Featured Application
This study provides a quantitative assessment of the environmental impact of minimally invasive nephrectomy, demonstrating that robot-assisted surgery produces lower CO2 emissions than laparoscopic surgery. These findings support the adoption of reusable surgical instruments and energy-efficient practices in operating rooms. The results can guide policymakers, hospital administrators, and surgical teams in implementing greener surgical protocols, reducing the carbon footprint of healthcare without compromising patient outcomes.
Abstract
Background: Minimally invasive surgery has improved patient outcomes but raises environmental concerns due to carbon emissions from disposable instruments, energy consumption, and hospital resource use. This study evaluates the carbon footprint of robot-assisted and laparoscopic nephrectomies. Methods: A multicenter prospective study analyzed 162 patients undergoing robot-assisted or laparoscopic partial (RAPN, LPN) and radical nephrectomy (RARN, LRN). Life cycle assessment (LCA) quantified CO2 emissions from instrument use, sterilization, and energy consumption. Results: Robot-assisted procedures had lower CO2 emissions than laparoscopic approaches. Emissions from instrument disposal were 9.04 kg in RAPN vs. 12.14 kg in LPN (p = 0.02) and 8.74 kg in RARN vs. 11.45 kg in LRN (p = 0.03). Despite higher intraoperative energy use, robot-assisted surgery produced 3–4 kg less CO2 per procedure due to reusable instruments and shorter hospitalization. Conclusions: Robot-assisted nephrectomy reduces environmental impact by minimizing waste and hospital stays. Efforts should focus on reusable instruments, energy efficiency, and sustainability initiatives to mitigate surgical carbon footprints while ensuring high-quality care.
1. Introduction
Minimally invasive surgery (MIS) has led to significant advancements in the field of abdominal, thoracic, orthopedic, and head and neck surgery over the past three decades, with numerous advantages over the open approach, such as faster recovery, shorter hospital stays, less postoperative pain, and more aesthetic results [1,2,3,4,5]. Reports show that the number of MIS procedures has dramatically increased in the past 20 years. In 2020, it was reported that 14 million laparoscopic procedures were performed worldwide, which is associated with an estimated global expenditure of 13.7 billion USD/year on laparoscopic instruments and devices [6]. Moreover, owing to recent advances in robot-assisted surgery, the number of robot-assisted procedures is exponentially increasing due to several factors, such as a shorter learning curve [7]. MIS has been embraced in urology (radical prostatectomy, partial nephrectomy (PN) and radical nephrectomy (RN), radical cystectomy (RC) with continent or non-continent urinary derivations [8,9]), general surgery (cholecystectomy, appendicectomy, bariatric surgery, colectomy, etc.) [10,11,12], and gynecology [13]. In the past, surgeons were more likely to use disposable laparoscopic instruments to establish sterility or to avoid failure of reusable tools. However, expenditures on disposable laparoscopic instruments are generally higher than those on reusable instruments, considering decontamination, repair, and replacement costs. In 2019, more than 4% of worldwide net greenhouse gas (GHG) emissions depended on the healthcare sector [14]. In contrast, the utilization of disposable instruments represents the major hotspots for CO2 emissions within operating rooms (ORs) [15]. The most common measure used to calculate environmental damage is carbon footprint (CF), and GHG emissions associated with a product, process, or system are equated and summed as CO2 equivalents. Several studies have proven that reusable instruments in the OR setting have less environmental impact than their single-use counterparts, including instruments such as scissors, gowns and drapes, laparotomy pads, sharp containers, and a vast array of anesthetic items, such as anesthetic drug trays, laryngeal masks, airways, laryngoscope handles, and blades [16,17,18,19,20,21,22]. Hybrid instruments, also called “reposable instruments” or “modular systems”, are mainly reusable but have some disposable components. As a result, these devices are likely to reduce the environmental impact and cost of single-use laparoscopic instruments. However, despite evidence supporting the environmental benefits of reusable instruments, many centers, including those in this study, rely on single-use tools due to sterility protocols, maintenance concerns, and administrative procurement preference. In this context, we hypothesize that robot-assisted nephrectomy has a lower CF than laparoscopic nephrectomy, primarily due to reduced reliance on single-use instruments and shorter hospital stays. This study aims to assess the environmental impact of minimally invasive surgery by comparing the CO2 emissions of laparoscopic and robot-assisted procedures. Using the GHG protocol and life cycle assessment (LCA) methodology, we evaluate the CF associated with surgical instruments and overall energy consumption for both RN and PN performed in two tertiary referral centers.
2. Materials and Methods
2.1. Study Design
This multicenter prospective comparative study aimed to evaluate the environmental impact of robot-assisted PN (RAPN), laparoscopic PN (LPN), robot-assisted RN (RARN), and laparoscopic RN (LRN). The analysis used an LCA to quantify CO2 emissions associated with surgical procedures, instrument use, and hospitalization. The study was conducted across two tertiary centers, with standardized protocols for surgical and environmental data collection (the Urology Department of ICOT in Latina and Sant’Andrea Hospital in Roma, both at the Sapienza University of Rome). The robot-assisted procedures were performed using the Robot Xi da Vinci surgical system, while the 3D laparoscopic system by Karl Storz was used for laparoscopic surgery.
2.2. Study Population
The study included patients diagnosed with renal tumors eligible for PN or RN. Inclusion criteria required tumors staged ≤T3a based on clinical and imaging evaluations. Patients were excluded if they required conversion to open surgery, underwent emergency surgical cases, had incomplete LCA data or missing instrument weights and energy consumption metrics, or presented significant comorbidities affecting hospitalization duration, such as advanced cardiovascular disease. Participants were divided into four groups based on the surgical approach and procedure type; Group A included patients undergoing RAPN, Group B underwent LPN, Group C underwent RARN, and Group D underwent LRN. Patients were not randomized but assigned based on the availability of robotic systems and surgeon–patient discussion. All surgeons involved had extensive experience (>150 cases each) in all four procedures.
2.3. Data Collection
Various patient data were assessed, including age, BMI, medical [diabetes mellitus (DM), metabolic syndrome (MS)] and surgical history, tumor stage, RENAL score [23], preoperative Hb and mean Hb drop, pre- and postoperative eGFRs, operative time, estimated blood loss (EBL), and hospital stay. Environmental metrics evaluated instrument weights by material (plastic, metal, composite fibers), energy consumption for surgical equipment, OR, hospital rooms, and CO2 emissions from the production, decontamination, and disposal of instruments. All data used for the analysis were derived from routine clinical documentation and operative reports. No additional data collection procedures were implemented, and the clinical workflow was not affected.
2.4. CO2 Consumption
The first step in estimating the CO2 emissions related to robot-assisted and laparoscopic procedures was to categorize the contributing components into emission scopes, following the GHG protocol. Scope 1 emissions include direct emissions from sources, such as CO2 used during surgical procedures for insufflation. Under normal conditions, CO2 escapes into the atmosphere directly through port site leaks, decompression at the end of surgery, or inadvertently. Indirectly, CO2 absorbed by intra-abdominal organs during surgery is later eliminated through the respiratory system. Scope 2 emissions encompass indirect emissions resulting from electricity generation, the disposal of single-use devices, and energy required for the heating, cooling, production, and sterilization of instruments. To contextualize, a typical CO2 cylinder used in our ORs contains compressed gas. Using the ideal gas law, where 1 mol of any gas occupies 22.4 L at 1 atm and weighs 44 g, each cylinder contains approximately 1.5 × 10−4 metric tons of CO2. We estimated the operative time and the corresponding CO2 consumption for robot-assisted and laparoscopic procedures by calculating the duration of surgeries and CO2 use per cylinder.
2.5. Life Cycle Assessment
The life cycle assessment (LCA) methodology provides a comprehensive framework for assessing environmental impact across all product lifecycle stages, from raw material extraction to disposal. This approach allows for identifying the critical points of environmental burden and opportunities for sustainable intervention. In this study, the LCA followed ISO 14044 guidelines [24] and included a “door-to-door” analysis.
2.5.1. Raw Material Extraction and Manufacturing
In our analysis, we assessed the composition of surgical instruments, quantifying the plastic, metal, and composite fiber components to calculate their associated CO2 emissions. Notably, producing 1 kg of steel requires approximately 14–16 kWh of energy at a melting temperature of 1.435 °C, emitting around 9 kg of CO2. In contrast, recycling the same amount of steel consumes only about 0.8 kWh, significantly reducing emissions. Plastic components, predominantly derived from fossil fuels, were also evaluated for their emissions during production and disposal. In 2019, virgin plastic production was responsible for approximately 2.24 billion metric tons of CO2 equivalent, accounting for 5.3% of total greenhouse gas emissions [25].
2.5.2. Use Phase
Our analysis evaluated the energy consumption during surgical procedures for both robot-assisted and laparoscopic systems. Additionally, we considered hospital infrastructure demands, including heating, cooling, and lighting, correlated with each patient’s length of stay. Studies have shown that energy consumption in inpatient departments is directly related to the number of hospital days, with an increase of 12.2 kWh/m2 for every 1.000 additional hospital days [26].
2.5.3. End-of-Life Disposal and Reusability
In our analysis, we compared the environmental impacts of single-use devices to reusable instruments, modeling reusable components to undergo 15 sterilization cycles with corresponding energy and material inputs. Studies indicate that single-use items often have a greater environmental impact from raw material extraction and manufacturing than reusables [27]. However, the environmental impact of reusable items primarily occurs during the use phase, particularly in the energy-intensive processes of washing and steam sterilization. Additionally, we calculated CO2 emissions from waste disposal for all instrument components, including those that could not be recycled.
2.6. Surgical Procedure
The same surgical technique was used for both the robot-assisted and laparoscopic approaches, and the same team of expert surgeons (>100 procedures in all 4 techniques) performed all the procedures in both institutions. All procedures were performed with a transperitoneal approach. Pneumoperitoneum at 12 mmHg was achieved through a Verres needle with a standard CO2 insufflator with no AirSeal system in robot-assisted procedures. Hasson’s open technique and Hasson’s trocar were used to achieve pneumoperitoneum in the laparoscopic procedures. PN procedures were performed off-clamp, and the renal pedicle was always prepared. In laparoscopic procedures, four single-use trocars were used, while in RARN, three 8 mm multiuse robotic trocars and one 12 mm single-use trocar were utilized, and for RAPN, four multiuse robotic trocars and 12 mm and 5 mm single-use trocars were utilized.
2.7. Statistical Analysis
Descriptive statistics were used to summarize patient demographics, surgical details, and environmental metrics. Continuous variables and standard deviations (SD). Categorical variables were expressed as percentages. Differences between groups were analyzed using the Student’s t-test for continuous variables and the chi-squared test for categorical variables. A p-value < 0.05 was considered statistically significant. All analyses were conducted using SPSS Statistics (version 27.0; IBM Corp., Armonk, NY, USA).
3. Results
The analysis included 41 patients in the RAPN (Group A) group and 38 in the LPN (Group B) group. Baseline characteristics, including age, BMI, diabetes mellitus (DM), metabolic syndrome (MS), and preoperative eGFR, were comparable between the two groups (p > 0.05). RAPN demonstrated a shorter operative time compared to LPN (110.4 ± 35.7 vs. 124.8 ± 38.1 min, p = 0.04, 95% CI −30.71 to 1.91) and lower EBL (199.4 ± 68.1 mL vs. 220.8 ± 66.6 mL, p = 0.03, 95% CI −51.11 to 8.31). Mean hemoglobin drop and postoperative eGFR values at discharge did not differ significantly between the groups. The hospital stay was slightly shorter for RAPN, though the difference was not statistically significant. In the RN cohort, 40 patients underwent RARN (Group C), and 43 underwent LRN (Group D). No significant differences were observed in baseline characteristics, including age, BMI, DM, MS, and preoperative eGFR. Although RARN had a slightly shorter operative time than LRN (121.8 ± 41.1 min vs. 132.6 ± 49.4 min), this difference was not statistically significant (p = 0.4, 95% CI −30.3 to 8.7). EBL and mean hemoglobin drop were comparable between the two groups. Postoperative eGFR and hospital stay were similar, with no statistically significant differences. Table 1 summarizes patients’ baseline characteristics and pathological and surgical details.

Table 1.
Summary of patient baseline characteristics and pathological and surgical details, SD: standard deviation; Hb: hemoglobin, BMI: body mass index, DM: diabetes mellitus, MS: metabolic syndrome, eGFR: estimated glomerular filtration rate, N/A: not applicable. Comparisons are made within surgical subgroups: Group A vs. B for partial nephrectomy and Group C vs. D for radical nephrectomy.
3.1. Partial Nephrectomy
Supplementary Table S1 lists the instruments used in the PN groups, their relative weights, and CO2 production. Since the procedures in question are MIS, some instrumentation overlap existed. The total weight of the instruments utilized was 1669.4 g and 1637.4 g in groups A and B, respectively. In Group A, the plastic, metal, and composite fiber weights totaled 1225.2 g, 225.5 g, and 185.2 g, respectively. In Group B, the plastic, metal, and composite fiber weighed 1288.2 g, 152.5 g, and 133.2 g, respectively. The CO2 emissions resulting from the production, disposal, and sterilization of the instruments were overall higher in Group B (12.14 kg vs. 9.04 kg, p = 0.02, 95% CI −4.04 to −2.16), with the majority of the emissions deriving from the plastic (Group B 8.37 kg vs. Group A 6.14 kg p = 0.01, 95% CI −2.87 to −1.59). The emissions from the metal and composite fiber components were higher in Group B, but the difference was not statistically significant. Summary statistics for instrument CO2 consumption are summarized in Table 2.

Table 2.
Weights and CO2 emissions of the partial nephrectomy groups. g: grams; kg: kilograms; CO2: carbon dioxide.
The power required for the robotic Xi Da Vinci system to function equals 3.5 kW/h, and considering an average surgical procedure time for RAPN in our institutions of 1.84 h, the resulting average CO2 emissions equaled 2.27 kg in Group A. In contrast, in Group B, the laparoscopic Storz column operates at 0.6 kW/h, emitting 0.44 kg of CO2 in 2.08 h of surgical time (p = 0.001, 95% CI −1.69 to 1.97). The power required for the OR to function equals to 3.0 kW/h, with the average time spent in it being 2.74 h in Group A and 3.1 h in Group B, with CO2 emissions being higher in Group B (3.27 kg vs. 2.89 kg). The power required for a standard hospital room differs between summer and winter, with more power required in summer than in winter (0.75 kW/h vs. 0.6 kW/h, respectively) due to ventilation and air conditioning. On average, patients required 56.6 and 62.3 h of hospital stay in Groups A and B, respectively. In the winter, the CO2 emissions were 11.97 kg and 13.17 in Groups A and B, respectively, and in the summer, they were 14.97 kg and 16.46 kg (p = 0.04, 95% CI −2.87 to −0.11) in Groups A and B, respectively. The total CO2 emissions from energy consumption were 32.1 kg in Group A and 33.34 kg in Group B (Table 3).

Table 3.
Summary of CO2 emissions deriving from energy consumption. kW: kilowatt; h: hour; m2: meters squared; OR: operative room; °C: degrees Celsius; Kg: kilograms; CO2: carbon dioxide. Values are expressed in kg of CO2 emissions with 95% CI.
3.2. Radical Nephrectomy
Supplementary Table S2 lists the instruments used in the RN groups, their relative weights, and CO2 production. As for the PN group, there was a degree of overlap in instrumentation. The total weight of the instruments utilized equaled 1471.09 g and 1501.45 g in Groups C and D, respectively. The plastic, metal, and composite fiber weights were 1130.2 g, 182.64 g, and 154.25 g, respectively, in Group C. In comparison, they were 1188.2 g, 147 g, and 133.25 g, respectively, in Group D. The CO2 emissions resulting from the production, disposal, and sterilization of the instruments equaled 8.74 kg and 11.45 kg in Groups C and D, respectively. Overall, the CO2 emissions per single component were higher in Group D, with plastics representing the major CO2 contributor (Group D 7.72 kg vs. Group C 5.9 kg, p = 0.02, 95% CI −2.42 to −1.22). The CO2 emissions from the metal and composite fiber components were higher in Group D, but the difference was not statistically significant (Table 4).

Table 4.
Weights and CO2 emissions of the radical nephrectomy groups. g: grams; kg: kilograms, CO2: carbon dioxide.
The average surgery time was 2.03 and 2.21 h in Groups C and D, respectively, resulting in CO2 emissions of 2.5 and 0.47 kg, respectively. The mean OR occupation time was 2.9 h in Group C and 3.19 h in Group D, resulting in CO2 emissions of 3.06 kg and 3.37 kg, respectively. The mean hospital stay was 54.3 h in Groups C and D, respectively, with emissions of 11.48 kg and 12.56 kg of CO2 in the winter and summer, respectively, in Group C and emissions of 14.35 kg in the winter and 15.7 in the summer in Group D (p = 0.04, 95% CI −2.77 to −0.13) (Table 5).

Table 5.
Summary of CO2 emissions deriving from energy consumption. kW: kilowatt; h: hour; m2: meters squared; OR: operative room; °C: degrees Celsius; Kg: kilograms; CO2: carbon dioxide. Values are expressed in kg of CO2 emissions with 95% confidence intervals.
3.3. Total CO2 Emissions
The total CO2 emissions in the PN groups equaled 41.14 kg per procedure in Group A, of which 9.04 kg was derived from instrument production, disposal, and sterilization and 32.1 kg from energy consumption. The CO2 emissions in Group B equaled 45.48 kg, with 12.14 kg from instrument use and 33.34 kg from energy consumption (p = 0.024, 95% CI −8.14 to −0.54). In Groups C and D, total CO2 emissions equaled 40.9 kg and 43.65, respectively (p = 0.03, 95% CI −7.23 to −0.11), with 8.7 kg and 12.14 kg deriving from instrument disposal in Groups C and D, respectively, and 31.39 kg and 32.2 kg deriving from energy consumption in Groups C and D, respectively (Figure 1).
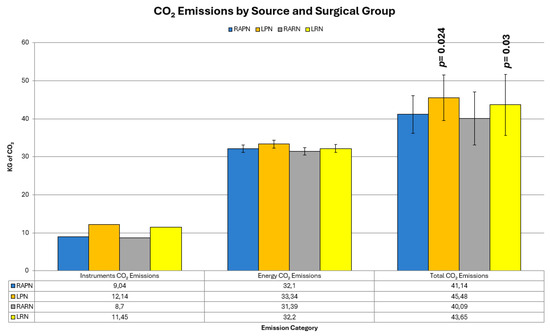
Figure 1.
Summary of CO2 emissions deriving from instrument use and energy consumption.
4. Discussion
The estimation of the CF of healthcare systems is a field of ever-growing interest and importance. The healthcare GHG footprint as a percentage of the national GHG footprint is 8–10% in the US [28,29], 3% in England [30,31], and 5% in Canada [32], thus representing a significant contributor in a country’s GHG emissions. Connor et al. published the first study assessing specialty-level CO2 emissions, quantifying the CF of a renal unit in a UK hemodialysis ward [33,34]. This growing interest in carbon reduction has also permeated healthcare policy; for instance, the UK National Health Service (NHS) has committed to becoming the world’s first “net zero” carbon national health service [6]. Surgical departments and operating theaters rank among hospitals’ most energy-intensive and waste-generating departments [35]. A recent systematic review by Kloevekorn et al. [36] identified several major sources of carbon emissions in surgical care, such as anesthetic gases, the sterilization processes, the use of disposable materials, and resistance to adopting greener practices among surgical staff.
Various strategies have been proposed to mitigate their environmental impact without compromising patient safety, including avoiding desflurane and adopting occupancy-based ventilation systems [37]. Building on this foundation, our initial study focused on prostate cancer [38]. To the best of our knowledge. This study was the first to compare CO2 emissions from two MIS approaches [6,39,40,41]. Notably, robot-assisted surgery demonstrated an 11% reduction in emissions compared to laparoscopy, saving 12.36 kg CO2 per procedure, equivalent to the emissions from driving 50 km in a petrol car [42]. These results prompted our group to investigate whether this trend was confirmed in MIS kidney surgery.
Similar to our previous study, the difference in CO2 emissions between the two robot-assisted procedures and the laparoscopic procedures was statistically significant due to the use of reusable materials and lower total energy consumption. RAPN and RARN produce on average 4 kg and 3 kg of CO2 less than their laparoscopic counterparts. Our findings highlight how the robot-assisted approach allows for the use of reusable instruments, as the main surgical instrumentation of the Da Vinci Xi System has a lifespan of up to 15 procedures. In contrast, laparoscopy relies heavily on single-use instruments in our institutions, resulting in higher energy consumption due to slightly longer surgical times and the need for closer postoperative monitoring. Single-use instruments, primarily composed of plastics, have a significantly higher CF than reusable instruments. In both laparoscopic arms of this study, the CO2 emissions from plastics alone accounted for ~1.8 and ~2.2 kg CO2. This discrepancy is largely attributed to the greater variety and quantity of single-use instruments required for laparoscopy. These results align with the existing literature [6], which emphasizes the advantages of hybrid instruments over single-use components. Although the per-case savings may seem modest, when multiplied across thousands of procedures in high-volume institutions, the cumulative environmental benefit could be substantial. While the robotic system consumes more energy intraoperatively compared to the laparoscopic column, the shorter hospitalization period compensated for this, leading to lower overall CO2 emissions. Initiatives like the “Power Down” program (turning off unused anesthesia and OR lights) have shown promise, saving USD 33,000 and reducing 234.3 metric tons of CO2 annually [42]. While we acknowledge that both hybrid and reusable instruments are used in laparoscopic procedures, these are not available in our institutions. In clinical and surgical settings resembling ours, robot-assisted surgery seems more environmentally sustainable. However, more systemic changes are essential to significantly reduce healthcare-related GHG emissions. Hospitals should focus on maximizing the lifespan of hybrid instruments, incorporating decontamination within main instrument sets, and ensuring low-carbon manufacturing and transportation practices; although, scaling these methods globally presents challenges. Furthermore, infrastructure development, policy reform, and behavioral changes [36] are mandatory to improve the current state of affairs in GHG emissions. Expanding the scope of biotechnology and exploring more efficient energy systems could help achieve substantial reductions in the environmental impact of surgery. Although robotic systems demonstrated environmental advantages in our study, their high cost and limited availability may restrict widespread implementation. Clinical benefits, institutional resources, and cost-effectiveness must be considered alongside environmental sustainability.
5. Limitations
This study has several limitations. First, the assignment of surgical techniques was not randomized but based on institutional availability and surgeon–patient decision, introducing potential selection bias. Second, the environmental metrics were calculated based on infrastructure and procurement practices specific to the participating institutions, which may limit the generalizability of our findings. Third, volatile anesthetic gases, which can substantially contribute to ORs’ CO2 emissions [40,43], were not included in the LCA due to data unavailability and differing protocols, and further research is needed on the matter. Fourth, although statistical significance was achieved for several comparisons, we did not correct for multiple testing, and no formal power calculation was performed given the exploratory nature of the study.
6. Conclusions
Systemic changes are imperative to reduce the environmental impact of surgery. Hospitals must prioritize sustainable practices, including transitioning to hybrid and reusable instruments, implementing energy-saving initiatives, like the “Power Down” program, and adopting policies to minimize single-use materials. Further innovation in hospital infrastructure and low-carbon manufacturing processes is needed to scale these practices globally. Although robotic systems, like Da Vinci Xi, are costly and not universally accessible, leveraging biotechnology and energy-efficient systems offers a pathway to mitigate surgical GHG emissions. Future efforts should focus on addressing disparities in accessibility, promoting global collaboration, and exploring solutions that balance surgical excellence with environmental sustainability. By aligning clinical advancements with environmental stewardship, the surgical field can continue to innovate, while minimizing its ecological footprint.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/app15095079/s1, Supplementary Table S1, Supplementary Table S2.
Author Contributions
Conceptualization, A.F., Y.A.S., A.L.P. and A.C. (Antonio Carbone); data curation, A.L.P., R.L., O.A.R., P.P.S., G.B., M.P. and A.Z.; formal analysis, A.F., M.B.S., F.C., A.D.A., S.N. and A.C. (Alessandro Corsini); investigation, M.B.S., R.L., O.A.R., F.M.V., S.N., G.B., D.G., G.C., F.G. and G.M.; methodology, A.F., A.L.P., P.P.S., A.D.A. and A.C. (Antonio Carbone); resources, C.D.N. and A.D.A.; software, M.B.S., S.N., G.C., F.G., G.M. and M.P.; supervision, Y.A.S., A.L.P. and C.D.N.; validation, C.D.N. and A.A.; writing—original draft, A.F., A.L.P., M.B.S., O.A.R. and A.S.; writing—review and editing, A.F., A.L.P., M.B.S., C.D.N., G.B., A.Z., A.S. and A.C. (Antonio Carbone). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This prospective comparative study was approved on 12.OCT.2023 by the Institutional Review Board and Ethics Committee of the Department of Medical and Surgical Sciences and Biotechnologies of Sapienza University in Rome (UROUNIVLT_OCT_23/7021). The principles of the Declaration of Helsinki were followed, and written informed consent was obtained from all participants.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is unavailable due to privacy or ethical restrictions imposed by our institution.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BMI | Body Mass Index |
| CI | Confidence Interval |
| CF | Carbon Footprint |
| CO2 | Carbon Dioxide |
| DM | Diabetes Mellitus |
| EBL | Estimated Blood Loss |
| eGFR | Estimated Glomerular Filtration Rate |
| GHG | Greenhouse Gas |
| Hb | Hemoglobin |
| ICOT | Urology Department of ICOT in Latina |
| ISO | International Organization for Standardization |
| LCA | Life Cycle Assessment |
| LPN | Laparoscopic Partial Nephrectomy |
| LRN | Laparoscopic Radical Nephrectomy |
| MIS | Minimally Invasive Surgery |
| MS | Metabolic Syndrome |
| NHS | National Health Service |
| OR | Operating Room |
| PN | Partial Nephrectomy |
| RAPN | Robot-Assisted Partial Nephrectomy |
| RARN | Robot-Assisted Radical Nephrectomy |
| RENAL | Radius, Exophytic/Endophytic, Nearness, Anterior/Posterior, Location Scoring System |
| RN | Radical Nephrectomy |
| SD | Standard Deviation |
| SPSS | Statistical Package for the Social Sciences |
| T | Tumor Staging |
| UK | United Kingdom |
| US | United States |
| USA | United States of America |
| USD | United States Dollar |
References
- Reddy, K.; Gharde, P.; Tayade, H.; Patil, M.; Reddy, L.S.; Surya, D. Advancements in Robotic Surgery: A Comprehensive Overview of Current Utilizations and Upcoming Frontiers. Cureus 2023, 15, e50415. [Google Scholar] [CrossRef] [PubMed]
- van der Vliet, W.J.; Haenen, S.M.; Solis-Velasco, M.; Dejong, C.H.C.; Neumann, U.P.; Moser, A.J.; van Dam, R.M. Systematic review of team performance in minimally invasive abdominal surgery. BJS Open 2019, 3, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Rafaqat, W.; Ahmad, T.; Ibrahim, M.T.; Kumar, S.; Bluman, E.M.; Khan, K.S. Is minimally invasive orthopedic surgery safer than open? A systematic review of systematic reviews. Int. J. Surg. 2022, 101, 106616. [Google Scholar] [CrossRef] [PubMed]
- Fuschi, A.; Al Salhi, Y.; Sequi, M.B.; Velotti, G.; Martoccia, A.; Suraci, P.P.; Scalzo, S.; Asimakopoulos, A.; Bozzini, G.; Zucchi, A.; et al. Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion. J. Clin. Med. 2021, 11, 136. [Google Scholar] [CrossRef]
- Finegersh, A.; Holsinger, F.C.; Gross, N.D.; Orosco, R.K. Robotic Head and Neck Surgery. Surg. Oncol. Clin. N. Am. 2019, 28, 115–128. [Google Scholar] [CrossRef]
- Rizan, C.; Bhutta, M.F. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg. Endosc. 2022, 36, 4067–4078. [Google Scholar] [CrossRef] [PubMed]
- Chahal, B.; Aydin, A.; Amin, M.S.A.; Khan, A.; Khan, M.S.; Ahmed, K.; Dasgupta, P. The learning curves of major laparoscopic and robotic procedures in urology: A systematic review. Int. J. Surg. 2023, 109, 2037–2057. [Google Scholar] [CrossRef]
- Picozzi, P.; Nocco, U.; Labate, C.; Gambini, I.; Puleo, G.; Silvi, F.; Pezzillo, A.; Mantione, R.; Cimolin, V. Advances in Robotic Surgery: A Review of New Surgical Platforms. Electronics 2024, 13, 4675. [Google Scholar] [CrossRef]
- Chughtai, B.; Scherr, D.; Del Pizzo, J.; Herman, M.; Barbieri, C.; Mao, J.; Isaacs, A.; Lee, R.; Te, A.E.; Kaplan, S.A.; et al. National Trends and Cost of Minimally Invasive Surgery in Urology. Urol. Pract. 2015, 2, 49–54. [Google Scholar] [CrossRef]
- Capretti, G.; Boggi, U.; Salvia, R.; Belli, G.; Coppola, R.; Falconi, M.; Valeri, A.; Zerbi, A. Application of minimally invasive pancreatic surgery: An Italian survey. Updates Surg. 2019, 71, 97–103. [Google Scholar] [CrossRef]
- Batchelder, A.J.; Williams, R.; Sutton, C.; Khanna, A. The evolution of minimally invasive bariatric surgery. J. Surg. Res. 2013, 183, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Elhage, S.; Schiffern, L.; Lauren Paton, B.; Ross, S.W.; Matthews, B.D.; Reinke, C.E. Use of minimally invasive surgery in emergency general surgery procedures. Surg. Endosc. 2020, 34, 2258–2265. [Google Scholar] [CrossRef]
- Stojko, R.; Sadlocha, M. Minimally invasive surgery in gynecology. Reconciling the past with a view to the future. Ginekol. Pol. 2022, 93, 859–860. [Google Scholar] [CrossRef]
- Health Care without Harm. Health Care’s Climate Footprint. Climate-Smart Health Care Series Green Paper Number One (2019). Available online: https://noharm-uscanada.org (accessed on 15 October 2023).
- Rizan, C.; Steinbach, I.; Nicholson, R.; Lillywhite, R.; Reed, M.; Bhutta, M.F. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann. Surg. 2020, 272, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Ibbotson, S.; Dettmer, T.; Kara, S.; Herrmann, C. Eco-efficiency of disposable and reusable surgical instruments—A scissors case. Int. J. Life Cycle Assess. 2013, 18, 1137–1148. [Google Scholar] [CrossRef]
- Overcash, M. A comparison of reusable and disposable perioperative textiles: Sustainability state-of-the-art 2012. Anesth. Analg. 2012, 114, 1055–1066. [Google Scholar] [CrossRef]
- McPherson, B.; Sharip, M.; Grimmond, T. The impact on life cycle carbon footprint of converting from disposable to reusable sharps containers in a large US hospital geographically distant from manufacturing and processing facilities. PeerJ 2019, 7, e6204. [Google Scholar] [CrossRef] [PubMed]
- Kümmerer, K.; Dettenkofer, M.; Scherrer, M. Comparison of reusable and disposable laparatomy pads. Int. J. Life Cycle Assess. 1996, 1, 67–73. [Google Scholar] [CrossRef]
- McGain, F.; McAlister, S.; McGavin, A.; Story, D. The financial and environmental costs of reusable and single-use plastic anaesthetic drug trays. Anaesth. Intensive Care 2010, 38, 538–544. [Google Scholar] [CrossRef]
- Eckelman, M.; Mosher, M.; Gonzalez, A.; Sherman, J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth. Analg. 2012, 114, 1067–1072. [Google Scholar] [CrossRef]
- Sherman, J.D.; Raibley, L.A.t.; Eckelman, M.J. Life Cycle Assessment and Costing Methods for Device Procurement: Comparing Reusable and Single-Use Disposable Laryngoscopes. Anesth. Analg. 2018, 127, 434–443. [Google Scholar] [CrossRef]
- Kutikov, A.; Uzzo, R.G. The R.E.N.A.L. nephrometry score: A comprehensive standardized system for quantitating renal tumor size, location and depth. J. Urol. 2009, 182, 844–853. [Google Scholar] [CrossRef] [PubMed]
- ISO 14044:2006; Environmental Management—Life Cycle Assessment—Requirements and Guidelines. International Organization for Standardization: Geneva, Switzerland, 2006. Available online: https://www.iso.org/standard/38498.html (accessed on 17 January 2023).
- Karali, N.; Khanna, N.; Shah, N. Climate Impact of Primary Plastic Production; Lawrence Berkeley National Laboratory: Berkeley, CA, USA, 2024. [Google Scholar]
- Sun, Y.; Kojima, S.; Nakaohkubo, K.; Zhao, J.; Ni, S. Analysis and Evaluation of Indoor Environment, Occupant Satisfaction, and Energy Consumption in General Hospital in China. Buildings 2023, 13, 1675. [Google Scholar] [CrossRef]
- McGain, F.; McAlister, S. Correction: Reusable versus single-use ICU equipment: What’s the environmental footprint? Intensive Care Med. 2024, 50, 156. [Google Scholar] [CrossRef] [PubMed]
- Pichler, P.-P.; Jaccard, I.S.; Weisz, U.; Weisz, H. International comparison of health care carbon footprints. Environ. Res. Lett. 2019, 14, 064004. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Sherman, J. Environmental Impacts of the U.S. Health Care System and Effects on Public Health. PLoS ONE 2016, 11, e0157014. [Google Scholar] [CrossRef]
- SDC. NHS England Carbon Emissions: Carbon Footprinting Study; Sustainable Development Commission: London, UK, 2008. [Google Scholar]
- Tennison, I.; Roschnik, S.; Ashby, B.; Boyd, R.; Hamilton, I.; Oreszczyn, T.; Owen, A.; Romanello, M.; Ruyssevelt, P.; Sherman, J.D.; et al. Health care’s response to climate change: A carbon footprint assessment of the NHS in England. Lancet Planet. Health 2021, 5, e84–e92. [Google Scholar] [CrossRef]
- Vogel, L. Canada’s health system is among the least green. CMAJ Can. Med. Assoc. J. 2019, 191, E1342–E1343. [Google Scholar] [CrossRef]
- Connor, A.; Lillywhite, R.; Cooke, M.W. The carbon footprints of home and in-center maintenance hemodialysis in the United Kingdom. Hemodial. Int. Int. Symp. Home Hemodial. 2011, 15, 39–51. [Google Scholar] [CrossRef]
- Connor, A.; Lillywhite, R.; Cooke, M.W. The carbon footprint of a renal service in the United Kingdom. QJM Mon. J. Assoc. Physicians 2010, 103, 965–975. [Google Scholar] [CrossRef]
- Pradere, B.; Mallet, R.; de La Taille, A.; Bladou, F.; Prunet, D.; Beurrier, S.; Bardet, F.; Game, X.; Fournier, G.; Lechevallier, E.; et al. Climate-smart Actions in the Operating Theatre for Improving Sustainability Practices: A Systematic Review. Eur. Urol. 2023, 83, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Kloevekorn, L.; Roemeling, O.; Fakha, A.; Hage, E.; Smailhodzic, E. Decarbonizing surgical care: A qualitative systematic review guided by the Congruence Model. BMC Health Serv. Res. 2024, 24, 1456. [Google Scholar] [CrossRef]
- MacNeill, A.J.; Lillywhite, R.; Brown, C.J. The impact of surgery on global climate: A carbon footprinting study of operating theatres in three health systems. Lancet Planet. Health 2017, 1, e381–e388. [Google Scholar] [CrossRef] [PubMed]
- Fuschi, A.; Pastore, A.L.; Al Salhi, Y.; Martoccia, A.; De Nunzio, C.; Tema, G.; Rera, O.A.; Carbone, F.; Asimakopoulos, A.D.; Sequi, M.B.; et al. The impact of radical prostatectomy on global climate: A prospective multicentre study comparing laparoscopic versus robotic surgery. Prostate Cancer Prostatic Dis. 2024, 27, 272–278. [Google Scholar] [CrossRef]
- Thiel, C.L.; Woods, N.C.; Bilec, M.M. Strategies to Reduce Greenhouse Gas Emissions from Laparoscopic Surgery. Am. J. Public Health 2018, 108, S158–S164. [Google Scholar] [CrossRef] [PubMed]
- Wormer, B.A.; Augenstein, V.A.; Carpenter, C.L.; Burton, P.V.; Yokeley, W.T.; Prabhu, A.S.; Harris, B.; Norton, S.; Klima, D.A.; Lincourt, A.E.; et al. The green operating room: Simple changes to reduce cost and our carbon footprint. Am. Surg. 2013, 79, 666–671. [Google Scholar] [CrossRef]
- Morris, D.S.; Wright, T.; Somner, J.E.; Connor, A. The carbon footprint of cataract surgery. Eye 2013, 27, 495–501. [Google Scholar] [CrossRef]
- Digital, N. Hospital Admitted Patient Care Activity, 2019–2020; NHS Digital: Leeds, UK, 2020. [Google Scholar]
- Slingo, J.M.; Slingo, M.E. The science of climate change and the effect of anaesthetic gas emissions. Anaesthesia 2024, 79, 252–260. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).