Simplified Model of Humidity in the Space of a Protective Mask and Experimental Verification—A Pilot Study
Abstract
1. Introduction
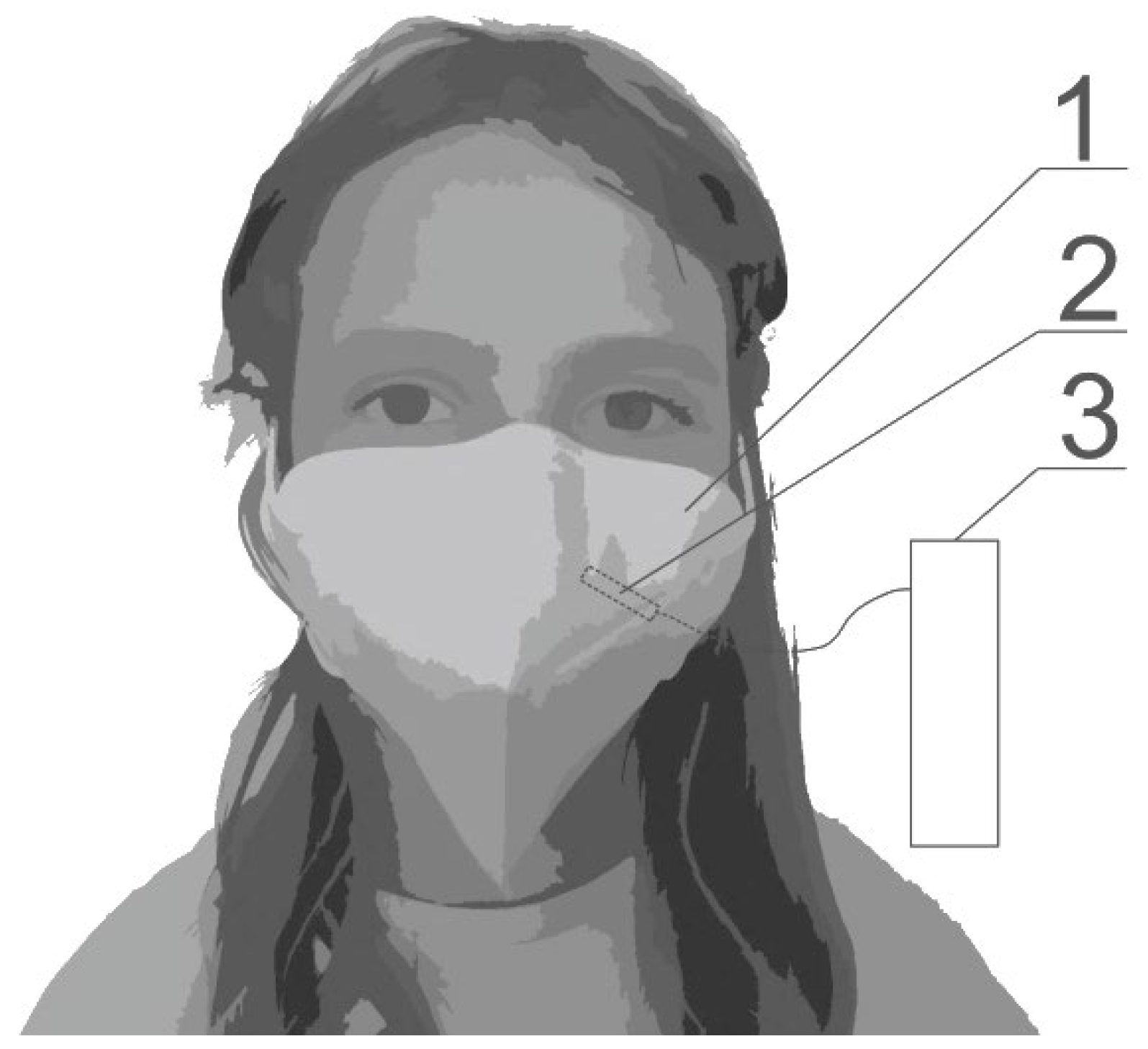
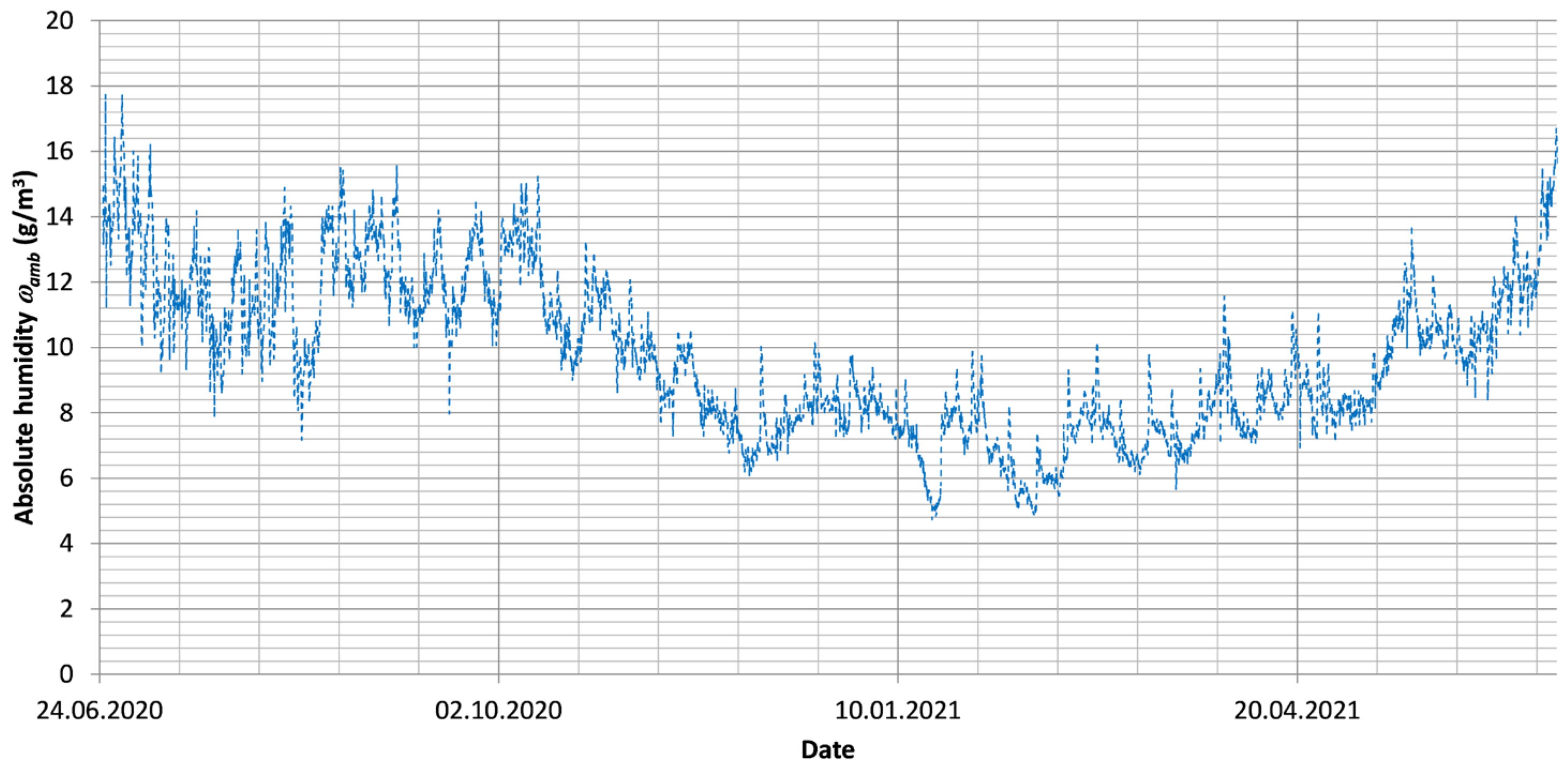
2. Materials and Methods
- -
- Person A: Female, age 35, height 164 cm, weight 64 kg.
- -
- Person B: Female, age 57, height 171 cm, weight 102 kg.
- -
- Person C: Male, age 43, height 180 cm, weight 87 kg.
- -
- Person D: Male, age 58, height 178 cm, weight 100 kg.
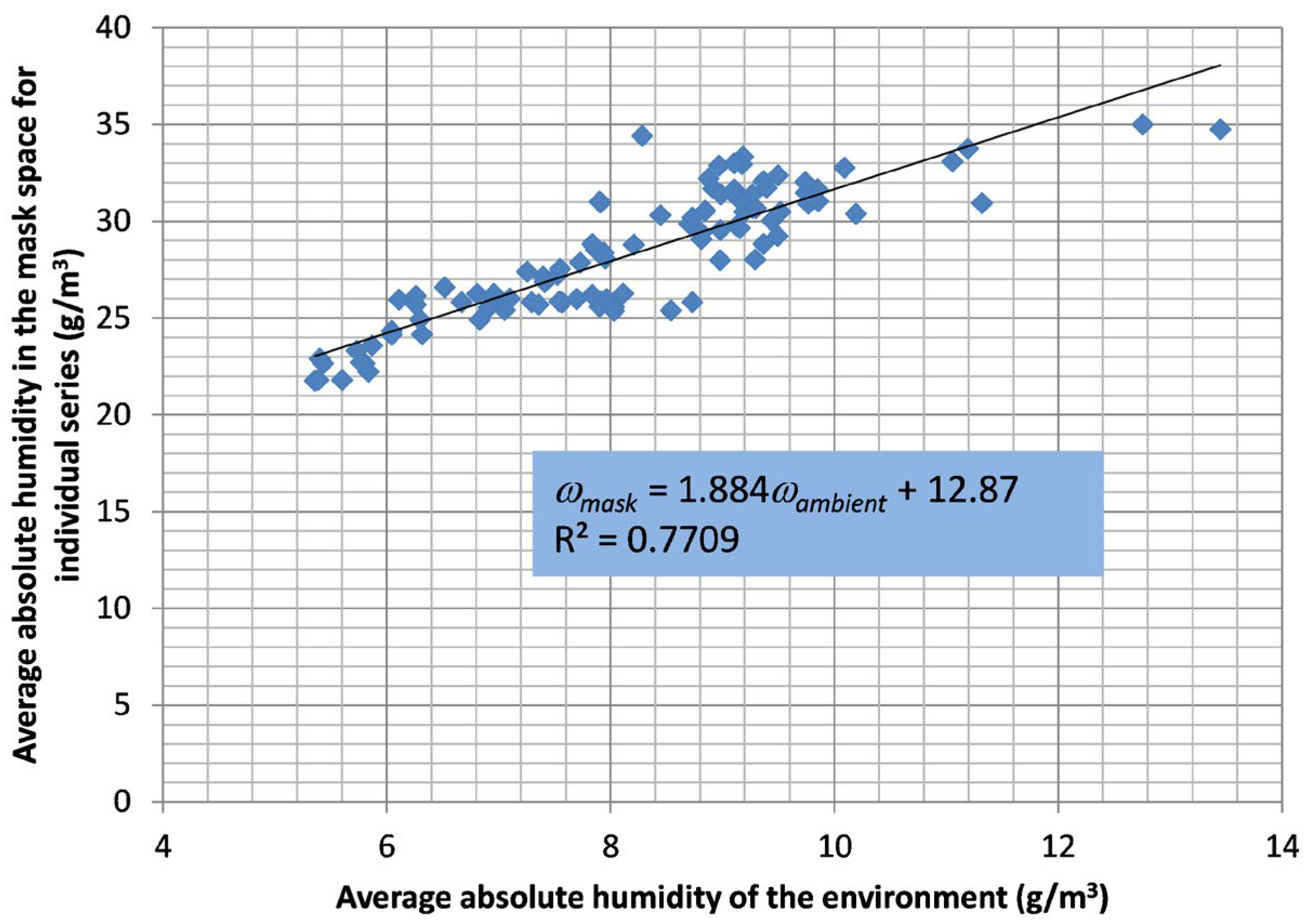
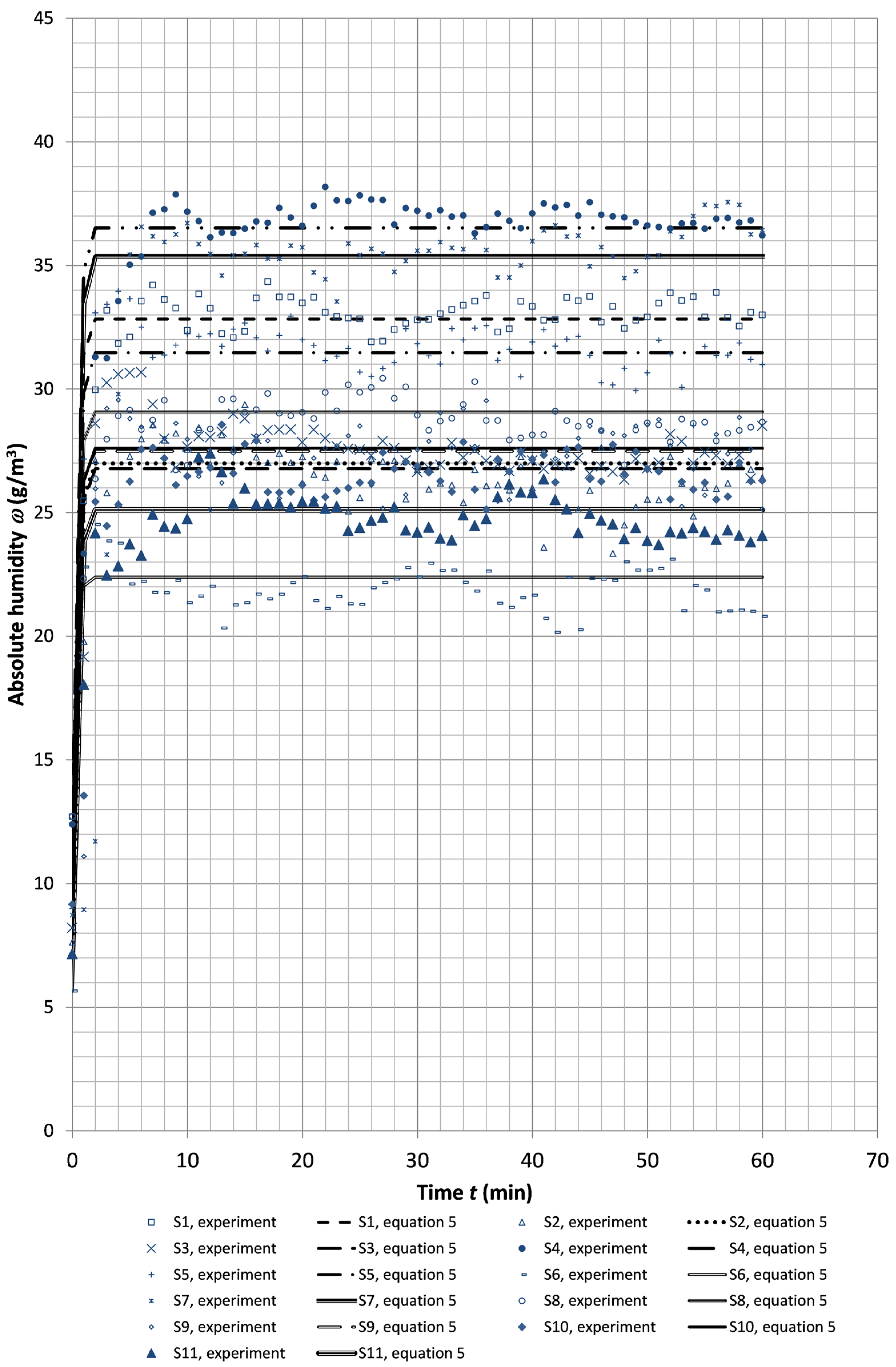
3. Results and Discussion
4. Simplified One-Dimensional Model of Absolute Humidity in the Mask Space
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Nomenclature
| n | air change rate in the mask (ACH) (h−1) |
| q | volumetric flow (m3/h) |
| Qg | humidity generated by the mask user (g/h) |
| Qn | moisture removed from the mask space and supplied to the mask from the outside (g/h) |
| T | temperature in the mask space (°C) |
| Tm | mean temperature in the mask space (°C) |
| Tm_max | maximum temperature from one-hour average temperatures in the mask space (°C) |
| Tm_min | minimum temperature from one-hour average temperatures in the mask space (°C) |
| t | time (min or h) |
| V | tidal volume (m3) |
| Greek symbols | |
| σTm | standard deviation for temperature in the mask space (°C) |
| σϕm | standard deviation for relative humidity in the mask space (%) |
| σωm | standard deviation for absolute humidity in the mask space (g/m3) |
| ϕm | average relative humidity in the mask space (%) |
| ϕm_max | maximum relative humidity from one-hour average relative humidity values in the mask space (%) |
| ϕm_min | minimum relative humidity from one-hour average relative humidity values in the mask space (%) |
| ω | absolute humidity in the mask space (g/m3) |
| ωamb | ambient absolute humidity (external) (g/m3) |
| ωexp | absolute humidity from measurements (g/m3) |
| ωm | mean absolute humidity in the mask space (g/m3) |
| ωm_max | maximum absolute humidity from one-hour average absolute humidity values in the mask space (g/m3) |
| ωm_min | minimum absolute humidity from one-hour average absolute humidity values in the mask space (g/m3) |
| ωnum | absolute humidity determined from Equation (5) (g/m3) |
| ωt=0 | initial value of absolute humidity in the mask space (g/m3) |
References
- ASHRAE Standard 55; Thermal Environmental Conditions for Human Occupancy. ASHRAE Standard: Peachtree Corners, GA, USA, 2012.
- Dumała, S.M.; Guz, Ł.; Badora, A. Indoor Air Quality in Schools Located in Poland, Lublin Province. J. Ecol. Eng. 2024, 25, 17–26. [Google Scholar] [CrossRef]
- Szczurek, A.; Maciejewska, M. Categorisation for air quality assessment in car cabin. Transp. Res. D Transp. Environ. 2016, 48, 161–170. [Google Scholar] [CrossRef]
- Gupta, D. Living with in-mask micro-climate. Med. Hypotheses 2020, 144, 110010. [Google Scholar] [CrossRef] [PubMed]
- Gładyszewska-Fiedoruk, K.; Teleszewski, T.J. Experimental studies of carbon dioxide concentration in the space under the face mask protecting against COVID-19—Pilot studies. J. Environ. Health. Sci. Eng. 2022, 20, 1111–1119. [Google Scholar] [CrossRef]
- Hayashi, C.; Tokura, H. The effects of two kinds of mask (with or without exhaust valve) on clothing microclimates inside the mask in participants wearing protective clothing for spraying pesticides. Int. Arch. Occup. Environ. Health 2004, 77, 73–78. [Google Scholar] [CrossRef]
- Teleszewski, T.J.; Gładyszewska-Fiedoruk, K.; Sulewska, M.J. Experimental Studies of Hydraulic Losses and Carbon Dioxide Concentration in the Space Under the Face Mask Protecting Against COVID-19. Civ. Environ. Eng. Rep. 2022, 32, 13–24. [Google Scholar] [CrossRef]
- Chughtai, A.A.; Stelzer-Braid, S.; Rawlinson, W.; Pontivivo, G.; Wang, Q.; Pan, Y.; Zhang, D.; Zhang, Y.; Li, L.; MacIntyre, C.R. Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers. BMC Infect. Dis. 2019, 19, 491. [Google Scholar] [CrossRef]
- McLaws, M.-L.; Chughtai, A.A.; Salmon, S.; MacIntyre, C.R. A highly precautionary doffing sequence for health care workers after caring for wet Ebola patients to further reduce occupational acquisition of Ebola. Am. J. Infect. Control 2016, 44, 740–744. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Infection Prevention and Control Of Epidemic- and Pandemic-Prone Acute Respiratory Infections In Health Care; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Li, Y.; Liang, M.; Gao, L.; Ahmed, M.A.; Uy, J.P.; Cheng, C.; Zhou, Q.; Sun, C. Face masks to prevent transmission of COVID-19: A systematic review and meta-analysis. Am. J. Infect. Control 2021, 49, 900–906. [Google Scholar] [CrossRef]
- Liao, M.; Liu, H.; Wang, X.; Hu, X.; Huang, Y.; Liu, X.; Brenan, K.; Mecha, J.; Nirmalan, M.; Lu, J.R. A technical review of face mask wearing in preventing respiratory COVID-19 transmission. Curr. Opin. Colloid Interface Sci. 2021, 52, 101417. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19): Masks. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-masks (accessed on 5 January 2024).
- Burgos-Blasco, B.; Arriola-Villalobos, P.; Fernandez-Vigo, J.I.; Oribio-Quinto, C.; Ariño-Gutierrez, M.; Diaz-Valle, D.; Benitez-Del-Castillo, J.M. Face mask use and effects on the ocular surface health: A comprehensive review. Ocul. Surf. 2023, 27, 56–66. [Google Scholar] [CrossRef]
- Tang, T.; Zhu, Y.; Zhou, X.; Guo, Z.; Mao, Y.; Jiang, H.; Fang, Z.; Zheng, Z.; Chen, X. Investigation of the effects of face masks on thermal comfort in Guangzhou, China. Build. Environ. 2022, 214, 108932. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Lin, J.; Han, J.; Gao, X.; Zhang, Y.; Hu, B.; Guidoin, R.; Wang, L. Prolonged Use of Surgical Masks and Respirators Affects the Protection and Comfort for Healthcare Workers. Materials 2022, 15, 7918. [Google Scholar] [CrossRef]
- Cherrie, J.W.; Wang, S.; Mueller, W.; Wendelboe-Nelson, C.; Loh, M. In-mask temperature and humidity can validate respirator wear-time and indicate lung health status. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 578–583. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, H.; Chen, H.; Li, X.; Ran, C.; Sun, H.; Wang, L. Does mask wearing affect skin health? An untargeted skin metabolomics study. Environ. Int. 2023, 178, 108073. [Google Scholar] [CrossRef]
- Park, A.; Khadka, S.; Sato, F.; Omura, S.; Fujita, M.; Hashiwaki, K.; Tsunoda, I. Bacterial and Fungal Isolation from Face Masks: Newly Emerged Hygiene Issues Under COVID-19 Pandemic. Sci. Rep. 2022, 12, 11361. [Google Scholar] [CrossRef]
- Gyapong, F.; Debra, E.; Ofori, M.O.; Ayerakwa, E.A.; Abban, M.K.; Mosi, L.; Isawumi, A. Multi-drug resistant microbes are resident on nose masks used as preventive protocols for COVID-19 in selected Ghanaian cohort. Wellcome Open Res. 2023, 8, 250. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, H.; Heo, D.W.; Ahn, I.-S.; Auh, Q.-S. Volatile sulfide compounds and oral microorganisms on the inner surface of masks in individuals with halitosis during COVID-19 pandemic. Sci. Rep. 2023, 13, 2487. [Google Scholar] [CrossRef]
- Merenstein, C.; Fitzgerald, A.S.; Khatib, L.A.; Graham-Wooten, J.; Bushman, F.D.; Collman, R.G. Effects of Mask Reuse on the Oropharyngeal, Skin, and Mask Microbiome. J. Infect. Dis. 2023, 228, 479–486. [Google Scholar] [CrossRef]
- Ostrowski, P.; Masiuk, H.; Kulig, P.; Skoryk, A.; Wcisłek, A.; Jursa-Kulesza, J.; Sarna, A.; Sławiński, M.; Kotowski, M.; Tejchman, K.; et al. Medical Face Masks Do Not Affect Acid-Base Balance Yet Might Facilitate the Transmission of Staphylococcus aureus in Hospital Settings during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2023, 20, 2474. [Google Scholar] [CrossRef]
- Liu, Z.; Chang, Y.; Chu, W.; Yan, M.; Mao, Y.; Zhu, Z.; Wu, H.; Zhao, J.; Dai, K.; Li, H.; et al. Surgical masks as source of bacterial contamination during operative procedures. J. Orthop. Transl. 2018, 14, 57–62. [Google Scholar] [CrossRef]
- Stoll, D.; Antonyuk, S. Influence of Humidity on FFP Masks with Electret Filter Media Under Real-Life Wearing Conditions. Atmosphere 2025, 16, 62. [Google Scholar] [CrossRef]
- Solano, T.; Shoele, K. Investigation of the Role of Face Shape on the Flow Dynamics and Effectiveness of Face Masks. Fluids 2022, 7, 209. [Google Scholar] [CrossRef]
- Barari, K.; Si, X.; Xi, J. Impacts of Mask Wearing and Leakages on Cyclic Respiratory Flows and Facial Thermoregulation. Fluids 2024, 9, 9. [Google Scholar] [CrossRef]
- Pisapia, F.; Rees, D.; Rasekh, M. Design and Evaluation of Face Mask Filtration: Mechanisms, Formulas, and Fluid Dynamics Simulations. Appl. Sci. 2024, 14, 5432. [Google Scholar] [CrossRef]
- Rasekh, M.; Pisapia, F.; Hafizi, S.; Rees, D. Filtering Efficiency and Design Properties of Medical- and Non-Medical-Grade Face Masks: A Multiscale Modeling Approach. Appl. Sci. 2024, 14, 4796. [Google Scholar] [CrossRef]
- Factors Shaping the Climate of Poland. Available online: https://zpe.gov.pl/a/factors-shaping-the-climate-of-poland/D12UnACu9 (accessed on 5 April 2022).
- EN 14683:2001; Medical Face Masks—Requirements and Test Methods. European Standards: Pilsen, Czech Republic, 2001.
- EN 149:2001+A1:2009; Respiratory Protective Devices—Filtering Half Masks to Protect Against Particles—Requirements, Testing, Marking. European Standards: Pilsen, Czech Republic, 2001.
- GB 2626-2006; Respiratory Protective Equipment—Non-Powered Air-Purifying Particle Respirator. Chinese GB Standards: Beijing, China, 2006.
- Statistical Yearbook. Available online: https://stat.gov.pl/metainformacje/slownik-pojec/pojecia-stosowane-w-statystyce-publicznej/861,pojecie.html (accessed on 5 April 2022).
- Statistical Yearbook. Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/ludnosc-piramida/ (accessed on 5 April 2022).
- ISO 16900-12:2016; Respiratory Protective Devices—Methods of Test and Test Equipment—Part 12: Determination of Volume-Averaged Work of Breathing and Peak Respiratory Pressures. ISO: Geneva, Switzerland, 2016.
- ISO/TS 16976-4:2012; Respiratory Protective Devices—Human Factors—Part 4: Work of Breathing and Breathing Resistance: Physiologically Based Limits. ISO: Geneva, Switzerland, 2012.
- Makowski, K. New requirements in regard of ergonomic parameters of filtering respiratory protective devices. Bezpieczeństwo Pr. Nauka I Prakt. 2020, 10, 22–25. (In Polish) [Google Scholar] [CrossRef]
- Bergman, T.L.; Lavine, A.S.; Incropera, F.P. Fundamentals of Heat and Mass Transfer, 7th ed.; John Wiley & Sons, Incorporated: New York, NY, USA, 2011; ISBN 9781118137253. [Google Scholar]
- Psychrometric Chart. Available online: https://drajmarsh.bitbucket.io/psychro-chart2d.html (accessed on 5 February 2022).
- Types of Respirators and Masks. Available online: https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/prevent-getting-sick/types-of-masks.html (accessed on 5 February 2022).
- Segovia, J.M.; Huang, C.-H.; Mamishev, M.; Yuan, N.; He, J.; Novosselov, I. Performance of Textile Mask Materials in Varied Humidity: Filtration Efficiency, Breathability, and Quality Factor. Appl. Sci. 2022, 12, 9360. [Google Scholar] [CrossRef]
- Zemitis, J.; Borodinecs, A.; Frolova, M. Measurements of moisture production caused by various sources. Energy Build. 2016, 127, 884–891. [Google Scholar] [CrossRef]
- Horak, J.; Schmerold, I.; Wimmer, K.; Schauberger, G. Cabin air temperature of parked vehicles in summer conditions: Life-threatening environment for children and pets calculated by a dynamic model. Theor. Appl. Climatol. 2017, 130, 107–118. [Google Scholar] [CrossRef]
- Sun-Ik, N.; Minsung, K.; Min, S.K. Performance analysis of an automotive heat pump system with desiccant coated heat exchangers. Appl. Therm. Eng. 2022, 213, 118723. [Google Scholar] [CrossRef]
- Batog, P.; Badura, M. Dynamic of Changes in Carbon Dioxide Concentration in Bedrooms. Procedia Eng. 2013, 57, 175–182. [Google Scholar] [CrossRef]
- Macarulla, M.; Casals, M.; Carnevali, M.; Forcada, N.; Gangolells, M. Modelling indoor air carbon dioxide concentration using grey-box models. Build Environ. 2017, 117, 146–153. [Google Scholar] [CrossRef]
- Gładyszewska-Fiedoruk, K.; Teleszewski, T.J. Modeling of Humidity in Passenger Cars Equipped with Mechanical Ventilation. Energies 2020, 13, 2987. [Google Scholar] [CrossRef]





| Mask Number | Tm | Tm_min | Tm_max | σTm |
| - | °C | °C | °C | °C |
| Mask 1 | 31.7 | 30.1 | 33.7 | 1.3 |
| Mask 2 | 32.2 | 29.3 | 34.1 | 2.1 |
| Mask 3 | 30.5 | 27.1 | 33.9 | 3.7 |
| Mask 4 | 32.7 | 29.2 | 33.8 | 1.4 |
| Mask 5 | 32.6 | 30.5 | 34.1 | 1.5 |
| Mask Number | ϕm | ϕm_min | ϕm_max | σϕm |
| - | % | % | % | % |
| Mask 1 | 82.5 | 76.0 | 92.9 | 5.8 |
| Mask 2 | 87.1 | 79.0 | 92.9 | 5.7 |
| Mask 3 | 83.5 | 81.9 | 87.1 | 2.4 |
| Mask 4 | 85.5 | 78.7 | 93.7 | 4.1 |
| Mask 5 | 80.8 | 75.3 | 86.4 | 5.2 |
| Mask Number | ωm | ωm_min | ωm_max | σωm |
| - | g/m3 | g/m3 | g/m3 | g/m3 |
| Mask 1 | 27.5 | 24.0 | 32.5 | 3.4 |
| Mask 2 | 29.8 | 24.1 | 33.4 | 3.6 |
| Mask 3 | 25.7 | 21.8 | 30.7 | 4.8 |
| Mask 4 | 29.9 | 24.9 | 34.8 | 3.0 |
| Mask 5 | 28.2 | 26.3 | 31.0 | 2.1 |
| Number of Measurement Series | Person | Mask | Month | Average Ambient Temperature | Average Ambient Relative Humidity | Average Ambient Absolute Humidity | Average Temperature in the Mask Space | Average Relative Humidity in the Mask Space | Average Absolute Humidity in the Mask Space |
|---|---|---|---|---|---|---|---|---|---|
| Tm | ϕm | ωm | |||||||
| - | - | - | - | °C | % | g/m3 | °C | % | g/m3 |
| S1 | B | 1 | September | 22.0 | 52.0 | 10.1 | 33.2 | 90.9 | 32.5 |
| S2 | D | 1 | April | 20.3 | 41.5 | 7.3 | 30.6 | 82.3 | 26.7 |
| S3 | D | 2 | April | 19.5 | 50.9 | 8.5 | 29.7 | 90.5 | 27.3 |
| S4 | C | 2 | September | 22.6 | 63.5 | 12.8 | 33.3 | 99.1 | 36.1 |
| S5 | B | 3 | September | 22.0 | 45.0 | 8.7 | 33.7 | 81.6 | 31.2 |
| S6 | D | 3 | March | 18.7 | 35.0 | 5.6 | 27.2 | 82.1 | 21.7 |
| S7 | C | 4 | November | 24.5 | 37.0 | 8.3 | 33.7 | 93.0 | 34.6 |
| S8 | B | 4 | September | 20.4 | 52.0 | 9.2 | 31.6 | 85.5 | 28.3 |
| S9 | A | 5 | April | 21.0 | 35.6 | 6.5 | 32.4 | 77.0 | 26.8 |
| S10 | D | 5 | April | 20.3 | 45.0 | 7.9 | 30.4 | 83.4 | 26.0 |
| S11 | B | 1 | December | 19.8 | 37.0 | 6.3 | 30.9 | 75.8 | 24.4 |
| Number of Measurement Series | S1 | S2 | S3 | S4 | S5 | S6 | S7 | S8 | S9 | S10 | S11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Human-generated moisture Qg [g/h] | 32.7 | 28.4 | 26.3 | 34.2 | 32.7 | 24.2 | 38.4 | 28.6 | 30.2 | 28.4 | 27.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teleszewski, T.J.; Gładyszewska-Fiedoruk, K.; Liu, J. Simplified Model of Humidity in the Space of a Protective Mask and Experimental Verification—A Pilot Study. Appl. Sci. 2025, 15, 12513. https://doi.org/10.3390/app152312513
Teleszewski TJ, Gładyszewska-Fiedoruk K, Liu J. Simplified Model of Humidity in the Space of a Protective Mask and Experimental Verification—A Pilot Study. Applied Sciences. 2025; 15(23):12513. https://doi.org/10.3390/app152312513
Chicago/Turabian StyleTeleszewski, Tomasz Janusz, Katarzyna Gładyszewska-Fiedoruk, and Jianming Liu. 2025. "Simplified Model of Humidity in the Space of a Protective Mask and Experimental Verification—A Pilot Study" Applied Sciences 15, no. 23: 12513. https://doi.org/10.3390/app152312513
APA StyleTeleszewski, T. J., Gładyszewska-Fiedoruk, K., & Liu, J. (2025). Simplified Model of Humidity in the Space of a Protective Mask and Experimental Verification—A Pilot Study. Applied Sciences, 15(23), 12513. https://doi.org/10.3390/app152312513









