Abstract
Background: Early interventions in high-risk children seek to improve prognosis, minimize developmental delays, and prevent functional deterioration. The objective of this study was to evaluate the level of agreement between the face-to-face assessment and tele-assessment of neuromotor development in high-risk children between 0 and 18 months of age. Methods: Forty-five children at high risk of developmental delays were included in this study (33% female, mean gestational age of 35.31 ± 4.03 weeks). The patients were included in a face-to-face and a tele-assessment using the Alberta Infant Motor Scale (AIMS) and the level of motor evolution (Niveaux d’Évolution Motrice, NEM) assessments. Results: The analysis showed excellent interrater reliability (ρ ≥ 0.99) for the AIMS. The NEM assessment showed almost perfect reliability (kappa ≥ 0.81) for most items. Seven of them showed substantial reliability (kappa = 0.61–0.80), one moderate reliability (kappa = 0.568), and one fair reliability (kappa = 0.338). Conclusions: This study reveals an excellent/substantial interrater reliability for most of the items assessed. The results are promising to increase the accessibility to a clinical diagnosis and a rehabilitation approach to minimize the development of neuromotor delays in children at high risk.
1. Introduction
Standard care for neonatal and pediatric healthcare includes surveillance and follow-up programs for neurodevelopmental outcomes. High-risk children require these programs to be more structured and specialized [1]. The American Academy of Pediatrics classifies high-risk children into four categories: (i) the preterm infant (born < 37 weeks’ gestation); (ii) the infant with special healthcare needs or dependence on technology; (iii) the infant at risk due to social issues; and (iv) the infant with anticipated early death [2]. Early detection of neuromotor development disorders in this population involves motor assessment through standardized instruments that aim to measure developmental outcomes, monitor motor evolution and the achievement of new skills, and detect neurodevelopmental concerns [3]. In addition, it allows for referral to diagnostic procedures and ensures early intervention within the time window offered by the neuroplasticity of the infant brain [4,5]. In this sense, early intervention seeks to improve prognosis, minimize developmental delays, and prevent functional deterioration [6,7].
People living in underserved areas lacking health infrastructure have difficulties accessing timely specialist care, which is relevant in pediatric care. These limitations range from geographical to economic issues, as well as organizational and cultural factors that can impact the use of telehealth services [8,9]. In addition, the recent COVID-19 pandemic became a major barrier to face-to-face attendance in health services due to the high risk of disease transmission. Restrictive measures, including the lockdown and limitations in face-to-face services, made it necessary to implement new strategies to maintain the quality of healthcare delivery while avoiding the aforementioned risk [10,11]. Kruizinga et al. [12] found that the lockdown caused a significant decrease in pediatric services’ utilization and hospitalization. The study conducted by Vidal-Alaball et al. [13] affirms that telemedicine in this context was useful to provide support to healthcare systems, being the doctors’ first line of defense to slow down the spread of the coronavirus. Additionally, Fuster-Casanovas et al. [14] assessed Spanish citizens’ satisfaction with an online medical consultation service, for which the findings pointed out a plausible paradigm shift concerning a mixed and complementary care service in healthcare.
Telerehabilitation refers to the telematic delivery of rehabilitation services, including assessments, diagnosis, and treatment. It utilizes telecommunication technologies either synchronously, such as real-time videoconferencing, or asynchronously, through recorded videos, images, or other forms of data sharing [15,16]. Several health professionals made an unexpected and rapid transition to telematic services to ensure the continuity of care, including those from pediatric rehabilitation, physiotherapy, and early intervention areas [10,15]. Telerehabilitation allows healthcare professionals to implement assessments and personalized therapeutic approaches tailored to the infant’s developmental needs [10,15]. In addition, it also ensures accessibility, particularly for families in remote or underserved areas, while allowing therapists to monitor progress and adjust treatment plans in real time. Telerehabilitation not only supports early and continuous intervention but also empowers caregivers to take an active role in their child’s developmental progress [10]. Through real-time interactions, therapists can monitor progress, provide feedback, and adjust treatment plans as needed.
An assessment of neuromotor development at an early age is key to identifying and intervening in time on a disorder that might compromise a person’s development throughout their life span. Practitioners within primary healthcare environments assume a critical function in the preliminary identification of neuromotor conditions, for which different assessment tools are available, typically selected based on customary practice and pragmatic considerations, rather than on the foundation of empirical knowledge concerning the precision and efficacy of the tests and their theoretical underpinnings [17]. Certain assessment tools are designed to emphasize a neurological evaluation from a holistic standpoint [18,19], while others are rooted in methodologies that employ standardized scoring systems [20], the observation of developmental milestones and particular facets of motor behavior [21,22], or the qualitative assessment of motor function [23,24].
A previous systematic review has shown positive results in the use of telerehabilitation approaches when face-to-face care is limited in pediatric care due to geographic or health-related situations [16]. To our knowledge, no previous study has evaluated the comparability between face-to-face and neuromotor development tele-assessment in high-risk children. Therefore, the objective of this study was to evaluate the level of agreement between the face-to-face assessment and tele-assessment of neuromotor development in a sample of high-risk children between 0 and 18 months of age. We hypothesized that the neurodevelopmental assessment based on the Alberta Infant Motor Scale (AIMS) and the levels of motor evolution (Niveaux d’Évolution Motrice, NEM) scores would not differ between telerehabilitation and face-to-face methods.
2. Materials and Methods
2.1. Study Design
A descriptive design was used to test interrater reliability. The parents provided voluntary written informed consent before the enrollment of their infants in this study. All the procedures and protocols followed were reviewed and approved by the Biomedical Research Ethics Committee of Granada (Granada, Spain), and this study was conducted in accordance with the Declaration of Helsinki 2013.
2.2. Participants
Participants were recruited from the Neuropediatric and Neurodevelopmental Physical Therapy Service at San Cecilio University Hospital in Granada, Spain. The inclusion criteria were as follows: (1) Children with a chronological age (time since birth) or corrected age of 0–18 months. The corrected age was considered as chronological age in months minus the number of months the infant was born preterm. (2) Children at high risk of neurodevelopmental delays according to the American Academy of Pediatrics criteria [2]. (3) Children whose family had at least minimal experience with smartphone-based videoconferences and Internet connectivity. The exclusion criteria included the following: independent walking as the preferred way of moving, health complications that impeded the child’s participation in the study, and non-Spanish-speaking parents.
2.3. Procedure
Before conducting the assessment, clinical data such as gestational age, chronological age or corrected age, gender, and perinatal antecedents, including the presence of prematurity, multiple gestations, intrauterine growth restriction, plagiocephaly, muscle tone alterations, congenital muscular torticollis, and perinatal asphyxia/mild hypoxic–ischemic encephalopathy, were recorded.
The participants underwent two assessments in two appointments: a traditional face-to-face and a real-time tele-assessment. Children were assessed face-to-face at the hospital service and at home through the tele-assessment. The assessments were conducted by two physical therapists, ABF and AIRL, each with more than 10 years of experience in the pediatric population. One therapist always conducted the face-to-face evaluation and the other the tele-assessment, and each was blinded to the assessments of the other. The two assessments were performed in the same week, and the order was randomized using a random sequence generator to counterbalance any testing-order effects.
During the face-to-face assessment, the therapist observed the children’s spontaneous movement, positioned them at the starting position, and encouraged the children to move as the evaluation required. The tele-assessment involved the participation of the caregiver, who received the following instructions: (1) to place the child on a flat surface that allows freedom of movement, (2) to use the front-facing camera with the smartphone situated in a place guaranteeing wide vision of the child when assistance was required, and (3) to encourage the child to move as much as needed and position him or her as instructed by the therapist.
2.4. Outcome Measures
The outcome measures used to assess neuromotor development were selected because they are frequently used in clinical practice, adaptable to online assessment, and easy to administer. These outcomes included motor acquisitions related to gross motor development, assessed using the AIMS and the NEM assessment. The assessors have specific training and wide experience in their use in clinical practice.
The AIMS is an observational assessment scale that evaluates children’s motor development and identifies gross motor delays in infants from birth to 18 months or until they achieve independent walking [21]. The assessment is based on the progressive development and integration of antigravity muscular control [25,26]. The AIMS includes 58 observational items organized into four subscales: 21 positions are evaluated for the prone scale; for the supine scale, 9 positions are evaluated; for the sitting scale, 12 positions are evaluated; and, for the standing scale, 16 positions are evaluated. Each item is scored as observed or not observed, assessing three qualitative components of spontaneous motor performance: weight-bearing, posture, and antigravity movement. A motor development window is established by identifying the lowest and highest observed items. The total score is determined by summing the observed items in the four positions and all items below this motor development window. This total score can be converted into a percentile rank (PR) when analyzed based on the chronological or corrected age [21,26]. This scale has been translated into Spanish, showing excellent validity and reliability [26]. In addition, it has also shown high interrater reliability when assessments are conducted remotely in prone (r = 0.976), supine (r = 0.965), sitting (r = 0.987), standing (r = 0.945), and total score (r = 0.980) [27].
The assessment of the NEM based on Le Metayer’s concept [24,28] is used to identify motor delays in high-risk children and to prevent functional and motor consequences. An NEM is defined as motor sequences acquired through the conjunction of central nervous system maturation, innate perceptive-motor skills, and repeated experiences that allow for the adjustment of intentional movement achieved by the child throughout their development. The main abilities to be acquired by the children involve postural skills, the antigravity function, and the locomotion function, including motor skills such as crawling or turning over. These motor sequences evolve from axis organization in the supine position or eye–hand–mouth coordination to gross motor skills such as rolling, sitting, or standing under different circumstances. The children progress through each level, moving from one to the next, until they develop standing and walking capabilities [29]. The NEM described includes the assessment of the following items: supine position (axis and upper extremities’ organization; eye–hand–mouth and two hands coordination), prone position (axis organization), turns (rolling supine to prone over right side/left side and rolling prone to supine over right side/left side), dragging, sitting (sitting control, sitting with/without support and sitting to prone over right side/left side, sitting to side sitting over right side/left side, right side sitting to sitting/left side sitting to sitting, right side sitting to crawling/left side sitting to crawling), crawling (crawling position to right side sitting/left side sitting, maintenance of 4-point position/swinging in 4-point position with the weight on hands and knees, crawling), 4 points for sitting on heels, passage to the standing position (sitting on heels to kneeling with hand support, high kneeling to half kneeling over right side/left side, half kneeling on right knee/half kneeling on left knee to standing, standing to half kneeling on right/left knee, half kneeling on right/left knee to high kneeling), standing (with support of both hands/one-handed support and standing without support), and walking (with support on two hands/one hand, pushing a toy car and independent walking on regular ground/irregular ground). Each NEM was scored on a 4-point scale ranging from 1 (normality) to 4 (severe difficulty).
2.5. Data Analysis
The statistical analyses were performed using Statistical Packages for the Social Sciences (SPSS, v. 23.0) software (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used for data analysis. The values were expressed as mean ± standard deviation or frequency and percentages. We analyzed the agreement between the face-to-face assessment and tele-assessment for the AIMS and its subscales by applying the two-way random-effects intraclass correlation coefficient (ICC) (ρ). Confidence intervals were calculated for the interrater reliability trials. A value of ρ < 0.5 was considered poor reliability; 0.5 to 0.75, moderate reliability; 0.75–0.9, good reliability, and >0.90, excellent reliability [30]. Agreement between the face-to-face assessment and tele-assessment for the AIMS total score was also analyzed using the Bland–Altman limits of agreement.
Values of kappa were calculated to analyze the categorical data from the NEM assessment. A value of Kappa of 0 was considered poor reliability; 0.01 to 0.20, slight reliability; 0.21 to 0.40, fair reliability; 0.41 to 0.60 moderate reliability; 0.61 to 0.80, substantial reliability; and 0.81 or higher, almost perfect reliability [31].
A minimum sample size of 44 patients was required to detect an expected mean difference between methods of 0.29 (based on a previous exploratory assessment) in the total score of the AIMS. Considering a drop-out of 15%, a sample size of 50 participants was estimated.
3. Results
Of the 50 patients assessed for eligibility, a total of 45 patients were included. The other five patients did not complete the evaluations within the same week, so they were excluded from the analysis. The descriptive data of the participants are presented in Table 1. The mean gestational age of the participants was 35.31 ± 4.03 weeks, and 33.33% were female. The most prevalent perinatal antecedents included prematurity (22%) and plagiocephaly (31%).

Table 1.
Descriptive characteristics of participants.
Table 2 displays the data from the face-to-face assessment and tele-assessment for the AIMS.

Table 2.
Descriptive values and interrater reliability of telerehabilitation and face-to-face clinical assessment of the Alberta Infant Motor Scale (AIMS).
As seen in Table 2, the data indicate excellent interrater reliability (ρ > 0.965) with narrow confidence intervals. The highest interrater reliability was for the total score of the AIMS (ρ = 0.996), and the lowest was for the supine subscale (ρ = 0.965).
The Bland–Altman plot for the AIMS total scores is shown in Figure 1. The mean and standard deviation values in the face-to-face assessment were 23.89 ± 10.59 and 24.07 ± 11.02 in the tele-assessment. The limits of agreement were −2.66 and 2.39. Excellent interrater reliability was found (ρ = 0.996, 95% confidence interval 0.994, 0.998).
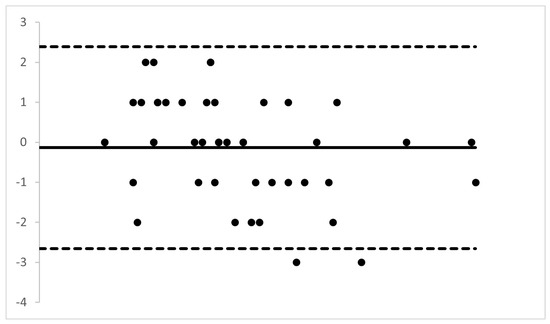
Figure 1.
Bland–Altman plot of the difference between the face-to-face assessment and tele-assessment for Alberta Infant Motor scale total score.
The Y-axis shows the difference between the two paired measurements and the X-axis represents the average of these measures. The solid line indicates the mean difference between the face-to-face assessment and tele-assessment. The dashed lines mark the limits of agreement.
The mean differences between the face-to-face assessment and tele-assessment for the main NEM scores and kappa coefficient values are included in Table 3. A detailed table is included as a Supplementary Table S1. The lowest Kappa coefficients were for the items related to axis organization in supine (Kappa = 0.338), followed by coordination between two hands with moderate reliability (Kappa coefficient data 0.568). Kappa coefficients ranging from 0.631 to 0.789 show substantial reliability for the following items: axis organization in prone position, eye–hand–mouth coordination, rolling supine to prone and prone to supine positions, control in sitting position, skills for transitions from sitting to crawling position, and independent walking on regular ground. Finally, the highest values of Kappa coefficients (Kappa 0.817–1) were obtained for the assessment of upper extremities’ organization, sitting position, skills for transitions from sitting to a prone position, dragging, skills for transition from sitting to side sitting and back, side sitting to crawling position and back, keep crawling position and swinging, crawling, sitting on heels to kneeling and back, kneeling to half kneeling to standing and back, standing with and without support, walking with and without support, walking pushing a toy car, and independent walking on irregular ground.

Table 3.
Descriptive values and interrater reliability of telerehabilitation and face-to-face clinical assessment of the levels of motor evolution (Niveaux d’Évolution Motrice, NEM).
4. Discussion
The objective of this study was to evaluate the level of agreement between the face-to-face assessment and tele-assessment of neuromotor development in a sample of infants between 0 and 18 months of age. Our results show excellent reliability when comparing the tele-assessment and face-to-face evaluation for both the total and subscales of the AIMS. Additionally, there is substantial to almost perfect reliability for most of the items of the NEM assessed. The lowest correlation in the NEM evaluation was observed in the axis organization in the supine position (Kappa = 0.338). This may be attributed to difficulties in perceiving the axis organization through telematics. Additionally, the fair correlation found in the coordination between the two hands item (Kappa = 0.568) could be influenced by factors related to the telerehabilitation method such as a lack of the child’s cooperation, disinterest in the activity or the toy offered, irritability, or environmental distractions.
Several studies support our findings regarding the validity of telematic assessment for gross motor skills’ evaluation in children. The review conducted by Noutsios et al. [32] explored a telemedicine-based examination of the lower limbs and back for children aged 3 to 18 years as a foundation for structured telematics pediatric musculoskeletal examination. Also, they found this assessment to increase providers’ confidence in telemedicine practice. Additionally, previous studies agree with our results about the validity of the telematic assessment on gross motor skills in minor infants with specific objectives and age ranges. Specifically, Boonzaaijer et al. [33,34] and Spittle et al. [35] used the AIMS and the General Movement Assessment. These studies also include the collaboration of caregivers to capture the child’s movement to be evaluated by a professional. The difference lies in the timing of the professional intervention because their assessments were asynchronous. The parents made a video of the child’s movement following some instructions and then uploaded the video to be analyzed later. In our study, the assessment allowed us to guide parents through the assessment.
The tools selected to evaluate motor development are designed to be used in early developmental stages. The AIMS is a well-validated scale previously used for telemonitoring [21,27]. The NEM focuses on sequential stages of motor evolution. It emphasizes a developmental framework, tracing milestones like postural control, locomotion, and manipulation, particularly suited for identifying delays in motor milestones [28,29]. Other scales, such as the Gross Motor Function Measure, focus on functional abilities rather than sequential milestones and are tailored toward children with cerebral palsy and other motor impairments [17]. The Bayley Scale of Infant Development assesses broader developmental domains (cognitive, language, motor) rather than focusing solely on motor evolution and can be used for a broader age range but requires more time and detailed observations [20].
Along the same line, some studies contribute to showing the potential for telerehabilitation services in the pediatric population as a feasible practice. In this sense, the studies of Nicola et al. [36], Gavazzi et al. [37], and Read et al. [38] support the reliability of synchronic tele-assessments of the gross motor function in pediatrics. Nicola et al. [36] aimed to investigate the feasibility and validity of the telematic use of the Movement Assessment Battery for Children—2nd Edition. This study included five 11-year-old children who performed one face-to-face and one telerehabilitation-mediated assessment using an iPad application. During the telematic evaluations, a non-expert adult helped the therapist when needed just as we received help from the children’s caregivers. Gavazzi et al. [37] included in their study mostly children with leukodystrophy to assess the reliability of the telematic Gross Motor Function Measure-88 compared to in-person assessments. They were also helped by the parents when needed with the telematic assessment. Read et al. [38] assessed the feasibility of the remote use of a short neurodevelopmental assessment tool, the Brief Developmental Assessment (BDA), via Zoom. This tool includes a domain for gross and fine motor skills. They assessed children younger than 5 years with congenital heart disease and concluded with the acceptability of the remote use of the BDA for the developmental screening of children with congenital heart disease.
Our study has implications for clinical practice and the development of telematic assessments and telematic surveillance of infants at high risk of developmental delays or motor impairment. Early intervention is key to addressing developmental challenges during critical periods of neuroplasticity when the nervous system exhibits more adaptability. Telerehabilitation allows healthcare professionals to implement targeted strategies to identify and address neuromotor delays at an early stage, preventing their progression. This approach may not only result in improved developmental outcomes but also alleviate the long-term burden on families and healthcare systems by reducing the need for interventions later in life. High interrater reliability in telerehabilitation of motor development delay ensures that children receive accurate and consistent care. In the long term, this reliability supports enhanced diagnostic precision, leading to more reliable diagnoses and interventions. Reliable assessments can be adapted in diverse settings, including low-resource areas, promoting equity in care delivery. Also, it contributes to the evidence of using this kind of telematic assessment for patients who may need it, either for the large distance between them and medical services, health matters, the COVID-19 pandemic situation, or convenience.
The implementation of telerehabilitation in the care of high-risk children in underserved or remote areas offers significant cost savings by reducing travel time and increasing accessibility to pediatric subspecialty care. Moreover, it has the potential to address disparities in access and improve the quality of care in these regions [39]. However, its adoption is not without challenges. Some of the key challenges previously reported include the overutilization or misuse of services, the exacerbation of existing care disparities, and concerns about patient data security. A requirement for telerehabilitation is access to high-speed Internet, which may not be available in certain rural areas. Additionally, the use of end-to-end encryption is essential to prevent patient data from being exposed to unauthorized access [40,41]. To address these issues, investments from governments and the private sector are necessary to expand broadband infrastructure. Furthermore, regulatory policies must be developed to ensure the security of telehealth applications and platforms.
Integrating this approach into clinical practice enables effective collaboration between caregivers and clinicians, creating a supportive framework for children’s development. In addition, the assessment proposed in our study may be easily applied given the absence of specialized or costly software or materials. This increased accessibility ensures that high-risk children receive timely support, reducing the risk of long-term motor development delays. Thus, the development of telerehabilitation for the pediatric population improves individual outcomes and contributes to broader public health goals of equity and inclusion in pediatric healthcare. In this sense, future studies need to evaluate the use of telerehabilitation to develop intervention programs in high-risk children and their effects on preventing motor delays and complications.
Limitations
The limitations in this study include that the participants were recruited from the same hospital. This fact may affect the external validity of the results given that they may not reflect broader demographic, socioeconomic, or cultural diversity, limiting the applicability to other settings. Future studies should include multi-site designs. Only Spanish-speaking families were included in this study. This may have introduced selection bias by excluding families who speak other languages and affected the generalizability of the findings. In our study, there were no patients excluded from this criterion. However, future studies should include participants from diverse linguistic and cultural backgrounds. In addition, the quality of the Internet connection at home was not the same in the different assessments. Although the participants included were familiar with an Internet connection, in some cases, some difficulty following the children required moving the camera to see the information needed for scoring. Given that the assessment was performed according to the AIMS and NEM, the results obtained cannot apply to other scales that evaluate the acquisition of motor milestones in children. Additionally, although it is frequently used in clinical practice, the lack of information regarding predictive validity and interrater reliability from previous studies of the NEM assessment is a limitation that may increase the risk of bias and limit the generalizability of the results to broader populations or contexts.
5. Conclusions
This study demonstrates high interrater reliability for neuromotor development tele-assessments in children at a high risk of developmental delays applying the AIMS and NEM assessments. The clinical application of these findings is of interest and will allow for increased accessibility to an early intervention to minimize the development of neuromotor delays in high-risk children.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15020723/s1, Table S1: Detailed information of the descriptive values and interrater reliability of telerehabilitation and face-to-face clinical assessment of the main levels of motor evolution (Niveaux d’Évolution Motrice, NEM).
Author Contributions
Conceptualization, M.C.V. and Á.B.-F.; methodology, A.I.R.-L. and Á.B.-F.; software, J.R.-B.; validation, G.V.-P., L.L.-L. and I.C.-M.; formal analysis, M.C.V. and A.I.R.-L.; investigation, A.I.R.-L. and Á.B.-F.; resources, L.L.-L., J.R.-B. and I.C.-M.; data curation, Á.B.-F.; writing—original draft preparation, A.I.R.-L., Á.B.-F. and M.C.V.; writing—review and editing, I.C.-M.; visualization, G.V.-P.; supervision, J.R.-B. and L.L.-L.; project administration, Á.B.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Andalusian Ethics Committee (date of approval 31 March 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to ethical reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Doyle, L.W.; Anderson, P.J.; Battin, M.; Bowen, J.R.; Brown, N.; Callanan, C.; Campbell, C.; Chandler, S.; Cheong, J.; Darlow, B.; et al. Long-term follow-up of high-risk children: Who, why, and how? BMC Pediatr. 2014, 14, 279. [Google Scholar] [CrossRef] [PubMed]
- Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate: Proposed guidelines. Pediatrics 1998, 102, 411–417. [Google Scholar] [CrossRef]
- Kepenek-Varol, B.; Hoşbay, Z.; Varol, S.; Torun, E. Assessment of motor development using the Alberta Infant Motor Scale in full-term infants. Turk. J. Pediatr. 2020, 62, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Hadders-Algra, M. Early Diagnostics and Early Intervention in Neurodevelopmental Disorders-Age-Dependent Challenges and Opportunities. J. Clin. Med. 2021, 10, 861. [Google Scholar] [CrossRef] [PubMed]
- Danks, M.; Flynn, E.J.; Gray, P.H.; Hurrion, E.M. “Low-normal” motor skills in infants at high risk for poor developmental outcomes: A prevalence and prognostic study. Dev. Med. Child Neurol. 2022, 64, 1517–1523. [Google Scholar] [CrossRef]
- McNamara, L.; Morgan, C.; Novak, I. Interventions for Motor Disorders in High-Risk Neonates. Clin. Perinatol. 2023, 50, 121–155. [Google Scholar] [CrossRef]
- Hutchon, B.; Gibbs, D.; Harniess, P.; Jary, S.; Crossley, S.; Moffat, J.V.; Basu, N.; Basu, A.P. Early intervention programmes for infants at high risk of atypical neurodevelopmental outcome. Dev. Med. Child Neurol. 2019, 61, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Ferrinho, P.; Van Lerberghe, W. Providing Health Care Under Adverse Conditions: Health Personnel Performance & Individual Coping Strategies; Studies in Health Services Organisation & Policies; ITGPress: Birmingham, UK, 2000. [Google Scholar]
- Chomitz, K.M.; Setiadi, G.; Azwar, A.; Ismail, N.; Widiyarti. What Do Doctors Want? Developing Incentives for Doctors to Serve in Indonesia’s Rural and Remote Areas; Policy Research Working Paper Series 1888; The World Bank: Washington, DC, USA, 1998. [Google Scholar]
- Maitre, N.L.; Benninger, K.L.; Neel, M.L.; Haase, J.A.; Pietruszewski, L.; Levengood, K.; Adderley, K.M.; Batterson, N.O.; Hague, K.M.; Lightfoot, M.M.-B.; et al. Standardized Neurodevelopmental Surveillance of High-risk Infants Using Telehealth: Implementation Study during COVID-19. Pediatr. Qual. Saf. 2021, 6, e439. [Google Scholar] [CrossRef]
- Pujolar, G.; Oliver-Anglès, A.; Vargas, I.; Vázquez, M.L. Changes in access to health services during the COVID-19 pandemic: A scoping review. Int. J. Environ. Res. Public Health 2022, 19, 1749. [Google Scholar] [CrossRef]
- Kruizinga, M.D.; Peeters, D.; van Veen, M.; van Houten, M.; Wieringa, J.; Noordzij, J.G.; Bekhof, J.; Tramper-Stranders, G.; Vet, N.J.; Driessen, G.J.A. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: A multicenter analysis and review of the literature. Eur. J. Pediatr. 2021, 180, 2271–2279. [Google Scholar] [CrossRef]
- Vidal-Alaball, J.; Acosta-Roja, R.; Hernández, N.P.; Luque, U.S.; Morrison, D.; Pérez, S.N.; Perez-Llano, J.; Vèrges, A.S.; Seguí, F.L. Telemedicine in the face of the COVID-19 pandemic. Aten. Primaria 2020, 52, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Fuster Casanovas, A.; Vidal Alaball, J.; El Iysaouy, M.; López Seguí, F.; Alzaga Reig, X.; Solans, O. Análisis descriptivo de una encuesta on-line a los usuarios del Servicio de teleconsulta de Cataluña: La COVID-19, ¿cambio de paradigma de los ciudadanos sobre la atención médica? Med. Gen. Fam. 2022, 11, 99–105. [Google Scholar] [CrossRef]
- Kaur, M.; Eddy, E.Z.; Tiwari, D. Exploring Practice Patterns of Pediatric Telerehabilitation During COVID-19: A Survey Study. Telemed. J. e-Health 2022, 28, 1505–1516. [Google Scholar] [CrossRef] [PubMed]
- Ogourtsova, T.; Boychuck, Z.; O’Donnell, M.; Ahmed, S.; Osman, G.; Majnemer, A. Telerehabilitation for children and youth with developmental disabilities and their families: A systematic review. Phys. Occup. Ther. Pediatr. 2023, 43, 129–175. [Google Scholar] [CrossRef] [PubMed]
- Ketelaar, M.; Vermeer, A.; Helders, P.J. Functional motor abilities of children with cerebral palsy: A systematic literature review of assessment measures. Clin. Rehabil. 1998, 12, 369–380. [Google Scholar] [CrossRef]
- Haataja, L.; Mercuri, E.; Regev, R.; Cowan, F.; Rutherford, M.; Dubowitz, V.; Dubowitz, L. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J. Pediatr. 1999, 135, 153–161. [Google Scholar] [CrossRef]
- Amiel-Tison, C. Update of the Amiel-Tison neurologic assessment for the term neonate or at 40 weeks corrected age. Pediatr. Neurol. 2002, 27, 196–212. [Google Scholar] [CrossRef] [PubMed]
- Michalec, D. Bayley Scales of Infant Development, 3rd ed.; Goldstein, S., Naglieri, J.A., Eds.; Encyclopedia of Child Behavior and Development; Springer: Boston, MA, USA, 2011. [Google Scholar] [CrossRef]
- Piper, M.C.; Pinnell, L.E.; Darrah, J.; Maguire, T.; Byrne, P.J. Construction and validation of the Alberta Infant Motor Scale (AIMS). Can. J. Public Health 1992, 83 (Suppl. S2), S46–S50. [Google Scholar] [PubMed]
- Persson, K.; Strömberg, B. Structured observation of motor performance (SOMP-I) applied to preterm and full term infants who needed neonatal intensive care. A cross-sectional analysis of progress and quality of motor performance at ages 0–10 months. Early Hum. Dev. 1995, 43, 205–224. [Google Scholar] [CrossRef] [PubMed]
- Hadders-Algra, M. General movements: A window for early identification of children at high risk for developmental disorders. J. Pediatr. 2004, 145 (Suppl. S2), S12–S18. [Google Scholar] [CrossRef] [PubMed]
- Perrin, L.; Le Métayer, M.; François, A.; Vanhulle, C.; Marret, S.; Jouve, A.; Clavel, C.; Picciolini, O.; Cozzaglio, M.; Macchi, M.; et al. Évaluation Du Potentiel Neuromoteur Du Nourrisson: Étude Multicentrique Internationale Comparative Longitudinale De Deux Méthodes Cliniques D’Examen. Mot. Cerebrale 2014, 35, 129–138. [Google Scholar] [CrossRef]
- Tupsila, R.; Bennett, S.; Mato, L.; Keeratisiroj, O.; Siritaratiwat, W. Gross motor development of Thai healthy full-term infants aged from birth to 14 months using the Alberta Infant Motor Scale: Inter individual variability. Early Hum. Dev. 2020, 151, 105169. [Google Scholar] [CrossRef] [PubMed]
- Morales-Monforte, E.; Bagur-Calafat, C.; Suc-Lerin, N.; Fornaguera-Martí, M.; Cazorla-Sánchez, E.; Girabent-Farrés, M. The Spanish version of the Alberta Infant Motor Scale: Validity and reliability analysis. Dev. Neurorehabil. 2017, 20, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.R.G.; Verdério, B.N.; de Abreu, R.W.F.; Brugnaro, B.H.; dos Santos, A.N.; dos Santos, M.M.; Rocha, N.A.C.F. Telemonitoring of motor skills using the Alberta Infant Motor Scale for at-risk infants in the first year of life. J. Telemed. Telecare 2022, 6, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Le Metayer, M. Balance cerebro motor del niño pequeño—Balanç cervell motor del nen petit. Desenvol. Infant. Atenció Precoç 2011, 32, 5. [Google Scholar]
- Le Métayer, M. Reeducación Cerebromotriz del Niño Pequeño: Educación Terapéutica; Masson: Paris, France, 1994. [Google Scholar]
- Koo, T.K.; Li, M.Y. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Noutsios, C.D.; Boisvert-Plante, V.; Laberge, E.; Perez, J.; Ingelmo, P. The telemedicine-based pediatric examination of the back and lower limbs: A narrative review. J. Pain Res. 2021, 14, 2959–2979. [Google Scholar] [CrossRef]
- Boonzaaijer, M.; Van Dam, E.; Van Haastert, I.C.; Nuysink, J. Concurrent Validity Between Live and Home Video Observations Using the Alberta Infant Motor Scale. Pediatr. Phys. Ther. 2017, 29, 146–151. [Google Scholar] [CrossRef]
- Boonzaaijer, M.; Van Wesel, F.; Nuysink, J.; Volman, M.J.M.; Jongmans, M.J. A home-video method to assess infant gross motor development: Parent perspectives on feasibility. BMC Pediatr. 2019, 19, 392. [Google Scholar] [CrossRef] [PubMed]
- Spittle, A.; Olsen, J.; Kwong, A.; Doyle, L.; Marschik, P.; Einspieler, C.; Cheong, J. The Baby Moves prospective cohort study protocol: Using a smartphone application with the General Movements Assessment to predict neurodevelopmental outcomes at age 2 years for extremely preterm or extremely low birthweight infants. BMJ Open 2016, 6, e013446. [Google Scholar] [CrossRef] [PubMed]
- Nicola, K.; Waugh, J.; Charles, E.; Russell, T. The feasibility and concurrent validity of performing the Movement Assessment Battery for Children—2nd Edition via telerehabilitation technology. Res. Dev. Disabil. 2018, 77, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Gavazzi, F.; Adang, L.; Waldman, A.; Jan, A.K.; Liu, G.; Lorch, S.A.; DeMauro, S.B.; Shults, J.; Pierce, S.R.; Ballance, E.; et al. Reliability of the Telemedicine Application of the Gross Motor Function Measure-88 in Patients With Leukodystrophy. Pediatr. Neurol. 2021, 125, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Read, J.S.; Brown, K.; Wray, J. The Feasibility and Acceptability of Remote Videoconference Use of the Brief Developmental Assessment Tool for Young Children with Congenital Heart Disease. Telemed. J. e-Health 2023, 29, 146–151. [Google Scholar] [CrossRef]
- Marcin, J.P.; Shaikh, U.; Steinhorn, R.H. Addressing health disparities in rural communities using telehealth. Pediatr. Res. 2016, 79, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Mahtta, D.; Daher, M.; Lee, M.T.; Sayani, S.; Shishehbor, M.; Virani, S.S. Promise and perils of telehealth in the current era. Curr. Cardiol. Rep. 2021, 23, 115. [Google Scholar] [CrossRef]
- Ko, J.S.; El-Toukhy, S.; Quintero, S.M.; Wilkerson, M.J.; Nápoles, A.M.; Stewart, A.L.; Strassle, P.D. Disparities in telehealth access, not willingness to use services, likely explain rural telehealth disparities. J. Rural Health 2023, 39, 617–624. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).