Predicting Risk Factors for Dyslipidemia Based on Health Behaviors by Age in Adults Using Machine Learning
Abstract
1. Introduction
2. Methods
2.1. Research Subjects and Data Collection
2.2. Research Tools
2.2.1. Demographic Characteristics and Health Status
2.2.2. Health Behavior Characteristics
2.2.3. Practice of Healthy Eating Habits
2.3. Data Analysis Methods
3. Results and Discussion
3.1. Differences in the Dyslipidemia Prevalence by Subject Characteristics by Age
3.1.1. Differences by General Characteristics and Health Status
3.1.2. Differences by Health Behavior and Eating Habits
3.2. The Effect of Health Behavior and Eating Habits on the Dyslipidemia Prevalence
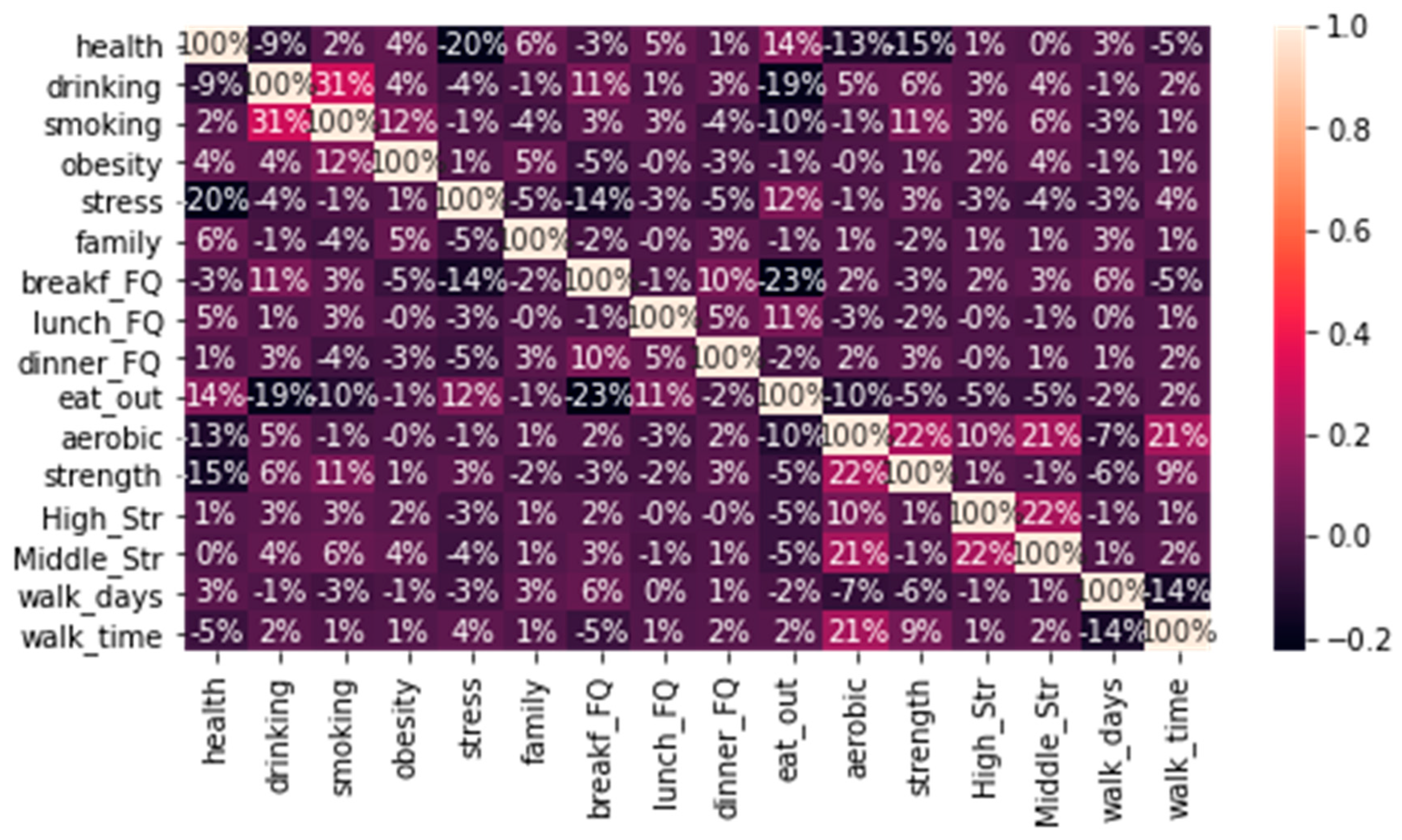
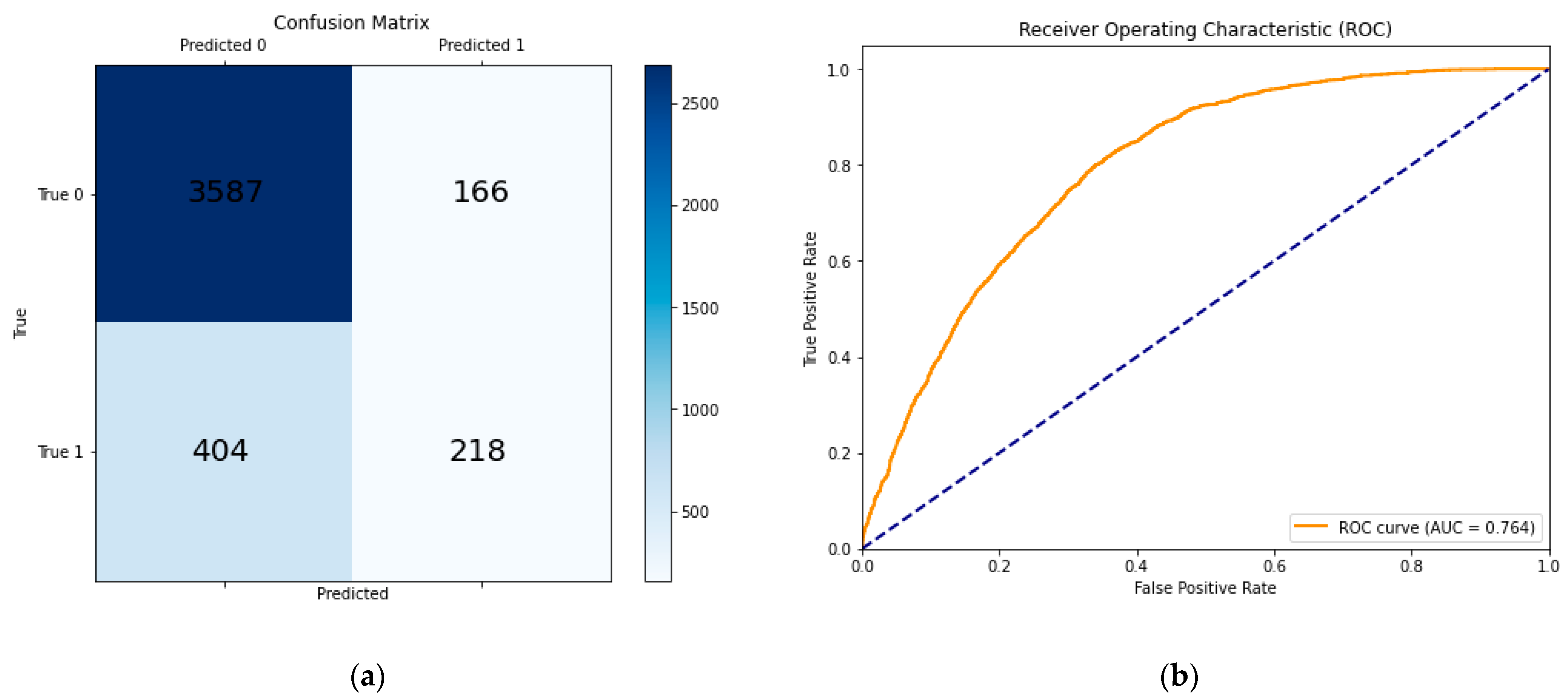
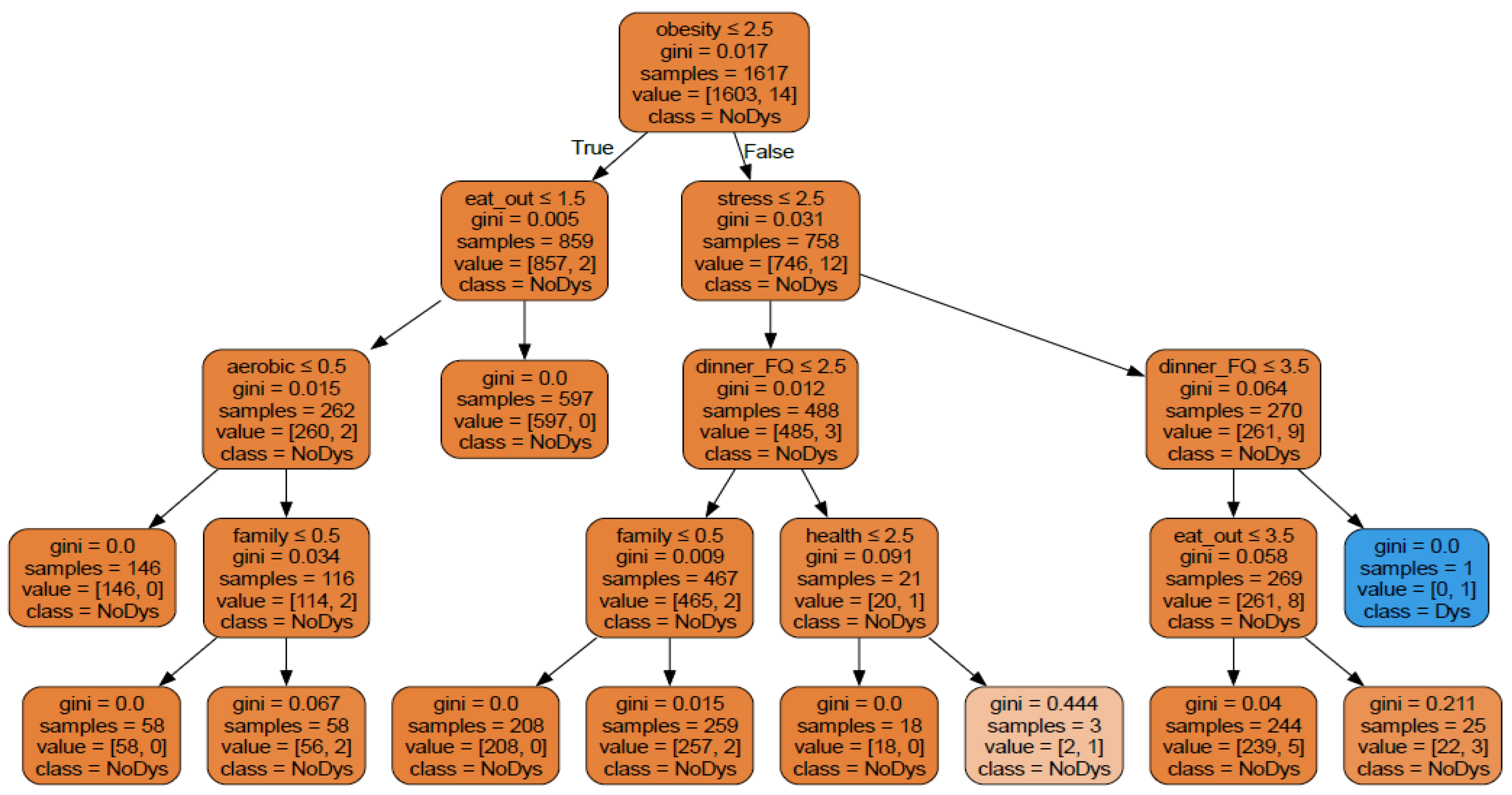
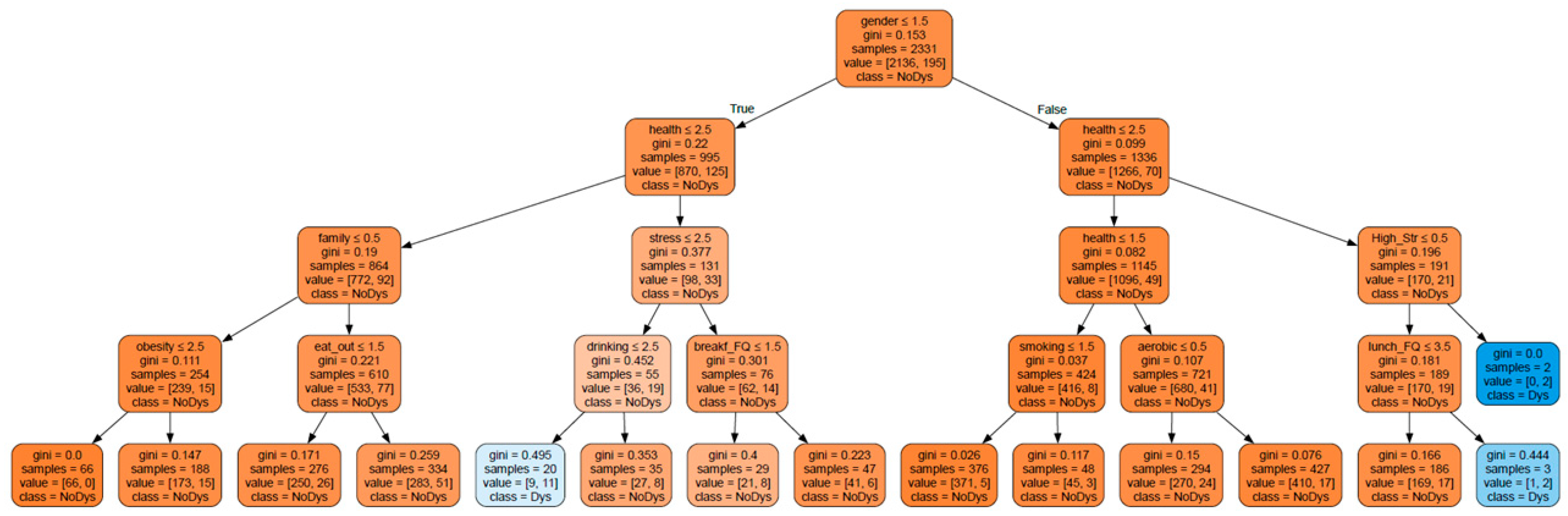
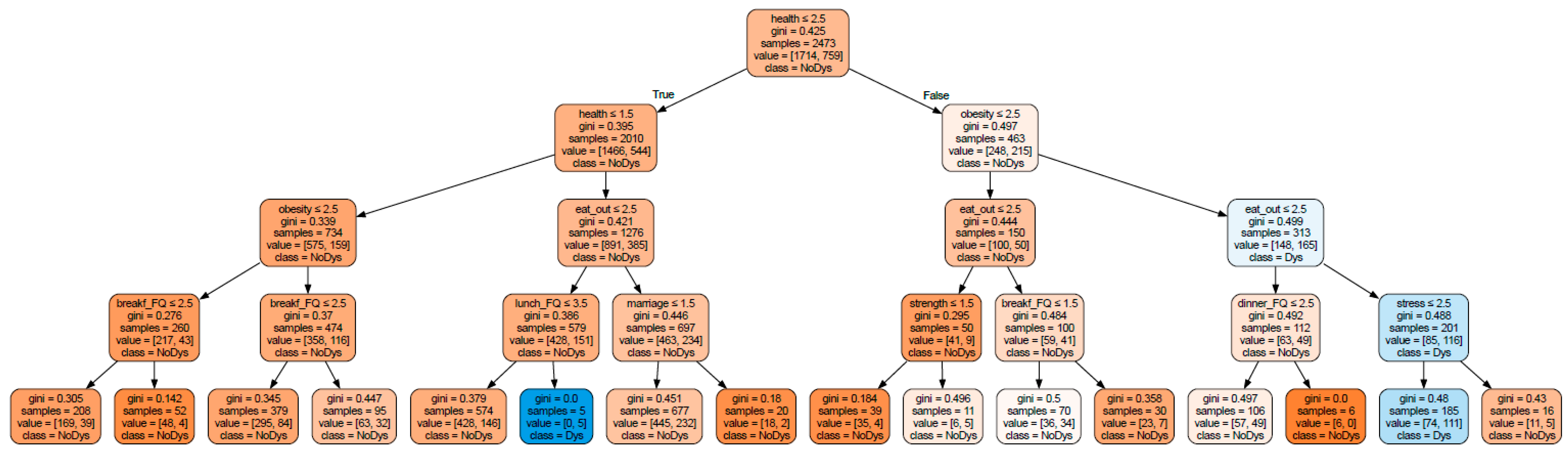
3.3. Prediction of Risk Factors for Dyslipidemia Based on Health Behavior by Age
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 1 October 2024).
- Korea Disease Control and Prevention Agency. National Health Information Portal, Dislipidemia. Available online: https://health.kdca.go.kr/healthinfo/biz/health/gnrlzHealthInfo/gnrlzHealthInfo/gnrlzHealthInfoView.do?cntnts_sn=6054 (accessed on 1 October 2024).
- Kim, H.C.; Oh, S.M. Noncommunicable diseases: Current status of major modifiable risk factors in Korea. J. Prev. Med. Public Health 2013, 46, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.C. Epidemiology of dyslipidemia in Korea. J. Korean Med. Assoc. 2016, 59, 352–357. [Google Scholar] [CrossRef]
- Korean Society of Lipid Atherosclerosis. The Committee of Clinical Practice Guideline of Korean Guidelines for the Management of Dyslipidemia, 4th ed.; The Korean Society of Lipid and Atherosclerosis: Seoul, Republic of Korea, 2018; pp. 31–33. [Google Scholar]
- Cha, B.K. Risk Factors affecting Dyslipidemia according to Age Group in Women: Data from the Korea National Health and Nutrition Examination Survey, 2014~2017. J. Korean Acad. Fundam. Nurs. 2020, 27, 310–322. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, M.H.; Shim, J.S.; Choi, D.P.; Song, B.M.; Lee, S.W.; Choi, H.; Kim, H.C. Effects of age, sex, and menopausal status on lood cholesterol profile in the Korean population. Korean Circ. J. 2015, 45, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Opoku, S.; Gan, Y.; Fu, W.; Chen, D.; Emmanuel, A.Y.; Trofimovitch, D.; Yue, W.; Yan, F.; Wang, Z.; Lu, Z. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: Findings from the China National Stroke Screening and prevention project (CNSSPP). BMC Public Health 2019, 19, 1500. [Google Scholar] [CrossRef] [PubMed]
- Yoo, L.H.; Baik, D.I.; Lee, M.J. Relationship between age-specific practicing of a healthy diet and dyslipidemia in Korean Adults: A study of Korean adults without diagnosed cardiovascular disease. J. Korea Acad.-Ind. Coop. Soc. 2023, 24, 387–397. [Google Scholar] [CrossRef]
- Choi, W.H.; Seo, Y.M.; Jeon, M.Y.; Choi, S.Y. Convergence Study on the Comparison of Risk Factors for Dyslipidemia by Age and Gender: Based on the Korea National Health and Nutrition Examination Survey (2013~2015 year). J. Korea Converg. Soc. 2018, 9, 571–587. [Google Scholar] [CrossRef]
- Jeong, J.H.; Choi, Y.S.; Kim, S.M.; Choi, S.Y.; Kim, J.E.; Kim, E.Y.; Lee, H.Y.; Jung, J.H.; Jin, R. Correlation between Physical Activity Status and Dyslipidemia in Korean Adults: The 2010 Korea National Health and Nutrition Examination Survey. Korean J. Geriatr. Gerontol. 2014, 15, 35–44. [Google Scholar] [CrossRef]
- Han, I.H.; Chong, M.Y. The Study on the Difference of Blood Level of HDL-Cholesterol by Obesity and Health Behavior from the Seventh (2016) Korea National Health and Nutrition Examination Survey. J. Korea Soc. Food Sci. Nutr. (JFKN) 2020, 49, 1377–1388. [Google Scholar] [CrossRef]
- Korea Centers of Disease Control and Prevention. Sampling Design of the 6th KNHNES and Weighting Adjustment of the 8th KNHNES. Available online: https://knhanes.kdca.go.kr/knhanes/main.do (accessed on 20 April 2024).
- Cox, D.R. The regression analysis of binary sequences. J. R. Stat. Soc. Ser. B (Methodol.) 1958, 20, 215–232, Correction in: J. R. Stat. Soc. Ser. B (Methodol.) 2018, 21, 238. [Google Scholar] [CrossRef]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; Wadsworth International Group: Belmont, CA, USA, 1984; pp. 237–251. [Google Scholar]
- Long, W.J.; Griffith, J.L.; Selker, H.P.; D’Agostino, R.B. A comparison of logistic regression to decision-tree induction in a medical domain. Comput. Biomed. Res. 1993, 26, 74–97. [Google Scholar] [CrossRef] [PubMed]
- Rudolfer, S.M.; Paliouras, G.; Peers, I.S. comparison of logistic regression to decision tree induction in the diagnosis of carpal tunnel syndrome. Comput. Biomed. Res. 1999, 32, 391–414. [Google Scholar] [CrossRef] [PubMed]
- QuantDare. Available online: https://quantdare.com/decision-trees-gini-vs-entropy (accessed on 15 December 2024).
- Scikit-Learn Machine Learning in Python. Available online: https://scikit-learn.org/stable/modules/tree.html (accessed on 20 February 2025).



| Variables and Categories | 19–34 (%) | p | 35–49 (%) | p | 50–64 (%) | p | ≥65 (%) | p | Rao-Scott χ2 (p) |
|---|---|---|---|---|---|---|---|---|---|
| Gender Male Female | 4.734 | ||||||||
| 1110 (48.1) | 0.350 | 1428 (42.9) | 0.390 | 1544 (43.7) | 0.005 | 1521 (53.3) | <0.001 | (<0.004) | |
| 1200 (51.9) | 1902 (57.1) | 1989 (56.3) | 1334 (46.7) | ||||||
| Marital status Married Not married | 1347.042 | ||||||||
| 512 (22.2) | <0.001 | 2925 (87.8) | <0.001 | 3396 (96.1) | <0.001 | 2833 (99.2) | <0.001 | (<0.001) | |
| 1798 (77.8) | 405 (12.2) | 137 (3.9) | 22 (0.8) | ||||||
| Household income Low Middle High | 158.485 | ||||||||
| 416 (18.0) | <0.001 | 533 (16.0) | <0.001 | 830 (23.5) | <0.001 | 1815 (63.6) | <0.001 | (<0.001) | |
| 506 (21.9) | 824 (24.7) | 735 (20.8) | 445 (15.6) | ||||||
| 1388 (60.1) | 1973 (59.2) | 1968 (55.7) | 595 (20.8) | ||||||
| Education level ≤Middle school graduate High school graduate ≥College graduate | 486.545 | ||||||||
| 31 (1.3) | <0.001 | 97 (2.9) | <0.001 | 897 (25.4) | <0.001 | 1918 (67.2) | <0.001 | (<0.001) | |
| 1040 (45.0) | 1057 (31.7) | 1487 (42.1) | 597 (20.9) | ||||||
| 1239 (53.6) | 2176 (65.3) | 1149 (32.5) | 340 (11.9) | ||||||
| Subjective health status Good Normal Bad | 35.501 | ||||||||
| 967 (41.9) | <0.001 | 1095 (32.9) | <0.001 | 1027 (29.1) | <0.001 | 742 (26.0) | <0.001 | (<0.001) | |
| 1053 (45.6) | 1781 (53.5) | 1827 (51.7) | 1358 (47.6) | ||||||
| 290 (12.6) | 454 (13.6) | 679 (19.2) | 755 (26.4) | ||||||
| BMI Underweight Healthy weight Obesity | 39.149 | ||||||||
| 199 (8.6) | <0.001 | 130 (3.9) | 0.006 | 82 (2.3) | <0.001 | 76 (2.7) | <0.001 | (<0.001) | |
| 1023 (44.3) | 1277 (38.3) | 1230 (34.8) | 920 (32.2) | ||||||
| 1088 (47.1) | 1923 (57.7) | 2221 (62.9) | 1859 (65.1) | ||||||
| Family history No Yes | 59.417 | ||||||||
| 1578 (68.3) | <0.001 | 1988 (59.7) | <0.001 | 2084 (59.0) | <0.001 | 1551 (54.3) | <0.001 | (<0.001) | |
| 732 (31.7) | 1342 (40.3) | 1449 (41.0) | 1304 (45.7) | ||||||
| Dyslipidemia No Yes | 392.767 | ||||||||
| 2288 (99.0) | <0.001 | 3052 (91.7) | <0.001 | 2448 (69.3) | <0.001 | 1732 (60.7) | <0.001 | (<0.001) | |
| 22 (1.0) | 278 (8.3) | 1085 (30.7) | 1123 (39.3) |
| Variables and Categories | 19–34 (%) | p | 35–49 (%) | p | 50–64 (%) | p | ≥65 (%) | p | Rao-Scott χ2 (p) |
|---|---|---|---|---|---|---|---|---|---|
| Drinking alcohol No drinking Once a month 2–4 times a month 2–3 times a week ≥4 times a week | 38.607 | ||||||||
| 758 (32.8) | <0.001 | 1207 (36.2) | <0.001 | 1641 (46.4) | <0.001 | 1594 (55.8) | <0.001 | (<0.001) | |
| 372 (16.1) | 396 (11.9) | 379 (10.7) | 253 (8.9) | ||||||
| 758 (32.8) | 874 (26.2) | 726 (20.5) | 433 (15.2) | ||||||
| 345 (14.9) | 639 (19.2) | 512 (14.5) | 348 (12.2) | ||||||
| 77 (3.3) | 214 (6.4) | 275 (7.8) | 227 (8.0) | ||||||
| Smoking (lifetime) Never smoked Less than 5 packs More than 5 packs | 35.910 | ||||||||
| 1455 (63.0) | <0.001 | 1892 (56.8) | <0.001 | 2033 (57.5) | <0.001 | 1522 (53.3) | <0.001 | (<0.001) | |
| 123 (5.3) | 96 (2.9) | 51 (1.5) | 29 (1.0) | ||||||
| 732 (31.7) | 1342 (40.3) | 1449 (41.0) | 1304 (45.7) | ||||||
| Stress perception Feel a lot Feel a little Do not feel | 80.621 | ||||||||
| 808 (35.0) | <0.001 | 1101 (33.1) | <0.001 | 815 (23.1) | <0.001 | 446 (15.6) | <0.001 | (<0.001) | |
| 1251 (54.2) | 1944 (58.4) | 2206 (62.4) | 1625 (56.9) | ||||||
| 251 (10.9) | 285 (8.6) | 512 (14.5) | 784 (27.5) | ||||||
| High-intensity physical activity None 1 h More than 2 h | 0.058 | 0.149 | 0.277 | <0.001 | 4.456 | ||||
| 2280 (98.7) | 3288 (98.7) | 3507 (99.3) | 2853 (99.9) | (<0.001) | |||||
| 24 (1.0) | 30 (0.9) | 18 (0.5) | 1 (0.0) | ||||||
| 6 (0.3) | 12 (0.4) | 8 (0.2) | 1 (0.0) | ||||||
| Medium-intensity physical activity None 1 h More than 2 h | <0.001 | <0.001 | <0.001 | <0.001 | 10.901 | ||||
| 2161 (93.5) | 3114 (93.5) | 3409 (96.5) | 2796 (97.9) | (<0.001) | |||||
| 118 (5.1) | 158 (4.7) | 85 (2.4) | 42 (1.5) | ||||||
| 31 (1.3) | 58 (1.7) | 39 (1.1) | 17 (0.6) | ||||||
| Walking days None Less than 5 days More than 5 days | <0.001 | <0.001 | <0.001 | <0.001 | 24.055 | ||||
| 718 (31.1) | 799 (24.0) | 993 (28.1) | 983 (34.4) | (<0.001) | |||||
| 1057 (45.8) | 1936 (58.1) | 1951 (55.2) | 1461 (51.2) | ||||||
| 535 (23.2) | 595 (17.9) | 589 (16.7) | 411 (14.4) | ||||||
| Walking duration None 1 h More than 2 h | <0.001 | <0.001 | <0.001 | 0.004 | 10.715 | ||||
| 1485 (64.3) | 2137 (64.2) | 1999 (56.6) | 1723 (60.4) | (<0.001) | |||||
| 613 (26.5) | 850 (25.5) | 1060 (30.0) | 761 (26.7) | ||||||
| 212 (9.2) | 343 (10.3) | 474 (13.4) | 371 (13.0) | ||||||
| Strength training days None Less than 3 days More than 3 days | <0.001 | <0.001 | 0.207 | 0.004 | 9.599 | ||||
| 0 (0.0) | 1 (0.0) | 0 (0.0) | 5 (0.2) | (<0.001) | |||||
| 1815 (78.6) | 2865 (86.0) | 2910 (82.4) | 2280 (79.9) | ||||||
| 495 (21.4) | 464 (13.9) | 623 (17.6) | 570 (20.0) | ||||||
| Aerobic exercise Non-practiced Practiced | <0.001 | 0.623 | <0.001 | <0.001 | 69.304 | ||||
| 1007 (43.6) | 1810 (54.4) | 2063 (58.4) | 1915 (67.1) | (<0.001) | |||||
| 1303 (56.4) | 1520 (45.6) | 1470 (41.6) | 940 (32.9) |
| Variables and Categories | 19–34 (%) | p | 35–49 (%) | p | 50–64 (%) | p | ≥65 (%) | p | Rao-Scott χ2 (p) |
|---|---|---|---|---|---|---|---|---|---|
| Breakfast Frequency Almost Never 1–2 times a week 3–4 times a week 5–7 times a week | 215.485 | ||||||||
| 838 (36.3) | <0.001 | 825 (24.8) | <0.001 | 436 (12.3) | <0.001 | 104 (3.6) | <0.001 | (<0.001) | |
| 541 (23.4) | 609 (18.3) | 288 (8.2) | 64 (2.2) | ||||||
| 352 (15.2) | 440 (13.2) | 283 (8.0) | 66 (2.3) | ||||||
| 579 (25.1) | 1456 (43.7) | 2526 (71.5) | 2621 (91.8) | ||||||
| Lunch Frequency Almost Never 1–2 times a week 3–4 times a week 5–7 times a week | 7.988 | ||||||||
| 37 (1.6) | <0.001 | 61 (1.8) | 0.055 | 82 (2.3) | <0.001 | 90 (3.2) | <0.001 | (<0.001) | |
| 66 (2.9) | 97 (2.9) | 75 (2.1) | 50 (1.8) | ||||||
| 191 (8.3) | 227 (6.8) | 149 (4.2) | 99 (3.5) | ||||||
| 2016 (87.3) | 2945 (88.4) | 3227 (91.3) | 2616 (91.6) | ||||||
| Dinner Frequency Almost Never 1–2 times a week 3–4 times a week 5–7 times a week | 18.498 | ||||||||
| 21 (0.9) | <0.001 | 27 (0.8) | 0.036 | 25 (0.7) | <0.001 | 21 (0.7) | <0.001 | (<0.001) | |
| 55 (2.4) | 89 (2.7) | 65 (1.8) | 30 (1.1) | ||||||
| 271 (11.7) | 293 (8.8) | 169 (4.8) | 68 (2.4) | ||||||
| 1963 (85.0) | 2921 (87.7) | 3274 (92.7) | 2736 (95.8) | ||||||
| Dining out Almost never 1–3 times a month 1–4 times a week 5–6 times a week More than once a day | 162.134 | ||||||||
| 758 (32.8) | <0.001 | 1207 (36.2) | <0.001 | 1641 (46.4) | <0.001 | 1594 (55.8) | <0.001 | (<0.001) | |
| 372 (16.1) | 396 (11.9) | 379 (10.7) | 253 (8.9) | ||||||
| 758 (32.8) | 874 (26.2) | 726 (20.5) | 433 (15.2) | ||||||
| 345 (14.9) | 639 (19.2) | 512 (14.5) | 348 (12.2) | ||||||
| 77 (3.3) | 214 (6.4) | 275 (7.8) | 227 (8.0) |
| Variables | Coef | Std Err | z | p > |z| | [0.025 (CI) | 0.975] (CI) | Odds Ratio |
|---|---|---|---|---|---|---|---|
| Age | 0.4732 | 0.045 | 10.629 | 0.000 *** | 0.386 | 0.560 | 1.605178 |
| Gender | −0.1400 | 0.081 | −1.724 | 0.085 | −0.299 | 0.019 | 0.869377 |
| Marital Status | −1.9933 | 0.188 | −10.586 | 0.000 *** | −2.362 | −1.624 | 0.136242 |
| Subjective health status | 0.3594 | 0.049 | 7.376 | 0.000 *** | 0.264 | 0.455 | 1.432420 |
| Drinking alcohol | −0.1432 | 0.026 | −5.588 | 0.000 *** | −0.193 | −0.093 | 0.866616 |
| Smoking | −0.1478 | 0.083 | −1.776 | 0.076 | −0.311 | 0.015 | 0.862626 |
| Stress perception | 0.0687 | 0.052 | 1.311 | 0.190 | −0.034 | 0.171 | 1.071074 |
| BMI | 0.3900 | 0.059 | 6.647 | 0.000 *** | 0.275 | 0.505 | 1.477005 |
| Family history | 0.3741 | 0.072 | 5.231 | 0.000 *** | 0.234 | 0.514 | 1.453676 |
| Breakfast frequency | −0.1305 | 0.034 | −3.839 | 0.000 *** | −0.197 | −0.064 | 0.877618 |
| Lunch frequency | −0.0807 | 0.058 | −1.392 | 0.164 | −0.194 | 0.033 | 0.922498 |
| Dinner frequency | −0.1578 | 0.084 | −1.874 | 0.061 | −0.323 | 0.007 | 0.853980 |
| Dining out | −0.1008 | 0.031 | −3.295 | 0.001 *** | −0.161 | −0.041 | 0.904153 |
| High-intensity activity | −0.0934 | 0.316 | −0.296 | 0.767 | −0.712 | 0.525 | 0.910874 |
| Medium-intensity activity | −0.1323 | 0.123 | −1.071 | 0.284 | −0.374 | 0.110 | 0.876100 |
| Aerobic exercise | −0.2139 | 0.070 | −3.055 | 0.002 *** | −0.351 | −0.077 | 0.807455 |
| Strength training days | 0.0185 | 0.043 | 0.428 | 0.668 | −0.066 | 0.103 | 1.018680 |
| Walking days | −0.0346 | 0.048 | −0.717 | 0.473 | −0.129 | 0.060 | 0.965952 |
| Walking duration | 0.0406 | 0.047 | 0.866 | 0.387 | −0.051 | 0.132 | 1.041410 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, J.-H.; Kim, J.-S.; Kim, K.-H. Predicting Risk Factors for Dyslipidemia Based on Health Behaviors by Age in Adults Using Machine Learning. Appl. Sci. 2025, 15, 5131. https://doi.org/10.3390/app15095131
Ku J-H, Kim J-S, Kim K-H. Predicting Risk Factors for Dyslipidemia Based on Health Behaviors by Age in Adults Using Machine Learning. Applied Sciences. 2025; 15(9):5131. https://doi.org/10.3390/app15095131
Chicago/Turabian StyleKu, Jin-Hui, Jong-Suk Kim, and Kwang-Hwan Kim. 2025. "Predicting Risk Factors for Dyslipidemia Based on Health Behaviors by Age in Adults Using Machine Learning" Applied Sciences 15, no. 9: 5131. https://doi.org/10.3390/app15095131
APA StyleKu, J.-H., Kim, J.-S., & Kim, K.-H. (2025). Predicting Risk Factors for Dyslipidemia Based on Health Behaviors by Age in Adults Using Machine Learning. Applied Sciences, 15(9), 5131. https://doi.org/10.3390/app15095131





