Abstract
Background: The integration of digital imaging tools in dentistry has transformed clinical workflows, diagnostic accuracy, and patient outcomes. However, less attention has been given to how these tools influence dentists’ self-reported outcomes, including clinical confidence, efficiency, perceived treatment quality, communication, and professional satisfaction. This article aimed at assessing AI-powered digital tools in dentistry and their self-reported impact on dental practitioners’ activity and treatment outcomes. Methods: A comprehensive survey was distributed to 126 dental professionals of different genders, ages, years of experience, and types of dental practice to assess their experiences and attitudes towards AI applications in diagnostics and treatment planning, as well as how patients and dentists perceive the benefits and challenges associated with digital dentistry. Results: Digital photographs and CBCT were regarded as essential tools to have in clinical practice, in contrast with intraoral scanners. However, barriers like high initial costs, specialty differences, and lack of formal training may influence the results. Conclusion: These findings suggest that when used appropriately, AI digital tools can significantly elevate the quality of clinical practice and professional fulfillment and underscore the importance of tailored training programs and supportive infrastructures to facilitate the effective integration of digital technologies in dental practice.
1. Introduction
The integration of digital technologies into dental practice represents a transformative shift, marked by enhanced diagnostic precision, workflow efficiency, and improved treatment outcomes, alongside heightened patient engagement [1]. Innovations such as CAD/CAM systems, digital radiography, and artificial intelligence (AI)-powered diagnostics have become essential components of contemporary dentistry [2,3,4]. These tools support a wide array of functions, from real-time imaging to personalized treatment planning, thereby streamlining clinical workflows and reducing reliance on time-intensive manual procedures [2,3].
While the technical capabilities of AI and other digital technologies are well-documented [5,6], their successful implementation in clinical practice is contingent upon treatment outcomes, as well as the acceptance and engagement of dental professionals. To date, research has predominantly focused on patient-centered outcomes and the operational efficacy of these tools [7,8]. In this context, less attention has been given to the perspectives of clinicians themselves regarding how the use of digital innovations influences their professional experience, clinical decision-making, and satisfaction. Furthermore, technological development in dentistry with AI is occurring faster than the creation of international clinical treatment protocols and guidelines [3], which can also be considered an important gap in the scientific literature.
Self-reported measures such as perceived clinical effectiveness, confidence in decision-making, time efficiency, as well as satisfaction with patient outcomes and professional life are key indicators of a sustainable and high-performing dental practice [9,10]. Despite their importance, the literature lacks information on how the advent of digital tools intersects with these self-reported experiences [1].
To address this gap, the present study aimed to offer a comprehensive analysis of the role of AI-powered digital tools in contemporary dental practice and their implications for future technological integration. We hypothesized that the use of digital technologies is significantly associated with improvements in clinicians’ self-reported outcomes [1,4].
Accordingly, the study’s primary objectives are threefold:
- (a)
- to assess, analyze, and correlate dental clinicians’ self-reported outcomes related to the impact of digital and AI technologies on their clinical activities;
- (b)
- to compare these outcomes between users and non-users of digital imaging tools;
- (c)
- to qualitatively evaluate the experiences and satisfaction levels among practitioners who currently utilize AI-based software applications.
Based on these objectives, the respective null hypotheses were as follows:
- (a)
- dental clinicians’ self-reported outcomes are not significantly correlated with the use of digital and AI technologies in their clinical activities;
- (b)
- users and non-users of digital imaging tools do not differ in self-reported outcomes;
- (c)
- AI-based software applications do not influence clinical experience and satisfaction.
2. Materials and Methods
2.1. Study Design
This study aimed to evaluate dental professionals’ perceptions regarding the integration of AI-powered digital tools, such as intraoral scanners, cone beam computed tomography (CBCT), digital photography, as well as AI software dedicated to digital treatment planning and diagnosis, into contemporary dental practice. For this purpose, a cross-sectional design was adopted to investigate whether the incorporation of these technologies contributes to improved clinical outcomes from the clinician’s perspective [6,11]. By examining how these tools are utilized in daily workflows, the study sought to elucidate their perceived benefits and limitations in enhancing clinical performance and decision-making.
To understand practitioners’ viewpoints, a structured questionnaire was developed, targeting key domains including self-reported job satisfaction, the adoption and utility of AI-enhanced technologies, perceived efficiency in time management and communication, as well as patient expectations and satisfaction [12,13]. This approach aimed to provide a comprehensive understanding of how digital innovation is reshaping professional experiences in dentistry [1].
2.2. Data Collection
This research employed an anonymized survey-based approach using a questionnaire that was conducted on dental practitioners to explore their self-reported perspective regarding the influence of artificial intelligence (AI)-enabled digital technologies on perceived treatment outcomes [11,14]. A questionnaire was chosen as the primary data collection tool after a thorough assessment of alternative methodologies. Due to its simplicity, adaptability, and capacity to collect standardized responses across a large participant pool, the questionnaire proved to be the most effective means for capturing nuanced self-reported professional experiences.
While qualitative methods such as interviews or focus groups may provide rich, in-depth insights, they are not always practical for studies with broader participant representation due to their time and resource demands. The selected survey method allowed for a comprehensive yet efficient data collection process, particularly suitable for subsequent statistical analysis. Anonymous participation further encouraged candid responses regarding professional attitudes and perceptions related to digital technology adoption in dentistry.
The main questionnaire used in this study was previously validated by similar studies [15,16] and structured into three main sections to ensure the collection of both background information and topic-specific insights. The first section gathered demographic and professional data, including age, gender, years of clinical experience, and practice type. These variables were considered essential for contextualizing the responses and identifying potential patterns in attitudes and experiences across different professional profiles.
The further sections present a series of statements (Table 1) addressing key focus areas of the study:

Table 1.
Sections and statements featured in the second subdivision of the questionnaire.
The second section of the questionnaire comprised 16 self-reported items, categorized into five thematic domains: Digital Imaging Tools (4 items), AI Software Usage (1 item), Job Satisfaction (3 items), Time and Communication (4 items), and Patient Expectations (4 items). These categories were designed to assess how different aspects of digital integration influence dentists’ perceptions of their clinical effectiveness, workflow optimization, and patient care quality.
- The Digital Imaging Tools domain included statements addressing the essential role of photographic cameras, intraoral scanners, and CBCT devices in dental clinics, along with a general assessment of satisfaction with available equipment.
- The AI Software domain consisted of a single item, focusing on the use of AI-powered software for diagnostic and treatment planning purposes, consisting of three different qualitative open-ended follow-up questions to identify specific tools, their functions, and rationale for use.
- The Job Satisfaction items explored whether dentists felt they had sufficient time for patient care, satisfaction with their workload, and whether they felt their work was appreciated by patients.
- The Time and Communication cluster assessed the clarity of treatment plan communication with patients, staff, and dental laboratories, as well as the ability to visually present treatment outcomes to patients before starting procedures.
- The Patient Expectations domain included items evaluating the frequency with which patient expectations were met, the quality of dentist–patient relationships, feedback on treatment comfort, and satisfaction with aesthetic results.
All closed-ended items in the second section were rated using a five-point Likert scale: Strongly Agree, Agree, Disagree, Strongly Disagree, and I Don’t Know (which was not included in the statistical analysis). This format enabled the quantification of subjective experiences and attitudes, while also capturing levels of certainty or ambivalence. Respondents were additionally prompted to indicate the directionality of their perceived experience with digital tools, whether trending positively (e.g., from Strongly Disagree to Strongly Agree) or negatively (e.g., from Strongly Agree to Strongly Disagree). In the final section, responses were recorded using a simplified three-point Likert scale (Positive, Neutral, Negative), providing a succinct summary of overall attitudes toward digital integration.
To ensure the instrument’s methodological soundness, a validation process based on Bell’s framework [15] was implemented. A multidisciplinary panel of five experts in digital dentistry, clinical AI integration, occupational health, and research methodology reviewed the preliminary version of the questionnaire and proposed refinements. Following expert validation, a pilot test was conducted with a small cohort of dental professionals to assess clarity, structure, and relevance. Feedback from this trial informed the final revision. [16].
The validated questionnaire was distributed during the 1st Artificial Intelligence in Dentistry Congress—Intelligent Dentistry 2024, held in Faro, Portugal, on 26–27 April. Participation was limited to dental professionals attending the event. All 132 distributed questionnaires were returned, resulting in a 100% response rate. Reliability analysis of the second section, which formed the basis for much of this study’s analysis, demonstrated strong internal consistency, with a Cronbach’s alpha coefficient of 0.88.
Data collection was conducted during and immediately following the conference, resulting in a 100% response rate, with all 132 questionnaires fully completed and returned.
2.3. Participants
A total of 126 dental professionals were included in the final analysis after excluding six responses (4.5%) due to incomplete sociodemographic information. The sample consisted of 71 female participants (56.3%) and 55 male participants (43.7%). Regarding age distribution, 38 participants (30.2%) were between 25 and 35 years old, 50 (39.7%) were aged 36 to 45, and 26 (20.6%) fell within the 46-to-55 age range. Additionally, 12 respondents, representing 9.5% of the sample, were within the 56-to-65 age range.
Regarding professional experience, 28 respondents (22.2%) had between 1 and 5 years of practice, 42 (33.3%) had 6 to 10 years, 32 (25.4%) had 11 to 15 years, and 24 participants (19.1%) had more than 16 years of clinical experience.
Concerning the type of dental practice, 64 respondents (50.8%) were engaged in general dentistry, 35 (27.8%) worked in a specialized practice, 12 (9.5%) were involved in academic or research positions, and 15 participants (11.9%) reported working in other settings, such as freelance practice across multiple clinics.
2.4. Statistical Analyses
Sample size was estimated using the Fisher’s Z test, considering a minimum significant correlation of r = 0.3, with a statistical power of 80% at a 5% level of significance. As a result, a minimum total sample size of 87 participants had previously been considered.
Considering that the data were categorical and non-parametric, Spearman’s rank correlation was used to examine relationships among all variables measured on the Likert scale. Subsequently, variables related to self-reported professional outcomes—specifically those in the Job Satisfaction, Time and Communication, and Patient Expectations sections—were compared between respondents who reported using digital imaging tools and those who did not. These group comparisons were conducted using the Mann–Whitney U test, a non-parametric method suitable for ordinal data.
All statistical procedures were conducted with a significance threshold of 5%, utilizing IBM SPSS Statistics software (Version 24.0 for Macintosh; IBM Corp., Armonk, NY, USA).
2.5. Ethical Aspects
All participants were fully informed of the study’s objectives and voluntarily took part without coercion. The Ethics Committee of CESPU University approved the study (CE/IUCS/CESPU-13/22) on 21 April 2022, ensuring adherence to the highest ethical standards. Informed consent was obtained from all participants, and personal data were anonymized.
3. Results
Normality was rejected for all Likert scale variables (p < 0.001). Therefore, non-parametric test comparisons were used for correlations and group comparisons.
All correlations assessed among Likert scale variables are shown in Table 2. The only statistically non-significant correlation was between Likert scale results for the variables “CBCT is indispensable in the dental clinic” and “my patients value my work”. Direct, very strong correlations were found between the use of photography and communication with staff; between the use of intraoral scanners and communication with the dental laboratory; and between the use of CBCT and showing the result before starting the treatment (Table 2).

Table 2.
Correlations between self-reported outcomes from dentists.
Regarding comparison results, all 12 Likert scale section variables about dental professional activity (listed in Table 2) presented statistically significant differences between users and non-users of clinical digital photography, according to the Mann–Whitney U test (p < 0.001). The greatest difference in median values was found for the variable “I can communicate the treatment plan with clarity to staff” (Figure 1), in which users of photography outperformed non-users regarding self-reported communication with the staff of the clinic.
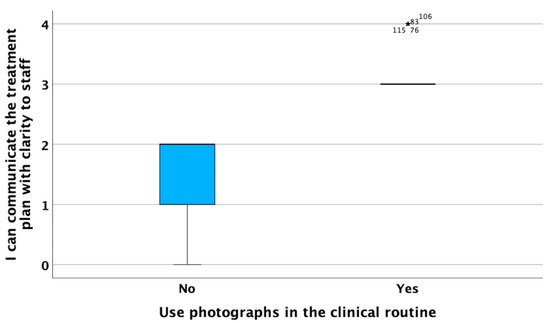
Figure 1.
Likert scale medians and standard deviation of the variable “I can communicate the treatment plan with clarity to staff” for users and non-users of photography (p < 0.001).
Similarly, all 12 Likert scale section variables about dental professional activity also presented statistically significant differences between users and non-users of intraoral scanners. A value of p < 0.001 was found for all variables with the exception of “I have enough time to devote to patients” (p = 0.002) and “I am happy with my current work rate” (p = 0.043). The greatest difference in median values between groups was found for the variables “I can communicate the treatment plan with clarity to the dental laboratory” (Figure 2) and “My patients often like the aesthetic result” (Figure 3). In both cases, intraoral scanner users showed higher median Likert scale values than non-users.
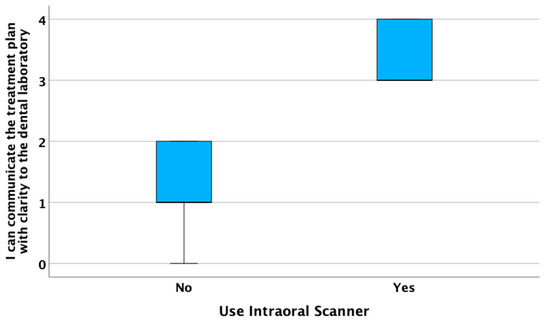
Figure 2.
Likert scale medians and standard deviations of the variable “I can communicate the treatment plan with clarity to the dental technician” for users and non-users of intraoral scanners (p < 0.001).
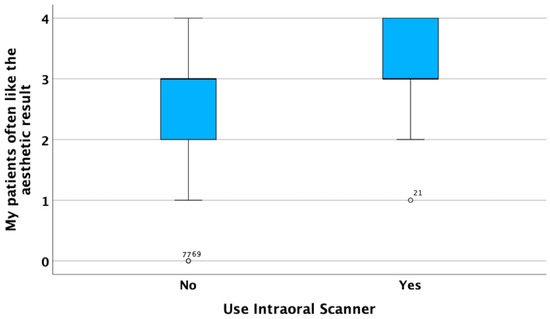
Figure 3.
Likert scale median and standard deviation of the variable “my patients often like the aesthetic result” for users and non-users of intraoral scanner (p < 0.001).
Finally, all Likert scale section variables about dental professional activity also presented statistically significant differences between users and non-users of CBCT (p < 0.001). The greatest difference in median values between groups was found for the variables “I am satisfied with the equipment I have” (Figure 4) and “I can communicate the treatment plan with clarity to my patients” (Figure 5). In both cases, CBCT users showed higher Likert scale values than non-users.
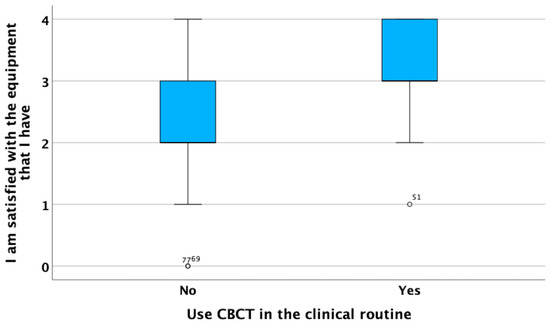
Figure 4.
Likert scale median and standard deviation of the variable “I am satisfied with the dental equipment I have” for CBCT users and non-users (p < 0.001).
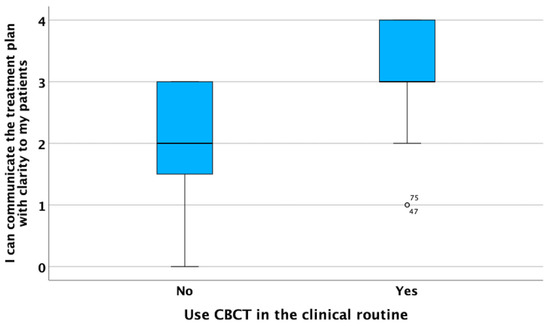
Figure 5.
Likert scale median and standard deviation of the variable “I can communicate the treatment plan with clarity to my patients” for CBCT users and non-users (p < 0.001).
Regarding the use of AI software, most of the users were also CBCT users (Figure 6). The sample size of AI software users was not large enough to run any statistical analyses with adequate statistical power (80%). Qualitative analyses of open-ended questions revealed that AI software was being used for either automated diagnosis or treatment planning (e.g., automated smile designs and tooth library selections). Among the most-used AI software programs for diagnosis were Second Opinion (Developed by Pearl Inc., Beverly Hills, CA, USA) and Diagnocat (developed by Diagnocat Ltd., San Francisco, CA, USA). These software programs were mostly used for the automated diagnosis of caries and periapical lesions. On the other hand, among the most-used AI software programs for treatment planning and dental digital design were Automate (3Shape A/S, Copenhagen, Denmark) and Smilecloud (Smilecloud Biometrics, Timisoara, Romania). These software programs were mostly used for automated digital design of dental prostheses and aesthetic analyses. All AI software users reported working with improved and faster workflows for their respective AI-powered activity (oral diagnosis on radiographic images and/or digital dental designs) since they started using their AI software programs.
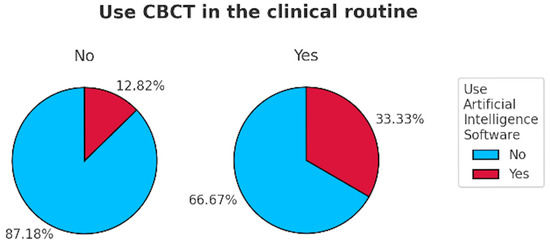
Figure 6.
Pie charts showing the distribution of AI software users in relation to the answers of participants regarding the use of CBCT in clinical practice.
4. Discussion
This study aimed to explore how the integration of digital imaging tools and artificial intelligence (AI) software into dental practice impacts clinicians’ self-reported perceptions of professional performance, communication, treatment quality, and satisfaction. The results offer strong empirical support for the hypothesis that the use of AI-enhanced digital technologies is positively associated with improved professional experiences and clinical confidence among dental practitioners.
4.1. Influence of Digital Imaging Tools on Self-Reported Outcomes
A key finding of this study is the consistent and statistically significant association between the use of digital imaging tools—namely, clinical photography, intraoral scanners, and CBCT—and improved self-reported outcomes across all surveyed domains. These include job satisfaction, perceived equipment adequacy, intra-team and inter-professional communication, and patient-centered indicators such as treatment comfort and aesthetic satisfaction.
Notably, digital photography emerged as a central facilitator of communication within the dental team. This was reflected in the very strong correlation between photography use and the ability to clearly communicate treatment plans to clinical staff (r = 0.985, p < 0.001). Photography also showed strong associations with improved communication with patients, enhanced time management, and greater confidence in clinical outcomes. These findings are in line with a prior study in the literature emphasizing the value of visual documentation in interdisciplinary collaboration, treatment planning, and patient education [1,2,17,18,19].
Intraoral scanners also demonstrated a substantial impact, particularly on communication with dental laboratories (r = 0.985, p < 0.001) and perceived aesthetic treatment results (Figure 3). These results suggest that the high-resolution, real-time visualization capabilities of scanners not only optimize restorative workflows but also align expectations between dentist, patient, and lab technician. These results align with the literature [10,17,18]. However, two items—“I have enough time to devote to my patients” (p = 0.002) and “I am happy with my current workload” (p = 0.043)—showed comparatively lower, though still significant, differences between users and non-users. This may indicate that while scanners enhance efficiency, their use may not necessarily reduce perceived workload or time constraints, possibly due to associated learning curves, which are considered a requirement in the advent of digital workflows in dentistry, or integration challenges [2,3,20].
CBCT use was also positively correlated with nearly all professional outcome variables, especially satisfaction with available equipment (r = 0.754, p < 0.001) and clarity in communicating treatment plans to patients (r = 0.653, p < 0.001). These findings align with the recognized diagnostic superiority of CBCT in complex pathology and surgical cases as well as its utility in patient communication by means of 3D visualization [21,22,23]. However, the one non-significant correlation found in this study—between CBCT use and the perception that “my patients value my work” (p = 0.083)—may reflect the fact that patients are less aware of CBCT’s actual diagnostic impact, which is clinically significant.
4.2. User–Non-User Comparisons and the Role of Training
The Mann–Whitney U test revealed significant differences across all 12 outcome variables between users and non-users of each digital tool. This supports the argument that digital imaging tools, when properly integrated, can substantively enhance clinical communication, precision, and professional satisfaction [10,18,20,21]. However, the variability in uptake between tools, such as the relatively lower perception of intraoral scanners as indispensable compared to photography and CBCT—suggests that practical barriers like cost, learning curves, and differing specialty needs continue to influence adoption rates [1,2,17]. These disparities point to the importance of providing tailored digital training and support systems to promote equitable integration across dental specialties and practice types. The present results also support the growing importance of the use of digital imaging tools and digital dentistry in dental education to offer the benefits of digital imaging, CAD-CAM, and AI to all dental clinicians [2]. Furthermore, it is noteworthy that digital imaging tools involve a learning curve for dental professionals. Therefore, an incomplete learning curve could be affecting the self-reported outcomes from users of digital tools at beginner or intermediate levels. Future long-term studies are recommended to address the impact of years of experience and level of expertise among dental clinicians, dental hygienists, and dental technologists.
4.3. The Emerging but Underpowered Role of AI Software
While the number of respondents using AI software was insufficient for robust statistical comparisons, the qualitative data nonetheless offer valuable insight. Most AI users also reported using CBCT, reflecting the synergistic relationship between advanced imaging and AI-driven diagnostic or planning applications. The use of tools such as Second Opinion and Diagnocat for radiographic diagnostics, as well as Smilecloud and Automate for aesthetic and prosthetic planning, illustrates a growing diversity in AI applications—from disease detection to digital smile design [24,25,26,27].
This emergent trend underscores the evolving role of AI not only as a clinical support tool but also as a mechanism for enhancing patient engagement and aesthetic outcome predictability. However, the limited adoption of AI software across the broader sample likely reflects a current lack of widespread access, regulatory clarity, and structured training in AI technologies in dental curricula and continuing education programs [9,28,29,30,31,32,33]. Future studies should investigate these factors and explore the extent to which increased training or exposure could expand AI integration and improve measurable outcomes.
4.4. Broader Implications for Digital Dentistry
The results of this study offer compelling evidence that AI-powered tools and digital imaging technologies have a tangible and positive effect on how dental professionals perceive their clinical work, interactions, and patient satisfaction. Importantly, these findings complement previous research that emphasized technical and patient-reported outcomes by contributing novel insights into the often-overlooked clinician’s perspective.
Furthermore, the high internal consistency of the questionnaire, as indicated by a Cronbach’s alpha of 0.88, supports the reliability of the self-reported data and lends credibility to the associations identified in the study. Collectively, these findings highlight the need for structured, accessible digital training modules and institutional support mechanisms that can help bridge the gap between technological innovation and everyday clinical practice.
4.5. Limitations and Future Directions
Despite the strengths of the current study, including its large and demographically diverse sample, validated instrument, and 100% response rate, several limitations should be acknowledged. First, it is noteworthy that the assessment of self-reported outcomes in dentistry can present several types of bias [34]. The cross-sectional nature of the data restricts causal inferences, and the reliance on self-reported outcomes may introduce bias related to personal attitudes or recall. Moreover, the small number of AI users limited the statistical power to examine differences in this subgroup, warranting caution in generalizing qualitative insights. Finally, the sample of this study was composed of dentists attending a dental congress about digital dentistry and AI, whereas general dental practitioners focused on different dental fields and with less interest or experience in these topics could present different self-reported results. For this reason, longitudinal studies with larger AI-adopting populations are recommended to further explore the causal and temporal relationships between AI integration and clinical practice outcomes.
5. Conclusions
Within its present limitations, this study demonstrates that the use of digital imaging tools and, to a lesser extent, AI software, is associated with enhanced self-reported outcomes among dental professionals, including improved communication, increased satisfaction, and stronger alignment with patient expectations. These results support the ongoing integration of the fast-developing digital technologies in dentistry and emphasize the importance of clinical training and infrastructure to ensure their effective and equitable implementation.
Author Contributions
Conceptualization, H.D.; methodology, C.R., H.D. and A.R.G.C.; formal analysis, J.N.-C., A.R.G.C. and H.D.; investigation, H.D., M.P.-D. and A.R.G.C.; resources, H.D., J.N.-C. and M.P.-D.; data curation, H.D. and J.N.-C.; writing—original draft preparation, H.D., J.N.-C. and A.R.G.C.; writing—review and editing, H.D., J.N.-C., M.P.-D., C.R., H.V. and A.R.G.C.; visualization, H.D., A.R.G.C. and J.N.-C.; supervision, A.R.G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Ethics Committee of CESPU University approved the study (CE/IUCS/CESPU-13/22).
Informed Consent Statement
Informed consent was obtained from all participants, and personal data were anonymized.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Suganna, M.; Nayakar, R.P.; Alshaya, A.A.; Khalil, R.O.; Alkhunaizi, S.T.; Kayello, K.T.; Alnassar, L.A. The Digital Era Heralds a Paradigm Shift in Dentistry: A Cross-Sectional Study. Cureus 2024, 16, e53300. [Google Scholar] [CrossRef] [PubMed]
- Van Noort, R. The Future of Dental Devices Is Digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Cortes, A.R.G. Digital Dentistry: A Step-By-Step Guide and Case Atlas, 1st ed.; Wiley Blackwell: Hoboken, NJ, USA, 2022; pp. 281–285. [Google Scholar]
- Yeslam, H.E.; von Maltzahn, N.F.; Nassar, H.M. Revolutionizing CAD/CAM-Based Restorative Dental Processes and Materials with Artificial Intelligence: A Concise Narrative Review. PeerJ 2024, 12, e17793. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Zhu, Y.; Shrestha, A. A Review of Advancements of Artificial Intelligence in Dentistry. Dent. Rev. 2024, 4, 100081. [Google Scholar] [CrossRef]
- Sikri, A.; Sikri, J.; Piplani, V.; Thakur, Y. Applications of Artificial Intelligence in Dentistry: A Narrative Review. South Asian Res. J. Oral Dent. Sci. 2024, 6, 1–10. [Google Scholar] [CrossRef]
- Moon, W.; Kim, S.; Lim, B.S.; Park, Y.S.; Kim, R.J.Y.; Chung, S.H. Dimensional Accuracy Evaluation of Temporary Dental Restorations with Different 3D Printing Systems. Materials 2021, 14, 1487. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.H.; Jeong, S.N.; Choi, S.H. Detection and Diagnosis of Dental Caries Using a Deep Learning-Based Convolutional Neural Network Algorithm. J. Dent. 2018, 77, 106–111. [Google Scholar] [CrossRef]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Mangano, F.; Veronesi, G.; Hauschild, U.; Mijiritsky, E.; Mangano, C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative In Vitro Study. PLoS ONE 2016, 11, e0163107. [Google Scholar] [CrossRef]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Halim, M.S.B.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. Biomed Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef]
- Buduru, S.; Cofar, F.; Mesaroș, A.; Tăut, M.; Negucioiu, M.; Almășan, O. Perceptions in Digital Smile Design: Assessing Laypeople and Dental Professionals’ Preferences Using an Artificial-Intelligence-Based Application. Dent. J. 2024, 12, 104. [Google Scholar] [CrossRef]
- Tabatabaian, F.; Vora, S.R.; Mirabbasi, S. Applications, Functions, and Accuracy of Artificial Intelligence in Restorative Dentistry: A Literature Review. J. Esthet. Restor. Dent. 2023, 35, 842–859. [Google Scholar] [CrossRef]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Özcan, M.; Att, W.; Krishnamurthy, V.R. Artificial Intelligence Applications in Restorative Dentistry: A Systematic Review. J. Prosthet. Dent. 2022, 128, 867–875. [Google Scholar] [CrossRef]
- Bell, J. Doing Your Research Project: A Guide for First-Time Researchers in Education, Health and Social Science, 5th ed.; Open University Press: Maidenhead, UK, 2010. [Google Scholar]
- Dawa, H.; Neves, J.; Vicente, H. Evaluating the Impact of Digital Tool Utilization in Dentistry on Burnout Syndrome Among Dentists: An Entropy Analysis and AI-Driven Approach. Eng 2025, 6, 47. [Google Scholar] [CrossRef]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral Scanners in Dentistry: A Review of the Current Literature. BMC Oral. Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Zarone, F.; Ferrari, M. The Complete Digital Workflow in Fixed Prosthodontics: A Systematic Review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Iniesta, M.; Pérez-Higueras, J.J. Global Trends in the Use of Artificial Intelligence in Dental Education: A Bibliometric Analysis. Eur. J. Dent. Educ. 2025. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Shibli, J.A.; Fortin, T. Digital Dentistry: New Materials and Techniques. Int. J. Dent. 2016, 2016, 5261247. [Google Scholar] [CrossRef]
- Kau, C.H.; Li, J.; Li, Q.; Abou Kheir, N. Update on Cone Beam Technology and Orthodontic Analysis. Curr. Dent. Technol. 2014, 58, 653–669. [Google Scholar] [CrossRef]
- Sarwar, S.; Jabin, S. AI Techniques for Cone Beam Computed Tomography in Dentistry: Trends and Practices. arXiv 2023, arXiv:2306.03025. [Google Scholar] [CrossRef]
- Subramanian, A.K.; Chen, Y.; Almalki, A.; Sivamurthy, G.; Kafle, D. Cephalometric Analysis in Orthodontics Using Artificial Intelligence—A Comprehensive Review. Biomed. Res. Int. 2022, 2022, 1880113. [Google Scholar] [CrossRef]
- Diagnocat. AI-Powered Dental Intelligence. Available online: https://diagnocat.com/uk/usage/doctors-claim-intelligence-platform/ (accessed on 3 July 2025).
- Hello Pearl. Second Opinion for Real-Time Diagnosis. Available online: https://www.hellopearl.com/products/second-opinion (accessed on 3 July 2025).
- Institute of Digital Dentistry. Diagnocat Review. Available online: https://instituteofdigitaldentistry.com/ai/ (accessed on 3 July 2025).
- Spot On Business Planning. Diagnocat and Patient Communication. Available online: https://www.spoton-businessplanning.co.uk/blog/ (accessed on 3 July 2025).
- Umer, F.; Adnan, S.; Lal, A. Research and Application of Artificial Intelligence in Dentistry from Lower-Middle Income Countries: A Scoping Review. BMC Oral Health 2024, 24, 220. [Google Scholar] [CrossRef] [PubMed]
- Villena, F.; Véliz, C.; García-Huidobro, R.; Aguayo, S. Generative Artificial Intelligence in Dentistry: Current Approaches and Future Challenges. arXiv 2024, arXiv:2407.17532. [Google Scholar] [CrossRef]
- Pérez de Frutos, J.; Helland, R.H.; Desai, S.; Nymoen, L.C.; Langø, T.; Remman, T.; Sen, A. AI-Dentify: Deep Learning for Proximal Caries Detection on Bitewing X-ray—HUNT4 Oral Health Study. arXiv 2023, arXiv:2310.00354. [Google Scholar] [CrossRef] [PubMed]
- Rokaya, D.; Jaghsi, A.A.; Jagtap, R.; Srimaneepong, V. Artificial Intelligence in Dentistry and Dental Biomaterials. Front. Dent. Med. 2024, 5, 1525505. [Google Scholar] [CrossRef]
- Stanford, C. Implant Dentistry and Artificial Intelligence: A Double-Edged Innovation? Int. J. Oral Maxillofac. Implants 2025, 40, 280. [Google Scholar] [CrossRef]
- Cortes, A.R.G. Artificial Intelligence in Planning Oral Rehabilitations: Current Status. Appl. Sci. 2024, 14, 4093. [Google Scholar] [CrossRef]
- Agrawal, A.A.; Prakash, N.; Almagbol, M.; Alobaid, M.; Alqarni, A.; Altamni, H. Synoptic review on existing and potential sources for bias in dental research methodology with methods on their prevention and remedies. World. J. Methodol. 2023, 13, 426–438. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).