Featured Application
This review synthesizes current evidence on artificial intelligence-based dental crown design, outlining prevalent algorithms, dataset characteristics, and performance metrics to inform future development and clinical translation.
Abstract
Artificial intelligence (AI), particularly deep learning, is increasingly applied in dental prosthetics, offering new approaches to dental crown design. This scoping review aimed to summarize current evidence on AI-assisted crown design, focusing on algorithm types, dataset characteristics, and evaluation methods. A comprehensive search of PubMed, Scopus, Web of Science, and IEEE Xplore was conducted in February 2025, covering studies published between January 2010 and February 2025. Ten studies met the inclusion criteria, of which four developed custom AI models—mainly based on generative adversarial networks—while six evaluated commercially available software. All studies used digitized dental models obtained from scanned stone casts or intraoral scans, and dataset sizes varied widely. Morphological accuracy was the most frequently reported outcome, assessed in six studies, followed by design time and occlusal contact evaluation. While most AI-generated crowns demonstrated clinically acceptable precision, only four studies fabricated physical crowns and none conducted in vivo validation. These findings suggest that AI-assisted crown design holds promise for improving anatomical accuracy and workflow efficiency, but methodological heterogeneity and the lack of clinical validation highlight the need for standardized evaluation protocols and further in vivo studies.
1. Introduction
Artificial intelligence (AI), a field of computer science, enables machines to perform tasks that mimic human cognition such as learning, reasoning, and problem-solving. Its growing ability to process large datasets and identify complex patterns has led to widespread adoption across many disciplines [1]. In healthcare, AI plays a key role in enhancing diagnostic accuracy, predicting disease progression, and personalizing treatment planning [2,3].
Dentistry is actively embracing AI across multiple specialties [4]. In dental radiology, it aids in image interpretation and pathology detection [5,6]; in periodontics, it helps forecast disease progression and guide treatment planning [7,8]; and in orthodontics, it supports simulation-based therapy using digital scans [9]. Prosthodontics and implantology have also begun applying AI to design restorations and assist with implant positioning and identification [10,11,12,13]. Recently, several studies have highlighted the growing role of AI in automating fixed dental prosthesis workflows, showing improvements in efficiency and accuracy compared with conventional techniques [14,15]. These advancements collectively contribute to improved clinical workflow and personalized patient care [16].
Among various AI techniques, machine learning (ML) allows computers to learn from data without explicit programming. Deep learning, a subset of ML, employs layered neural networks to automatically extract complex features and has transformed medical imaging and diagnostics [17,18,19,20,21]. Convolutional Neural Networks (CNNs), for instance, excel at tasks like image classification, segmentation, and object detection across radiological applications and electronic health records [22,23]. Generative Adversarial Networks (GANs) are another powerful class capable of realistic image synthesis, data augmentation, and cross-modality translation in diagnostic imaging [24,25]. More recently, transformer-based architectures—renowned from natural language processing—have gained traction in medical image analysis for their ability to capture long-range dependencies and improve tasks such as segmentation and synthesis [26,27].
A particularly promising application of AI lies in the design of dental crowns. Crowns restore function and esthetics to damaged teeth and require high precision to ensure clinical success [28]. AI offers the potential to enhance this process by improving anatomical accuracy and workflow efficiency [29]. Historically, crown fabrication was a manual process involving physical impressions and technician-made wax-ups [30]. The advent of intraoral scanners and Computer-aided design/computer-aided manufacturing (CAD/CAM) technology has since streamlined this workflow into a more standardized digital process [31]. CAD/CAM-fabricated crowns have been shown to offer comparable accuracy to conventional methods with greater efficiency [32,33,34].
Despite these improvements, crown design remains a complex process requiring both anatomical expertise and clinical judgment [35]. While research on AI-assisted crown design has been expanding rapidly [29], there is still a lack of comprehensive reviews that examine the specific algorithms employed and their relevance to clinically important outcomes such as crown morphology, fit, and occlusion.
Therefore, the purpose of this scoping review is to map and synthesize the current evidence on artificial intelligence-assisted dental crown design and to discuss its potential clinical implications.
The central research question guiding this review is:
“How has artificial intelligence been applied to dental crown design, and what is the current evidence regarding its accuracy, efficiency, and potential clinical relevance?”
2. Methodology
2.1. Protocol
The methodological framework of this review is illustrated in Figure 1. The review process followed the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [36]. This study aimed to explore how AI has been applied to the design of full-coverage dental crowns and to assess its reported performance.
Figure 1.
Overview of the scoping review workflow.
To better align with scoping review methodology, we structured our research framework using the PCC (Population, Concept, Context) model [37]:
- Population (P): Studies involving the design of dental crowns in the field of prosthodontics, based on digital datasets such as scanned stone casts or intraoral scans.
- Concept (C): Application of artificial intelligence models or software for dental crown design, including performance evaluation.
- Context (C): Studies conducted in prosthodontic research or clinical laboratory settings, focusing on AI-driven crown design.
2.2. Literature Search
A comprehensive electronic search was conducted in February 2025 across PubMed, Scopus, Web of Science, and IEEE Xplore. Both MeSH terms and free-text keywords were used, combining relevant terms with Boolean operators. The main search strategy included combinations of terms related to dental crowns (“dental crown,” “dental prosthesis,” “dental prosthesis design”) and artificial intelligence (“artificial intelligence,” “machine learning,” “deep learning”). Search expressions were adapted for each database to ensure compatibility and reproducibility. All search results from the four databases were exported into Microsoft Excel (version 2021; Microsoft Corp., Redmond, WA, USA). Duplicate records were identified by comparing titles, authors, and DOIs and were manually removed by the reviewers to ensure accuracy.
The selection process was conducted in three stages. First, all potentially relevant studies were identified using the predefined search string. Second, titles and abstracts were screened to exclude studies unrelated to dental crown design or those not involving AI-based applications. Finally, the full texts of the remaining articles were carefully reviewed to confirm their eligibility based on predefined inclusion and exclusion criteria. The overall process, including the number of studies excluded at each stage, is summarized in the PRISMA-ScR flow diagram (Figure 2).
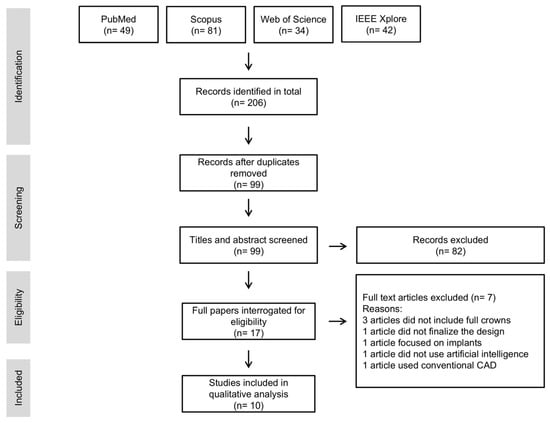
Figure 2.
PRISMA-ScR flow diagram illustrating the study selection process.
2.3. Eligibility Criteria
Inclusion criteria were as follows:
- Peer-reviewed original research articles presenting primary data.
- Studies specifically focused on full-coverage crown restorations.
- Publications available in English, dated between January 2010 and February 2025.
Exclusion criteria included:
- Studies not directly related to dental crown design (e.g., studies on implants).
- Articles lacking objective performance data or outcome measures.
- Studies for which the full text was unavailable.
- Reviews, opinion pieces, and editorial letters.
2.4. Quality Assessment of Included Studies
A quality assessment was conducted to evaluate methodological transparency and clinical applicability. Each study was reviewed for three objective aspects: (1) whether the AI methodology was clearly described, (2) whether physical crowns were fabricated for validation, and (3) whether in vivo validation was performed.
Two independent reviewers (H.J.K. and Y.L.K.) evaluated the titles and abstracts of the identified articles based on predefined inclusion and exclusion criteria. If the information provided in the titles and abstracts was deemed insufficient for determining relevance, a comprehensive review of the full text was conducted. Both reviewers carefully assessed studies that appeared to meet the eligibility criteria and collaboratively selected articles for further analysis. In cases of disagreement, the reviewers revisited the eligibility criteria and discussed the evidence thoroughly until full agreement was achieved, ensuring a transparent and unbiased selection process. Data extracted from the included studies were organized and charted using Microsoft Excel. This software was used to systematically manage study characteristics and evaluation metrics, facilitating a structured qualitative synthesis.
3. Results
3.1. Selection of Sources
Figure 2 presents the article selection process conducted in accordance with the PRISMA-ScR guidelines. The initial electronic search yielded a total of 206 records. After removing duplicates, 99 unique records remained for screening. Following a review of titles and abstracts, 17 articles were selected for full-text evaluation. Of these, 7 were excluded for not fulfilling the predefined inclusion criteria. Ultimately, 10 studies met all eligibility requirements and were included in the qualitative synthesis (Table 1). The two reviewers independently assessed the studies and reached full agreement on final selection and classification.

Table 1.
Summary of included articles on AI applications in dental crown prosthesis.
3.2. Publication Trends by Year
Among the 10 studies included in this review, the earliest was published in 2022, with a notable increase in publications observed in 2023 and 2024. Specifically, three studies were published in 2022, two in 2023, four in 2024, and one in 2025, reflecting a growing interest in the application of AI for dental crown design.
3.3. AI Architecture
Of the 10 studies included in this review, four developed custom artificial intelligence models based on generative adversarial networks (GANs). These studies trained their algorithms using datasets of digitized natural dentition to generate 3D crown morphologies.
The remaining six studies utilized commercially available AI-powered crown design software. These platforms were employed without modification of their underlying algorithms, and specific architectural details were not disclosed in the respective publications.
3.4. Dataset Characteristics
All 10 studies utilized digitized dental models as input data for both training and evaluation. These models were obtained either by scanning stone casts or through direct intraoral scanning.
The size of the datasets varied significantly across studies. Those involving the development of custom AI models employed relatively large training sets, typically ranging from 159 to 700 cases, to facilitate robust learning of dental morphology. In contrast, studies that focused on evaluating commercially available AI software used smaller datasets, generally comprising between 12 and 33 cases, reflecting an emphasis on performance comparison rather than algorithm training.
3.5. Outcome Metrics
Among the included studies, morphological accuracy was the most frequently evaluated aspect. Six studies assessed the similarity between AI-generated crowns and reference models using root-mean-square (RMS) error, which quantifies the average deviation between the two 3D surfaces. RMS values under 100 μm were generally considered clinically acceptable, though thresholds were not consistently defined across studies.
In addition to morphology, several studies also evaluated parameters related to the functional performance of crowns, including occlusal contact points, cusp angles, and tooth axis alignment. These metrics were typically assessed through digital superimposition techniques or virtual articulation simulations to determine biomechanical relevance.
Design time was another commonly reported metric, evaluated in three studies by comparing the duration of AI-assisted crown design with conventional CAD/CAM workflows. Across these studies, AI integration reduced the design process by approximately 30–50%, demonstrating a clear benefit in workflow efficiency.
However, despite the variety of reported metrics, there was no standardized evaluation framework across studies. Differences in definitions, measurement tools, and thresholds limited direct comparisons and highlight the need for unified guidelines to assess the accuracy and clinical performance of AI-generated crowns.
3.6. Quality Assessment of Included Studies
To evaluate the methodological transparency and clinical applicability of the included studies, we assessed whether the AI methodology was clearly described, whether physical crowns were fabricated, and whether in vivo validation was conducted. Table 2 summarizes the findings.

Table 2.
Quality assessment of included studies.
4. Discussion
4.1. Summary of Findings
This scoping review identified and analyzed ten studies focusing on the application of AI in the design of dental crowns. Among them, four studies developed custom AI models based on GANs, while six utilized commercially available AI-powered crown design software. The studies employed a variety of evaluation metrics, with morphological accuracy being the most common. Functional parameters such as occlusal contact and cusp angle, as well as time efficiency, were also evaluated. Overall, AI-assisted crown design showed promising potential for improving productivity and standardization in prosthodontics. However, differences in dataset size, AI architecture, and outcome measures limit the comparability of findings and the generalizability of clinical implications.
4.2. AI Architectures for Crown Design
The studies included in this review employed a range of AI architectures, with GANs being the most prevalent. Chau et al. [38,39], Tian et al. [42], and Ding et al. [45] used customized GAN-based models to replicate crown morphology by learning from digitized casts of natural dentition. Advanced modifications, such as two-stage GANs and 3D deep convolutional GANs, aimed to improve accuracy in surface geometry and occlusal function.
GAN-based algorithms have also been widely adopted in various areas of dentistry, particularly in tasks requiring three-dimensional anatomical reconstruction. Originally introduced by Goodfellow et al. [48], GANs are composed of two competing neural networks—a generator and a discriminator—that iteratively improve each other’s performance through adversarial training. This architecture enables the generation of highly realistic 3D morphological structures, which is especially useful in restorative dentistry.
In addition to crown design, GANs have been used to reconstruct root canal systems, synthesize tooth surfaces, and generate realistic 3D dental arch forms. For instance, Yang et al. [49] developed a 3D GAN model to simulate root canal morphology for endodontic planning. These applications highlight the utility of GANs in producing anatomically precise 3D models essential for diagnosis, planning, and prosthetic design [50].
Some studies also utilized commercially available AI design platforms that integrate GAN and convolutional neural network (CNN) technologies within semi-automated CAD workflows. These tools were often compared with technician-generated or traditional CAD/CAM designs to evaluate usability in real-world clinical settings. However, a notable limitation of such AI-driven design platforms is that their underlying algorithms are often proprietary and not publicly disclosed, which limits transparency and hinders objective performance validation.
4.3. Performance of AI-Designed Crowns
Performance outcomes varied across studies but were generally positive in terms of morphological accuracy and efficiency. Ding et al. [45] reported highly accurate crown surfaces with RMS error within clinically acceptable thresholds. Çakmak et al. [34] and Cho et al. [40] found that AI-generated crowns exhibited comparable occlusal morphology to those designed manually, although minor deviations in anterior guidance and contact points were noted. Internal fit and marginal adaptation were examined using methods such as CBCT and microscopy, and AI designs were close to technician-level outputs but sometimes required post-processing [41,43,46,47].
In terms of time efficiency, Wu et al. [41], Liu et al. [43], and Cho et al. [46] demonstrated that AI design software significantly reduced working time, highlighting one of the key advantages of AI integration. In addition to prosthodontics, AI has demonstrated time-saving benefits in other dental specialties. In orthodontics, AI-based cephalometric analysis has been shown to reduce landmarking time by over 50% compared to manual tracing while maintaining comparable accuracy [51]. Similarly, in implantology, AI-assisted segmentation and planning significantly shortened CBCT analysis time, with some studies reporting reductions of up to 50% [52,53]. These findings support the broader applicability of AI in enhancing clinical efficiency across various dental workflows.
4.4. Dataset Characteristics and Real-World Applications
The datasets used for model training and validation varied significantly across studies in both size and type. Most utilized digitized casts of natural dentition with sizes ranging from as few as 12 cases [44] to over 700 [42]. In studies employing commercially available AI software, dataset sizes were generally smaller, as the algorithms were pre-trained and did not require task-specific model training by the researchers. This limited the ability to evaluate how training data characteristics influenced model performance.
The limited size and scope of existing datasets pose notable challenges to AI generalizability; however, recent dental AI studies trained on large, multi-center datasets—such as over 150,000 implant radiographs—have demonstrated significantly improved diagnostic performance even with low-quality images [54]. This highlights the critical need for multi-institutional dataset development to validate AI tools across diverse clinical conditions.
Notably, only four studies [38,41,43,44] proceeded to fabricate physical crowns based on AI-generated designs to evaluate clinical fit and function. The remaining studies relied solely on digital evaluations, limiting our ability to assess real-world applicability, generalizability, and reproducibility of AI-generated crowns.
4.5. Outcome Metrics: Lack of Standardization
A major challenge in comparing the performance of AI-designed crowns is the heterogeneity of outcome metrics. Studies employed a wide range of parameters, including RMS, intersection-over-union, cusp angle, internal gap, marginal fit, and occlusal contact points. However, inconsistencies in how these metrics were defined and measured make it difficult to directly compare results across studies. Furthermore, none of the included studies evaluated long-term clinical outcomes such as crown durability, patient-reported satisfaction, or functional wear during mastication. All studies were conducted in vitro, without in vivo trials or real-world follow-up, which significantly limits the ability to assess the true clinical effectiveness of AI-designed crowns. To advance this field, future research must incorporate standardized evaluation frameworks that include both quantitative accuracy metrics and qualitative clinical performance indicators.
To improve transparency and replicability, the adoption of AI-specific reporting standards such as CONSORT-AI is recommended; studies have shown that adherence to such guidelines significantly enhances methodological clarity in AI clinical trials [55,56].
4.6. Clinical Relevance and Limitations
While AI systems show potential to streamline crown design and reduce reliance on technician experience, several limitations remain. Compared with traditional CAD/CAM workflows—which are well validated for predictable and accurate outcomes—AI-based tools are still in the early stages of clinical integration. Current evidence suggests that AI can achieve comparable morphological accuracy while significantly reducing design time, indicating its value as a complementary tool rather than a replacement for CAD/CAM.
However, most studies relied on retrospective datasets or in silico evaluations without in vivo validation, limiting the generalizability of their findings. Minor discrepancies in occlusal morphology or incisal paths observed in AI-generated crowns may affect anterior guidance, often necessitating manual adjustment [40]. Additionally, knowledge-based or rule-based systems, such as the one described by Chen et al. [44], demonstrated lower performance compared to technician-driven CAD workflows, emphasizing the need for more advanced data-driven models.
Challenges such as training bias, overfitting, and limited dataset diversity remain critical barriers to broader clinical applicability. Until prospective trials and real-world validations are conducted, AI-assisted crown design should be regarded as a supportive technology that complements, rather than replaces, clinician expertise and traditional CAD/CAM processes.
This scoping review also has several limitations. First, we did not conduct a formal risk of bias assessment or meta-analysis, as our primary goal was to map the existing evidence rather than synthesize quantitative findings. Second, all included studies were conducted in vitro, and none reported long-term clinical outcomes or in vivo validations, which limits the generalizability of our conclusions. Therefore, the findings should be interpreted cautiously, and further in vivo studies are necessary to validate the clinical applicability of AI-assisted dental crown design. Lastly, substantial heterogeneity across AI algorithms, datasets, and outcome metrics among the included studies prevented direct comparison and meta-analytic synthesis. These factors should be considered when interpreting the findings of this review.
4.7. Future Directions
Future research should aim to expand dataset size and diversity, including various tooth types, arch positions, and occlusal schemes. Collaborations between academic institutions, industry partners, and multi-center research groups will be essential to validate AI-assisted crown design systems under real-world conditions. Large-scale clinical trials are particularly important for assessing long-term success, reproducibility, and integration into routine dental workflows. Additionally, the development of explainable AI models can foster clinician trust and enhance understanding of decision-making processes. Finally, establishing regulatory guidelines and standardized performance benchmarks will be critical to safely and effectively incorporating AI into prosthodontic practice.
5. Conclusions
This scoping review highlights the emerging role of artificial intelligence, particularly deep learning models such as GANs, in the design of dental crowns. AI systems demonstrated favorable outcomes in replicating crown morphology and reducing working time compared to traditional methods. However, as the current evidence is derived exclusively from in vitro studies, there is a pressing need for well-designed in vivo trials to confirm the clinical performance and reliability of AI-generated crowns.
To fully realize the clinical potential of AI in prosthodontics, future research must focus on expanding dataset diversity, standardizing evaluation protocols, and validating AI-designed crowns in real-world settings. With continued development and rigorous assessment, AI is poised to become an essential tool in crown prosthesis design that will enhance precision, efficiency, and patient care.
Author Contributions
Conceptualization, H.-J.K.; methodology, H.-J.K. and Y.-L.K.; software, H.-J.K.; validation, H.-J.K. and Y.-L.K.; investigation, H.-J.K. and Y.-L.K.; resources, H.-J.K. and Y.-L.K.; writing—original draft preparation, H.-J.K.; writing—review and editing, H.-J.K.; supervision, Y.-L.K.; funding acquisition, Y.-L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Wonkwang University in 2025.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial intelligence |
| ML | Machine learning |
| CAD/CAM | Computer-aided design/computer-aided manufacturing |
| CAD | Computer-aided design |
| DCGAN | Deep convolutional generative adversarial network |
| DCPR-GAN | Two-stage deep generative adversarial network |
| GAN | Generative adversarial network |
| RMS | Root-mean-square |
| CNN | Convolutional neural network |
References
- Xu, Y.; Liu, X.; Cao, X.; Huang, C.; Liu, E.; Qian, S.; Liu, X.; Wu, Y.; Dong, F.; Qiu, C.W.; et al. Artificial intelligence: A powerful paradigm for scientific research. Innovation 2021, 2, 100179. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Han, K. Methodologic Guide for Evaluating Clinical Performance and Effect of Artificial Intelligence Technology for Medical Diagnosis and Prediction. Radiology 2018, 286, 800–809. [Google Scholar] [CrossRef]
- Wang, C.; Zhu, X.; Hong, J.C.; Zheng, D. Artificial Intelligence in Radiotherapy Treatment Planning: Present and Future. Technol. Cancer Res. Treat. 2019, 18, 1533033819873922. [Google Scholar] [CrossRef]
- Shan, T.; Tay, F.R.; Gu, L. Application of Artificial Intelligence in Dentistry. J. Dent. Res. 2021, 100, 232–244. [Google Scholar] [CrossRef]
- Hung, K.; Montalvao, C.; Tanaka, R.; Kawai, T.; Bornstein, M.M. The use and performance of artificial intelligence applications in dental and maxillofacial radiology: A systematic review. Dentomaxillofac. Radiol. 2020, 49, 20190107. [Google Scholar] [CrossRef]
- Pauwels, R. A brief introduction to concepts and applications of artificial intelligence in dental imaging. Oral Radiol. 2021, 37, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Biancardi, A.M.; Jones, O.; Andrew, D. Artificial Intelligence in Periodontology: A Scoping Review. Dent. J. 2023, 11, 43. [Google Scholar] [CrossRef]
- Revilla-León, M.; Gómez-Polo, M.; Barmak, A.B.; Inam, W.; Kan, J.Y.K.; Kois, J.C.; Akal, O. Artificial intelligence models for diagnosing gingivitis and periodontal disease: A systematic review. J. Prosthet. Dent. 2023, 130, 816–824. [Google Scholar] [CrossRef]
- Kazimierczak, N.; Kazimierczak, W.; Serafin, Z.; Nowicki, P.; Nożewski, J.; Janiszewska-Olszowska, J. AI in Orthodontics: Revolutionizing Diagnostics and Treatment Planning—A Comprehensive Review. J. Clin. Med. 2024, 13, 344. [Google Scholar] [CrossRef]
- Bernauer, S.A.; Zitzmann, N.U.; Joda, T. The Use and Performance of Artificial Intelligence in Prosthodontics: A Systematic Review. Sensors 2021, 21, 6628. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Gallucci, G.O.; Att, W.; Özcan, M.; Krishnamurthy, V.R. Artificial intelligence models for tooth-supported fixed and removable prosthodontics: A systematic review. J. Prosthet. Dent. 2023, 129, 276–292. [Google Scholar] [CrossRef]
- Mohammad-Rahimi, H.; Motamedian, S.R.; Pirayesh, Z.; Haiat, A.; Zahedrozegar, S.; Mahmoudinia, E.; Rohban, M.H.; Krois, J.; Lee, J.H.; Schwendicke, F. Deep learning in periodontology and oral implantology: A scoping review. J. Periodontal Res. 2022, 57, 942–951. [Google Scholar] [CrossRef]
- Kong, H.J.; Yoo, J.Y.; Lee, J.H.; Eom, S.H.; Kim, J.H. Performance evaluation of deep learning models for the classification and identification of dental implants. J. Prosthet. Dent. 2023, 133, 1521–1527. [Google Scholar] [CrossRef]
- Tsoi, J.K.H. ‘New’ AI in prosthodontics—What has changed two years on? Br. Dent. J. 2025, 238, 799. [Google Scholar] [CrossRef]
- Schwendicke, F.; Mohammad Rahimi, H.; Tichy, A. Artificial Intelligence in Prosthodontics. Dent. Clin. N. Am. 2025, 69, 315–326. [Google Scholar] [CrossRef]
- Mahesh Batra, A.; Reche, A. A New Era of Dental Care: Harnessing Artificial Intelligence for Better Diagnosis and Treatment. Cureus 2023, 15, e49319. [Google Scholar] [CrossRef]
- Chen, X.; Wang, X.; Zhang, K.; Fung, K.M.; Thai, T.C.; Moore, K.; Mannel, R.S.; Liu, H.; Zheng, B.; Qiu, Y. Recent advances and clinical applications of deep learning in medical image analysis. Med. Image Anal. 2022, 79, 102444. [Google Scholar] [CrossRef] [PubMed]
- Litjens, G.; Kooi, T.; Bejnordi, B.E.; Setio, A.A.A.; Ciompi, F.; Ghafoorian, M.; van der Laak, J.A.W.M.; van Ginneken, B.; Sánchez, C.I. A survey on deep learning in medical image analysis. Med. Image Anal. 2017, 42, 60–88. [Google Scholar] [CrossRef] [PubMed]
- Krois, J.; Garcia Cantu, A.; Chaurasia, A.; Patil, R.; Chaudhari, P.K.; Gaudin, R.; Gehrung, S.; Schwendicke, F. Generalizability of deep learning models for dental image analysis. Sci. Rep. 2021, 11, 6102. [Google Scholar] [CrossRef]
- Fatima, A.; Shafi, I.; Afzal, H.; Mahmood, K.; Díez, I.T.; Lipari, V.; Ballester, J.B.; Ashraf, I. Deep Learning-Based Multiclass Instance Segmentation for Dental Lesion Detection. Healthcare 2023, 11, 347. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Liu, P.; Chen, Z.; Chen, Q.; Wen, Z.; Xie, Z. Predicting sequenced dental treatment plans from electronic dental records using deep learning. Artif. Intell. Med. 2024, 147, 102734. [Google Scholar] [CrossRef]
- Chen, C.; Mat Isa, N.A.; Liu, X. A review of convolutional neural network based methods for medical image classification. Comput. Biol. Med. 2025, 185, 109507. [Google Scholar] [CrossRef]
- Singh, S.P.; Wang, L.; Gupta, S.; Goli, H.; Padmanabhan, P.; Gulyás, B. 3D Deep Learning on Medical Images: A Review. Sensors 2020, 20, 5097. [Google Scholar] [CrossRef]
- Hussain, J.; Båth, M.; Ivarsson, J. Generative adversarial networks in medical image reconstruction: A systematic literature review. Comput. Biol. Med. 2025, 191, 110094. [Google Scholar] [CrossRef]
- Jeong, J.J.; Tariq, A.; Adejumo, T.; Trivedi, H.; Gichoya, J.W.; Banerjee, I. Systematic Review of Generative Adversarial Networks (GANs) for Medical Image Classification and Segmentation. J. Digit. Imaging 2022, 35, 137–152. [Google Scholar] [CrossRef]
- Azad, R.; Kazerouni, A.; Heidari, M.; Aghdam, E.K.; Molaei, A.; Jia, Y.; Jose, A.; Roy, R.; Merhof, D. Advances in medical image analysis with vision Transformers: A comprehensive review. Med. Image Anal. 2024, 91, 103000. [Google Scholar] [CrossRef] [PubMed]
- Shamshad, F.; Khan, S.; Zamir, S.W.; Khan, M.H.; Hayat, M.; Khan, F.S.; Fu, H. Transformers in medical imaging: A survey. Med. Image Anal 2023, 88, 102802. [Google Scholar] [CrossRef]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef] [PubMed]
- Kong, H.J.; Kim, Y.L. Application of artificial intelligence in dental crown prosthesis: A scoping review. BMC Oral Health 2024, 24, 937. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthet. Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef]
- Shamseddine, L.; Mortada, R.; Rifai, K.; Chidiac, J.J. Marginal and internal fit of pressed ceramic crowns made from conventional and computer-aided design and computer-aided manufacturing wax patterns: An in vitro comparison. J. Prosthet. Dent. 2016, 116, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Suganna, M.; Kausher, H.; Tarek Ahmed, S.; Sultan Alharbi, H.; Faraj Alsubaie, B.; Ds, A.; Haleem, S.; Meer Rownaq Ali, A.B. Contemporary Evidence of CAD-CAM in Dentistry: A Systematic Review. Cureus 2022, 14, e31687. [Google Scholar] [CrossRef]
- Bessadet, M.; Drancourt, N.; El Osta, N. Time efficiency and cost analysis between digital and conventional workflows for the fabrication of fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2025, 133, 71–84. [Google Scholar] [CrossRef]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011, 56 (Suppl. S1), 97–106. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Chau, R.C.W.; Hsung, R.T.; McGrath, C.; Pow, E.H.N.; Lam, W.Y.H. Accuracy of artificial intelligence-designed single-molar dental prostheses: A feasibility study. J. Prosthet. Dent. 2024, 131, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Chau, R.C.W.; Chong, M.; Thu, K.M.; Chu, N.S.P.; Koohi-Moghadam, M.; Hsung, R.T.; McGrath, C.; Lam, W.Y.H. Artificial intelligence-designed single molar dental prostheses: A protocol of prospective experimental study. PLoS ONE 2022, 17, e0268535. [Google Scholar] [CrossRef]
- Çakmak, G.; Cho, J.H.; Choi, J.; Yoon, H.I.; Yilmaz, B.; Schimmel, M. Can deep learning-designed anterior tooth-borne crown fulfill morphologic, aesthetic, and functional criteria in clinical practice? J. Dent. 2024, 150, 105368. [Google Scholar] [CrossRef]
- Wu, Z.; Zhang, C.; Ye, X.; Dai, Y.; Zhao, J.; Zhao, W.; Zheng, Y. Comparison of the Efficacy of Artificial Intelligence-Powered Software in Crown Design: An In Vitro Study. Int. Dent. J. 2025, 75, 127–134. [Google Scholar] [CrossRef]
- Tian, S.; Wang, M.; Dai, N.; Ma, H.; Li, L.; Fiorenza, L.; Sun, Y.; Li, Y. DCPR-GAN: Dental Crown Prosthesis Restoration Using Two-Stage Generative Adversarial Networks. IEEE J. Biomed. Health Inform. 2022, 26, 151–160. [Google Scholar] [CrossRef]
- Liu, C.M.; Lin, W.C.; Lee, S.Y. Evaluation of the efficiency, trueness, and clinical application of novel artificial intelligence design for dental crown prostheses. Dent. Mater. 2024, 40, 19–27. [Google Scholar] [CrossRef]
- Chen, Y.; Lee, J.K.Y.; Kwong, G.; Pow, E.H.N.; Tsoi, J.K.H. Morphology and fracture behavior of lithium disilicate dental crowns designed by human and knowledge-based AI. J. Mech. Behav. Biomed. Mater. 2022, 131, 105256. [Google Scholar] [CrossRef]
- Ding, H.; Cui, Z.; Maghami, E.; Chen, Y.; Matinlinna, J.P.; Pow, E.H.N.; Fok, A.S.L.; Burrow, M.F.; Wang, W.; Tsoi, J.K.H. Morphology and mechanical performance of dental crown designed by 3D-DCGAN. Dent. Mater. 2023, 39, 320–332. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Yi, Y.; Choi, J.; Ahn, J.; Yoon, H.I.; Yilmaz, B. Time efficiency, occlusal morphology, and internal fit of anatomic contour crowns designed by dental software powered by generative adversarial network: A comparative study. J. Dent. 2023, 138, 104739. [Google Scholar] [CrossRef]
- Cho, J.H.; Çakmak, G.; Yi, Y.; Yoon, H.I.; Yilmaz, B.; Schimmel, M. Tooth morphology, internal fit, occlusion and proximal contacts of dental crowns designed by deep learning-based dental software: A comparative study. J. Dent. 2024, 141, 104830. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, I.; Pouget-Abadie, J.; Mirza, M.; Xu, B.; Warde-Farley, D.; Ozair, S.; Courville, A.; Bengio, Y. Generative adversarial nets. Adv. Neural Inf. Process. Syst. 2014, 27, 2672–2680. [Google Scholar]
- Yang, S.; Kim, K.D.; Ariji, E.; Takata, N.; Kise, Y. Evaluating the performance of generative adversarial network-synthesized periapical images in classifying C-shaped root canals. Sci. Rep. 2023, 13, 18038. [Google Scholar] [CrossRef]
- Bobeică, O.; Iorga, D. Artificial neural networks development in prosthodontics—A systematic mapping review. J. Dent. 2024, 151, 105385. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Cho, J.M.; Ryu, S.; Ryu, S.; Chang, E.; Jung, Y.S.; Kim, J.Y. Automatic identification of posteroanterior cephalometric landmarks using a novel deep learning algorithm: A comparative study with human experts. Sci. Rep. 2023, 13, 15506. [Google Scholar] [CrossRef]
- Moufti, M.A.; Trabulsi, N.; Ghousheh, M.; Fattal, T.; Ashira, A.; Danishvar, S. Developing an Artificial Intelligence Solution to Autosegment the Edentulous Mandibular Bone for Implant Planning. Eur. J. Dent. 2023, 17, 1330–1337. [Google Scholar] [CrossRef]
- Ntovas, P.; Marchand, L.; Finkelman, M.; Revilla-León, M.; Att, W. Accuracy of artificial intelligence–based segmentation of the mandibular canal in CBCT. Clin. Oral Implant. Res. 2024, 35, 1163–1171. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, Y.T.; Lee, J.B. Identification of dental implant systems from low-quality and distorted dental radiographs using AI trained on a large multi-center dataset. Sci. Rep. 2024, 14, 12606. [Google Scholar] [CrossRef]
- Schwendicke, F.; Krois, J. Better Reporting of Studies on Artificial Intelligence: CONSORT-AI and Beyond. J. Dent. Res. 2021, 100, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Pattathil, N.; Zhao, J.Z.L.; Sam-Oyerinde, O.; Felfeli, T. Adherence of randomised controlled trials using artificial intelligence in ophthalmology to CONSORT-AI guidelines: A systematic review and critical appraisal. BMJ Health Care Inform. 2023, 30, e100757. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).