Abstract
There have been significant breakthroughs in developing highly functional myoelectric prostheses, yet individuals who have experienced upper-limb loss consistently report low levels of satisfaction when performing daily tasks while using myoelectric prostheses. This research aims to evaluate the change in the user’s experience after completing a training program in which tasks are designed to facilitate adaptation to the myoelectric arm in performing the activities of daily living. One participant with a left transradial limb difference was recruited for this project. The user’s experience was evaluated by comparing task completion time, trunk and shoulder angles, object control, movement smoothness, vertical ground reaction forces, the center of pressure location, and selected muscle activation of her affected arm between baseline and post-training. The data collection was performed through a motion capture system, a pressure mat, and wireless EMG modules. While indications of potential improvements in balance, muscle efficiency, and functionality were present, the data were inconclusive as to the effectiveness of the training procedure. One outcome measure that showed improvement across most tasks was the task completion time, which, on average, for the targeted Box and Block Test (tBBT) task was reduced by 24.0 s, box lifting by 1.6 s, bottle pouring by 9.0 s, and the pulley task by 8.4 s. This project serves as part of a larger multi-visit study evaluating the effects of home-based functional training on facilitating users’ adaptation to the myoelectric arm.
1. Introduction
In 2005, there were roughly 41,000 individuals who experienced limb loss at or above the wrist. In that same year, 68.6% of upper limb amputations were related to trauma []. In 2013, there were 10,365 upper limb amputations in the U.S., with 13.6% being at the transradial, which is between the elbow and wrist; the transhumeral, which is above the elbow but below the shoulder, or the shoulder level []. These data were significant when considering the amputees’ quality of life and how the functionality of modern prosthetics affects their everyday tasks. Losing a hand or arm presents severe challenges, often impairing work status, independence, and quality of life. While prostheses cannot fully replicate hand function, they assist in performing basic tasks and maintaining the use of both hands []. This is even more significant when considering the high prosthetic rejection rate. While some studies report a prosthetic rejection rate of nearly 44% [], a review on upper limb prosthetic rejection rates reports device abandonment in one of every five users []. The upper extremities consist of the shoulder girdle, arm, forearm, and hand and play a crucial role in fine motor control and manipulative tasks. They are characterized by a high degree of mobility and dexterity, enabling both gross motor activities, such as lifting, and intricate movements, such as grasping and manipulating small objects. The greater the degree of freedom (DOFs) in the upper extremities in relation to movement, the more significant the challenge of designing a functional prosthesis []. Due to the variety of tasks the upper limb can perform, its dexterity and sensory capacity pose major challenges to a user performing functional tasks with a prosthesis [].
Considering the number of individuals who experience limb loss each year and the challenges with designing a functionally sound upper limb prosthesis, it is important to evaluate the current prostheses on the market to determine their functionality and how best to design training procedures that increase user functionality. While great advances have been made in prosthesis, such as enhanced sensory and motor control through targeted reinnervation and hand transplantation, users still report low levels of satisfaction related to functionality when performing unimanual and bimanual tasks, making effective prosthesis training essential for user–prosthesis integration []. In the context of this research, a unimanual task is a task that requires only one hand, such as brushing teeth or writing, while a bimanual task requires two hands, such as opening a jar, putting toothpaste on the toothbrush, or tying shoelaces.
A myoelectric prosthesis operates using electrical signals from muscles in the residual limb, allowing for more natural and intuitive movement compared to traditionally body-powered prostheses. These electrical signals are captured by electrodes on the skin or within the prosthetic socket, translating the user’s intended movements into physical movement via the actuators in the prosthesis. Several studies have demonstrated the potential for myoelectric prostheses to increase the functional ability of transradial amputees, especially in bimanual tasks. Biddiss and Chau (2007) [] conducted a systematic literature review and found that people using myoelectric prostheses report improvements in activities such as holding, lifting, and turning things with their articulated hands. Nevertheless, they have emphasized the need for ongoing support to address any challenges users face in transitioning from traditional prostheses to myoelectric prostheses.
Similarly, Østlie et al. (2012) [] conducted a randomized controlled trial comparing myoelectric and body-powered prostheses in radial amputees and found that myoelectric prosthesis users showed more improvement in gripping control and efficiency in bimanual tasks. In their study, they emphasized the importance of user training and proper socket fit to maximize the benefits of myoelectric prostheses for transradial amputees. Ensuring proper fit and comfort is essential for the successful use of a myoelectric prosthetic arm, prompting the need for continued research to optimize design for a snug and pleasant fit. To facilitate device adaptation, training, and adjustment, individuals must learn how to operate these devices smoothly, highlighting the need for effective training programs and support mechanisms. Maintaining and ensuring the longevity of myoelectric prosthetic arms is also crucial, necessitating research to enhance durability and reliability to reduce repair and replacement frequency.
A participant with a congenital limb difference is usually recommended directly into the outpatient prosthetic training with a myoelectric arm. The framework of the training can be broken down into four levels, with the idea of increasing task difficulty through each level to match the increased complexity of activities of daily living (ADLs). At the first level, the participant is trained to perform movements such as opening/closing the terminal device. At the second level, object manipulation is incorporated into tasks with objects of different sizes and shapes. This level also focuses on rote training and grip control to create natural movements with the myoelectric arm and to achieve good grip control, in which the patient learns how much pressure to exert with the device based on the density and durability of the object []. Functional tasks with increasing complexity are introduced at the third level. Functional tasks often start with basic ADLs []. While the participants with unilateral upper extremity amputations master one-handed techniques for ADL performance, they will be given basic bilateral tasks for their prosthesis to work with their intact limb []. The fourth and final level of training would cover various household tasks, community, and work reintegration [].
Currently, few standardized tests are available for assessing upper extremity prosthesis performance in outpatient prosthetic training, with few upper limb prosthetic-specific outcome measures in number []. The ‘Unilateral Upper Extremity Amputation: Activities of Daily Living Assessment’ is a task list that the therapist uses to only qualitatively rate the task smoothness during therapy sessions []. The Assessment of Capacity for Myoelectric Control (ACMC) [] focuses on the performance of a myoelectric prosthesis but lacks standardization for different types of prostheses or functional contexts. While useful for assessing task performance and dexterity, the Jebsen–Taylor Test of Hand Function [], Box and Blocks Test [], Nine-Hole Peg Test [], and Southampton Hand Assessment Procedure (SHAP) [] are not standardized for prosthetic use. More research in standardized assessment for prosthetic use is thus needed to objectively gather a core set of outcome measures, which can be assessed by using motion analysis tools. For example, the level of object manipulation can be quantified by the smoothness of hand module movement, which is calculated as the derivative of hand acceleration, and reliance on visual feedback, which can be calculated as a correlation coefficient between head movement trajectory and hand module movement trajectory. Head and hand module movement can be measured by using a marker-based motion capture tool.
In addition, current research effort focuses on assessing the myoelectric arm in the lab environment, often with able-bodied participants [,], which does not examine how amputees learn to use a prosthesis in actual ADLs, especially not how they learn to integrate multi-grip modes into their daily lives []. Nevertheless, an effective training program needs the prosthesis user to perform the tasks in the context of ADLs []. Furthermore, environmental factors such as support from family, support and training from professionals, optimal training location, proper fit, and good understating of the function of the prosthesis can facilitate the embodiment of the prosthesis when in use [].
This research aims to design an evaluation protocol to assess a home-based training program implemented to increase user functionality. Due to time and budget constraints, the training program utilizes the above-mentioned four-level framework with the goal of helping the participant master the movements at the first and second levels. The participant primarily practices object manipulation using different gripping patterns, force control, and arm positioning with different objects through repetitions. It is expected that the participant should operate the prosthesis successfully without consistent visual feedback.
The structure of this research paper consists of an introduction that highlights the current literature on prosthetic training and evaluation and discusses the gap in user satisfaction, particularly in performing daily tasks. The Methodology section details the evaluation protocol, including participant recruitment and the data collection techniques. This section also describes the training program and outcome measures. The Results section compares baseline and post-training evaluation data, focusing on task completion times, movement metrics, muscle activation, and ground reaction forces. The Discussion section interprets these findings, considering potential reasons for the observed outcomes and their implications for future research in prosthetic adaptation. The paper concludes by outlining the next steps in the larger study to continue exploring effective means of training and evaluation.
2. Methodology
An evaluation protocol was implemented to collect kinematics and kinetics data during baseline and post-training evaluation to investigate the training effect. The data was processed, and the outcome measures were created to quantify the user’s experience while performing unimanual and bimanual tasks in order to evaluate the effectiveness of the developed training program.
2.1. Participant
To be eligible for this study, the participant must be a transradial amputee, over the age of 18, be able to provide verbal or written consent, be able to fit into the myoelectric arm and be able to understand and perform the tasks described in the training program and the evaluation program. The participant should not have any neurological or cardiorespiratory condition or diagnosis. In addition, the participant should not have a history of seizures in the past year.
One participant (24 years old, 160 cm, 54 kg) was recruited under the University of the District of Columbia (UDC)’s Institutional Review Board-approved protocol (2136093-1). This participant was born with a congenital limb difference (likely a transverse deficiency) at the transradial level. She has the presence of underdeveloped vestigial digits at the end of her residual limb, and her limb length is ~80% relative to her contralateral forearm length. The participant uses a body-powered device to perform activities three times per week at the gym with no training required but does not use the device to perform daily activities. The participant’s experience with the myoelectric arm began at the onset of the research. Informed consent was obtained before data collection. The data presented here is part of a larger multi-visit study evaluating the effects of home-based functional training on facilitating user’s adaptation to the myoelectric arm.
2.2. Myoelectric Arm
A custom-fit myoelectric arm prosthesis was obtained via a certified prosthetist and orthotist (CPO) at Medical Center Orthotics & Prosthetics (Silver Spring, MD, USA). Due to budget constraints, the participant used the i-Limb Access (Ossur, Reykjavik, Iceland) without powered wrist pronation and supination. Our CPO created a custom-shaped prosthesis for the participant’s arm. The prosthesis contains all the components, including batteries, electrodes, and controls. The i-Limb was connected to the prosthesis as the chosen terminal device for the research study.
To ensure research safety, the participant was myotested and has been deemed appropriate to be fit with a myoelectric prosthesis and to be able to perform the functional and bimanual tasks before enrolling into our study. Moreover, a clinician ensured that the participants would have the cognitive and physical capacity to perform tasks with the prosthesis and would be able to complete training. In addition, as some amputees may have traumatic brain injuries or other physical challenges, considerations were made regarding the demographics of patients who are using these devices as real-life users, unlike typical research that studies able-bodied individuals.
2.3. Training Program
The purpose of these tasks is to help the participant perform the tasks involved in ADLs, such as reaching and grasping the objects (cup and fruit) by using the prosthesis, cutting vegetables, opening jars, holding food trays, or typing on a keyboard, which involves using both hands. The training procedure was developed by considering the range of motion, center of mass, and moment of the arm while performing these daily tasks []. The fact that the training should be able to broadly apply to daily tasks, incorporating compound movements while also being simple and not strenuous was also considered []. The five training exercises were thus created. The description of these tasks can be found in Appendix A. The first three exercises were developed during a UDC Senior Capstone project and focused on mimicking daily activities with very little resistance to developing motor skills while using the prosthetic device with the aim of increasing functionality. All exercises are designed to improve control, using slow movements with time markers indicating when a movement should be completed. The first exercise consists of raising and lowering the hand via rotation about the elbow in the sagittal plane while opening and closing the hand, which mimics pulling objects, such as doors, towards the body with a tightened grip. The second exercise entails raising a dowl overhead and then lowering the dowl again. This is a critical movement to master as daily overhead movements have increased moment arms and can generate a large amount of force in the shoulder complex and back muscles if the movement is not performed effectively. Exercise three is performed in the seated position and consists of moving a ball over a divider and rotating the wrist to let the ball fall onto a table. While standing introduces more complex compound motor skills, seated activities, such as movements during a meal where the lower extremities cannot be recruited, also require practice. Exercise four was developed by Ossur and involves multiple activities that help the user with more fine motor skills and to become more accustomed to the device features such as grip strength control, adjustments to thumb position, finger position, and finger control. Lastly, exercise five, also developed by Ossur, helps the user become more familiar with the device’s preprogrammed grips by practicing them via Ossur’s mobile application.
The participants were trained for 30 minutes each day for two weeks after the baseline evaluation. To develop good control and positioning of the i-Limb hand, the participant was asked to successfully perform each task at least three times during each training session. During the training program, the participant continued working with the CPO to discuss her performance. The duration and intensity of treatment were selected based on literature sources, discussion with CPO and other clinical researchers in this field, and the device’s limited three-week loan period. Egermann et al. reported that the initial adaptation training can be structured for the length of one or two weeks []. Powell et al. found that the performance of prosthetic control could be improved after two weeks of training with visual biofeedback []. Moreover, the relative changes in EMG signal features would decrease exponentially after about two weeks as amputees adapt to the way of muscle contraction after training [].
2.4. Evaluation Protocol
The performance evaluation consists of two visits to the Center of Biomechanics and Rehabilitation Engineering (CBRE) at UDC and the training program at home for two weeks. The first and second visits were used to evaluate the baseline and post-training performances of the user with i-Limb Access, respectively. Each visit took roughly two hours. The evaluation protocol implemented an experimental setup, as shown in Figure 1, utilizing the Vicon motion capture system (Vicon Motion Systems, Oxford, UK), Tekscan Strideway pressure mat (Tekscan, Inc., Norwood, MA, USA), and wireless EMG modules (Delsys, Natick, MA, USA) to identify the outcome measures. The sampling rates for these systems are 100 Hz, 40 Hz, and 1000 Hz, respectively. The participant stood in front of a testing platform made of a lab stool whose height was adjusted by placing the non-metal boards on the top to ensure that the participant could comfortably perform the experimental tasks.

Figure 1.
The experimental setup in which a participant performed a bottle pour task with i-Limb Access.
The data was collected and analyzed via a pipeline that calculates joint kinematics, muscle activities, and the location of the center of pressure from preprocessed marker data, EMG data, and vertical ground reaction force (vGRF) data. At the beginning of each visit, 41 reflective markers were placed on the participant’s body. In detail, 39 14-mm markers were placed at bony anatomical landmarks of the full body in accordance with the Vicon Full Body Plug-In-Gait body model []. Two additional 14-mm markers were placed at the medial side of the elbow joints. EMG electrodes were placed on the muscle belly region of the middle deltoids, biceps, and triceps muscle in the left arm, and thoracolumbar fascia muscle in the lower back. As there is very limited access to forearm muscles, these muscle groups are selected to evaluate the improvement in upper limb muscle synergy and trunk compensation reduction when performing the tasks. It is expected that the EMG activations recorded from these muscles will decrease as the participant learns to be adapted to the device to achieve the desired movement. Monitoring the activation of these muscles helps assess indirectly how well the user was able to generate and control the signals needed for precise prosthetic control while also ensuring proper alignment and stability during movement. Preprocessing the motion capture and EMG data was performed by using Vicon Nexus. The vGRF data were preprocessed using Strideway software (7.80 x64). The Strideway and Nexus software (2.12.1) was integrated using a USB 6008 data acquisition card, enabling the systems to start and stop data collection at the same time.
For the evaluation tasks, it is necessary to have a combination of unimanual and bimanual tasks that are similar to the training exercises to determine if the user has become more effective in using the device as opposed to simply more effective at performing the training exercises. There are two bimanual (box lift and bottle cap) and two unimanual (functional) (target Box and Block Test (tBBT) [], bottle pour, and pulley) tasks. The box lift task consists of the participant bending down to pick up a box from the ground and placing it on the table. The bottle cap task requires the participant to pick up a bottle with a screw-on cap with an unimpaired hand and then use the prosthetic device to unscrew the cap. The tBBT task consists of moving colored blocks from one side of a box across a partition to the other side. The bottle pour task involves lifting a bottle and pouring its contents out into a cup. The pulley task involves reaching up to grab a ring handle hanging from a pulley system. The participant then pulls the handles down until they are at waist level, then lets the handles rise back to the starting position.
This participant performed two sessions for each task. Each session was suggested to be completed in less than 40 s if possible. A full list of these tasks with their descriptions can be found in Appendix B. We chose two repetitions for each task as two repetitions were reported to be enough to reduce data variability and to ensure data reliability and consistency for upper limb prostheses []. The participant was able to complete all the tasks for two trials within the given time frame during the baseline evaluation. We thus kept the same number of trials for each task during post-evaluation.
2.5. Outcome Measures
The primary outcome measures refer to the upper body kinematics and muscle activations during the functional tasks and bimanual tasks of using the prosthesis, as well as the postural stability when standing to perform evaluation tasks. They include the following items: (1) Task completion time; (2) Angles of the trunk (tilt, list, and rotation) and left shoulder (flexion, abduction, and rotation); Trunk and shoulder angles were included as these segments will be engaged compensate for limitations in prosthetic function, which is inefficient and can lead to injury [,]; Vicon angle convention table was used to define these angles. The trunk tilt, list, and rotation angles are absolute angles. The trunk tilt is measured as the angle in the laboratory sagittal plane between the projected sagittal thorax axis and the sagittal laboratory axis. The trunk list is measured between the projection into the plane of the transverse thorax axis and the projection into the plane of the laboratory transverse axis; the trunk rotation is measured between the sagittal axis of the thorax and the sagittal laboratory axis (axis closest to the participant’s direction of progression) projected into the thorax transverse plane. The shoulder flexion, abduction, and rotation angles are relative angles. The shoulder flexion, abduction, and rotation are calculated between the projected sagittal–humerus axis and the sagittal–thorax axis around the fixed transverse axis of the thorax, between the transverse axis of the humerus and the transverse axis of the thorax around a floating sagittal axis, and between sagittal axis of the humerus and the sagittal axis of the thorax around a floating frontal axis, respectively []. Figure 2 provides a demonstration of these angle definitions in an OpenSim model []. We expect that the participant will become more adapted to the myoelectric arm after the completion of the training program. To put it into the perspective of joint angle change at post-evaluation, across all tasks, all three trunk angles should decrease as the participant would rely less on the trunk compensation, and shoulder flexion and abduction shoulder increase, whereas the shoulder internal rotation should decrease. (3) object control. The linear correlation coefficient (r value) is calculated to quantify the head and object coordination, which indicates how well the object is handled during the task. The value of r is between −1 and 1. The head moves in phase with the object as r reaches 1, whereas the head moves 180° out of phase with the object as r reaches −1. This outcome measure assesses the participant’s ability to manipulate and interact with objects, which is critical for daily functional tasks. Improved object control (towards r = 1) indicates that the participant can use the myoelectric arm to grasp, release, and handle objects with precision more effectively, enhancing overall prosthetic functionality and quality of life []. (4) Smoothness of movement. Using the marker on the back of the hand, smoothness can be quantified as jerk using the derivative of acceleration of that marker. This outcome measure was selected as it directly reflects the control and precision with which the participant is able to replicate natural hand and arm movements using a prosthesis. Improved smoothness indicates enhanced coordination between the user’s muscle signals and the prosthesis, contributing to more functional use in daily activities []. (5) Muscle activation. These data provide insights into the participant’s neuromuscular coordination and the effectiveness of the training in optimizing prosthetic functionality []. (6) vertical ground reaction force (vGRF) from left and right feet and (7) center of pressure (COP) location closeness to the right foot (closeness to the Right), which calculates the ratio of the distance between the total COP coordinates and the COP coordinates of left foot to the distance between the COP coordinates of left foot and the COP coordinates of right foot and is displayed in percentage. vGRF and COP location closeness to the right foot outcome measures can reflect the level of postural stability, as their adaptation to the prosthesis can impact overall balance and gait, influencing the forces exerted through the ground during everyday tasks [,].
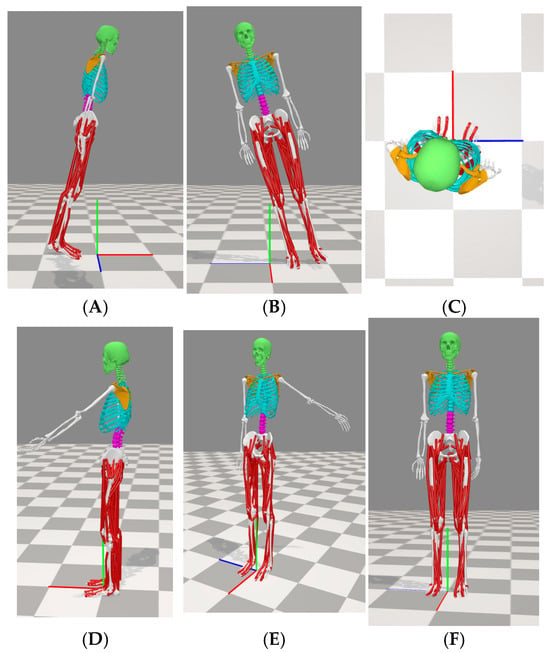
Figure 2.
Joint angle demonstration. (A) Trunk tilting—a positive value corresponds to forward trunk tilt. Here, the trunk is tilting at +15°. (B) Trunk listing—a positive value corresponds to leaning to the right side. Here, the trunk is listing at +15°. (C) Trunk rotation—a positive value corresponds to rotating toward the right side. Here, the trunk rotates +15°. (D) Shoulder flexion—a positive value corresponds to the situation in which the arm is in front of the body. Here, the left shoulder has a flexion angle of +60°. (E) Shoulder abduction—a negative value corresponds to an outwardly moved left arm. Here, the left shoulder has an abducted angle of −60°. (F) Shoulder rotation—a positive value corresponds to an internally rotated humerus of the left arm. Here, the left shoulder has a rotation angle of +60°. As a result, the left palm faces into the body.
2.6. Data Analysis
Our data analysis includes three components: data preprocessing, data storage, and data postprocessing. Preprocessing the motion capture data in Vicon Nexus began with reconstructing the markers in the visualizer and auto-initializing labeling using the full-body plug-in gait model. The participant was then scaled by applying Vicon labeling skeleton measurements, followed by a static skeleton calibration where marker locations related to joints were saved. The data were cropped into the region of interest, and any unlabeled or mislabeled markers were manually corrected. Missing data were filled using one of Nexus’ four gap-fill strategies, and the trajectory was smoothed using the Woltring filter. The static plug-in gait model was applied to obtain and verify biomechanical outputs, such as joint angles, in the calibration trial before proceeding to the dynamic trial. The dynamic trial followed similar steps, applying the dynamic plug-in gait model and exporting the marker and joint angle data in a .csv format. A wireless Delsys EMG system was used to record muscle activation of the biceps, triceps, and mid-deltoid from the left arm and from at 1000 Hz. EMG data were band-pass filtered at 15–380 Hz, full-wave rectified, and low-pass filtered at 7 Hz to create a linear envelope using a custom script [,] developed in MATLAB R2023b (MathWorks, Natick, MA, USA).
A data storage plan was created using a MATLAB-based structure to store processed data (marker data, joint angle data, EMG data, vGRF, and COP data) collected from Vicon Nexus integrated with Delsys wireless EMG and Strideway platform, and the participant’s anthropometric data. Time normalization was then used to compare the outcome measures between baseline and post. A data postprocessing pipeline was also developed in MATLAB to achieve batch processing for these outcome measures in all experimental conditions and by implementing statistical tools to compare the joint kinematics (including trunk and shoulder rotation angles in three axes), smoothness of movement, muscle activities, and center of pressure before and after completion of the training program.
3. Results
The time it takes to complete each trial of the task was normalized to 1001 timeframes between 0 and 100 in the comparison of the outcome measures such as temporal angle of trunk and shoulder, movement smoothness (Jerk), vertical ground reaction forces, and selected muscle activations. A normalized time of 0 means the start of the task, whereas 100 means the completion of the task. vGRFs were also normalized with respect to the participant’s body mass. Figure 3, Figure 4, Figure 5, Figure 6 and Figure 7 show the exemplary plots for shoulder and trunk angles, object control, movement smoothness, normalized vGRFs, and muscle activation against normalized time between baseline and post-evaluation for the box lift task, respectively.

Figure 3.
Trunk and left shoulder angle comparison in their three primary rotation axes. The color-shaded regions represent the mean and standard deviation of the joint angles across all trials of the box lift task at that time point.
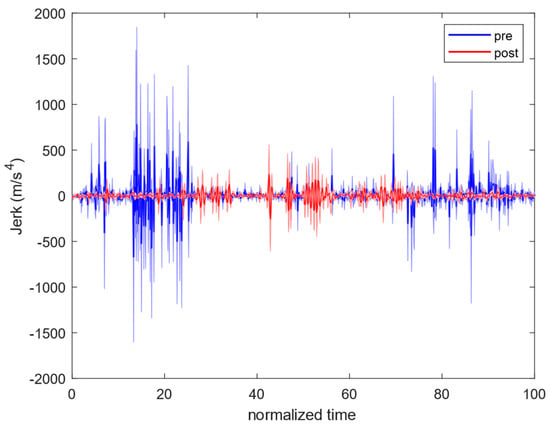
Figure 4.
Myoelectric arm movement smoothness (jerk) comparison. The color-shaded regions represent the mean and standard deviation of the jerk across all trials of the box lift task at that time point.
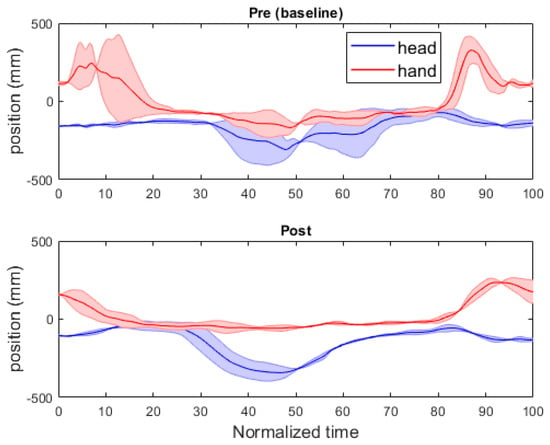
Figure 5.
Hand and head movement trajectory comparison of box lift task. The color-shaded regions represent the mean and standard deviation of the head and hand trajectories across all trials of the box lift task at that time point.
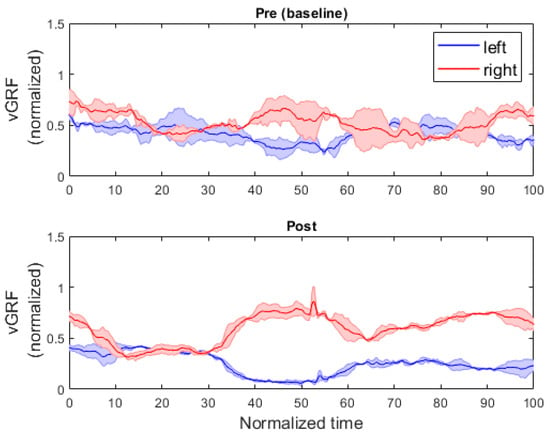
Figure 6.
vGRFs of left and right feet comparison of box lift task. The color-shaded regions represent the mean and standard deviation of the vGRFs across all trials of the box lift task at that time point.
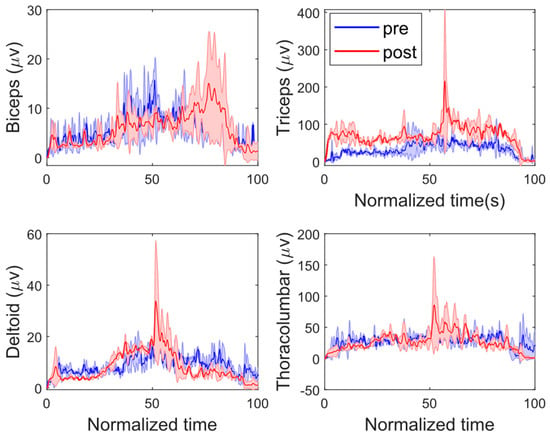
Figure 7.
Comparison of muscle activation of four muscle groups on left arm during box lift task. The color-shaded regions represent the mean and standard deviation of each muscle activation across all trials of the box lift task at that time point.
All five tasks between baseline and post-evaluation were compared. MATLAB Boxchart was used to display the data of the following outcome measures with the median, the lower and upper quartiles, any outliners, and the minimum and maximum values that are not outliers: trunk and shoulder angles (Figure 8), movement smoothness (Figure 9), vGRFs (Figure 10) and muscle activations (Figure 11).
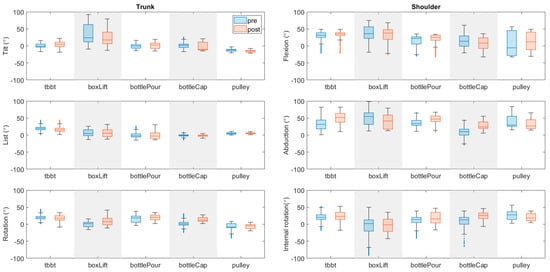
Figure 8.
Comparison of trunk and shoulder angles in all three axes for each task. The outliners are jittered, and the marker style has been changed for better display.
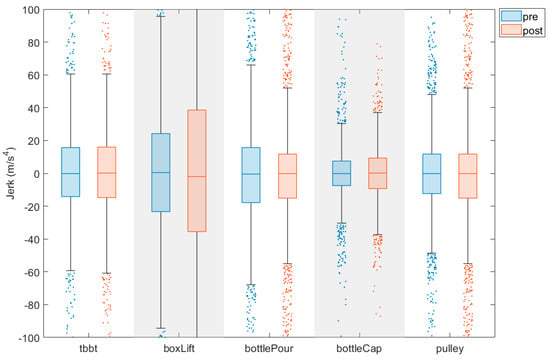
Figure 9.
Comparison of hand smoothness for each task. The outliners are jittered, and the marker style has been changed for better display.
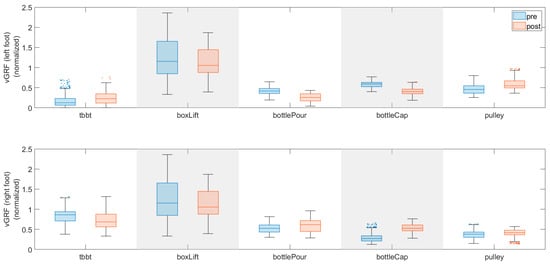
Figure 10.
Comparison of vGRF for each task. The outliners are jittered, and the marker style has been changed for better display.
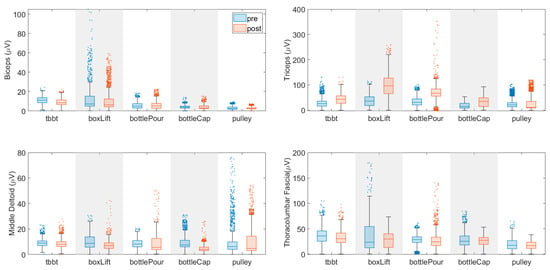
Figure 11.
Comparison of four muscle activations for each task. The outliners are jittered, and the marker style has been changed for better display.
Table 1 was created to display the task completion time, task-dependent object control factor (correlation coefficient), and the COP closeness to the Right value. Only one trial was performed for the tBBT task during post-evaluation. This is because the actuator of the thumb module in the i-Limb Access did not facilitate the thumb linkage to create the proper pinch force to grasp the small box during its second trial. The participant performed two trials for the other four tasks during baseline and post-evaluation. In total, 19 trials were conducted. In addition, during the box lift task for both pre and post-evaluation sessions, the participant’s left and right feet moved into the same contact area on the pressure mat at certain time points. The vGRFs on the left foot cannot thus be separated from the vGRFs on the right foot. As a result, the total force is reported for both the left side and right side and leaves the entry for closeness to the Right blank, which is called not applicable in Table 1.

Table 1.
Outcome measures related to task performance.
A one-sample Kolmogorov–Smirnov test was first performed to show that the data collected were not from a standard normal distribution. The ranksum test in MATLAB (equivalent to a Mann–Whitney U-test) was thus used to compare joint angles, jerk, vGRF, and muscle activation values between baseline and post-evaluation. The trunk forward tilt angle increased significantly by 4° in tBBT (p < 0.01) and by 2° in bottle pour task (p < 0.01). Trunk list angle increased significantly in box lift by 3° (p < 0.01) and pulley task by 2° (p < 0.01). The trunk rotation angle increased significantly in tBBT by 2° (p < 0.01), in box lift by 9° (p < 0.01), and in bottle pour task by 3° (p < 0.01). Left shoulder flexion angle increased significantly in tBBT by 3° (p < 0.01), in bottle pour by 8° (p < 0.01), and in pulley tasks by 8° (p < 0.01). Left shoulder abduction angle increased significantly in tBBT by 17° (p < 0.01), in bottle pour by 11° (p < 0.01), and in bottle cap task by 17° (p < 0.01). No significant change is displayed in jerk. vGRFs on the left side increased significantly in tBBT by 4 kg-force with p < 0.01 and pulley tasks by 7 kg-force with p < 0.01. vGRFs on the right side increased significantly in pulley by 2 kg-force with p < 0.01, bottle pour by 3 kg-force with p < 0.01, and bottle cap tasks by 12 kg-force with p < 0.01. Biceps muscle activation decreased significantly in the pulley task by 0.2 with p < 0.01. The triceps muscle activation increased significantly in tBBT by 15.2 with p < 0.01 and bottle cap tasks by 15.6 with p < 0.01. No statistically significant change was displayed in other muscles.
4. Discussion
On average, the time for the tBBT, box lifting, bottle pouring, and pulley task tasks decreased by 24.0, 1.6, 9.0, and 8.4 s, respectively, while the time for the bottle cap task did not change. The increased average shoulder angle in all three axes in most tasks during post-evaluation may indicate that the left shoulder joint became more engaged in performing these tasks. However, the increased average trunk angle in all three axes in some of these tasks may also indicate that the trunk compensation was not reduced to some extent. In addition, the post-evaluation angle changes also appear smoother than the angle changes in the baseline evaluation, which may indicate that the participant had greater control of movement. When comparing these angle data, one caveat is that these joint angle differences for both the trunk and shoulder may not be clinically meaningful enough to conclude whether the training procedure was effective or ineffective. There does appear to be larger spikes in the baseline evaluation, meaning there may have been larger jerk movements, although no significant change was shown in the averaged jerk value.
In the comparison of the baseline evaluation to the post-evaluation, the vGRFs results of tBBT and pulley tasks show that the average vGRFs on the left foot tend to increase, whereas the average vGRFs on the right foot tend to decrease. The data from closeness to the Right may indicate that the participant was overcompensating by leaning more on the right foot while performing functional tasks during the baseline evaluation and that the training program may have contributed to the participant more effectively keeping the center of mass towards the midline of the body by more evenly distributing weight between the left foot and the right foot. The vGRFs results of box lift and bottle cap tasks show that the average vGRFs on the left foot tend to decrease, whereas the average vGRFs on the right foot tend to increase. The data from closeness to the Right may indicate that the participant was overcompensating by leaning more on the left foot while performing the bimanual tasks during the baseline evaluation. They also indicate that the training program may have contributed to the participant more effectively keeping the center of mass towards the midline of the body by more evenly distributing weight between the left foot and the right foot.
Muscle activation is expected to decrease as the participant becomes more adaptive to performing bimanual and unimanual tasks after the first two weeks of training []. However, the participant showed increased muscle activations across all muscles in all tasks during the post-evaluation when compared to baseline. The prosthetic hand opens and closes when the extensor carpi radialis and flexor digitorum profundus muscles activate, respectively. We suspect that the participant may have become more cognitively attuned to flexion as the muscle activation that opens the hand and may have translated that to more activation in all four muscles during the post-evaluation.
On the one hand, the statistical comparison was cautiously applied to some outcome measures. Wilcoxon ranksum test [], an equivalent to the t-test from a non-parametric category, was applied to the calculated value of joint angles, movement smoothness of hand module, vGRFs from the left side and right side, and four muscle activations at each normalized time point. On the other hand, we performed a direct comparison of task completion time, correlation coefficient values, and closeness to the Right, as the sample size was too small for each measure. As data are collected from more participants, the ranksum test will be utilized to compare all outcome measures to determine if there is a significant change in each measure.
To evaluate the effect of the training program and sensitivity of the selected outcome measures, ideally, all markers in every time frame should be captured by the Vicon system when the participant performs a task. However, a few technical aspects of motion capture data analysis may have compromised the evaluation. During a motion capture trial, part of the markers that were attached to the torso and upper extremities were blocked either by moving arms or moving objects in certain time frames. As a result, no marker position data were available to be used to calculate the instantaneous shoulder and trunk angles and movement smoothness for those time frames and to calculate the correlation coefficient (r value). To maintain data integrity, those time frames were not counted when calculating the mean and standard deviation of joint angles, the jerk, and the r value. To improve the marker capture rate in the future, a well-calibrated task space will be prepared for the motion capture system by reducing the optical obstruction coming from the test environment and task setup; a standing desk will be utilized with minimal surface area as the testing platform to further reduce the interference on motion capture caused by surface reflection. A minimal surface area where task items were placed may impose some challenge on an individual acclimating to a prosthesis. However, based on the feedback from the participants and our clinician, we currently do not think small surfaces will be that limiting to the participants. What matters most is the height of the table relative to the participant. If a table is too low or too high, that can impact how they compensate. The size of the table itself is usually not an issue. Nevertheless, we will continue checking on whether the minimal surface would impose undue stress on each participant as the research goes on.
The Ossur i-Limb used in this study has a passive wrist pronation/supination function and no wrist flexion/extension function, as a powered wrist function would add more length to the participant’s left limb to make her arms look asymmetrical. The participant needed to use her right hand to manually set the wrist unit to the proper pronation/supination angle at the beginning of each task. The wrist was kept at this angle throughout each task, which might have compromised the evaluation of the training effect and the sensitivity of outcome measures. One aim of future research would be to test a myoelectric arm with a powered wrist unit in which the pronation can be controlled by muscle signals like the hand, whereas the flexion/extension would still be passive.
There was an initial attempt to capture the finger movement to validate the gripping pattern of the hand module of the myoelectric arm by attaching the 4 mm markers to the anatomical landmarks on the fingers of the hand module during a preliminary evaluation on a device similar to Ossur i-Limb. However, these 4 mm markers turned out to be too small to be captured. Moreover, the Ossur hand module has a determined gripping pattern. Therefore, the finger markers were not attached during the actual i-Limb evaluation, as it might be redundant to capture the gripping pattern.
The correlation coefficient value was used to assess object control by evaluating hand–eye coordination. This is important because, without sensation from a prosthesis, users need to rely on vision to know if they are picking items up as they cannot feel it. We used the head marker movement to represent the eye movement for all evaluation tasks. This outcome measure might be suitable for a task such as tBBT when the eyes move along with the hand. However, it might not be a good indicator for the other four tasks reflected by the data in Table 1. A new outcome measure will be identified to assess object control for these tasks.
In terms of muscle activations, we did not collect the maximum voluntary contractions (MVC) for the selected muscles due to time constraints. Therefore, the reported muscle activation values were not normalized with respect to their MAVs, respectively. For the participants in the future, we will use Delsys EMG sensors to record the MVCs of the biceps, triceps, deltoid, and thoracolumbar muscles during both baseline and post-evaluation using the following procedure. The biceps MVC will be obtained by having the participant sit or stand with the forearm supported and the elbow flexed at a 90° angle and then instructing the participant to pull against a fixed resistance (e.g., a researcher’s hand) as hard as possible, focusing on elbow flexion. The triceps MVC will be obtained by positioning the participant with the forearm supported and the elbow extended at a 90° angle and then instructing them to push against a fixed resistance (e.g., a researcher’s hand), focusing on extending the elbow. To obtain the deltoid MVC, the participant will be positioned with the left arm abducted at a 90° angle from the side, and they will then be instructed to push against a fixed resistance (e.g., a researcher’s hand), focusing on the shoulder abduction. To obtain the thoracolumbar muscle MVC, the participant will be instructed first to lay prone on a mat with arms extended overhead and then to lift legs and chest off the ground, focusing on contracting the middle and lower back muscles.
Furthermore, the current research lacks user feedback to adequately capture the user’s satisfaction with the device. Recent studies have incorporated electroencephalography (EEG) to measure a participant’s satisfaction while controlling a robotic arm []. Other studies have found that surveys, such as the Reintegration to Normal Living Index, can accurately measure the level of satisfaction a user has regarding a prosthetic device []. Incorporating a means such as EEG and surveys to measure user satisfaction into this research would paint a clearer picture of the effectiveness of a training procedure and if the user has become more proficient at performing functional tasks.
In summary, future researchers should consider a few key limitations identified in this research. First, the participant may have become more cognitively attuned to the flexor muscle as the muscle responsible for opening the hand, which could have led to increased muscle activation due to abnormal muscle synergy during the post-evaluation. It is also important to point out that this research utilized a small sample size; future research may need to increase the sample size in terms of task number and trial number to improve the confidence of statistical assessment of changes as more participants will be recruited. Lastly, metrics of user satisfaction should be established to quantify the effectiveness of the evaluation protocol.
5. Conclusions
The results of this study demonstrated some improvements in user experience during both bimanual and unimanual tasks in post-training evaluation compared to baseline evaluation. An outcome measure to note was the task completion time, which showed improvement across all tasks except the bottle cap task. The research successfully employed an experimental protocol to capture data that quantified the users’ experience while using a transradial myoelectric arm prosthesis. Overall, these findings suggest that training and refined protocols may positively influence the user’s experience and functionality while using a transradial myoelectric prosthesis, contributing to the understanding of prosthesis performance and user satisfaction. The experimental protocol will be utilized for future work as the aim of this research is to collect and analyze data on more participants with transradial arm loss.
Author Contributions
Conceptualization, M.T., O.O., J.A. and J.C.; methodology, M.T., O.O., J.A., M.I., L.A.T. and J.C.; experiment evaluation, M.T., O.O., J.A. and J.C.; data collection and analysis, J.A., O.O., M.T. and J.C.; investigation, M.T., O.O., J.A., M.I., L.A.T. and J.C.; resources, L.A.T.; data curation, J.C.; writing—original draft preparation, M.T., J.C., O.O., J.A., M.I. and L.A.T.; funding acquisition, L.A.T. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by National Science Foundation of United States Waterman Award grant (No. 2229575) and National Institutes of Health of United States NIA MSTEM (No. 1R25AG067896).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the University of the District of Columbia (protocol code: #2136093-1).
Informed Consent Statement
Informed consent was obtained from the participants involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
Special thanks to Kimberly Kontson for providing us with insights into outcome measures with respect to the motion-capture-based evaluation of the myoelectric arm and lending the door-knob assessment tool.
Conflicts of Interest
Author Michelle Intintoli was employed by Medical Center Orthotics & Prosthetics (MCOP). The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Appendix A. i-Limb Access Training Program
- -
- The first three tasks are developed out of the UDC senior capstone project.
- Flex the elbow with the hand supine and close the hand using flexor muscles. Extend elbow to lower hand while opening i-Limb using extensor muscles.
- A family member or a researcher will hold a dowel vertically. From a standard anatomical position, reach out and grab the dowl, and then, while counting to five seconds, raise the dowel overhead. Movement should end at five seconds. Then, lower the dowel for five seconds till it is placed back in the researcher’s hand.
- In the seated position, pick up a small ball with a sound, unaffected, and non-prosthetic hand. With the prosthetic hand supine, place the ball in the center of the palm. Counting to five seconds, move the prosthetic hand with the ball in the palm over a six-inch divider. Movement should end at five seconds. Then, turn the wrist, open the hand, and let the ball fall onto the table.
- I-Limb Hand Iterative Training (essential training) []
Goal: This involves developing control of opening/closing, correct positioning of objects within the hand, and applying the appropriate strength of grip.
- Pick up objects
Objects (e.g., apples and cups) in the kitchen are picked up with the i-Limb hand by the user, who controls the opening and closing motion of the fingers. An example of this task can be seen here: https://res.cloudinary.com/ossur-dam/video/upload/q_auto:best/vc_auto/v1/Shared/i-Limb-Quantum_Stage-1_Picking-up-objects-3_Functional-Training-Video_en-global_19.webm?_a=ATAMhAA0 (accessed on 1 March 2025).
- b.
- Positioning the thumb
The user practices positioning the thumb in lateral or opposition in order to perform one of five gripping techniques (key, tripod, precision pinch, cylindrical, and hook grip) to pick up objects of different sizes and shapes. The reference video can be seen here: https://res.cloudinary.com/ossur-dam/video/upload/q_auto:best/vc_auto/v1/Shared/i-Limb-Quantum_Stage-1_Positioning-the-thumb-2_Functional-Training-Video_en-global_19.webm?_a=ATAMhAA0 (accessed on 1 March 2025).
- c.
- Varying the grip force
The user practices the task of releasing stacked paper cups and placing them side by side as shown in the video: https://res.cloudinary.com/ossur-dam/video/upload/q_auto:best/vc_auto/v1/Shared/i-Limb-Quantum_Stage-1_Varying-grip-force-2_Functional-Training-Video_en-global_19.webm?_a=ATAMhAA0 (accessed on 1 March 2025).
- 5.
- The user follows the instructions in the My i-Limb App to practice preprogrammed Automated Grips on the selected objects using i-Limb [].
Appendix B. Myoelectric Arm Evaluation Tasks (Figure A1)
Functional tasks:
- (1)
- Targeted Box and Blocks Test (tBBT) []: Transport 16 blocks, one at a time, over a partition using only the prosthesis, starting with the innermost left block and moving across each row, placing the block in its mirrored position (Figure A1a).
- (2)
- Bottle pour: Empty a squeeze bottle of water into a cup (Figure A1c).
- (3)
- Pulley: Reach overhead to grasp one ring suspended in the air on a pulley system, bring the rings down to the waist, and then control the placement of rings back in their suspended position (Figure A1d).
Bimanual tasks:
- (1)
- Bottle cap: Start with both hands placed in a relaxed position on the table in front of you. Reach and grasp the coffee cup with the unimpaired hand and bring the cup up at the chin level in front of you and 12 inches away from your body, then use the prosthetic hand to unscrew and open the cap of a coffee cup (two trials: one terminal) (Figure A1e).
- (2)
- Box Lift: Pick up the basket on the ground and place it on the table (Figure A1f).
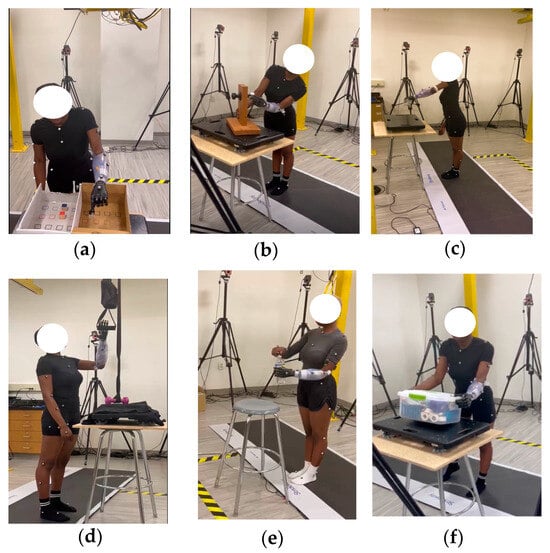
Figure A1.
Prothesis evaluation tasks: (a) Targeted Box and Blocks Test (tBBT); (b) Doorknob—AMULA; (c) Bottle pour; (d) Pulley (e) Bottle Cap; (f) Box Lift. Note: The Doorknob task was initially practiced. But it was removed in the actual evaluation of i-Limb Access as the hand module cannot grasp the knob.
References
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, and Committee on the Use of Selected Assistive Products and Technologies in Eliminating or Reducing the Effects of Impairments. The Promise of Assistive Technology to Enhance Activity and Work Participation; National Academies Press: Washington, DC, USA, 2017; Available online: http://www.ncbi.nlm.nih.gov/books/NBK453289/ (accessed on 1 August 2024).
- Orr, A.E. Rehabilitation for Persons with Upper Extremity Amputation. In Orthotics and Prosthetics in Rehabilitation, 4th ed.; Chui, K.K., Jorge, M.M., Yen, S.-C., Lusardi, M.M., Eds.; Elsevier: St. Louis, MO, USA, 2020; pp. 784–797. [Google Scholar] [CrossRef]
- Salminger, S.; Stino, H.; Pichler, L.H.; Gstoettner, C.; Sturma, A.; Mayer, J.A.; Szivak, M.; Aszmann, O.C. Current rates of prosthetic usage in upper-limb amputees—Have innovations had an impact on device acceptance? Disabil. Rehabil. 2022, 44, 3708–3713. [Google Scholar] [CrossRef] [PubMed]
- Marshall, C.; Barakat, T.; Stansby, G. Amputation and rehabilitation. Surg. Oxf. 2016, 34, 188–191. [Google Scholar] [CrossRef]
- Østlie, K.; Lesjø, I.M.; Franklin, R.J.; Garfelt, B.; Skjeldal, O.H.; Magnus, P. Prosthesis use in adult acquired major upper-limb amputees: Patterns of wear, prosthetic skills and the actual use of prostheses in activities of daily life. Disabil. Rehabil. Assist. Technol. 2012, 7, 479–493. [Google Scholar] [CrossRef]
- Soyer, K.; Ünver, B.; Tamer, S.; Ülger, Ö.G. The importance of rehabilitation concerning upper extremity amputees: A Systematic review. Pak. J. Med. Sci. 2016, 32, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Chau, T. Upper-limb prosthetics: Critical factors in device abandonment. Am. J. Phys. Med. Rehabil. 2007, 86, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Butkus, J.; Dennison, C.; Orr, A.; Laurent, M.S. Occupational Therapy with the Military Upper Extremity Amputee: Advances and Research Implications. Curr. Phys. Med. Rehabil. Rep. 2014, 2, 255–262. [Google Scholar] [CrossRef]
- Wright, V. Prosthetic Outcome Measures for Use with Upper Limb Amputees: A Systematic Review of the Peer-Reviewed Literature, 1970 to 2009. JPO J. Prosthet. Orthot. 2009, 21, P3–P63. [Google Scholar] [CrossRef]
- Hermansson, L.; Fisher, A.; Bernspång, B.; Eliasson, A.-C. Assessment of capacity for myoelectric control: A new Rasch-built measure of prosthetic hand control. J. Rehabil. Med. 2005, 37, 166–171. [Google Scholar] [CrossRef][Green Version]
- Jebsen, R.H.; Taylor, N.; Trieschmann, R.B.; Trotter, M.J.; Howard, L.A. An objective and standardized test of hand function. Arch. Phys. Med. Rehabil. 1969, 50, 311–319. [Google Scholar]
- Mathiowetz, V.; Volland, G.; Kashman, N.; Weber, K. Adult norms for the Box and Block Test of manual dexterity. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 1985, 39, 386–391. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Weber, K.; Kashman, N.; Volland, G. Adult Norms for the Nine Hole Peg Test of Finger Dexterity. Occup. Ther. J. Res. 1985, 5, 24–38. Available online: https://journals.sagepub.com/doi/abs/10.1177/153944928500500102 (accessed on 7 March 2025).
- Light, C.M.; Chappell, P.H.; Kyberd, P.J. Establishing a standardized clinical assessment tool of pathologic and prosthetic hand function: Normative data, reliability, and validity. Arch. Phys. Med. Rehabil. 2002, 83, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Bouwsema, H.; van der Sluis, C.K.; Bongers, R.M. The Role of Order of Practice in Learning to Handle an Upper-Limb Prosthesis. Arch. Phys. Med. Rehabil. 2008, 89, 1759–1764. [Google Scholar] [CrossRef] [PubMed]
- Bloomer, C.; Wang, S.; Kontson, K. Kinematic analysis of motor learning in upper limb body-powered bypass prosthesis training. PLoS ONE 2020, 15, e0226563. [Google Scholar] [CrossRef]
- Widehammar, C.; Holmqvist, K.L.; Hermansson, L. Training for users of myoelectric multigrip hand prostheses: A scoping review. Prosthet. Orthot. Int. 2021, 45, 393–400. [Google Scholar] [CrossRef]
- Law, M.; Cooper, B.; Strong, S.; Stewart, D.; Rigby, P.; Letts, L. The Person-Environment-Occupation Model: A Transactive Approach to Occupational Performance. Can. J. Occup. Ther. 1996, 63, 9–23. [Google Scholar] [CrossRef]
- Widehammar, C.; Pettersson, I.; Janeslätt, G.; Hermansson, L. The influence of environment: Experiences of users of myoelectric arm prosthesis—A qualitative study. Prosthet. Orthot. Int. 2018, 42, 28–36. [Google Scholar] [CrossRef]
- Thomas, K.U.; Scott, L.D. Biomechanics of Movement; MIT Press: Cambridge, MA, USA, 2021; Available online: https://mitpress.mit.edu/9780262044202/biomechanics-of-movement/ (accessed on 6 August 2024).
- Abdulla, S.Y. Becoming a Supple Leopard: The Ultimate Guide to Resolving Pain, Preventing Injury, and Optimizing Athletic Performance. J. Can. Chiropr. Assoc. 2014, 58, 328. [Google Scholar]
- Egermann, M.; Kasten, P.; Thomsen, M. Myoelectric hand prostheses in very young children. Int. Orthop. 2008, 33, 1101–1105. [Google Scholar] [CrossRef][Green Version]
- Powell, M.A.; Kaliki, R.R.; Thakor, N.V. User Training for Pattern Recognition-Based Myoelectric Prostheses: Improving Phantom Limb Movement Consistency and Distinguishability. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 522–532. [Google Scholar] [CrossRef]
- He, J.; Zhang, D.; Jiang, N.; Sheng, X.; Farina, D.; Zhu, X. User adaptation in long-term, open-loop myoelectric training: Implications for EMG pattern recognition in prosthesis control. J. Neural Eng. 2015, 12, 046005. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Romero, R.; Thompson, L.A. Motion Analysis of Balance Pre and Post Sensorimotor Exercises to Enhance Elderly Mobility: A. Case Study. Appl. Sci. 2023, 13, 889. [Google Scholar] [CrossRef]
- Kontson, K. Instructions for targeted Box and Blocks Test (tBBT). Available online: https://cdrh-rst.fda.gov/sites/default/files/2024-05/Instructions%20for%20targeted%20Box%20and%20Blocks%20Test-Jul22%202022.pdf (accessed on 31 January 2025).
- Creating An Evidence-Based Training Protocol for Upper Limb Bypass Prostheses. Available online: https://www.resna.org/sites/default/files/conference/2018/outcomes/Bloomer.html (accessed on 23 February 2025).
- Major, M.J.; Stine, R.L.; Heckathorne, C.W.; Fatone, S.; A Gard, S. Comparison of range-of-motion and variability in upper body movements between transradial prosthesis users and able-bodied controls when executing goal-oriented tasks. J. NeuroEngineering Rehabil. 2014, 11, 132. [Google Scholar] [CrossRef]
- Cutti, A.G.; Morosato, F.; Gruppioni, E.; Teti, G.; De Michieli, L.; Gentile, C. The Effect of the Poly-Articulated Prosthetic Hand on Shoulder and Trunk Compensatory Movements during Manipulation and Grasp Tasks. Prosthesis 2023, 5, 182–196. [Google Scholar] [CrossRef]
- Plug-in Gait Reference Guide. Available online: https://help.vicon.com/download/attachments/11378719/Plug-in%20Gait%20Reference%20Guide.pdf (accessed on 2 March 2025).
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-Source Software to Create and Analyze Dynamic Simulations of Movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef] [PubMed]
- Touillet, A.; Gouzien, A.; Badin, M.; Herbe, P.; Martinet, N.; Jarrassé, N.; Roby-Brami, A. Kinematic analysis of impairments and compensatory motor behavior during prosthetic grasping in below-elbow amputees. PLoS ONE 2022, 17, e0277917. [Google Scholar] [CrossRef]
- 33. Pancholi, S.; Joshi, A.M. Portable EMG Data Acquisition Module for Upper Limb Prosthesis Application. IEEE Sens. J. 2018, 18, 3436–3443. [Google Scholar]
- Alunan, A. Postural Stability in Unilateral Transtibial Amputees Using Two Suspension Systems: SmartpuckTM vs Lock and Pin. Master’s Thesis, University of Northern Colorado, Greeley, CO, USA, May 2021. Available online: https://digscholarship.unco.edu/theses/196 (accessed on 1 March 2025).
- Hong, C.-Y.; Guo, L.-Y.; Song, R.; Nagurka, M.L.; Sung, J.-L.; Yen, C.-W. Assessing postural stability via the correlation patterns of vertical ground reaction force components. Biomed. Eng. OnLine 2016, 15, 90. [Google Scholar] [CrossRef]
- Chen, J.; Hochstein, J.; Kim, C.; Tucker, L.; Hammel, L.E.; Damiano, D.L.; Bulea, T.C. A Pediatric Knee Exoskeleton with Real-Time Adaptive Control for Overground Walking in Ambulatory Individuals with Cerebral Palsy. Front. Robot. AI 2021, 8, 702137. [Google Scholar] [CrossRef]
- Wilcoxon, F. Individual Comparisons by Ranking Methods. In Breakthroughs in Statistics: Methodology and Distribution; Kotz, S., Johnson, N.L., Eds.; Springer: New York, NY, USA, 1992; pp. 196–202. [Google Scholar] [CrossRef]
- Kim, H.; Miyakoshi, M.; Kim, Y.; Stapornchaisit, S.; Yoshimura, N.; Koike, Y. Electroencephalography Reflects User Satisfaction in Controlling Robot Hand through Electromyographic Signals. Sensors 2023, 23, 277. [Google Scholar] [CrossRef]
- Demirdel, S.; Bayramlar, K. Reliability and Validity of the Turkish Reintegration to Normal Living Index in Amputees. OTJR Occup. Ther. J. Res. 2020, 40, 151–158. [Google Scholar] [CrossRef]
- i-Limb Hand Functional Therapy|Össur Academy Touch Solutions. Available online: https://www.ossur.com/en-us/prosthetics/upper-limb-training/i-limb/i-limb-hand-interactive-training (accessed on 31 January 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).