Marginal and Internal Fit of Zirconia Crowns with Varying Yttria Content and Finish Line Configurations: An In Vitro Study
Abstract
1. Introduction
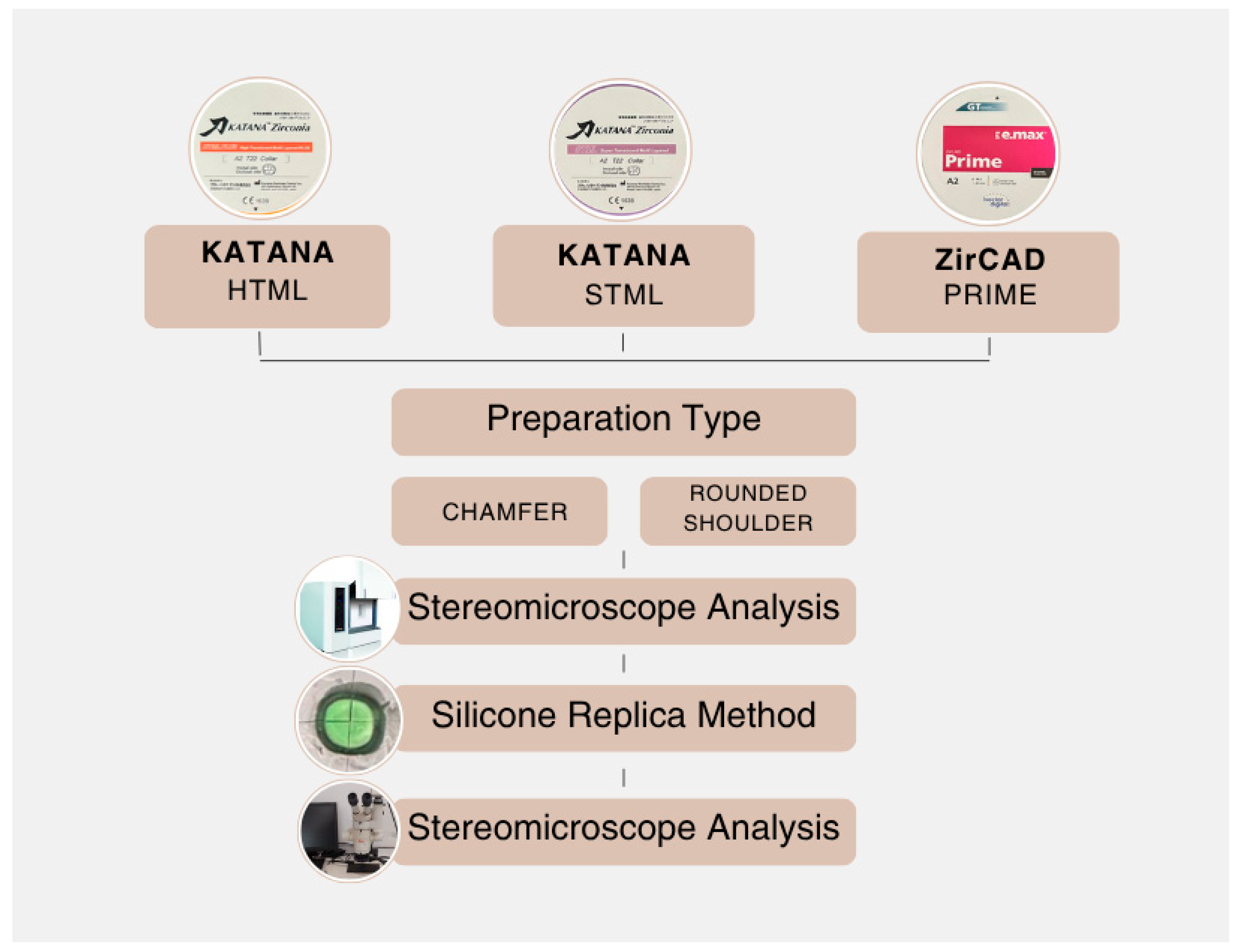
2. Materials and Methods
2.1. Sample Size Calculation
2.2. Sample Preparation
2.3. Evaluation of Marginal and Internal Fit
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HTML | KATANA High Translucent Multilayer Zirconia |
| STML | KATANA Super Translucent Multilayer Zirconia |
| ZirCAD | IPS e.max ZirCAD Prime |
| R | Rounded Shoulder |
| C | Chamfer |
| µm | Micrometer |
| ANOVA | A three-way analysis of variance |
| Y-TZP | Yttria-stabilized tetragonal zirconia polycrystal |
| 2D | Two Dimensions |
References
- Cesar, P.F.; de Paula Miranda, R.B.; Santos, K.F.; Scherrer, S.S.; Zhang, Y. Recent advances in dental zirconia: 15 years of material and processing evolution. Dent. Mater. 2024, 40, 824–836. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Evaluating dental zirconia. Dent. Mater. 2019, 35, 15–23. [Google Scholar] [CrossRef]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. PeerJ 2023, 11, e15669. [Google Scholar] [CrossRef]
- Hasanzade, M.; Moharrami, M.; Alikhasi, M. How adjustment could affect internal and marginal adaptation of CAD/CAM crowns made with different materials. J. Adv. Prosthodont. 2020, 12, 344. [Google Scholar] [CrossRef]
- Baig, M.R.; Akbar, A.A.; Embaireeg, M. Effect of finish line design on the fit accuracy of CAD/CAM monolithic polymer-infiltrated ceramic-network fixed dental prostheses: An in vitro study. Polymers 2021, 13, 4311. [Google Scholar] [CrossRef]
- Suzuki, S.; Katsuta, Y.; Ueda, K.; Watanabe, F. Marginal and internal fit of three-unit zirconia fixed dental prostheses: Effects of prosthesis design, cement space, and zirconia type. J. Prosthodont. Res. 2020, 64, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.-C.; Chung, K.-H.; Yau, H.-T. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef]
- Rizonaki, M.; Jacquet, W.; Bottenberg, P.; Depla, L.; Boone, M.; De Coster, P.J. Evaluation of marginal and internal fit of lithium disilicate CAD-CAM crowns with different finish lines by using a micro-CT technique. J. Prosthet. Dent. 2022, 127, 890–898. [Google Scholar] [CrossRef]
- Lyu, J.; Cao, X.; Yang, X.; Tan, J.; Liu, X. Effect of finish line designs on the dimensional accuracy of monolithic zirconia crowns fabricated with a material jetting technique. J. Prosthet. Dent. 2025, 134, 176.e1–176.e8. [Google Scholar] [CrossRef]
- Mancuso, E.; Gasperini, T.; Maravic, T.; Mazzitelli, C.; Josic, U.; Forte, A.; Pitta, J.; Mazzoni, A.; Fehmer, V.; Breschi, L.; et al. The influence of finishing line and luting material selection on the seating accuracy of CAD/CAM indirect composite restorations. J. Dent. 2024, 148, 105231. [Google Scholar] [CrossRef]
- Miura, S.; Tsukada, S.; Fujita, T.; Fujisawa, M.; Vallittu, P.; Lassila, L. Effects of sintering protocols, yttria content, and zirconia thickness on the optical properties of monolithic zirconia. J. Oral Sci. 2025, 67, 122–126. [Google Scholar] [CrossRef]
- Bruhnke, M.; Awwad, Y.; Müller, W.-D.; Beuer, F.; Schmidt, F. Mechanical properties of new generations of monolithic, multi-layered zirconia. Materials 2022, 16, 276. [Google Scholar] [CrossRef]
- Fasih, P.; Tavakolizadeh, S.; Monfared, M.S.; Sofi-Mahmudi, A.; Yari, A. Marginal fit of monolithic versus layered zirconia crowns assessed with 2 marginal gap methods. J. Prosthet. Dent. 2023, 130, 250.e1–250.e7. [Google Scholar] [CrossRef]
- Molin, M.; Karlsson, S. The fit of gold inlays and three ceramic inlay systems: A clinical and in vitro study. Acta Odontol. Scand. 1993, 51, 201–206. [Google Scholar] [CrossRef]
- Abduo, J.; Ho, G.; Centorame, A.; Chohan, S.; Park, C.; Abdouni, R.; Le, P.; Ngo, C. Marginal accuracy of monolithic and veneered zirconia crowns fabricated by conventional and digital workflows. J. Prosthodont 2023, 32, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Zhou, Y.; Jiang, J.; Wang, Y.; He, F. Accuracy and margin quality of advanced 3D-printed monolithic zirconia crowns. J. Prosthet. Dent. 2023, 133, 1284–1292. [Google Scholar] [CrossRef]
- Tabata, L.F.; de Lima Silva, T.A.; de Paula Silveira, A.C.; Ribeiro, A.P.D. Marginal and internal fit of CAD-CAM composite resin and ceramic crowns before and after internal adjustment. J. Prosthet. Dent. 2020, 123, 500–505. [Google Scholar] [CrossRef]
- de Paula Silveira, A.C.; Chaves, S.B.; Hilgert, L.A.; Ribeiro, A.P.D. Marginal and internal fit of CAD-CAM-fabricated composite resin and ceramic crowns scanned by 2 intraoral cameras. J. Prosthet. Dent. 2017, 117, 386–392. [Google Scholar] [CrossRef]
- McLean, J.W. Evolution of dental ceramics in the twentieth century. J. Prosthet. Dent. 2001, 85, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Baldi, A.; Comba, A.; Rozzi, D.; Pereira, G.K.R.; Valandro, L.F.; Tempesta, R.M.; Scotti, N. Does partial adhesive preparation design and finish line depth influence trueness and precision of intraoral scanners? J. Prosthet. Dent. 2023, 129, 637.e1–637.e9. [Google Scholar] [CrossRef] [PubMed]
- Sirous, S.; Navadeh, A.; Ebrahimgol, S.; Atri, F. Effect of preparation design on marginal adaptation and fracture strength of ceramic occlusal veneers: A systematic review. Clin. Exp. Dent. Res. 2022, 8, 1391–1403. [Google Scholar] [CrossRef]
- Haggag, K.; Abbas, M.; Ramadan, H. Effect of thermo-mechanical aging on the marginal fit of two types of monolithic zirconia crowns with two finish line designs. Al-Azhar Dent. J. Girls 2018, 5, 121–128. [Google Scholar] [CrossRef]
- Yu, H.; Chen, Y.-H.; Cheng, H.; Sawase, T. Finish-line designs for ceramic crowns: A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 122, 22–30.e5. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Sharma, V.; Paliwal, J.; Meena, K.K.; Madaan, R.; Gurjar, B. An in vitro comparison of zirconia and hybrid ceramic crowns with heavy chamfer and shoulder finish lines. Cureus 2023, 15, e33940. [Google Scholar] [CrossRef]
- Angerame, D.; De Biasi, M.; Agostinetto, M.; Franzò, A.; Marchesi, G. Influence of preparation designs on marginal adaptation and failure load of full-coverage occlusal veneers after thermomechanical aging simulation. J. Esthet. Restor. Dent. 2019, 31, 280–289. [Google Scholar] [CrossRef]
- Euán, R.; Figueras-Álvarez, O.; Cabratosa-Termes, J.; Oliver-Parra, R. Marginal adaptation of zirconium dioxide copings: Influence of the CAD/CAM system and the finish line design. J. Prosthet. Dent. 2014, 112, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E. Influence of surface treatment on the bond strength of resin cements to monolithic zirconia. J. Adhes. Dent. 2016, 18, 387–395. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Novel zirconia materials in dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Michailova, M.; Elsayed, A.; Fabel, G.; Edelhoff, D.; Zylla, I.-M.; Stawarczyk, B. Comparison between novel strength-gradient and color-gradient multilayered zirconia using conventional and high-speed sintering. J. Mech. Behav. Biomed. Mater. 2020, 111, 103977. [Google Scholar] [CrossRef]
- Kang, C.-M.; Hsu, W.-C.; Chen, M.-S.; Wu, H.-Y.; Mine, Y.; Peng, T.-Y. Fracture characteristics and translucency of multilayer monolithic zirconia crowns of various thicknesses. J. Dent. 2024, 145, 105023. [Google Scholar] [CrossRef]
- Güntekin, N.; Kızılırmak, B.; Tunçdemir, A.R. Comparison of mechanical and optical properties of multilayer zirconia after high-speed and repeated sintering. Materials 2025, 18, 1493. [Google Scholar] [CrossRef] [PubMed]
- Biçer, E.Y.; Öztürk, E.K.; Güngör, M.B. Strength-gradient multilayer zirconia ceramics: A narrative review of the mechanical and optical properties. J. Am. Ceram. Soc. 2025, 108, e20711. [Google Scholar] [CrossRef]
- Giordano, R., II. Ceramics overview. Br. Dent. J. 2022, 232, 658–663. [Google Scholar] [CrossRef]
- Kim, J.-H.; Oh, S.; Uhm, S.-H. Effect of the crystallization process on the marginal and internal gaps of lithium disilicate CAD/CAM crowns. BioMed Res. Int. 2016, 2016, 8635483. [Google Scholar] [CrossRef]
- Yildirim, G.; Uzun, I.H.; Keles, A. Evaluation of marginal and internal adaptation of hybrid and nanoceramic systems with microcomputed tomography: An in vitro study. J. Prosthet. Dent. 2017, 118, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef]
- Son, K.; Lee, S.; Kang, S.H.; Park, J.; Lee, K.-B.; Jeon, M.; Yun, B.-J. A comparison study of marginal and internal fit assessment methods for fixed dental prostheses. J. Clin. Med. 2019, 8, 785. [Google Scholar] [CrossRef] [PubMed]
- Boitelle, P.; Tapie, L.; Mawussi, B.; Fromentin, O. Evaluation of the marginal fit of CAD-CAM zirconia copings: Comparison of 2D and 3D measurement methods. J. Prosthet. Dent. 2018, 119, 75–81. [Google Scholar] [CrossRef]
- Ueda, K.; Watanabe, F.; Katsuta, Y.; Seto, M.; Ueno, D.; Hiroyasu, K.; Suzuki, S.; Erdelt, K.; Güth, J.-F. Marginal and internal fit of three-unit fixed dental prostheses fabricated from translucent multicolored zirconia: Framework versus complete contour design. J. Prosthet. Dent. 2021, 125, 340.e1–340.e6. [Google Scholar] [CrossRef]
- Cunali, R.S.; Saab, R.C.; Correr, G.M.; Cunha, L.F.; Ornaghi, B.P.; Ritter, A.V.; Gonzaga, C.C. Marginal and internal adaptation of zirconia crowns: A comparative study of assessment methods. Braz. Dent. J. 2017, 28, 467–473. [Google Scholar] [CrossRef]
- Doan, T.M.; Nguyen, T.N.; Pham, V.-K.; Chotprasert, N.; Vu, C.T.B. Comparative analysis of the fit quality of monolithic zirconia veneers produced through traditional and digital workflows using silicone replica technique: An in vitro study. BMC Oral Health 2024, 24, 1566. [Google Scholar] [CrossRef] [PubMed]
- Arezoobakhsh, A.; Shayegh, S.S.; Ghomi, A.J.; Hakimaneh, S.M.R. Comparison of marginal and internal fit of 3-unit zirconia frameworks fabricated with CAD-CAM technology using direct and indirect digital scans. J. Prosthet. Dent. 2020, 123, 105–112. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Al-Sardi, M.; Goodacre, B.J.; Goodacre, C.J.; Al Hamad, K.Q.; Özcan, M.; Husain, N.A.-H.; Baba, N.Z. Evaluation of marginal and internal fit of ceramic laminate veneers fabricated with five intraoral scanners and indirect digitization. Materials 2023, 16, 2181. [Google Scholar] [CrossRef]
- Guachetá, L.; Stevens, C.D.; Cardona, J.A.T.; Murgueitio, R. Comparison of marginal and internal fit of pressed lithium disilicate veneers fabricated via a manual waxing technique versus a 3D printed technique. J. Esthet. Restor. Dent. 2022, 34, 715–720. [Google Scholar] [CrossRef]
- Sakornwimon, N.; Leevailoj, C. Clinical marginal fit of zirconia crowns and patients’ preferences for impression techniques using intraoral digital scanner versus polyvinyl siloxane material. J. Prosthet. Dent. 2017, 118, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, Z.N.; Alkhatatbeh, R.M.; Baba, N.Z.; Goodacre, C.J. A comparison of the marginal and internal fit of porcelain laminate veneers fabricated by pressing and CAD-CAM milling and cemented with 2 different resin cements. J. Prosthet. Dent. 2019, 121, 470–476. [Google Scholar] [CrossRef] [PubMed]
| Finish Line | Material | Occlusal Mean ± SD | Axio-Occlusal Mean ± SD | Axial Mean ± SD | Marginal Mean ± SD | Total Mean ± SD |
|---|---|---|---|---|---|---|
| Chamfer (C) | HTML | 51.117 ± 19.01 | 40.085 ± 13.215 | 23.317 ± 3.306 | 34.426 ± 10.245 | 37.237 ± 15.928 |
| STML | 42.913 ± 6.140 | 30.795 ± 5.516 | 19.750 ± 2.950 | 35.901 ± 8.060 | 32.340 ± 10.290 | |
| ZirCAD | 36.654 ± 6.266 | 28.287 ± 2.433 | 21.311 ± 3.184 | 40.944 ± 6.300 | 31.799 ± 8.988 | |
| Overall (mean) | 43.562 ± 13.131 | 33.056 ± 9.598 | 21.460 ± 3.383 | 37.091 ± 8.551 | 33.792 ± 12.262 | |
| Rounded Shoulder (RS) | HTML | 66.663 ± 14.895 | 55.164 ± 12.050 | 29.179 ± 13.233 | 56.598 ± 10.364 | 51.901 ± 18.616 |
| STML | 53.664 ± 20.243 | 37.166 ± 12.458 | 20.283 ± 4.331 | 54.962 ± 15.504 | 41.519 ± 19.870 | |
| ZirCAD | 43.004 ± 10.589 | 35.036 ± 6.548 | 25.508 ± 2.950 | 43.227 ± 5.370 | 36.694 ± 9.918 | |
| Overall (mean) | 54.444 ± 18.101 | 42.456 ± 13.815 | 24.990 ± 8.755 | 51.596 ± 12.392 | 43.371 ± 17.771 | |
| Overall (C + RS) | HTML | 58.890 ± 18.440 | 47.625 ± 14.538 | 26.249 ± 9.857 | 45.512 ± 15.164 | 44.569 ± 18.729 |
| STML | 48.289 ± 15.569 | 33.980 ± 9.931 | 20.017 ± 3.617 | 45.432 ± 15.500 | 36.929 ± 16.387 | |
| ZirCAD | 39.829 ± 9.073 | 31.662 ± 5.925 | 23.409 ± 3.683 | 42.085 ± 5.816 | 34.246 ± 9.722 | |
| Overall (mean) | 49.003 ± 16.610 | 37.756 ± 12.711 | 23.225 ± 6.817 | 44.343 ± 12.842 | 38.582 ± 15.973 |
| Variable | df | F | p-Value |
|---|---|---|---|
| Model | 23 | 15.510 | <0.001 |
| Model intercept | 1 | 3.355.358 | <0.001 |
| Finish Line Type | 1 | 51.712 | <0.001 |
| Material Type | 2 | 21.554 | <0.001 |
| Measured Region | 3 | 71.062 | <0.001 |
| Finish Line Type ∗ Material Type | 2 | 4.505 | 0.012 |
| Finish Line Type ∗ Measured Region | 3 | 2.939 | 0.034 |
| Material Type ∗ Measured Region | 6 | 4.034 | 0.001 |
| Finish Line Type ∗ Material Type ∗ Region | 6 | 1.117 | 0.354 |
| Group | Group2 | Mean | p-Value |
|---|---|---|---|
| Material Type | HTML | 43.939 ± 18.714 a | <0.001 |
| STML | 37.224 ± 16.489 b | ||
| ZirCAD | 34.246 ± 9.722 bc | ||
| Overall | 38.582 ± 15.973 | ||
| Measured Region | Occlusal | 49.003 ± 16.610 a | <0.001 |
| Axio-occlusal | 37.756 ± 12.711 b | ||
| Axial | 23.225 ± 6.817 c | ||
| Marginal | 44.343 ± 12.842 a | ||
| Overall | 38.582 ± 15.973 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doğan, D.G.; Yaluğ, Ö.S. Marginal and Internal Fit of Zirconia Crowns with Varying Yttria Content and Finish Line Configurations: An In Vitro Study. Appl. Sci. 2025, 15, 12440. https://doi.org/10.3390/app152312440
Doğan DG, Yaluğ ÖS. Marginal and Internal Fit of Zirconia Crowns with Varying Yttria Content and Finish Line Configurations: An In Vitro Study. Applied Sciences. 2025; 15(23):12440. https://doi.org/10.3390/app152312440
Chicago/Turabian StyleDoğan, Dilan Gizem, and Ömer Suat Yaluğ. 2025. "Marginal and Internal Fit of Zirconia Crowns with Varying Yttria Content and Finish Line Configurations: An In Vitro Study" Applied Sciences 15, no. 23: 12440. https://doi.org/10.3390/app152312440
APA StyleDoğan, D. G., & Yaluğ, Ö. S. (2025). Marginal and Internal Fit of Zirconia Crowns with Varying Yttria Content and Finish Line Configurations: An In Vitro Study. Applied Sciences, 15(23), 12440. https://doi.org/10.3390/app152312440






