Abrasiveness and Bleaching Level of Toothpastes on Composite Resins: A Quantitative Analysis Using a Novel Brushing Simulator
Abstract
1. Introduction
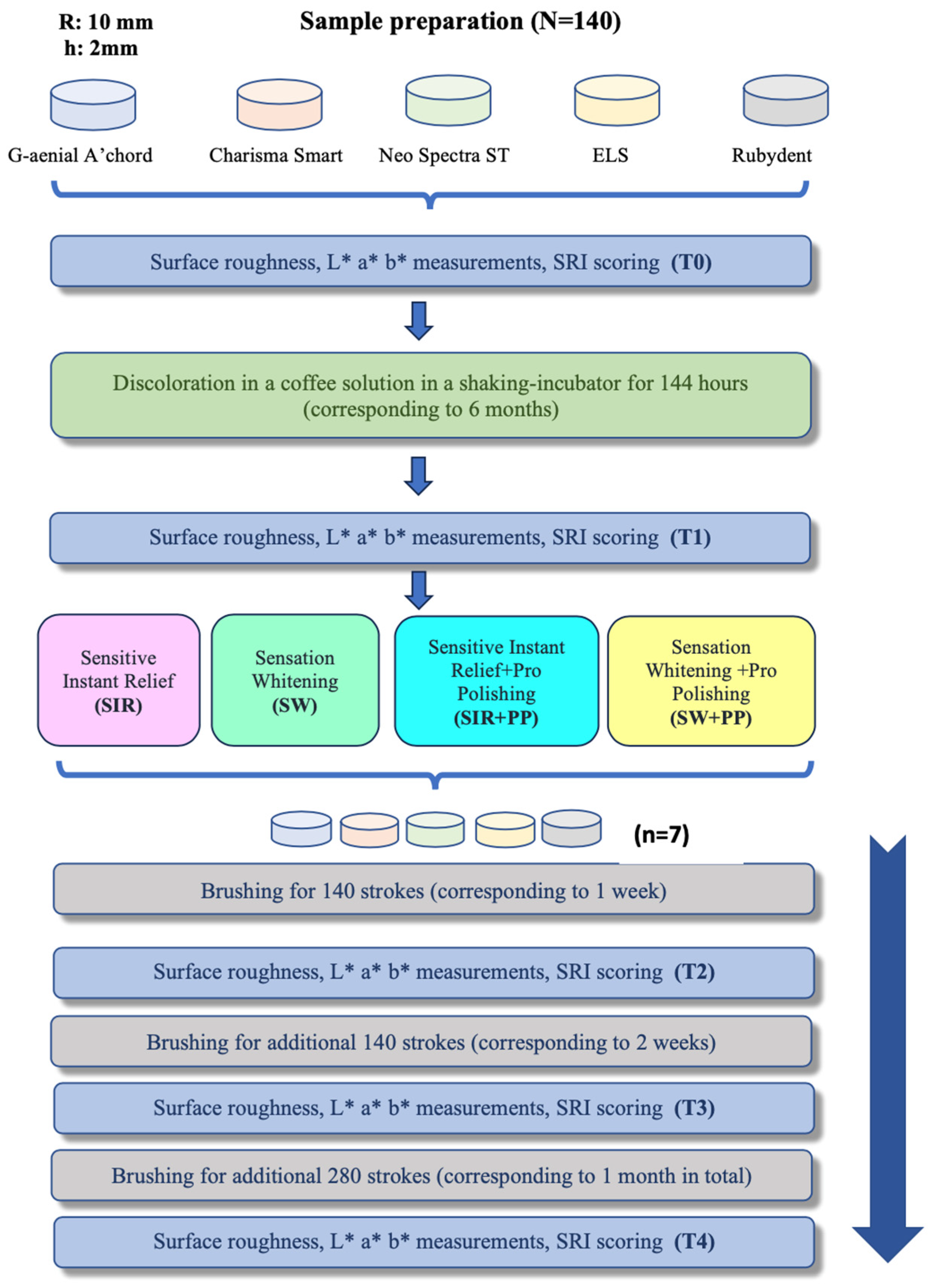
2. Materials and Methods
2.1. Preparation and Distribution of Samples
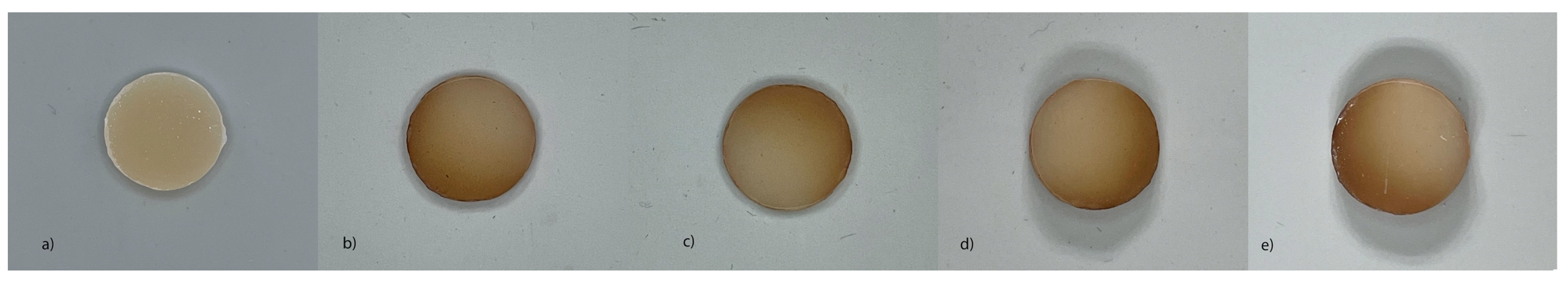
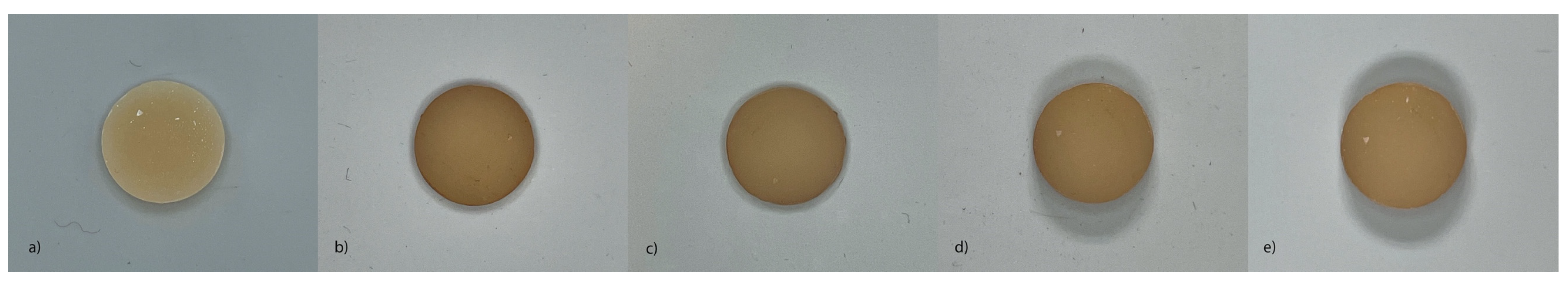
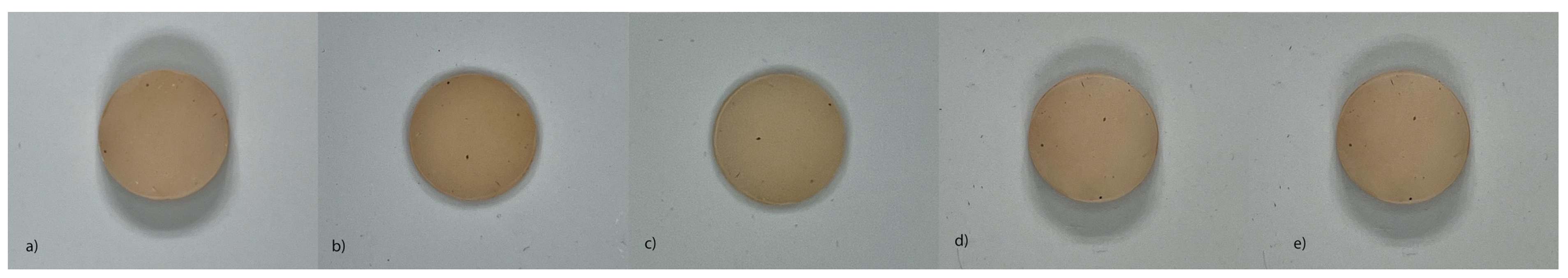
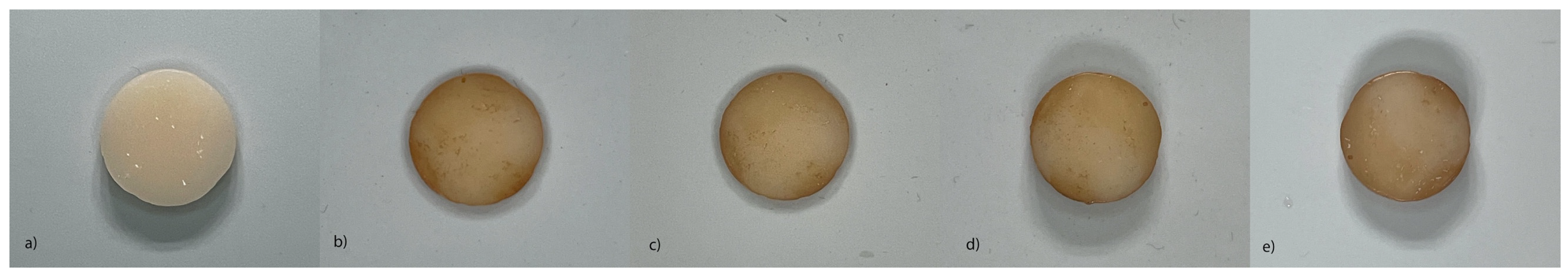
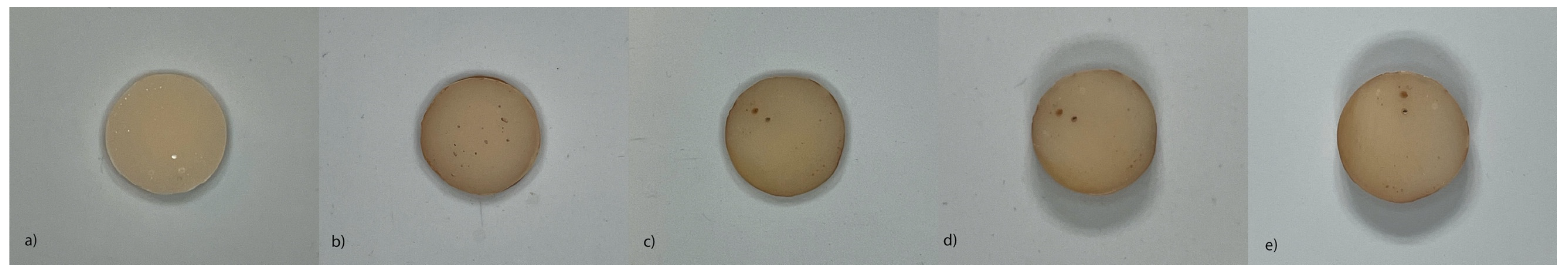
2.2. Discoloration Protocol and ΔE* Assessment
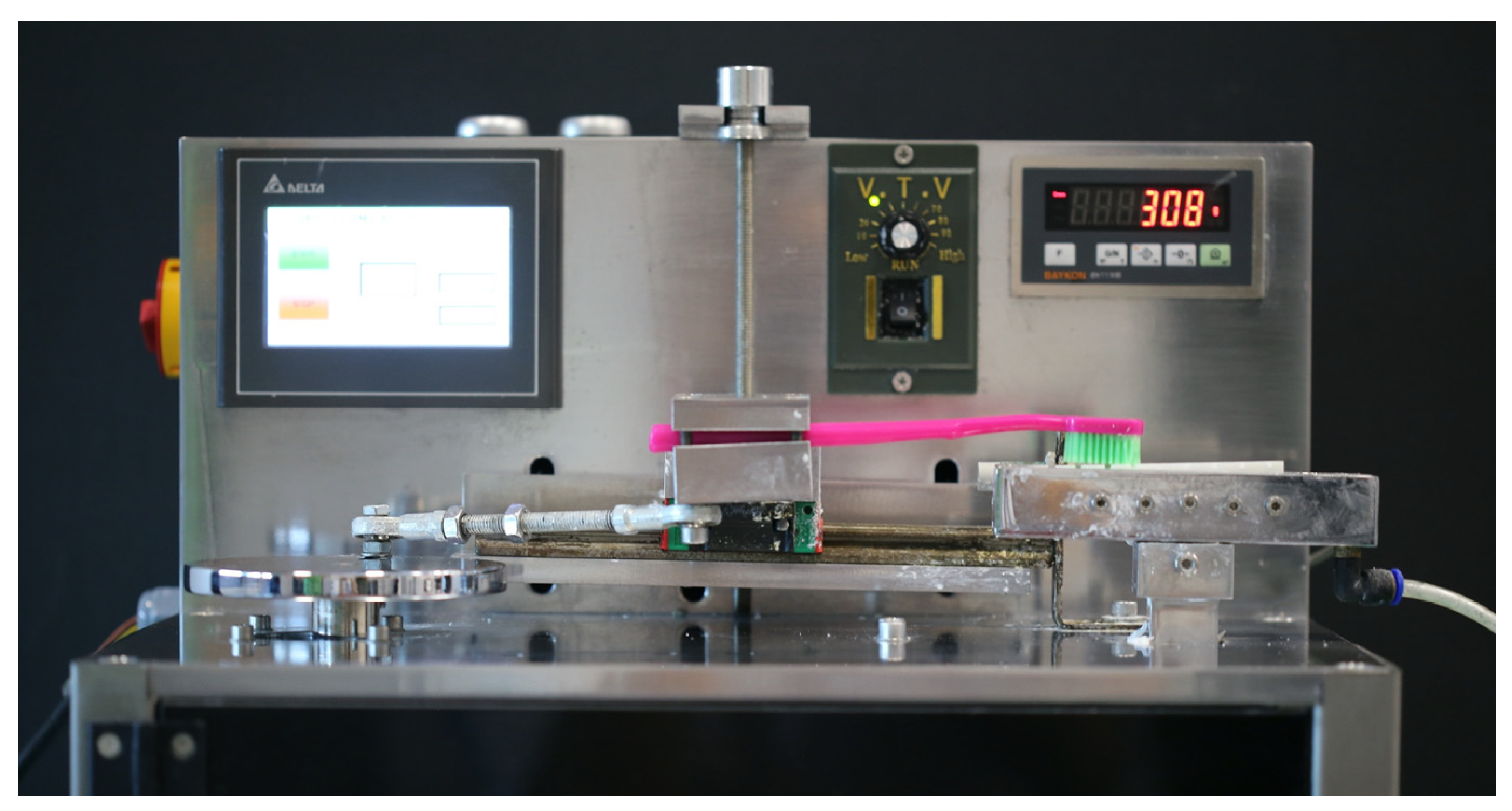
2.3. Brushing Protocol
2.4. Surface Roughness Assessment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- de Abreu, J.L.B.; Sampaio, C.S.; Benalcázar Jalkh, E.B.; Hirata, R. Analysis of the color matching of universal resin composites in anterior restorations. J. Esthet. Restor. Dent. 2021, 33, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.F.; Feng, L.; Serban, D.; Malmstrom, H.S. Effects of common beverage colorants on color stability on dental composite resins: The utility of a thermocycling stain challenge model in vitro. J. Dent. 2012, 40, e48–e56. [Google Scholar] [CrossRef]
- Jesus, L.S.d.; Reis, T.L.d.S.; Machado, B.G.M.d.M.; Costa, A.L.M.d.; Savaris, J.M.; Volpato, C.A.M.; Bortoluzzi, E.A.; Teixeira, C.D.S.; Fernandes, P.C.D.S.V.; Garcia, L.D.F.R. Dental and composite resin discoloration induced by different hydraulic calcium silicate-based cements: Two-year in vitro assessment. J. Appl. Oral Sci. 2023, 31, e20220444. [Google Scholar] [CrossRef]
- Uctasli, M.; Garoushi, S.; Uctasli, M.; Vallittu, P.; Lassila, L. A comparative assessment of color stability among various commercial resin composites. BMC Oral Health 2023, 23, 789. [Google Scholar] [CrossRef] [PubMed]
- Pisano, M.; Iandolo, A.; Abdellatif, D.; Chiacchio, A.; Galdi, M.; Martina, S. Effects of different curing methods on the color stability of composite resins. Restor. Dent. Endod. 2024, 49, e33. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.S.; Ajay, R.; Sahib, S.M.; Chittrarasu, M.; Navarasu, M.; Ragavendran, N.; Mohammed, O.F. Color stability assessment of two different composite resins with variable immersion time using various beverages: An in vitro study. J. Pharm. Bioallied Sci. 2017, 9 (Suppl. S1), S161. [Google Scholar]
- Esmaeili, B.; Afkhami, S.; Abolghasemzadeh, F. The effect of time between curing and tea immersion on composite resin discoloration. General. Dent. 2018, 66, 64–68. [Google Scholar]
- Chu, S.J. Fundamentals of Color: Shade Matching and Communication in Esthetic Dentistry; Quintessence Publishing Company: Batavia, IL, USA, 2004. [Google Scholar]
- Kim-Pusateri, S.; Brewer, J.D.; Dunford, R.G.; Wee, A.G. In vitro model to evaluate reliability and accuracy of a dental shade-matching instrument. J. Prosthet. Dent. 2007, 98, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Turgut, S.; Kılınç, H.; Eyüpoglu, G.B.; Bağış, B. Color relationships of natural anterior teeth: An In vivo study. Niger. J. Clin. Pract. 2018, 21, 925–931. [Google Scholar]
- Türkün, L.Ş.; Türkün, M. Effect of bleaching and repolishing procedures on coffee and tea stain removal from three anterior composite veneering materials. J. Esthet. Restor. Dent. 2004, 16, 290–301. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Ardu, S.; Bortolotto, T.; Krejci, I. In-office bleaching efficacy on stain removal from CAD/CAM and direct resin composite materials. J. Esthet. Restor. Dent. 2018, 30, 51–58. [Google Scholar] [CrossRef]
- de Moraes Rego Roselino, L.; Tonani Torrieri, R.; Sbardelotto, C.; Alves Amorim, A.; Noronha Ferraz de Arruda, C.; Tirapelli, C.; de Carvalho Panzeri Pires-de-Souza, F. Color stability and surface roughness of composite resins submitted to brushing with bleaching toothpastes: An in situ study. J. Esthet. Restor. Dent. 2019, 31, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Koc Vural, U.; Bagdatli, Z.; Yilmaz, A.E.; Yalçın Çakır, F.; Altundaşar, E.; Gurgan, S. Effects of charcoal-based whitening toothpastes on human enamel in terms of color, surface roughness, and microhardness: An in vitro study. Clin. Oral Investig. 2021, 25, 5977–5985. [Google Scholar] [CrossRef] [PubMed]
- Van Loveren, C.; Duckwort, R.M. Anti-calculus and whitening toothpastes. Monogr. Oral Sci. 2013, 23, 61–74. [Google Scholar] [PubMed]
- Vertuan, M.; de Souza, B.M.; Machado, P.F.; Mosquim, V.; Magalhães, A.C. The effect of commercial whitening toothpastes on erosive dentin wear in vitro. Arch. Oral Biol. 2020, 109, 104580. [Google Scholar] [CrossRef] [PubMed]
- Barutcigil, Ç.; Yıldız, M. Intrinsic and extrinsic discoloration of dimethacrylate and silorane based composites. J. Dent. 2012, 40, e57–e63. [Google Scholar] [CrossRef] [PubMed]
- Korkut, B.; Hacıali, C. Color stability of flowable composites in different viscosities. Clin. Exp. Health Sci. 2020, 10, 454–461. [Google Scholar] [CrossRef]
- Ertas, E.; Gueler, A.U.; Yuecel, A.C.; Koepruelue, H.; Gueler, E. Color stability of resin composites after immersion in different drinks. Dent. Mater. J. 2006, 25, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Addy, M.; Hughes, J.; Pickles, M.; Joiner, A.; Huntington, E. Development of a method in situ to study toothpaste abrasion of dentine: Comparison of 2 products. J. Clin. Periodontol. 2002, 29, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Celik, N.; Iscan Yapar, M. Colour stability of stained composite resins after brushing with whitening toothpaste. Int. J. Dent. Hyg. 2021, 19, 413–420. [Google Scholar] [CrossRef]
- Wang, Z.; Jiang, T.; Sauro, S.; Pashley, D.H.; Toledano, M.; Osorio, R.; Liang, S.; Xing, W.; Sa, Y.; Wang, Y. The dentine remineralization activity of a desensitizing bioactive glass-containing toothpaste: An in vitro study. Aust. Dent. J. 2011, 56, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Malik, R.; Kalha Osre, A.S.; Chandna, A.K.; Puri, A.; Chawla, R. Effects of debonding a conventional & custimized lingual appliance on enamel structure- an invitro study. Orthod. J. Nepal. 2020, 3, 14–20. [Google Scholar]
- Turssi, C.P.; Messias, D.C.F.; Taeko Hara, A.; Hughes, N.; Garcia-Godoy, F. Brushing abrasion of dentine: Effect of diluent and dilution rate of toothpaste. Am. J. Dent. 2010, 23, 247–250. [Google Scholar] [PubMed]
- Harte, D.B.; Manly, R.S. Four variables affecting magnitude of dentrifice abrasiveness. J. Dent. Res. 1976, 55, 322–327. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.M.; Dantas, D.C.B.; Franco, T.T.; Franco, L.T.; Huhtala, M.F.R.L. Surface degradation of composite resins under staining and brushing challenges. J. Dent. Sci. 2019, 14, 87–92. [Google Scholar] [CrossRef]
- EL-Sharkawy, F.M.; Zaghloul, N.M.; Ell-kappaney, A.M. Effect of water absorption on color stability of different resin based restorative materials in vitro study. Int. J. Compos. Mater. 2012, 2, 7–10. [Google Scholar] [CrossRef][Green Version]
- Mehrgan, S.; Kermanshah, H.; Omrani, L.R.; Ahmadi, E.; Rafeie, N. Comparison the effect of charcoal-containing, hydrogen peroxide-containing, and abrasive whitening toothpastes on color stability of a resin composite; an in vitro study. BMC Oral Health 2021, 21, 594. [Google Scholar] [CrossRef]
- Rohym, S.; Tawfeek, H.E.M.; Kamh, R. Effect of coffee on color stability and surface roughness of newly introduced single shade resin composite materials. BMC Oral Health 2023, 23, 236. [Google Scholar] [CrossRef] [PubMed]
- Abd ElAziz, R.H.; Gadallah, L.K.; Saleh, R.S. Evaluation of Charcoal and Sea Salt-Lemon-based Whitening Toothpastes on Color Change and Surface Roughness of Stained Teeth. J. Contemp. Dent. Pract. 2022, 23, 169–175. [Google Scholar] [CrossRef]
- Demir, F.; Oktay, E.A.; Karaoğlanoğlu, S.; Topçu, F.T.; Bilgeç, E.; Aydın, N. Examining the effect of in vitro toothbrushing and the effect of different whitening toothpaste usages on the color change of a nanofilled composite. Gulhane Med. J. 2021, 63, 30–34. [Google Scholar] [CrossRef]
- Yilmaz, M.N.; Gul, P.; Unal, M.; Turgut, G. Effects of whitening toothpastes on the esthetic properties and surface roughness of a composite resin. J. Oral Sci. 2021, 63, 320–325. [Google Scholar] [CrossRef]
- Manis, R.B.; Da Silva, T.M.; Franco, T.T.; Dantas, D.C.B.; Franco, L.T.; Huhtala, M.F.R.L. Influence of whitening toothpaste on color, roughness, and microhardness of composite resins. Eur. J. Gen. Dent. 2017, 6, 92–98. [Google Scholar]
- Lobene, R.R. Effect of dentifrices on tooth stains with controlled brushing. J. Am. Dent. Assoc. 1968, 77, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Lippert, F. An introduction to toothpaste-its purpose, history and ingredients. In Toothpastes; Karger Publishers: Basel, Switzerland, 2013; Volume 23, pp. 1–14. [Google Scholar]
- Ucuncu, M.K.; Guven, K.; Yazicioglu, O. Investigation of the constituents of commercially available toothpastes. Int. J. Dent. Hyg. 2024, 22, 913–932. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Forjanic, M. Surface roughness of different dental materials before and after simulated toothbrushing in vitro. Oper. Dent.-Univ. Wash. 2005, 30, 617. [Google Scholar]
- Mozzaquatro, L.R.; Rodrigues, C.S.; Kaizer, M.R.; Lago, M.; Mallmann, A.; Jacques, L.B. The effect of brushing and aging on the staining and smoothness of resin composites. J. Esthet. Restor. Dent. 2017, 29, E44–E55. [Google Scholar] [CrossRef]
- Meshki, R.; Rashidi, M. Effect of natural and commercially produced juices on colour stability of microhybrid and nanohybrid composites. BDJ Open 2022, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Nasim, I.; Neelakantan, P.; Sujeer, R.; Subbarao, C.V. Color stability of microfilled, microhybrid and nanocomposite resins-an in vitro study. J. Dent. 2010, 38 (Suppl. S2), 137–142. [Google Scholar] [CrossRef] [PubMed]
- Gurgan, S.; Koc Vural, U.; Miletic, I. Comparison of mechanical and optical propertiesof a newly marketed universal composite resin with contemporary universal composite resins: An in vitro study. Microsc. Res. Tech. 2022, 85, 1171–1179. [Google Scholar] [CrossRef]
- Scholl, J.A.; Koh, A.L.; Dionne, J.A. Quantum plasmon resonances of individual metallic nanoparticles. Nature 2012, 483, 421–427. [Google Scholar] [CrossRef]
- Colak, G.; Katirci, G. In Vitro evaluation of the effects of whitening toothpastes on the color and surface roughness of different composite resin materials. BMC Oral Health 2023, 23, 580. [Google Scholar] [CrossRef] [PubMed]
- Ardu, S.; Duc, O.; Di Bella, E.; Krejci, I.; Daher, R. Color stability of different composite resins after polishing. Odontology 2018, 106, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, G.U.d.; Mondelli, R.F.L.; Charantola Rodrigues, M.; Franco, E.B.; Ishikiriama, S.K.; Wang, L. Impact of filler size and distribution on roughness and wear of composite resin after simulated toothbrushing. J. Appl. Oral Sci. 2012, 20, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Ganss, C.; Marten, J.; Hara, A.; Schlueter, N. Toothpastes and enamel erosion/abrasion–Impact of active ingredients and the particulate fraction. J. Dent. 2016, 54, 62–67. [Google Scholar] [CrossRef]
- Pires-de, F.d.C.P.; Garcia, L.d.F.R.; Roselino, L.d.M.R.; Naves, L.Z. Color stability of silorane-based composites submitted to accelerated artificial ageing—An in situ study. J. Dent. 2011, 39, e18–e24. [Google Scholar]
- Yılmaz, C.; Kanık, Ö. Investigation of surface roughness values of various restorative materials after brushing with blue covarine containing whitening toothpaste by two different methods: AFM and profilometer. Microsc. Res. Tech. 2022, 85, 521–532. [Google Scholar] [CrossRef]
- Roselino, L.d.M.R.; Cruvinel, D.R.; Chinelatti, M.A.; Pires-de, F.d.C.P. Effect of brushing and accelerated ageing on color stability and surface roughness of composites. J. Dent. 2013, 41, e54–e61. [Google Scholar] [CrossRef] [PubMed]
- Puleio, F.; Di Spirito, F.; Lo Giudice, G.; Pantaleo, G.; Rizzo, D.; Lo Giudice, R. Long-term chromatic durability of white spot lesions through employment of infiltration resin treatment. Medicina 2023, 59, 749. [Google Scholar] [CrossRef] [PubMed]
- Joiner, A. Tooth colour: A review of the literature. J. Dent. 2004, 32, 3–12. [Google Scholar] [CrossRef] [PubMed]
| Composite Resin | Manufacturer | Type | Composition |
|---|---|---|---|
| Charisma Smart (LOT: M010541) | Kulzer GmbH, Hanau, Germany | Microhybrid | Bis GMA matrix, TEGDMA, HEDMA, filler load: 78% by weight: barium aluminum fluoride glass (0.02–2 μm), pyrogenic silicon dioxide (0.02–0.07 μm) |
| G-aenial A’chord (LOT: 2012232) | GC Corp., Tokyo, Japan | Nanohybrid | BisMEPP, filler load: 82% by weight: glass filler (300 nm barium glass), 16 nm (fumed silica), organic filler (300 nm barium glass; 16 nm fumed silica). |
| Neo Spectra ST HV (LOT: 2210000448) | Dentsplay, Konstans, Germany | Nanohybrid | Methacylate-modified polysiloxane (organically modified ceramic) dimethacrylate resins, ethyl-4 (dimethylamino) benzoate, and bis(4-methyl-phenyl) iodonium hexafluorophosphate. Filler load: 78–80% by weight: spherical, prepolymerized SphereTEC fillers (d3,50 ≈ 15 μm) non-agglomerated barium glass and ytterbium fluoride |
| ELS (LOT: E561) | Saremco, Rebstein, Switzerland | Microhybrid | Bis GMA 15 < 20%, Bisphenol A Glycerolate Dimethacrylate 10 <15%, 1000 D, L-Campherchinon-dl-Bornan-2.3-dion, Ironoxid black, Iron(III)oxid red, inorganic filler (50–3000 nm), Bis-EMA |
| RubyDent (LOT: RCNA2089) | Incidental, Istanbul, Türkiye | Nanohybrid | N/A |
| Toothpaste | Contents | RDA |
|---|---|---|
| Instant Relief (R.O.C.S., Russia) | Aqua, Glycerin, Dicalcium Phosphate Dihidrate, Xylitol, Hydroxyapatite, Silica, Xanthan Gum, Aroma, Calcium Glycerophosphate, Cocamidoprophyl Betaine, Sodium Lauroyl Sarcosinate, Hydroxyacetophenone, Sodium Benzoate, Sodium Saccharine, Magnesium Chloride, Sodium Methylparaben, Sodium Propylparaben, O-cymen-5-ol, Limonene. | 30 |
| Sensation Whitening (R.O.C.S., Russia) | Sorbitol, Silica, Glycerin, Aqua, Xylitol, Cocamidoprophyl Betaine, Aroma, Xanthan Gum, Calcium Glycerophosphate, Bromelain, Magnesium Chloride, Sodium Sacharine, Sodium Benzoate, O-cymen-5-ol, Titanium Dioxide. | 100 |
| Pro Polishing (R.O.C.S., Russia) | Aqua, Glycerin, 2–3 μm Silica, Hydroxyapatite, Xanthan Gum, Calcium Glycerophosphate, Polysorbate-20, Aroma, Sodium Lauryl Sulfate, Sodium Methylparaben, Sodium Saccharin, Sodium Benzoate, Sodium Propylparaben, O-cymen-5-ol, Potassium Hydroxide, Limonene. | 105 |
| Artificial saliva [22] | 1.5 mmol/L, CaCl2, 50 mmol/L KCl, 0.9 mmol/L, KH2PO4, 20 mmol/L Tris, (pH = 7.4) | - |
| T0–T1 | T0–T2 | T0–T3 | T0–T4 | |
|---|---|---|---|---|
| SIR | 5.92 ± 1.99 | 4.33 ± 2.12 | 4.13 ± 2.29 | 3.47 ± 1.56 B |
| SW | 5.99 ± 3.49 | 4.37 ± 3.92 | 3.47 ± 1.84 | 2.82 ± 1.24 A |
| SIR + PP | 5.95 ± 1.75 | 3.83 ± 2.54 | 3.50 ± 1.81 | 2.78 ± 0.98 A |
| SW + PP | 6.06 ± 1.92 | 3.20 ± 1.21 | 3.41 ± 1.76 | 2.84 ± 1.22 A |
| p | 0.995 | 0.217 | 0.367 | 0.007 |
| T0–T1 | T0–T2 | T0–T3 | T0–T4 | |
|---|---|---|---|---|
| Charisma Smart | 3.75 ± 1.54 A | 2.27 ± 1.17 A | 1.98 ± 1.06 A | 3.06 ± 1.53 AB |
| G-aenial A’chord | 6.49 ± 3.34 B | 4.32 ± 4.31 B | 3.46 ± 1.47 B | 3.92 ± 1.11 B |
| ELS | 7.13 ± 1.55 B | 5.09 ± 2.37 B | 5.69 ± 1.66 C | 3.45 ± 1.12 B |
| Neo Spectra ST | 6.50 ± 1.63 B | 3.89 ± 1.65 AB | 3.38 ± 1.63 B | 3.01 ± 1.48 AB |
| Ruby | 6.04 ± 1.78 B | 4.11 ± 1.82 AB | 3.64 ± 1.82 B | 2.45 ± 0.75 A |
| p | <0.001 | 0.001 | <0.001 | <0.001 |
| T0 | T1 | T2 | T3 | T4 | p | |
|---|---|---|---|---|---|---|
| SIR | 0.343 ± 0.049 a | 0.349 ± 0.048 a | 0.345 ± 0.044 a | 0.447 ± 0.072 b | 0.458 ± 0.063 b | <0.001 |
| SW | 0.344 ± 0.058 a | 0.349 ± 0.059 a | 0.359 ± 0.066 a | 0.450 ± 0.085 b | 0.481 ± 0.073 b | <0.001 |
| SIR + PP | 0.336 ± 0.053 a | 0.341 ± 0.054 a | 0.336 ± 0.051 a | 0.438 ± 0.110 b | 0.449 ± 0.058 b | <0.001 |
| SW + PP | 0.351 ± 0.058 a | 0.354 ± 0.058 a | 0.349 ± 0.063 a | 0.455 ± 0.048 b | 0.462 ± 0.069 b | <0.001 |
| p | 0.719 | 0.812 | 0.405 | 0.855 | 0.237 |
| T0 | T1 | T2 | T3 | T4 | p | |
|---|---|---|---|---|---|---|
| Charisma Smart | 0.305 ± 0.036 aA | 0.309 ± 0.04 aA | 0.296 ± 0.041 aA | 0.444 ± 0.089 b | 0.457 ± 0.065 b | <0.001 |
| G-aenial A’chord | 0.296 ± 0.039 aA | 0.304 ± 0.037 aA | 0.310 ± 0.032 aA | 0.430 ± 0.069 b | 0.451 ± 0.080 b | <0.001 |
| ELS | 0.405 ± 0.034 aC | 0.411 ± 0.031 aC | 0.406 ± 0.041 aC | 0.460 ± 0.038 b | 0.478 ± 0.058 b | <0.001 |
| Neo Spectra ST | 0.365 ± 0.038 aB | 0.368 ± 0.039 aB | 0.375 ± 0.039 aB | 0.461 ± 0.059 b | 0.467 ± 0.069 b | <0.001 |
| Ruby | 0.346 ± 0.039 aB | 0.349 ± 0.042 aB | 0.349 ± 0.045 aB | 0.443 ± 0.126 b | 0.458 ± 0.059 b | <0.001 |
| p | <0.001 | <0.001 | <0.001 | 0.585 | 0.606 |
| T0 | T1 | T2 | T3 | T4 | p | |
|---|---|---|---|---|---|---|
| SIR | 29/6/0/0 a | 29/6/0/0 a | 5/26/4/0 b | 0/21/12/2 b | 0/16/17/2 b | <0.001 |
| SW | 28/7/0/0 a | 28/7/0/0 a | 6/22/6/1 b | 3/20/11/1 b | 2/17/15/1 b | <0.001 |
| SIR + PP | 30/5/0/0 a | 30/5/0/0 a | 6/27/2/0 b | 1/19/15/0 bc | 0/13/21/1c | <0.001 |
| SW + PP | 32/3/0/0 a | 32/3/0/0 a | 5/27/3/0 b | 1/25/7/2 b | 0/19/15/1 b | <0.001 |
| p | 0.584 | 0.584 | 0.720 | 0.493 | 0.381 |
| T0 | T1 | T2 | T3 | T4 | p | |
|---|---|---|---|---|---|---|
| Charisma Smart | 26/2/0/0 a | 26/2/0/0 a | 14/13/1/0 abA | 4/18/6/0 bcA | 2/17/9/0 cA | <0.001 |
| G-aenial A’chord | 25/3/0/0 a | 25/3/0/0 a | 3/22/2/1 bB | 0/19/8/1 bAB | 0/17/10/1 bA | <0.001 |
| ELS | 21/7/0/0 a | 21/7/0/0 a | 2/20/6/0 bB | 0/10/16/2 bcB | 0/0/26/2cB | <0.001 |
| Neo Spectra ST | 22/6/0/0 a | 22/6/0/0 a | 0/28/0/0 bB | 1/21/6/0 bA | 0/16/12/0 bA | <0.001 |
| Ruby | 25/3/0/0 a | 25/3/0/0 a | 3/19/6/0 bB | 0/17/9/2 bAB | 0/15/11/2 bA | <0.001 |
| p | 0.261 | 0.265 | <0.001 | 0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meseli, S.; Alkan, E.; Korkut, B.; Kanar, O.; Tagtekin, D. Abrasiveness and Bleaching Level of Toothpastes on Composite Resins: A Quantitative Analysis Using a Novel Brushing Simulator. Appl. Sci. 2025, 15, 2314. https://doi.org/10.3390/app15052314
Meseli S, Alkan E, Korkut B, Kanar O, Tagtekin D. Abrasiveness and Bleaching Level of Toothpastes on Composite Resins: A Quantitative Analysis Using a Novel Brushing Simulator. Applied Sciences. 2025; 15(5):2314. https://doi.org/10.3390/app15052314
Chicago/Turabian StyleMeseli, Simge, Elif Alkan, Bora Korkut, Ozlem Kanar, and Dilek Tagtekin. 2025. "Abrasiveness and Bleaching Level of Toothpastes on Composite Resins: A Quantitative Analysis Using a Novel Brushing Simulator" Applied Sciences 15, no. 5: 2314. https://doi.org/10.3390/app15052314
APA StyleMeseli, S., Alkan, E., Korkut, B., Kanar, O., & Tagtekin, D. (2025). Abrasiveness and Bleaching Level of Toothpastes on Composite Resins: A Quantitative Analysis Using a Novel Brushing Simulator. Applied Sciences, 15(5), 2314. https://doi.org/10.3390/app15052314






