1. Introduction
Eating disorders (EDs) represent a significant challenge in the mental health of adolescents and young adults. Recent years have seen a trend towards the earlier onset of EDs, particularly among young women, which increases the risk of chronicity [
1,
2,
3]. The lifetime prevalence is 8.4% (3.3–18.6%) for women and 2.2% (0.8–6.5%) for men [
4]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classification [
5], EDs are divided into eight subtypes: anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder, pica, rumination disorder, avoidant/restrictive food intake disorder, other specified feeding or eating disorders, and unspecified feeding or eating disorders. Since 2018, ED cases have increased by 79.2% in Catalonia. The day hospitals for community care in the province of Tarragona handle the largest proportion of ED cases compared to other hospitals in Catalonia [
6]. The Terres de l’Ebre region, located in the south of Tarragona, Catalonia, is characterized by a low population density and vast rural areas and is therefore considered a rural setting. Currently, mental health care faces numerous challenges, especially in rural areas with limited access to specialized services. This situation highlights the need to expand the reach of mental health care and reduce geographical and socioeconomic barriers.
Various studies agree on the higher prevalence of EDs in women, although the exact ratio varies depending on the type of disorder, methodological design, and diagnostic criteria used. Estimates of the female-to-male ratio range from 2:1 to 10:1 [
7]. Beyond physical changes, EDs can cause hormonal alterations, cardiac problems, and bone demineralization and are associated with higher risks of depression, anxiety, and suicidal ideation. Anxiety is a symptom that affects individuals with various mental disorders. Comparative studies between the general population and individuals treated in mental health units have shown statistically significant differences in anxiety levels, confirming that individuals with mental disorders have notably higher anxiety scores [
8,
9,
10,
11].
Body image distortion is defined as “an alteration in the way weight or body shape is experienced, with undue influence of weight or body shape on self-evaluation or a persistent lack of recognition of the seriousness of current low body weight” [
5]. Anxiety related to eating and associated with body image distortion is a common symptom [
12,
13,
14].
Although an improvement in body mass index (BMI) may occur, this does not necessarily guarantee an improvement in body image distortion, as it can persist or even worsen, exacerbating symptoms of depression and anxiety [
13,
15]. This highlights the complexity of EDs, where physical recovery is not always accompanied by psychological recovery, requiring a comprehensive therapeutic approach that addresses the nutritional, emotional, and cognitive aspects involved in body perception.
Systematic reviews have observed that some studies have combined IVR with other techniques, such as cognitive behavioral therapy (CBT), yielding better results [
15,
16,
17]. The high acceptance of IVR therapy in clinical contexts is widely supported by the recent scientific literature [
18]. However, there is still limited literature on immersive virtual reality (IVR) and EDs [
19] and even less evidence regarding IVR with remote therapy for EDs [
20]. Experiences in this remote therapy are based on pilot studies with heterogeneous samples and technologies used. In this context, immersive therapies with IVR offer new opportunities to address various clinical aspects through exposure to controlled environments, helping to overcome fear and anxiety related to eating [
21]. This multisensory interaction allows body image to be confronted from a new perspective. This is particularly relevant as it favors the recalibration of the brain’s internal models through receiving precise and real-time sensory feedback. These strategies are based on predictive coding theories [
22]. Predictive coding is a cognitive model that suggests that the brain constantly makes predictions about the external world and adjusts these predictions based on sensory information received. In the context of EDs, this model is particularly relevant because adolescents with EDs often have distorted perceptions of their bodies, according to which the brain updates its internal representation of the body based on new sensory experiences, especially when discrepancies between the expected and perceived occur.
Nevertheless, the literature also warns about the potential adverse effects associated with the use of immersive virtual reality (IVR), particularly cybersickness—a set of symptoms similar to motion sickness. Initially, these symptoms were recorded only after the intervention; however, recent studies suggest the need to evaluate them before the start of virtual exposure to identify potential predisposing factors and improve therapy tolerance [
23].
Although the existing literature has explored the use of IVR in the treatment of EDs, there is a lack of studies that specifically evaluate the combination of IVR and remote intervention in adolescents with EDs [
20]. This gap is significant, as remote interventions can offer a viable solution for populations in rural areas or with limited access to specialized services. This pilot study presents an innovative intervention that connects professionals from different care areas through the use of IVR technology and fifth-generation mobile network (5G) communication. Thus, the aim of this study is to assess whether remote VR-based therapy can be a practical and acceptable option for young people with eating disorders, especially in rural areas. It also examines how this method affects anxiety and body image perception, which are key challenges in early treatment.
Unlike previous studies, this research explores the feasibility of using immersive VR in decentralized settings with minimal supervision, highlighting its potential to make early therapeutic interventions more accessible and emotionally engaging for underserved populations. Given the exploratory nature of the study, no prior hypotheses were formulated.
2. Materials and Methods
2.1. Design
This is an exploratory pilot study with a control group and a quasi-experimental pre-test/post-test design. The primary objective is to evaluate the feasibility, tolerance, and preliminary effects of remote virtual reality intervention on body perception. The participant assignment was not random, given the initial focus on proof of concept and procedure validation. This study was designed and reported following the international guidelines established by the CONSORT 2010 statement—specifically, its extension for pilot and feasibility trials (CONSORT 2010 Statement: Extension to Randomised Pilot and Feasibility Trials) [
24]. This guide provides a rigorous methodological framework to ensure the transparency, reproducibility, and quality of the design, execution, and reporting of preliminary studies aimed at assessing the feasibility of larger-scale clinical trials. All relevant items from the adapted checklist have been considered, including the justification for the pilot design, predefined feasibility criteria, and exploratory analytical treatment, avoiding inferential interpretations about the treatment’s efficacy at this initial stage.
2.2. Study Participants
The study involved adolescents and young adults aged between 12 and 24 years who were treated at the mental health center of Fundació Pere Mata Terres de l’Ebre (Catalonia, Spain), the sole provider of mental health services in this Health Region. This center is located in the Terres de l’Ebre Health Region, in Southern Catalonia—a territory comprising four counties: Baix Ebre, Montsià, Terra Alta, and Ribera d’Ebre. The region is characterized by significant geographical dispersion and a low population density, posing an additional challenge for the provision of mental health services. In total, it encompasses an approximate population of 190,000 inhabitants, distributed among medium and small urban centers, as well as rural areas with difficult access. This territorial and sociodemographic context provides a particularly relevant environment for the development and evaluation of pilot interventions aimed at the youth population in the field of community mental health.
A total of 12 participants were recruited. Participants had to possess a clinical diagnosis of an ED, current or previous. The 12 participants were recruited at the reference outpatient mental health center. Of the 12 participants, one declined to participate and another, from the non-experimental group, dropped out of the treatment, resulting in a final sample of 10 participants (5 cases and 5 controls).
The experimental group (cases) included three individuals with anorexia nervosa (DSM-V: 307.1), one case of an unspecified eating disorder (DSM-V: 307.50), and one case of other specified feeding or eating disorders (DSM-V: 307.59). The control group included two individuals with anorexia nervosa (DSM-V: 307.1), two individuals with bulimia nervosa (DSM-V: 307.51), and one case of an unspecified eating disorder (DSM-V: 307.50).
The distribution was performed equitably into two conditions: an experimental group (cases = 5), which was administered the studied treatment, and a control group (control = 5), which continued with the usual treatment, without receiving the proposed intervention. Both groups were in the study for a period of 6 weeks.
The inclusion criteria for participating in the pilot study were an age between 12 and 24 years, the primary diagnosis of an ED, and having informed consent signed by the participant and their legal representative. Individuals with epilepsy, intellectual disabilities, or pregnancy were excluded.
2.3. Material
2.3.1. VR Software and Device
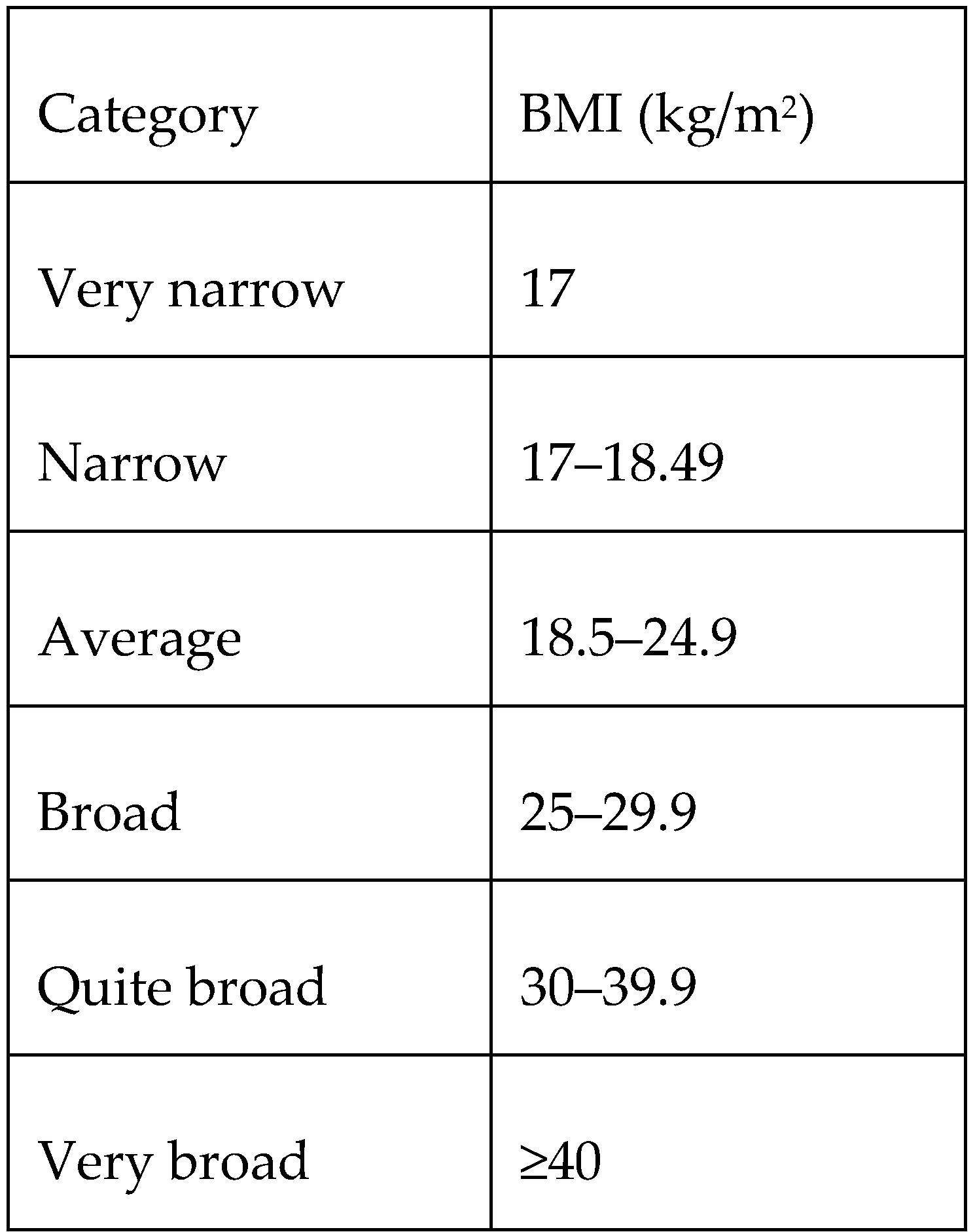
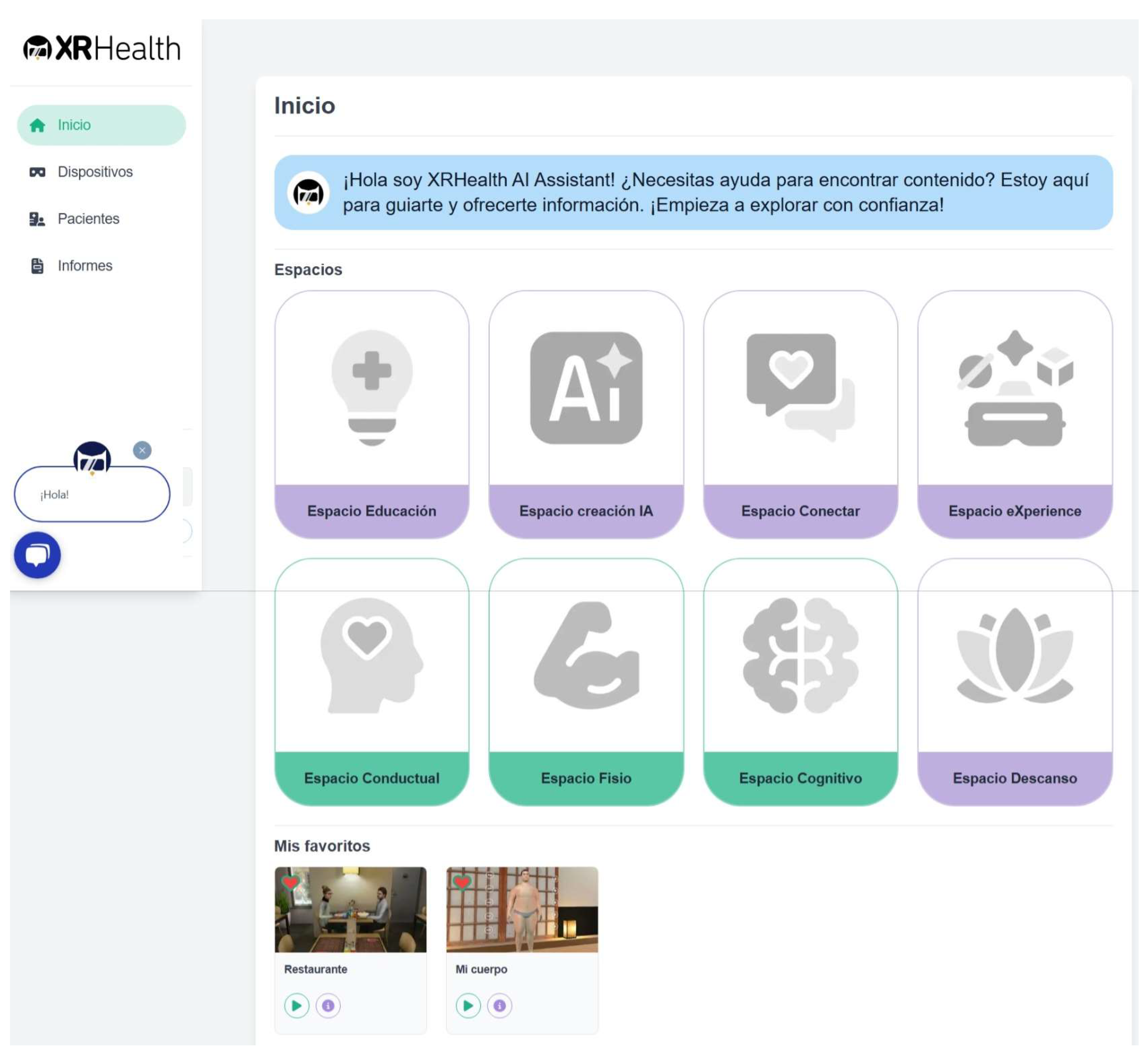
The software used was Amelia by XRHealth, version 0.3.1 (
Figure 1), an advanced virtual reality platform specifically designed for mental health professionals and originally developed by Amelia Virtual Care (Barcelona, Spain), which is now part of XRHealth.
This platform includes the Pico Neo 2 headset (
Figure A2), which features integrated headphones and weighs 690g, providing an immersive and comfortable experience (
Figure 2). Additionally, the system includes two wireless controllers, one for each hand, allowing precise and natural interaction with the virtual environment (
Figure 2). For more information, visit Amelia Virtual Care (
https://ameliavirtualcare.com, accessed on 1 January 2024).
Although this project focuses on working with individuals with eating disorders, the software offers various intervention proposals that are also available for use. An example of this is relaxation and mindfulness, which can be practiced in different virtual spaces and situations.
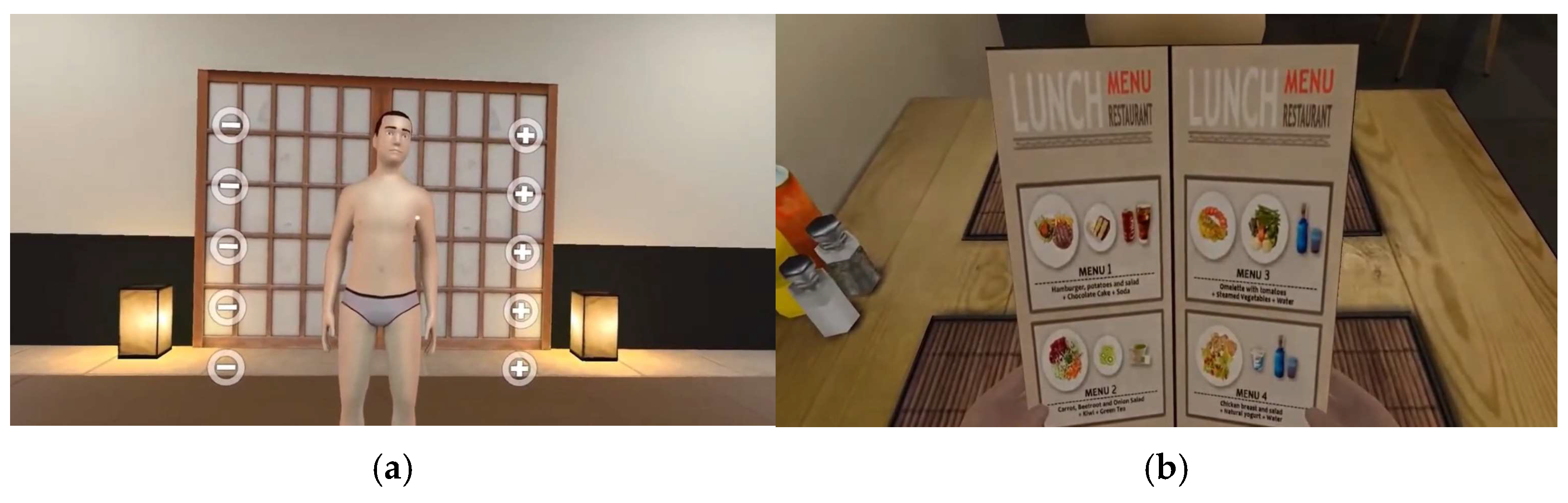
The two scenarios that we worked with in the experimental group are described below (
Figure 3).
In the first two sessions, we focused on body image perception. The intervention aimed to address body image distortion. The program configured the variables according to the body mass index (BMI) guidelines (
Figure A1) provided by the tool. These guidelines ensure that the BMI is as accurate as possible for the individual receiving the intervention. The participant can view their body based on the measurements provided. The body is surrounded by “+” and “−”symbols, allowing the participant to adjust the avatar’s body according to their self-perception of body image. After this modification, we proceed to compare the two avatars, superimposing one onto the other to visualize the differences. The dimensions selected by the patient are superimposed as a red outline on the avatar initially configured by the therapist. This visual overlay allows the patient to observe the discrepancy between their perceived body image and the baseline avatar, facilitating the clinical exploration of body image distortion.
The BPS allows for the observation and addressing of biases in body self-perception as participants confront the avatar generated from their own anthropometric measurements. In the first session, the patient was confronted with their own image, and, in the second session, work was performed involving the comparison of avatars. This spontaneous reaction enabled the real-time exploration of the dissociation between internal body perception and objective visual representation, generating clinically relevant material to guide the development of the intervention during the session.
In the third and fourth sessions, we focused on food exposure. This intervention creates a simulated environment for food intake in a restaurant setting. The type of diet can be selected according to the objectives of the intervention. The environment can include furniture that simulates eating alone or in a restaurant with more people. Additionally, different levels of interaction can be added, such as a companion who converses with the participant during the meal or simply shares the table without engaging in conversation.
In the RS, two sessions were conducted with the aim of progressively modulating the participants’ emotional responses. In the first session, each patient was allowed to freely select the virtual environment, thus fostering a greater sense of control and initial familiarity. In the second session, an environment with greater emotional demands was deliberately introduced. This strategy allowed for the gradual confrontation of anxiety-generating elements, facilitating emotional processing in a controlled context.
2.3.2. 5G Connectivity
The system also includes a router with 5G connectivity (
Figure 4), which connects to the headset and allows the user to take the kit home or to rural areas with coverage. This ensures a high-speed, low-latency connection, facilitating interaction with the mental health professional. Additionally, it provides a secure internet connection independent of the home network. Therefore, it is not necessary for the user to have Wi-Fi at home, which facilitates access for people in different socioeconomic conditions and in various rural areas, regardless of their access to Wi-Fi.
2.3.3. Visit Management System
As part of the technological infrastructure supporting the intervention, the professionals utilized a visit management system. This system is integrated into the monitoring of sessions and secure video calls, allowing professionals to conduct remote sessions in accordance with institutional protocols. The system ensured the continuity of care for virtual interactions throughout the study period.
2.4. Measures
Participants underwent an initial and post-intervention evaluation using specific instruments aligned with the study objectives to ensure the precise and relevant measurement of the variables of interest.
2.4.1. State Trait Anxiety Inventory (STAI)
The State Trait Anxiety Inventory (STAI), Spanish version [
25], is derived from the original State Trait Anxiety Inventory [
26]. The STAI is a self-report scale consisting of 40 items in total, which separately assess anxiety as a transient state or condition and anxiety as a stable trait or propensity. State Anxiety (SA): This subscale evaluates a transient emotional state characterized by subjective feelings of tension and apprehension and heightened autonomic nervous system activity. Trait Anxiety (TA): This subscale indicates a relatively stable anxious propensity, characterizing individuals who tend to perceive situations as threatening.
The scores have a direct interpretation: higher scores indicate greater state anxiety, and lower scores indicate less state anxiety. In the SA scale, there are ten items that affirm anxiety and ten that negate it (these items are 1, 2, 5, 8, 10, 11, 15, 16, 19, and 20, and the intensity score assigned will be reversed). The STAI provides a state anxiety score and a trait anxiety score, each obtained by summing the scores of the respective 20 items. The total score for each concept ranges from 0 to 60 points. In the TA scale, there are 13 items that affirm anxiety and seven that negate it (these items are 21, 26, 27, 30, 33, 36, and 39, and the frequency score assigned will be reversed). There is no cut-off point for the questionnaire, but the authors provide normative percentiles.
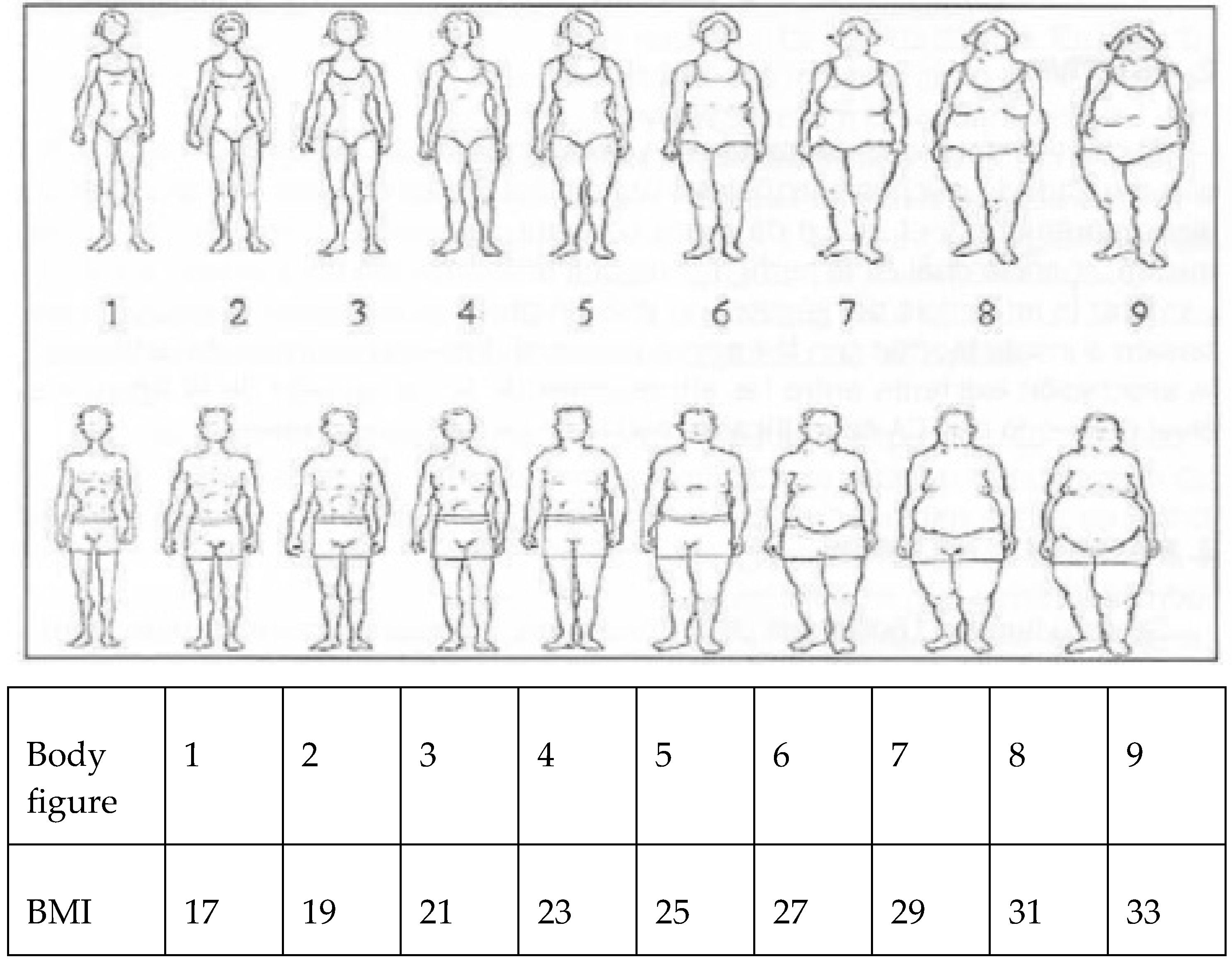
2.4.2. Figure Test
The Stunkard and Stellar Figure Rating Test (1990) [
27], modified by Collins (1991) [
28], consists of nine male and nine female body silhouettes, arranged progressively from the smallest to the largest body size. Each silhouette is assigned a body mass index (BMI) value, ranging from a minimum of 17 kg/m
2 (thinnest figure) to a maximum of 33 kg/m
2 (most corpulent figure) (
Figure A3). Each participant selected the silhouette that, in their judgment, corresponded to their body image, in relation to the questions posed during the protocol. Each person chooses the model according to the questions, “When you look at yourself naked in the mirror, which of these images do you feel most identified with?”, “Which is the image you would like to have?”, and “Which is the image you believe is the healthiest?” Based on the model chosen according to their perception, each person is assigned a perceived, desired, and healthy BMI. This variable allows the quantification of the discrepancy between subjective body perception and anthropometric reality. The person is weighed and measured to obtain their actual BMI. The classification of the sample concludes with groups of normal weight, overweight, and obesity according to the actual BMI. The difference between the perceived and desired BMI reflects body image distortion.
2.4.3. Simulator Sickness Questionnaire
The Simulator Sickness Questionnaire (SSQ) [
29] focuses on adverse symptoms associated with the use of virtual reality (VR). Permission has been obtained from the authors for its use. It consists of 16 items divided into two dimensions or subscales of discomfort: oculomotor (items 11, 5, 4, 10, 3, 9, 2) and nausea (items 1, 15, 8, 13, 14, 7, 6, 12, 16). Responses are given on a Likert scale from 0 to 3, indicating the degree to which these symptoms are typically experienced by the individual, ranging from absent to severe. The Spanish version by [
30] presents high content validity (0.89) and a kappa index also of 0.89. The authors recommend evaluation based on absolute values, as the questionnaire does not provide standardized cut-off scores to classify the severity of symptoms.
To complement the SSQ results, the descriptive thresholds proposed in the Brown Symptomatology Score [
23] were used as an additional reference to describe the degree of symptom severity. Although both instruments assess cybersickness-related symptoms, they are separate measures: the SSQ was administered to collect participants’ responses, while the Brown scale served exclusively as a framework to support the interpretation of the total scores in descriptive terms.
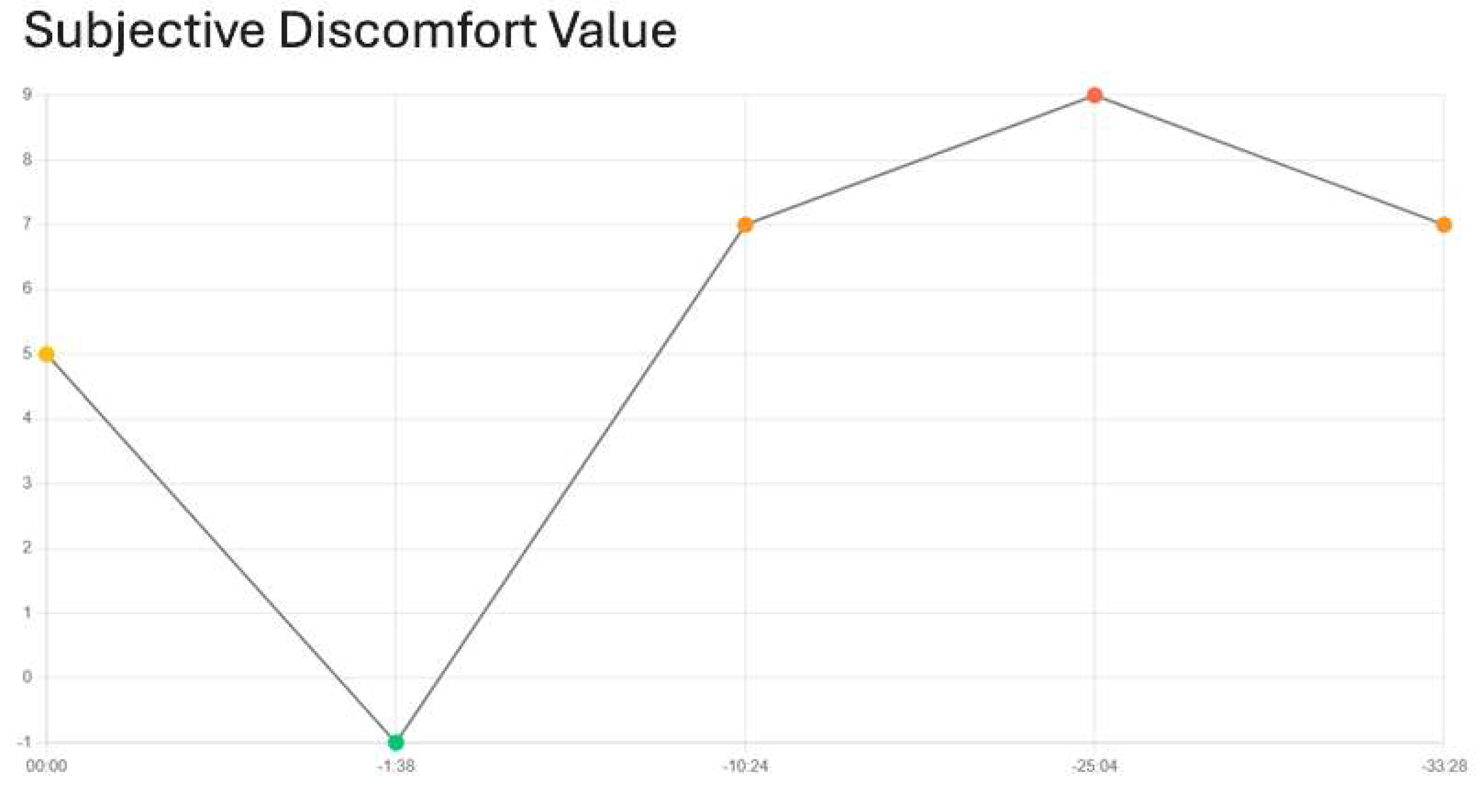
2.4.4. Perceived Discomfort Score
The platform offers a scoring scale from 1 to 10 (
Figure 5) to evaluate the degree of perceived discomfort experienced by the patient in the virtual scenario. The mental health professional can launch this scale into the scenario, allowing the patient to assess and record their level of discomfort in real time. A higher score indicates a greater perception of discomfort. This score is automatically stored on the platform for subsequent analysis and monitoring.
2.4.5. Sociodemographic and Clinical Variables
Sociodemographic and clinical variables were collected, including age, diagnosis, sex, and medication (antidepressants: yes/no; anxiolytics: yes/no; antipsychotics: yes/no) and body mass index (BMI).
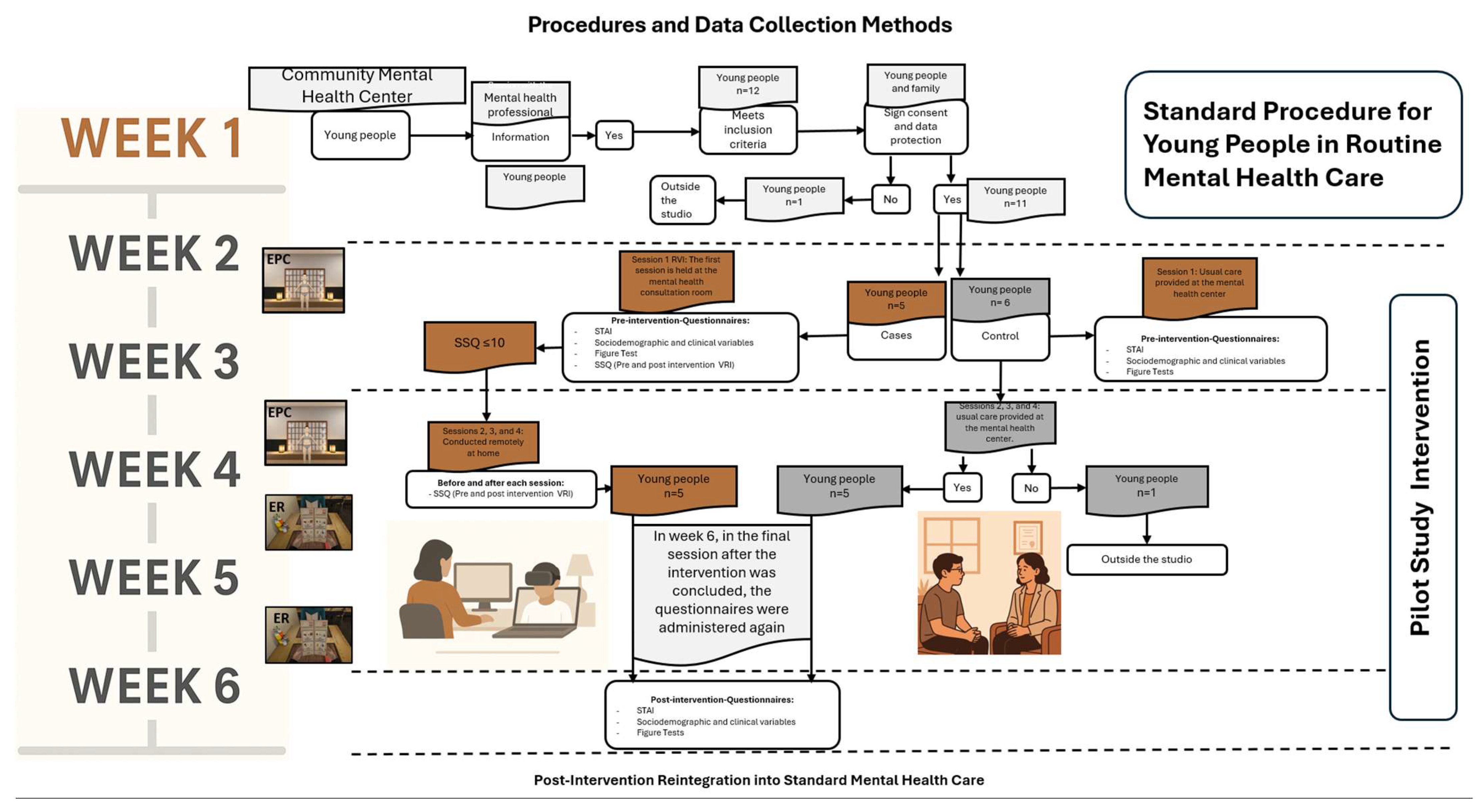
2.5. Procedure
The intervention began in July 2024 with the first participant and concluded in February 2025 (
Figure 6). Each patient completed a total of four sessions of immersive virtual reality (IVR) or standard therapy, depending on the group, at a rate of one session per week. In the control group, participants continued with their usual treatment at the eating disorders unit. This standard care consisted of alternating weekly visits with psychiatry, psychology, and nursing staff, providing regular clinical monitoring and support throughout the 6-week period. Participant recruitment was conducted during nursing and psychology consultations at the mental health center. Once participation in the study was accepted, informed consent was obtained, and the assigned visits for the intervention were communicated. Each participant remained in the study for 6 weeks.
Table 1 presents the structured timeline of the six-week pilot intervention based on RVI.
The first week consisted of recruitment and document management (consent and visit management).
In the second week, coinciding with the first session, questionnaires were administered, and variables were collected. A brief user manual was developed to facilitate the autonomous use of the immersive virtual reality (IVR) system at home. The guide provided clear, step-by-step instructions about activating the 5G router, powering on the headset, pairing the controllers, and accessing the virtual environment. It also included directions for sharing the session code with the supervising clinician, navigating the menu, and safely exiting the application. Additionally, participants were instructed on how to charge the headset and controllers using a USB connection, with LED indicators confirming the battery status. This protocol aimed to minimize technical difficulties and promote adherence throughout the intervention.
From the third to the fifth week, the interventions continued, and, in the sixth week, participants were scheduled for a follow-up visit, where the questionnaires were readministered and variables were collected again. At that time, the corresponding material was provided. In the first IVR session, the STAI scales and the body silhouette test were applied, and anthropometric measurements were taken. Before and after the IVR intervention, the SSQ was administered. Although the previous literature discourages the assessment of cybersickness before virtual reality exposure due to the risk of increasing patient concern, this study followed more recent recommendations that advocate for its prior evaluation, as proposed in [
31], in order to identify individual susceptibility and enhance the intervention’s safety.
The first session in the experimental group took place at the mental health center, in the presence of the professional team, to evaluate individual tolerance to IVR and the risk of cybersickness. This initial in-person phase ensured the suitability of the treatment before starting remote sessions. Tolerance was considered adequate when the SSQ score was within an acceptable range of discomfort, between 5 and 10 points, according to criteria established in previous reviews [
23]. Good tolerance to the intervention allowed subsequent sessions to be conducted remotely. These were carried out at the participants’ homes, with real-time support through specific software integrated into the center’s visit management system, which included video calls. To ensure optimal connectivity during the sessions, each participant was provided with a Wi-Fi connection kit with 5G technology.
During the IVR intervention, two scenarios were worked on. In both scenarios, there were no sudden movements; the person was either standing or seated, depending on the scenario, and only moved their arms and hands slightly to modify the scenarios and answer questions using sensors.
Most actions were performed with the controllers held in their hands. This design feature is expected to mitigate cybersickness symptoms. The exposure time to VR varied depending on the case, although it was attempted not to exceed the 20 min recommended by the protocol. The scenes were progressively adapted to each patient based on the criteria of perceptual distortion, gradual tolerance, and emotional safety.
At the end of their 6-week inclusion in the pilot study, participants continued with their usual treatment.
3. Results
The following section presents the results of the pilot study using a combination of technical, descriptive, and inferential analyses. Depending on the nature of the variables, different measures of central tendency were applied: mean values were used in some cases, while medians were reported in others. This approach allowed for a more accurate and meaningful representation of the data.
First, we assessed the feasibility of the intervention, focusing on software functionality, connectivity, and remote implementation. Then, descriptive statistics were used to summarize participant characteristics, clinical profiles, and usability observations. To evaluate therapeutic effects, we conducted within-group comparisons (pre- vs. post-intervention) using the Wilcoxon signed-rank test and Cohen’s d to estimate the magnitude of changes. Between-group comparisons (VR vs. control) were performed using the Mann–Whitney U test and rank-biserial correlations as effect sizes. In addition, we examined anxiety percentile trajectories based on STAI norms, cybersickness symptoms (SSQ) across sessions, and self-reported discomfort ratings in the two virtual exposure scenarios.
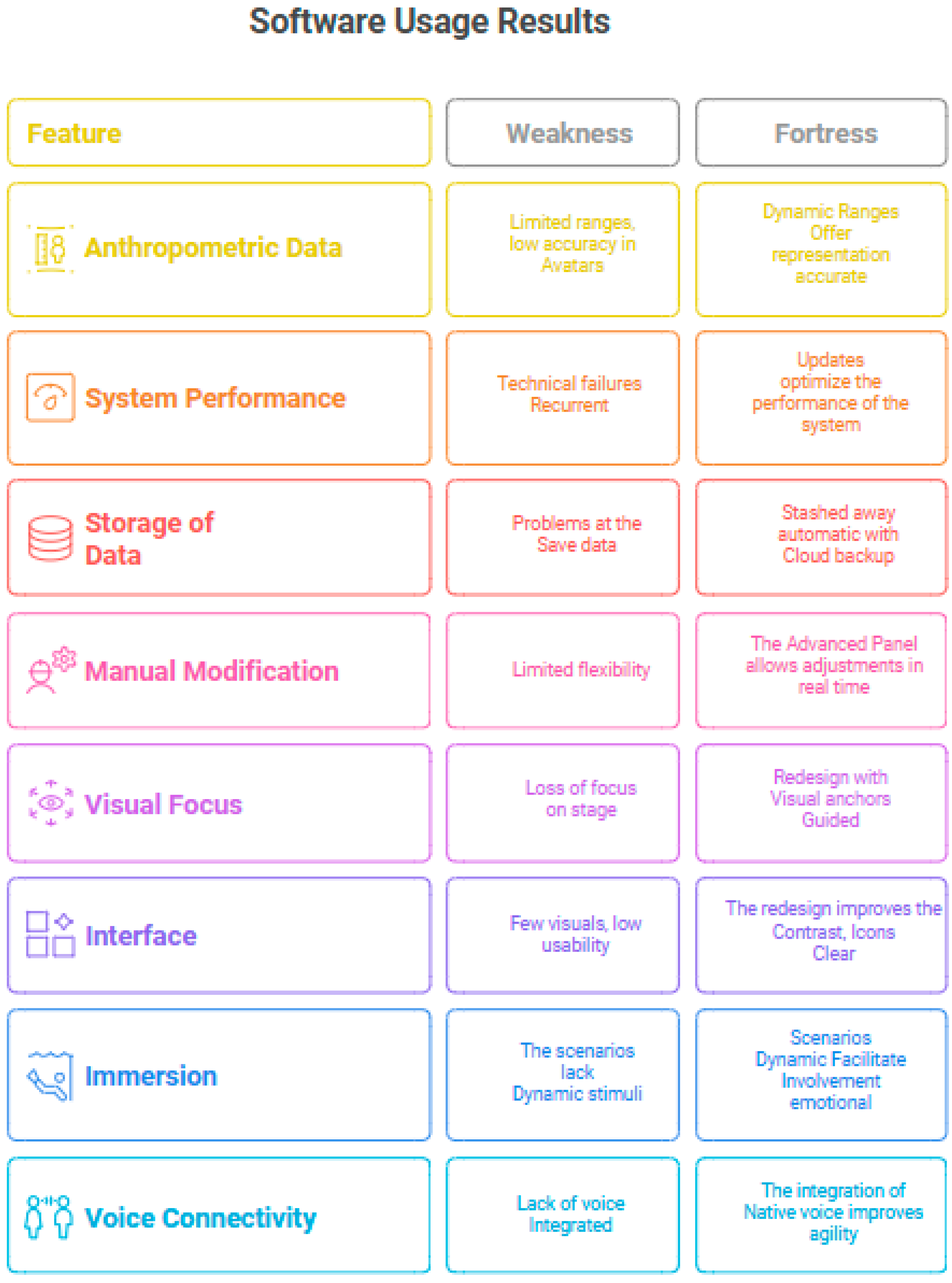
The results obtained in this pilot study provide a preliminary assessment of the feasibility and effectiveness of the intervention. Feasibility was evaluated based on technical aspects such as connectivity, software usage, and the development of remote sessions. On the other hand, therapeutic effectiveness was analyzed based on changes in measured psychological variables, as well as acceptance, tolerance, and perceived improvements by the participants.
Some stability issues were detected in the software (
Figure A4), and there were certain restrictions related to anthropometric representation ranges. For example, the height of the patient could not be less than 1.60 m, and any values outside these standards could not be selected. Similarly, the BMI had excessively large ranges. The interface was understandable but had room for improvement in navigation and graphical loading, and there was a need for more dynamic and emotionally connected scenarios. Regarding the connectivity of the 5G Wi-Fi kit for remote connection with participants, it remained stable during the sessions.
The total sample consisted of nine adolescent females and one adolescent male, with a median age of 15.5 ± 1.2 years. Fifty percent of the participants were undergoing treatment with antidepressants, while 20% were receiving anxiolytics. Regarding clinical diagnoses, anorexia nervosa was the most frequent, present in 50% of the total sample, followed by other unspecified eating disorders in 30% and bulimia nervosa in 20% (two cases).
The table below presents the median (Md) and standard deviation (SD) values of the different dimensions of the body mass index (BMI) before and after the intervention, both for the total sample and for the case and control groups (
Table 2). In the total population (
n = 10), a slight increase in the actual BMI was observed, from a median of 21.7 kg/m
2 ± 5.7 to 22.8 ± 5.3 kg/m
2 in the post-intervention phase. In the Figure Rating Test, the perceived BMI increased from 19.0 ± 1.6 to 23.0 ± 3.2, while the desired BMI decreased from 25.0 ± 2.3 to 20.0 ± 1.4. The healthy BMI remained practically stable (21.0 pre and post). In the case group (
n = 5), the actual BMI moderately increased after the intervention (21.4 → 22.5), and the perceived BMI decreased from 25.0 ± 3.3 to 23.0 ± 4.4.
The desired BMI remained unchanged (19.0 in both phases), while the healthy BMI increased from 19.0 ± 1.7 to 21.0 ± 1.4, aligning with the healthy values of the control group. Conversely, in the control group (n = 5), the actual BMI remained stable (23.5 in both phases). A slight decrease in the perceived BMI was also observed, from 25.0 ± 0.9 to 23.0 ± 1.8, with no changes in the desired BMI (21.0) or healthy BMI, which remained constant at 21.0.
BMI-related variables were compared within each group (VR and control) using the Wilcoxon signed-rank test for paired samples, and Cohen’s d was computed to assess the magnitude of the change, based on individual participant data (
Table 3). In the case group, moderate to large effect sizes were observed for the actual BMI and healthy BMI, suggesting a trend toward meaningful changes post-intervention, despite the lack of statistical significance. The perceived and desired BMIs showed small or negligible effects. In the control group, no statistically significant changes were observed, and all effect sizes were small or negligible.
Group differences in BMI-related outcomes (actual BMI, perceived BMI, Desired BMI, and healthy BMI) were analyzed pre- and post-intervention using the Mann–Whitney U test.
Table 4 presents the results of these comparisons. None of the BMI measures showed statistically significant differences between the VR and control groups (all
p > 0.05). For each comparison, we report the U statistic,
p-value, and effect size (r).
None of the BMI-related variables showed statistically significant differences between the VR and control groups, either before or after the intervention. However, some effect sizes suggested potentially meaningful trends. Participants in the VR group tended to have slightly higher actual BMI values and a different perception of what constituted a healthy BMI. While the perceived BMI remained similar between groups, the desired BMI showed some differences, although these were not statistically significant.
These preliminary patterns suggest that the intervention may influence certain aspects of body perception, but larger samples are needed to confirm this.
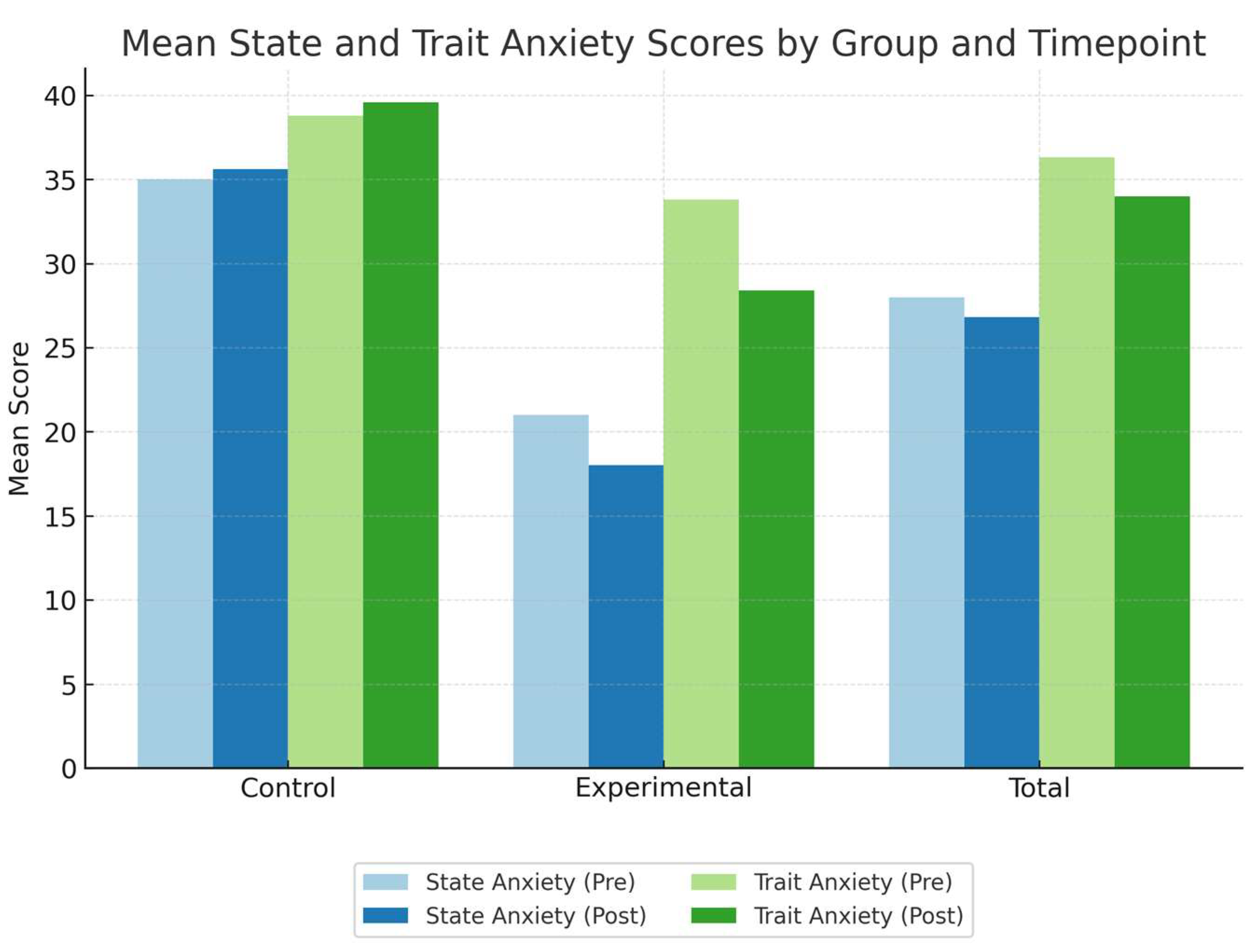
For state anxiety, the experimental group showed a reduction in mean scores (
Figure 7), decreasing from 21.0 (SD = 10.75) before the intervention to 18.0 (SD = 15.94) after. In contrast, the control group experienced a slight increase, from 35.0 (SD = 7.35) to 35.6 (SD = 8.05). For trait anxiety, a similar pattern was observed: the experimental group’s mean scores decreased from 33.8 (SD = 9.98) to 28.4 (SD = 15.04), whereas the control group showed a slight increase, from 38.8 (SD = 11.23) to 39.6 (SD = 10.16).
To facilitate the comparison of the results obtained with the percentiles proposed by the authors of the STAI questionnaire, linear interpolation was performed on the mean score. This technique allowed for the estimation of values corresponding to the cut-off points defined in the original scale, thus ensuring a more precise and coherent comparison with the established standards (
Table 5).
The interpolated percentile values revealed a general reduction in state and trait anxiety scores in the experimental group, with the pre-intervention percentiles ranging from the 40th to 85th and the post-intervention values showing consistent decreases. In contrast, the control group showed stable or slightly increased percentiles over time. These percentile estimates provide a standardized interpretation of the score changes relative to normative adolescent female data.
Wilcoxon signed-rank tests were conducted to assess pre–post changes in state (AS) and trait (AT) anxiety within each group (
Table 6). No statistically significant differences were observed in any condition. In the case group, a small reduction in state anxiety and a moderate to large reduction in trait anxiety were detected, although neither reached significance. In the control group, changes in both dimensions were minimal.
Effect sizes were estimated using Cohen’s d for paired samples. The direction and magnitude of the observed changes are summarized in the table below.
To compare anxiety outcomes between the experimental and control groups at both the pre- and post-intervention time points, we conducted Mann–Whitney U tests for the state and trait anxiety scores. Rank-biserial correlation coefficients were calculated to estimate effect sizes. The results are summarized in the table below (
Table 7).
Between-group comparisons of the state and trait anxiety scores revealed no statistically significant differences between the experimental (VR) and control groups, either before or after the intervention. Although all comparisons showed non-significant p-values, the effect sizes suggested moderate to large differences, especially for post-intervention measures. Notably, participants in the experimental group tended to show lower anxiety scores after the intervention, as indicated by the direction and magnitude of the rank-biserial correlations.
Regarding symptoms of cybersickness (SSQ) in the four sessions of the case group, the median scores indicate a general trend of decreasing discomfort across sessions: Session 1 (3 ± 3.51), Session 2 (1 ± 1.92), Session 3 (1 ± 1.09), and Session 4 (1 ± 0.50). Despite this downward trend in median values, the median SSQ score slightly increased from 1.95 in the first phase to 2.47 in the last phase. This apparent contradiction was due to a single participant reporting a localized increase in symptoms during the final session, which influenced the central tendency despite overall low symptom levels. Importantly, all SSQ scores remained within the range considered as minimal or clinically insignificant, suggesting that the intervention was generally well tolerated (
Table 8). The session duration had a Md of 24:06 min and an SD of 8:06 min.
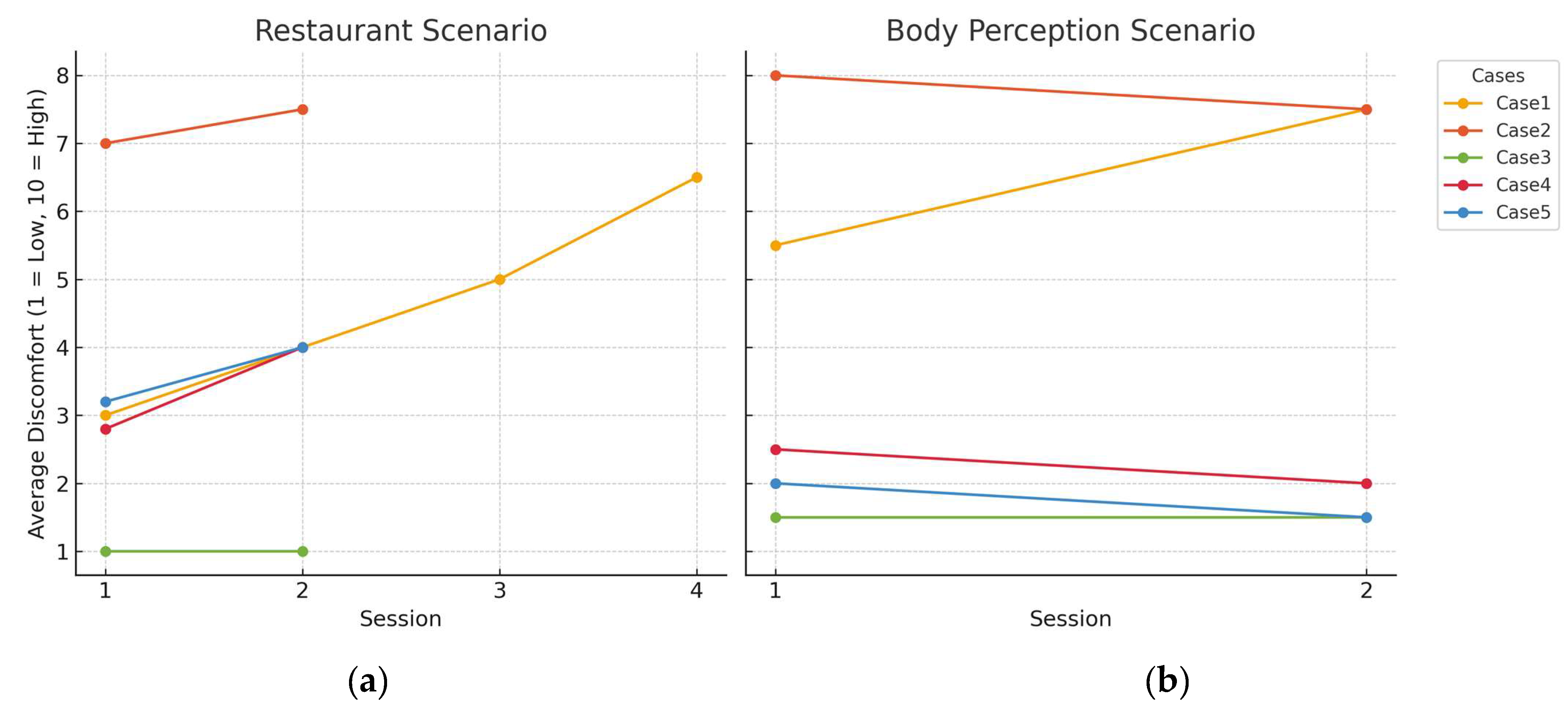
Figure 8 displays the progression of perceived discomfort across VR sessions in two scenarios: a restaurant setting and a body perception experience. Each line represents an individual from the experimental group. Case 1 shows a steady increase in discomfort, suggesting high emotional sensitivity to both scenarios. Case 2 maintains a high discomfort level, particularly in the body scenario. Cases 3, 4, and 5 report consistently low to moderate discomfort across sessions. This figure highlights the diverse emotional responses among participants and underlines the importance of tailoring the pace and content of therapeutic exposure to individual tolerance levels.
4. Discussion
This exploratory pilot study, with a quasi-experimental design and control group, provides a preliminary assessment of the applicability and tolerability of a virtual reality (VR)-based intervention to address body perception and anxiety levels in adolescents. Given the exploratory nature of the study and the small sample size, the results should be interpreted with caution, as they reflect initial trends and we sought to test the feasibility of the tool rather than evaluate its definitive clinical efficacy. The main findings are discussed below.
Regarding viability and technical aspects, the findings reaffirm the importance of developing user-centered technological solutions adapted to clinical diversity and therapeutic contexts [
19,
20]. The intervention was carried out remotely and benefited from the stable connectivity provided by the 5G Wi-Fi kit, which ensured smooth and uninterrupted sessions. This demonstrates the feasibility of remote therapy, overcoming geographical barriers and potentially enhancing participant comfort and adherence. Cybersickness levels were generally low and decreased over time, indicating good physical adaptation to the virtual environment. Although a single participant experienced an increase in symptoms in the last session, all scores remained in the negligible range, supporting the physical feasibility of the intervention. This approach allowed for the observation that scores did not start from zero and, contrary to what might be feared, did not generate concern or hypervigilance in the participants [
23].
Software limitations were also observed, such as height and BMI configuration restrictions, reduced navigation fluidity, and a lack of emotionally resonant scenarios. These observations highlight areas for technical improvement to enhance user engagement and therapeutic relevance.
In line with the existing literature, the composition of the sample in this study—nine females and one male— reflects the widely documented distribution in eating disorders, with an approximate female-to-male ratio of 9:1, as reported in [
7], which highlights the marked overrepresentation of females in these disorders.
The imbalance in our sample was not intentional but reflects the actual clinical profile of patients attending the mental health center during the recruitment period.
The average age of the sample in this study was 15.5 years, a figure that aligns with recent research indicating a growing trend towards the earlier onset of eating disorders (EDs) [
3]. Compared to previous studies, which placed the average age between 15 and 19 years [
1], these results point to a shift in the clinical profile towards younger ages, which could reflect greater vulnerability in the young adolescent population, especially in the current social and digital context. Half of the sample in this study was undergoing pharmacological treatment, specifically with anxiolytics and/or antidepressants [
13]. Although the evidence on the specific efficacy of pharmacotherapy in eating disorders (EDs) [
32] remains limited and inconclusive, various studies agree that these drugs are part of first-line therapeutic approaches, especially when EDs are accompanied by comorbidities such as anxiety or depression. Their use reflects the need to comprehensively address associated symptoms and stabilize the patient’s emotional state during the therapeutic process.
Regarding the representation of diagnoses, anorexia nervosa was the most frequent diagnosis, followed by other unspecified eating disorders and bulimia nervosa. This composition is consistent with clinical evidence indicating the greater diagnostic visibility of anorexia nervosa in specialized healthcare contexts [
4]. These preliminary data capture the heterogeneity of EDs in the adolescent population.
Statistical analyses using Wilcoxon tests and Cohen’s d showed that, although none of the changes reached statistical significance, some moderate to large effect sizes were observed in the VR group. These results suggest potential clinical relevance, particularly in the actual and healthy BMI dimensions. However, given the small sample, these trends should be interpreted cautiously.
The present pilot study explored changes in state and trait anxiety levels before and after the intervention, comparing both the experimental and control groups. While no statistically significant differences were observed in any within-group comparisons, the direction and magnitude of the changes offer preliminary insights.
In the experimental group, a reduction was observed in both state and trait anxiety scores following the intervention. This decrease was more marked for trait anxiety, where the effect size suggested a moderate to large change [
13,
15,
22]. Although these findings did not reach statistical significance, possibly due to the limited sample size, they may suggest that the intervention could influence not only temporary anxiety states but also more persistent patterns like trait anxiety. These results suggest that controlled virtual exposure may help to promote more adaptive responses to emotionally challenging situations, by allowing participants to engage with anxiety-inducing content in a safe and structured setting [
21].
In contrast, the control group showed minimal variation in both state and trait anxiety between pre- and post-assessments, with negligible effect sizes and non-significant results. The stability of the scores in the control group helps to contextualize the reductions observed in the experimental group, reinforcing the need for further research to examine the potential effects of the intervention.
Taken together, these initial findings suggest a possible trend toward anxiety reduction following the intervention, particularly in trait anxiety [
10]. However, given the exploratory nature of the study and the small sample, these results must be interpreted with caution.
Immersive VR for food exposure has allowed the recreation of environments that typically trigger anxiety or dysfunctional eating behaviors, offering a safe and controlled space for the progressive confrontation of these stimuli. In this context, the intervention facilitated the therapist’s precise identification of underlying fears and specific situations generating discomfort, allowing for the design of an intervention that was more tailored to the individual needs of each patient.
The gradual use of virtual environments with increasing levels of emotional activation proved useful in exploring individual emotional reactions and working on factors involved in avoidance or discomfort related to food. This strategy not only allowed for addressing the fear of food and associated discomfort but also could favor a reduction in episodes of loss of control over eating in the case of bulimia nervosa.
Additionally, the potential of this technique is reinforced by the key role of prediction errors, which emerge when discrepancies occur between the patient’s expectations and real experiences in the virtual environment. This mechanism can facilitate the reorganization of cognitive and emotional patterns related to eating, contributing to improved emotional regulation and perceptions of control [
10].
In relation to body exposure, it allowed for the capture of spontaneous reactions, constituting a clinically relevant starting point, as it enabled the therapist to explore perceptual distortions more explicitly and work from the direct experience of the body. The perceived discrepancy acted as a therapeutic trigger, facilitating awareness of the divergence between the real body and the perceived body and offering a safe context to initiate interventions focused on body image reconstruction. Body perceptions are constructed in a constant comparison process based on experiences stored in memory. These findings reinforce the potential of immersive VR as a useful tool to generate prediction errors and provoke updating processes in the internal body model, reinforced with real-time multisensory body integration [
22]. In both scenarios, heterogeneous emotional profiles were observed. Some cases presented high and sustained discomfort, while others showed progressive tolerance. This diversity emphasizes the need to individualize interventions and suggests that repeated exposure could induce habituation mechanisms.
Although the preliminary results are promising, it is important to consider the potential biases arising from the small and heterogeneous sample. One of the limitations of this pilot study is the non-randomized assignment of participants to the case and control groups. Allocation was based on the order of arrival at the mental health center and conditioned by the duration of the software license. This convenience sampling approach may have introduced selection bias, and the results should be interpreted with caution. Another limitation concerns the gender composition of the sample, which included nine females and only one male. Although this reflects the typical gender distribution in eating disorder cases, it restricted our ability to explore gender-related differences in response to the intervention.
Future studies should aim for more balanced recruitment or stratified analysis to examine potential disparities in how males and females engage with immersive VR therapy. The diagnostic differences among participants may have influenced their emotional responses to the intervention. For instance, adolescents with anorexia nervosa may respond differently to IVR compared to those with bulimia nervosa or other eating disorders. Additionally, the small sample size limits the generalizability of the results and suggests the need for future studies with larger and more homogeneous samples. These should include larger samples, integrate qualitative components, and leverage more advanced technologies. Another important limitation to consider is the limited range of anthropometry in the software used, which could have affected the accuracy of body representations for some participants. It is essential to improve these technological tools to enhance the precision, interactivity, and personalization of future interventions. These technological limitations may have influenced the participants’ body perceptions and, consequently, the results of the intervention.
Therefore, this study provides preliminary evidence supporting the feasibility of the proposed approach and justifying the expansion of the experimental design. Additionally, the remote implementation of the intervention—without connectivity incidents thanks to the use of 5G technology—reinforces its feasibility in rural contexts or with limited access to healthcare resources, opening new possibilities for more equitable, accessible, and personalized care.
5. Conclusions
This pilot study evaluated the feasibility, tolerability, and therapeutic potential of a remotely delivered immersive virtual reality (IVR) intervention for adolescents with eating disorders (EDs). Despite the small sample size, the preliminary results reveal meaningful patterns related to body perception, anxiety, and emotional responses to virtual exposure.
The IVR group showed a reduction in anxiety levels following the sessions, particularly in trait anxiety. This decrease may suggest a positive impact of the intervention, potentially reflecting the benefits of repeated exposure to emotionally relevant scenarios in a safe and controlled virtual environment. While preliminary, these results align with the expected outcomes of therapeutic approaches aimed at reducing anxiety through structured experiential learning.
The observed reduction in anxiety levels within the IVR group, particularly in trait anxiety, suggests that immersive interventions may contribute to emotional regulation in individuals with eating disorders. These findings support the potential therapeutic value of controlled virtual exposure in facilitating adaptive responses to emotionally challenging content.
Future studies should incorporate structured support strategies to enhance treatment adherence and further examine how the pacing and content of the intervention can be tailored to individual emotional profiles. This may be particularly relevant during initial sessions, when emotional activation is likely to occur.
Beyond its clinical implications, this study introduces an innovative intervention model that integrates remote immersive technology as a complementary component in the treatment of eating disorders. The remote delivery format proved feasible even in geographically isolated areas with limited access to specialized care. This approach holds promise in expanding the reach of mental health services, reducing geographic and socioeconomic disparities, and advancing toward more equitable, accessible, and person-centered treatment pathways.