Three-Dimensional Finite Element Analysis (FEM) of Tooth Stress: The Impact of Cavity Design and Restorative Materials
Abstract
1. Introduction
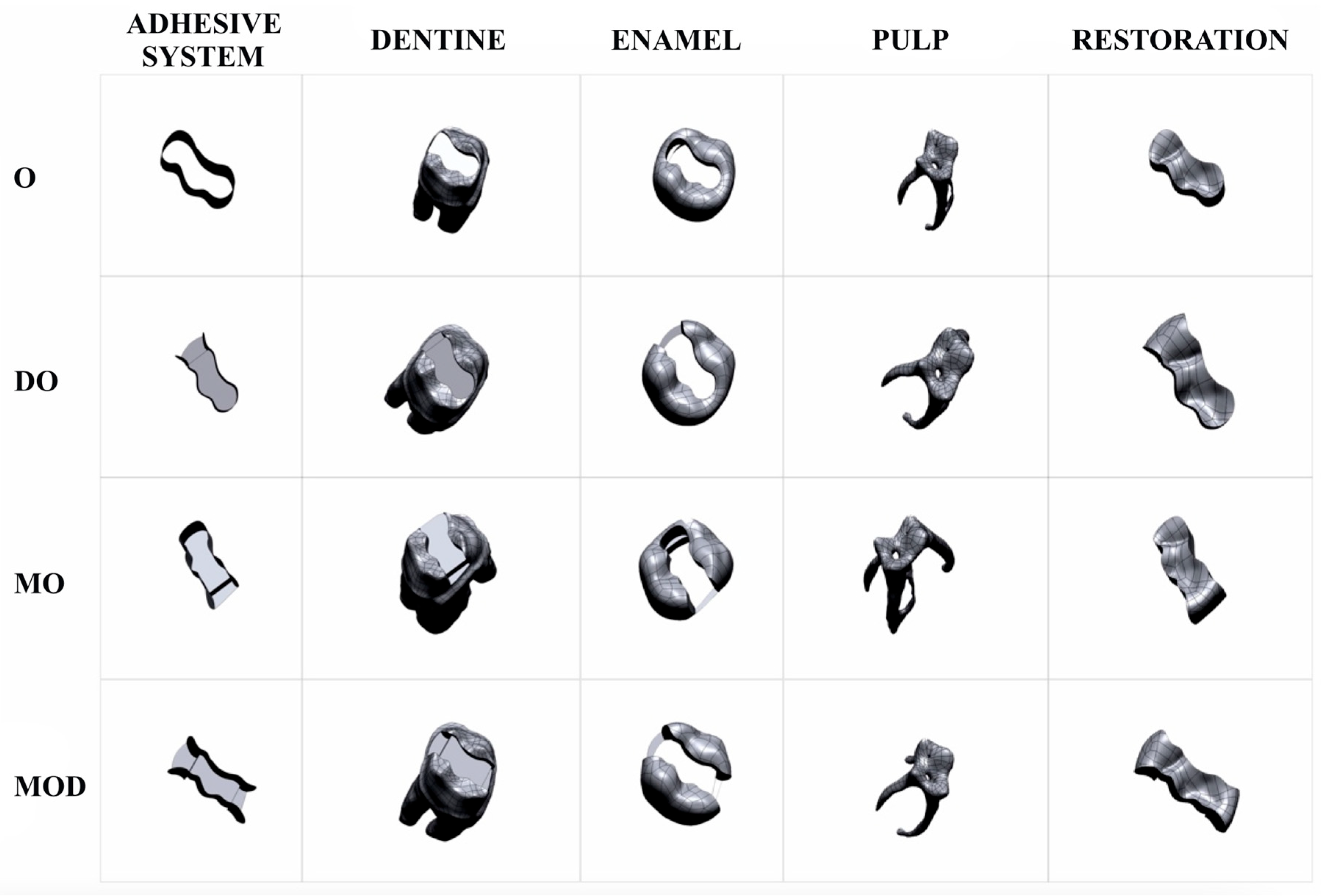
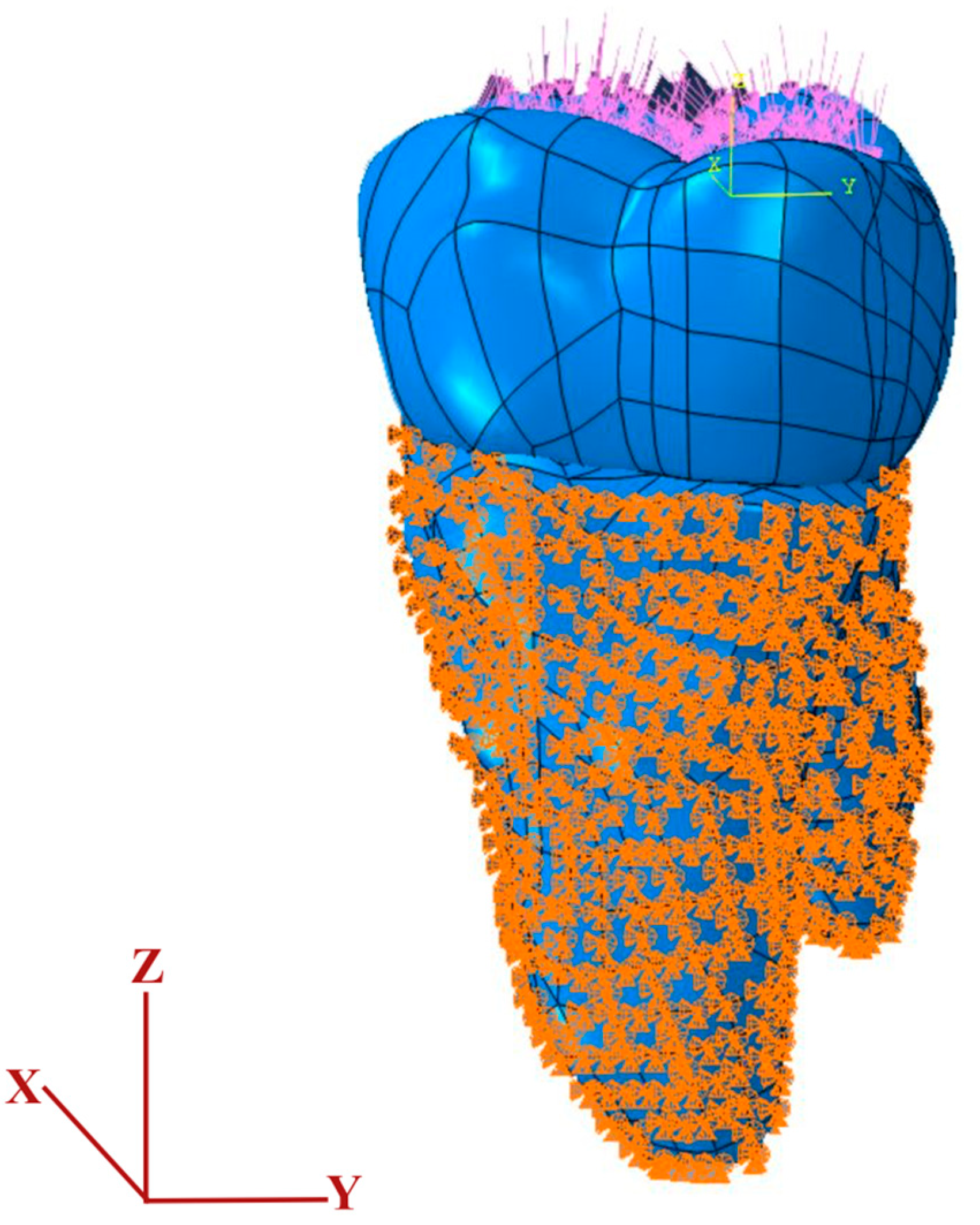
2. Material and Methods
| Material | Elastic Modulus (GPa) | Poisson’s Ratio | Tensile Strength (MPa) | Compressive Strength (MPa) |
|---|---|---|---|---|
| Dentine | 18.600 | 0.31 | 98.7 | 297.0 |
| Enamel | 84.100 | 0.33 | 10.3 | 384.0 |
| Pulp | 0.002 | 0.45 | - | - |
| Amalgam | 35.000 | 0.35 | 3–58 | 45–550 |
| Bulk-fill composite | 12.000 | 0.25 | 42 | 169.0 |
| Adhesive system | 4.500 | 0.3 |
| Model | Total Elements | Total Nodes | Mesh Type |
|---|---|---|---|
| A (Amalgam-Occlusal Cavity) | 7,066,486 | 1,277,802 | Linear tetrahedral elements of C3D4 |
| A′ (Composite-Occlusal Cavity) | 7,235,860 | 1,321,741 | Linear tetrahedral elements of C3D4 |
| B (Amalgam-Disto-occlusal Cavity) | 7,404,615 | 1,338,833 | Linear tetrahedral elements of C3D4 |
| B′ (Composite-Disto-occlusal Cavity) | 7,544,862 | 1,381,242 | Linear tetrahedral elements of C3D4 |
| C (Amalgam-Mesio-occlusal Cavity) | 7,275,590 | 1,315,887 | Linear tetrahedral elements of C3D4 |
| C′ (Composite-Mesio-occlusal Cavity) | 7,354,655 | 1,345,655 | Linear tetrahedral elements of C3D4 |
| D (Amalgam-Mesio-occluso-distal Cavity) | 7,412,739 | 1,342,075 | Linear tetrahedral elements of C3D4 |
| D′ (Composite-Mesio-occluso-distal Cavity) | 7,510,328 | 1,379,288 | Linear tetrahedral elements of C3D4 |
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef]
- Fejerskov, O.; Nyvad, B.; Kidd, E. (Eds.) Dental Caries: The Disease and İts Clinical Management; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Yadav, R.K.; Verma, U.P.; Tiwari, R.; Chaurasia, A. Mercury or mercury free restorations in oral cavity. Int. J. Public Health Sci. 2018, 7, 201–206. [Google Scholar] [CrossRef]
- Gönder, H.Y.; Demirel, M.G.; Mohammadi, R.; Alkurt, S.; Fidancioğlu, Y.D.; Yüksel, I.B. The Effects of Using Cements of Different Thicknesses and Amalgam Restorations with Different Young’s Modulus Values on Stress on Dental Tissue: An Investigation Using Finite Element Analysis. Coatings 2022, 13, 6. [Google Scholar] [CrossRef]
- Borgia, E.; Baron, R.; Borgia, J.L. Quality and survival of direct light-activated composite resin restorations in posterior teeth: A 5- to 20-year retrospective longitudinal study. J. Prosthodont. 2019, 28, e195–e203. [Google Scholar] [CrossRef] [PubMed]
- Sideridou, I.D.; Karabela, M.M.; Vouvoudi, E.C. Physical properties of current dental nanohybrid and nanofill light-cured resin composites. Dent. Mater. 2011, 27, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Resin-based composite performance: Are there some things we can’t predict? Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef]
- Yazici, A.R.; Kutuk, Z.B.; Ergin, E.; Karahan, S.; Antonson, S.A. Six-year clinical evaluation of bulk-fill and nanofill resin composite restorations. Clin. Oral Investig. 2022, 26, 417–426. [Google Scholar] [CrossRef]
- Rosatto, C.M.; Bicalho, A.A.; Veríssimo, C.; Bragança, G.F.; Rodrigues, M.P.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J. Dent. 2015, 43, 1519–1528. [Google Scholar] [CrossRef]
- Benetti, A.R.; Havndrup-Pedersen, C.; Honoré, D.; Pedersen, M.K.; Pallesen, U. Bulk-fill resin composites: Polymerization contraction, depth of cure, and gap formation. Oper. Dent. 2015, 40, 190–200. [Google Scholar] [CrossRef]
- Ulusoy, M.; Aydın, A.K. Diş Hekimliğinde Hareketli Bölümlü Protezler, Cilt II; Ankara Üniversitesi Basımevi: Ankara, Turkey, 2003; pp. 687–689. [Google Scholar]
- Geng, J.P.; Tan, K.B.; Liu, G.R. Application of finite element analysis in implant dentistry: A review of the literature. J. Prosthet. Dent. 2001, 85, 585–598. [Google Scholar] [CrossRef]
- Çalıkkocaoğlu, S. Dişsiz Hastaların Protetik Tedavisi: Klasik Tam Protezler; Quintessence: Istanbul, Turkey, 2010. [Google Scholar]
- Şen, S.; Bayındır, Y.Z.; Güler, Ç. İnsan dişi kaplamalarında kullanılan farklı özelliklerdeki yapıştırıcı simanların gerilme dağılımına etkilerinin sonlu elemanlar yöntemi ile incelenmesi. Atatürk Üniversitesi Diş Hekim. Fakültesi Derg. 2012, 2012, 31–39. [Google Scholar]
- Mohammed, S.D.; Desai, H. Basic concepts of finite element analysis and its applications in dentistry: An overview. J. Oral Hyg. Health 2014, 2, 156. [Google Scholar]
- Shetty, P.; Hegde, A.; Rai, K. Finite element method–an effective research tool for dentistry. J. Clin. Pediatr. Dent. 2010, 34, 281–285. [Google Scholar] [CrossRef]
- Wakabayashi, N.; Ona, M.; Suzuki, T.; Igarashi, Y. Nonlinear finite element analyses: Advances and challenges in dental applications. J. Dent. 2008, 36, 463–471. [Google Scholar] [CrossRef]
- Gómez, F.S.; Lorza, R.L.; Bobadilla, M.C.; García, R.E. Improving the Process of Adjusting the Parameters of Finite Element Models of Healthy Human Intervertebral Discs by the Multi-Response Surface Method. Materials 2017, 10, 1116. [Google Scholar] [CrossRef]
- Adigüzel, O. Finite Element Analysis: Review Part I: The uses in dentistry, basic concepts and description of elements. Dent. J. Dicle 2010, 11, 18–23. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; Fabianelli, A.; Gloria, A.; Martorelli, M.; Lanzotti, A.; Watts, D.C. Mechanical behavior of bulk direct composite versus block composite and lithium disilicate indirect Class II restorations by CAD-FEM modeling. Dent. Mater. 2017, 33, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; Di Rienzo, A.; Lanzotti, A.; Ventre, M.; Watts, D.C. Adhesive class I restorations in sound molar teeth incorporating combined resin-composite and glass ionomer materials: CAD-FE modeling and analysis. Dent. Mater. 2019, 35, 1514–1522. [Google Scholar] [CrossRef]
- de Abreu, R.A.; Pereira, M.D.; Furtado, F.; Prado, G.P.; Mestriner, W., Jr.; Ferreira, L.M. Masticatory efficiency and bite force in individuals with normal occlusion. Arch. Oral Biol. 2014, 59, 1065–1074. [Google Scholar] [CrossRef]
- Liu, T.; Huang, Y.; Li, Y.; Meng, J.; Liu, Y.; Wei, Y.; Huang, Y.; Zhou, Q.; Yang, W.; Yan, F.; et al. Effect of different restorative design and materials on stress distribution in cracked teeth: A finite element analysis study. BMC Oral Health 2025, 25, 31. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Borba, M.; Benetti, P.; Duan, Y.; Griggs, J.A. Three-dimensional finite element modelling of all-ceramic restorations based on micro-CT. J. Dent. 2013, 41, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Pałka, K.; Bieniaś, J.; Dębski, H.; Niewczas, A. Finite element analysis of thermo-mechanical loaded teeth. Comput. Mater. Sci. 2012, 64, 289–294. [Google Scholar] [CrossRef]
- Jiang, W.; Bo, H.; Yongchun, G.; Longxing, N. Stress distribution in molars restored with inlays or onlays with or without endodontic treat-ment: A three-dimensional finite element analysis. J. Prosthet. Dent. 2010, 103, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Babaei, B.; Shouha, P.; Birman, V.; Farrar, P.; Prentice, L.; Prusty, G. The effect of dental restoration geometry and material properties on biomechanical behaviour of a treated molar tooth: A 3D finite element analysis. J. Mech. Behav. Biomed. Mater. 2022, 125, 104892. [Google Scholar] [CrossRef]
- Rodrigues, M.D.; Soares, P.B.; Gomes, M.A.; Pereira, R.A.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Direct resin composite restoration of endodontically-treated permanent molars in adolescents: Bite force and patient-specific finite element analysis. J. Appl. Oral Sci. 2020, 28, e20190544. [Google Scholar] [CrossRef]
- Sengul, F.; Gurbuz, T.; Sengul, S. Finite element analysis of different restorative materials in primary teeth restorations. Eur. J. Paediatr. Dent. 2014, 15, 317–322. [Google Scholar]
- Valin Rivera, J.L.; Gonçalves, E.; Vinicius Soares, P.; Milito, G.; Ricardo Perez, J.O.; Palacios Roque, G.F.; Valin Fernández, M.; Figueredo Losada, H.; Araújo Pereira, F.; Garcia del Pino, G.; et al. The Restored Premolars Biomechanical Behavior: FEM and Experimental Moiré Analyses. Appl. Sci. 2022, 12, 6768. [Google Scholar] [CrossRef]
- Gönder, H.Y.; Öz, C. Bulk-fill kompozit rezinler. Necmettin Erbakan Üniversitesi Diş Hekim. Derg. 2020, 2, 117–123. [Google Scholar] [CrossRef]
- Eraslan, O.; Aykent, F.; Yücel, M.T.; Akman, S. The finite element analysis of the effect of ferrule height on stress distribution at post-and-core-restored all-ceramic anterior crowns. Clin. Oral Investig. 2009, 13, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Alberto, L.H.; Zhang, Z.; Duan, Y. Effect of Ferrule Design on Stress Distribution of Maxillary Incisor Rehabilitated with Ceramic Crown and PEEK Post–Core Material: A 3D Finite Element Analysis. Ceramics 2023, 6, 2256–2268. [Google Scholar] [CrossRef]
- Cosola, S.; Toti, P.; Babetto, E.; Covani, U.; Penarrocha-Diago, M.; Penarrocha-Oltra, D. In-vitro fatigue and fracture performance of three different ferrulized implant connections used in fixed prosthesis. J. Dent. Sci. 2021, 16, 397–403. [Google Scholar] [CrossRef]
- Epifania, E.; di Lauro, A.E.; Ausiello, P.; Mancone, A.; Garcia-Godoy, F.; Mendes Tribst, J.P. Effect of crown stiffness and prosthetic screw absence on the stress distribution in implant-supported restoration: A 3D finite element analysis. PLoS ONE 2023, 18, e0285421. [Google Scholar] [CrossRef] [PubMed]
- Agnihotri, H.; Bhatnagar, N.; Rao, G.V.; Jain, V.; Parkash, H.; Kar, A.K. Evaluation of the onset of failure under mechanical and thermal stresses on luting agent for metal–ceramic and metal crowns by finite element analysihons. Contemp. Clin. Dent. 2010, 1, 227–233. [Google Scholar] [CrossRef]
- Dejak, B.; Młotkowski, A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent. Mater. 2015, 31, e77–e87. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; Garcia-Godoy, F.; Gloria, A.; Lanzotti, A.; Maietta, S.; Martorelli, M. The effects of cavity-margin-angles and bolus stiffness on the mechanical behavior of indirect resin composite class II restorations. Dent. Mater. 2017, 33, e39–e47. [Google Scholar] [CrossRef] [PubMed]
- Darwich, A.; Adel, O.; Nazha, H. Finite element analysis of onlay restorations: Influence of design and onlay material on stress distribution in mandibular molars. SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Tuncdemir, M.T.; Yeşilyurt, N.G.; Arıkan, M. Comparison of the Stress Distribution in Class I and Class II Amalgam and Bulk-Fill Composite Restorations Using CAD-FEM Modeling. Int. J. Periodontics Restor. Dent. 2021, 41, e1–e9. [Google Scholar] [CrossRef]
- Yang, H.; Park, C.; Shin, J.H.; Yun, K.D.; Lim, H.P.; Park, S.W.; Chung, H. Stress distribution in premolars restored with inlays or onlays: 3D finite element analysis. J. Adv. Prosthodont. 2018, 10, 184–190. [Google Scholar] [CrossRef]
- Gönder, H.Y.; Mohammadi, R.; Harmankaya, A.; Yüksel, İ.B.; Fidancıoğlu, Y.D.; Karabekiroğlu, S. Teeth Restored with Bulk–Fill Composites and Conventional Resin Composites; Investigation of Stress Distribution and Fracture Lifespan on Enamel, Dentin, and Restorative Materials via Three-Dimensional Finite Element Analysis. Polymers 2023, 15, 1637. [Google Scholar] [CrossRef]
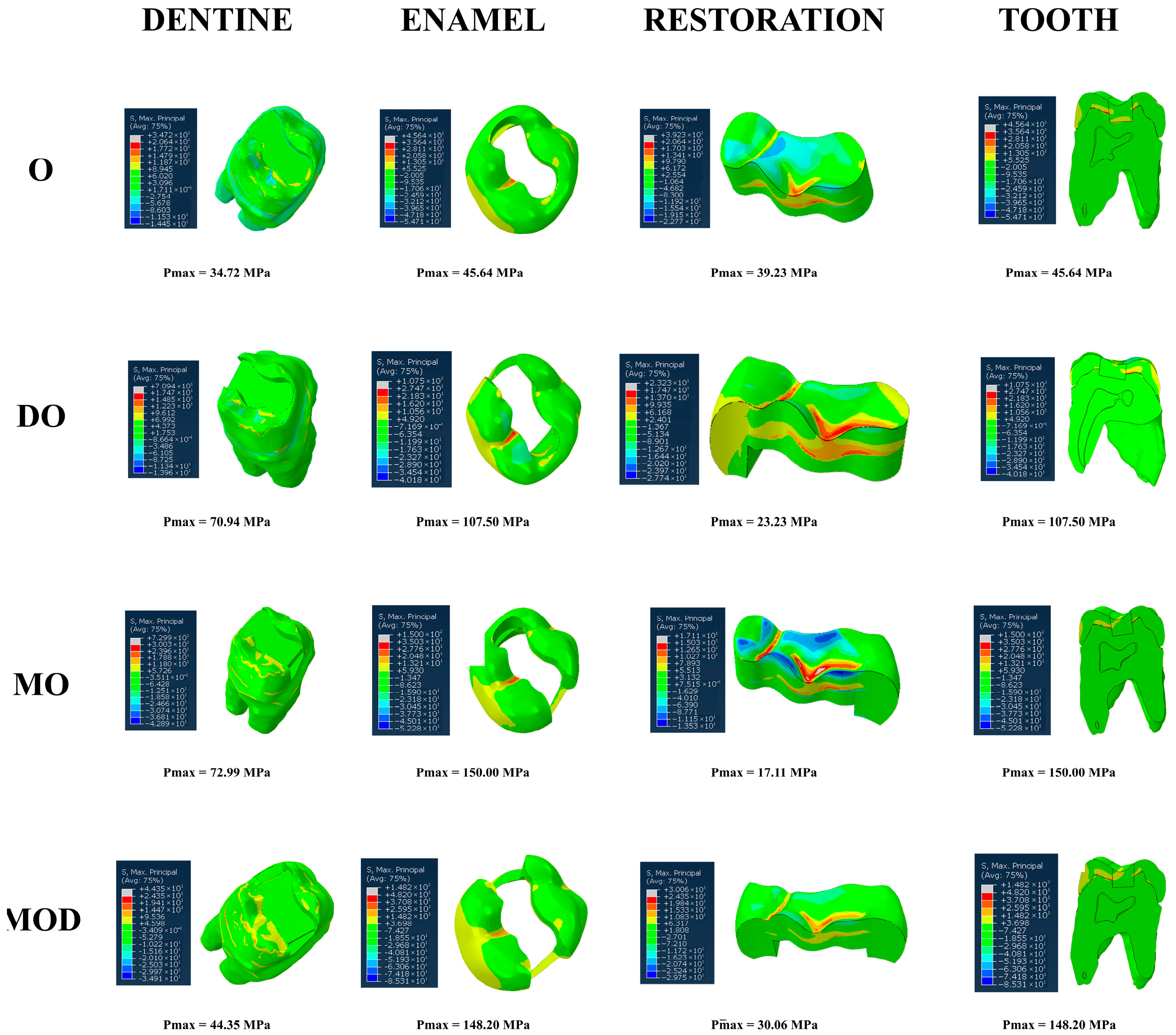

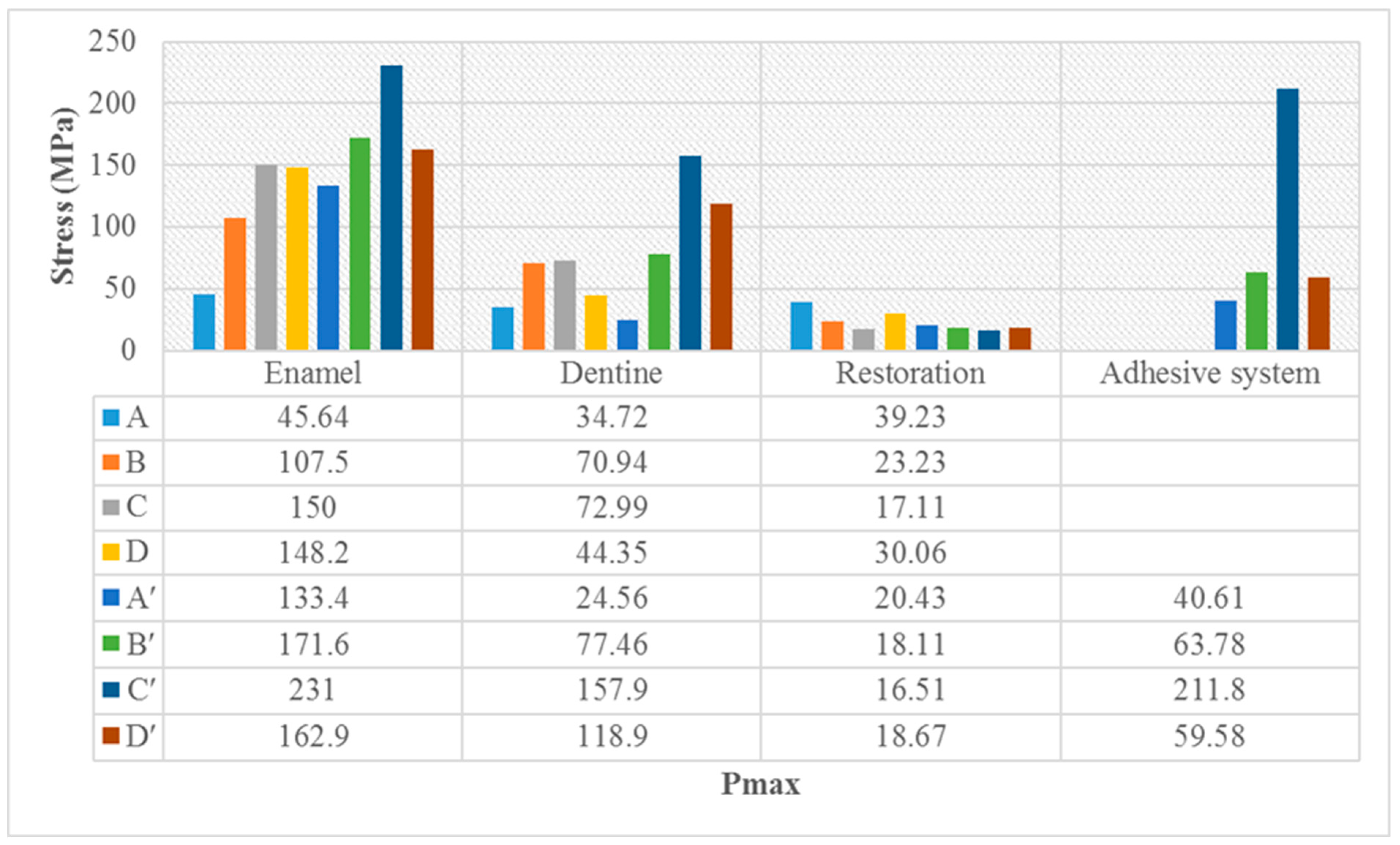
| Cavity Type | Dentin | Enamel | Restoration | Tooth |
|---|---|---|---|---|
| Occlusal (O) | 34.72 | 45.64 | 39.23 | 45.64 |
| Disto-occlusal (DO) | 70.94 | 107.50 | 23.23 | 107.50 |
| Mesio-occlusal (MO) | 72.99 | 150.00 | 17.11 | 150.00 |
| Mesio-occluso-distal (MOD) | 44.35 | 148.20 | 30.06 | 148.20 |
| Cavity Type | Dentin | Enamel | Restoration | Tooth | Adhesive System |
|---|---|---|---|---|---|
| Occlusal (O) | 24.56 | 33.40 | 20.43 | 33.40 | 40.61 |
| Disto-occlusal (DO) | 77.46 | 171.60 | 18.11 | 171.60 | 63.78 |
| Mesio-occlusal (MO) | 157.90 | 231.00 | 16.51 | 231.00 | 211.80 |
| Mesio-occluso-distal (MOD) | 118.90 | 162.90 | 18.67 | 162.90 | 59.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fidancioğlu, Y.D.; Alkurt Kaplan, S.; Mohammadi, R.; Gönder, H.Y. Three-Dimensional Finite Element Analysis (FEM) of Tooth Stress: The Impact of Cavity Design and Restorative Materials. Appl. Sci. 2025, 15, 9677. https://doi.org/10.3390/app15179677
Fidancioğlu YD, Alkurt Kaplan S, Mohammadi R, Gönder HY. Three-Dimensional Finite Element Analysis (FEM) of Tooth Stress: The Impact of Cavity Design and Restorative Materials. Applied Sciences. 2025; 15(17):9677. https://doi.org/10.3390/app15179677
Chicago/Turabian StyleFidancioğlu, Yasemin Derya, Sinem Alkurt Kaplan, Reza Mohammadi, and Hakan Yasin Gönder. 2025. "Three-Dimensional Finite Element Analysis (FEM) of Tooth Stress: The Impact of Cavity Design and Restorative Materials" Applied Sciences 15, no. 17: 9677. https://doi.org/10.3390/app15179677
APA StyleFidancioğlu, Y. D., Alkurt Kaplan, S., Mohammadi, R., & Gönder, H. Y. (2025). Three-Dimensional Finite Element Analysis (FEM) of Tooth Stress: The Impact of Cavity Design and Restorative Materials. Applied Sciences, 15(17), 9677. https://doi.org/10.3390/app15179677






