Abstract
Background: Patellofemoral instability is a pathological condition that is characterized by altered joint congruence, which manifests as episodes of subluxation or dislocation of the patella. The aim of this study was to systematically review the literature on this condition by comparing the results of various studies evaluating the effectiveness of surgical versus conservative treatment approaches for patellar instability, particularly in patients experiencing a first episode of patellar dislocation. Methods: The research was conducted using three different databases: PubMed, Cochrane Library, and PEDro. Both randomized controlled trials (RCTs) and non-randomized studies of interventions (NRSIs) with full text availability were included. All articles were in English, and no temporal limits were imposed during the search. Results: In total, 10 articles met the inclusion criteria and were included in the systematic review. The standard for statistical significance was p < 0.05. The statistical analysis of re-dislocation rates indicated a statistically significant difference between the conservative and surgical groups (p = 0.023). The statistical analysis also showed that the mean Kujala score was significantly lower in the non-operative group (80.94) than the surgical group (89.83) (p = 0.017). These results indicate that surgical treatment is significantly more effective in reducing re-dislocation rates than conservative treatment and has better Kujala scores than conservative treatment. Conclusions: A reduction in the re-dislocation rate and improved scores on subjective tests related to pain and quality of life were observed with surgical treatment. Nevertheless, a higher level of evidence is needed to more clearly and accurately determine the most effective treatment approach.
1. Introduction
Patellofemoral instability is a pathological condition characterized by altered joint congruence between the patella and the femoral trochlea, which manifests as episodes of subluxation or dislocation of the patella. Dislocation may be associated with osteochondral and chondral fractures of the facets of the patella and femoral condyle or injuries to the ligaments of the medial compartment, particularly the medial patellofemoral ligament. This condition is especially frequent in young and active populations. It can lead to significant functional limitations and negatively impact quality of life [1,2]. The negative effects include recurrent pain; difficulty in walking, climbing stairs, or sports activities; and frequent episodes of knee dislocation [2].
Women are more frequently affected than men, which probably results from anatomical and biomechanical differences, such as a greater Q-angle (the line of traction of the quadriceps muscle), greater ligamentous laxity, and the muscle strength of the quadriceps femoris, which is generally lower for women [3]. Several risk factors are known for predisposal to joint instability. These include dysplasia of the patella alta, genu valgum, patella, and trochlea; generalized hyperlaxity; increased tibial external rotation and femoral anteversion; high Q angle; ligamentous laxity; and loss of integrity of the soft tissues that function as static and dynamic constraints [4].
Patellar luxation is a traumatic event that results in a complete loss of joint relationship between the patella and the femoral trochlea. It usually involves lateral dislocation, and almost all cases involve damage to the medial patellofemoral ligament, which provides an essential medial restraint against lateral patellar dislocation during the first 30° of flexion [4,5]. Clinically significant patellar instability presents with a subjective sensation of instability or locking and anterior knee pain. In true dislocation, there may be deformity, pain upon palpation, swelling, and loss of function of the knee joint.
Diagnosis can be carried out using clinical tests, such as the apprehension test [6]. This test is widely used and involves a clinical maneuver in which lateral pressure is applied to the patella while the knee is gently flexed, which elicits pain or apprehension if instability is present [2]. Instrumental examinations may also be employed, such as standard radiography (X-ray) and magnetic resonance imaging (MRI), which provide crucial information about bone structure and soft tissue integrity.
An important factor in evaluating patients with patellofemoral joint pain or instability is the lateral positioning of the tibial tubercle (TT). This is typically assessed by measuring the mediolateral distance between the anterior TT and the deepest point of the trochlear groove (TG), which is known as the TT-TG distance. According to computed tomography (CT) imaging, a TT-TG distance < 13 mm is generally considered normal, while a distance > 13 mm is regarded as abnormal. A TT-TG distance exceeding 20 mm is classified as pathological and is frequently recommended as an indication for surgical intervention in symptomatic patients, as outlined in various treatment protocols [7,8].
The treatment approach for patella luxation can be conservative or surgical. In conservative treatment, the initial approach involves reducing the luxation and pharmacological management of pain and inflammation. A typical aspect of this treatment option is immobilization. A light brace can be used to reduce pain during the first week [9]. The use of crutches and partial weight bearing are suggested for the first few weeks [10]. Further therapeutic action involves a rehabilitation program.
After the first patellar luxation, surgery could be required in cases of osteochondral fractures and mobile bodies, significant cartilage damage, rupture of the stabilizing structures with subluxation, or complete displacement of the patella. For the first episode of dislocation, the technique most frequently mentioned in recent studies is the reconstruction or repair of the medial patellofemoral ligament using a mini-open approach and a graft stronger than the native medial patellofemoral ligament (MPFL) [11,12]. According to recent studies, the success rate of MPFL reconstruction ranges from 80% to 95%, with most patients experiencing significant improvements in quality of life and knee function. However, the outcomes may vary based on factors, such as patient age, the presence of associated knee pathologies, and the timing of surgery [2,13]. Common complications associated with MPFL reconstruction include graft failure, recurrent patellar dislocations, patellar fracture, stiffness, and infection. On the other hand, conservative treatment is more commonly associated with recurrences, leading to subsequent re-dislocations of the patella [13].
The fundamental step following surgical treatment is rehabilitation. There is no precise explanation of specific exercises or exercise parameters in the literature. Despite this, overall, it is necessary to recover the range of motion (ROM) and strengthen the quadriceps femoris muscle [14]. When comparing conservative and surgical treatment, numerous rating scales are used to help determine which treatment works best on a study sample. One of the most commonly used is the Kujala score, which evaluates anterior knee pain through a questionnaire assessing symptoms, functional limitations, and alignment-related issues. Other scales include the Tegner activity score, mean Norwich patellar instability score, and Cincinnati Knee Rating System, which measure physical activity levels, quantify patellar instability severity, and evaluate treatment outcomes in knee disorders [15,16,17].
This systematic review was performed to assess the outcomes of conservative versus surgical treatments for patellofemoral instability. We compared the effectiveness of these approaches by analyzing rehabilitation protocols and evaluating scores from previous research. Our objective was to determine the optimal treatment strategy by synthesizing and interpreting data from scientific studies on the subject.
2. Materials and Methods
2.1. Search Strategy and Criteria
This systematic review was performed by two researchers (E.P. and M.I.) according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search was conducted on the PubMed, Cochrane, and PEDro databases. The search string “Conservative and Surgical Treatment in Patellofemoral Instability” was used for the searches, which were carried out from March to September 2024. Disagreements were resolved by a senior researcher. The risk of bias was constantly considered as it is greater given the nature of a mixed systematic review.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: only studies that directly compared conservative and surgical treatment approaches; randomized controlled trials (RCTs), non-randomized intervention studies (NRSIs); full-text articles; studies with twenty or more patients; studies written in English.
The exclusion criteria were as follows: duplicate studies, studies with no abstracts available, articles with poor scientific methodology, and studies with follow-up of less than 12 months; case reports; articles with fewer than twenty patients; articles written in languages other than English; non-human studies; absence of full text articles.
No limits were imposed on the year of publication as the patient age.
2.3. Data Extraction, Bias, and Outcomes
The following data were extracted from each article: the name of the first author, publication year, country, type of study, number of patients, age and sex of patients, type of treatment, and outcome. The risk of bias was assessed independently by two auditors (E.P. and M.I.), and disagreements were resolved by a senior auditor. The quality of evidence was analyzed with the GRADE (grading of recommendations, assessment, development, and evaluation) system [18] which is a framework for evaluating and formulating recommendations in healthcare. It involves a systematic assessment of study quality, considering factors such as risk of bias, consistency of results, precision, and relevance. Recommendations are classified as “strong” or “weak” based on the robustness of the available evidence. The assessment of the risk of bias was carried out for NRSIs according to the ROBINS-I tool (risk of bias in non-randomized studies of interventions) [19] and Cochrane Risk of Bias Tool (RoB 2.0) [20] for the RCTs. ROBINS-I assesses the risk of bias across 7 domains, which correspond to different phases of the study. Each domain includes a series of questions to be answered to determine the risk of bias.
Bias in any domain can distort findings, leading to overestimation or underestimation of intervention effects. For example, selection bias may arise from non-equivalent groups, while measurement bias can stem from inconsistent intervention documentation. These biases compromise the validity of conclusions and highlight the importance of meticulous, independent, and senior-level review to mitigate subjective interpretations and ensure robustness of the risk assessment process. The results were categorized using Endnote, and duplicates were excluded. The outcomes assessed were the recurrence of patellar dislocation and the score on the Kujala test [21].
3. Results
3.1. Eligible Studies
The search yielded 95 articles. After duplicates were eliminated, 73 articles remained. Of these, only 33 initially met the eligibility criteria and were checked one by one. Ultimately, 10 articles were included in the systematic review. A flow chart of the study-selection process is shown in Figure 1.
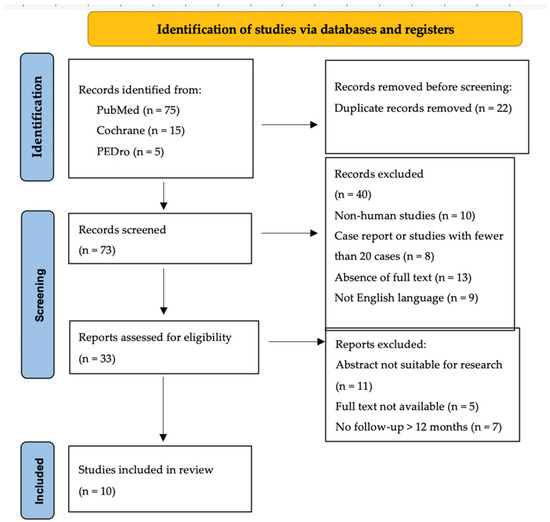
Figure 1.
PRISMA checklist.
3.2. Demographics, Outcomes, and Success Rates
We included 10 studies, which were all in English. The studies involved 546 participants and were published between 1997 and 2020. There were three studies conducted in Finland [22,23,24], two in Brazil [25,26], one in Germany [27], one in Denmark [28], one in Sweden [29], one in China [30], and one in Serbia [31]. The age at the beginning of treatment varied significantly between studies. The youngest participants were 8 years old [24], while the oldest were 74 years old [26].
Ji et al. did not report on age. Only three studies involved a purely pediatric population: those by Askenberger et al. [29] (age range 9–14 years), Regalado et al. [24] (8–16 years), and Apostolovic et al. [31] (12–16 years). In many of the studies, there was a prevalence of female participants, except for the one by Sillanpää et al. [22], in which there were only three female patients, as the study examined a military population.
Table 1 shows all the articles that met the inclusion criteria. All studies included were accurately read, and the values of the outcomes are shown in Table 2. In all 10 articles, the re-dislocation rate was observed as an outcome. All studies, except for those by Nikku et al. [23] and Apostolovic et al. [31], found a lower re-dislocation rate among patients with surgical treatment.

Table 1.
Summary of the main elements of the scientific articles considered for systematic review.

Table 2.
Study outcomes.
3.3. Success Rate
In all 10 articles, the re-dislocation rate was observed as an outcome. All studies, except for those by Nikku et al. [23] and Apostolovic et al. [31], found a lower re-dislocation rate in patients who had surgical treatment. We chose to conduct a statistical analysis based on the results obtained by comparing the re-dislocation rates and Kujala scores between those who had conservative treatment and those who had surgical treatment.
3.4. Re-Dislocation Rates
Starting with a comparison of re-dislocation rates, the conservative treatment group had an average rate of 33.14% (standard deviation (SD) 13.44%), whereas the surgical treatment group had an average rate of 17.16% (SD 15.19%). The result of the t-test was 2.49 with a p-value of 0.023. The p-value was less than the standard significance level (p = 0.05), indicating a statistically significant difference between the re-dislocation rates of the two groups. This demonstrates that surgical treatment is much more effective in reducing re-dislocation rates than conservative treatment. These findings are illustrated in Figure 2, whereas in Figure 3, there is a chart that displays the re-dislocation rates for both conservative and surgical treatments.
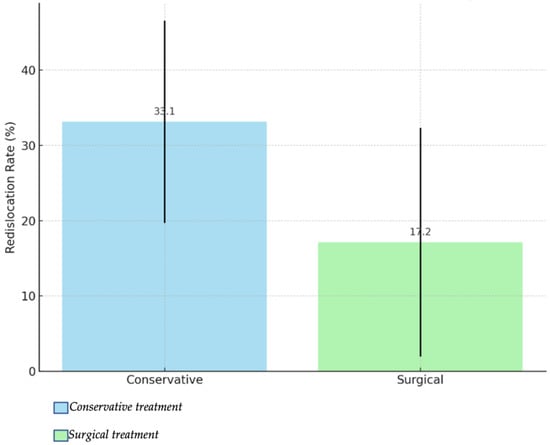
Figure 2.
Comparison of re-dislocation rates between conservative treatment and surgical treatment.
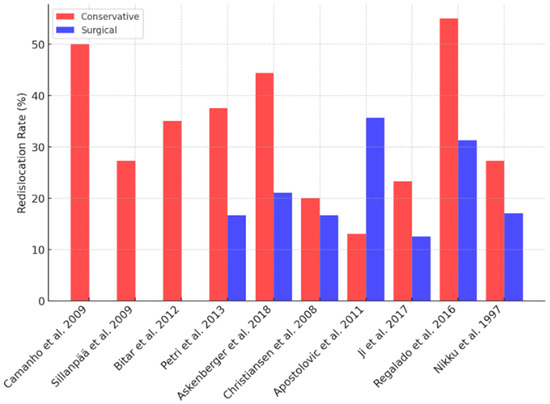
Figure 3.
Chart displaying the re-dislocation rates for both conservative (red) and surgical (blue) treatments.
3.5. Kujala Scores
The Kujala scores are found using a series of self-reported questions designed to measure pain, functional limitations, and the impact of symptoms on daily activities [21]. The score is derived from a total of 13 items, with higher scores indicating better functional outcomes and lower pain levels. The Kujala score has demonstrated reliability, validity, and sensitivity to change, making it an effective instrument for clinical assessment [21,32]. The conservative treatment group had a mean Kujala score of 80.7 (SD 9.66), while the surgical treatment group had a mean score of 89.8 (SD 2.92). The result of the t-test was −2.49 with a p-value of 0.034, indicating that the difference in Kujala scores between the two groups was statistically significant. Surgical surgery outperformed conservative treatment in terms of Kujala scores, which indicated improved knee function and quality of life. Figure 4 illustrates the clear difference between the average scores, with error bars representing the standard deviation of each group. In addition, Figure 5 illustrates a chart that presents the Kujala score of each study analyzed for both treatment approaches. Forest plots are showed in Figure 6 and Figure 7.
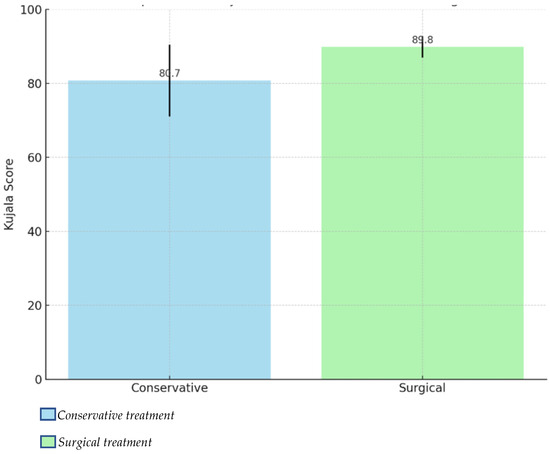
Figure 4.
Comparison of Kujala scores between conservative treatment and surgical treatment.
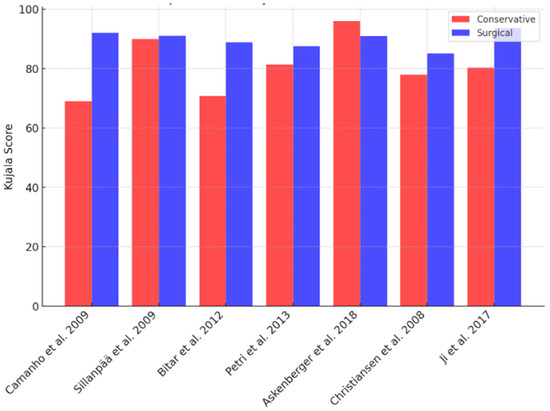
Figure 5.
The chart presents the Kujala scores of each study analyzed for both treatment approaches.
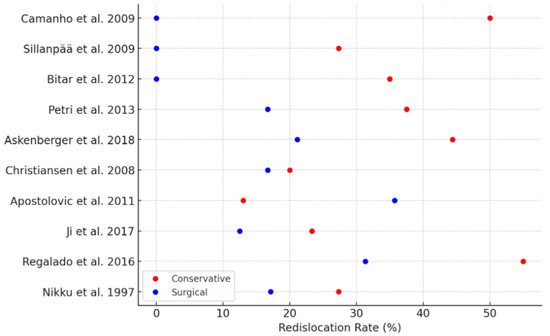
Figure 6.
Forest plot comparing re-dislocation rates for conservative and surgical treatments.
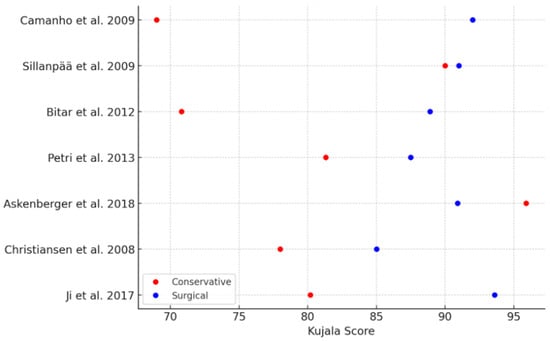
Figure 7.
Forest plot comparing Kujala scores for conservative and surgical treatment.
4. Discussion
Ten articles with a total of 543 patients were included in this review. Seven articles were randomized studies [22,24,25,26,27,28,29], and two performed randomization according to odd or even birth years [23,30]. One study was non-randomized [31]. All 10 studies only recruited participants who had a primary patellar dislocation [22,23,24,25,26,27,28,29,30,31] and were followed with periodic checks for at least 2 years. The findings on the re-dislocation rates and Kujala scores underscore the advantages of surgical treatment, particularly in reducing re-dislocation rates and enhancing functional outcomes. Surgical intervention consistently showed lower re-dislocation rates (17.16%) than conservative methods (33.14%).
Reconstruction or repair of the MPFL in surgical cases plays a pivotal role in restoring patellar stability and effectively addresses the anatomical deficiencies that are not directly targeted by conservative methods. This finding aligns with prior studies emphasizing the importance of stabilizing the patella to prevent recurrent dislocations, particularly in young and active individuals. Some case series also present encouraging results with MPFL reconstruction in the treatment of acute patellar dislocation. Using techniques that restore the anatomy and biomechanics of the MPFL is essential in surgery [33].
In addition to having a lower dislocation rate (p = 0.023), the Kujala scores were higher for surgical treatment (averaging 89.8 versus 80.7 for conservative management), which indicated better pain control and functional outcomes (p = 0.034). This significant difference underscores the functional advantages of surgical intervention in managing patellar instability, particularly in improving knee functionality and patient-reported quality of life. The higher score suggests that procedures such as MPFL reconstruction effectively address the anatomical and biomechanical causes of patellar instability [34]. By restoring proper alignment and joint stability, surgery not only helps to prevent recurrence, but also enhances knee function and reduces discomfort during daily activities and physical exertion.
While conservative management achieved moderate Kujala scores, its reliance on physiotherapy and bracing appears insufficient for addressing severe instability or structural anomalies such as trochlear dysplasia or patella alta. These limitations likely explain the poorer functional outcomes and highlight the need for surgical intervention in complex cases. These results reflect those of Bitar et al., whose statistical analysis actually showed even better results in the surgical group [25]. Surgical interventions not only address the mechanical stability of the knee but also improve patient-reported outcomes related to mobility and quality of life, and they are recommended for cases where immediate and sustained functional improvement is critical. Nonetheless, the conservative group still achieved moderate Kujala scores, reflecting potential efficacy in cases of mild instability or contraindications to surgery, although the same functional benefits may not be achieved [25].
This was confirmed by Johnson et al., who outlined the management for first-time lateral patellar dislocation and emphasized using conservative treatment as the initial approach. Key components include brief immobilization, physiotherapy focusing on quadriceps strengthening, and gait re-education. Surgery was reserved for recurrent or complex cases and often involved MPFL reconstruction [35,36]. Non-surgical management in all studies generally consisted of initial immobilization in a cast, splint, or locked orthosis, followed by active mobilization with physiotherapy. The aim of this approach is to restore stability, ROM, and strength, while minimizing the risk of re-injury.
In each study, physiotherapy consisted of exercises to strengthen the muscles of the lower limbs, with a focus on the quadriceps femoris. Early exercises include quadriceps sets, straight-leg raises, and ankle pumps. Progression involves ROM activities and strengthening exercises such as wall squats, step-ups, lunges, and resistance-band drills. Proprioceptive training with tools like wobble boards and dynamic movements like lateral hops are added later. Advanced phases involve preparation for sports with plyometric drills and sport-specific agility exercises [37]. However, none of the articles provided detailed descriptions of the exercises performed.
The predominant surgical intervention was the repair and reconstruction of soft tissue, particularly the medial compartment of the knee joint. Four studies reported that all participants in their surgical groups underwent MPFL repair exclusively [26,28,29,30]. An arthroscopic procedure was used in two studies [26,29], and an open procedure was used in two other studies [29,30]. In biomechanical studies, some authors concluded that the MPFL accounts for approximately 50 to 70% of total lateral restriction, making it the primary medial stabilizer of the patella [38].
Some reviews [33] consider nonoperative treatment as the first option, but some studies associate this treatment with eventual recurrences. Maenpa and Lehto monitored 100 patients treated non-operatively after patellar dislocation for 13 years on average. Of these patients, 44% had recurrence, and another 19% experienced subluxation and patellofemoral pain. All participants that received surgical management had a period of postoperative rehabilitation. Apart from two studies [22,25], the postoperative rehabilitation program used in each study was identical to that used in the conservative group. The longest follow-up was in the study by Sillanpää et al., which had a mean duration of 7 years.
Our study has some limitations. The follow-up duration in the studies analyzed significantly impacts the validity of their results. Short follow-up periods, such as 24 months, may fail to capture long-term outcomes like re-dislocation rates or functional recovery. In contrast, longer follow-ups, such as 7 years in some studies, provide a more comprehensive evaluation of the treatment’s sustainability and risks of late complications. The variability in re-dislocation rates among studies could be attributed to differences in follow-up durations, patient demographics, and the severity of patellar instability at baseline, which must be considered in our results.
Furthermore, there is no evidence of the rehabilitation treatment being adopted. This lack of specificity and in-depth descriptions significantly limits the possibility of extrapolating information about rehabilitation guidelines to follow. Additionally, sample representativeness is a concern. Many studies predominantly included younger or female participants, which limits generalizability to other populations, such as older adults or males.
The statistical results of the Kujala score should be interpreted with caution due to a critical limitation in the dataset. Our analysis was based on data extracted from only 7 of the 10 articles included. This partial representation may introduce bias and reduce the robustness of our conclusions. Furthermore, the excluded studies might contain additional insights or data that could either support or contradict our results.
Significant variability exists in the study designs, which limits any definitive conclusions. Further analysis revealed disparities based on age and severity. Younger patients or those with more severe instability benefited more from surgery, while mild cases responded well to conservative care. Sex differences were negligible in the outcomes, but sample representation varied. These limitations highlight the need for further comprehensive investigations to validate the findings and assess the true efficacy of surgical treatment relative to conservative approaches.
The studies included in this systematic review present varying levels of evidence based on the GRADE (grading of recommendations, assessment, development, and evaluation) framework; in addition, the risk of bias was evaluated using the ROBINS-I (risk of bias in non-randomized studies of interventions) tool for the NRSI and the Cochrane Risk of Bias Tool (RoB 2.0) for the RCTs. Overall, the evidence from this systematic review, as well as the quality of evidence, is predominantly moderate to high, with well-conducted RCTs forming most of the included studies and supporting the conclusions of this review. The results indicate that surgical treatment is superior to conservative treatment in reducing re-dislocation rates and improving Kujala scores. However, limitations such as attrition bias, blinding inconsistencies, and selection bias in non-randomized studies should be considered when interpreting the results.
Future research should focus on long-term follow-up studies to assess treatment sustainability and late complications. Standardized rehabilitation protocols should be evaluated to determine their impact on outcomes. Larger, more diverse samples are needed to improve generalizability. Further analysis should address the influence of age and severity on treatment efficacy. Additionally, comprehensive datasets are required to enhance the robustness of statistical analyses and minimize potential biases.
5. Conclusions
Surgical treatment led to better results than conservative treatment in reducing re-dislocation rates and enhancing functional outcomes in patellar instability according to the significant differences in Kujala scores. However, the optimal treatment protocol remains unclear due to study limitations. Further research should refine rehabilitation strategies, improve postoperative care, and minimize recovery time through large, multicenter studies addressing variability and biases.
Author Contributions
Conceptualization, M.S.; methodology, M.I.; software, E.P.; validation, G.S.P.; formal analysis, A.C.; investigation, M.I.; resources, E.P.; data curation, M.S.; writing—original draft preparation, G.T.; writing—review and editing, G.T.; visualization, V.P.; supervision, V.P.; project administration, V.P.; funding acquisition, V.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are included in the text.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kasitinon, D.; Li, W.-X.; Wang, E.X.S.; Fredericson, M. Physical Examination and Patellofemoral Pain Syndrome: An Updated Review. Curr. Rev. Musculoskelet. Med. 2021, 14, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and Natural History of Acute Patellar Dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Csintalan, R.P.; Schulz, M.M.; Woo, J.; McMahon, P.J.; Lee, T.Q. Gender Differences in Patellofemoral Joint Biomechanics. Clin. Orthop. Relat. Res. 2002, 402, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Maffulli, N.; Vaishya, R. Patellofemoral Instability: Current Status and Future Perspectives. J. Orthop. 2022, 36, 49–50. [Google Scholar] [CrossRef]
- Hayat, Z.; El Bitar, Y.; Case, J.L. Patella Dislocation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Smith, T.O.; Davies, L.; O’Driscoll, M.-L.; Donell, S.T. An Evaluation of the Clinical Tests and Outcome Measures Used to Assess Patellar Instability. Knee 2008, 15, 255–262. [Google Scholar] [CrossRef]
- Anley, C.M.; Morris, G.V.; Saithna, A.; James, S.L.; Snow, M. Defining the Role of the Tibial Tubercle-Trochlear Groove and Tibial Tubercle-Posterior Cruciate Ligament Distances in the Work-up of Patients With Patellofemoral Disorders. Am. J. Sports Med. 2015, 43, 1348–1353. [Google Scholar] [CrossRef]
- Frings, J.; Balcarek, P.; Tscholl, P.; Liebensteiner, M.; Dirisamer, F.; Koenen, P. Conservative Versus Surgical Treatment for Primary Patellar Dislocation. Dtsch. Arztebl. Int. 2020, 117, 279–286. [Google Scholar] [CrossRef]
- Dejour, D.H.; Mesnard, G.; Giovannetti de Sanctis, E. Updated Treatment Guidelines for Patellar Instability: “Un Menu à La Carte”. J. Exp. Orthop. 2021, 8, 109. [Google Scholar] [CrossRef]
- Flores, G.W.; de Oliveira, D.F.; Ramos, A.P.S.; Sanada, L.S.; Migliorini, F.; Maffulli, N.; Okubo, R. Conservative Management Following Patellar Dislocation: A Level I Systematic Review. J. Orthop. Surg. Res. 2023, 18, 393. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V. Guidelines for Medial Patellofemoral Ligament Reconstruction in Chronic Lateral Patellar Instability. JAAOS-J. Am. Acad. Orthop. Surg. 2014, 22, 175. [Google Scholar] [CrossRef]
- Migliorini, F.; Oliva, F.; Maffulli, G.D.; Eschweiler, J.; Knobe, M.; Tingart, M.; Maffulli, N. Isolated Medial Patellofemoral Ligament Reconstruction for Recurrent Patellofemoral Instability: Analysis of Outcomes and Risk Factors. J. Orthop. Surg. Res. 2021, 16, 239. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.N.; Howard, J.S.; Flanigan, D.C.; Brophy, R.H.; Carey, J.L.; Lattermann, C. A Systematic Review of Complications and Failures Associated with Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation. Am. J. Sports Med. 2012, 40, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Lieber, A.C.; Steinhaus, M.E.; Liu, J.N.; Hurwit, D.; Chiaia, T.; Strickland, S.M. Quality and Variability of Online Available Physical Therapy Protocols From Academic Orthopaedic Surgery Programs for Medial Patellofemoral Ligament Reconstruction. Orthop. J. Sports Med. 2019, 7, 2325967119855991. [Google Scholar] [CrossRef] [PubMed]
- Barber-Westin, S.D.; Noyes, F.R.; McCloskey, J.W. Rigorous Statistical Reliability, Validity, and Responsiveness Testing of the Cincinnati Knee Rating System in 350 Subjects with Uninjured, Injured, or Anterior Cruciate Ligament-Reconstructed Knees. Am. J. Sports Med. 1999, 27, 402–416. [Google Scholar] [CrossRef] [PubMed]
- Briggs, K.K.; Lysholm, J.; Tegner, Y.; Rodkey, W.G.; Kocher, M.S.; Steadman, J.R. The Reliability, Validity, and Responsiveness of the Lysholm Score and Tegner Activity Scale for Anterior Cruciate Ligament Injuries of the Knee: 25 Years Later. Am. J. Sports Med. 2009, 37, 890–897. [Google Scholar] [CrossRef]
- Smith, T.O.; Choudhury, A.; Navratil, R.; Hing, C.B. Psychometric Properties of the Norwich Patellar Instability Score in People with Recurrent Patellar Dislocation. Knee 2019, 26, 1192–1197. [Google Scholar] [CrossRef]
- Xie, C.X.; Machado, G.C. Clinimetrics: Grading of Recommendations, Assessment, Development and Evaluation (GRADE). J. Physiother. 2021, 67, 66. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Kujala, U.M.; Jaakkola, L.H.; Koskinen, S.K.; Taimela, S.; Hurme, M.; Nelimarkka, O. Scoring of Patellofemoral Disorders. Arthroscopy 1993, 9, 159–163. [Google Scholar] [CrossRef]
- Sillanpää, P.J.; Mattila, V.M.; Mäenpää, H.; Kiuru, M.; Visuri, T.; Pihlajamäki, H. Treatment with and without Initial Stabilizing Surgery for Primary Traumatic Patellar Dislocation. A Prospective Randomized Study. J. Bone Joint Surg. Am. 2009, 91, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Nikku, R.; Nietosvaara, Y.; Kallio, P.E.; Aalto, K.; Michelsson, J.E. Operative versus Closed Treatment of Primary Dislocation of the Patella. Similar 2-Year Results in 125 Randomized Patients. Acta Orthop. Scand. 1997, 68, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Regalado, G.; Lintula, H.; Kokki, H.; Kröger, H.; Väätäinen, U.; Eskelinen, M. Six-Year Outcome after Non-Surgical versus Surgical Treatment of Acute Primary Patellar Dislocation in Adolescents: A Prospective Randomized Trial. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 6–11. [Google Scholar] [CrossRef]
- Bitar, A.C.; Demange, M.K.; D’Elia, C.O.; Camanho, G.L. Traumatic Patellar Dislocation: Nonoperative Treatment Compared with MPFL Reconstruction Using Patellar Tendon. Am. J. Sports Med. 2012, 40, 114–122. [Google Scholar] [CrossRef]
- Camanho, G.L.; de Christo Viegas, A.; Bitar, A.C.; Demange, M.K.; Hernandez, A.J. Conservative versus Surgical Treatment for Repair of the Medial Patellofemoral Ligament in Acute Dislocations of the Patella. Arthroscopy 2009, 25, 620–625. [Google Scholar] [CrossRef]
- Petri, M.; Liodakis, E.; Hofmeister, M.; Despang, F.J.; Maier, M.; Balcarek, P.; Voigt, C.; Haasper, C.; Zeichen, J.; Stengel, D.; et al. Operative vs Conservative Treatment of Traumatic Patellar Dislocation: Results of a Prospective Randomized Controlled Clinical Trial. Arch. Orthop. Trauma. Surg. 2013, 133, 209–213. [Google Scholar] [CrossRef]
- Christiansen, S.E.; Jakobsen, B.W.; Lund, B.; Lind, M. Isolated Repair of the Medial Patellofemoral Ligament in Primary Dislocation of the Patella: A Prospective Randomized Study. Arthroscopy 2008, 24, 881–887. [Google Scholar] [CrossRef]
- Askenberger, M.; Bengtsson Moström, E.; Ekström, W.; Arendt, E.A.; Hellsten, A.; Mikkelsen, C.; Janarv, P.-M. Operative Repair of Medial Patellofemoral Ligament Injury Versus Knee Brace in Children With an Acute First-Time Traumatic Patellar Dislocation: A Randomized Controlled Trial. Am. J. Sports Med. 2018, 46, 2328–2340. [Google Scholar] [CrossRef]
- Ji, G.; Wang, S.; Wang, X.; Liu, J.; Niu, J.; Wang, F. Surgical versus Nonsurgical Treatments of Acute Primary Patellar Dislocation with Special Emphasis on the MPFL Injury Patterns. J. Knee Surg. 2017, 30, 378–384. [Google Scholar] [CrossRef]
- Apostolovic, M.; Vukomanovic, B.; Slavkovic, N.; Vuckovic, V.; Vukcevic, M.; Djuricic, G.; Kocev, N. Acute Patellar Dislocation in Adolescents: Operative versus Nonoperative Treatment. Int. Orthop. 2011, 35, 1483–1487. [Google Scholar] [CrossRef]
- Cerciello, S.; Corona, K.; Morris, B.J.; Visonà, E.; Maccauro, G.; Maffulli, N.; Ronga, M. Cross-Cultural Adaptation and Validation of the Italian Versions of the Kujala, Larsen, Lysholm and Fulkerson Scores in Patients with Patellofemoral Disorders. J. Orthop. Traumatol. 2018, 19, 18. [Google Scholar] [CrossRef]
- Dopirak, R.M.; Steensen, R.N.; Maurus, P.B. The Medial Patellofemoral Ligament. Orthopedics 2008, 31, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Hinckel, B.; Smith, J.; Tanaka, M.J.; Matsushita, T.; Martinez-Cano, J.P. Patellofemoral Instability Part 1 (When to Operate and Soft Tissue Procedures): State of the Art. J. ISAKOS 2024, 10, 100278. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.S.; Turner, P.G. Management of the First-Time Lateral Patellar Dislocation. Knee 2019, 26, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Arendt, E.A.; Donell, S.T.; Sillanpää, P.J.; Feller, J.A. The Management of Lateral Patellar Dislocation: State of the Art. J. ISAKOS 2017, 2, 205–212. [Google Scholar] [CrossRef]
- Amis, A.A.; Firer, P.; Mountney, J.; Senavongse, W.; Thomas, N.P. Anatomy and Biomechanics of the Medial Patellofemoral Ligament. Knee 2003, 10, 215–220. [Google Scholar] [CrossRef]
- Mäenpää, H.; Lehto, M.U. Patellar Dislocation. The Long-Term Results of Nonoperative Management in 100 Patients. Am. J. Sports Med. 1997, 25, 213–217. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).