Featured Application
This study supports the employment of the Elastic Force Evaluation Bracelet to measure tensile force and time under tension in lower- and upper-limb exercises performed with elastic bands.
Abstract
(1) Background: Several tools have been proposed to measure elastic band tension and time under tension (TUT) during elastic band exercise performance. However, current methods are often indirect, non-objective, or expensive. The Elastic Force Evaluation Bracelet (EFEB) is a simple, wearable system designed to estimate both variables. Therefore, the aim of this study was to evaluate the concurrent validity and test–retest reliability of the EFEB as a portable measurement device for application in a therapeutic exercise context. (2) Methods: Thirty-five healthy volunteers were recruited. Exercises with elastic bands were performed on the dominant upper and lower limbs in two sessions with a one-week interval between them, and peak elastic force values were obtained. Validity was assessed in the first session by comparing the force values obtained simultaneously using a force gauge, and the TUT compared to a linear encoder. Test–retest reliability was examined by comparing the measurements obtained between the two sessions. (3) Results: EFEB showed excellent correlation with the force gauge for elastic force (r = 0.883 for shoulder abduction and r = 0.981 for knee extension) and with the linear encoder for TUTs (r = 0.873 and r = 0.883, respectively). EFEB showed good levels of reliability for all four of the following parameters measured: elastic force for shoulder abduction and knee extension (ICC = 0.880 and 0.855, respectively), and TUT in both movements (ICC = 0.768 and 0.765, respectively). (4) Conclusions: In conclusion, EFEB is a valid and reliable device for the measurement of TUT during shoulder abduction and knee extension exercises performed with elastic bands.
1. Introduction
Therapeutic exercise is widely recognized as the most evidence-based intervention for the recovery and prevention of musculoskeletal and neuromotor conditions amenable to physical rehabilitation [1,2]. Among the modalities of therapeutic exercise, resistance training has demonstrated significant clinical efficacy, particularly when it is dosed based on the individual’s habitual physical activity, physical function, injury characteristics, irritability, stage of healing, exercise responses, stated goals, and personal factors, thereby minimizing the risk of adverse effects [1,3].
Therefore, exercise prescription variables such as type, frequency, intensity, and duration are critical determinants of successful rehabilitation outcomes [4]. These variables are typically managed by physiotherapists in supervised clinical settings where training quality and adherence can be optimized. Even so, the need for face-to-face attendance in this modality reduces adherence, as patients must go to the centre and incur additional financial costs. In response to this, home-based programs are increasingly favoured for their accessibility, cost-effectiveness, and potential to enhance patient engagement, self-efficacy, self-care, and adherence [5,6,7].
Resistance training is characterised by offering different ways of applying load during exercise practice, where elastic bands have gained popularity due to their low cost, portability, adaptability to different environments, and suitability for progressive loading [8,9]. Training with elastic bands is unique because the resistance varies as the band is stretched, providing a curvilinear load profile throughout the entire movement [10]. This characteristic allows for progressive overload and adaptation, making elastic bands suitable for a wide range of populations and exercise settings [11,12]. Among the most critical variables in elastic band training are the elastic force—determined by the degree of band stretch and its material properties—and the time under tension (TUT), understood as the cumulative duration during which an elastic band is under mechanical load throughout a repetition, essential for optimizing therapeutic outcomes [13,14]. Accurate monitoring of these variables is essential, as they directly influence the intensity and effectiveness of the training stimulus [15].
The importance of elastic force lies in its direct role as the primary source of resistance during exercise, dictating the mechanical load applied to muscles and thus driving strength adaptations [11]. TUT, on the other hand, captures the temporal dimension of the stimulus, with longer TUTs being associated with greater increases in muscle protein synthesis and strength development [16]. Together, these variables allow practitioners to fine-tune exercise dosage for rehabilitation or performance goals.
Several tools have been proposed to measure elastic band tension and TUT during exercise. However, current methods are often indirect, lack objectivity, or require expensive laboratory equipment [17]. Tensile dynamometers, for example, measure the force within the band but do not account for biomechanical factors such as joint angles or the direction of applied force. Similarly, sensors engaged in the elastic band can track elongation and estimate TUT but cannot directly quantify tensile load [17]. Given that, and the importance of accurate load quantification to ensure appropriate progressive overload, there is clearly a need for practical, cost-effective, and reliable tools to monitor real-time force and TUT, particularly in home-based or minimally supervised settings. Such devices would enhance objectivity in therapeutic exercise monitoring and could contribute to more reproducible treatment outcomes. In response to this need, the Elastic Force Evaluation Bracelet (EFEB) has been developed as a simple, wearable system designed to estimate and monitor actual tensile force and TUT during elastic resistance exercises. The EFEB attaches to the user’s wrist or ankle (depending on the limb involved) and calculates applied force and TUT using input parameters such as limb lever length, initial band length, and the angle of incidence at the start of the exercise. The device integrates an inertial measurement unit (IMU) with custom firmware, which captures angular motion in real time and allows the computation of band elongation and joint movement through trigonometric models. These values are converted into tensile force and TUT using manufacturer-based regression equations and pre-defined movement thresholds.
Despite EFEB’s practical potential, it has not yet been validated against standard measurement tools, and its reliability remains unknown. Therefore, the main aim of this study was to evaluate the concurrent validity of the EFEB as a portable measurement device for application in a therapeutic exercise context and its reliability when used autonomously without supervision by physiotherapists.
2. Materials and Methods
2.1. Design
To determine the concurrent validity and reliability of the EFEB, exercises with elastic bands were performed on the dominant upper and lower limbs in two sessions with a one-week interval between them. During these tests, peak elastic force values were obtained at the end of the range of motion (ROM) and the TUT of each repetition. Validity was assessed in the first session by comparing the force values obtained simultaneously using a force gauge and the TUT compared to a linear encoder, both of which are MuscleLab 4020e devices (Ergotest Technology AS, Porsgrunn, Norway) and which are linked to their ML6000 Data Synchronization Unit (DSU).
Reliability was examined by comparing the measurements obtained between the two sessions, the first one supervised by a physiotherapist and the second one performed by the participants autonomously (Figure 1). The examiner was a physiotherapist with more than 12 years of experience in strength measurement devices and elastic band exercises.
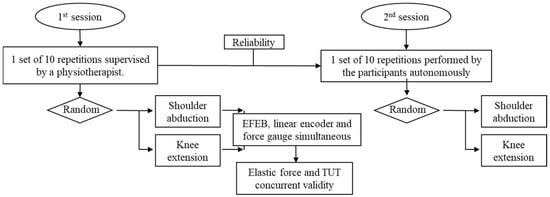
Figure 1.
Flow chart represents a process of the study.
2.2. Participants
Thirty-five healthy volunteers engaged in recreational physical activity were included in the study [15]. Inclusion criteria required that participants were aged 18–30 years, had no upper- or lower-extremity injuries or pain in the year prior to the study, and performed at least 90 min of physical activity per week. The experimental protocol was approved by the Ethics Committee of the University of Valencia (Spain) (2023-FIS-2811071). Once the study procedures had been explained to the participants in detail, they signed an informed consent and completed the demographic information sheet prior to data collection.
2.3. Procedures
Prior to the measurements, participants were instructed to refrain from engaging in any strenuous physical activity during the preceding 48 h. The evaluation session began with a standard warm-up, which consisted of walking up and down several flights of stairs and performing weight-free shoulder abductions.
Shoulder abduction and knee extension exercises using elastic bands were evaluated under a common training scenario characterized by a 0–90° range of motion performed at low velocity. This method was considered representative of traditional strength training protocols. Each repetition followed a fixed timing structure for the three movement phases—concentric, isometric, and eccentric—along with a rest period between repetitions, following a 3/2/3/2 s scheme [15]. The execution velocity for each scenario was guided by a metronome, and participants received verbal cues if they failed to follow the rhythm. The guidelines for performing shoulder abduction were based on previous studies [14] and included the following: (I) feet positioned hip-width apart, (II) 30° of horizontal shoulder flexion, (III) palms facing downward, and (IV) a slight elbow flexion.
For the knee extension exercise, participants were seated on a quadriceps extension machine with 90° hip flexion. An elastic band was perpendicularly anchored to the ankle, approximately 5 cm above the malleoli (Figure 2). EFEB was attached to the ankle brace on the anterior aspect of the tibia or at the wrist.
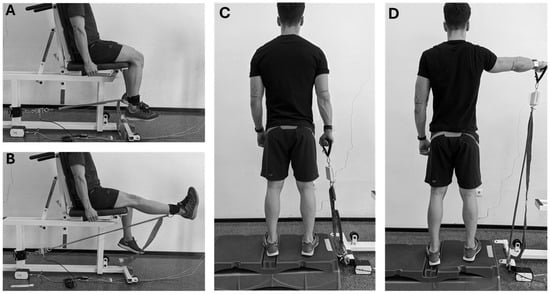
Figure 2.
Knee extension (A,B) and shoulder abduction (C,D) setup using a force gauge anchored to the traction end of the elastic band and a linear encoder to assess velocity and elongation, starting at 90° of hip and knee flexion (A) or 0° of shoulder abduction (C) and reaching maximum knee extension (B) or 90° shoulder abduction (D) and ending in the starting point. EFEB was attached to the ankle brace on the anterior aspect of the tibia or on the wrist.
The order of exercises was randomized using a computerized randomization method. TheraBand CLX elastic bands (The Hygenic Corporation, Akron, OH, USA) were used: blue for shoulder abduction and gold for knee extension, both measuring 40 cm in length (i.e., two loops), as commonly employed in rehabilitation research [18,19,20]. The free end of the elastic band was attached to a handle (abduction) or ankle brace (extension), while the fixed end was secured to the force gauge (Figure 2). Since shoulder abduction exercises are typically performed by stepping on the band [13,14,21], subjects stood on an elevated platform to accommodate the height of the force gauge [15]. Movement velocity and band elongation were assessed using the linear encoder attached to either the handle or ankle (Figure 2). Each participant performed two familiarization trials. Exercises were performed with the elastic band under slight initial tension—just enough to avoid visible wrinkles—and consisted of one set of ten repetitions per exercise, with two minutes of rest between exercises. Movement phases and TUT, as well as force parameters, were calculated using custom-written scripts computed with Python (version 3.13.1; Python Software Foundation). Movement phases were determined based on velocity data: positive for the concentric phase, near-zero for the isometric phase, and negative for the eccentric phase. Once the movement phases were identified, the total repetition TUT (sum of concentric TUT, isometric TUT, and eccentric TUT) and peak tension of elastic force were calculated. The mean values across the ten repetitions for each parameter were computed.
2.4. Elastic Force Assessment Bracelet (EFEB)
EFEB is a bracelet developed from the Liip Smart Monitor bracelet (Liip Care, Valencia, Spain) designed by the ai2 Institute at the UPV (Universitat Politècnica de València, Valencia, Spain) (Figure 3). Thanks to the use of an IMU and the inclusion of individual parameters (e. g. limb length, band and sensor placement, and band type), the device can estimate elastic force applied. It also features dedicated software for recording values via Android app.
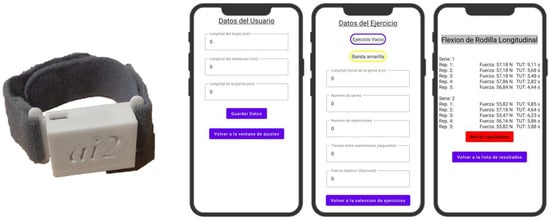
Figure 3.
Elastic Force Evaluation Bracelet and its interface for the Android app. Legend: Datos de usuario: User data; Longitud de antebrazo: Forearm length; Longitud de pierna: Leg length; Guardar datos: Save data; Volver a la ventana de ajustes: Return to settings window; Datos del Ejercicio: Exercise data; Ejercicio Vacio: Empty exercise; Banda amarilla: Yellow band; Longitud inicial de la goma (cm); Numero de series: Number of sets; Numero de repeticiones: Number of repetitions; Tiempo entre repeticiones (segundos): Time between repetitions (seconds); Fuerza objetivo (Opcional): Target strength (optional); Volver a la seleccion de ejercicios: Return to exercise selection; Flexion de Rodilla Longitudinal: Longitudinal knee flexión; Serie: Set; Rep.:repetition; Fuerza: Strength; Borrar resultados: Clear results; Volver a la lista de resultados: Return to results list.
The EFEB integrates the 9-axis IMU sensor (Liip Smart Monitor), which includes a triaxial accelerometer, gyroscope, and magnetometer, with a sampling frequency of 100 Hz and sensitivity ranges of ±16 g (accelerometer) and ±2000°/s (gyroscope). Prior to each use, the device was calibrated. This calibration consisted of taking measurements from the accelerometer and gyroscope sensors for a specific period of time, 20 s, while the wristband was resting horizontally, so that EFEB could calculate the average of the measurements during this period of time, subtracting the value of gravity from the accelerometer, and saving the results as the offset values for each sensor. The IMU data are transmitted via Bluetooth Low Energy to a mobile application, where basic signal smoothing is applied to reduce noise. From the real-time angular measurements, the system estimates joint ROM and computes the instantaneous elongation of the elastic band based on a predefined trigonometric model. Using band-specific regression equations (i.e., Theraband®), the tensile force is calculated, and the muscular force is inferred by applying the sine of the angle between the band and the limb. The equations for the blue elastic band are y = 2 × 10−5·x3 − 0.0047x2 + 0.5683x − 0.6196 and for the gold band y= 8 × 10−5·x3 − 0.018x2 + 1.8375x − 2.7949, where x is the elongation percentage ([final length − initial length]/initial length) and y is the estimated elastic force. TUT is derived by identifying movement direction changes above/below 10% of the target ROM. To calculate the TUT per repetition, the application first monitors whether the instantaneous angle exceeds the threshold of 10% of the target ROM, approximately 90° in this study, thus confirming the participant’s movement and identifying the start of the repetition, saving that exact moment in milliseconds. Secondly, if an instantaneous ROM value of less than 10% of the target ROM is reached again, between 0 and 9 degrees, the end of a repetition is confirmed and the exact moment, in milliseconds, when the repetition ends is saved, with the difference between the two moments (i.e., end minus start) being the resulting TUT per repetition.
2.5. Statistics
Participant characteristics and elastic force values (Newtons) or TUTs (s) are presented as mean ± standard deviation (SD) or percentages, as appropriate. The mean between repetitions was utilized for analysis. Custom-written scripts computed with Python (version 3.13.1; Python Software Foundation) were used to perform all statistical analyses by a researcher blinded to the measurements.
First, for the analysis of the concurrent validity and agreement between EFEB and criterion-tools measurements (force gauge or linear encoder), Pearson’s product moment correlation coefficient (r) with 95% confidence intervals (CI) and Bland–Altmann plots were, respectively, used. Furthermore, we calculated the following: the upper and lower limits of agreement (LoA), the mean, and the SD of the difference between EFEB and criterion tools (in both with absolute difference and percentage term).
Second, for the analysis of the EFEB reliability, indexes of relative reliability—the intraclass correlation coefficient (ICC2,1)—and absolute reliability—the standard error of measurement (SEM) and the minimal detectable change (MDC)—were calculated. ICC2,1 was selected because only one measurement per movement was taken by a single evaluator [22]. Reliability was classified as excellent (ICC > 0.90), good (ICC = 0.76–0.90), moderate (ICC = 0.51− 0.75), and poor (ICC < 0.50) [22,23]. MDC was calculated for the 95% CI as MDC95 = SEM × 1.96 × , where SEM = .
The sample size was calculated using the formula for reliability studies based on confidence intervals (CI) described by Streiner and Norman [24]. With the number of instruments (k) equal to 2, the CI around r (the reliability coefficient) of 0.05, and an estimated r of 0.95, the sample size (n) was calculated as a minimum of 25 participants. The sample size was increased to improve the precision of reliability estimates and reduce measurement error [25].
3. Results
Clinical and sociodemographic characteristics of the participants are showed in Table 1.

Table 1.
Clinical and sociodemographic characteristics of the participants.
3.1. Concurrent Validity and Agreement
EFEB showed excellent correlation and acceptable levels of agreement with both the force gauge for elastic force (r = 0.883; mean difference: 1.08% for shoulder abduction, and r = 0.981; 0.96% for knee extension) and the linear encoder for TUT (r = 0.873; mean difference: 1.62% for shoulder abduction, and r = 0.883; 0.27% for knee extension). Detailed information is presented in Table 2 and Figure 4.

Table 2.
Validity between EFEB and criterion tools for elastic forces and TUTs during shoulder abduction and knee extension exercises.
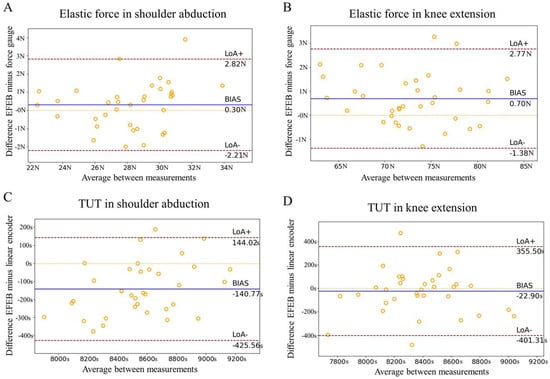
Figure 4.
Bland–Altman plots for EFEB and force gauge (A,B) and EFEB and linear encoder (C,D) for shoulder abduction (A–C) and knee extension (B–D).
3.2. Reliability
EFEB showed good levels of reliability for all four parameters measured: elastic force for shoulder abduction and knee extension (ICC = 0.880 and 0.855, respectively), and TUT for both movements (ICC = 0.768 and 0.765, respectively). According to commonly used classification criteria, ICC values were considered good for elastic forces and for TUTs. In addition, absolute reliability levels were excellent, with SEM percentages of less than 1.61%. Moreover, the MDC remained below 2.1% of the mean values for all parameters. Detailed information is presented in Table 3.

Table 3.
EFEB reliability for elastic force and TUT assessment during shoulder abduction and knee extension exercises performed autonomously.
4. Discussion
The present study showed that EFEB is a valid and reliable device for the measurement of elastic tension and TUT during shoulder abduction and knee extension exercises performed with elastic bands. This investigation is, to our knowledge, the first to evaluate the validity and reliability of the EFEB. The results indicate an excellent correlation between EFEB and the force gauge or linear encoder—the reference standards—and good consistency between the measurements, supporting the utility of the EFEB as a tool for quantifying elastic load and TUT.
Regarding elastic load, our results are particularly notable, matching or exceeding the standards set by previous investigations utilizing elastic bands for maximal strength assessment [26,27]. For instance, Guex, et al. (2015) [27], who compared 1-repetition maximal strength using elastic bands and peak torque on an isokinetic dynamometer, reported very high values of validity and reliability for knee extensors (r = 0.93, ICC = 0.99, respectively) in athletes, which are comparable to ours (r = 0.98, ICC = 0.86). Similarly, Brad et al. (2006) [26] evaluated elbow flexion as a functional upper-limb movement in older adults using a 30 s test against elastic resistance. While their findings supported the use of elastic bands, the validity and reliability coefficients (r = 0.62, ICC = 0.89) [26] were lower and similar, respectively, to those obtained in our investigation (r = 0.87, ICC = 0.88). The MCD values for all parameters measured in this trial were low (e.g., less than 1.8 N or 98 s), suggesting that EFEB is sensitive enough to detect small but potentially meaningful changes in patient performance. Notably, the validity coefficient for knee extension in the present study (r = 0.98) stands out as exceptionally high, suggesting that our protocol may offer improved accuracy in force measurement, particularly for larger muscles. Moreover, although both methods have demonstrated high values of validity and reliability in elbow, shoulder, and knee measurements, our device provides a numerical value, offering a more objective estimate than visual or subjective assessment using elastic bands.
Regarding TUT, the EFEB demonstrated good reliability values, compared to those reported by the only commercially registered device designed for TUT—the Bandcizer [17]. The Bandcizer is a sensor consisting of two parts connected on either side of the elastic band via internal magnets, measuring deformation and thereby the stretch of the band, with data transmitted to a mobile device via Bluetooth [21,28], reporting excellent interrater reliability (ICC > 0.99) [17]. In contrast, the EFEB showed lower but acceptable reliability values (ICC = 0.77) for shoulder abduction and knee extension. The relatively low MDC values suggest the device can be used to monitor meaningful changes over time. A key reason for this discrepancy is the use of different gold standards (linear encoder versus video recording) in the validation procedures, that can significantly affect the resulting reliability coefficients. Furthermore, Bandcizer’s output is directly derived from stretch measurements of the elastic material itself, whereas the EFEB estimates force and TUT based on multi-input parameters, such as limb length and anchor points, which are more sensitive to small input errors. Then, while the EFEB’s multi-input model introduces more potential sources of measurement error—due to its reliance on user-entered anthropometric and setup parameters—it was intentionally designed to reflect the complexity and variability of real-world exercise conditions. This complexity, while posing challenges for precision, also allows for a more personalized and context-aware estimation of force and TUT. However, for applicability, future iterations of the EFEB should aim to reduce user dependency by integrating automatic sensing technologies or default calibration routines. Moreover, differences in sensor technology between EFEB and Bandcizer and placement protocol may contribute to measurement variability, particularly in more complex and ecologically valid testing setups like those employed with the EFEB. Therefore, while the reliability values differ, these differences must be interpreted within the context of the distinct methodological frameworks and reference system used in each case.
All the aforementioned considerations support a broad range of clinical applications for the EFEB. A key clinical advantage of the EFEB lies in its wearable, non-intrusive design, which has been shown to be preferred by both clinicians and patients over devices that attach directly to the elastic band [29]. Devices affixed to the band may alter its mechanical properties—such as stiffness and resistance curve—or restrict the natural range of motion, potentially compromising exercise execution. In contrast, EFEB preserves the integrity of movement while integrating individualized parameters, including limb length, anchor position, and band type, through dedicated software. This enables the estimation of actual user-applied force, rather than relying solely on band deformation [21,30], accounting for biomechanical variables such as joint angles and movement arms that vary with each exercise. Although this multi-parametric approach introduces more potential sources of error, it also enhances ecological validity and relevance to clinical practice. The accompanying software facilitates parameter input and data recording, thereby streamlining workflow, minimizing user error, and supporting routine use outside research settings. Importantly, the second test–retest session in this study was conducted without supervision of a physiotherapist, highlighting the EFEB’s potential for telerehabilitation and remote monitoring applications [31]. Moreover, although previous studies have established the utility of elastic bands for assessing maximal strength in both upper- and lower-limb exercises [26,27], the EFEB expands this potential by enabling accurate quantification of training load and TUT, a key determinant of exercise efficacy [16]. Traditional training logs often fail to capture TUT, potentially underestimating the actual physiology stimulus, even when adherence appears comparable. By offering precise and automated TUT monitoring, the EFEB supports improved prescription, progression, and monitoring of resistance-based interventions. Furthermore, future integration with mobile applications may enable real-time feedback and longitudinal tracking, promoting adherence—a critical factor in therapeutic outcomes [31,32,33]. The device’s capacity to deliver parameter-based notifications—via visual, auditory, or tactile cues—adds an additional layer of user engagement and safety, reinforcing its suitability for widespread clinical and home-based rehabilitation settings. Importantly, the second test–retest session in this study was conducted without physiotherapist supervision, highlighting EFEB’s potential for telerehabilitation and remote monitoring.
Despite all these strengths, the study is subject to several limitations. First, the sample consisted exclusively of healthy young participants, which considerably limits the generalizability of the findings to other populations, such as older adults or individuals with musculoskeletal or neurological conditions. Second, only two movements and one type of elastic band were evaluated, which restricts the ecological validity and the extrapolation of the results to a wider range of exercises, functional tasks, or resistance materials. Third, elastic bands inherently produce a changing direction of resistance throughout the range of motion. In free-space exercises like shoulder abduction, the force vector is only optimally aligned at the beginning of the movement, and this shift may introduce variability that affects the effective training load. Fourth, the use of a linear encoder as the reference standard, as opposed to the video recording employed by Rathleff et al. (2013) [17], may also explain differences in validity metrics between studies. Finally, the laboratory setting used in this study may not accurately reflect real-world or home-based environments, which can introduce additional variability in device performance. Therefore, caution is advised when interpreting the clinical applicability of the EFEB based on this preliminary validation.
Future research should focus on studying the EFEB reliability in clinical populations (e.g., older adults, patients with musculoskeletal or neurological disorder, or paediatric patients), testing its application in home or community setting, and conducting longitudinal studies to assess its impact on functional clinical outcomes. Further development of a notification system—using visual, acoustic, or tactile feedback—could also improve user experience and adherence.
5. Conclusions
In conclusion, EFEB is a valid and reliable device for the measurement of TUT during shoulder abduction and knee extension exercises performed with elastic bands. Its combination of wearable design, multi-axis biomechanical data capture, and integrated software offers distinct advantages over existing devices, particularly for clinical and telerehabilitation applications. While further validation in diverse populations and settings is warranted, the potential of the EFEB to enhance exercise prescription, progression, and monitoring is evident.
Author Contributions
Conceptualization: J.A.-F. and R.M.-S.A.; Data curation; F.J.M.-S.A. and B.T.-C.; Formal analysis: F.J.M.-S.A.; Investigation: J.A.-F. and R.M.-S.A.; Methodology: B.T.-C. and N.M.-S.; Software: F.J.M.-S.A.; Supervision: R.M.-S.A.; Validation: N.M.-S.; Writing—original draft: J.A.-F., R.M.-S.A. and N.M.-S.; and Writing—review & editing: All the authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Valencia (register number 2023-FIS-2811071).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
We thank the volunteers who kindly participated in this study.
Conflicts of Interest
Rodrigo Martín-San Agustín is one of the creators of EFEB, so he was not responsible for or involved in the measurements or statistical analysis.
References
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Fakontis, F.; Kasimis, K.; Lytras, D.; Koutras, G.; Fetlis, A.; Algiounidis, I. Efficacy of Resistance Training with Elastic Bands Compared to Proprioceptive Training on Balance and Self-Report Measures in Patients with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Phys. Ther. Sport. 2023, 64, 74–84. [Google Scholar] [CrossRef]
- Taylor, N.F.; Dodd, K.J.; Shields, N.; Bruder, A. Therapeutic Exercise in Physiotherapy Practice Is Beneficial: A Summary of Systematic Reviews 2002–2005. Aust. J. Physiother. 2007, 53, 7–16. [Google Scholar] [CrossRef]
- ACSM. ACSM’s Guidelines for Exercise Testing and Prescription, 12th ed.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2023. [Google Scholar]
- Jordan, J.L.; Holden, M.A.; Mason, E.E.; Foster, N.E. Interventions to Improve Adherence to Exercise for Chronic Musculoskeletal Pain in Adults. Cochrane Database Syst. Rev. 2010, 2010, CD005956. [Google Scholar] [CrossRef] [PubMed]
- Almarwani, M.; Alosaimi, B. Exercise Self-Efficacy and Fatigue as Predictors of Adherence to Home-Based Exercise Among Patients with Multiple Sclerosis. Patient Prefer. Adherence 2023, 15, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Chen, W.; Xu, S.; Yang, X.; Xue, D.; Peng, Y.; Lin, X.; Yu, Y.; Huang, H.; Huang, P.; et al. Understanding Facilitators and Barriers to Adherence in Home-Based Pulmonary Rehabilitation for Chronic Obstructive Pulmonary Disease Patients Using the Health Belief Model: A Qualitative Study. Front. Public. Health 2025, 2, 1553744. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Sun, Y.; Li, M.; Wang, D.; Ma, X. Effects of Elastic Band Resistance Training on the Physical and Mental Health of Elderly Individuals: A Mixed Methods Systematic Review. PLoS ONE 2024, 19, e0303372. [Google Scholar] [CrossRef]
- de Oliveira, P.A.; Blasczyk, J.C.; Junior, G.S.; Lagoa, K.F.; Soares, M.; de Oliveira, R.J.; Gutierres Filho, P.J.B.; Carregaro, R.L.; Martins, W.R. Effects of Elastic Resistance Exercise on Muscle Strength and Functional Performance in Healthy Adults: A Systematic Review and Meta-Analysis. J. Phys. Act. Health 2017, 14, 317–327. [Google Scholar] [CrossRef]
- McMaster, D.; Cronin, J.; McGuigan, M. Quantification of Rubber and Chain-Based Resistance Modes. J. Strength. Cond. Res. 2010, 24, 2056–2064. [Google Scholar] [CrossRef]
- Fang, Q.; Zhang, X.; Xia, Y.; Huang, F. Integrating Elastic Band into Physical Education Classes to Enhance Strength Training. Front. Psychol. 2023, 14, 1037736. [Google Scholar] [CrossRef]
- Lima, D.P.; de Almeida, S.B.; de Carvalho Bonfadini, J.; Sobreira, E.S.T.; Damasceno, P.G.; Júnior, A.B.V.; de Alencar, M.S.; de Luna, J.R.G.; Rodrigues, P.G.B.; de Sousa Pereira, I.; et al. Effects of a Power Strength Training Using Elastic Resistance Exercises on the Motor and Non-Motor Symptoms in Patients with Parkinson’s Disease H&Y 1-3: Study Protocol for a Randomised Controlled Trial (PARK-BAND Study). BMJ Open 2020, 10, e039941. [Google Scholar]
- McGirr, K.; Harring, S.I.; Kennedy, T.S.R.; Pedersen, M.F.S.; Hirata, R.P.; Thorborg, K.; Bandholm, T.; Rathleff, M.S. An Elastic Exercise Band Mounted with a BandcizerTM Can Differentiate between Commonly Prescribed Home Exercises for the Shoulder. Int. J. Sports Phys. Ther. 2015, 10, 332–340. [Google Scholar]
- Faber, M.; Andersen, M.H.; Sevel, C.; Thorborg, K.; Bandholm, T.; Rathleff, M. The Majority Are Not Performing Home-Exercises Correctly Two Weeks after Their Initial Instruction-an Assessor-Blinded Study. PeerJ 2015, 3, e1102. [Google Scholar] [CrossRef] [PubMed]
- González-Rosalén, J.; Medina-Mirapeix, F.; Cuerda-Del Pino, A.; Moreno-Segura, N.; Gacto-Sánchez, M.; Martín-San Agustín, R. Analysis of Compliance with Time under Tension and Force during Strengthening Exercises with Elastic Bands. Diagnostics 2021, 11, 2016. [Google Scholar] [CrossRef] [PubMed]
- Burd, N.A.; Andrews, R.J.; West, D.W.; Little, J.P.; Cochran, A.J.; Hector, A.J.; Cashaback, J.G.; Gibala, M.J.; Potvin, J.R.; Baker, S.K.; et al. Muscle Time under Tension during Resistance Exercise Stimulates Differential Muscle Protein Sub-Fractional Synthetic Responses in Men. J. Physiol. 2012, 590, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Rathleff, M.S.; Thorborg, K.; Bandholm, T. Concentric and Eccentric Time-Under-Tension during Strengthening Exercises: Validity and Reliability of Stretch-Sensor Recordings from an Elastic Exercise-Band. PLoS ONE 2013, 8, e68172. [Google Scholar] [CrossRef]
- Holmgren, T.; Bjornsson Hallgren, H.; Oberg, B.; Adolfsson, L.; Johansson, K. Effect of Specific Exercise Strategy on Need for Surgery in Patients with Subacromial Impingement Syndrome: Randomised Controlled Study. BMJ 2012, 344, e787. [Google Scholar] [CrossRef]
- Kuhn, J.E. Exercise in the Treatment of Rotator Cuff Impingement: A Systematic Review and a Synthesized Evidence-Based Rehabilitation Protocol. J. Shoulder Elb. Surg. 2009, 18, 138–160. [Google Scholar] [CrossRef]
- Walther, M.; Werner, A.; Stahlschmidt, T.; Woelfel, R.; Gohlke, F. The Subacromial Impingement Syndrome of the Shoulder Treated by Conventional Physiotherapy, Self-Training, and a Shoulder Brace: Results of a Prospective, Randomized Study. J. Shoulder Elb. Surg. 2004, 13, 417–423. [Google Scholar] [CrossRef]
- Rathleff, M.S.; Bandholm, T.; Ahrendt, P.; Olesen, J.L.; Thorborg, K. Novel Stretch-Sensor Technology Allows Quantification of Adherence and Quality of Home-Exercises: A Validation Study. Br. J. Sports Med. 2014, 48, 724–728. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2009; ISBN 978-0-13-171640-7. [Google Scholar]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales; Oxford University Press: Oxford, UK, 2008; ISBN 978-0-19-923188-1. [Google Scholar]
- Mokkink, L.B.; de Vet, H.; Diemeer, S.; Eekhout, I. Sample Size Recommendations for Studies on Reliability and Measurement Error: An Online Application Based on Simulation Studies. Health Serv. Outcomes Res. Methodol. 2022, 23, 241–265. [Google Scholar] [CrossRef]
- Manor, B.; Topp, R.; Page, P. Validity and Reliability of Measurements of Elbow Flexion Strength Obtained from Older Adults Using Elastic Bands. J. Geriatr. Phys. Ther. 2006, 29, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Guex, K.; Daucourt, C.; Borloz, S. Validity and reliability of maximal-strength assessment of knee flexors and extensors using elastic bands. J. Sport. Rehabil. 2015, 24, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Kappel, S.; Rathleff, M.S.; Hermann, D.; Simonsen, O.; Karstoft, H.; Ahrendt, P. A Novel Method for Measuring In-Shoe Navicular Drop during Gait. Sensors 2019, 12, 11697–11711. [Google Scholar] [CrossRef] [PubMed]
- de Beukelaar, T.T.; Mantini, D. Monitoring Resistance Training in Real Time with Wearable Technology: Current Applications and Future Directions. Bioengineering 2023, 10, 1085. [Google Scholar] [CrossRef]
- Fernandez-Gamez, B.; Pulido-Muñoz, Á.; Olvera-Rojas, M.; Solis-Urra, P.; Corral-Pérez, J.; Morales, J.S.; Jiménez-Pavón, D.; Mora-Gonzalez, J.; Esteban-Cornejo, I. Examining Elastic Band Properties for Exercise Prescription: AGUEDA Equations. Physiother. Res. Int. 2025, 30, e70010. [Google Scholar] [CrossRef]
- Russell, T.G. Physical Rehabilitation Using Telemedicine. J. Telemed. Telecare 2007, 13, 217–220. [Google Scholar] [CrossRef]
- Laver, K.E.; Schoene, D.; Crotty, M.; George, S.; Lannin, N.A.; Sherrington, C. Telerehabilitation Services for Stroke. Cochrane Database Syst. Rev. 2020, 1, D010255. [Google Scholar] [CrossRef]
- O’Connor, C.; McNamara, J.; Fahy, K.; Cleary, N.; Deering, P.; McCreesh, K. 32 To Investigate Feasibility of a BandcizerTM Device to Evaluate Adherence to Home Exercise (HEP) for Adults with Shoulder Pain. Br. J. Sports Med. 2019, 53, A11–A12. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).