Abstract
The management of spinal infections, such as spondylodiscitis, remains a complex challenge. With advancements in technology, spinal endoscopy has emerged as a promising minimally invasive approach. This systematic review and case series aims to evaluate the efficacy of endoscopic techniques in treating primary and post-operative spinal infections. A comprehensive literature review was conducted using databases such as PubMed, MEDLINE, and Cochrane Library, focusing on studies from 2000 to 2023. Our case series included patients treated with endoscopy for spinal infections in our institution between 2020 and 2023. The findings suggest that endoscopic techniques are associated with reduced tissue trauma, shorter hospital stays, and faster recovery, while maintaining comparable clinical outcomes to traditional open surgery. Despite the relatively high pathogen identification rates and favorable clinical outcomes, complications such as residual infection and the need for re-operations were noted. These results emphasize the need for further research to optimize endoscopic procedures in spinal infection management, potentially paving the way for this technique to become a standard treatment option.
1. Introduction
Spinal endoscopy, though introduced over two decades ago, has experienced rapid development in the last 10–15 years thanks to technological advancements [1]. Initially limited to the treatment of discopathies, its application now extends broadly within the realm of spinal degenerative diseases, including multi-level stenosis and spinal stabilization [2]. These advancements open new horizons, suggesting that the only limit to endoscopy’s application might be our imagination. The method’s utilization is also expanding into oncology [3] and spinal infections [4], where its minimally invasive approach and operation in a fluid environment—ensuring continuous irrigation of the surgical field—seem to be an ideal solution.
Spinal endoscopy, a minimally invasive technique used for diagnosing and treating various spinal conditions, has gained traction in recent years due to its favorable risk–benefit profile. The primary benefits of spinal endoscopy include reduced post-operative pain, shorter recovery times, and lower rates of complications compared to traditional open surgery. Patients typically experience a quicker return to normal activities, enhancing overall quality of life. However, risks associated with spinal endoscopy may include bleeding, infection, nerve injury, and incomplete decompression, necessitating careful patient selection and meticulous procedural execution. The relatively low complication rates, combined with the effectiveness in managing conditions like herniated discs and spinal stenosis, make spinal endoscopy an attractive option. Overall, as techniques and technologies advance, spinal endoscopy continues to evolve, promoting safer and more effective management of spinal disorders.
Spinal infections, while relatively rare, present significant public health concerns with varied epidemiological profiles. The estimated prevalence of spinal infections ranges from 0.2 to 2.0 cases per 100,000 individuals, with an incidence rate of approximately 2.5 to 18 cases per million annually [5]. The condition shows a male-to-female ratio of about 2:1, suggesting a higher susceptibility among males. The impact of spinal infections on activities of daily living (ADLs) can be profound, often leading to significant physical disability and impaired quality of life (QOL) [6]. Individuals may experience chronic pain, mobility issues, and psychological distress, ultimately reducing their ability to perform daily tasks. Furthermore, years lived with a disability (YLD) can be considerable, as many patients endure prolonged symptoms and complications, contributing to the global burden of disease (GBD) assessments that indicate substantial economic costs associated with healthcare utilization and loss of productivity. Other epidemiological data reveal an increasing incidence linked to risk factors such as diabetes, immunosuppression, and certain infectious conditions, underscoring the need for increased awareness and timely intervention.
Spinal infections, with their unique challenges, represent a promising domain for the application of endoscopy [2,7]. The intricacies of managing primary spondylodiscitis, alongside infections arising as post-operative complications, underscore the need for innovative treatment approaches. The aim of our article is to conduct a comprehensive literature review to assess whether endoscopy could herald a new standard in the treatment of these diverse spinal infections. This inquiry is enriched by the presentation of a series of our own cases, which illustrate the practical application of endoscopic techniques in both contexts. Our study endeavors not merely to map the current landscape of knowledge but also to illuminate the potential advantages and hurdles linked with the expanded use of endoscopy in the management of inflammatory spinal diseases. By doing so, we seek to underline endoscopy’s versatility and efficacy, whether confronting primary infections of the spine or tackling the complex challenges presented by post-operative infections. In exploring these facets, our article aims to contribute to a nuanced understanding of endoscopy’s role in advancing spinal infection therapy, paving the way for more targeted and less invasive interventions.
2. Materials and Methods
2.1. Study Design
This study was structured as a systematic literature review combined with a retrospective analysis of cases from our practice. We aimed to evaluate the efficacy and feasibility of endoscopic techniques in the management of spinal infections, including primary spondylodiscitis and infections secondary to spinal surgery. This review was conducted in alignment with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, ensuring a structured and transparent approach to data collection and analysis, and registered in the International Prospective Register of Systematic Reviews (PROSPERO) No. CRD42024528290.
2.2. Literature Search
A comprehensive search was conducted in databases including PubMed, MEDLINE, EMBASE, and the Cochrane Library. The search terms used were “spinal endoscopy” and “spondylodiscitis”, or “spinal infection”, or “postoperative spinal infection”. Both primary research articles and review articles, 24 in total with 996 participants, published in English from January 2000 to December 2023, were included. The search was supplemented by manual screening of references from relevant articles.
2.3. Inclusion and Exclusion Criteria
Studies were included if they reported on the use of endoscopic techniques in the treatment of spinal infections, detailing clinical outcomes, procedural details, and follow-up data. Exclusion criteria were studies focusing solely on traditional open-surgical techniques, non-infectious spinal conditions, and articles not available in full text or not in English.
2.4. Case Series
Our case series consisted of patients treated in our institution for spinal infections using endoscopic methods from January 2020 to December 2023. We included cases of primary spondylodiscitis and post-operative infections. Data collected included patient demographics, infection etiology, details of the endoscopic procedure, clinical outcomes, and any complications. We included the only three cases we encountered between 2020 and 2023.
2.5. Endoscopic Technique
The endoscopic procedure was performed using a standard protocol adapted for spinal infections. Under general anesthesia, with the patient in the prone position, a posterolateral approach was employed. The technique involved the use of a rigid endoscope for visualization and special endoscopic instruments for debridement, irrigation, and, if necessary, biopsy. Continuous irrigation with saline was used throughout the procedure to aid in the removal of infected material and reduce bacterial load. Then, the percutaneous screw fixation in a typical manner was performed. The specifics of the technique varied depending on the infection’s location and extent.
2.6. Data Analysis
Clinical outcomes were assessed based on the resolution of infection symptoms, improvement in pain scores using the Visual Analog Scale (VAS), and radiological evidence of infection resolution. Complications and recurrence of infection were also recorded. Descriptive statistics were used to summarize the findings from the literature review and our case series. In this analysis, a post hoc approach was employed to assess statistical power and effect size (Cohen’s d) for key clinical parameters, including pain (PAIN), Oswestry Disability Index (ODI), and inflammatory markers (CRP). The primary objective was to determine whether the sample size was sufficient to detect significant changes between pre- and post-operative outcomes.
The analysis utilized pooled standard deviation as a measure of variability across study groups, enabling precise effect size estimation and robust evaluation of clinical and statistical significance. Statistical power was calculated using the TTestPower tool from the Python statsmodels 0.14.4 library, incorporating parameters such as effect size, sample size, and significance level (alpha = 0.05).
The analysis was based on a rigorous statistical model that included the following:
- Mean values of outcomes before and after the intervention;
- Standard deviations before and after the intervention;
- Sample size in the study;
- A standard significance level of 0.05.
2.7. Ethical Considerations
For the retrospective analysis of patient cases, informed consent was waived due to the non-invasive nature of the review. However, patient confidentiality was rigorously maintained, with all data anonymized before analysis.
3. Results
The process of identifying and selecting studies followed a systematic approach. Initially, a total of 225 records were identified through a comprehensive database search. This included both peer-reviewed articles and relevant publications related to the topic of endoscopic treatment for spondylodiscitis.
The post hoc power analysis and effect size (Cohen’s d) calculations provide robust and clear evidence supporting the statistical and clinical significance of the study results. Key findings include the following:
- 1.
- Power Analysis: All analyzed data sets demonstrated near-perfect power (e.g., 0.977 in one case), indicating almost zero probability of Type II errors. This confirms that the sample size was sufficient to detect true differences between pre- and post-operative data.
- 2.
- Effect Size (Cohen’s d): The results indicate very large effect sizes (e.g., d = 1.460 for Wang, d = 1.149 for Lin, and d = 3.505 for Zheng). These values exceed standard thresholds for interpretation, signifying substantial, clinically meaningful changes in patients’ outcomes.
- 3.
- Pooled Standard Deviation (SD_pooled): The pooled standard deviations were computed as a measure of variability. For example, for Wang’s data (CRP), SD_pooled = 3.93, providing a robust basis for calculating effect size and power.
After removing 102 duplicate records, the remaining 123 records underwent screening based on their titles and abstracts. At this stage, 99 records were excluded, with 15 articles disqualified for being in non-English languages and 84 articles found to be unrelated to the scope of this review.
Following this, 24 full-text articles were assessed for eligibility, and one article was excluded for not focusing fully on endoscopic treatment.
Ultimately, 23 studies met the inclusion criteria and were included in the final systematic review (Figure 1). These studies exclusively focused on fully endoscopic techniques for treating spinal infections. This selection process ensured that the review maintained high relevance and focused on the most pertinent data available regarding endoscopic management of spondylodiscitis.
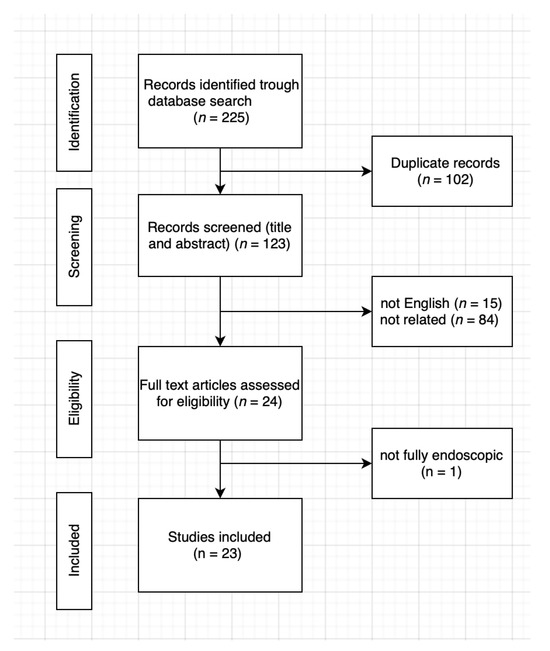
Figure 1.
Flowchart of study selection process.
3.1. Studies And Participants
A total of 23 studies were included in this systematic review, all focusing on the efficacy and outcomes of endoscopic treatment for spondylodiscitis. The studies encompass a range of retrospective case series, prospective cohort studies, and comparative analyses (Table 1). Of the included research, 95% was conducted between 2010 and 2023, reflecting the growing interest in minimally invasive techniques over the last decade. The sample sizes in these studies varied from small cohorts of 10 patients to larger groups exceeding 100 patients. Of the studies, 95% focused on adult populations, with a mean age ranging between 45 and 70 years. In some studies, detailed demographic data such as patient comorbidities, duration of symptoms, and the severity of infections were included, providing a comprehensive view of the treated populations.

Table 1.
Study characteristics: participant demographics, follow-up duration, and most commonly affected spinal levels.
3.2. Pathogens and Identification Rates
The studies included in this review reported a wide range of pathogens responsible for spondylodiscitis, with Staphylococcus aureus being the most frequently identified organism, found in 53% of all studies that identified pathogens. While 8% of studies included only patients with monomicrobial infections, 85% explored polymicrobial cases or refractory infections (Table 2). The most frequently reported pathogens were Staphylococcus aureus [7,10,17,20,25,26,27], Escherichia coli [15,25], and Pseudomonas aeruginosa [10,28]. In many cases, methicillin-resistant S. aureus (MRSA) was also reported, particularly in patients with more severe or refractory infections [16]. Other commonly identified pathogens included Streptococcus species and, occasionally, fungal organisms such as Candida [10,13]. Several studies also noted polymicrobial infections, which posed greater challenges in both diagnosis and treatment. The identification rates of pathogens varied between studies, ranging from 0.54 [18] to 0.9 [13], reflecting differences in diagnostic methods, sample sizes, and patient populations. These variations suggest the need for standardized diagnostic protocols to improve pathogen detection and tailor treatment strategies more effectively. Nevertheless, it should be emphasized that tuberculosis remains the most common cause of death due to an infectious, bacterial disease worldwide according to the World Health Organization [29], and the vertebral column is the most common site for osseous involvement by tuberculosis. Although, in our country, spinal tuberculosis is not very common, a resurgence of this disease has also been observed in developed countries [30]. Thus, 75% of studies presented in our study show that Mycobacterium tuberculosis is the pivotal agent of spinal infections in spontaneous spinal infections observed in developed countries.

Table 2.
Summary of identified pathogens and their identification rates.
3.3. Comparison with Other Surgical Techniques
Of the 24 studies included in this review, 25% provided direct comparisons between endoscopic treatments and more traditional surgical methods, such as open surgery or microdiscectomy [7,8,17,18,25,26]. These studies consistently highlighted the advantages of endoscopic techniques, particularly in terms of reduced tissue trauma, shorter recovery times, and lower complication rates. For example, patients who underwent endoscopic procedures generally experienced shorter hospital stays and faster returns to daily activities compared to those who had open surgeries. In terms of clinical outcomes, such as pain reduction and functional recovery, the results were comparable between endoscopic and traditional techniques. However, endoscopic approaches showed a lower incidence of wound infections and post-operative complications, likely due to the minimally invasive nature of the procedure [11,20]. Importantly, the studies did not demonstrate significant differences in long-term recurrence rates between the two methods, suggesting that endoscopic surgery is a viable and potentially superior alternative for the treatment of spondylodiscitis in appropriate cases.
3.4. Imaging Methods
Imaging played a crucial role in both the diagnosis and intra-operative guidance of endoscopic procedures for spondylodiscitis across the included studies. Pre-operative imaging most commonly involved magnetic resonance imaging (MRI), which was used to confirm the diagnosis, assess the extent of infection, and plan the surgical approach. MRI was particularly valuable in identifying abscesses, vertebral destruction, and spinal cord involvement. Intra-operatively, most studies employed fluoroscopy to guide the placement of instruments during endoscopic debridement or discectomy. Some studies also reported the use of computed tomography (CT) scans, either pre-operatively or post-operatively, to further evaluate bone integrity and ensure the completeness of infection removal [9]. Overall, the combination of MRI and fluoroscopy was the most frequently used imaging protocol, providing accurate visualization while minimizing radiation exposure. This imaging strategy contributed significantly to the precision and safety of endoscopic procedures, especially in complex or multi-level infections.
3.5. Follow-Up Periods and Clinical Outcomes
The included studies reported varying follow-up periods, ranging from 6 months to 5 years [9], with most studies having a mean follow-up duration of 12 to 24 months [7,8,20,24,26,31]. This range allowed for a comprehensive assessment of both short- and long-term outcomes of endoscopic treatment for spondylodiscitis (Table 3). Across the studies, clinical outcomes were generally favorable, with most patients experiencing significant reductions in pain and improvements in functional status within the first few months post-surgery [9,20]. Long-term follow-up data indicated sustained improvements in mobility and a low recurrence of infection in the majority of cases (Table 4). A few studies reported cases of re-infection or the need for additional surgical interventions, but these were typically associated with more severe pre-operative conditions or polymicrobial infections. Overall, the results suggest that endoscopic surgery not only provides effective short-term relief but also offers durable long-term outcomes for patients suffering from spondylodiscitis.

Table 3.
Summary of results for ODI, PAIN, and CRP (pre-op and post-op).

Table 4.
Comparison of clinical outcomes.
3.6. Data Analyses
All results demonstrate extremely high effect sizes, reflecting significant differences between pre- and post-intervention outcomes.
- PAIN: Effect sizes such as 10.425 for Suresh [26] and 9.615 for Duan [15] indicate a massive impact of the intervention on pain reduction. Even the lowest values (e.g., 4.152 for Zheng [20]) are far above the thresholds for large effects (0.8).
- ODI: Values of 5.205 for Wang [11] and 2.413 for Lin [13] confirm a substantial improvement in physical functioning, as measured by the Oswestry Disability Index (ODI).
- CRP: Effect sizes ranging from 1.149 to 3.505 (for Lin, Wang, and Zheng) demonstrate significant reductions in inflammatory markers, underscoring the intervention’s effectiveness in controlling inflammation.
Most results show a power of 1.000, indicating virtually zero probability of a Type II error (failing to detect a true effect). The only exception is Lin [13] (CRP), with a power of 0.977, which is still highly acceptable. The pooled standard deviations, ranging from 0.728 (Duan [15]) to 11.344 (Wang [11], ODI), reflect variability within the groups. Lower SD values (e.g., PAIN for Duan) indicate more precise data. These results highlight significant clinical benefits in reducing pain, improving physical functioning, and reducing inflammatory markers. Such large effect sizes indicate the high effectiveness of the methods used, while the high power of the study confirms the reliability of these findings.
3.7. Complications and Re-Operations
In most of the publications, no complications related to endoscopic procedures were reported, despite many cases involving high-risk patients with significant comorbidities. Even in studies that did report complications, such as Mireles-Cano et al. (3.3%) [25], Zheng et al. (4.8%) [20], and Huang et al. [4] and Fu et al. [17], these were minor and mainly involved sensory disturbances, such as paresthesia. Barber et al. [24], on the other hand, reported a 5.25% complication rate, though these complications were related to the stabilization component of the procedure rather than the endoscopic approach itself. This reinforces the notion that endoscopic procedures are associated with fewer and generally less severe complications compared to traditional open surgery. Additionally, re-operations were required in approximately 10% [17] of cases, primarily due to persistent infection or symptom recurrence (Table 5). However, the overall complication and re-operation rates for endoscopic surgery remain lower than those typically observed in open procedures, further supporting the safety and efficacy of minimally invasive techniques in the treatment of spondylodiscitis.

Table 5.
Comparison of pre-operative, discharge, and long-term CRP levels in relation to antibiotic duration and re-operation rates.
3.8. Case Series
3.8.1. Case Description No. 1: Endoscopic Treatment of Spondylodiscitis in a 50-Year-Old Female with Obesity
Patient Background: A 50-year-old female patient with a body mass index (BMI) of 32 was admitted to the neurology emergency department due to an acute spinal pain syndrome persisting for three days. The pain, VAS 7, was located in the lower spine, radiating bilaterally to both lower limbs, and exacerbated by movement. The patient had undergone a gynecological procedure under epidural anesthesia one month prior to this episode. Initial MRI (Figure 2) of the spine revealed a collapse of the L5/S1 space with a small central protrusion. The disc signal raised suspicion of early inflammatory changes in the eyes of the consulting neurosurgeon, though the radiologist conclusively denied inflammatory features. The patient presented with slightly elevated inflammatory markers, with a CRP level of 20 mg/L.

Figure 2.
Pre-operative T2 axial MRI image at the L5/S1 level on the day of the patient’s admission to the neurology department.
Diagnostic Evolution: After a week of conservative treatment without improvement, a follow-up MRI was ordered(Figure 3), which unambiguously identified spondylodiscitis with an abscess in the canal, causing compression of the dural sac and both S1 nerves (Figure 4). The patient’s pain syndrome worsened significantly, VAS 9 in the lower spine, leading to her qualification for surgical treatment.

Figure 3.
Pre-operative T2 sagittal MRI image at the L5/S1 level on the day of the patient’s admission to the neurology department.
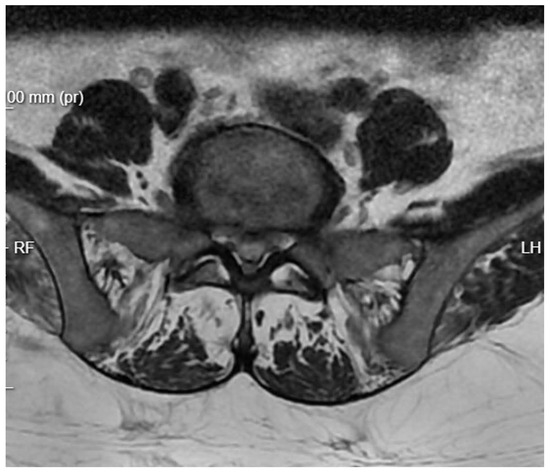
Figure 4.
Pre-operative T2 axial MRI image at the L5/S1 level one week after admission to the neurology department.
Surgical Intervention: The patient underwent an Interlaminar Endoscopic Lumbar Discectomy (IELD) with slight dilation of the right inferior articular process of L5. A minor fenestration of the ligamentum flavum was performed. Inflammatory granulation masses, which were pressing under the root and dural sac, were removed for culture (Figure 5). The procedure revealed a freely pulsating dural sac, indicating successful decompression. Subsequently, percutaneous transpedicular stabilization of L5/S1 was executed. Post-operatively, the patient reported a significant reduction in pain symptoms. Follow-up MRI showed a reduction in inflammatory changes.
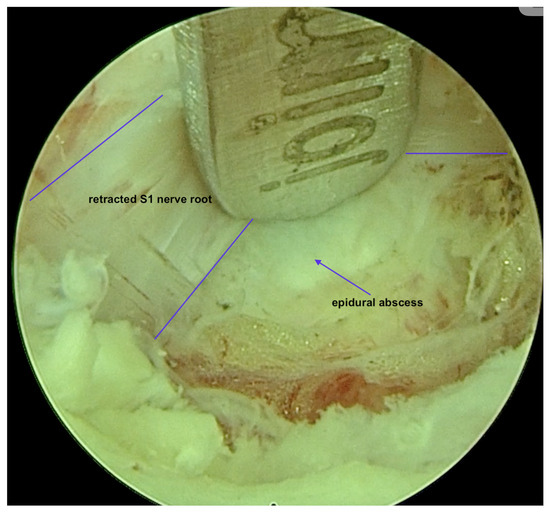
Figure 5.
Intra-operative view of a fully endoscopic debridement of an epidural abscess.
Post-operative Course and Antibiotic Therapy: Initially, an increase in inflammatory markers was observed, with CRP levels rising to 50 mg/L. However, over the following days of empirical antibiotic therapy (vancomycin + ceftriaxone + metronidazole), there was a gradual decrease in these levels. Cultures obtained during surgery returned sterile.
Outcome: The patient experienced a notable improvement in symptoms post-operatively, with VAS reduced to 2 and CRP dropped to a normal level, and with MRI confirming the reduction in inflammatory changes in the spine. Despite the initial spike in inflammatory markers, the patient responded well to empirical antibiotic therapy, underscoring the effectiveness of the combined endoscopic and stabilization approach in treating spinal infections complicated by abscess formation.
3.8.2. Case Description No. 2: Post-Operative Spinal Infection in a 70-Year-Old Male with Diabetes and Chronic Renal Failure
Patient Background: A 70-year-old male patient with a history of diabetes and chronic renal failure was scheduled for surgical treatment of discopathy at the L3/L4 level (Figure 6). The patient underwent microdiscectomy using a minimally invasive access retractor Spotlight (Johnson and Johnson, New Brunswick, NJ, USA).

Figure 6.
Pre-operative T2 sagittal MRI image at the L3/L4.
Post-operative Course: Initially, the patient reported significant pain relief and was mobilized and discharged home. However, two weeks post-discharge, he presented with copious watery discharge from the surgical wound.
Diagnostic Evaluation: Upon admission, the patient’s inflammatory markers were significantly elevated (CRP > 490 mg/L, procalcitonin = 1.13 ng/ML). An urgent re-operation was indicated due to the presence of inflammatory changes extending to the spinal canal. Cultures were taken, the wound was cleaned, and a drain was placed. Empirical antibiotic therapy with vancomycin, ceftriaxone, and metronidazole was initiated. Culture results later revealed an MSSA (Methicillin-Sensitive Staphylococcus aureus) infection, prompting the inclusion of cloxacillin and amikacin in the treatment regimen.
Clinical Challenges: Despite a decrease in inflammatory markers, the patient continued to experience severe pain that hindered mobilization, accompanied by persistent wound discharge. Follow-up MRI indicated persistent stenosis at the operated level, likely due to post-operative and inflammatory changes. A decision for further revision was made, leading to extensive decompression through laminotomy and removal of the entire ligamentum flavum at that level. An incidental dural tear occurred during the procedure and was sealed with Tachosil.
Subsequent Complications: Although there was temporary clinical improvement, acute pain returned after a few days. Two weeks later, the wound healed and the drain was removed, but the patient still reported disabling pain and exhibited a worsening of renal parameters due to the exacerbation of chronic renal failure, attributed to prolonged antibiotic therapy. Inflammatory markers rose again.
Further Intervention: Another MRI confirmed that despite extensive decompression, significant narrowing persisted at the operated level, with a markedly increased T2 signal in the disc space (Figure 7). A subsequent endoscopic transforaminal approach was employed. Inflammatory disc material and granulation tissue from the spinal canal were removed. Post-operative MRI showed a satisfactory degree of decompression of the canal. The patient was mobilized and transferred to the nephrology department due to further deterioration of renal function.
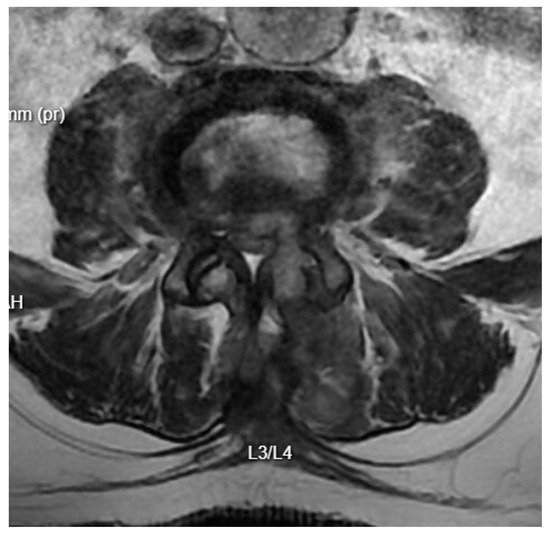
Figure 7.
T2 axial MRI image at the L4/L5 level following previous open surgical treatment.
Long-term Outcome: Two months later, after stabilization of his renal condition, the patient underwent control diagnostics. MRI results were satisfactory, and clinically, the patient was able to move with the assistance of a walker (Figure 8). The pain was moderate and allowed for relatively normal functioning. The patient was referred to the rehabilitation department for further improvement.
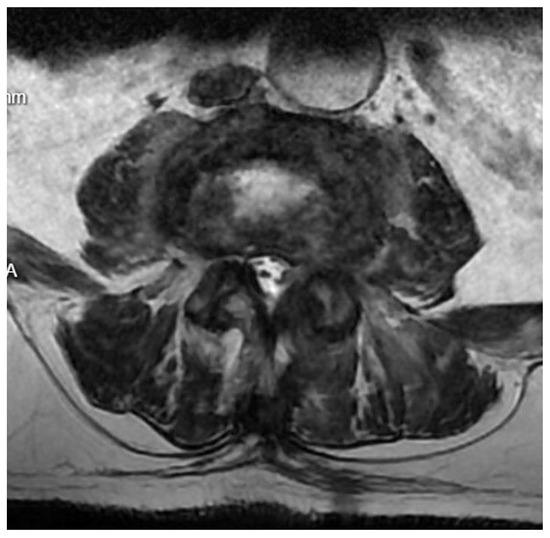
Figure 8.
T2 axial MRI image at the L4/L5 level following previous transforaminal endoscopic debridement.
3.8.3. Case Description No. 3: Spondylodiscitis in an HIV-Positive Patient, Endoscopic Revision Following Previous MISS Treatment
Patient Background: A 35-year-old male, known to be HIV-positive, was diagnosed due to dull pain in the thoracic spine. MRI diagnostics revealed a pathological fracture at the L1 level with a mass expanding towards the spinal canal, causing critical compression of the conus medullaris. Despite the dramatic radiological appearance, the patient exhibited only pain symptoms. A decision was made to perform stabilization using a percutaneous technique with biopsy of the lesion. During the procedure, it was determined that the lesion was fluid-filled, leading to a decision to expand the scope of the operation to include left-sided facetectomy of TH12/L1 and removal of the dense purulent content filling the spinal canal.
Diagnostic Evaluation: Cultures taken were sterile, and the patient was empirically treated with antibiotics until inflammatory markers decreased. He was discharged in good condition without pain. Six months later, the surgical site re-opened with purulent discharge seeping out. A new culture was taken, which returned sterile. Laboratory tests showed an increase in inflammatory markers, and the patient periodically experienced fever. CT scans showed the stabilization was in the correct position but without signs of bone fusion, and MR images showed inflammatory masses within the spinal canal (Figure 9 and Figure 10).
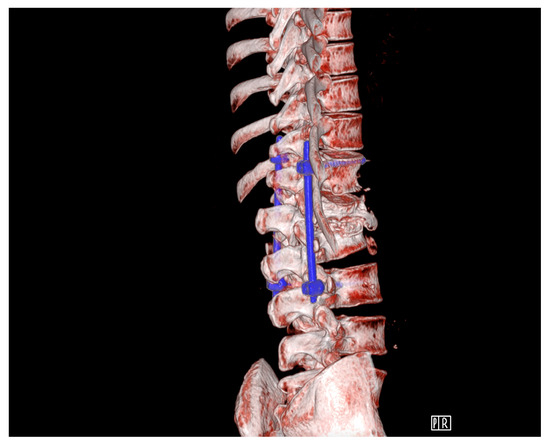
Figure 9.
Pre-operative transpedicular stabilization Th12-L3, CT 3D reconstruction.

Figure 10.
Pre-operative T2 sagittal MRI.
Clinical Intervention: A decision was made for endoscopic repair. Through the open wound at the posterior access, an 8 mm laminoscope was introduced medially from the rod into the spinal canal. Inflammatory granulation masses were gradually removed from the spinal canal and intervertebral space. Intra-operatively, moderate bleeding from the entire exposed surface of the boundary laminae presented considerable difficulty. More than 2 cubic centimeters of granulation tissue were removed. The wound was closed without placing a drain.
Post-operative Course: Post-operatively, cultures were again negative, and broad-spectrum antibiotic therapy led to a decrease in inflammatory markers. The patient reported improvement and was discharged on oral clindamycin, which was discontinued upon complete wound healing.
Long-term Outcome: The patient continued to recover well without any further complications or pain, showing satisfactory resolution of inflammation and maintenance of spinal integrity on subsequent follow-ups.
4. Discussion
Our study investigates the role of minimally invasive spinal endoscopy in the management of spinal infections, such as spondylodiscitis and post-operative infections. The findings demonstrate that spinal endoscopy offers several advantages, including reduced tissue trauma, shorter hospital stays, faster recovery, and outcomes comparable to traditional open surgery. Importantly, the pathogen identification rates were high, and the technique effectively managed pain and improved functional status. However, complications like residual infections and the need for re-operations, though infrequent, highlight areas for optimization. This research reinforces the growing potential of spinal endoscopy as a viable alternative to open surgery in managing complex spinal infections. The study addresses whether spinal endoscopy can serve as a safe and effective alternative to traditional surgical techniques for treating spinal infections, offering similar or superior clinical outcomes with fewer complications. The study contributes original insights into the application of spinal endoscopy for infections, a field where research is limited. It highlights endoscopy’s ability to manage infections with less morbidity compared to open surgery. The combination of a systematic review and a case series strengthens the relevance of the findings. Spinal infections pose significant challenges in management due to their complexity and potential for complications. Traditional open surgeries, while effective, are associated with greater surgical trauma. This study addresses the gap by evaluating a less invasive option, showcasing its efficacy and safety. The findings align with existing literature, which supports the use of minimally invasive techniques for faster recovery and fewer complications. However, this study uniquely combines a systematic review with real-world case analyses, providing a comprehensive perspective on clinical applicability.
Further research should focus on standardizing protocols for pathogen identification to improve diagnostic accuracy; conducting randomized controlled trials to compare long-term outcomes between endoscopic and traditional techniques; and evaluating the learning curve for surgeons adopting this method and its impact on outcomes, including diverse patient populations to validate results across varied clinical scenarios.
The management of spinal infections, including primary infections such as spondylodiscitis and secondary, iatrogenic post-operative infections, remains a complex and contentious issue in the clinical field [21,32]. Despite significant advancements in both diagnostic and therapeutic modalities, there is still no universally accepted guideline that delineates the optimal approach to treatment. Clinicians must often choose between conservative management, involving empirical or targeted antibiotic therapy, and surgical intervention, which can range from simple debridement to more complex procedures involving spinal stabilization [33]. Each of these treatment pathways comes with its own set of potential benefits and drawbacks, making the decision-making process highly individualized and dependent on patient-specific factors.
Conservative treatment, which typically involves bed rest, immobilization, and prolonged antibiotic therapy, has been the cornerstone of managing spondylodiscitis for decades [34]. However, this approach, while avoiding surgical risks, is associated with prolonged hospital stays, the need for immobilization, and often significant residual pain. Success rates of conservative treatment hover around 75–80%, as reported in various studies, with approximately 20–25% of patients ultimately requiring surgical intervention due to persistent or worsening symptoms, especially in cases involving neurological deficits [34].
Surgical intervention is generally reserved for those cases where conservative measures fail or when a rapid deterioration in neurological status occurs. The objectives of surgery include the identification of the causative pathogen—particularly when laboratory tests are inconclusive—debridement of infected tissues, stabilization of the affected spinal segments, and overall improvement in the patient’s quality of life. Various surgical techniques have been employed, ranging from needle biopsies and flow-through drainage to more invasive procedures such as discectomy, Extreme Lateral Interbody Fusion (XLIF), and posterior spinal fixation [35,36]. Recently, the focus has shifted towards minimally invasive techniques, with endoscopic spinal surgery gaining traction as a viable alternative to traditional open procedures.
Several studies have highlighted the potential advantages of endoscopic techniques in the management of spinal infections. For instance, Mireles-Cano et al. (2023) [25] compared fluoroscopy-guided percutaneous transpedicular biopsy with posterolateral endoscopy in a cohort of 30 patients, finding that the endoscopic approach had a higher rate of pathogen identification (14 out of 30 cases) compared to the fluoroscopy-guided method (12 out of 30 cases). These findings are echoed in other studies that demonstrate the efficacy of endoscopic procedures not only in pathogen identification but also in significantly reducing pain, as measured by visual analogue scale (VAS) scores.
Further comparisons between various surgical techniques reveal that endoscopic approaches often result in better outcomes in terms of pain relief and functional recovery. For example, Suresh et al. [26] reported a significant reduction in VAS scores—from a pre-operative mean of 9.25 to 0.67 one year post-operatively—following antibiotic instillation and posterior discectomy in 12 patients. Similarly, Hongwei et al. [37] observed an improvement in VAS scores from 6.8 pre-operatively to 1.0 post-operatively in a study involving 30 patients treated with XLIF and posterior fixation. The use of endoscopic techniques in these cases not only facilitated pathogen identification but also contributed to more rapid and sustained pain relief.
In another study, Manabu et al. (2007) [8] evaluated posterolateral spinal endoscopic surgery in 15 patients, achieving pathogen identification in 11 out of 15 cases. This study reported a reduction in VAS scores from 8.6 pre-operatively to 2.5 one week post-operatively, with further improvement to 1.4 at three weeks. Such outcomes suggest that endoscopic approaches may offer a superior alternative to more invasive surgical techniques, particularly in terms of patient recovery and post-operative pain management.
Duan et al. (2019) [15] further explored the benefits of percutaneous endoscopic debridement combined with percutaneous pedicle screw fixation in 45 patients. Their findings were notable, with pathogen identification in 32 cases and a reduction in VAS scores from 7.5 pre-operatively to 0.5 during a follow-up period of six to 24 months. These results underscore the potential of minimally invasive endoscopic surgery not only for effective infection control but also for achieving long-term pain relief and functional improvement.
The efficacy of endoscopic procedures is also supported by our own case series, which demonstrated significant improvements in patient outcomes even when the causative pathogen was not identified. In one case, despite the absence of pathogen identification, the patient experienced a marked reduction in pain and an improvement in quality of life following surgery. Another patient with a known pathogen from a previous operation showed similar improvements. These findings suggest that the benefits of endoscopic surgery may extend beyond mere pathogen identification, offering substantial clinical value in terms of pain management and overall patient well-being.
In addition to these individual studies, several systematic reviews and meta-analyses have reinforced the growing role of spine endoscopy in the management of spinal infections. For instance, a systematic review by Barber et al. (2022) [24], which included data from 188 patients, reported an average positive culture rate of 76% with significant reductions in VAS scores post-operatively. The review also highlighted the relatively low complication rates associated with endoscopic procedures, further cementing their role as a viable and effective alternative to traditional open surgery.
Similarly, Abreu et al. (2021) [21] performed a systematic review of 14 studies involving 342 participants, reporting microorganism identification rates ranging from 54.2% to 90.4% and significant improvements in pain and functional status following endoscopic procedures. These reviews collectively emphasize the advantages of minimally invasive techniques, including reduced surgical trauma, lower blood loss, faster recovery times, and effective infection control, making endoscopic approaches particularly attractive for high-risk patients who may not tolerate more invasive surgical options.
The endoscopic method, although it offers many advantages, is not without its limitations. First and foremost, it requires the surgeon to have appropriate experience and advanced technical skills. Acquiring such competencies can be time-consuming, which means this technique is associated with a relatively long learning curve. Therefore, before opting for the endoscopic approach, the surgeon should not be bold and realistically assess their skills and experience in performing such procedures. Additionally, the patient’s anatomical conditions may pose a significant challenge. Limited space and difficult access to neural structures can potentially reduce the effectiveness of the procedure.
Of course, there are key limitations to this study, including the retrospective design; for instance, the case series relied on retrospective data, which may introduce biases. Sample size, which consists of a limited number of cases from a single institution, reduces generalization. Furthermore, heterogeneity, as demonstrated by variability in patient conditions, techniques, and follow-up durations, limits direct comparability. Last is the lack of randomized comparisons—particularly, a control group treated with open surgery for direct efficacy comparison. No prior power analysis was conducted to ensure the adequacy of the sample size.
By addressing these limitations in future studies, the evidence for the spinal endoscopy role in infection management can be significantly strengthened.
5. Conclusions
The cumulative evidence strongly supports the efficacy and safety of minimally invasive endoscopic treatment for spinal infections. While traditional open surgery remains a cornerstone of treatment for many cases, the increasing adoption of endoscopic techniques offers a promising alternative, particularly for patients who are poor candidates for conventional surgery. However, despite the encouraging results, further research is needed to refine these techniques and establish clear guidelines for their use in clinical practice. The ongoing evolution of endoscopic technology and its application in spine surgery is likely to continue shifting paradigms in the management of spinal infections, with the potential to improve patient outcomes significantly.
Author Contributions
Conceptualization, K.Ł. and D.Ł.; methodology, K.Ł.; software, D.P.; validation, D.P., T.K. and W.K.; formal analysis, M.T.; investigation, K.D.; resources, B.Ł.-R.; data curation, K.Ł.; writing—original draft preparation, K.Ł., D.Ł., W.K. and K.D.; writing—review and editing, K.Ł. and K.D.; visualization, D.P.; supervision, D.Ł.; project administration, M.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
In accordance with the policy of our institution, case descriptions do not require the approval of the Institutional Review Board or an ethics committee (Decision No. L.dz. 83800.0050.44.2024). All patients described in the case report section have provided both verbal and written consent for publication.
Informed Consent Statement
Written informed consent was obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| FELD | Full Endoscopic Lumbar Discectomy |
| MRI | Magnetic Resonance Imaging |
| ODI | Oswestry disability index |
| IELD | Interlaminar Endoscopic Lumbar Discectomy |
| VAS | Visual Analogue Scale |
| CT | Computer Tomography |
| CRP | C-Reactive Protein |
| PRISMA | Preferred Reporting Items for Systematic reviews and Meta-Analyses |
| PROSPERO | International prospective register of systematic reviews |
| MRSA | The International Prospective Register of Systematic Reviews |
| ESBL | Extended Spectrum Beta-Lactamase |
| BMI | Body Mass Index |
| HIV | Human Immunodeficiency Virus |
| XLIF | Extreme Lateral Interbody Fusion |
| MSSA | Methicillin-Susceptible Staphylococcus Areus |
| NRS | Numeric Rating Scale |
References
- Gibson, J.N.; Cowie, J.G.; Iprenburg, M. Transforaminal endoscopic spinal surgery: The future ‘gold standard’ for discectomy?—A review. Surgeon 2012, 10, 290–296. [Google Scholar] [CrossRef]
- Gunjotikar, S.; Pestonji, M.; Tanaka, M.; Komatsubara, T.; Ekade, S.J.; Heydar, A.M.; Hieu, H.K. Evolution, Current Trends, and Latest Advances of Endoscopic Spine Surgery. J. Clin. Med. 2024, 13, 3208. [Google Scholar] [CrossRef] [PubMed]
- Latka, K.; Kołodziej, W.; Pawlak, K.; Sobolewski, T.; Rajski, R.; Chowaniec, J.; Olbrycht, T.; Tanaka, M.; Łątka, D. Fully Endoscopic Spine Separation Surgery in Metastatic Disease—Case Series, Technical Notes, and Preliminary Findings. Medicina 2023, 59, 993. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Gu, Q.; Song, J.; Yan, F.; Lin, X.L. The effectiveness of percutaneous endoscopic lumbar discectomy combined with external lumbar drainage in the treatment of intervertebral infections. Front. Surg. 2022, 9, 975681. [Google Scholar] [CrossRef] [PubMed]
- Nayak, N.R.; Stephen, J.H.; Piazza, M.A.; Obayemi, A.A.; Stein, S.C.; Malhotra, N.R. Quality of Life in Patients Undergoing Spine Surgery: Systematic Review and Meta-Analysis. Glob. Spine J. 2019, 9, 67–76. [Google Scholar] [CrossRef]
- Koleck, M.; Mazaux, J.M.; Rascle, N.; Bruchon-Schweitzer, M. Psycho-social factors and coping strategies as predictors of chronic evolution and quality of life in patients with low back pain: A prospective study. Eur. J. Pain 2006, 10, 1–11. [Google Scholar] [CrossRef]
- Wang, X.; Zhou, S.; Bian, Z.; Li, M.; Jiang, W.; Hou, C.; Zhu, L. Unilateral percutaneous endoscopic debridement and drainage for lumbar infectious spondylitis. J. Orthop. Surg. Res. 2018, 13, 306. [Google Scholar] [CrossRef]
- Ito, M.; Abumi, K.; Kotani, Y.; Kadoya, K.; Minami, A. Clinical Outcome of Posterolateral Endoscopic Surgery for Pyogenic Spondylodiscitis Results of 15 Patients With Serious Comorbid Conditions. Spine 2007, 32, 200–206. [Google Scholar] [CrossRef]
- Chen, H.T.; Lin, C.Y.; Chang, C.C.; Chen, Y.J.; Tsai, C.H.; Tsou, H.K.; Lin, C.S.; Ho, M.W.; Hsu, H.C. Observational Study New Strategy for Minimally Invasive Endoscopic Surgery to Treat Infectious Spondylodiscitis in the Thoracolumbar Spine. Pain Physician 2019, 22, 281–293. [Google Scholar] [CrossRef]
- Yang, S.C.; Chen, W.J.; Chen, H.S.; Kao, Y.H.; Yu, S.W.; Tu, Y.K. Extended indications of percutaneous endoscopic lavage and drainage for the treatment of lumbar infectious spondylitis. Eur. Spine J. 2014, 23, 846–853. [Google Scholar] [CrossRef]
- Wang, S.F.; Tsai, T.T.; Li, Y.D.; Chiu, P.Y.; Hsieh, M.K.; Liao, J.C.; Lai, P.L.; Kao, F.C. Percutaneous Endoscopic Interbody Debridement and Fusion (PEIDF) Decreases Risk of Sepsis and Mortality in Treating Infectious Spondylodiscitis for Patients with Poor Physical Status, a Retrospective Cohort Study. Biomedicines 2022, 10, 1659. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.; Barot, M.P.; Dave, B.R.; Bang, P.; Devanand, D.; Patel, D.; Jain, A. Percutaneous transforaminal endoscopic discectomy and drainage for spondylodiscitis: A technical note and review of literature. J. Orthop. Spine 2018, 6 (Suppl. S1), S16–S20. [Google Scholar] [CrossRef]
- Lin, G.X.; Kim, J.S.; Sharma, S.; Sun, L.W.; Wu, H.H.; Chang, K.S.; Chen, Y.C.; Chen, C.M. Full Endoscopic Discectomy, Debridement, and Drainage for High-Risk Patients with Spondylodiscitis. World Neurosurg. 2019, 127, e202–e211. [Google Scholar] [CrossRef]
- Youn, M.S.; Shin, J.K.; Goh, T.S.; Lee, J.S. Minimally invasive percutaneous endoscopic treatment for acute pyogenic spondylodiscitis following vertebroplasty. Eur. Spine J. 2018, 27, 458–464. [Google Scholar] [CrossRef]
- Duan, K.; Qin, Y.; Ye, J.; Zhang, W.; Hu, X.; Zhou, J.; Gao, L.; Tang, Y. Percutaneous endoscopic debridement with percutaneous pedicle screw fixation for lumbar pyogenic spondylodiscitis: A preliminary study. Int. Orthop. 2020, 44, 495–502. [Google Scholar] [CrossRef]
- Kolcun, J.P.G.; Wang, M.Y. Endoscopic Treatment of Thoracic Discitis with Robotic Access: A Case Report Merging Two Cutting-Edge Technologies. World Neurosurg. 2019, 126, 418–422. [Google Scholar] [CrossRef]
- Fu, T.S.; Wang, Y.C.; Lin, T.Y.; Chang, C.W.; Wong, C.B.; Su, J.Y. Comparison of percutaneous endoscopic surgery and traditional anterior open surgery for treating lumbar infectious spondylitis. J. Clin. Med. 2019, 8, 1356. [Google Scholar] [CrossRef]
- Kono, M.; Koda, M.; Abe, T.; Miura, K.; Nagashima, K.; Fujii, K.; Kumagai, H.; Noguchi, H.; Funayama, T.; Yamazaki, M. Percutaneous endoscopic discectomy might be effective in selected cases of pyogenic spondylitis. J. Orthop. Surg. 2019, 27, 2309499019885446. [Google Scholar] [CrossRef]
- Kang, T.; Park, S.Y.; Lee, S.H.; Park, J.H.; Suh, S.W.; Hospenthal, D.R. Spinal epidural abscess successfully treated with biportal endoscopic spinal surgery. Medicine 2019, 98, e18231. [Google Scholar] [CrossRef]
- Zheng, Q.; Ying, X.; Jin, Y.; Zhu, B.; Shen, J.; Wang, Y.; Zheng, M.; Liu, F. Treatment of single-segment suppurative spondylitis with the transforaminal endoscopic focal cleaning and drainage. J. Spinal Cord Med. 2021, 44, 267–275. [Google Scholar] [CrossRef]
- Abreu, P.G.P.; Lourenço, J.A.; Romero, C.; d’Almeida, G.N.; Pappamikail, L.; Lopes, M.F.; Brito, M.; Teles, P.; Correia, J.P. Endoscopic treatment of spondylodiscitis: Systematic review. Eur. Spine J. 2022, 31, 1765–1774. [Google Scholar] [CrossRef]
- Ishihama, Y.; Sakai, T.; Manabe, H.; Tezuka, F.; Yamashita, K.; Takata, Y.; Maeda, T.; Sairyo, K. CASE REPORT Debridement for Infectious Spondylodiscitis in a 9-year-old Girl Using Full-Endoscopic Discectomy System: A Case Report and literature review. J. Med. Investig. 2020, 67, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, F.H.P.; Henriques, C.E.P.; Moreira, D.L.; Leira, F.N.; Reis, R.D.D. Endoscopic Approach at Two Non-Sequential Levels in Lumbar Discitis. Cureus 2022, 14, e22158. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.M.; Sofoluke, N.; Reardon, T.; Telfeian, A.; Konakondla, S. Treatment of Refractory Multilevel Thoracic Spondylodiscitis Using Ultra-Minimally Invasive Endoscopic Approach for Debridement and Drainage: A Technical Note, Intraoperative Video, and Literature Review. World Neurosurg. 2022, 167, e456–e463. [Google Scholar] [CrossRef] [PubMed]
- Mireles-Cano, N.; Álvarez-Canales, J.A.; Huitrón-García, M.J.; Quezada, M.; Macías, A.E.; Mosqueda-Gómez, J.L. Fluoroscopy-Guided Percutaneous Transpedicular Biopsy Versus Posterolateral Endoscopy for Infective Spondylodiskitis Diagnosis: A Comparative Study. World Neurosurg. 2023, 170, e827–e833. [Google Scholar] [CrossRef]
- Suresh, V.; Suresh, H.S.; Raju, B.; Jindal, H.; Ozair, A. Management of Postoperative Discitis with Debridement and Novel Technique of Local Antibiotic Instillation: Functional Outcomes from a Resource-Limited Setting. World Neurosurg. 2024, 181, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Huang, T.L.; Chen, Y.J.; Tsou, H.K.; Lin, W.C.; Hung, C.H.; Tsai, C.H.; Hsu, H.C.; Chen, H.T. A minimally invasive endoscopic surgery for infectious spondylodiscitis of the thoracic and upper lumbar spine in immunocompromised patients. BioMed Res. Int. 2015, 2015, 780451. [Google Scholar] [CrossRef]
- Fu, T.S.; Chen, L.H.; Chen, W.J. Minimally invasive percutaneous endoscopic discectomy and drainage for infectious spondylodiscitis. BioMed J. 2013, 36, 168–174. [Google Scholar] [CrossRef]
- Trecarichi, E.M.; Di Meco, E.; Mazzotta, V.; Fantoni, M. Tuberculous spondylodiscitis: Epidemiology, clinical features, treatment, and outcome. Eur. Rev. Med. Pharmacol. Sci. 2012, 16 (Suppl. S2), 58–72. [Google Scholar]
- Tay, B.K.; Deckey, J.; Hu, S.S. Spinal infections. J. Am. Acad. Orthop. Surg. 2002, 10, 188–197. [Google Scholar] [CrossRef]
- Lin, G.X.; Sun, L.W.; Jhang, S.W.; Chen, C.M.; Rui, G.; Hu, B.S. Postoperative Pain Management after Full Endoscopic Lumbar Discectomy: An Observational Study. Medicina 2022, 58, 1817. [Google Scholar] [CrossRef] [PubMed]
- Ogihara, S.; Yamazaki, T.; Inanami, H.; Oka, H.; Maruyama, T.; Miyoshi, K.; Takano, Y.; Chikuda, H.; Azuma, S.; Kawamura, N.; et al. Risk factors for surgical site infection after lumbar laminectomy and/or discectomy for degenerative diseases in adults: A prospective multicenter surveillance study with registry of 4027 cases. PLoS ONE 2018, 13, e0205539. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, J.E.; Eichholz, K.M.; Fessler, R.G. Surgical site infection rates after minimally invasive spinal surgery: Clinical article. J. Neurosurg. Spine 2009, 11, 471–476. [Google Scholar] [CrossRef]
- Bonura, E.M.; Morales, D.J.O.; Fenga, D.; Rollo, G.; Meccariello, L.; Leonetti, D.; Traina, F.; Centofanti, F.; Rosa, M.A. Conservative Treatment of Spondylodiscitis: Possible Therapeutic Solution in Case of Failure of Standard Therapy. Med. Arch. 2019, 73, 39–43. [Google Scholar] [CrossRef]
- Timothy, J.; Pal, D.; Akhunbay-Fudge, C.; Knights, M.; Frost, A.; Derham, C.; Selvanathan, S. Extreme lateral interbody fusion (XLIF) as a treatment for acute spondylodiscitis: Leeds spinal unit experience. J. Clin. Neurosci. 2019, 59, 213–217. [Google Scholar] [CrossRef]
- Kabil, M.S. The microendoscopic approach for far lateral lumbar disc herniation: A preliminary series of 33 patients. Egypt. J. Neurosurg. 2019, 34, 22. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, Y.; Li, C.; Liu, J.; Xiang, L. Risk factors for failure of single-level percutaneous endoscopic lumbar discectomy. J. Neurosurg. Spine 2015, 23, 320–325. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).