Abstract
Corpectomy is the surgical procedure of resecting a vertebral body or a part of it in order to decompress neural structures. Corpectomy is performed in patients with degenerative disease or cancer and following injury to the spine. We present a case of multilevel corpectomy in a female patient with massive degenerative disease associated with rheumatoid arthritis, combined with cervical myelopathy and osteoporosis. We present the case of a female patient who underwent C4-C5-C6 corpectomy and spinal stabilisation with a Cervical 3D Expandable cage and a cervical plate attached to the C3-C7 bodies. The rheumatoid arthritis caused degenerative changes, which, combined with the impact of environmental conditions and the patient’s postural defects, led to a pathological profile of the spine along the vertical and transverse axis, manifesting clinically as a cervical myelopathy with its characteristic neurological symptoms. Pre-operative imaging studies revealed a critical stenosis of the spinal canal. This report showcases an effective surgical technique for severe degenerative disease bearing an increased risk of tetraplegia that could be brought on by even a minor injury to the cervical spine in the presence of this kind of pathology. Multilevel cervical corpectomy can be an effective method for treating spinal canal stenosis to prevent the onset of neurological deficits. This procedure requires careful diagnostic work-up, surgical planning and an interdisciplinary approach, especially in patients with co-morbidities.
1. Introduction
This article sets out to present a rare case of C4-C5-C6 multilevel anterior cervical corpectomy with an expandable corpectomy prosthesis and a cervical plate in a female patient. Rheumatoid arthritis had led to degenerative changes causing a massive deformity of the cervical spine. Sequelae comprised compression of neural structures in the spinal canal and the presence of neurological deficits and cervical myelopathy causing increasing problems in ambulation and independent performance of basic living activities. The patient additionally presented with a number of co-morbidities, including osteoporosis. With these clinical circumstances, this case was particularly complicated with regard to both treatment planning and the surgical procedure itself. Cervical myelopathy is a progressive disorder secondary to spinal cord compression that may cause progressive neurological deficits such as muscle weakness, sensory deficits and difficulty performing fine movements, and, in extreme cases, the complete loss of physiological functions supplied by the damaged segment of the spinal cord [1]. In cases of advanced myelopathy secondary to significant displacement of vertebrae producing direct compression of the spinal cord, corpectomy is a necessary solution allowing for decompression of the spinal cord. Extensive spinal cord decompression by corpectomy aims to minimise further progression of the neurological deficits. After corpectomy, the operated segment of the spine needs to be stabilised, which is most often accomplished with a vertebral body prosthesis and a cervical plate [2,3,4,5,6]. Rheumatoid arthritis (RA), an autoimmune process, manifests as a chronic inflammation contributing to the destruction of articular surfaces and degeneration of the bone stock, which augments the risk of cervical spine instability and the possibility of damage to the spinal cord [7,8]. Osteoporosis, which often accompanies RA, decreases bone mineral density, making bones more susceptible to deformation, especially at sites subjected to mechanical stress [8,9]. This combination of disorders, leading to a decrease in bone mass, weakening of the trabecular structure of bone, destruction of chondral tissue and impaired wound healing [10], significantly compounded the level of difficulty and risk of the planned surgery, necessitating careful planning and precise execution of the procedure [11,12,13]. In this patient, the severe displacement of bony elements in the spinal canal, progressive neurological manifestations and a risk of severe complications required urgent surgery. Even a minor injury could lead to tetraplegia.
The aim of the study was to present a rare case of multilevel cervical corpectomy (C4-C5-C6) using an expandable vertebral body prosthesis and cervical plate in a patient with severe degenerative cervical spine disease, rheumatoid arthritis, and osteoporosis, focusing on the surgical challenges, clinical outcomes and the need for individualised treatment in complex cases.
2. Case Report
The patient was a 74-year-old woman known to have severe abnormalities of the spinal axes with cervical myelopathy caused by vertebral body compression of the spinal cord. She had a history of RA and osteoporosis of over 10 years. Evidence of RA was visible, especially in the hands. She gave a history of progressive myelopathy symptoms, including muscle weakness in the upper and lower extremities, difficulty moving about, impaired balance and significant pain in the right shoulder region. These symptoms considerably limited the patient’s daily functioning and independent performance of basic living activities. The patient had been receiving pharmacotherapy for RA and osteoporosis and saw her rheumatologist regularly. Supportive therapy included sessions of rehabilitation from time to time, which did not bring about spectacular effects, but their positive influence consisted chiefly in stimulating the patient to undertake physical activity, which was a key intervention in her case. Thanks to the rehabilitation, the patient was able to assume an erect position with the help of an assistant with a rehabilitation walker. Nevertheless, the patient reported significant and gradual deterioration of her physical condition within the preceding two years. In the period immediately preceding surgery, she could not leave her home. She would stand up with assistance only for self-care and her mobility was limited to a few steps. A clinical examination revealed muscle weakness of the whole body (Lovett 3). The most intense pain was felt in the region of the right shoulder and was accompanied by a definite limitation of the range of motion. The range of active motion was limited; passive movements could still be performed. Standing up was only possible with assistance and with a low walker. She was able to walk a maximum of 5 steps with a walker. She marked her pain intensity at 10 on a VAS scale. Her mJOA score was 11 points, indicating severe myelopathy. A Nurick score of 4 confirmed her advanced pathology. The decision to operate was taken on the basis of history, a physical examination and alarming data from imaging studies, with CT and MRI scans revealing severe degenerative disease of the cervical spine with a deformity, vertebral body displacement, critical stenosis and altered spinal cord signal typical of myelopathy, with all these findings being most prominent at the level of the C4 vertebral body (Figure 1).

Figure 1.
Pre-operative imaging studies: MRI scan (A) and CT scan (B) demonstrating degenerative disease and critical stenosis of the spinal canal. Sagittal views (A1,B1) and transverse views at the level of the C4 vertebral body (A2,B2).
The decision taken was to operate from an anterior approach. C4-C5-C6 corpectomy was performed with extensive decompression of the spinal canal/spinal cord. The next step was to mount an expandable vertebral body prosthesis Owing to adjustable height and angulation; the prosthesis can optimally fit the C3 and C7 vertebral bodies. A cervical plate was also put in place with the fixing screws in the C3 and C7 vertebral bodies. A possibility considered before the surgery was to perform additional spinal stabilisation from a posterior approach, but with a detailed analysis of the pre-operative imaging results, assessment of the bony structures and the finding of no subluxation of the posterior column within the facet joints, the final decision was to operate from an anterior approach only. The patient’s co-morbidities, the additional risk of complications associated with an additional incision and the quality of bone tissue were also taken into account for the decision. Accordingly, it was considered that an anterior approach would allow for sufficient decompression of neural structures while ensuring spinal stability. The course of the procedure was uneventful. A CT scan was obtained within the first post-operative day to inspect in detail the positioning of the bony structures, corpectomy implant and cervical plate. The appearances were typical post-operative CT appearances. With the assistance of a physiotherapist, the patient stood up on the second day post-surgery. Breathing, antithrombotic, active, passive–active and relaxation exercises were introduced. Finally, the patient’s condition allowed her to walk 10 m with a rehabilitation walker. She reported diminished pain in the right shoulder region, assessing her overall pain intensity at 6 on a VAS scale. An important parameter was her improved mood after the surgery, as she was now aware that her spine was protected from possible outcomes threatening her functioning. Her mobility was visibly better post-surgery. She was instructed about recommended exercises designed to expedite her convalescence and improve her physical ability. She was subsequently referred to a specialist rehabilitation centre where, under the care of a physiotherapist, she worked to gradually improve the range of motion of her cervical spine and generally increase muscle strength and mobility. The rehabilitation program included a combination of isometric and dynamic exercises tailored to her condition, focusing on strengthening the cervical and upper thoracic muscles while avoiding excessive strain on the spine. Additionally, the program incorporated balance training and postural correction exercises to enhance stability and reduce the risk of falls, which is particularly important in patients with osteoporosis. Regular follow-up assessments were conducted to monitor her progress and adjust the rehabilitation plan as needed, ensuring a safe and effective recovery process. Follow-up visits were scheduled together with follow-up imaging studies to assess the stability of the stabilisation system, the degree of spinal canal decompression and her overall and neurological health status. Follow-up cervical spine MRI and CT scans were obtained at three months post-surgery (Figure 2).
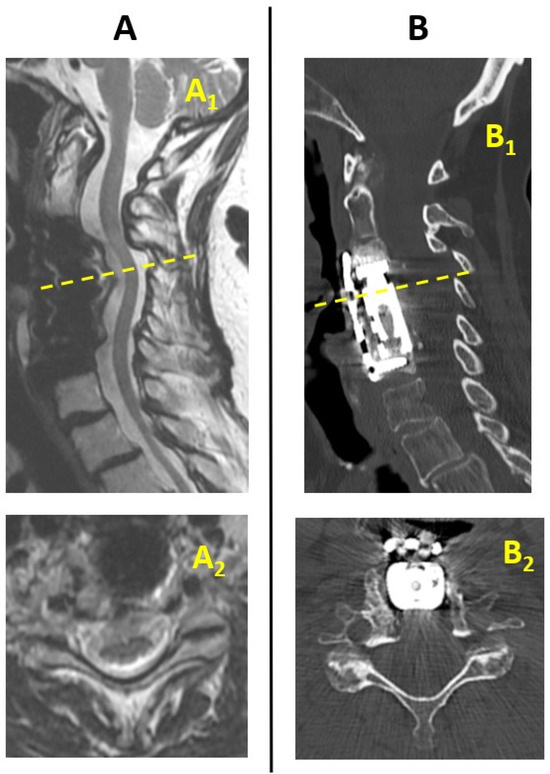
Figure 2.
Post-operative imaging studies: MRI scan (A) and CT scan (B) obtained at 3 months after the surgery showing the decompression and stability. Sagittal views (A1,B1) and transverse views at the level of the C4 vertebral body (A2,B2).
As the spinal CT appearances obtained immediately after the surgery and 3 months later were almost identical, we present an image from the 3 months’ CT scan to document the degree of decompression of the spinal canal and the arrangement of the stabilisation system. On the basis of the imaging results, we concluded that the stability of the cervical spine was intact. Accordingly, we decided against an additional stabilisation procedure from a posterior approach. The patient has been attending regular follow-up visits at a neurosurgery clinic. There is sustained improvement in her neurological status, mobility and independence compared to the situation before the surgery.
3. Discussion
The literature reports wide use of anterior cervical corpectomy and fusion with a variety of implants, including both static and expandable ones [4]. This procedure is an effective and safe option for treating degenerative disease of the cervical spine or traumatic cervical spine disorders. If performed correctly, it has a low rate of complications and revision surgery [5]. Expandable implants shorten surgical time, contribute to the achievement of appropriate vertebral height and restore balance in the sagittal axis [14]. Another study comparing clinical outcomes between static and expandable implants points to minimal risk of damage to vertebral endplates and, generally, points out the ability to restore near-anatomical spinal dimensions with expandable implants [15]. Achieving good implant placement is very much dependent on the choice of an appropriate implant size. In our patient, additional adjustments made it possible to precisely fit the implant to the adjacent vertebral bodies and, consequently, minimise the risk of inappropriate implant positioning [16]. The literature also indicates significant improvements in pain intensity and mobility in patients who received expandable cages [17]. These findings weighed on the operating team’s decision to use a Cervical 3D Expandable cage, which, by virtue of adjustable height and angulation, allowed sufficient anterior column support and stability.
Published reports suggest that multilevel corpectomy is an indication for using a fusion plate to ensure necessary support for the anterior spinal column. Another aspect of this procedure is the use of additional stabilisation placed from a posterior surgical approach. Research results are equivocal and indicate a number of factors that would weigh on a decision to use additional posterior stabilisation or not. Each case needs to be considered individually as indicated by the patient’s overall health, neurological status and imaging results. We based our choice of the surgical technique on a detailed assessment of the CT appearances of bony structures, which indicated the presence of a stable posterior column and absence of subluxations of facet joints and the risk of additional complications from performing additional stabilisation surgery (and using an additional posterior approach) [4,5,17,18].
Rheumatoid arthritis, which the patient had suffered from for a rather long time, is a significant risk factor for spinal deformities, often in the cervical segment, as in our patient. A chronic autoimmune condition affecting nearly 2% of the global population, RA contributes to damage to articular surfaces and, secondarily, to a significant deterioration of overall physical ability in patients [7,19,20]. In the case of our patient, considering the additional risk factors associated with RA and osteoporosis, such as increased risk of infection, intraoperative complications, implant-associated complications and the risk of revision surgery, the surgical team took the decision to perform the above-described procedures as they were indispensable for improving the patient’s health status. This decision was based on published reports on degenerative disease of the spine developing via diverse mechanisms, including those associated with RA and osteoporosis, and the experience of the surgical team [4,9,12,13,21,22].
Corpectomy with expandable implants is a preferred procedure in various spinal pathologies, such as spinal canal stenosis with spinal cord compression [23], fractures [24], spondylodiscitis [25] and spinal metastases [26]. The main objective of this procedure is to remove the pathology and reconstruct the anterior spinal column while ensuring stability of the operated segment [17]. Some interesting clinical cases of patients operated on with this procedure are adduced below, accounting for various attending risk factors. A case report of multilevel cervical corpectomy and segment reconstruction by A. Reig presents a severe pathological condition of the cervical spine of their female patient and the management scheme used to treat her problem. The author discusses the essence of a multidisciplinary and multifaceted approach to surgical planning and reports on possible complications arising from the extensive surgical procedure that corpectomy is. The report concludes by indicating a positive outcome of this procedure despite the patient’s extensive spinal pathology, thus raising hopes that patients’ level of comfort can be improved even in the presence of such severe pathologies of the cervical spine [27]. An article by Kinoshita H. presents the handling of corpectomy in a patient with a paravertebral giant-cell tumour. Despite pharmacotherapy with denosumab before the surgery, the lesion was so advanced that a corpectomy was necessary. The outcome of the surgery was positive and the tumour did not recur [28]. A similar case of corpectomy for a giant-cell tumour is described by Al- Shamary E., whose paper stresses that surgery is the mainstay of treatment for lesions of this type [29]. In turn, Loui K P. discusses the surgical procedure of corpectomy with fusion plate placement in a patient with symptoms of cervical myelopathy secondary to degenerative disease of the spine, emphasising the safety of this procedure and its significance for positive outcomes of spinal cord decompression. Loui points to several factors that help avoid adverse post-operative complications [3].
Finally, Saekhu M. describes the use of corpectomy in a 7-year-old boy who developed spinal cord compression as a result of vertebral body displacement following an injury to the neck. He presented typical symptoms of cervical myelopathy, including limited mobility of the upper and lower extremities and intense pain, in particular in the cervical spine. The surgery was clinically successful and the boy recovered his previous physical ability. This report confirms the safety level and efficacy of this procedure both in children and in adults [30].
4. Conclusions
Multilevel cervical corpectomy with an expandable prosthesis of vertebral bodies and a cervical plate can represent an optimal surgical procedure for severe degenerative conditions of the spine producing symptoms attributable to spinal canal stenosis and direct compression of the spinal cord, leading to cervical myelopathy. This procedure requires an individualised, multidisciplinary approach, especially in patients with multiple co-morbidities such as RA or osteoporosis. Critical components include the diagnostic process and a correct decision regarding the specifics of the surgical procedure. In our patient, the surgery turned out to be clinically beneficial, with the general and neurological condition described and imaging studies presented at the 3-month follow-up. However, it is important to note that the patient’s clinical status and imaging findings may evolve over a longer period, highlighting the need for extended follow-up to assess the durability of outcomes. This should not obviate the need for further studies of long-term outcomes of expandable implants in patients with RA and osteoporosis, which could result in the development of guidelines that would improve the safety level and efficacy of these procedures.
Author Contributions
Conceptualization, J.M. and B.G.; validation, J.M., A.J. and B.G.; investigation, A.J. and J.M.; resources, A.J. and J.M.; writing—original draft preparation, J.M. and A.J.; writing—review and editing, J.M.; supervision, B.G.; project administration, B.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
In accordance with local standards, the Institutional Review Board does not require ethical approval or institutional review board approval for reporting individual cases or case series when informed consent is provided by the patient. According to Article 31, Section 2 of the Act on the Professions of Doctor and Dentist, written informed consent was obtained from the patient for the disclosure of information included in this case report.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| RA | rheumatoid arthritis |
| CT | Computed Tomography |
| MRI | Magnetic Resonance Imaging |
References
- Zhang, A.S.; Myers, C.; McDonald, C.L.; Alsoof, D.; Anderson, G.; Daniels, A.H. Cervical Myelopathy: Diagnosis, Contemporary Treatment, and Outcomes. Am. J. Med. 2022, 135, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Foreman, M.; Foster, D.; Gillam, W.; Ciesla, C.; Lamprecht, C.; Lucke-Wold, B. Management Considerations for Cervical Corpectomy: Updated Indications and Future Directions. Life 2024, 14, 651. [Google Scholar] [CrossRef] [PubMed]
- Louie, P.K.; Nemani, V.M.; Leveque, J.A. Anterior Cervical Corpectomy and Fusion for Degenerative Cervical Spondylotic Myelopathy: Case Presentation with Surgical Technique Demonstration and Review of Literature. Clin. Spine Surg. 2022, 35, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Tohamy, M.H.; Osterhoff, G.; Abdelgawaad, A.S.; Ezzati, A.; Heyde, C.E. Anterior Cervical Corpectomy and Fusion with Stand-Alone Cages in Patients with Multilevel Degenerative Cervical Spine Disease Is Safe. BMC Musculoskelet. Disord. 2022, 23, 20. [Google Scholar] [CrossRef]
- Tatter, C.; Persson, O.; Burström, G.; Edström, E.; Elmi-Terander, A. Anterior Cervical Corpectomy and Fusion for Degenerative and Traumatic Spine Disorders, Single-Center Experience of a Case Series of 119 Patients. Oper. Neurosurg. 2020, 20, 8–17. [Google Scholar] [CrossRef]
- Luo, J.; Cao, K.; Huang, S.; Li, L.; Yu, T.; Cao, C.; Zhong, R.; Gong, M.; Zhou, Z.; Zou, X. Comparison of Anterior Approach versus Posterior Approach for the Treatment of Multilevel Cervical Spondylotic Myelopathy. Eur. Spine J. 2015, 24, 1621–1630. [Google Scholar] [CrossRef]
- Al-Daoseri, H.A.; Mohammed Saeed, M.A.; Ahmed, R.A. Prevalence of Cervical Spine Instability among Rheumatoid Arthritis Patients in South Iraq. J. Clin. Orthop. Trauma 2020, 11, 876–882. [Google Scholar] [CrossRef]
- Kirkham-Wilson, F.; Dennison, E. Osteoporosis and Rheumatoid Arthritis: A Review of Current Understanding and Practice. Br. J. Hosp. Med. 2024, 85, 1–11. [Google Scholar] [CrossRef]
- Tanaka, Y. Managing Osteoporosis and Joint Damage in Patients with Rheumatoid Arthritis: An Overview. J. Clin. Med. 2021, 10, 1241. [Google Scholar] [CrossRef]
- Roux, C. Osteoporosis in Inflammatory Joint Diseases. Osteoporos. Int. 2011, 22, 421–433. [Google Scholar] [CrossRef]
- Filley, A.; Baldwin, A.; Ben-Natan, A.R.; Hansen, K.; Arora, A.; Xiao, A.; Hammond, D.; Chen, C.; Tweedt, I.; Rohde, J.; et al. The Influence of Osteoporosis on Mechanical Complications in Lumbar Fusion Surgery: A Systematic Review. N. Am. Spine Soc. J. 2024, 18, 100327. [Google Scholar] [CrossRef] [PubMed]
- Honda, S.; Murata, K.; Sakamoto, M.; Shiroshita, A.; Saka, N.; Otsuki, B.; Shimizu, T.; Sono, T.; Masuda, S.; Shima, K.; et al. Effect of Rheumatoid Arthritis on Postoperative Outcomes in Patients with Lumbar Spinal Disorders: A Systematic Review and Meta-Analysis. Glob. Spine J. 2025; 21925682251318265 online ahead of print. [Google Scholar] [CrossRef]
- Song, Z.; Fan, L.; Wang, H.; Cao, J.; Wen, Z.; Tao, Y.; Zhang, X. Associated Factors of Osteoporosis in Chinese Patients with Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. J. Chin. Med. Assoc. 2024, 87, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Luo, G.; Xu, D.; Li, Y.; Wang, Z.; Yang, H.; Liu, Y.; Jia, Y.; Sun, T. Comparison of Radiological and Clinical Outcomes of 3D-Printed Artificial Vertebral Body with Titanium Mesh Cage in Single-Level Anterior Cervical Corpectomy and Fusion: A Meta-Analysis. Front. Surg. 2023, 9, 1077551. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.H.; Wu, P.K.; Wu, M.H.; Wong, K.W.; Li, W.W.; Chou, S.H. Comparison of the Radiographic and Clinical Outcomes Between Expandable Cage and Static Cage for Transforaminal Lumbar Interbody Fusion: A Systematic Review and Meta-Analysis. World Neurosurg. 2023, 179, 133–142. [Google Scholar] [CrossRef]
- Bębenek, A.; Dominiak, M.; Karpiński, G.; Pawełczyk, T.; Godlewski, B. Impact of Implant Size and Position on Subsidence Degree after Anterior Cervical Discectomy and Fusion: Radiological and Clinical Analysis. J. Clin. Med. 2024, 13, 1151. [Google Scholar] [CrossRef]
- Pojskic, M.; Saß, B.; Nimsky, C.; Carl, B. Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients. Medicina 2020, 56, 642. [Google Scholar] [CrossRef]
- Godlewski, B.; Bebenek, A.; Dominiak, M.; Bochniak, M.; Cieslik, P.; Pawelczyk, T. Reliability and Utility of Various Methods for Evaluation of Bone Union after Anterior Cervical Discectomy and Fusion. J. Clin. Med. 2022, 11, 6066. [Google Scholar] [CrossRef]
- Myasoedova, E.; Davis, J.; Matteson, E.L.; Crowson, C.S. Is the Epidemiology of Rheumatoid Arthritis Changing? Results from a Population-Based Incidence Study, 1985–2014. Ann. Rheum. Dis. 2020, 79, 440–444. [Google Scholar] [CrossRef]
- Radu, A.F.; Bungau, S.G. Management of Rheumatoid Arthritis: An Overview. Cells 2021, 10, 2857. [Google Scholar] [CrossRef]
- Streufert, B.D.; Onyedimma, C.; Yolcu, Y.U.; Ghaith, A.K.; Elder, B.D.; Nassr, A.; Currier, B.; Sebastian, A.S.; Bydon, M. Rheumatoid Arthritis in Spine Surgery: A Systematic Review and Meta-Analysis. Glob. Spine J. 2022, 12, 1583–1595. [Google Scholar] [CrossRef]
- Towner, J.E.; Li, Y.I.; Pieters, T.A.; Li, Y.M. Descriptive Analysis of 1972 Cervical Corpectomy Patients and 30-Day Postoperative Outcomes. Int. J. Spine Surg. 2020, 14, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Waschke, A.; Kaczor, S.; Walter, J.; Duenisch, P.; Kalff, R.; Ewald, C. Expandable Titanium Cages for Anterior Column Cervical Reconstruction and Their Effect on Sagittal Profile: A Review of 48 Cases. Acta Neurochir. 2013, 155, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Graillon, T.; Farah, K.; Rakotozanany, P.; Blondel, B.; Adetchessi, T.; Dufour, H.; Fuentes, S. Anterior Approach with Expandable Cage Implantation in Management of Unstable Thoracolumbar Fractures: Results of a Series of 93 Patients. Neurochirurgie 2016, 62, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Calvert, G.; May, L.A.; Theiss, S. Use of Permanently Placed Metal Expandable Cages for Vertebral Body Reconstruction in the Surgical Treatment of Spondylodiscitis. Orthopedics 2014, 37, e536–e542. [Google Scholar] [CrossRef]
- Alfieri, A.; Gazzeri, R.; Neroni, M.; Fiore, C.; Galarza, M.; Esposito, S. Anterior Expandable Cylindrical Cage Reconstruction after Cervical Spinal Metastasis Resection. Clin. Neurol. Neurosurg. 2011, 113, 914–917. [Google Scholar] [CrossRef]
- Reig, A.; Parker, S.L.; McGirt, M.J. Five-Level Sub-Axial Cervical Vertebrectomy and Reconstruction: Technical Report. Eur. Spine J. 2014, 23, 172–180. [Google Scholar] [CrossRef]
- Kinoshita, H.; Orita, S.; Yonemoto, T.; Ishii, T.; Iwata, S.; Kamoda, H.; Tsukanishi, T.; Inage, K.; Abe, K.; Inoue, M.; et al. Successful Total En Bloc Spondylectomy of the L3 Vertebra with a Paravertebral Giant Cell Tumor Following Preoperative Treatment with Denosumab: A Case Report. J. Med. Case Rep. 2019, 13, 116. [Google Scholar] [CrossRef]
- Al-Shamary, E.; Al-Dhafeeri, W.; Al-Sharydah, A.; Al-Suhibani, S.; Kussaibi, H.; Al-Issawi, W. Total Spondylectomy for Upper Thoracic Spine Giant Cell Tumor: A Case Report. Case Rep. Oncol. 2019, 12, 131–138. [Google Scholar] [CrossRef]
- Saekhu, M.; Ashari, S.; Tandian, D.; Nugroho, S.W. Anterior Cervical Corpectomy and Fusion in a 7-Year-Old Boy: A Case Report. Med. J. Indones. 2019, 28, 183–187. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).