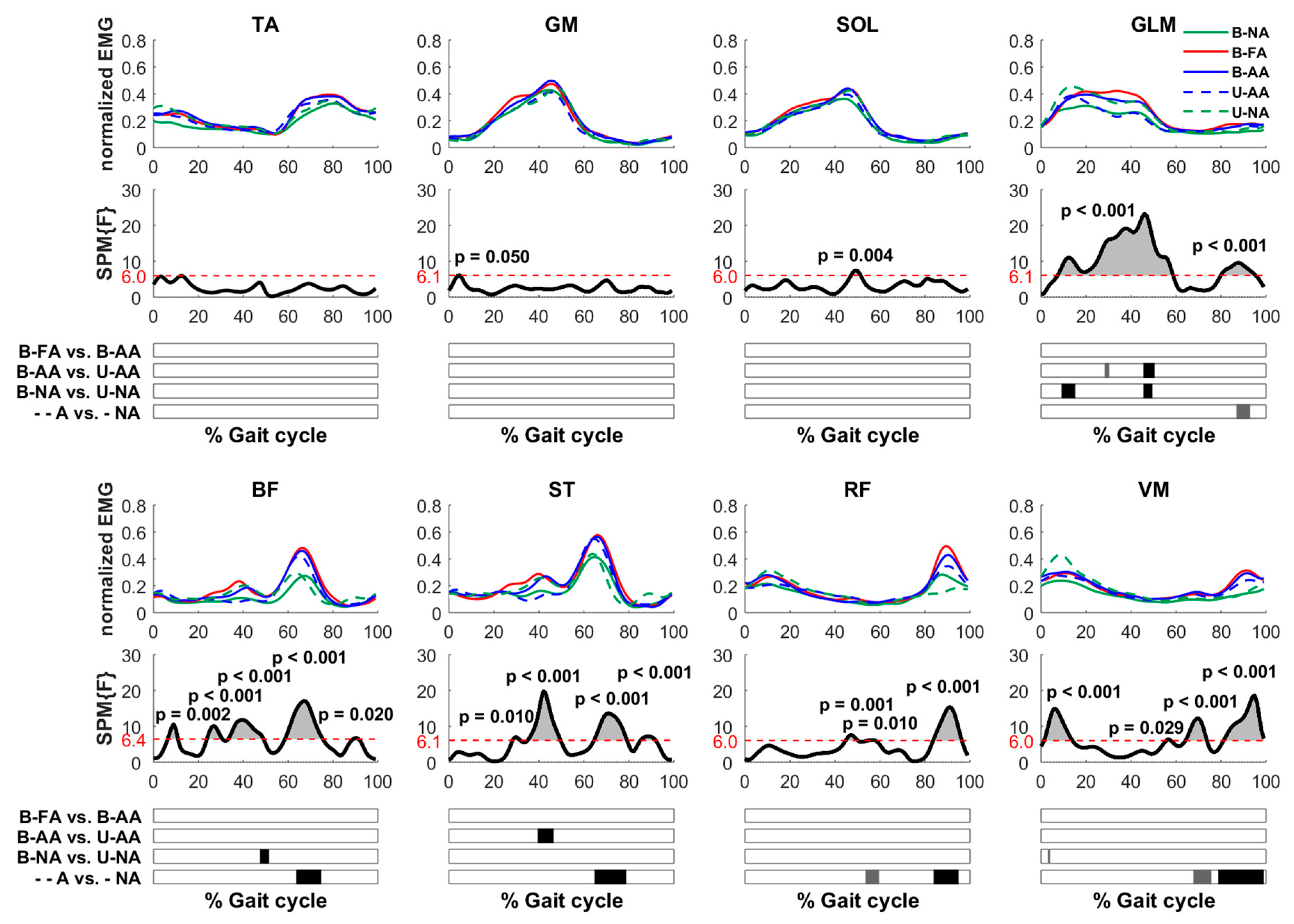
3.2. Muscle Activations When Walking with the Ekso under Different Conditions
- There was no difference between the muscle patterns between the B-FA, with the Ekso providing a fixed maximum assistance, independently of the subjects’ voluntary contribution, with respect to B-AA with the assistance adapted by the device, depending on the subject’s performance.
- In the second half of the gait cycle, the level of activations of both the unassisted modalities, B-NA, U-NA, was lower than those of the assistive modalities for the BF, ST RF, VM, and GLM muscles between 60–80% of the gait cycle for the first two muscles (in correspondence with the peak of muscle activation, both p < 0.001) and between 80–100% for the other three (RF and VM p < 0.001; GLM p < 0.05).
- Under unilateral assistance, both the assisted (U-AA) and unassisted (U-NA) leg had significant differences when compared to the corresponding case where the contralateral leg was in the same assistive condition i.e., B-AA and B-NA, respectively. These differences were mainly evident and significant in the middle of the walking cycle (40–50%) for the GLM muscle in both comparisons (p < 0.001) for BF when comparing the unassisted conditions B-NA versus U-NA (p < 0.001) and for the ST when comparing the assistive conditions B-AA versus U-AA (p < 0.001). Specifically for the unassisted modalities, the activation was mainly higher for the unilateral condition, while it was lower for the assistive modalities.
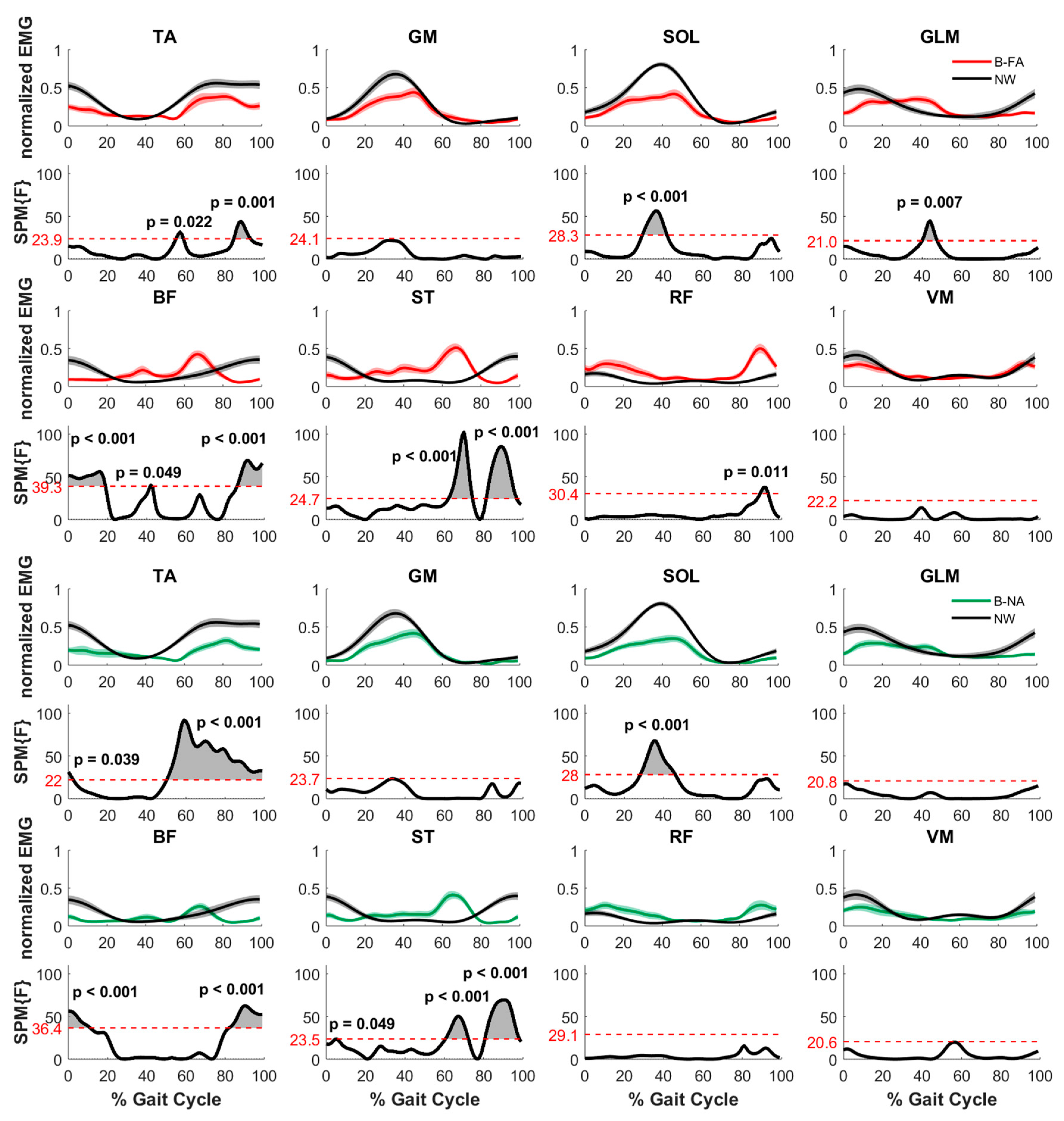
3.3. Muscle Activations When Walking with and without the Ekso
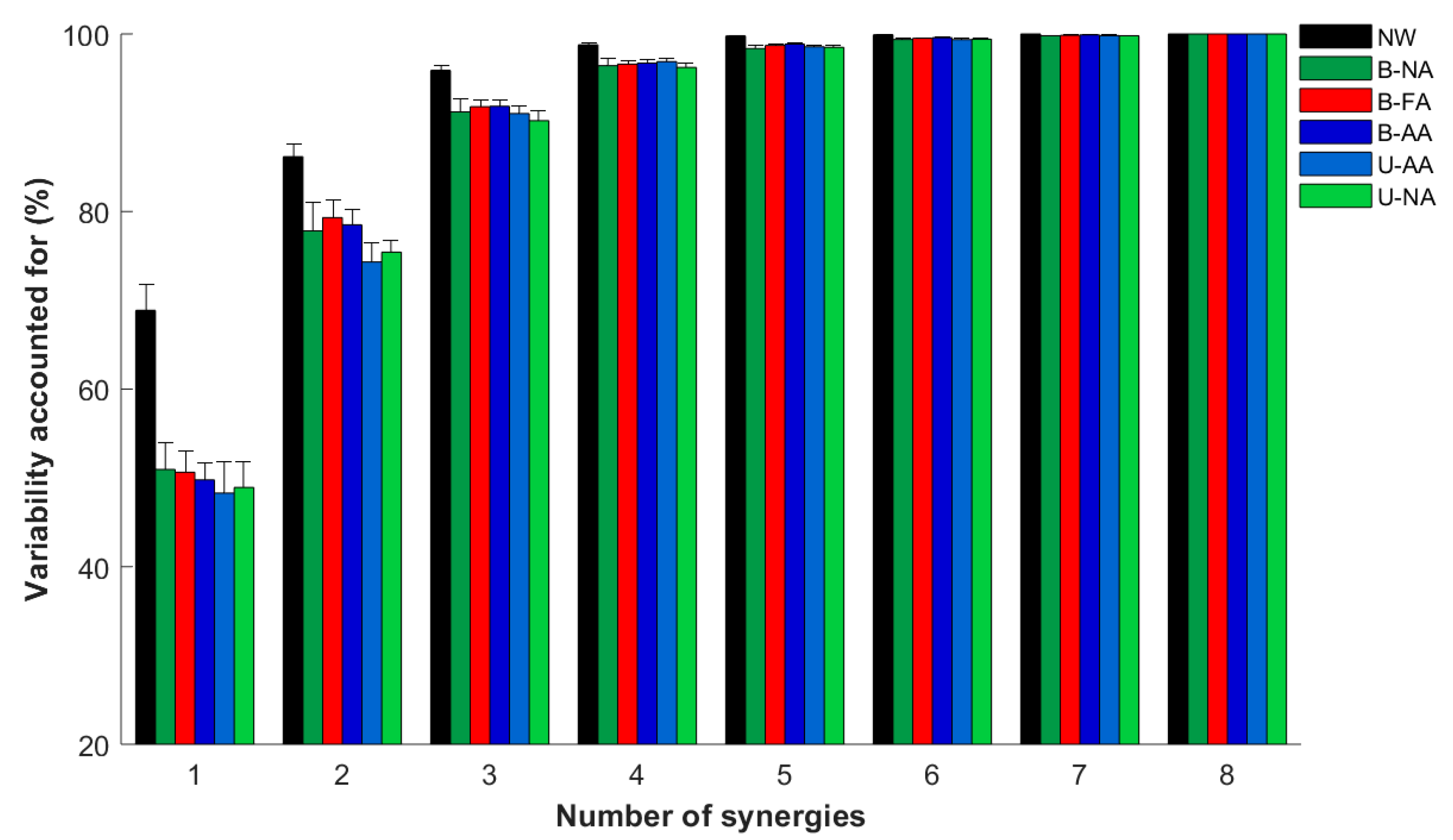
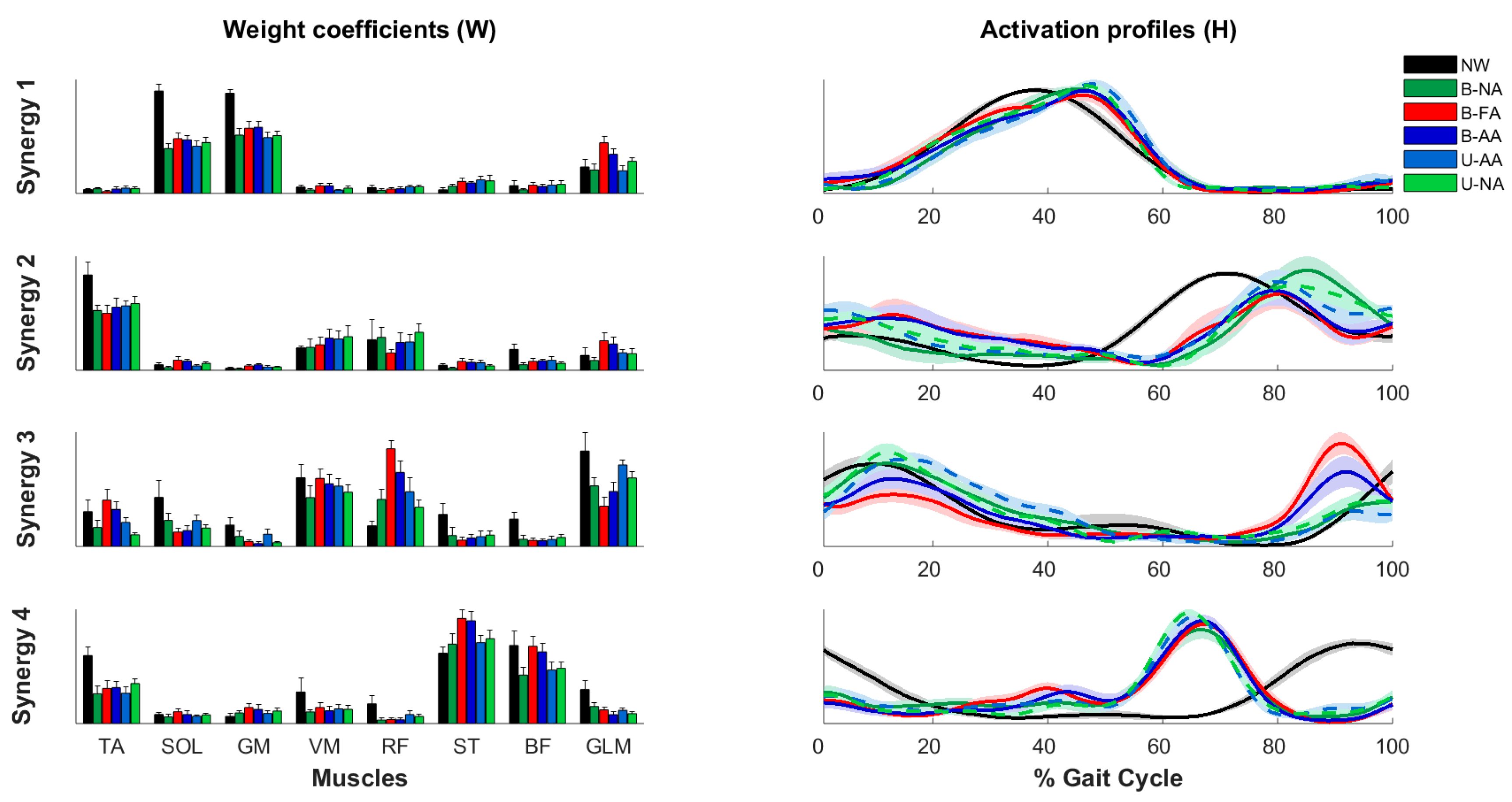
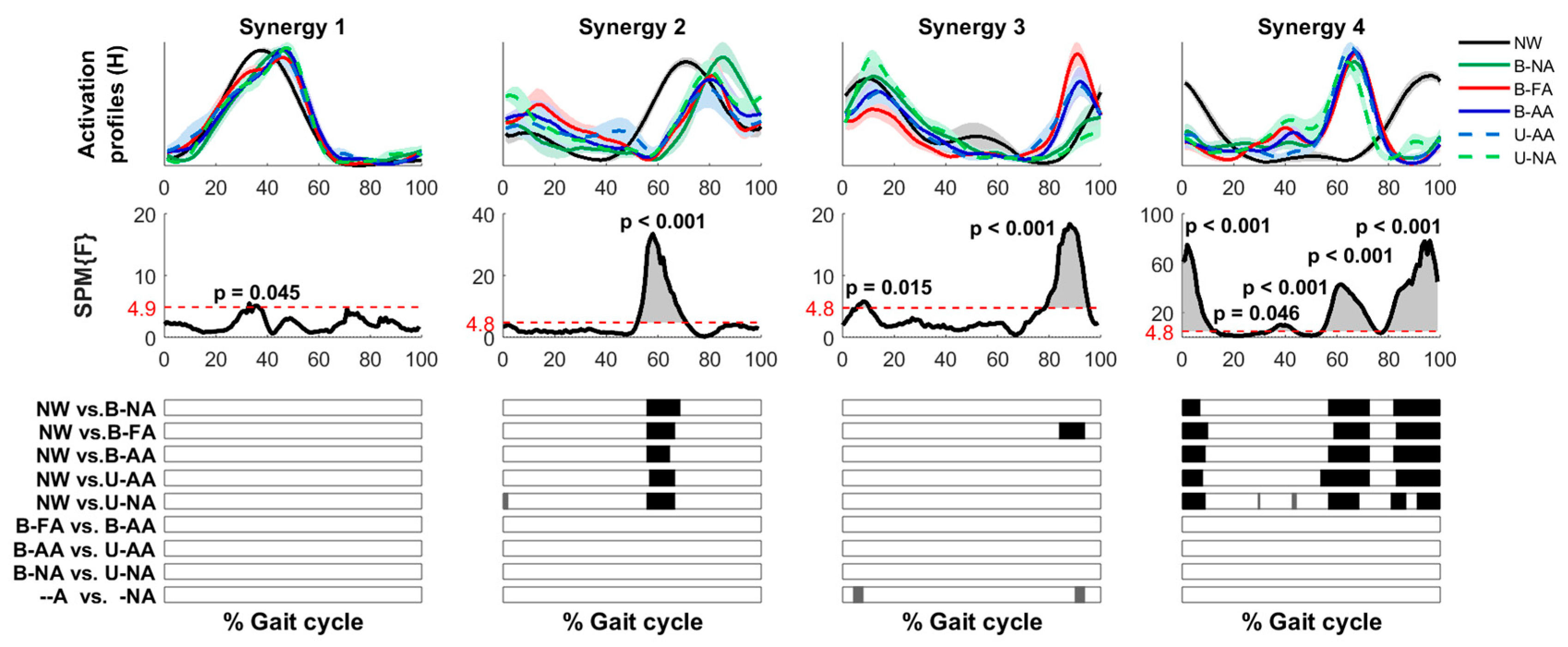
3.4. Muscle Synergies
4. Discussion
4.1. Comparison between Assistance Modalities with the Ekso
4.2. Comparison between Normal Walking and Ekso-Assisted Walking
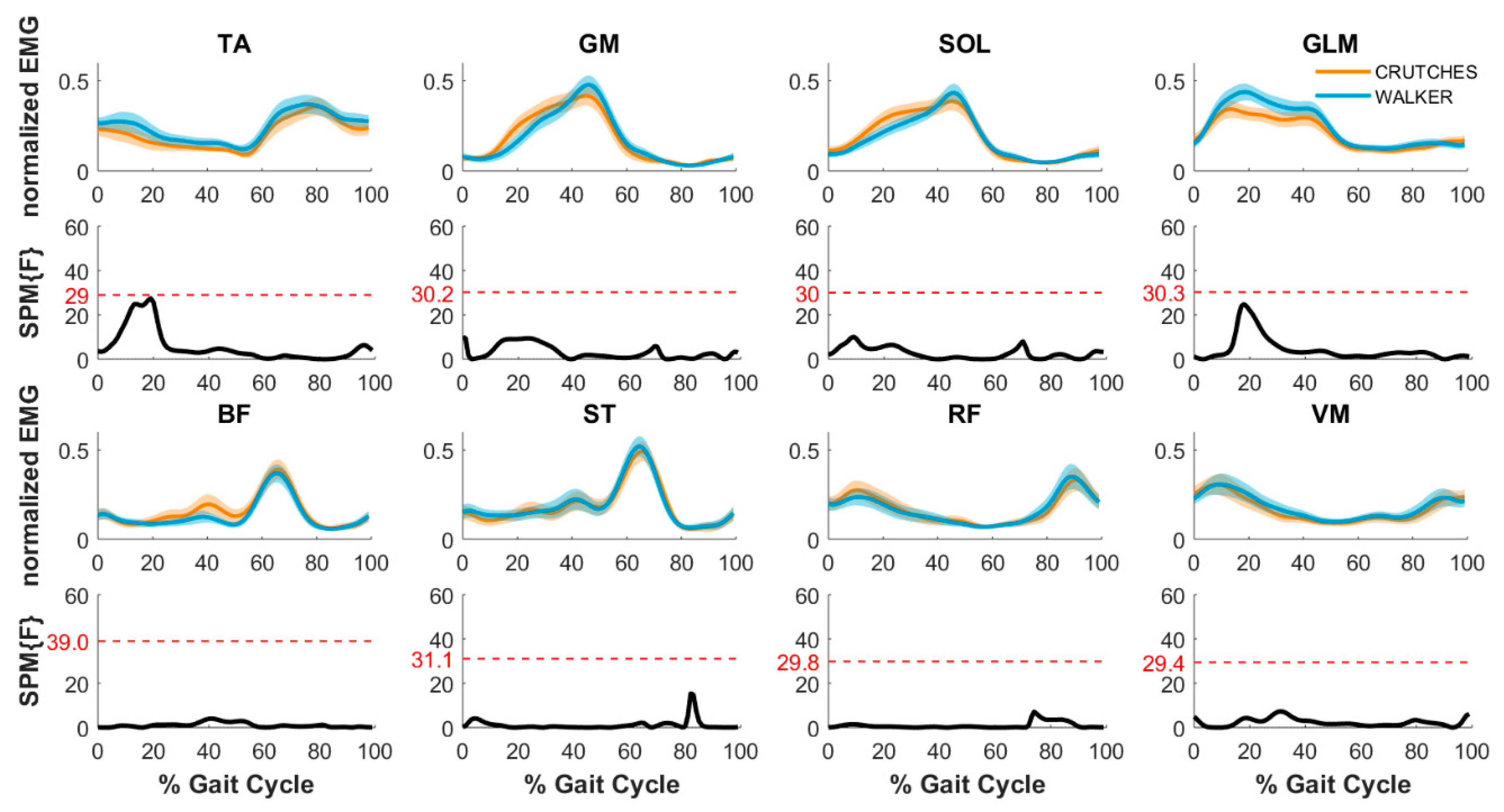
4.3. Walking with the Aids
4.4. Cautionary Notes
4.5. Future Work and Clinical Applications
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sale, P.; Franceschini, M.; Waldner, A.; Hesse, S. Use of the robot assisted gait therapy in rehabilitation of patients with stroke and spinal cord injury. Eur. J. Phys. Rehabil. Med. 2012, 48, 111–121. [Google Scholar] [PubMed]
- Esquenazi, A.; Packel, A. Robotic-Assisted Gait Training and Restoration. Am. J. Phys. Med. Rehabil. 2012, 91, 217. [Google Scholar] [CrossRef] [PubMed]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and tolerance of the ReWalk™ exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Hornby, T.G.; Zemon, D.H.; Campbell, D. Robotic-Assisted, Body-Weight–Supported Treadmill Training in Individuals Following Motor Incomplete Spinal Cord Injury. Phys. Ther. 2005, 85, 52–66. [Google Scholar] [PubMed]
- Tefertiller, C.; Pharo, B.; Evans, N.; Winchester, P. Efficacy of rehabilitation robotics for walking training in neurological disorders: A review. J. Rehabil. Res. Dev. 2011, 48, 387. [Google Scholar] [CrossRef] [PubMed]
- Benito-Penalva, J.; Edwards, D.J.; Opisso, E.; Cortes, M.; López-Blázquez, R.; Murillo, N.; Costa, Ú.; Tormos, J.M.; Vidal-Samso, J.; Valls-Solé, J.; et al. Gait Training in Human Spinal Cord Injury Using Electromechanical Systems: Effect of Device Type and Patient Characteristics. Arch. Phys. Med. Rehabil. 2012, 93, 404–412. [Google Scholar] [CrossRef]
- Sale, P.; Russo, E.F.; Scarton, A.; Calabrò, R.S.; Masiero, S.; Filoni, S. Training for mobility with exoskeleton robot in spinal cord injury patients: A pilot study. Eur. J. Phys. Rehabil. Med. 2018, 54, 745–751. [Google Scholar] [CrossRef]
- Chang, S.-H.; TIRR SCI Clinical Exoskeleton Group; Afzal, T.; Berliner, J.; Francisco, G.E.; Kern, M. Exoskeleton-assisted gait training to improve gait in individuals with spinal cord injury: A pilot randomized study. Pilot Feasibility Stud. 2018, 4, 62. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.-W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 5819. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, A.J.; Mrachacz-Kersting, N.; Van Asseldonk, E.; Turner, D.L.; Spaich, E.G. Spinal plasticity in robot-mediated therapy for the lower limbs. J. Neuroeng. Rehabil. 2015, 12, 81. [Google Scholar] [CrossRef] [PubMed]
- Dobkin, B.; Apple, D.; Barbeau, H.; Basso, M.; Behrman, A.; Deforge, D.; Ditunno, J.; Dudley, G.; Elashoff, R.; Fugate, L.; et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006, 66, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Alcobendas-Maestro, M.; Esclarín-Ruz, A.; Casado-López, R.M.; Muñoz-González, A.; Perez-Mateos, G.; Gonzalez-Valdizan, E.; Martin, J.L.R. Lokomat robotic-assisted versus overground training within 3 to 6 months of incomplete spinal cord lesion: Randomized controlled trial. Neurorehabil. Neural Repair 2012, 26, 1058–1063. [Google Scholar] [CrossRef] [PubMed]
- Louie, D.R.; Eng, J.J.; Lam, T. Spinal Cord Injury Research Evidence Research, “Gait speed using powered robotic exoskeletons after spinal cord injury: A systematic review and correlational study”. J. Neuroeng. Rehabil. 2015, 12, 82. [Google Scholar] [CrossRef] [PubMed]
- Swinnen, E.; Duerinck, S.; Baeyens, J.; Meeusen, R.; Kerckhofs, E. Effectiveness of robot-assisted gait training in persons with spinal cord injury: A systematic review. J. Rehabilitation Med. 2010, 42, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Gorgey, A.S.; Wade, R.; Sumrell, R.; Villadelgado, L.; Khalil, R.E.; Lavis, T. Exoskeleton Training May Improve Level of Physical Activity After Spinal Cord Injury: A Case Series. Top. Spinal Cord Inj. Rehabil. 2017, 23, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Palermo, A.E.; Maher, J.L.; Baunsgaard, C.B.; Nash, M.S. Clinician-Focused Overview of Bionic Exoskeleton Use After Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2017, 23, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Molteni, F.; Gasperini, G.; Gaffuri, M.; Colombo, M.; Giovanzana, C.; Lorenzon, C.; Farina, N.; Cannaviello, G.; Scarano, S.; Proserpio, D.; et al. Wearable robotic exoskeleton for over-ground gait training in sub-acute and chronic hemiparetic stroke patients: Preliminary results. Eur. J. Phys. Rehabil. Med. 2017, 53, 676–684. [Google Scholar] [PubMed]
- Moreno, J.C.; Barroso, F.; Farina, D.; Gizzi, L.; Santos, C.; Molinari, M.; Pons, J.L. Effects of robotic guidance on the coordination of locomotion. J. Neuroeng. Rehabil. 2013, 10, 79. [Google Scholar] [CrossRef]
- Jin, X.; Cai, Y.; Prado, A.; Agrawal, S.K. Effects of exoskeleton weight and inertia on human walking. In Proceedings of the 2017 IEEE International Conference on Robotics and Automation (ICRA), Singapore, 29 May–3 June 2017; pp. 1772–1777. [Google Scholar]
- Labini, F.S.; La Scaleia, V.; D’Avella, A.; Pisotta, I.; Tamburella, F.; Scivoletto, G.; Molinari, M.; Wang, S.; Wang, L.; Van Asseldonk, E.; et al. EMG patterns during assisted walking in the exoskeleton. Front. Hum. Neurosci. 2014, 8, 423. [Google Scholar]
- Swank, C.; Wang-Price, S.; Gao, F.; Almutairi, S. Walking in A Robotic Exoskeleton Does Not Mimic Natural Gait (Preprint) Walking with a Robotic Exoskeleton Does Not Mimic Natural Gait: A Within-Subjects Study. JMIR Rehabil. Assist. Technol. 2018, 6, e11023. [Google Scholar] [CrossRef]
- Ekkelenkamp, R.; Van Asseldonk, E.H.F.; Veneman, J.F.; Buurke, J.H.; Van Der Helm, F.C.T.; Van Der Kooij, H. The Effects on Kinematics and Muscle Activity of Walking in a Robotic Gait Trainer During Zero-Force Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 16, 360–370. [Google Scholar]
- Emken, J.L.; Benitez, R.; Reinkensmeyer, D.J. Human-robot cooperative movement training: Learning a novel sensory motor transformation during walking with robotic assistance-as-needed. J. Neuroeng. Rehabil. 2007, 4, 8. [Google Scholar] [CrossRef] [PubMed]
- Ekso Bionics. Ekso Bionics Homepage. 2019. Available online: https://eksobionics.com/ (accessed on 18 July 2019).
- Landau, I.D.; Lozano, R.; M’Saad, M.; Karimi, A. Adaptive Control: Algorithms, Analysis AND Applications; Springer Science & Business Media: Berlin, Germany, 2011. [Google Scholar]
- Davis, R.B. Clinical gait analysis. IEEE Eng. Med. Biol. Mag. 1988, 7, 35–40. [Google Scholar] [CrossRef] [PubMed]
- De Luca, A.; Giannoni, P.; Vernetti, H.; Capra, C.; Lentino, C.; Checchia, G.A.; Casadio, M. Training the Unimpaired Arm Improves the Motion of the Impaired Arm and the Sitting Balance in Chronic Stroke Survivors. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 873–882. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.M.; Thorpe, S.K.; O’Malley, M.J.; Vaughan, C.L. Automatic detection of gait events using kinematic data. Gait Posture 2007, 25, 469–474. [Google Scholar] [CrossRef] [PubMed]
- De Luca, A.; Vernetti, H.; Capra, C.; Pisu, I.; Cassiano, C.; Barone, L.; Gaito, F.; Danese, F.; Antonio Checchia, G.; Lentino, C.; et al. Recovery and compensation after robotic assisted gait training in chronic stroke survivors. Disabil. Rehabil. Assist. Technol. 2018, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.; Polygerinos, P.; Allen, S.; Panizzolo, F.A.; Walsh, C.J.; Holland, D.P. A Quasi-Passive Knee Exoskeleton to Assist During Descent. In Wearable Robotics: Challenges and Trends; Springer: Cham, Switzerland, 2017; pp. 63–67. [Google Scholar]
- Naik, G.R.; Al-Ani, A.; Gobbo, M.; Nguyen, H.T. Does Heel Height Cause Imbalance during Sit-to-Stand Task: Surface EMG Perspective. Front. Physiol. 2017, 8, 626. [Google Scholar] [CrossRef]
- Cheung, V.C.K.; Piron, L.; Agostini, M.; Silvoni, S.; Turolla, A.; Bizzi, E. Stability of muscle synergies for voluntary actions after cortical stroke in humans. Proc. Natl. Acad. Sci. USA 2009, 106, 19563–19568. [Google Scholar] [CrossRef]
- Pellegrino, L.; Coscia, M.; Muller, M.; Solaro, C.; Casadio, M. Evaluating upper limb impairments in multiple sclerosis by exposure to different mechanical environments. Sci. Rep. 2018, 8, 2110. [Google Scholar] [CrossRef]
- Clark, D.J.; Ting, L.H.; Zajac, F.E.; Neptune, R.R.; Kautz, S.A. Merging of healthy motor modules predicts reduced locomotor performance and muscle coordination complexity post-stroke. J. Neurophysiol. 2010, 103, 844–857. [Google Scholar] [CrossRef]
- Lee, D.D.; Hill, M.; Seung, H.S. Algorithms for Non-negative Matrix Factorization. Adv. Neural Inf. Process. Syst. 2001, 13, 556–562. [Google Scholar]
- Ting, L.H.; McKay, J.L. Neuromechanics of muscle synergies for posture and movement. Curr. Opin. Neurobiol. 2007, 17, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Flanders, M. Temporal patterns of muscle activation for arm movements in three-dimensional space. J. Neurosci. 1991, 11, 2680–2693. [Google Scholar] [CrossRef] [PubMed]
- Coscia, M.; Cheung, V.C.; Tropea, P.; Koenig, A.; Monaco, V.; Bennis, C.; Micera, S.; Bonato, P. The effect of arm weight support on upper limb muscle synergies during reaching movements. J. Neuroeng. Rehabil. 2014, 11, 22. [Google Scholar] [CrossRef] [PubMed]
- D’Avella, A.; Saltiel, P.; Bizzi, E. Combinations of muscle synergies in the construction of a natural motor behavior. Nat. Neurosci. 2003, 6, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Cheung, V.C.; Turolla, A.; Agostini, M.; Silvoni, S.; Bennis, C.; Kasi, P.; Paganoni, S.; Bonato, P.; Bizzi, E. Muscle synergy patterns as physiological markers of motor cortical damage. Proc. Natl. Acad. Sci. USA 2012, 109, 14652–14656. [Google Scholar] [CrossRef]
- Friston, K. A short history of SPM. Stat. Parametr. Mapp. Anal. Funct. Brain Images 2007, 3–9. [Google Scholar] [CrossRef]
- Neptune, R.R.; Clark, D.J.; Kautz, S.A. Modular control of human walking: A simulation study. J. Biomech. 2009, 42, 1282–1287. [Google Scholar] [CrossRef]
- Wang, S.; Wang, L.; Meijneke, C.; Van Asseldonk, E.; Hoellinger, T.; Cheron, G.; Ivanenko, Y.; La Scaleia, V.; Sylos-Labini, F.; Molinari, M.; et al. Design and control of the MINDWALKER exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 23, 277–286. [Google Scholar] [CrossRef]
- Cheron, G.; Bengoetxea, A.; Pozzo, T.; Bourgeois, M.; Draye, J. Evidence of a preprogrammed deactivation of the hamstring muscles for triggering rapid changes of posture in humans. Electroencephalogr. Clin. Neurophysiol. Mot. Control. 1997, 105, 58–71. [Google Scholar] [CrossRef]
- Perry, J.; Davids, J.R. Gait analysis: Normal and pathological function. J. Pediatr. Orthop. 1992, 12, 815. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M.; Ordway, N.R.; Ploutz-Snyder, L.L. Leg muscle activity during walking with assistive devices at varying levels of weight bearing. Arch. Phys. Med. Rehabil. 2004, 85, 1555–1560. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Iosa, M.; Tamburella, F.; Muzzioli, L.; Pisotta, I.; Moreno, J.C.; Pons, J.L.; Paolucci, S.; Cincotti, F.; Molinari, M. An EMG Pattern Comparison of Exoskeleton vs. End-Effector Robotic Device for Assisted Walking Training BT-Replace, Repair, Restore, Relieve–Bridging Clinical and Engineering Solutions in Neurorehabilitation; Springer: Cham, Switzerland, 2014; pp. 563–567. [Google Scholar]
- Hussein, S.; Schmidt, H.; Volkmar, M.; Werner, C.; Helmich, I.; Piorko, F.; Kruger, J.; Hesse, S. Muscle coordination in healthy subjects during floor walking and stair climbing in robot assisted gait training. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 1961–1964. [Google Scholar]
- Gizzi, L.; Nielsen, J.F.; Felici, F.; Moreno, J.C.; Pons, J.L.; Farina, D. Motor modules in robot-aided walking. J. Neuroeng. Rehabil. 2012, 9, 76. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, G.; Ivanenko, Y.P.; Poppele, R.E.; Lacquaniti, F. Motor Patterns in Human Walking and Running. J. Neurophysiol. 2006, 95, 3426–3437. [Google Scholar] [CrossRef] [PubMed]
- Arsenault, A.B.; Winter, D.A.; Marteniuk, R.G.; Hayes, K.C. How many strides are required for the analysis of electromyographic data in gait? Scand. J. Rehabil. Med. 1986, 18, 133–135. [Google Scholar]
- Lee, S.J.; Hidler, J. Biomechanics of overground vs. treadmill walking in healthy individuals. J. Appl. Physiol. 2008, 104, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Shiavi, R.; Frigo, C.; Pedotti, A. Electromyographic signals during gait: Criteria for envelope filtering and number of strides. Med Boil. Eng. 1998, 36, 171–178. [Google Scholar] [CrossRef]
- Hof, A.; Elzinga, H.; Grimmius, W.; Halbertsma, J.; Hof, A. Speed dependence of averaged EMG profiles in walking. Gait Posture 2002, 16, 78–86. [Google Scholar] [CrossRef]
- Kirshblum, S.C.; Burns, S.P.; Biering-Sorensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Johansen, M.; Jones, L.; Krassioukov, A.; Mulcahey, M.J.; et al. International standards for neurological classification of spinal cord injury (revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef]
- Asselin, P.; Knezevic, S.; Kornfeld, S.; Cirnigliaro, C.; Agranova-Breyter, I.; Bauman, W.A.; Spungen, A.M. Heart rate and oxygen demand of powered exoskeleton-assisted walking in persons with paraplegia. J. Rehabil. Res. Dev. 2015, 52, 147–158. [Google Scholar] [CrossRef]
- AlAmro, R.A.; Chisholm, A.E.; Williams, A.M.M.; Carpenter, M.G.; Lam, T. Overground walking with a robotic exoskeleton elicits trunk muscle activity in people with high-thoracic motor-complete spinal cord injury. J. Neuroeng. Rehabil. 2018, 15, 109. [Google Scholar] [CrossRef] [PubMed]

| Age [Y] | Gender [M/F] | Height [cm] | Weight [Kg] | |
|---|---|---|---|---|
| S1 | 45 | M | 179 | 68 |
| S2 | 24 | F | 175 | 62 |
| S3 | 25 | F | 155 | 54 |
| S4 | 22 | F | 183 | 70 |
| S5 | 22 | M | 178 | 75 |
| S6 | 23 | M | 182 | 86 |
| S7 | 24 | F | 158 | 60 |
| S8 | 32 | M | 184 | 74 |
| Subjects Height [cm] | Step Length [inches] | Step Height [inches] | Swing Time [s] | |
|---|---|---|---|---|
| S1 | 179 | 15.0 | 1 | 1.35 |
| S2 | 175 | 14.5 | 1 | 1.30 |
| S3 | 155 | 13.5 | 1 | 1.20 |
| S4 | 183 | 15.5 | 1 | 1.40 |
| S5 | 178 | 15.0 | 1 | 1.35 |
| S6 | 182 | 15.5 | 1 | 1.40 |
| S7 | 158 | 13.5 | 1 | 1.20 |
| S8 | 184 | 15.5 | 1 | 1.40 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Luca, A.; Bellitto, A.; Mandraccia, S.; Marchesi, G.; Pellegrino, L.; Coscia, M.; Leoncini, C.; Rossi, L.; Gamba, S.; Massone, A.; et al. Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations. Appl. Sci. 2019, 9, 2868. https://doi.org/10.3390/app9142868
De Luca A, Bellitto A, Mandraccia S, Marchesi G, Pellegrino L, Coscia M, Leoncini C, Rossi L, Gamba S, Massone A, et al. Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations. Applied Sciences. 2019; 9(14):2868. https://doi.org/10.3390/app9142868
Chicago/Turabian StyleDe Luca, Alice, Amy Bellitto, Sergio Mandraccia, Giorgia Marchesi, Laura Pellegrino, Martina Coscia, Clara Leoncini, Laura Rossi, Simona Gamba, Antonino Massone, and et al. 2019. "Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations" Applied Sciences 9, no. 14: 2868. https://doi.org/10.3390/app9142868
APA StyleDe Luca, A., Bellitto, A., Mandraccia, S., Marchesi, G., Pellegrino, L., Coscia, M., Leoncini, C., Rossi, L., Gamba, S., Massone, A., & Casadio, M. (2019). Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations. Applied Sciences, 9(14), 2868. https://doi.org/10.3390/app9142868




