Three-Dimensional-Printed Models: A Novel Approach to Ultrasound Education of the Placental Cord Insertion Site
Abstract
1. Introduction
2. Materials and Methods
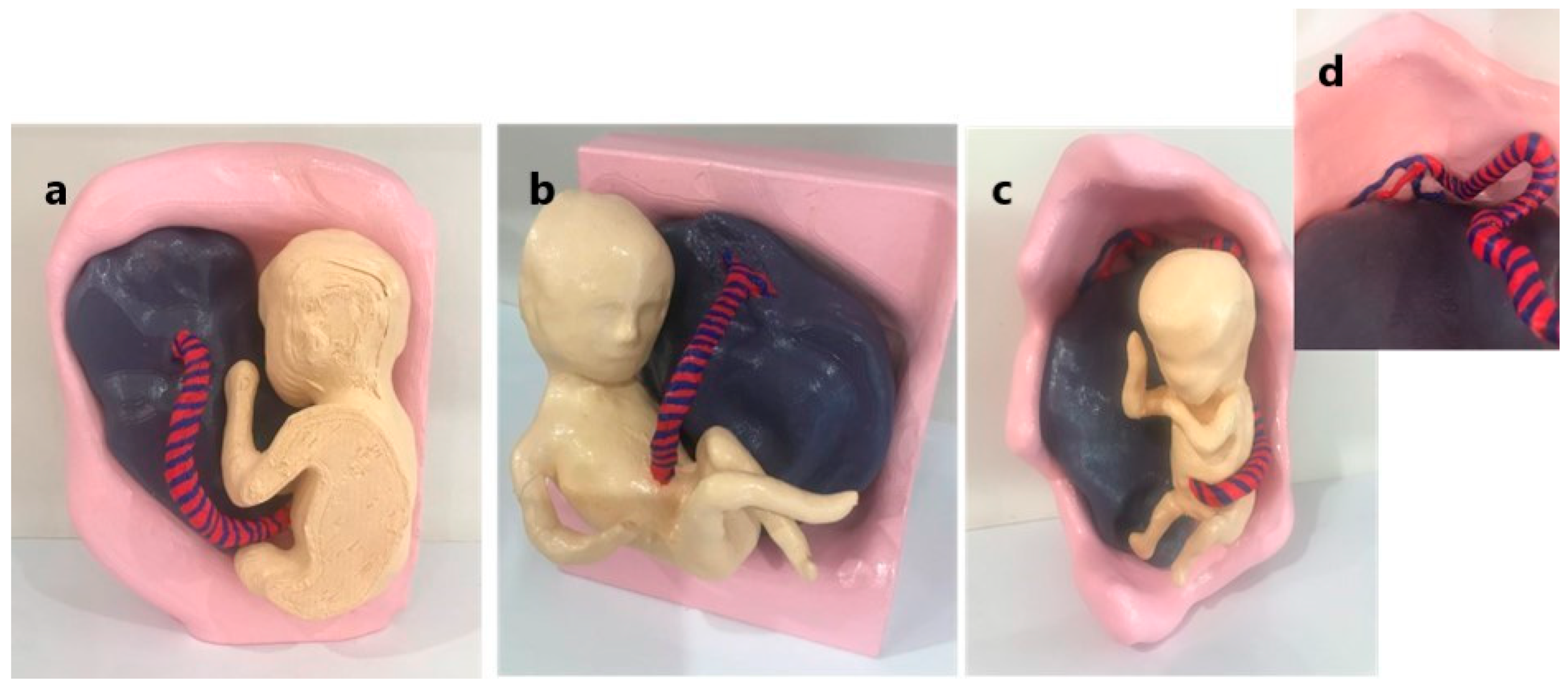
2.1. Three-Dimensional Model Development
2.2. Participant Recruitment and Data Collection
- Informed consent;
- Demographics (years of experience as a sonographer);
- Confidence in assessing the PCI with ultrasound and ability to spatially visualise the placenta and PCI utilising a five-level Likert-scale rating (with 1 indicating extremely poor and 5 indicating excellent).
- Increased confidence in identifying the NCI, MCI, and VCI with ultrasound;
- Improved the understanding of the structural relationship between the placenta and the PCI;
- Enhanced the ability to spatially visualise the placenta and the PCI.
2.3. Statistical Analysis
2.4. Ethics Approval
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ward, S.; Sun, Z.; Maresse, S. Current practice of placental cord insertion documentation in Australia—A sonographer survey. Australas J. Ultrasound Med. 2023, 26, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Allaf, M.B.; Andrikopoulou, M.; Crnosija, N.; Muscat, J.; Chavez, M.R.; Vintzileos, A.M. Second trimester marginal cord insertion is associated with adverse perinatal outcomes. J. Matern Fetal Neonatal Med. 2019, 32, 2979–2984. [Google Scholar] [CrossRef] [PubMed]
- Wax, I.R.; Craig, W.Y.; Pinette, M.G.; Wax, J.R. Second-Trimester Ultrasound-Measured Umbilical Cord Insertion-to-Placental Edge Distacne: Determining an Outcome-Based Threshold for Identifying Marginal Cord Insertion. J. Ultrasound Med. 2020, 39, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Backhouse, S.; Taylor, D.; Armitage, J.A. Is This Mine to Keep? Three-dimensional Printing Enables Active, Personalized Learning in Anatomy. Anat. Sci. Educ. 2019, 12, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Loke, Y.H.; Harahsheh, A.S.; Krieger, A.; Olivieri, L.J. Usage of 3D models of tetralogy of Fallot for medical education: Impact on learning congenital heart disease. BMC Med. Educ. 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Ma, Q.; Zhao, X.; Pan, G.; Zhang, G.; Zhu, B.; Xue, Y.; Li, D.; Lu, B. Feasibility Analysis of 3D Printing With Prenatal Ultrasound for the Diagnosis of Fetal Abnormalities. J. Ultrasound Med. 2022, 41, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Bastawrous, S.; Wake, N.; Levin, D.; Ripley, B. Principles of three-dimensional printing and clinical applications within the abdomen and pelvis. Abdom. Radiol. 2018, 43, 2809–2822. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Yu, L.; Li, H.; Wang, H.; Liang, W.; Wang, H.; Wang, H. Evaluation of placental growth potential and placental bed perfusion by 3D ultrasound for early second-trimester prediction of preeclampsia. J. Assist. Reprod. Genet. 2022, 39, 1545–1554. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; He, H.; Song, T.; Su, C.; Chen, D. Utilizing 3D Printing Model of Placenta Percreta to Guide Obstetric Operation [3D]. Obstet. Gynecol. 2017, 129, 42S. [Google Scholar] [CrossRef]
- Hu, C.; Zhang, W.; Li, P. 3D Printing and Its Current Status of Application in Obstetrics and Gynecological Diseases. Bioengineering 2023, 10, 299. [Google Scholar] [CrossRef] [PubMed]
- You, Y.; Niu, Y.; Sun, F.; Huang, S.; Ding, P.; Wang, X.; Zhang, X.; Zhang, J. Three-dimensional printing and 3D slicer powerful tools in understanding and treating neurosurgical diseases. Front. Surg. 2022, 9, 1030081. [Google Scholar] [CrossRef] [PubMed]
- Kiesel, M.; Beyers, I.; Kalisz, A.; Joukhadar, R.; Wöckel1, A.; Herbert, S.-L.; Curtaz, C.; Wulff, C. A 3D printed model of the female pelvis for practical education of gynecological pelvic examination. 3D Print. Med. 2022, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Recker, F.; Jin, L.; Veith, P.; Lauterbach, M.; Karakostas, P.; Schäfer, V.S. Development and Proof of Concept of a Low-Cost Ultrasound Training Model for Diagnosis of Giant Cell Arteritis Using 3D Printing. Diagnostics 2021, 11, 1106. [Google Scholar] [CrossRef] [PubMed]
- Recker, F.; Remmersmann, L.; Jost, E.; Jimenez-Cruz, J.; Haverkamp, N.; Gembruch, U.; Strizek, B.; Schäfer, V.S. Development of a 3D-printed nuchal translucency model: A pilot study for prenatal ultrasound training. Arch. Gynecol. Obstet. 2024, 310, 2055–2064. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Wong, Y.H.; Yeong, C.H. Patient-Specific 3D-Printed Low-Cost Models in Medical Education and Clinical Practice. Micromachines 2023, 14, 464. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Wee, C. 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines 2022, 13, 1575. [Google Scholar] [CrossRef] [PubMed]
- Wittek, A.; Strizek, B.; Recker, F. Innovations in ultrasound training in obstetrics. Arch. Gynecol. Obstet. 2024, 311, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Yasli, M.; Dabbagh, S.R.; Tasoglu, S.; Aydin, S. Additive manufacturing and three-dimensional printing in obstetrics and gynecology: A comprehensive review. Arch. Gynecol. Obstet. 2023, 308, 1679–1690. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawlowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals-Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed]
- Traynor, G.; Shearn, A.I.; Milano, E.G.; Ordonez, M.V.; Nieves, M.; Forte, V.; Caputo, M.; Schievano, S.; Mustard, H.; Wray, J.; et al. The use of 3D-printed models in patient communication: A scoping review. J. 3D Print. Med. 2022, 6, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Squelch, A.; Sun, Z. Investigation of the Clinical Value of Four Visualization Modalities for Congenital Heart Disease. J. Cardiovasc. Dev. Dis. 2024, 11, 278. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Koniordou, D.; Gasparini, M.; Capelli, C.; Leaver, L.-K.; Khambadkone, S.; Schievano, S.; Taylor, A.M.; Wray, J. Piloting the Use of Patient-Specific Cardiac Models as a Novel Tool to Facilitate Communication During Cinical Consultations. Pediatr. Cardiol. 2017, 38, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Li, Y.; Yu, K.; Liu, L.; Fu, J.; Yao, X.; Zhang, A.; He, Y. 3D Printing of Physical Organ Models: Recent Developments and Challenges. Adv. Sci. 2021, 8, 2101394. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Gupta, A.; Ihdayhid, A.; Sun, Z. Clinical Applications of Mixed Reality and 3D Printing in Congenital Heart Disease. Biomolecules 2022, 12, 1548. [Google Scholar] [CrossRef] [PubMed]
- Coté, J.J.; Coté, B.P.; Badura-Brack, A.S. 3D printed models in pregnancy and its utility in improving psychological constructs: A case series. 3D Print. Med. 2022, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Coté, J.J.; Thomas, B.; Marvin, J. Improved maternal bonding with the use of 3D-printed models in the setting of a facial cleft. J. 3D Print. Med. 2018, 2, 97–102. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using GPower 3.1: Tests for correlation and regression analyses. Behav. Res. Methods. 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Sun, Z. Dimensional accuracy and clinical value of 3d printed models in congenital heart disease: A systematic review and meta-analysis. J. Clin. Med. 2019, 8, 1483. [Google Scholar] [CrossRef] [PubMed]
- Young, J.C.; Quayle, M.R.; Adams, J.W.; Bertram, J.F.; McMenamin, P.G. Three-Dimensional Printing of Archived Human Fetal Material for Teaching Purposes. Anat. Sci. Edu. 2019, 12, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, H.; Hansen, K.; Nørgård, M.Ø.; Wang, T.; Pedersen, M. From tissue to silicon to plastic: Three-dimensional printing in comparative anatomy and physiology. R. Soc. Open Sci. 2016, 3, 150643. [Google Scholar] [CrossRef] [PubMed]
- Hadeed, K.; Acar, P.; Dulac, Y.; Cuttone, F.; Alacoque, X.; Karsenty, C. Cardiac 3D printing for better understanding of congenital heart disease. Arch. Cardiovasc. Dis. 2018, 111, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Pan, Z.; Wu, Y.; Gu, Z.; Li, M.; Liang, Z.; Zhu, H.; Yao, Y.; Shui, W.; Shen, Z.; et al. The role of three-dimensional printed models of skull in anatomy education: A randomized controlled trail. Sci. Rep. 2017, 7, 575. [Google Scholar] [CrossRef] [PubMed]
- Halpern, S.A.; Brace, E.J.; Hall, A.J.; Morrison, R.G.; Patel, D.V.; Yuh, J.Y.; Brolis, N.V. 3-D modeling applications in ultrasound education: A systematic review. Ultrasound Med. Biol. 2022, 48, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wang, Z.; Jiang, H.; Han, B.; Tang, J.; Kang, C.; Zhang, N.; Xu, Y. Full color 3D printing of anatomical models. Clin. Anat. 2022, 35, 598–608. [Google Scholar] [CrossRef] [PubMed]
- WFUMB/ISUOG. WFUMB/ISUOG Statement on the Safe Use of Doppler Ultrasound During 11–14 Week Scans (or Earlier in Pregnancy). Ultrasound Med. Biol. 2013, 39, 373. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.E.; Biffi, B.; Sivera, R.; Dall’Asta, A.; Fessey, L.; Wong, T.-L.; Paramasivam, G.; Dunaway, D.; Schievano, S.; Lees, C.C. Developing and testing an algorithm for automatic segmentation of the fetal face from three-dimensional ultrasound images. R. Soc. Open Sci. 2020, 7, 201342. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.; Ding, C.; Xu, H.; Huang, T.; Kang, D.; Wang, D. Three-Dimensional Printed Models in Anatomy Education of the Ventricular System: A Randomized Controlled Study. World Neurosurg. 2019, 125, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Awori, J.; Friedman, S.D.; Howard, C.; Kronmal, R.; Buddhe, S. Comparative effectiveness of virtual reality (VR) vs. 3D printed models of congenital heart disease in resident and nurse practitioner educational experience. 3D Print Med. 2023, 9, 2. [Google Scholar] [CrossRef] [PubMed]





| Question Please Rate Your… | Mean (SD) | p-Value | Effect Size η2 |
|---|---|---|---|
| Confidence in assessing PCI with ultrasound | 3.87 (1.01) | 0.005 | 0.28 |
| Confidence in identifying NCI with ultrasound | 4.03 (0.98) | <0.001 | 0.40 |
| Confidence in identifying MCI with ultrasound | 3.79 (1.02) | 0.002 | 0.34 |
| Confidence in identifying VCI with ultrasound | 3.58 (1.03) | 0.002 | 0.35 |
| Ability to spatially visualise placenta and PCI while performing ultrasound | 4.00 (1.00) | 0.17 | |
| Ability to spatially visualise placenta and NCI while performing ultrasound | 4.09 (1.10) | 0.002 | 0.35 |
| Ability to spatially visualise placenta and MCI while performing ultrasound | 3.84 (1.08) | 0.22 | |
| Ability to spatially visualise placenta and VCI while performing ultrasound | 3.55 (1.15) | 0.007 | 0.26 |
| Group 1 vs. Group 2 p-Value (Effect Size η2) | Group 1 vs. Group 3 p-Value | Group 2 vs. Group 3 p-Value | |
|---|---|---|---|
| Confidence in assessing the PCI with ultrasound | 0.002 (0.32) | 0.021 | 0.337 |
| Confidence in identifying NCI with ultrasound | <0.001 (0.39) | 0.026 | 0.104 |
| Confidence in identifying MCI with ultrasound | <0.001 (0.36) | 0.019 | 0.222 |
| Confidence in identifying VCI with ultrasound | <0.001 (0.40) | 0.033 | 0.126 |
| Ability to spatially visualise the placenta and PCI | 0.005 (0.30) | 0.077 | 0.236 |
| Ability to spatially visualise the placenta and NCI | <0.001(0.38) | 0.14 | 0.265 |
| Ability to spatially visualise the placenta and MCI | 0.009 (0.28) | 0.41 | 0.481 |
| Ability to spatially visualise the placenta and VCI | 0.003 (0.34) | 0.02 | 0.433 |
| PCI Type | Ranking 1 n (%) | Ranking 2 n (%) | Ranking 3 n (%) | p-Value | |
|---|---|---|---|---|---|
| NCI | Image | 27 (81.8) | 3 (9.1) | 3 (9.1) | 0.348 |
| Video | 3 (9.1) | 23 (69.7) | 7 (21.2) | 0.785 | |
| Model | 3 (9.1) | 7 (21.2) | 23 (69.7) | 0.862 | |
| MCI | Image | 26 (78.8) | 5 (15.2) | 2 (6.1) | 0.341 |
| Video | 3 (9.1) | 24 (72.7) | 6 (18.2) | 0.824 | |
| Model | 4 (12.1) | 4 (12.1) | 25 (75.8) | 0.452 | |
| VCI | Image | 28 (84.8) | 2 (6.1) | 3 (9.1) | 0.483 |
| Video | 0 | 29 (87.9) | 4 (12.1) | 0.492 | |
| Model | 5 (15.2) | 2 (6.1) | 26 (78.8) | 0.586 |
| Question: Have the 3DPMs Improved Your… | Mean | SD |
|---|---|---|
| Confidence in assessing the PCI with ultrasound | 3.84 | 1.14 |
| Confidence in assessing NCI with ultrasound | 3.73 | 1.28 |
| Confidence in assessing MCI with ultrasound | 3.84 | 1.23 |
| Confidence in assessing a VCI with ultrasound | 4.36 | 0.89 |
| Understanding of the structural relationship between the placenta and NCI | 3.33 | 1.34 |
| Understanding of the structural relationship between the placenta and MCI | 3.82 | 1.26 |
| Understanding of the structural relationship between the placenta and VCI | 4.45 | 0.90 |
| Ability to spatially visualise the placenta and NCI | 3.64 | 1.41 |
| Ability to spatially visualise the placenta and MCI | 3.94 | 1.25 |
| Ability to spatially visualise the placenta and VCI | 4.39 | 1.00 |
| Question: Have the 3D Models Improved Your … | p-Value |
|---|---|
| Confidence in assessing the PCI with ultrasound? | 0.223 |
| Confidence in identifying an NCI with ultrasound | 0.092 |
| Confidence in identifying an MCI with ultrasound | 0.157 |
| Confidence in identifying a VCI with ultrasound | 0.099 |
| Understanding of the structural relationship between an NCI and the placenta | 0.906 |
| Understanding of the structural relationship between an MCI and the placenta | 0.272 |
| Understanding of the structural relationship between a VCI and the placenta | 1.000 |
| Ability to spatially visualise the placenta and an NCI | 0.192 |
| Ability to spatially visualise the placenta and an MCI | 0.714 |
| Ability to spatially visualise the placenta and a VCI | 0.960 |
| Opinions | Mean | SD | p-Value |
|---|---|---|---|
| Do you think the 3D model of the NCI would be useful in ultrasound education? | 4.55 | 0.97 | 0.605 |
| Do you think the 3D model of the MCI would be useful in ultrasound education? | 4.73 | 0.72 | 0.601 |
| Do you think the 3D model of the VCI would be useful in ultrasound education? | 4.97 | 0.17 | 1.000 |
| Would you recommend the 3D model of the NCI as an educational device? | 4.42 | 1.09 | 0.582 |
| Would you recommend the 3D model of the MCI as an educational device? | 4.54 | 0.83 | 0.930 |
| Would you recommend the 3D model of the VCI as an educational device? | 4.81 | 0.39 | 0.622 |
| Theme | Feedback | Total |
|---|---|---|
| Use of 3DPMs of the PCI as educational tools | Useful teaching resources for trainees and junior staff (n = 4) Useful educational tool to explain different types of PCI (n = 2) | n = 6 |
| Improved visualisation of the PCI | Better visualisation and understanding of PCI (n = 6) The VCI model was particularly helpful (n = 2) | n = 8 |
| Extended use of the 3D models | The 3D models could help spatially visualise placental location (n = 1) and placental developmental variations (n = 1) | n = 2 |
| General comments | Could be helpful in explaining our images/videos of the PCI to radiologist (n = 1) Excellent for dyslexic students who require a more visual approach to study (n = 1) The videos and 3D models pair nicely together (n = 1) | n = 3 |
| Limitations | Cost and availability (n = 1) | n = 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ward, S.; Maresse, S.; Sun, Z. Three-Dimensional-Printed Models: A Novel Approach to Ultrasound Education of the Placental Cord Insertion Site. Appl. Sci. 2025, 15, 8221. https://doi.org/10.3390/app15158221
Ward S, Maresse S, Sun Z. Three-Dimensional-Printed Models: A Novel Approach to Ultrasound Education of the Placental Cord Insertion Site. Applied Sciences. 2025; 15(15):8221. https://doi.org/10.3390/app15158221
Chicago/Turabian StyleWard, Samantha, Sharon Maresse, and Zhonghua Sun. 2025. "Three-Dimensional-Printed Models: A Novel Approach to Ultrasound Education of the Placental Cord Insertion Site" Applied Sciences 15, no. 15: 8221. https://doi.org/10.3390/app15158221
APA StyleWard, S., Maresse, S., & Sun, Z. (2025). Three-Dimensional-Printed Models: A Novel Approach to Ultrasound Education of the Placental Cord Insertion Site. Applied Sciences, 15(15), 8221. https://doi.org/10.3390/app15158221







