Association Between Maxillary Incisor Inclination and Sagittal Condylar Guidance Across Different Skeletal Malocclusions: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Sample
2.3. Procedure
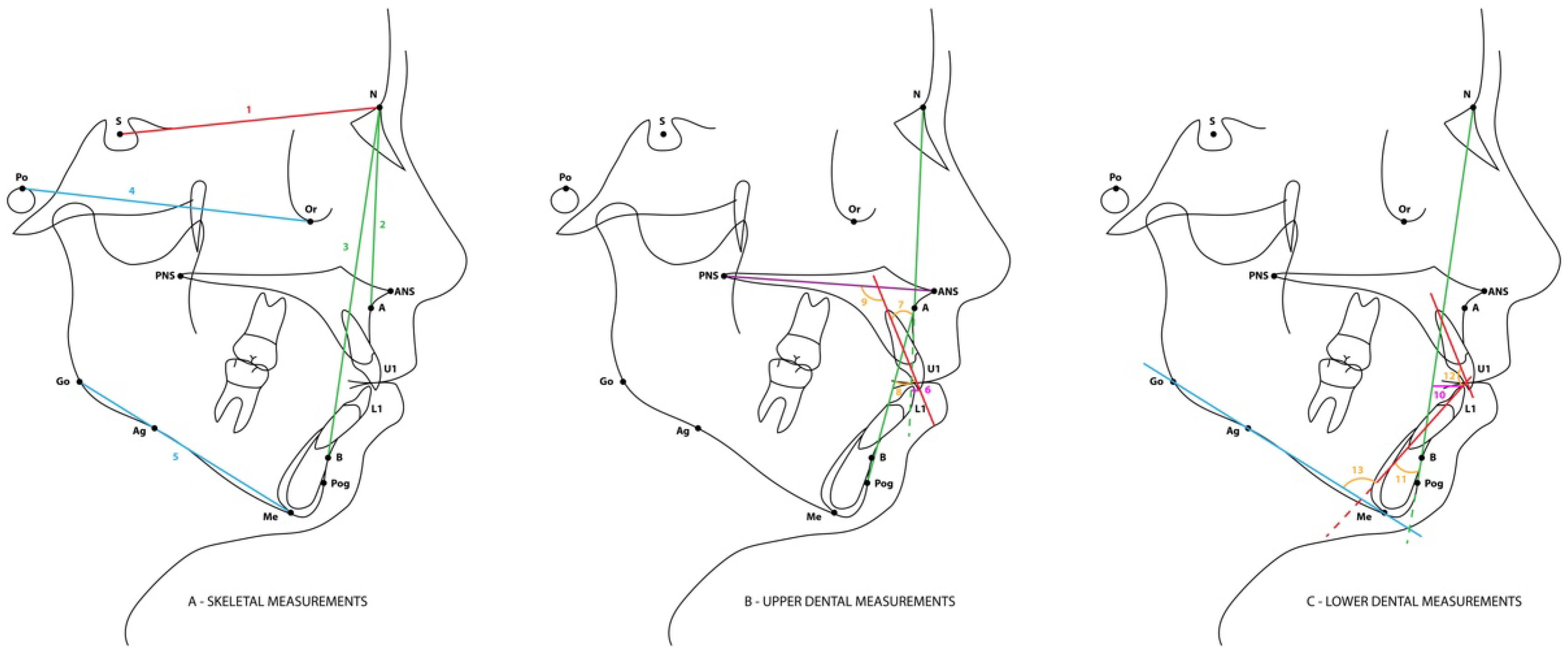
2.4. Data Collection
2.5. Statistical Analysis
3. Results
Descriptive Statistics of the Variables Included in the Study Are Presented in Table 2
| TOTAL (n = 154) Mean (SD) | Class I (n = 54) Mean (SD) | Class II (n = 52) Mean (SD) | Class III (n = 48) Mean (SD) | p (ANOVA) | |
|---|---|---|---|---|---|
| Sagittal condylar guidance right (°) | 49.16 (12.11) | 47.50 a (11.47) | 50.26 a (11.22) | 49.81 (14.79) | 0.013 * |
| Sagittal condylar guidance left (°) | 47.94 (11.81) | 48.63 (9.94) | 47.97 (11.74) | 46.69 (14.89) | 0.335 |
| Overjet (mm) | 2.75 (2.73) | 2.66 a,b (2.41) | 4.28 a,b (1.93) | −0.26 a,b (2.08) | 0.000 *** |
| Overbite (mm) | 2.21 (2.41) | 2.42 a (2.14) | 2.92 b (2.54) | 0.37 a,b (1.54) | 0.000 *** |
| U1–NA (°) | 19.93 (8.32) | 19.33 a (6.37) | 15.90 b (8.17) | 24.96 a,b (7.94) | 0.000 *** |
| U1–APog (°) | 23.72 (7.66) | 24.94 a (6.51) | 26.04 b (8.50) | 19.83 a,b (6.43) | 0.001 ** |
| U1–PP (°) | 109.66 (8.61) | 109.43 (7.25) | 107.08 a (9.75) | 112.73 a (7.86) | 0.001 ** |
| Mandibular plane angle (°) | 24.41 (6.52) | 24.35 (6.72) | 25.25 (6.75) | 23.56 (6.03) | 0.273 |
| Interincisal angle (°) | 132.58 (11.22) | 132.00 (9.70) | 130.52 (13.04) | 135.48 (10.26) | 0.204 |
4. Discussion
TMD and Other Variables
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TMJ | Temporomandibular joint |
| TMD | Temporomandibular dysfunction |
| MJ | Modjaw |
| L | Left |
| R | Right |
| U1 | Maxillary central incisor |
| PP | Palatal plan |
| APog | A point to Pogonion plan |
| FH | Frankfort horizontal |
| NA | Nasion to A Point plan |
References
- Kohaut, J. Anterior guidance-movement and stability. Int. Orthod. 2014, 12, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Broderson, S. Anterior guidance-the key to successful occlusal treatment. J. Prosthet. Dent. 1978, 39, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Maddalone, M.; Losi, F.; Rota, E.; Baldoni, M. Relationship between the Position of the Incisors and the Thickness of the Soft Tissues in the Upper Jaw: Cephalometric Evaluation. Int. J. Clin. Pediatr. Dent. 2019, 12, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Roth, R.H. Functional occlusion for the orthodontist. J. Clin. Orthod. 1981, 15, 32–40, 44–51. [Google Scholar]
- Roth, R.H. Functional occlusion for the Orthodontist—Part III. J. Clin. Orthod. 1981, 15, 174–179, 182–198. [Google Scholar]
- Roth, R.H.; Rolfs, D.A. Functional occlusion for the orthodontist—Part II. J. Clin. Orthod. 1981, 15, 100–123. [Google Scholar]
- Shildkraut, M.; Wood, D.P.; Hunter, W.S. The CR-CO discrepancy and its effect on cephalometric measurements. Angle Orthod. 1994, 64, 333–342. [Google Scholar]
- Abdi, A.H.; Hannam, A.G.; Stavness, I.K.; Fels, S. Minimizing fiducial localization error using sphere-based registration in jaw tracking. J. Biomech. 2018, 68, 120–125. [Google Scholar] [CrossRef]
- Cordray, F.E. Three-dimensional analysis of models articulated in the seated condylar position from a deprogrammed asymptomatic population: A prospective study—Part 1. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 619–630. [Google Scholar] [CrossRef]
- Darendeliler, N.; Dinçer, M.; Soylu, R. The biomechanical relationship between incisor and condylar guidances in deep bite and normal cases. J. Oral Rehabil. 2004, 31, 430–437. [Google Scholar] [CrossRef]
- Bapelle, M.; Dubromez, J.; Savoldelli, C.; Tillier, Y.; Ehrmann, E. Modjaw(R) device: Analysis of mandibular kinematics recorded for a group of asymptomatic subjects. Cranio 2024, 42, 483–489. [Google Scholar] [CrossRef]
- Okeson, J. Management of Temporomandibular Disorders and Occlusion, 7th ed.; Elsevier: St. Louis, MO, USA, 2008. [Google Scholar]
- Isberg, A.M. Temporomandibular Joint Dysfunction; Isis Medical Ltd.: Saint-Martin-Boulogne, France, 2001. [Google Scholar]
- Laird, M.; Ross, C.; O’Higgins, P. Jaw kinematics and mandibular morphology in humans. J. Hum. Evol. 2020, 139, 102639. [Google Scholar] [CrossRef] [PubMed]
- Dawson, P.E. Functional Occlusion from TMJ to Smile Design, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Woodford, S.; Robinson, D.; Mehl, A.; Lee, P.; Ackland, D. Measurement of normal and pathological mandibular and temporomandibular joint kinematics: A systematic review. J. Biomech. 2020, 111, 109994. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, L.; Nowak, Z.; Orthlieb, J.D.; Zoltowska, A. Complicated Relationships between Anterior and Condylar Guidance and Their Clinical Implications-Comparison by Cone Beam Computed Tomography and Electronic Axiography-An Observational Cohort Cross-Sectional Study. Life 2023, 13, 335. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, Ł.; Nowak, Z.; Żółtowska, A. Sagittal condylar guidance angle measurement methods: A systematic review. J. Prosthet. Dent. 2023, 132, 81–92. [Google Scholar] [CrossRef]
- Rosner, D. Hinge axis translation from retruded contact position to intercuspal position in dentulous subjects in treatment. J. Prosthet. Dent. 1982, 48, 713–718. [Google Scholar] [CrossRef]
- Alexander, S.R.; Moore, R.N.; DuBois, L.M. Mandibular condyle position: Comparison of articulator mountings and magnetic resonance imaging. Am. J. Orthod. Dentofac. Orthop. 1993, 104, 230–239. [Google Scholar] [CrossRef]
- Freeland, T. Articulators in Orthodontics. Semin. Orthod. 2012, 18, 51–62. [Google Scholar] [CrossRef]
- Valesan, L.A.-O.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Warzocha, J.; Gadomska-Krasny, J.; Mrowiec, J. Etiologic Factors of Temporomandibular Disorders: A Systematic Review of Literature Containing Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) and Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) from 2018 to 2022. Healthcare 2024, 5, 575. [Google Scholar] [CrossRef]
- Roth, R.H. The maintenance system and occlusal dynamics. Dent. Clin. North Am. 1976, 20, 761–788. [Google Scholar] [CrossRef] [PubMed]
- Zoghby, A.; Ré, J.P.; Perez, C. Functional harmony between the sagittal condylar path inclination and the anterior guidance inclination. J. Stomat. Occ. Med. 2009, 2, 131–136. [Google Scholar] [CrossRef]
- Cordray, F.E. Articulated dental cast analysis of asymptomatic and symptomatic populations. Int. J. Oral Sci. 2016, 8, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Bedrossian, E.A.; Bedrossian, E.; Kois, J.C.; Revilla-Leon, M. Use of an optical jaw-tracking system to record mandibular motion for treatment planning and designing interim and definitive prostheses: A dental technique. J. Prosthet. Dent. 2022, 132, 659–674. [Google Scholar] [CrossRef]
- Palmares, S.; Caseiro, R.; Pereira, R.; Jardim, L. Perception of maxillary incisor inclination and its correlation with dental cephalometric measurements. J. Orthod. 2024, 51, 354–365. [Google Scholar] [CrossRef]
- Nalçaci, R.; Oztürk, F.; Sökücü, O. A comparison of two-dimensional radiography and three-dimensional computed tomography in angular cephalometric measurements. Dentomaxillofac. Radiol. 2010, 2, 100–106. [Google Scholar] [CrossRef]
- Al-Saleh, M.A.; Alsufyani, N.A.; Saltaji, H.; Jaremko, J.L.; Major, P.W. MRI and CBCT image registration of temporomandibular joint: A systematic review. J. Otolaryngol. Head Neck Surg. 2016, 45, 30. [Google Scholar] [CrossRef]
- Revilla-Leon, M.; Zeitler, J.M.; Gomez-Polo, M.; Kois, J.C. Utilizing additively manufactured custom devices to record mandibular motion by using optical jaw tracking systems: A dental technique. J. Prosthet. Dent. 2022, 131, 560–566. [Google Scholar] [CrossRef]
- Revilla-Leon, M.; Zeitler, J.M.; Kois, J.C. Digital maxillomandibular relationship and mandibular motion recording by using an optical jaw tracking system to acquire a dynamic virtual patient. J. Prosthet. Dent. 2024, 132, 14–19. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, G.H.; Moon, D.N.; Kim, J.C.; Park, M.; Lee, K.M. A digital approach to the evaluation of mandibular position by using a virtual articulator. J. Prosthet. Dent. 2021, 125, 849–853. [Google Scholar] [CrossRef]
- Silva, J.; Azevedo, A.; Martins, E.; Canabez, A.; Martin, D.; Martin, C. Mandibular Kinematics on an Orthodontic Population Assessed with an Optical Jaw Tracking System: A Comparative Study. Dent. J. 2025, 13, 184. [Google Scholar] [CrossRef]
- Kubein-Meesenburg, D.; Nägerl, H.; Klamt, B. The biomechanical relation between incisal and condylar guidance in man. J. Biomech. 1988, 21, 997–1009. [Google Scholar] [CrossRef]
- Oancea, L.; Munteanu, I.; Macris, A.; Radulescu, S.; Ciocan, T. A Cone-Beam Computed Tomography Assessment of the Relationship between Incisal and Condylar Guidance. Maedica 2023, 18, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Parakh, M.; Prasad, D.; Hegde, C. A Comparison of Occlusal Schemes with Condylar Inclination and Anterior Guidance in Dentate Individuals. Int. J. Prosthodont. 2024, 37, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.; Egger, M.; Pocock, S.; Gøtzsche, P.; Vandenbroucke, J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Siangloy, T.; Charoemratrote, C. Incisor and Soft Tissue Characteristics of Adult Bimaxillary Protrusion Patients among Different Skeletal Anteroposterior Classifications. Diagnostics 2024, 14, 1031. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Ricketts, R. Foundation for cephalometric communication. Am. J. Orthod. Dentofac. Orthop. 1960, 46, 330–357. [Google Scholar] [CrossRef]
- Steiner, C. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1960, 46, 731–735. [Google Scholar] [CrossRef]
- Jarabak, J.R.; Fizzell, J.A. Technique and Treatment with Light Wire Appliances, 2nd ed.; C. V. Mosby Co.: St Louis, MO, USA, 1972. [Google Scholar]
- Proffit, W.; Fields, H.; Sarver, D. Contemporary Orthodontics; Elsevier: Mosby, MO, USA, 2007. [Google Scholar]
- Zieliński, G. Effect Size Guidelines for Individual and Group Differences in Physiotherapy. Arch. Phys. Med. Rehabil. 2025, in press. [Google Scholar] [CrossRef]
- Ma, L.; Liu, F.; Mei, J.; Chao, J.; Wang, Z.; Shen, J. A comparative study to measure the sagittal condylar inclination using mechanical articulator, virtual articulator and jaw tracking device. J. Adv. Prosthodont. 2023, 15, 11–21. [Google Scholar] [CrossRef]
- Silva, J.; Martins, E.; Canabez, A.; Martin, D.; Martin, C. Comparison of Condylar Position Discrepancies Assessed Using an Optical Jaw Tracking System and a Conventional Condylar Position Indicator. Prosthesis 2025, 7, 40. [Google Scholar] [CrossRef]
- Burstone, C.J.; James, R.B.; Legan, H.; Murphy, G.A.; Norton, L.A. Cephalometric for orthognatic surgery. J. Oral Surg. 1978, 36, 269–277. [Google Scholar]
- Lai, Y.C.; Yap, A.U.; Turp, J.C. Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J. Oral Rehabil. 2020, 47, 270–280. [Google Scholar] [CrossRef]
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J. Oral Rehabil. 2017, 44, 908–923. [Google Scholar] [CrossRef]
| n | % | ||
|---|---|---|---|
| Gender | Male | 42 | 27.3 |
| Female | 112 | 72.7 | |
| Age (years) | 10–19 | 66 | 42.9 |
| Minimum = 11 | 20–29 | 35 | 22.7 |
| Maximum = 66 | 30–39 | 19 | 12.3 |
| Mean = 26.9 | 40–49 | 24 | 15.6 |
| Standard deviation = 14.0 | 50–59 | 7 | 4.5 |
| 60+ | 3 | 1.9 | |
| Skeletal classification | Class I | 54 | 35.1 |
| Class II | 52 | 33.8 | |
| Class III | 48 | 31.2 | |
| Angle classification | Class I | 59 | 38.3 |
| Class II | 40 | 26.0 | |
| Class III | 55 | 35.7 |
| TMD Signs/Symptoms | Chi-Squared Test | |||
|---|---|---|---|---|
| n | No | Yes | ||
| All sample | 154 | 105 (68.2%) | 49 (31.8%) | |
| By skeletal classification | ||||
| Class I | 54 | 39 (72.2%) | 15 (27.8%) | p = 0.377 |
| Class II | 52 | 37 (71.2%) | 15 (28.8%) | |
| Class III | 48 | 29 (60.4%) | 19 (39.6%) | |
| By Angle classification | ||||
| Class I | 59 | 40 (67.8%) | 19 (32,2%) | p = 0.958 |
| Class II | 40 | 28 (70.0%) | 12 (30.0%) | |
| Class III | 55 | 37 (67.3%) | 18 (32.7%) | |
| Incisor Inclination | |||
|---|---|---|---|
| U1–NA | U1–APog | U1–PP | |
| Sagittal condylar guidance right (n = 154) | R = −0.082 | R = −0.086 | R = −0.085 |
| Skeletal Class I (n = 54) | R= −0.200 | R= −0.135 | R= −0.236 |
| Skeletal Class II (n = 52) | R= −0.135 | R= −0.146 | R= −0.122 |
| Skeletal Class III (n = 48) | R= 0.072 | R= −0.034 | R= 0.095 |
| Sagittal condylar guidance left (n = 154) | R = −0.117 | R = −0.070 | R = −0.135 |
| Skeletal Class I (n = 54) | R= −0.232 | R= −0.064 | R= −0.202 |
| Skeletal Class II (n = 52) | R= −0.192 | R= −0.226 | R= −0.197 |
| Skeletal Class III (n = 48) | R= −0.017 | R= 0.083 | R= −0.045 |
| Overjet (n = 154) | R = −0.162 | R = 0.481 *** | R = −0.092 |
| Skeletal Class I (n = 54) | R= 0.103 | R= 0.207 | R= −0.077 |
| Skeletal Class II (n = 52) | R= 0.527 ** | R= 0.581 ** | R= 0.443 ** |
| Skeletal Class III (n = 48) | R= −0.126 | R= 0.267 | R= −0.133 |
| Overbite (n = 154) | R = −0.472 *** | R = −0.129 | R = −0.468 *** |
| Skeletal Class I (n = 54) | R= −0.289 * | R= −0.241 | R= −0.369 |
| Skeletal Class II (n = 52) | R= −0.400 ** | R= −0.401 ** | R= −0.419 ** |
| Skeletal Class III (n = 48) | R= −0.419 ** | R= −0.187 | R= −0.461 ** |
| Mandibular plane angle (n = 154) | R = −0.034 | R = 0.188 * | R = −0.057 |
| Skeletal Class I (n = 54) | R= 0.131 | R= 0.219 | R= 0.091 |
| Skeletal Class II (n = 52) | R= 0.057 | R= 0.104 | R= 0.039 |
| Skeletal Class III (n = 48) | R= −0.159 | R= −0.203 | R= −0.278 |
| Sub-sample: overjet > 0 and overbite > 0 (n = 108) | |||
| Sagittal condylar guidance right | R = −0.156 | R = −0.160 | R = −0.177 |
| Sagittal condylar guidance left | R = −0.122 | R = −0.159 | R = −0.167 |
| Overjet | R = 0.039 | R = 0.414 *** | R = 0.066 |
| Overbite | R = −0.483 ** | R = −0.233 * | R = −0.451 ** |
| Mandibular plane angle | R = 0.047 | R = 0.169 | R = −0.035 |
| Interincisal angle | R = −0.498 ** | R = −0.872 ** | R = −0.596 ** |
| TMD Signs/Symptoms | |||
|---|---|---|---|
| No (n = 105) | Yes (n = 49) | p | |
| Sagittal condylar guidance right | 49.30 (10.77) | 48.88 (14.70) | 0.755 (1) |
| Sagittal condylar guidance left | 48.31 (9.89) | 47.14 (15.22) | 0.664 (1) |
| Overjet | 2.82 (2.65) | 2.59 (2.92) | 0.820 (1) |
| Overbite | 2.16 (2.42) | 2.32 (2.41) | 0.709 (1) |
| U1–NA | 19.81 (8.24) | 20.18 (8.58) | 0.796 (2) |
| U1–APog | 24.26 (7.73) | 22.57 (7.44) | 0.204 (2) |
| U1–PP | 109.99 (9.01) | 108.96 (7.71) | 0.490 (2) |
| Mandibular plane angle | 24.89 (6.06) | 23.39 (7.36) | 0.183 (1) |
| Interincisal angle | 131.89 (10.12) | 134.06 (13.25) | 0.312 (2) |
| Sub-sample: overjet > 0 and overbite > 0 (N = 108) | |||
| U1–NA | 18.56 (8.11) | 17.73 (6.38) | 0.603 (2) |
| U1–APog | 24.76 (7.27) | 23.58 (6.71) | 0.427 (2) |
| U1–PP | 108.60 (9.24) | 106.55 (5.00) | 0.139 (2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, J.; Guedes, V.; Silva, J.C.; Martins, E.; Canabez, A.; Martin, D.; Martin, C. Association Between Maxillary Incisor Inclination and Sagittal Condylar Guidance Across Different Skeletal Malocclusions: A Cross-Sectional Study. Appl. Sci. 2025, 15, 10231. https://doi.org/10.3390/app151810231
Silva J, Guedes V, Silva JC, Martins E, Canabez A, Martin D, Martin C. Association Between Maxillary Incisor Inclination and Sagittal Condylar Guidance Across Different Skeletal Malocclusions: A Cross-Sectional Study. Applied Sciences. 2025; 15(18):10231. https://doi.org/10.3390/app151810231
Chicago/Turabian StyleSilva, Joana, Vanessa Guedes, Joana Correia Silva, Eugénio Martins, Alberto Canabez, Domingo Martin, and Conchita Martin. 2025. "Association Between Maxillary Incisor Inclination and Sagittal Condylar Guidance Across Different Skeletal Malocclusions: A Cross-Sectional Study" Applied Sciences 15, no. 18: 10231. https://doi.org/10.3390/app151810231
APA StyleSilva, J., Guedes, V., Silva, J. C., Martins, E., Canabez, A., Martin, D., & Martin, C. (2025). Association Between Maxillary Incisor Inclination and Sagittal Condylar Guidance Across Different Skeletal Malocclusions: A Cross-Sectional Study. Applied Sciences, 15(18), 10231. https://doi.org/10.3390/app151810231







