Assessment of Inspiratory Muscle Function and Glenohumeral Motion in the Throwing Arm of Division I Collegiate Baseball Players
Abstract
1. Introduction
2. Materials and Methods
2.1. TIRE Testing
2.2. Participants
2.3. Procedures
2.3.1. Shoulder Mobility Testing
2.3.2. Test of Incremental Respiratory Endurance (TIRE)
2.4. Statistical Analyses
3. Results
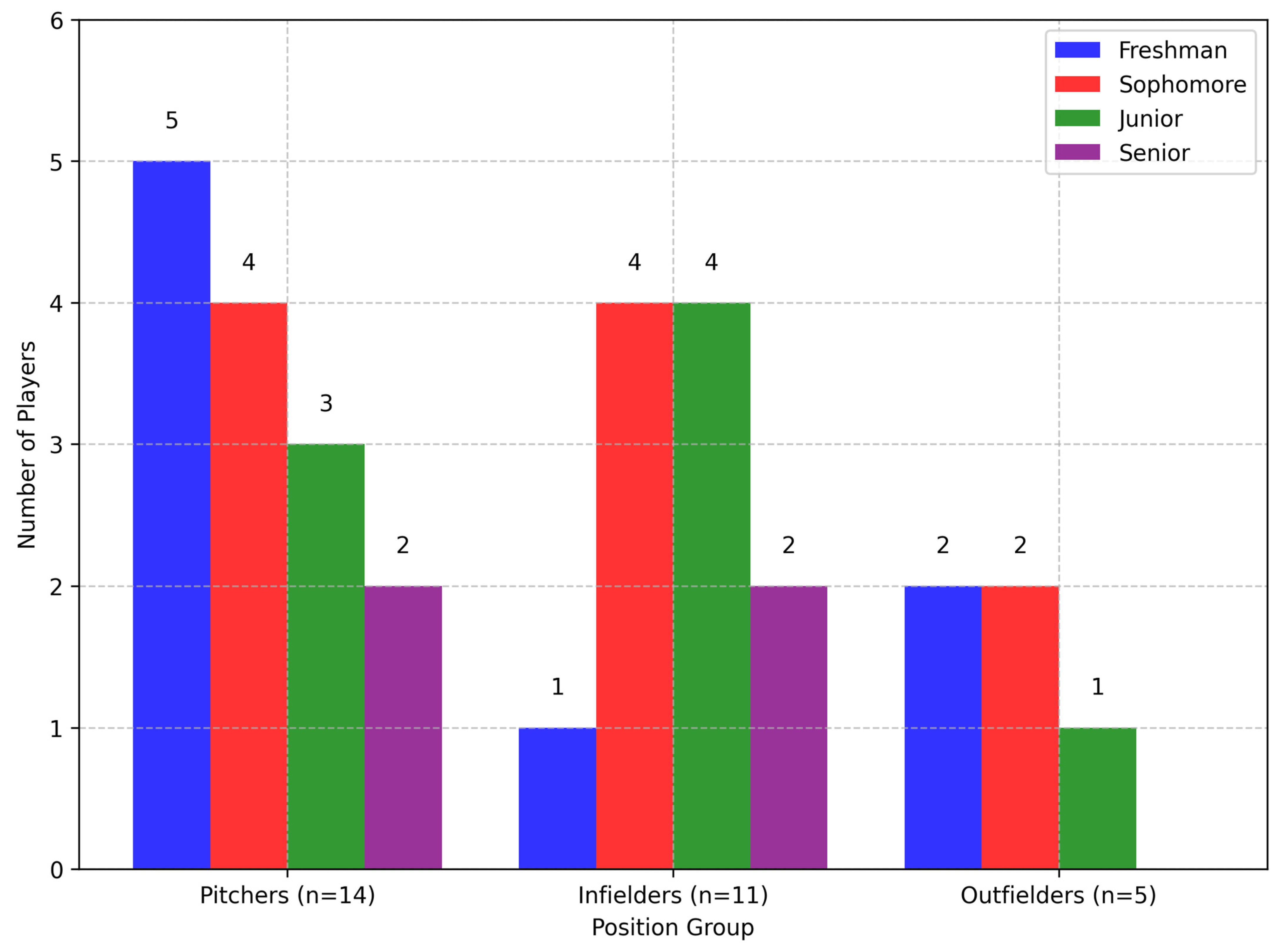
3.1. Descriptive Statistics
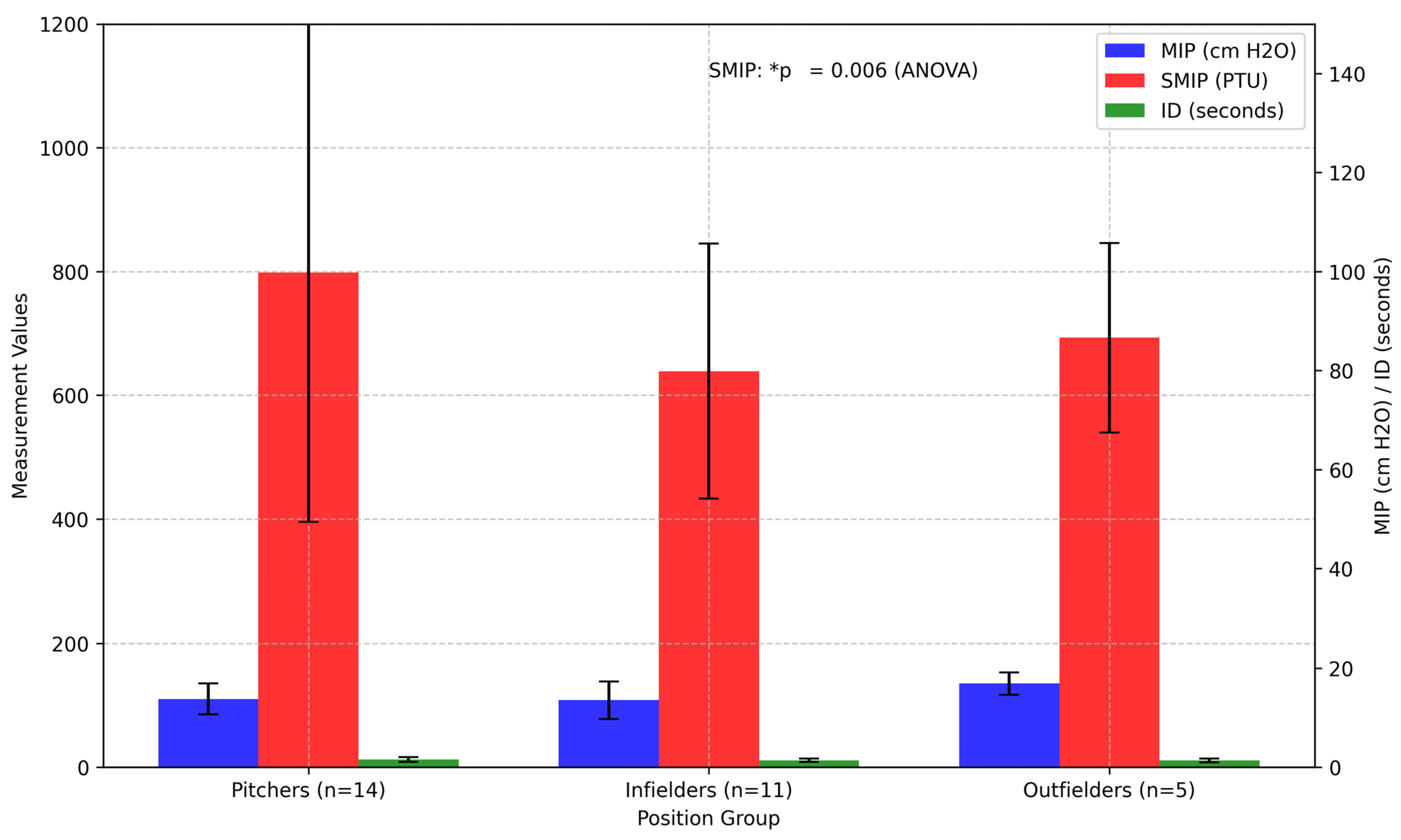
3.2. Between-Group Comparison
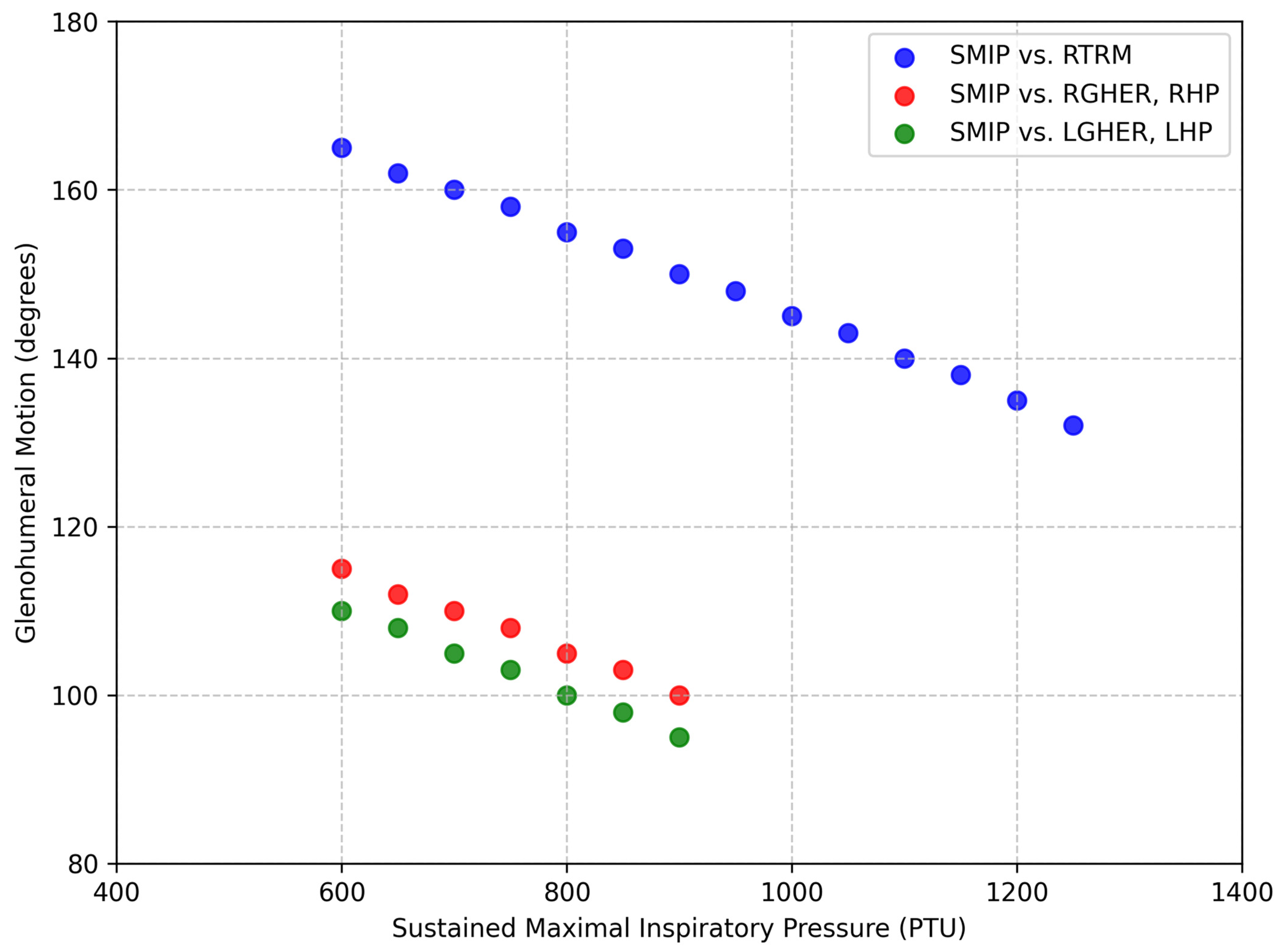
3.3. Correlation Analysis
4. Discussion
4.1. Positional Differences
4.2. Correlations with Anthropometrics
4.3. Correlations with ROM
4.4. Practical Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Escamilla, R.; Andrews, J.R. Shoulder muscle recruitment patterns and biomechanics during upper extremity sports. Sports Med. 2009, 39, 569–590. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D., 2nd; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef]
- Hart, E.; Godek, S.F.; Kulig, K. Inspiratory muscle training in athletes: A systematic review. J. Strength. Cond. Res. 2020, 34, 2353–2361. [Google Scholar]
- Shanley, E.; Rauh, M.J.; Michener, L.A.; Ellenbecker, T.S. Incidence of injuries in high school softball and baseball players. J. Athl. Train. 2011, 46, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Conte, S.; Camp, C.L.; Dines, J.S. Injury trends in Major League Baseball over 18 seasons: 1998–2015. Am. J. Orthop. 2016, 45, 116–123. [Google Scholar] [PubMed]
- Reagan, K.M.; Meister, K.; Horodyski, M.B.; Werner, D.W.; Carruthers, C.; Wilk, K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am. J. Sports Med. 2002, 30, 354–360. [Google Scholar] [CrossRef]
- Manske, R.; Wilk, K.E.; Davies, G.; Ellenbecker, T.; Reinold, M. Glenohumeral motion deficits: Friend or foe? Int. J. Sports Phys. Ther. 2013, 8, 537–553. [Google Scholar]
- Takenaga, T.; Sugimoto, K.; Goto, H.; Nozaki, M.; Fukuyoshi, M.; Tsuchiya, A.; Murase, A.; Ono, T.; Otsuka, T. Posterior shoulder capsules are thicker and stiffer in the throwing shoulders of healthy college baseball players: A quantitative assessment using shear-wave ultrasound elastography. Am. J. Sports Med. 2015, 43, 2935–2942. [Google Scholar] [CrossRef]
- Thomas, S.J.; Swanik, C.B.; Kaminski, T.W.; Higginson, J.S.; Swanik, K.A.; Bartolozzi, A.R.; Nazarian, L.N. Humeral retroversion and its association with posterior capsule thickness in collegiate baseball players. J. Shoulder Elbow Surg. 2012, 21, 910–916. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthroscopy 2003, 19, 404–420. [Google Scholar] [CrossRef]
- Dodds, F.T.; Knotts, S.S.; Penrod, M.I.; Scoggins, W.A.; Conners, R.T. Shoulder strength and range of motion between collegiate pitchers and position players in baseball. Int. J. Exerc. Sci. 2020, 13, 123–130. [Google Scholar] [CrossRef]
- Oyama, S.; Yu, B.; Blackburn, J.T.; Padua, D.A.; Li, L.; Myers, J.B. Effect of excessive contralateral trunk tilt on pitching biomechanics and performance in high school baseball pitchers. Am. J. Sports Med. 2013, 41, 2430–2438. [Google Scholar] [CrossRef]
- Rose, M.B.; Noonan, T. Glenohumeral internal rotation deficit in throwing athletes: Current perspectives. Open Access J. Sports Med. 2018, 9, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; Sciascia, A.; Thomas, S.J. Glenohumeral internal rotation deficit: Pathogenesis and response to acute throwing. Sports Med. Arthrosc. Rev. 2012, 20, 34–38. [Google Scholar] [CrossRef] [PubMed]
- McConnell, A.K. Respiratory Muscle Training: Theory and Practice; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Hart, E.; Kulig, K. Inspiratory muscle performance is significantly related to acceleration and deceleration of isokinetic knee extension and flexion in Division I collegiate women soccer players: A pilot study. Sci 2024, 6, 67. [Google Scholar] [CrossRef]
- Laudner, K.G.; Wong, R.; Meister, K. The influence of lumbopelvic control on shoulder and elbow kinetics in elite baseball pitchers. J. Shoulder Elbow Surg. 2019, 28, 330–336. [Google Scholar] [CrossRef]
- Oliver, G.D.; Plummer, H.; Brambeck, A. The relationship between trunk stability and pitching velocity in NCAA Division I baseball pitchers. J. Strength. Cond. Res. 2016, 30, S45–S46. [Google Scholar]
- Kibler, W.B.; Press, J.; Sciascia, A. The role of core stability in athletic function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Gallego-Gallego, D.; Corchete, L.A.; Fernández Zoppino, D.; González-Bernal, J.J.; García Gómez, B.; Mielgo-Ayuso, J. Inspiratory muscle training program using the PowerBreath®: Does it have ergogenic potential for respiratory and/or athletic performance? A systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 6703. [Google Scholar] [CrossRef]
- McConnell, A.K.; Romer, L.M. Respiratory muscle training in healthy humans: Resolving the controversy. Int. J. Sports Med. 2004, 25, 284–293. [Google Scholar] [CrossRef]
- Tremblay, M.; Anderson Sirois, S.; Verville, W.; Auger, M.; Abboud, J.; Descarreaux, M. Acute Upper-Body and Lower-Body Neuromuscular Fatigue Effect on Baseball Pitchers’ Velocity: A Pilot Study. J. Strength. Cond. Res. 2024, 38, 1447–1452. [Google Scholar] [CrossRef]
- Johnson, A.L.; Kokott, W.; Dziuk, C.; Cross, J.A. Assessment of Muscular Fatigue on Hip and Torso Biomechanics in Adolescent Baseball Pitchers. J. Strength. Cond. Res. 2025. ahead of print. [Google Scholar]
- Witt, J.D.; Guenette, J.A.; Rupert, J.L.; McKenzie, D.C.; Sheel, A.W. Inspiratory muscle training attenuates the human respiratory muscle metaboreflex. J. Physiol. 2007, 584, 1019–1028. [Google Scholar] [CrossRef]
- Sheel, A.W.; Romer, L.M. Ventilation and respiratory mechanics. Compr. Physiol. 2012, 2, 1093–1142. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Chang, H.Y.; Ho, C.C.; Lee, P.F.; Chou, Y.C.; Tsai, M.W.; Chou, L.W. Effects of 4-Week Inspiratory Muscle Training on Sport Performance in College 800-Meter Track Runners. Medicina 2021, 57, 72. [Google Scholar] [CrossRef] [PubMed]
- Ohya, T.; Kusanagi, K.; Koizumi, J.; Ando, R.; Katayama, K.; Suzuki, Y. Effect of Moderate- or High-Intensity Inspiratory Muscle Strength Training on Maximal Inspiratory Mouth Pressure and Swimming Performance in Highly Trained Competitive Swimmers. Int. J. Sports Physiol. Perform. 2022, 17, 343–349. [Google Scholar] [CrossRef]
- Yañez-Sepulveda, R.; Alvear-Ordenes, I.; Tapia-Guajardo, A.; Verdugo-Marchese, H.; Cristi-Montero, C.; Tuesta, M. Inspiratory muscle training improves the swimming performance of competitive young male sprint swimmers. J. Sports Med. Phys. Fitness. 2021, 61, 1348–1353. [Google Scholar] [CrossRef]
- Cirino, C.; Marostegan, A.B.; Hartz, C.S.; Moreno, M.A.; Gobatto, C.A.; Manchado-Gobatto, F.B. Effects of Inspiratory Muscle Warm-Up on Physical Exercise: A Systematic Review. Biology 2023, 12, 333. [Google Scholar] [CrossRef]
- Hodges, P.W.; Gandevia, S.C. Activation of the human diaphragm during a repetitive postural task. J. Physiol. 2000, 522, 165–175. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Barrentine, S.W.; Fleisig, G.S.; Zheng, N.; Takada, Y.; Kingsley, D.; Andrews, J.R. Pitching biomechanics as a pitcher approaches muscular fatigue during a simulated baseball game. Am. J. Sports Med. 2007, 35, 23–33. [Google Scholar] [CrossRef]
- Crotin, R.L.; Conforti, C. A Case Study Exploring the Effects of a Novel Intra-Abdominal Pressure Belt on Fastball and Change-Up Velocity, Command, and Deception Among Collegiate Baseball Pitchers. Appl. Sci. 2024, 14, 10471. [Google Scholar] [CrossRef]
- Lebowitz, M.; Lowell, G.H.; April, M.; Ritchie, Z.; van der Putten Landau, M.; Ehrenberg, M. Case Study: Using Healables® ElectroGear® Wearable E-Textile Sleeve with Embedded Microcurrent Electrodes and WelMetrix® Physiologic Motion Sensors to Enhance and Monitor the Sporting Performance of a Baseball Pitcher. Eng. Proc. 2023, 52, 34. [Google Scholar]
- Cheng, S.C.; Wan, T.Y.; Chang, C.H. The Relationship between the Glenohumeral Joint Internal Rotation Deficit and the Trunk Compensation Movement in Baseball Pitchers. Medicina 2021, 57, 243. [Google Scholar] [CrossRef]
- da Silva, L.S.; da Silva Vieira, R.G.; Wanderley e Lima, T.B.; Resqueti, V.R.; Vilaro, J.; da Fonseca, J.D.M.; Ribeiro-Samora, G.A.; de Freitas Fregonezi, G.A. Effect of Body Position on Electrical Activity of Respiratory Muscles During Mouth and Nasal Maximal Respiratory Pressure in Healthy Adults: A Pilot Study. J. Funct. Morphol. Kinesiol. 2024, 9, 241. [Google Scholar] [CrossRef]
- Deliceoğlu, G.; Kabak, B.; Çakır, V.O.; Ceylan, H.İ.; Raul-Ioan, M.; Alexe, D.I.; Stefanica, V. Respiratory Muscle Strength as a Predictor of VO2max and Aerobic Endurance in Competitive Athletes. Appl. Sci. 2024, 14, 8976. [Google Scholar] [CrossRef]

| Variables | Mean ± SD |
|---|---|
| Age (years) | 20 ± 1.5 |
| Height (cm) | 184.5 ± 5.9 |
| Weight (kg) | 89.1 ± 8.1 |
| Body Mass Index | 26.1 ± 1.7 |
| Maximal Inspiratory Pressure (cm H2O) | 113.4 ± 27 |
| Sustained Maximal Inspiratory Pressure (PTU) | 722.1 ± 309.9 |
| Inspiratory Duration (s) | 11.6 ± 3.5 |
| Right Glenohumeral Internal Rotation (deg) | 54 ± 13.5 |
| Right Glenohumeral External Rotation (deg) | 103.8 ± 12 |
| Right Glenohumeral Total Rotational Motion (deg) | 157.8 ± 15.9 |
| Left Glenohumeral Internal Rotation (deg) | 59.8 ± 13.9 |
| Left Glenohumeral External Rotation (deg) | 98.2 ± 13.3 |
| Left Glenohumeral Total Rotational Motion (deg) | 158.0 ± 18.3 |
| MIP (cm H2O) | SMIP (PTU) | ID (s) | |
|---|---|---|---|
| Pitchers (n = 14) | 110 ± 25 | 798 ± 403 | 12.4 ± 4.2 |
| Infielders (n = 11) | 108 ± 30 | 639 ± 206 | 11.1 ± 2.6 |
| Outfielders (n = 5) | 135 ± 18 | 693 ± 153 | 10.7 ± 3.1 |
| Variable | Full Cohort (n = 30) | Pitchers Only (n = 14) | RHP (n = 7) | LHP (n = 7) |
|---|---|---|---|---|
| Height | r = 0.38, p = 0.008 * | - | - | - |
| Weight | r = 0.42, p = 0.003 * | - | - | - |
| RTRM | r = −0.41, p = 0.004 * | R = −0.56, p = 0.005 * | - | - |
| RGHER | - | - | R = −0.88, p < 0.001 * | ns |
| LGHER | - | ns | R = −0.82, p = 0.04 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feigenbaum, L.A.; Rivera, J.J.; Raya, M.A.; Cohen, M.I.; Kaplan, L.D.; Cahalin, L.P. Assessment of Inspiratory Muscle Function and Glenohumeral Motion in the Throwing Arm of Division I Collegiate Baseball Players. Appl. Sci. 2025, 15, 8815. https://doi.org/10.3390/app15168815
Feigenbaum LA, Rivera JJ, Raya MA, Cohen MI, Kaplan LD, Cahalin LP. Assessment of Inspiratory Muscle Function and Glenohumeral Motion in the Throwing Arm of Division I Collegiate Baseball Players. Applied Sciences. 2025; 15(16):8815. https://doi.org/10.3390/app15168815
Chicago/Turabian StyleFeigenbaum, Luis A., Julian J. Rivera, Michele A. Raya, Meryl I. Cohen, Lee D. Kaplan, and Lawrence P. Cahalin. 2025. "Assessment of Inspiratory Muscle Function and Glenohumeral Motion in the Throwing Arm of Division I Collegiate Baseball Players" Applied Sciences 15, no. 16: 8815. https://doi.org/10.3390/app15168815
APA StyleFeigenbaum, L. A., Rivera, J. J., Raya, M. A., Cohen, M. I., Kaplan, L. D., & Cahalin, L. P. (2025). Assessment of Inspiratory Muscle Function and Glenohumeral Motion in the Throwing Arm of Division I Collegiate Baseball Players. Applied Sciences, 15(16), 8815. https://doi.org/10.3390/app15168815






