In Vitro Flexural Testing of Clear Aligner Materials: A Scoping Review of Methods, Results, and Clinical Relevance
Abstract
1. Introduction
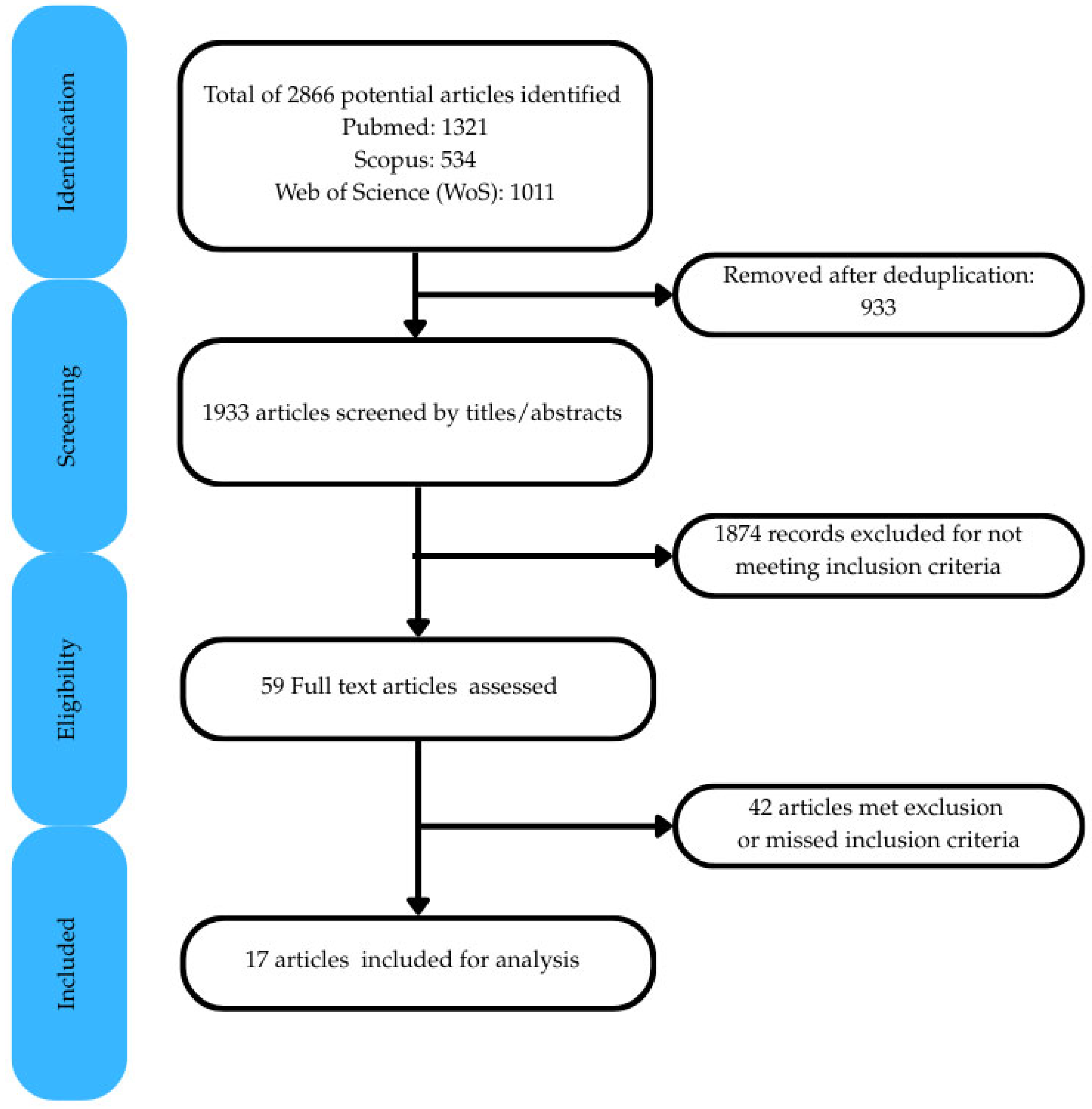
2. Materials and Methods
2.1. Framework and Guidelines
2.2. Eligibility Criteria
- Inclusion Criteria:
- Studies reporting in vitro flexural testing of clear aligners;
- Studies comparing different aligner materials or testing methodologies;
- Studies analyzing the influence of clinically relevant factors (e.g., aging, moisture, temperature);
- Peer-reviewed articles in English.
- Exclusion Criteria:
- Studies focusing solely on 3D-printed aligners or non-thermoformed materials;
- Studies on orthodontic retainer materials;
- Clinical studies without an in vitro testing component;
- Reviews, editorials, or opinion pieces;
- Full-text articles not available.
2.3. Information Sources and Search Strategy
2.4. Study Selection Process
2.5. Risk of Bias
2.6. Data Extraction
3. Results
3.1. Study Selection, Risk of Bias, and Testing Overview
3.2. Test Parameters
3.2.1. Temperature Conditions
| Albertini et al. [20] | Astasov-Frauenhoffer et al. [26] | Atta et al. [27] | Bhate and Nagesh [28] | Chen et al. [29] | Dalaie et al. [25] | Elkholy et al. (2019) [30] | Elkholy et al. (2023) [31] | Golkhani et al. [24] | Iijima et al. [32] | Kaur et al. [33] | Krishnakumaran et al. [34] | Kwon et al. [23] | Lombardo et al. [19] | Ranjan et al. [21] | Ryu et al. [22] | Yu et al. [35] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clearly stated aims/objectives | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 |
| Detailed explanation of sample size calculation | 0 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Detailed explanation of sampling technique | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 |
| Details of comparison group | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 1 |
| Detailed explanation of methodology | 2 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 |
| Operator details | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Randomization | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Method of measurement of outcome | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 |
| Outcome assessor details | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Blinding | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Statistical analysis | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 |
| Presentation of results | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 |
| Total score | 13 | 12 | 12 | 13 | 12 | 16 | 14 | 13 | 14 | 13 | 14 | 11 | 15 | 13 | 12 | 14 | 7 |
| Applied criteria | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 |
| Final score (%) | 54.2 | 50.0 | 50.0 | 54.2 | 50.0 | 66.7 | 58.3 | 54.2 | 58.3 | 54.2 | 58.3 | 45.8 | 62.5 | 54.2 | 50.0 | 58.3 | 29.2 |
| Risk of bias | Medium | Medium | Medium | Medium | Medium | Medium | Medium | Medium | Medium | Medium | Medium | High | Medium | Medium | Medium | Medium | High |
| First Author, Year | Material Tested | Test | Testing Machine | Specimen Preparation | Testing Method | Specimen Size | Span Length | Testing Standard Used | Test Results |
|---|---|---|---|---|---|---|---|---|---|
| Albertini et al., 2022 [20] | F22 Evoflex (TPU) 0.76 mm thickness. F22 Aligner (TPU) 0.76 mm thickness. Duran (PET-G) 0.75 mm thickness. Erkoloc-Pro (PET-G/TPU) 1 mm thickness. Durasoft (TPU/PC) 1.2 mm thickness. | Three-point bending test to measure stiffness, stress–strain curve, yield stress, and stress relaxation | Instron 4467 dynamometer with 100 N load cell | Nil | Load-deflection test with deformation of 100 mm/min to max deflection of 7 mm, immersed in bath of distilled water at 37 °C | 25 mm × 50 mm raw sheets | 25 mm | ASTM D790-03 [36] | Rapid stress decay and stress relaxation for all materials during first few hours of application before reaching a plateau. Single-layer samples (Duran, F22 Aligner, and F22 Evoflex) had similar yield strength, deformation, yield load, and stiffness. Double-layer samples (Erkoloc-Pro and Durasoft) had far lower stiffness values and were similar to each other. |
| Astasov-Frauenhoffer et al., 2023 [26] | Naturaligner 0.75 mm thickness. Naturaligner 0.55 mm. Zendura FLX (control). | Three-point bending test to assess maximum force (initial force), maximum stress (initial stress), and stress relaxation over a 24 h loading period | Electromechanical universal testing machine FMT-313 Alluris equipped with a 50 N load sensor | Laser cut from thermoformed materials (40 W cw CO2 laser), samples were placed in water (unloaded) or in antibacterial solution (loaded for 1 and 6 h) | 2 mm vertical deflection to achieve internal elongation of 1.6%, under wet conditions. Force (N) recorded every 59 s for 24 h. Stress ratio between initial stress and the reduced stress was calculated at 8, 12, and 24 h to determine relaxation | 40 mm × 15 mm | 22 mm | NP | Antimicrobial loading of samples did not significantly influence the initial force nor the initial stress. Naturaligner 0.75 mm, antibacterial-loaded for 6 h resulted in a lower initial force and initial stress than unloaded and 1 h loaded but similar to Zendura (control). Naturaligner 0.55 mm initial stress and force (loaded and unloaded) was significantly lower than 0.75 mm and Zendura. Zendura had the lowest stress ratio (stress relaxation) at 8, 12, and 24 h. Loading with bioactive molecules for 1 h did not significantly increase stress ratios (relaxation) in the 0.75 and 0.55 mm samples of Naturaligner. |
| Atta et al., 2024 [27] | CA Pro (3 layers: soft thermoplastic elastomeric between two hard layers of copolyester) 0.75 mm. Zendura A (TPU) 0.75 mm. Zendura FLX (3 layers: thermoplastic soft TPU between two hard layers of copolyester) 0.75 mm. Graphy Tera Harz TC-85 (3D-printed material) 0.6 mm. | Three-point bending test to measure the maximum force at different temperatures (30 °C, 37 °C, and 45 °C) | Custom-made orthodontic measurement and simulation system (OMSS) | Samples thermoformed on Biostar device according to manufacturer’s guidelines on a custom-made metal mold and scissor-cut into strips. TC-85: 3D-printed. | Test in a temperature-controlled cabin, and with 2 mm vertical deflection | 50 mm × 10 mm × 0.6 mm | 24 mm | NP | Highest force measurement for Zendura A (30 °C and 37 °C). No significant differences between all thermoformed materials at 45 °C. TC-85 consistently showed lowest forces at all temperatures. No significant differences between Zendura FLX and CA Pro at 30 °C, but at 37 °C, CA Pro displayed higher values. CA Pro maintained consistent force levels throughout. |
| Bhate and Nagesh, 2024 [28] | Duran (PET-G) 0.75 mm thickness. Zendura (PU) 0.75 mm thickness. | Three-point bending test to measure flexural modulus: as-received, thermoformed, and thermoformed and aged | Instron E-3000 universal testing machine | 3 groups/materials: i. As-received and cut into shape; ii. Thermoformed on metal plate and cut into shape, iii. Thermoformed in metal plate, cut into shape, kept in distilled water 37 °C/24 h, and thermocycled (200 cycles). | Loading at cross-head speed of 1 mm/min until fracture. | 40 mm × 9 mm | NP | NP | Duran as-received showed the highest flexural strength and reduced significantly between T0–T1 and T0–T2. Zendura strength reduced significantly when thermoformed and aged (T2) compared to as-received (T0). Significant flexural strength differences between materials were found in T0 and T1 (Duran > Zendura). |
| Chen et al., 2023 [29] | Duran T (PET-G). Biolon (PET). Zendura (TPU). All 0.75 mm thickness. | Three-point bending to evaluate changes in strength | Digital push–pull force gauge | Nil | Preload of 10 g. Displacement distance of 3 mm at speed of 5 cm/min | 10 mm × 40 mm | 10 mm | NP | For Biolon and Duran T, there were significant differences between samples soaked in artificial saliva and those soaked in different liquids (wine, Coca-Cola, coffee) on the first and fourth days. For Zendura, there were no significant differences between samples soaked in beverages and those soaked in artificial saliva. |
| Dalaie et al., 2021 [25] | Duran (PET-G) 1 mm thickness. Erkodur (PET-G) 0.8 mm thickness. | Three-point bending test to determine flexural modulus of specimens | UTM model Zwick/Roell Z020 universal testing machine | Three groups: control, thermoforming, and thermoforming and aging. Thermoforming on 40 mm × 7 mm × 2 mm model and samples of 4 mm × 20 mm cut for testing. Thermocycling used to simulate intraoral aging | Loading at rate of 1 mm/min with max deflection of 5 mm | 4 mm × 20 mm | 11 mm | NP | Flexural modulus decreased significantly after thermoforming (Duran = 88%, Erkodur = 70%). No significant difference between thermoforming and thermoforming and aging groups (p value = 0.190 for Duran, p value = 0.979 for Erkodur). |
| Elkholy et al., 2023 [31] | Duran (PET-G) 0.4, 0.5, 0.625, and 0.75 mm thicknesses | Three-point bending test to measure force-deflection curves, plastic deformation, and stiffness changes after different loading/unloading cycles | (1) Z2.5 universal testing machine with 100 N load sensor to measure bending force. (2) Custom-made ‘loading devices’ for long term loading | Films thermoformed on flat metal plate | (1) Bending force measured in Z2.5 machine. (2) Samples subjected to 3 loading/unloading cycles in custom machine and short-force measurement performed in testing machine after reaching maximum deflection | Four 10 mm × 40 mm specimens cut from each thermoformed film. Three specimens of each thickness at three different loading/unloading modes (n = 36 specimens) | 8 mm | NP | Force decay values increased significantly after the first loading cycle in 12 h/12 h loading/unloading mode. Force decay increased over subsequent loading cycles until a nearly constant median residual force level of 9.7% was reached. For 18 h/6 h and 23 h/1 h loading/unloading cycles, force decay increased significantly as the length of loading interval increased. |
| Elkholy et al., 2019 [30] | Duran (PET-G) 0.4–0.75 mm thicknesses | Three-point bending test to measure deflection forces | Zwick Z2.5 universal testing machine with 100 N force sensor | Samples thermoformed on 4 shapes: stainless-steel plate, model base plate, round disc, and gable-roof-shaped specimen | Displacement rate of 1 mm/min to different distances (0.25 or 0.5 mm) | 40 mm × 10 mm rectangular specimens from untreated and thermoformed sheets | 8–16 mm | NP | Thermoforming led to thinning of samples and a decrease in forces delivered. Max deflection before cracking was 0.20 mm for the 0.4 mm sample, 0.15 mm for the 0.5 mm, 0.15 mm for the 0.625, and 0.10 mm for the 0.75 mm sample. Storage in water for 24 h without loading did not alter deflection forces. Force levels reduced by 50% after storage in water for 24 h with loading. |
| Golkhani et al., 2022 [24] | Duran Plus (PET-G) 0.75 mm thickness. Zendura (polyurethane) 0.75 mm thickness. Essix ACE (copolyester) 0.75 mm thickness. Essix PLUS (copolyester) 0.9 mm thickness. | Three-point bending test before and after thermoforming to measure thickness changes and modulus of elasticity | Zwick/Roell ZmartPro universal testing machine | 1. Untreated raw sheets × 10. 2. 10 specimens deep drawn on a master plate, dimension 10 mm × 10 mm × 50 mm Specimens cut from upper side and lateral walls and then tested | Central displacement of 0.25, 0.50, and 2.00 mm at lengths of 8, 16, and 24 mm | Test 1—10 specimens 50 mm × 10 mm of each material. Test 2—10 specimens cut from upper side and side of cuboid with 50 mm × 10 mm dimensions | 8 mm, 16 mm, 24 mm | NP | Force reduction for samples from upper side was 50%, and 90% for the side walls. Minor influence of span distance. Reductions in modulus of elasticity from as-received to thermoformed samples were statistically significant for Duran Plus (2746 MPa to 2189 MPa) and Essix PLUS (1869 MPa to 1144 MPa). Reduction in E values for Essix ACE was not statistically significant (2274 MPa to 1798 MPa). Zendura showed a reduction in E from 2218 MPa to 1718 MPa. |
| Iijima et al., 2015 [32] | Duran (PET-G) 0.5 mm thickness. Hardcast (polypropylene) 0.4 mm thickness. SMP MM (polyurethane) 0.5 mm thickness. | Three-point bending test to determine load-deflection curves, elastic modulus, yield strength, and shape recovery | EZ Test universal testing machine | 1. Specimens prepared. 2. Specimens heat treated at Tg + 25 °C. 3. Specimens inserted in straight slot formed in gypsum block. | 1. Specimens loaded at 25 °C to 3 mm deflection at 1 mm/min. 2. Specimens heated to 100 °C using dry heat sterilizer to observe shape memory | Specimens with dimensions of 1 mm × 0.4 or 0.5 mm and 20 mm in length | 12 mm | ANSI/ADA Specification No. 32 | Elastic moduli and yield strengths were similar for Duran, SMP MM 6520, and SMP MM 9520. Elastic moduli and yield strengths for Hardcast and SMP MM 3520 were much lower than the other materials. For shape memory tests, a slight residual deflection was observed for Hardcast, SMP MM 3520, and SMP MM 9520. Duran and SMP MM 6520 showed a large residual deflection. |
| Kaur et al., 2023 [33] | Essix A+ (PET) 0.75 mm thickness. Taglus (PET-G) 0.75 mm thickness. Zendura (PU) 0.75 mm thickness. | Three-point bending test on raw and thermoformed samples to determine flexural modulus from force-displacement curve | ElectroPlus E3000 universal testing machine | Samples thermoformed using Biostar machine on stone simplified dental arch shape following manufacturer’s recommendations | Displacement rate of 2 mm/min | 5 mm × 40 mm samples cut from thermoformed and raw sheets. Sixty samples (ten raw and ten thermoformed sheets per material). | 24 mm | ASTM D790-03 [36] | Flexural modulus for Zendura increased during thermoforming (2264.72 MPa to 2913.46 MPa). Insignificant increase in flexural modulus after thermoforming for Essix A+ (2196.46 MPa to 2412.66 MPa). Flexural modulus for Taglus decreased from 2462.36 MPa to 2457.95 MPa. |
| Krishnakumaran et al., 2023 [34] | Thermoplastic polyurethane (TPU) 1 mm thickness (manufacturer not mentioned) | Three-point bending test to determine tensile strength and elastic modulus: as-received (TPU), nanocoated CMC-CHI (coated TPU), and nanocoated CMC-CHI and thermoformed (thermoformed coated TPU) | Universal testing machine (no further details) | Three groups: i. Control (TPU), ii. Coated with carboxymethyl cellulose (CMC), chitosan (CHI), and iii. Coated and thermoformed TPU | Loading at 25 °C, with a deflection of 3 mm applied at a strain rate of 1 mm/min | 20 mm × 1 mm × 1 mm | 15 mm | NP | Elastic modulus and tensile strength increased when TPU was coated with carboxymethyl cellulose (CMC) and chitosan (CHI). However, thermoforming coated-specimens appeared to counteract the effects of higher mechanical properties due to coating. |
| Kwon et al., 2008 [23] | Essix A+ 0.5 mm, 0.75 mm, and 1 mm thicknesses. Essix ACE 0.75 mm thickness. Essix C+ 1 mm thickness. | Three-point bending recovery test to measure force delivery properties during recovery from deflection | Instron model 4465 | Materials thermoformed on stone model, 30 mm × 60 mm × 10 mm | 1. Specimen deflected vertically 2 mm at 5 mm/min. 2. Force delivery properties during recovery from deflection recorded. 3. Thermocycled between 5 °C and 55 °C and test repeated | Specimens of 20 mm × 50 mm cut out (10 specimens for each material) | 24 mm | NP | Amount of delivered force decreased after thermocycling. No significant difference in the force delivery properties after thermocycling when deflection was in the range of optimum force delivery (0.2–0.5 mm). Amount of delivered force generally decreased after repeated load cycling. |
| Lombardo et al., 2016 [19] | F 22 Aligner (TPU) 0.75 mm thickness. Duran (PET-G) 0.75 mm thickness. Erkoloc-Pro (PET-G/TPU) 1 mm thickness. Durasoft (TPU/PC) 1.2 mm thickness. | Three-point bending test to measure stiffness, stress–strain curve, yield stress, and stress relaxation | Instron 4467 dynamometer with 100 N load cell | Nil | Preload 1 N, load-deflection test with deformation of 100 mm/min to max deflection of 7 mm, immersed in bath of distilled water at 37 °C | 25 mm × 50 mm raw sheets | 25 mm | ASTM D790 | Stress relaxation and stress decay for each sample was high during the first 8 h and then plateaued. Yield strength test showed single-layer samples (Duran and F22 Aligner) had similar stiffness values (2.9 and 2.7 MPa). Double-layer samples (Erkoloc-Pro and Durasoft) values were 0.6 MPa. |
| Ranjan et al., 2020 [21] | Duran (PET-G) 0.75 mm thickness. Erkodur (PET-G/TPU) 0.8 mm. Track (PET-G) 0.8 mm. | Three-point bending test to assess load deflection, stress relaxation, and yield strengths | Star universal testing machine | Nil | Preload of 1 N. Displacement rate of 100 mm/min to max deflection of 7 mm | 25 mm × 50 mm | 25 mm | NP | Duran had more yield load and yield strength than Erkodur and Track. Duran had greater total initial stress and the highest decay during first 24 h. Erkodur had the lowest initial and final stress values. Duran had a higher percentage of stress relaxation. |
| Ryu et al., 2018 [22] | Duran (PET-G) 0.5, 0.75, and 1.0 mm. Essix A+ (copolyester) 0.5, 0.75, and 1 mm. eCligner (PET-G) 0.5 and 0.75 mm. Essix ACE (copolyester) 0.75 and 1 mm. | Three-point bending test to measure flexural modulus before and after thermoforming | Instron model 3366 universal testing machine | Samples thermoformed at 220 °C on 8.5 mm × 7 mm × 2 mm block | Strain interval of 0.5 mm from 0.5 mm to 1 mm at cross-head speed of 5 mm/min. | 40 mm × 9 mm specimens cut out for analysis (5 specimens of each material and thickness) | 24 mm | ISO 20795-2 (2013) | Flexural force for all materials and thicknesses significantly lowered after thermoforming. Flexural modulus after thermoforming: 1: 0.5 mm samples: significant increase. 2: 0.75 mm: Duran and eCligner increased significantly, no significant changes for Essix A+ and Essix ACE. 3: 1 mm: significant decrease for all materials. |
| Yu et al., 2022 [35] | Thermoplastic polyurethane (no further description) | Three-point bending test to determine flexural modulus and stress/strain curve | Universal testing machine Instron 5943 | NP | Cross-head speed was 0.5 mm/min | NP | NP | NP | TPU achieved a bending modulus of 2511 Mpa. |
3.2.2. Thermoforming Protocols
3.2.3. Span Lengths
3.2.4. Deflection Levels
3.3. Materials
3.4. Investigated Influencing Factors
3.4.1. Thermoforming Effects
3.4.2. Liquid Absorption
3.4.3. Temperature Changes
3.4.4. Constant and Interval Loading
3.4.5. Influence of Aligner Thickness
4. Discussion
4.1. Testing
4.2. Test Parameters
4.2.1. Temperature Conditions
4.2.2. Thermoforming Protocols
4.2.3. Span Length
4.2.4. Deflection Levels
4.3. Materials
4.4. Influencing Factors
4.4.1. Thermoforming
4.4.2. Liquid Absorption
4.4.3. Temperature Changes
4.4.4. Constant and Interval Loading
4.4.5. Aligner Thickness
4.5. Other Factors
4.6. Future Research
5. Conclusions
- Thermoforming typically reduces the thickness and mechanical properties of clear aligner materials, particularly PET-G.
- Water or saliva exposure, especially under loading, can accelerate force decay; TPU may offer better moisture resistance.
- Increases in temperature or thermal cycling may reduce force output and modulus in several materials.
- Constant loading leads to stress relaxation and force decay, most notably during the initial hours of wear.
- Testing at 37 °C, using span lengths of ~8 mm and deflection values within clinically relevant ranges, may better simulate intraoral conditions and improve translational relevance.
- To improve clinical relevance and facilitate future comparisons, a minimum experimental reference protocol is recommended: testing at 37 °C, using a span length of ~8 mm, and applying deflection values within clinically relevant ranges (e.g., 0.2–0.5 mm).
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CAT | Clear aligner therapy |
| FAT | Fixed appliance therapy |
| PET | Polyethylene terephthalate |
| PET-G | Polyethylene terephthalate glycol |
| PU | Polyurethane |
| TPU | Thermoplastic polyurethane |
| PP | Polypropylene |
| PC | Polycarbonate |
| CAD-CAM | Computer-aided design/Computer-aided manufacturing |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| Tg | Glass transition temperature |
| 3-PBT | Three-point bending test |
References
- Lagravère, M.O.; Flores-Mir, C. The Treatment Effects of Invisalign Orthodontic Aligners. J. Am. Dent. Assoc. 2005, 136, 1724–1729. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, B.; Padmanabhan, S.; Srinivasan, S. Comparative Evaluation of Physical and Mechanical Properties of Clear Aligners—A Systematic Review. Evid. Based Dent. 2024, 25, 53. [Google Scholar] [CrossRef] [PubMed]
- Kesling, H.D. Coordinating the Predetermined Pattern and Tooth Positioner with Conventional Treatment. Am. J. Orthod. Oral. Surg. 1946, 32, 285–293. [Google Scholar] [CrossRef]
- Eliades, T.; Athanasiou, A.E. Orthodontic Aligner Treatment: A Review of Materials, Clinical Management, and Evidence; Thieme Publishing Group: Stuttgart, Germany, 2021; ISBN 978-3-13-241148-7. [Google Scholar]
- Beers, A.; Choi, W.; Pavlovskaia, E. Computer-assisted Treatment Planning and Analysis. Orthod. Craniofacial Res. 2003, 6, 117–125. [Google Scholar] [CrossRef]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of Clear Aligner Therapy for Orthodontic Treatment: A Systematic Review. Orthod. Craniofacial Res. 2020, 23, 133–142. [Google Scholar] [CrossRef]
- Hennessy, J.; Al-Awadhi, E.A. Clear Aligners Generations and Orthodontic Tooth Movement. J. Orthod. 2016, 43, 68–76. [Google Scholar] [CrossRef]
- Jiang, T.; Jiang, Y.-N.; Chu, F.-T.; Lu, P.-J.; Tang, G.-H. A Cone-Beam Computed Tomographic Study Evaluating the Efficacy of Incisor Movement with Clear Aligners: Assessment of Incisor Pure Tipping, Controlled Tipping, Translation, and Torque. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 635–643. [Google Scholar] [CrossRef]
- Charalampakis, O.; Iliadi, A.; Ueno, H.; Oliver, D.R.; Kim, K.B. Accuracy of Clear Aligners: A Retrospective Study of Patients Who Needed Refinement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 47–54. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Weir, T. Clear Aligners in Orthodontic Treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef]
- Cortona, A.; Rossini, G.; Parrini, S.; Deregibus, A.; Castroflorio, T. Clear Aligner Orthodontic Therapy of Rotated Mandibular Round-Shaped Teeth: A Finite Element Study. Angle Orthod. 2020, 90, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Al-Moghrabi, D.; Salazar, F.C.; Pandis, N.; Fleming, P.S. Compliance with Removable Orthodontic Appliances and Adjuncts: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Bai, Y.; Ding, X.; Zhang, Y. Preparation and Characterization of Thermoplastic Materials for Invisible Orthodontics. Dent. Mater. J. 2011, 30, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Kapila, S.; Sachdeva, R. Mechanical Properties and Clinical Applications of Orthodontic Wires. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 100–109. [Google Scholar] [CrossRef]
- ISO 20795-2:2013; Dentistry—Base Polymers. Part. 2: Orthodontic Base Polymers. International Organization for Standardization: Geneva, Switzerland, 2013.
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and Validation of a Risk-of-Bias Tool for Assessing in Vitro Studies Conducted in Dentistry: The QUIN. J. Prosthet. Dent. 2024, 131, 1038–1042. [Google Scholar] [CrossRef]
- Lombardo, L.; Martines, E.; Mazzanti, V.; Arreghini, A.; Mollica, F.; Siciliani, G. Stress Relaxation Properties of Four Orthodontic Aligner Materials: A 24-Hour in Vitro Study. Angle Orthod. 2016, 87, 11–18. [Google Scholar] [CrossRef]
- Albertini, P.; Mazzanti, V.; Mollica, F.; Pellitteri, F.; Palone, M.; Lombardo, L. Stress Relaxation Properties of Five Orthodontic Aligner Materials: A 14-Day In-Vitro Study. Bioengineering 2022, 9, 349. [Google Scholar] [CrossRef]
- Ranjan, A.; Biradar, A.K.; Patel, A.; Varghese, V.; Pawar, A.; Kulshrestha, R. Assessment of the Mechanical Properties of Three Commercially Available Thermoplastic Aligner Materials Used for Orthodontic Treatment. Iran. J. Ortho 2020, 15, 1–7. [Google Scholar] [CrossRef]
- Ryu, J.-H.; Kwon, J.-S.; Jiang, H.B.; Cha, J.-Y.; Kim, K.-M. Effects of Thermoforming on the Physical and Mechanical Properties of Thermoplastic Materials for Transparent Orthodontic Aligners. Korean J. Orthod. 2018, 48, 316. [Google Scholar] [CrossRef]
- Kwon, J.-S.; Lee, Y.-K.; Lim, B.-S.; Lim, Y.-K. Force Delivery Properties of Thermoplastic Orthodontic Materials. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Golkhani, B.; Weber, A.; Keilig, L.; Reimann, S.; Bourauel, C. Variation of the Modulus of Elasticity of Aligner Foil Sheet Materials Due to Thermoforming. J. Orofac. Orthop. 2022, 83, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Dalaie, K.; Fatemi, S.M.; Ghaffari, S. Dynamic Mechanical and Thermal Properties of Clear Aligners after Thermoforming and Aging. Prog. Orthod. 2021, 22, 15. [Google Scholar] [CrossRef] [PubMed]
- Astasov-Frauenhoffer, M.; Göldi, L.; Rohr, N.; Worreth, S.; Dard, E.; Hünerfauth, S.; Töpper, T.; Zurflüh, J.; Braissant, O. Antimicrobial and Mechanical Assessment of Cellulose-Based Thermoformable Material for Invisible Dental Braces with Natural Essential Oils Protecting from Biofilm Formation. Sci. Rep. 2023, 13, 13428. [Google Scholar] [CrossRef]
- Atta, I.; Bourauel, C.; Alkabani, Y.; Mohamed, N.; Kim, H.; Alhotan, A.; Ghoneima, A.; Elshazly, T. Physiochemical and Mechanical Characterisation of Orthodontic 3D Printed Aligner Material Made of Shape Memory Polymers (4D Aligner Material). J. Mech. Behav. Biomed. Mater. 2024, 150, 106337. [Google Scholar] [CrossRef]
- Bhate, M.; Nagesh, S. Assessment of the Effect of Thermoforming Process and Simulated Aging on the Mechanical Properties of Clear Aligner Material. Cureus 2024, 16, e64933. [Google Scholar] [CrossRef]
- Chen, S.-M.; Huang, T.-H.; Ho, C.-T.; Kao, C.-T. Force Degradation Study on Aligner Plates Immersed in Various Solutions. J. Dent. Sci. 2023, 18, 1845–1849. [Google Scholar] [CrossRef]
- Elkholy, F.; Schmidt, S.; Amirkhani, M.; Schmidt, F.; Lapatki, B.G. Mechanical Characterization of Thermoplastic Aligner Materials: Recommendations for Test Parameter Standardization. J. Healthc. Eng. 2019, 2019, 1–10. [Google Scholar] [CrossRef]
- Elkholy, F.; Schmidt, S.; Schmidt, F.; Amirkhani, M.; Lapatki, B.G. Force Decay of Polyethylene Terephthalate Glycol Aligner Materials during Simulation of Typical Clinical Loading/Unloading Scenarios. J. Orofac. Orthop. 2023, 84, 189–201. [Google Scholar] [CrossRef]
- Iijima, M.; Kohda, N.; Kawaguchi, K.; Muguruma, T.; Ohta, M.; Naganishi, A.; Murakami, T.; Mizoguchi, I. Effects of Temperature Changes and Stress Loading on the Mechanical and Shape Memory Properties of Thermoplastic Materials with Different Glass Transition Behaviours and Crystal Structures. EORTHO 2015, 37, 665–670. [Google Scholar] [CrossRef]
- Kaur, H.; Khurelbaatar, T.; Mah, J.; Heo, G.; Major, P.W.; Romanyk, D.L. Investigating the Role of Aligner Material and Tooth Position on Orthodontic Aligner Biomechanics. J. Biomed. Mater. Res. 2023, 111, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Krishnakumaran, M.; Mahalingam, J.; Arumugam, S.; Prabhu, D.; Parameswaran, T.M.; Krishnan, B. Evaluation of the Effect of Nanocoating on Mechanical and Biofilm Formation in Thermoplastic Polyurethane Aligner Sheets. Contemp. Clin. Dent. 2023, 14, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Li, G.; Zheng, Y.; Gao, J.; Fu, Y.; Wang, Q.; Huang, L.; Pan, X.; Ding, J. ‘Invisible’ Orthodontics by Polymeric ‘Clear’ Aligners Molded on 3D-Printed Personalized Dental Models. Regen. Biomater. 2022, 9, rbac007. [Google Scholar] [CrossRef] [PubMed]
- ASTM D790-03; Standard Test Methods for Flexural Properties of Unreinforced and Reinforced Plastics and Electrical Insulating Materials. ASTM International: West Conshohocken, PA, USA, 2003. [CrossRef]
- Moore, R.; Watts, J.; Hood, J.; Burritt, D. Intra-Oral Temperature Variation over 24 Hours. Eur. J. Orthod. 1999, 21, 249–261. [Google Scholar] [CrossRef]
- Barclay, C.W.; Spence, D.; Laird, W.R.E. Intra-oral Temperatures during Function. J. Oral Rehabil. 2005, 32, 886–894. [Google Scholar] [CrossRef]
- Burstone, C.J. The Biophysics of Bone Remodeling during Orthodontics-Optimal Froce Considerations-. In The Biology of Tooth Movement; CRC Press: Boca Raton, FL, USA, 1989; pp. 321–333. [Google Scholar]
- Proffit, W.R.; Fields, H.W.; Larson, B.E.; Sarver, D.M. Contemporary Orthodontics, 6th ed.; Elsevier: Philadelphia, PA, USA, 2019; ISBN 978-0-323-54387-3. [Google Scholar]
- Sheridan, J.; Ledoux, W.; McMinn, R. Essix Appliances: Minor Tooth Movement with Divots and Windows. J. Clin. Orthod. 1994, 28, 659–663. [Google Scholar]
- Boyd, R.L.; Miller, R.J.; Vlaskalic, V. The Invisalign System in Adult Orthodontics: Mild Crowding and Space Closure Cases. J. Clin. Orthod. 2000, 34, 203–212. [Google Scholar]
- Elkholy, F.; Schmidt, F.; Jäger, R.; Lapatki, B.G. Forces and Moments Delivered by Novel, Thinner PET-G Aligners during Labiopalatal Bodily Movement of a Maxillary Central Incisor: An in Vitro Study. Angle Orthod. 2016, 86, 883–890. [Google Scholar] [CrossRef]
- Ihssen, B.A.; Willmann, J.H.; Nimer, A.; Drescher, D. Effect of in Vitro Aging by Water Immersion and Thermocycling on the Mechanical Properties of PETG Aligner Material. J. Orofac. Orthop. 2019, 80, 292–303. [Google Scholar] [CrossRef]
- Buschang, P.H.; Shaw, S.G.; Ross, M.; Crosby, D.; Campbell, P.M. Comparative Time Efficiency of Aligner Therapy and Conventional Edgewise Braces. Angle Orthod. 2014, 84, 391–396. [Google Scholar] [CrossRef]
- Ihssen, B.A.; Kerberger, R.; Rauch, N.; Drescher, D.; Becker, K. Impact of Dental Model Height on Thermoformed PET-G Aligner Thickness—An In Vitro Micro-CT Study. Appl. Sci. 2021, 11, 6674. [Google Scholar] [CrossRef]
- Haouili, N.; Kravitz, N.D.; Vaid, N.R.; Ferguson, D.J.; Makki, L. Has Invisalign Improved? A Prospective Follow-up Study on the Efficacy of Tooth Movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 420–425. [Google Scholar] [CrossRef]
| Database | Search String | Results Found |
|---|---|---|
| PubMed | (“Clear aligners” OR Invisalign OR thermoform* OR orthodontic* OR “thermoplastic appliance*” OR “orthodontic retainer*” OR “orthodontic splint*”) AND (“Flexural Strength”[MeSH] OR “three-point bending” OR “three point bending” OR “four-point bending” OR “four point bending” OR “biaxial flexural” OR “mechanical properties” OR “flexural modulus” OR “elastic modulus”) AND (Journal Article[PT]) AND (English[lang]) | 1321 Articles |
| Scopus | TITLE-ABS-KEY (“clear aligners” OR invisalign OR thermoform* OR orthodontic*) AND TITLE-ABS-KEY (“flexural strength” OR “three-point bending” OR “three point bending” OR “four-point bending” OR “four point bending” OR “biaxial flexural” OR “mechanical properties” OR “flexural modulus” OR “elastic modulus”) AND SUBJAREA (mater OR dent OR eng) AND DOCTYPE (ar) AND LANGUAGE (english) | 534 Articles |
| WoS | TS = (“clear aligners” OR Invisalign OR thermoform* OR orthodontic*) AND TS = (“flexural strength” OR “three-point bending” OR “three point bending” OR “four-point bending” OR “four point bending” OR “biaxial flexural” OR “mechanical properties” OR “flexural modulus” OR “elastic modulus”) AND WC = (“Materials Science” OR “Dentistry, Oral Surgery & Medicine”) AND DT = (Article) | 1011 Articles |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nugent, G.; Munoz, A.; Louca, C.; Vichi, A. In Vitro Flexural Testing of Clear Aligner Materials: A Scoping Review of Methods, Results, and Clinical Relevance. Appl. Sci. 2025, 15, 7516. https://doi.org/10.3390/app15137516
Nugent G, Munoz A, Louca C, Vichi A. In Vitro Flexural Testing of Clear Aligner Materials: A Scoping Review of Methods, Results, and Clinical Relevance. Applied Sciences. 2025; 15(13):7516. https://doi.org/10.3390/app15137516
Chicago/Turabian StyleNugent, Gavin, Alvaro Munoz, Chris Louca, and Alessandro Vichi. 2025. "In Vitro Flexural Testing of Clear Aligner Materials: A Scoping Review of Methods, Results, and Clinical Relevance" Applied Sciences 15, no. 13: 7516. https://doi.org/10.3390/app15137516
APA StyleNugent, G., Munoz, A., Louca, C., & Vichi, A. (2025). In Vitro Flexural Testing of Clear Aligner Materials: A Scoping Review of Methods, Results, and Clinical Relevance. Applied Sciences, 15(13), 7516. https://doi.org/10.3390/app15137516






