Abstract
This systematic review aimed to evaluate the efficacy of clear aligner therapy (CAT) in leveling the curve of Spee (CoS) in adult patients with permanent dentition. The clinical relevance of CoS correction lies in its impact on overbite reduction, occlusal function, and overall treatment outcomes. A comprehensive literature search was conducted across five electronic databases (PubMed, Scopus, Cochrane Library, Embase, and Web of Science), supplemented by grey literature. Eligible studies were retrospective clinical investigations assessing changes in CoS with CAT. Two reviewers independently performed data extraction and risk of bias assessment using the ROBINS-I tool, while the quality of evidence was graded using the GRADE approach. Seven retrospective studies met the inclusion criteria. All reported a reduction in CoS depth after CAT, ranging from 0.01 mm to 2.2 mm. Anterior intrusion was achieved to a limited extent, while posterior extrusion was inconsistent and often poorly expressed. Overbite reduction was observed in some studies, but none provided data on long-term stability. The predictability of CoS correction varied widely from 35% to 72%. All studies were judged to have a serious risk of bias, and the certainty of evidence was rated as low to very low. CAT appears capable of reducing CoS depth with outcomes comparable to fixed appliances; however, vertical control, especially posterior extrusion, remains unpredictable. In clinical practice, aligners may be considered for mild to moderate CoS correction, provided limitations are acknowledged. Further high-quality prospective trials with standardized protocols and long-term follow-up are required to strengthen the evidence base.
1. Introduction
The curve of Spee (CoS) is a natural curvature of the occlusal surfaces, first described by Ferdinand Graf Von Spee in 1890 [1]. It extends from the mandibular canine through the buccal cusps of the posterior teeth to the second molar, showing a concavity in the mandibular arch and a complementary convexity in the maxillary arch [2]. The depth and morphology of the CoS vary among individuals and are influenced by genetic, skeletal, and dental factors [3].
A balanced CoS is essential for masticatory efficiency, functional occlusion, and facial esthetics [4]. Deviations from this balance are frequently linked to malocclusion and functional disturbances. An accentuated CoS is often associated with deep bite malocclusions, where anterior overeruption and insufficient posterior support lead to excessive vertical overlap of incisors, with consequences such as incisor wear, periodontal trauma, muscular imbalance, and even temporomandibular joint (TMJ) dysfunction [5,6,7]. Conversely, a flattened CoS may predispose to open bite, impaired occlusal contact, functional instability, and reduced chewing efficiency [8]. For these reasons, leveling the CoS is a central objective in orthodontic treatment, as proper alignment improves posterior support, redistributes occlusal forces and enhance anterior guidance [9]. Conventional correction of the CoS relies on fixed appliances, typically involving anterior intrusion, posterior extrusion, or a combination of both, often achieved using continuous or segmented archwire mechanics [10]. Although effective, these strategies can present drawbacks such as longer treatment time, anchorage loss, and a higher risk of root resorption [11].
Clear aligner therapy (CAT) has emerged as an alternative to fixed appliances, offering esthetic advantages, greater comfort, and easier maintenance of oral hygiene [12,13,14,15].
Recent technological advances in aligner materials and digital workflows, such as SmartTrackTM and three-dimensional (3D) planning software, have further improved treatment precision [16]. Nevertheless, the capacity of aligners to provide reliable vertical control remains debated. Anterior intrusion and, in particular, posterior extrusion—both crucial for CoS leveling—can be difficult to achieve predictably due to the mechanical limitations of thermoplastic materials [17,18].
Posterior extrusion is especially challenging in the absence of a rigid wire framework, as aligners may slip or lose grip during extrusion [19].
To overcome these limitations, auxiliary features such as attachments and bite ramps are often incorporated. Attachments enhance aligner retention and control tooth inclination, while bite ramps, usually placed on the palatal side of upper incisors, facilitate anterior intrusion by disoccluding posterior teeth [20,21].
Despite the growing use of aligners, their true efficacy in leveling the CoS remains uncertain, with limited evidence compared to the well-established outcomes of fixed appliances. Importantly, to date, no systematic review has comprehensively addressed this specific question, highlighting a relevant gap in the orthodontic literature.
Therefore, the aim of this systematic review is to evaluate the efficacy of clear aligners in leveling the CoS, analyze the biomechanical strategies employed, and identify the main factors influencing treatment outcomes. The null hypothesis is that clear aligners are not effective in leveling the CoS in adult patients with permanent dentition.
2. Materials and Methods
2.1. Protocol Registration
This systematic review was designed and conducted according to the PRISMA 2020 guidelines (Preferred Reporting Items for Systematic and Meta-Analyses) [22].
The protocol was prospectively registered in the PROSPERO database (registration number CRD420251017336).
2.2. Search Strategy
A comprehensive electronic search was carried out across the following databases: PubMed, Scopus, Cochrane Library, Embase, and Web of Science. In addition, the grey literature was also screened through OpenGrey, Google Scholar, and ProQuest Dissertations to retrieve potentially relevant unpublished or non-indexed studies. The search was finalized in March 2025. No restrictions regarding publication year or language were applied. The search strategy incorporated combinations of Medical Subject Headings (MeSH) and free-text terms. The following keywords were used across databases: (“clear aligners” OR “Invisalign”) AND (“deep bite treatment” OR “curve of Spee”). The research question was developed according to the PICO framework and formulated as follows: “In orthodontic patients with permanent dentition, how effective are clear aligners in leveling the curve of Spee, in terms of reducing its depth and improving occlusal outcomes, compared to baseline conditions?” A comprehensive overview of the search strategy is shown in Table 1.

Table 1.
Search strategy for each database.
2.3. Eligibility Criteria
Inclusion and exclusion criteria were established according to the PICO framework as follows:
- -
- Population (P)—Orthodontic patients with permanent dentition undergoing treatment with clear aligners.
- -
- Intervention (I)—Orthodontic treatment with clear aligners aimed at leveling the curve of Spee.
- -
- Comparison (C)—No direct comparison group.
- -
- Outcome (O)—Effectiveness in leveling the curve of Spee (CoS), including changes in CoS depth and related occlusal outcomes.
Studies were included if they evaluated changes in the curve of Spee (CoS) as a primary outcome, measured through clinical records, digital models, or cephalometric analysis, before and after treatment with clear aligners. Eligible designs encompassed randomized controlled trials (RCT), prospective studies, retrospective cohort studies, and comparative observational studies that reported quantitative data on CoS correction with aligner.
Studies were excluded if they involved fixed appliances or combined treatments rather than clear aligners alone. Research that did not specifically assess the leveling of the curve of Spee or lacked relevant outcome data was not considered. Further exclusions included studies on syndromic patients, those with craniofacial anomalies or patients in mixed dentition. Case reports, case series, reviews, and in vitro or animal studies were also excluded.
2.4. Data Collection
Two reviewers (S.Z. and M.F.E.) independently extracted data from all included studies using a standardized data collection form based on the Cochrane Consumers and Communication Review Group model. The extracted data included:
- -
- Study information (authors, year of publication, and country);
- -
- Study design and sample size;
- -
- Patient characteristics (age and type of malocclusion);
- -
- Treatment protocol (aligner system, presence and type of attachments, use of auxiliaries such as elastics or bite-ramps, number of aligners, refinement, or staging);
- -
- Follow-up duration;
- -
- Primary outcome (changes in CoS depth);
- -
- Secondary outcome (overbite reduction, anterior intrusion, posterior extrusion, treatment duration, success rate, predictability, and stability).
To assess inter-reviewer agreement, Cohen’s Kappa coefficient was calculated (K = 0.78, substantial agreement). Discrepancies were resolved by discussion; if consensus was not reached, a third reviewer (S.C.) acted as arbiter. This ensured accuracy and reduced bias in the extraction process.
2.5. Risk of Bias Assessment
Since all included studies were retrospective observational, the risk of bias was evaluated exclusively with the ROBINS-I tool [23]. Two reviewers independently assessed seven domains: confounding, participant selection, classification of interventions, deviations from intended interventions, missing data, outcome measurement, and selective reporting. Disagreements were resolved by consensus. Each study was rated as having low, moderate, or serious risk of bias.
2.6. Certainty of Evidence
The certainty of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach [24]. Five domains were considered: risk of bias, inconsistency, indirectness, imprecision, and publication bias. Downgrading mainly resulted from the serious risk of bias across studies, heterogeneity in outcome measurement, small sample sizes, and absence of long-term follow-up. Accordingly, the overall certainty of evidence was judged as low to very low.
3. Results
The electronic database search yielded a total of 1758 records, identified from Embase (n = 252), PubMed (n = 263), Scopus (n = 19), Cochrane Library (n = 163), and Web of Science (n = 1061). No additional studies were found through the grey literature (n = 0) or manual searching (n = 0). After removing 445 duplicates, 1313 unique articles remained and were screened by title and abstract. During the initial screening phase, 1265 studies were excluded as they were deemed irrelevant to the focus of the review. The remaining 48 full-text articles were assessed for eligibility according to the predefined inclusion and exclusion criteria. Of these, 41 studies were excluded for the following reasons: use of fixed appliances or combined orthodontic approaches (n = 11), absence of specific evaluation of the curve of Spee (n = 9), finite element models or in vitro research designs (n = 7), case reports, reviews or editorials (n = 6), studies conducted on patients with mixed dentition or craniofacial syndromes (n = 5), and insufficient or missing data on outcomes related to the leveling of the curve of Spee (n = 3). Ultimately, seven clinical studies met the eligibility criteria and were incorporated into the qualitative synthesis. A detailed overview of the screening and selection process is illustrated in the PRISMA flowchart (Figure 1).
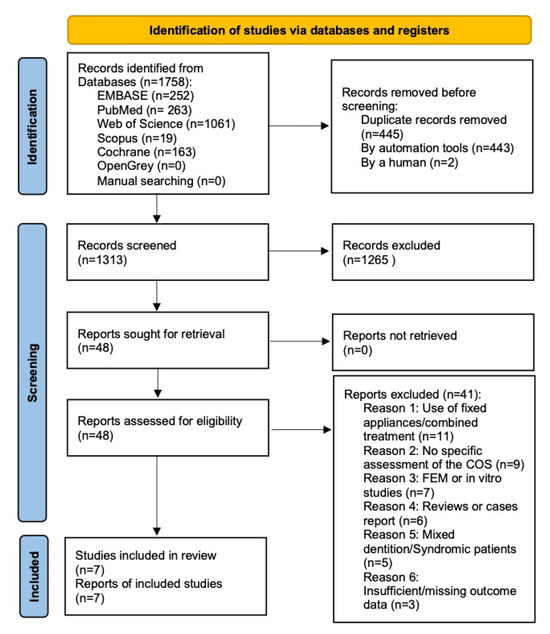
Figure 1.
PRISMA flowchart; flow diagram of the performed search.
3.1. Characteristics of the Included Studies
The seven selected studies were all observational clinical studies with retrospective design, published between 2022 and 2025. The total sample size ranged from 32 to 106 subjects.
The studies were conducted in various countries: three in Italy [25,26,27], two in Australia [28,29], one in China [30], and one in collaboration between Italy and Slovakia [31].
The mean age of patients ranged from 22.3 to 24 years in most studies.
Gender distribution was reported in all included studies, with a generally balanced proportion of male and female participants. Most studies enrolled Class I patients with deep bite, though some also included mild Class II cases.
A summary of the key characteristics of the included studies and type of malocclusion is presented in Table 2.

Table 2.
The main characteristics of included studies and type of malocclusion.
3.2. Treatment Protocols
All included studies employed clear aligner systems, with Invisalign® being the most commonly used brand [26,28,29,30,31]. Only one study utilized a different system, specifically Doris® [27].
The number of aligners varied across studies, with reported means ranging from 18.3 [29] to 42.6 [30,31], with some cases requiring refinements or staged protocols.
All included studies reported the use of attachments as an integral component of the treatment protocol with clear aligners. Ciavarella et al. [26], specifying the use of vertical rectangular attachments on posterior teeth, aimed at enhancing anterior intrusion and posterior anchorage control. Zhang et al. [30] described the use of rectangular attachments positioned on premolars, while three studies [25,28,29] reported the use of optimized or a combination of optimized and conventional attachments. Two studies [27,31] confirmed the presence of attachments but did not report any information on their type.
The use of inter-arch elastics was reported in only one study [31], indicating that the majority of treatments were performed exclusively with clear aligners. Conversely, bite ramps were used in three studies [26,27,30]. These features, typically positioned on the palatal surfaces of upper anterior aligners, aim to facilitate anterior intrusion and posterior control. A summary of the treatment protocols and clinical features of the included studies is presented in Table 3.

Table 3.
Treatment protocols and clinical features of the included studies.
3.3. Quantitative Outcomes
All studies reported a reduction in CoS depth, ranging from minimal values (−0.01 mm) [26] to more substantial decreases (−2.2 ± 1.92 mm) [25]. Overbite reduction was explicitly measured in several studies, with the most notable values being 2.00 mm [31] and 1.6 ± 1.24 [25]. Anterior intrusion was reported in a limited number of studies. Posterior extrusion was inconsistent and poorly expressed across studies. The predictability of COS correction varied widely, ranging from 35% [28] to 71.8% [30] across studies. Importantly, none of the studies assessed post-treatment stability, leaving the long-term effectiveness of vertical corrections with aligners uncertain.
A detailed overview of the numerical results extracted from each study is presented in Table 4.

Table 4.
Quantitative outcomes of curve of Spee correction with clear aligners.
3.4. Risk of Bias and Study Quality
All included studies were rated as having a serious risk of bias according to the ROBINS-I tool, mainly due to confounding, retrospective design and small sample sizes. No study was rated as “low risk” or “moderate risk”. The most frequent sources of bias were related to confounding factors (D1) and the selection of participants (D2), as shown in Figure 2. The high risk of bias is unfortunately common in orthodontic studies, particularly in those involving clear aligner therapy. The nature of the interventions often makes it impossible to blind patients, operators, or outcome assessors, which inherently increases the risk of performance and detection bias.
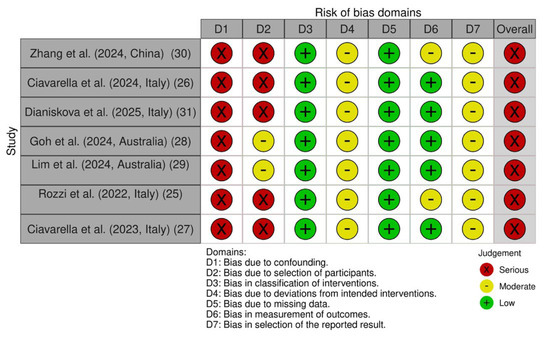
Figure 2.
Risk of bias of the included studies according to the Risk of Bias In Non-randomized Studies of Interventions (ROBINS-I).
3.5. Quality of Evidence
The quality of evidence for each outcome was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach. The certainty of evidence was judged as low to very low for all outcomes due to the serious risk of bias, inconsistency among results, small sample size, and absence of long-term follow-up. The summary of findings and GRADE ratings are presented in Table 5.

Table 5.
Summary of the quality of evidence (GRADE) for the main outcome evaluated.
4. Discussion
Based on the results of this systematic review, clear aligners demonstrated the ability to reduce the depth of the curve of Spee (CoS) in adult patients, with reported values ranging from 0.01 mm to 2.2 mm [25,26,27,28,29,30,31]. From a clinical standpoint, even small reductions in CoS may contribute to improved overbite control and functional occlusion, since leveling of the occlusal plane facilitates redistribution of occlusal forces and anterior guidance [5,32]. However, the variability observed across studies highlights the limited predictability of aligner therapy in achieving consistent vertical changes.
Unlike with fixed appliances—where leveling protocols typically involve sequential intrusion of the anterior teeth and posterior extrusion [8,9,33]—aligners rely on programed staging that often prioritizes alignment from posterior to anterior segments before anterior intrusion is expressed. This difference in biomechanics may explain why aligners tend to achieve modest levels of intrusion, while extrusion—particularly of posterior teeth—remains inconsistent. Moreover, while fixed appliances have historically been considered the gold standard for CoS correction, they are often associated with longer treatment duration, anchorage loss, and a higher risk of root resorption [34].
Therefore, although aligners can represent a viable alternative for vertical corrections in mild to moderate cases, their effectiveness depends strongly on the applied protocol, staging sequence, and patient compliance [12,13,35].
Despite these limitations, recent advances in attachment design and digital treatment planning have significantly improved the potential of aligners for vertical corrections. Optimized attachments, such as vertical rectangular attachments, play a crucial role in enhancing aligner retention and controlling tooth inclination, thereby increasing the predictability of vertical movements [36,37,38]. Clinically, this is relevant because adequate anterior intrusion is a prerequisite for effective leveling of the CoS; by intruding the incisors, the excessive vertical overlap is reduced and space is created for functional posterior contacts. In this sense, the findings of Ciavarella et al. [26] and Zhang et al. [30] confirm that attachments are not merely auxiliary features but essential biomechanical tools to achieve vertical control with aligners.
Similarly, the incorporation of bite ramps positioned on the palatal side of upper incisors facilitates anterior intrusion by disoccluding the posterior teeth, reducing occlusal interferences and allowing forces to be expressed more efficiently [39,40,41]. From a clinical perspective, bite ramps represent a simple but effective strategy to improve the vertical effectiveness of aligners, especially in deep bite cases where anterior intrusion is critical to reduce the CoS and improve functional occlusion.
Nevertheless, achieving predictable posterior extrusion remains the most challenging aspect of aligner therapy. While Dianiskova et al. [31] reported moderate extrusion of premolars, Lim et al. [29] found that posterior teeth underwent slight intrusion despite planned extrusion, confirming the biomechanical limitations of thermoplastic aligners in delivering stable vertical forces. Earlier studies by Kravitz et al. [12] and Simon et al. [13] had already highlighted this weakness and suggested adjunctive approaches such as intermaxillary elastics or skeletal anchorage devices (TADs), despite their documented potential to enhance posterior vertical control [42,43,44].
To overcome underexpression of movements, several authors recommended digital overcorrection [15,26] and refinement phases [45,46], which allow re-staging of aligners and modification of attachment design. However, the success of these strategies remains strongly dependent on patient compliance, further limiting the predictability of posterior extrusion and, consequently, of complete CoS leveling [47]. Kravitz et al. [12] recommended a minimum daily wear time of 20–22 h to optimize outcomes, especially in cases involving complex vertical corrections.
A significant limitation of the current evidence is the lack of long-term follow-up data. None of the included studies reported on post-treatment stability of the CoS correction achieved with aligners, leaving the risk of relapse unaddressed. Previous studies on fixed appliances have shown that vertical corrections, including deep bite and CoS leveling, are particularly susceptible to relapse in the absence of appropriate retention protocols [48]. Future studies should therefore incorporate standardized retention strategies and extended follow-up periods to evaluate the durability of aligner-based CoS corrections.
From a methodological perspective, all included studies were retrospective, with relatively small and heterogeneous samples. According to the ROBINS-I tool, every study was judged to carry a serious risk of bias—mainly due to confounding, lack of randomization, and participant selection. Moreover, outcome measurement methods varied (digital models vs. cephalometric radiographs), further complicating comparisons and limiting the possibility of quantitative syntheses. Standardized outcome measures are therefore needed to improve comparability across studies and to enable meta-analytic evaluations [49,50,51]. As a result, the certainty of the evidence, assessed using GRADE framework, was consistently graded as low to very low. Within this context, the null hypothesis—that clear aligners are not effective in leveling the CoS in adult patients—cannot be confidently rejected. While reduction in CoS depth was reported, the limited predictability of posterior extrusion, the absence of long-term stability data, and the overall low certainty of the available evidence substantially limit the strength of the conclusion.
Despite these limitations, this review provides valuable insights by focusing exclusively on CoS correction with clear aligners. The findings suggest that, when employed with appropriate biomechanical strategies such as optimized attachments, bite ramps, overcorrection protocols, and refinement phases, clear aligners may effectively reduce CoS depth and contribute to overbite correction. Clinically, aligners appear most suitable in mild to moderate cases where anterior intrusion is prioritized, whereas complex vertical corrections requiring significant posterior extrusion may still necessitate adjunctive mechanics or fixed appliances.
Future research should focus on prospective, randomized controlled trials with larger sample sizes, standardized treatment protocols, and sufficient follow-up to assess the long-term stability. Moreover, the integration of skeletal anchorage, intermaxillary elastics, and digital predictive modeling should be further investigated to enhance the predictability of vertical corrections achieved with aligners.
5. Conclusions
This systematic review indicates that clear aligner therapy (CAT) can achieve a reduction in the curve of Spee (CoS) in adult patients with permanent dentition, with reported values ranging from minimal to more substantial changes. Anterior intrusion was observed to a limited extent, whereas posterior extrusion proved inconsistent and often poorly expressed, confirming the biomechanical challenges inherent to aligner therapy. While these vertical effects may contribute to overbite correction and improved occlusal function, their clinical predictability remains limited. Importantly, no study provided data on long-term stability, leaving the durability of these corrections uncertain.
All included studies were retrospective, with relatively small and heterogeneous samples, a uniformly serious risk of bias according to the ROBINS-I tool, and variable outcome measurements, leading to the certainty of the evidence being graded as low to very low within the GRADE framework. The available evidence is insufficient to establish the effectiveness of clear aligners in leveling the curve of Spee, and the strength of the conclusions must be regarded as limited. Future prospective randomized trials with standardized protocols and long-term follow-up are required to provide more robust evidence and clarify the clinical role of aligners in CoS correction.
Author Contributions
S.Z. and M.F.E. conceptualized the review and performed the literature search, data extraction, and analysis. S.C. supervised the methodology and resolved discrepancies. F.C., N.S., T.C., A.V. and E.S. contributed to manuscript drafting and critical revisions. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Spee, F.G. The gliding path of the mandible along the skull. J. Am. Dent. Assoc. 1980, 100, 670–675. [Google Scholar] [CrossRef]
- Andrews, L.F. The six keys to normal occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Schudy, F.F. The curve of Spee: Past, present, and future. Am. J. Orthod. Dentofac. Orthop. 1963, 43, 311–318. [Google Scholar]
- Ricketts, R.M. A foundation for orthodontic research. Am. J. Orthod. 1975, 67, 206–214. [Google Scholar]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics, 5th ed; Mosby: St. Louis, MO, USA, 2012. [Google Scholar]
- Baldridge, D.W. Leveling the curve of Spee: Its effect on bite depth. Angle Orthod. 1969, 39, 175–184. [Google Scholar]
- Weiland, F.J.; Bantleon, H.P. Treatment of deep bite with the segmented arch technique. World J. Orthod. 2000, 1, 117–126. [Google Scholar]
- Benetti, M.; Montresor, L.; Trevisiol, L.; D’Agostino, A.; Zerman, N.; Verdecchia, A.; Spinas, E. Health and TMJ Function in Adult Patients Treated for Dentoskeletal Open Bite with Orthognathic Surgery—A Retrospective Cohort Study. Appl. Sci. 2024, 14, 8559. [Google Scholar] [CrossRef]
- Burstone, C.J. Deep overbite correction by intrusion. Am. J. Orthod. 1977, 72, 1–22. [Google Scholar] [CrossRef]
- Andrews, L.F. The straight-wire appliance. Br. J. Orthod. 1979, 6, 125–143. [Google Scholar] [CrossRef]
- Boyd, R.L. Esthetic orthodontic treatment using the Invisalign appliance for moderate to complex malocclusions. J. Dent. Educ. 2008, 72, 948–967. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment outcome and efficacy of an aligner technique—Regarding incisor torque, premolar derotation, and molar distalization. BMC Oral Health 2014, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Lione, R.; Franchi, L.; Noviello, A.; Cozza, P. Effectiveness of treatment of deep bite in growing subjects with Invisalign: A retrospective controlled study. Angle Orthod. 2021, 91, 157–164. [Google Scholar]
- Haouili, N.; Kravitz, N.D.; Vaid, N.R.; Ferguson, D.J.; Makki, L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 420–425. [Google Scholar] [CrossRef]
- Castroflorio, T.; Bargellini, A.; Lucchese, A.; Manuelli, M.; Casasco, F.; Cugliari, G.; Cioffi, I.; Deregibus, A. Effects of clear aligners on sleep bruxism: A randomized controlled trial. J. Biol. Regul. Homeost. Agents 2018, 32, 21–29. [Google Scholar]
- Clements, K.M.; Bollen, A.M.; Huang, G.; King, G.; Hujoel, P.; Ma, T. Activation time and material stiffness of sequential removable orthodontic appliances. Part 1: Ability to complete treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 496–501. [Google Scholar] [CrossRef]
- Elkordy, S.A.; Shohdy, K.S.; Naga, M.A.; Naga, I.A. The effect of Invisalign aligners on the occlusal contact pattern in adult orthodontic patients: A prospective clinical study. Angle Orthod. 2022, 92, 78–85. [Google Scholar]
- Kuncio, D.; Maganzini, A.; Shelton, C.; Freeman, K. Invisalign and traditional orthodontic treatment postretention outcomes compared using the American Board of Orthodontics objective grading system. Angle Orthod. 2007, 77, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Jackson, T. The Invisalign appliance in adult orthodontics: A retrospective analysis of efficacy and efficiency. Clin. Orthod. Res. 2000, 3, 171–178. [Google Scholar]
- Womack, W.R.; Day, R.H. Clinical assessments of patients treated with the Invisalign system. J. Clin. Orthod. 2007, 41, 557–568. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Rozzi, M.; Mucedero, M.; Pezzuto, C.; Lione, R.; Cozza, P. Leveling the curve of Spee: Comparison between continuous archwire treatment and Invisalign system: A retrospective study. Am. J. Orthod. Dentofacial Orthop. 2022, 162, 645–655. [Google Scholar] [CrossRef]
- Ciavarella, D.; Fanelli, C.; Suriano, C.; Cazzolla, A.P.; Campobasso, A.; Guida, L.; Laurenziello, M.; Illuzzi, G.; Tepedino, M. Curve of Spee modification in different vertical skeletal patterns after clear aligner therapy: A 3D set-up retrospective study. Prog. Orthod. 2024, 25, 5. [Google Scholar] [CrossRef]
- Ciavarella, D.; Fanelli, C.; Suriano, C.; Cazzolla, A.P.; Campobasso, A.; Guida, L.; Laurenziello, M.; Illuzzi, G.; Tepedino, M. Occlusal plane modification in clear aligners treatment: Three-dimensional retrospective longitudinal study. Dent. J. 2023, 11, 8. [Google Scholar] [CrossRef]
- Goh, S.; Dreyer, C.; Weir, T. The predictability of the mandibular curve of Spee leveling with the Invisalign appliance. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.W.; Meade, M.J.; Weir, T. The predictability of maxillary curve of Spee leveling with the Invisalign appliance. Angle Orthod. 2023, 93, 638–643. [Google Scholar] [CrossRef]
- Zhang, L.; Gong, B.; Xie, X.; Cao, L.; Gu, Y.; Sun, Y.; Bai, Y. The effectiveness of clear aligners in levelling the curve of Spee and related maxillofacial factors in patients with a deep overbite. BMC Oral Health 2024, 24, 338. [Google Scholar] [CrossRef]
- Dianiskova, S.; Rongo, R.; Sirignano, D.; D’Amelio, R.; Oliva, G.; Valletta, R.; D’Antò, V. Assessment of Clinical Predictability of Overbite Reduction and Curve of Spee Levelling in Clear Aligner Treatment. Orthod. Craniofac. Res. 2025, 28, 56–65. [Google Scholar] [CrossRef]
- Nanda, R. Biomechanics and Esthetic Strategies in Clinical Orthodontics; Elsevier: Maryland Heights, MO, USA, 2005. [Google Scholar]
- Weiland, F.J.; Bantleon, H.P.; Droschl, H. Evaluation of continuous arch and segmented arch leveling techniques in adult patients—A clinical study. Am. J. Orthod. Dentofacial Orthop. 1996, 110, 647–652. [Google Scholar] [CrossRef]
- Weltman, B.; Vig, K.W.; Fields, H.W.; Shanker, S.; Kaizar, E.E. Root resorption associated with orthodontic tooth movement: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 462–476. [Google Scholar] [CrossRef] [PubMed]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Guo, D.; Zhang, X.; Cheng, Y.; Zhang, H.; Xu, Y.; Jin, Z.; Ma, Y. Biomechanical effects of different staging and attachment designs in maxillary molar distalization with clear aligner: A finite element study. Prog. Orthod. 2023, 24, 43. [Google Scholar] [CrossRef]
- Aakriti, V.; Varun, G.; Gurkeerat, S.; Sridhar, K.; Raj, K.S.; Ankit, C. Unraveling the Role of Attachments in Clear Aligner Therapy. Int. J. Innov. Sci. Res. Technol. (IJISRT) 2023, 8, 3112–3115. [Google Scholar]
- Keilig, L.; Fittgen, A.; Schneider, H.; Sifa, R.; Schwarze, J.; Bourauel, C.; Konermann, A. Accuracy of Digital Orthodontic Treatment Planning: Assessing Aligner-Directed Tooth Movements and Exploring Inherent Intramaxillary Side Effects. J. Clin. Med. 2024, 13, 2298. [Google Scholar] [CrossRef]
- Husain, F.; Warunek, S.; Gurav, A.; Giangreco, T.; Tanberg, W.; Al-Jewair, T. Influence of Invisalign precision bite ramp utilization on deep bite correction and root length in adults. Angle Orthod. 2024, 94, 488–495. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Moshiri, M.; Nicozisis, J.; Miller, S. Mechanical considerations for deep-bite correction with aligners. Semin. Orthod. 2020, 26, 134–138. [Google Scholar] [CrossRef]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Di Venere, D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Marinelli, G.; Inchingolo, A.M.; Inchingolo, A.D.; Ferrante, L.; Avantario, P.; Campanelli, M.; Palermo, A.; Inchingolo, F.; Dipalma, G. Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review. Bioengineering 2025, 12, 531. [Google Scholar] [CrossRef]
- Geramy, A.; Ebrahimi, S. Evaluation of different models of intrusive force application and temporary anchorage device (TAD) placement in total arch intrusion using clear aligners; a finite element analysis. BMC Oral Health 2023, 23, 740. [Google Scholar] [CrossRef] [PubMed]
- Rongo, R.; Dianišková, S.; Spiezia, A.; Bucci, R.; Michelotti, A.; D’Antò, V. Class II Malocclusion in Adult Patients: What Are the Effects of the Intermaxillary Elastics with Clear Aligners? A Retrospective Single Center One-Group Longitudinal Study. J. Clin. Med. 2022, 11, 7333. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.J.; Ng, E.; Weir, T. Digital treatment planning and clear aligner therapy: A retrospective cohort study. J. Orthod. 2023, 50, 361–366. [Google Scholar] [CrossRef] [PubMed]
- D’Antò, V.; Bucci, R.; De Simone, V.; Huanca Ghislanzoni, L.; Michelotti, A.; Rongo, R. Evaluation of Tooth Movement Accuracy with Aligners: A Prospective Study. Materials 2022, 15, 2646. [Google Scholar] [CrossRef]
- Lai, W.L. Clear aligner in orthodontic retreatment. Zhonghua Kou Qiang Yi Xue Za Zhi 2024, 59, 400–406. (In Chinese) [Google Scholar]
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016, 29, CD002283. [Google Scholar] [CrossRef]
- Song, F.; Parekh, S.; Hooper, L.; Loke, Y.K.; Ryder, J.; Sutton, A.J.; Hing, C.; Kwok, C.S.; Pang, C.; Harvey, I. Dissemination and publication of research findings: An updated review of related biases. Health Technol. Assess. 2010, 14, 1–193. [Google Scholar] [CrossRef]
- Narkhede, S.; Rao, P.; Sawant, V.; Sachdev, S.S.; Arora, S.; Pawar, A.M.; Reda, R.; Testarelli, L. Digital versus Manual Tracing in Cephalometric Analysis: A Systematic Review and Meta-Analysis. J. Pers. Med. 2024, 14, 566. [Google Scholar] [CrossRef]
- Serafin, M.; Baldini, B.; Cabitza, F.; Carrafiello, G.; Baselli, G.; Del Fabbro, M.; Sforza, C.; Caprioglio, A.; Tartaglia, G.M. Accuracy of automated 3D cephalometric landmarks by deep learning algorithms: Systematic review and meta-analysis. Radiol Med. 2023, 128, 544–555. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).