Importance of CBCT Analysis in the Preoperative Planning of TAD Placement in the Anterior Maxillary Region
Abstract
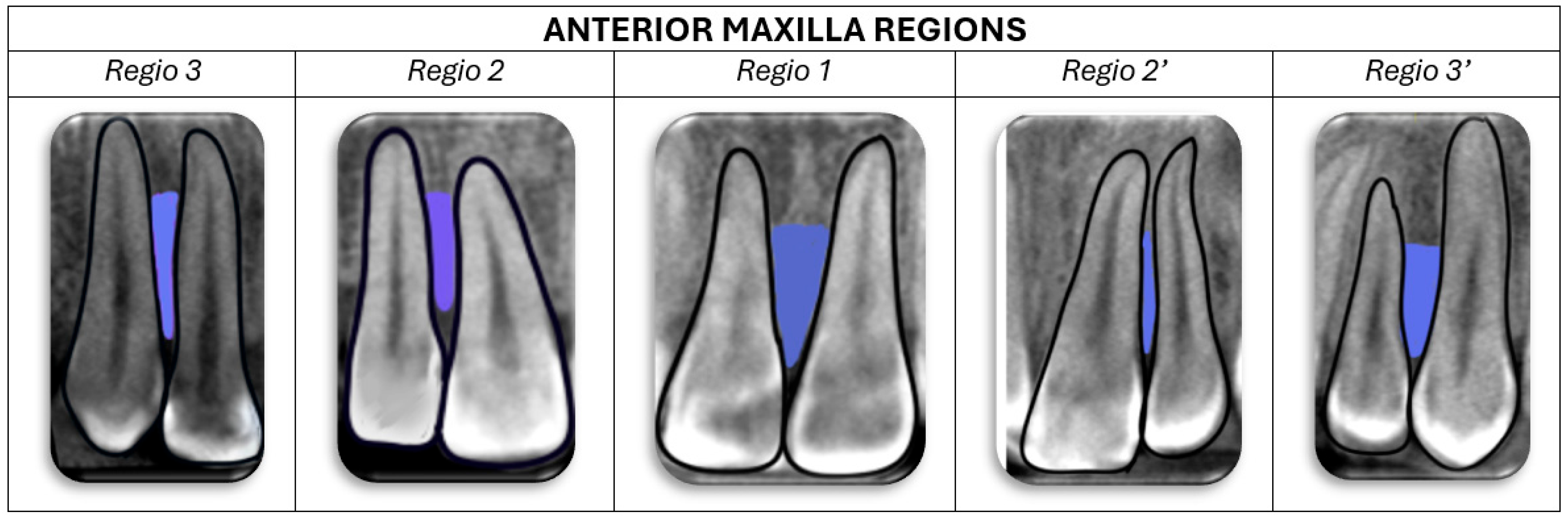
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. CBCT Imaging Device and Software Characteristics
2.3. Morphometric Parameters
- Sagittal cross-section:
- Level A—8 mm from the alveolar crest;
- Level B—6 mm from the alveolar crest;
- Level C—4 mm from the alveolar crest;
- Level D—2 mm from the alveolar crest.

- 2.
- Axial cross-section:
- Buccopalatal depth (BPD)—the linear distance between buccal and palatal cortical plates (Figure 3).

- Interdental width (IDW)—the narrowest mesiodistal distance between the roots of adjacent teeth (Figure 3).
2.4. Relationship Between Radiological Ideal Placement Point (IPP) and Dental Structures
2.5. Statistical Analysis
3. Results
- Interclass Correlation
- Demographics and Group Classification
- Statistical Differences Between the Groups
- Descriptive Data on Mean Interdental Width and Buccopalatal Depth
- Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baxi, S.; Bhatia, V.; Tripathi, A.; Prasad Dubey, M.; Kumar, P.; Mapare, S. Temporary Anchorage Devices. Cureus 2023, 15, e44514. [Google Scholar] [CrossRef]
- Cousley, R.R.; Sandler, P.J. Advances in orthodontic anchorage with the use of mini-implant techniques. Br. Dent. J. 2015, 218, E4. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, Z.J.; Zhou, J.; Xiong, P.; Wang, Q.; Yang, Y.; Hu, Y.; Hu, J.T. Comparison of Anchorage Efficiency of Orthodontic Mini-implant and Conventional Anchorage Reinforcement in Patients Requiring Maximum Orthodontic Anchorage: A Systematic Review and Meta-analysis. J. Evid. Based Dent. Pract. 2020, 20, 101401. [Google Scholar] [CrossRef] [PubMed]
- Marquezan, M.; de Souza, M.M.G.; Araújo, M.T.; Oliveira, D.D. Evaluating the center of resistance of upper incisors by different finite element models. Dent. Press. J. Orthod. 2010, 15, 88–92. [Google Scholar]
- Park, H.S.; Kwon, T.G.; Kwon, O.W. Treatment of open bite with microscrew implant anchorage. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 627–636. [Google Scholar] [CrossRef]
- Parayaruthottam, P.; Antony, V. Midline Mini-Implant-Assisted True Intrusion of Maxillary Anterior Teeth for Improved Smile Esthetics in Gummy Smile. Contemp. Clin. Dent. 2021, 12, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Panaite, T.; Balcos, C.; Savin, C.; Olteanu, N.D.; Karvelas, N.; Romanec, C.; Vieriu, R.M.; Chehab, A.; Zetu, I. Exploring the use, perceptions, and challenges of mini-implants in orthodontic practice: A survey study. Front. Oral Health 2025, 5, 1483068. [Google Scholar] [CrossRef]
- Murugesan, A.; Dinesh, S.P.S.; Muthuswamy Pandian, S.; Ashwin Solanki, L.; Alshehri, A.; Awadh, W.; Alzahrani, K.J.; Alsharif, K.F.; Alnfiai, M.M.; Mathew, R.; et al. Evaluation of Orthodontic Mini-Implant Placement in the Maxillary Anterior Alveolar Region in 15 Patients by Cone Beam Computed Tomography at a Single Center in South India. Med. Sci. Monit. 2022, 28, e937949. [Google Scholar] [CrossRef]
- Arnaut, A.; Milanovic, P.; Vasiljevic, M.; Jovicic, N.; Vojinovic, R.; Selakovic, D.; Rosic, G. The Shape of Nasopalatine Canal as a Determining Factor in Therapeutic Approach for Orthodontic Teeth Movement-A CBCT Study. Diagnostics 2021, 11, 2345. [Google Scholar] [CrossRef]
- Vasiljevic, M.; Milanovic, P.; Jovicic, N.; Vasovic, M.; Milovanovic, D.; Vojinovic, R.; Selakovic, D.; Rosic, G. Morphological and Morphometric Characteristics of Anterior Maxilla Accessory Canals and Relationship with Nasopalatine Canal Type-A CBCT Study. Diagnostics 2021, 11, 1510. [Google Scholar] [CrossRef]
- Nanda, R.; Uribe, F. Temporary Anchorage Devices in Orthodontics, 2nd ed.; Mosby Elsevier: St. Louis, MI, USA, 2019. [Google Scholar]
- Gurdan, Z.; Szalma, J. Evaluation of the success and complication rates of self-drilling orthodontic mini-implants. Niger. J. Clin. Pract. 2018, 21, 546–552. [Google Scholar] [PubMed]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: A systematic review and meta-analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef]
- Deguchi, T.; Nasu, M.; Murakami, K.; Yabuuchi, T.; Kamioka, H.; Takano-Yamamoto, T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am. J. Orthod. Dentofac. Orthop. 2006, 129, e7–e12. [Google Scholar] [CrossRef] [PubMed]
- Ferrillo, M.; Nucci, L.; Gallo, V.; Bruni, A.; Montrella, R.; Fortunato, L.; Giudice, A.; Perillo, L. Temporary anchorage devices in orthodontics: A bibliometric analysis of the 50 most-cited articles from 2012 to 2022. Angle Orthod. 2023, 93, 591–602. [Google Scholar] [CrossRef]
- Chang, C.H.; Lin, L.Y.; Roberts, W.E. Orthodontic bone screws: A quick update and its promising future. Orthod. Craniofac. Res. 2020, 24, 75–82. [Google Scholar] [CrossRef]
- Ozdemir, F.; Tozlu, M.; Germec-Cakan, D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 190–196. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Malcangi, G.; Costa, S.; Fatone, M.C.; Avantario, P.; Campanelli, M.; Piras, F.; Patano, A.; Ferrara, I.; Di Pede, C.; et al. Tooth Complications after Orthodontic Miniscrews Insertion. Int. J. Environ. Res. Public Health 2023, 20, 1562. [Google Scholar] [CrossRef] [PubMed]
- Purmal, K.; Alam, M.; Pohchi, A.; Abdul Razak, N.H. 3D Mapping of Safe and Danger Zones in the Maxilla and Mandible for the Placement of Intermaxillary Fixation Screws. PLoS ONE 2013, 8, e84202. [Google Scholar] [CrossRef]
- Lim, H.J.; Choi, Y.J.; Evans, C.A.; Hwang, H.S. Predictors of initial stability of orthodontic miniscrew implants. Eur. J. Orthod. 2011, 33, 528–532. [Google Scholar] [CrossRef]
- Schnelle, M.A.; Beck, F.M.; Jaynes, R.M.; Huja, S.S. A radiographic evaluation of the availability of bone for placement of miniscrews. Angle Orthod. 2004, 74, 832–837. [Google Scholar]
- MacDonald, D.; Telyakova, V. An Overview of Cone-Beam Computed Tomography and Dental Panoramic Radiography in Dentistry in the Community. Tomography 2024, 10, 1222–1237. [Google Scholar] [CrossRef] [PubMed]
- Caetano, G.R.; Soares, M.Q.; Oliveira, L.B.; Junqueira, J.L.; Nascimento, M.C. Two-dimensional radiographs versus cone-beam computed tomography in planning mini-implant placement: A systematic review. J. Clin. Exp. Dent. 2022, 14, e669–e677. [Google Scholar] [CrossRef] [PubMed]
- Abbassy, M.A.; Sabban, H.M.; Hassan, A.H.; Zawawi, K.H. Evaluation of mini-implant sites in the posterior maxilla using traditional radiographs and cone-beam computed tomography. Saudi Med. J. 2015, 36, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Kapila, S.; Conley, R.S.; Harrell, W.E., Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac. Radiol. 2011, 40, 24–34. [Google Scholar] [CrossRef]
- De Grauwe, A.; Ayaz, I.; Shujaat, S.; Dimitrov, S.; Gbadegbegnon, L.; Vande Vannet, B.; Jacobs, R. CBCT in orthodontics: A systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur. J. Orthod. 2019, 41, 381–389. [Google Scholar] [CrossRef]
- Elhammali, N.A.; Gupta, P.; Deb, S.; Chhaparwal, A.; Mohanty, R.; Tiwari, S. RNR Evaluation of anterior maxilla bone condition using CBCT for placing dental implant. Bioinformation 2024, 20, 1038–1041. [Google Scholar] [CrossRef]
- DeVos, W.; Casselman, J.; Swennen, G.R. Cone beam computerized tomography (CBCT) imaging of oral and maxillofacial region: A systemic review of literature. Int. J. Oral Maxillofac. Surg. 2009, 38, 609–625. [Google Scholar] [CrossRef]
- Wu, Y.; Xu, Z.; Tan, L.; Tan, L.; Zhao, Z.; Yang, P.; Li, Y.; Tang, T.; Zhao, L. Orthodontic mini-implant stability under continuous or intermittent loading: A histomorphometric and biomechanical analysis. Clin. Implant. Dent. Relat. Res. 2015, 17, 163–172. [Google Scholar] [CrossRef]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe zones”: A guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar]
- Zago, H.; Navarro, R.L.; Laranjeira, V.; Fernandes, T.M.; Conti, A.C.; Oltramari, P.V. 3-D Evaluation of temporary skeletal anchorage sites in the maxilla. J. Clin. Exp. Dent. 2021, 13, e1131–e1139. [Google Scholar] [CrossRef]
- Park, J.; Cho, H.J. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am. J. Orthod. Dentofac. Orthop. 2019, 136, 314.e1–314.e12. [Google Scholar] [CrossRef] [PubMed]
- Leo, M.; Cerroni, L.; Pasquantonio, G.; Condò, S.G.; Condò, R. Temporary anchorage devices (TADs) in orthodontics: Review of the factors that influence the clinical success rate of the mini-implants. Clin. Ter. 2016, 167, e70–e77. [Google Scholar] [PubMed]
- Vasoglou, G.; Stefanidaki, I.; Apostolopoulos, K.; Fotakidou, E.; Vasoglou, M. Accuracy of Mini-Implant Placement Using a Computer-Aided Designed Surgical Guide, with Information of Intraoral Scan and the Use of a Cone-Beam CT. Dent. J. 2022, 10, 104. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E.Y.; Suzuki, B. Accuracy of miniscrew implant placement with a 3-dimensional surgical guide. J. Oral Maxillofac. Surg. 2008, 66, 1245–1252. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhu, C.; Zhu, M.; Lei, L. Difference in the alveolar bone remodeling between the adolescents and adults during upper incisor retraction: A retrospective study. Sci. Rep. 2022, 12, 9161. [Google Scholar] [CrossRef]
- Centeno, A.C.T.; Fensterseifer, C.K.; Chami, V.O.; Ferreira, E.S.; Marquezan, M.; Ferrazzo, V.A. Correlation between cortical bone thickness at mini-implant insertion sites and age of patient. Dent. Press. J. Orthod. 2022, 27, e222098. [Google Scholar] [CrossRef]
- Fayed, M.M.; Pazera, P.; Katsaros, C. Optimal sites for orthodontic mini-implant placement assessed by cone beam computed tomography. Angle Orthod. 2010, 80, 939–951. [Google Scholar] [CrossRef]
- Hou, Z.; Qu, X.; Hou, L.; Ren, F. Comparison between effects of mini-implant anchorage and face-bow anchorage in orthodontics for children. J. Clin. Pediatr. Dent. 2024, 48, 198–203. [Google Scholar]
- Fan, Y.; Han, B.; Zhang, Y.; Guo, Y.; Li, W.; Chen, H.; Meng, C.; Penington, A.; Schneider, P.; Pei, Y.; et al. Natural reference structures for three-dimensional maxillary regional superimposition in growing patients. BMC Oral Health 2023, 23, 655. [Google Scholar]
- Sandler, J.; Murray, A.; Thiruvenkatachari, B.; Gutierrez, R.; Speight, P.; O’Brien, K. Effectiveness of 3 methods of anchorage reinforcement for maximum anchorage in adolescents: A 3-arm multicenter randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 10–20. [Google Scholar] [CrossRef]
- Maino, G.B.; Maino, G.; Dalessandri, D.; Paganelli, C. Orthodontic correction of malpositioned teeth before restorative treatment: Efficiency improvement using Temporary Anchorage Devices (TADs). Orthod. Fr. 2016, 87, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Halim, M.S.; Aslam, A.; Ghani, Z.A.; Safdar, J.; Alam, M.K. An Analysis of Maxillary Anterior Teeth Crown Width-Height Ratios: A Photographic, Three-Dimensional, and Standardized Plaster Model’s Study. BioMed Res. Int. 2022, 2022, 4695193. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, Y.M.; Samsudin, A.B.R.; Al-Bayatti, S.; Pattanaik, S.; Gaballah, K.; Badran, S.; Manila, N.; Kamath, V.; Mathew, A.; Shetty, S.R.; et al. A Study on the Association between Skeletal Malocclusion, Upper Airway Cross-Sectional Area, and Upper Airway Volume Using CBCT Scans. Eur. J. Gen. Dent. 2025. [Google Scholar] [CrossRef]
- Schwarz, L.; Andrukhov, O.; Rausch, M.A.; Rausch-Fan, X.; Jonke, E. Difference in Buccal Gingival Thickness between the Mandible and Maxilla in the Aesthetic Zone: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1789. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cha, B.K.; Lee, Y.H.; Lee, N.K.; Choi, D.S.; Baek, S.H. Soft tissue thickness for placement of an orthodontic miniscrew using an ultrasonic device. Angle Orthod. 2008, 78, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Dumitrache, M.; Grenard, A. Mapping mini-implant anatomic sites in the area of the maxillary first molar with the aid of the NewTom 3G® system. Orthod. Fr. 2010, 81, 287–299. [Google Scholar] [CrossRef]
- Ichiki, S.; Muraoka, H.; Hirahara, N.; Ito, K.; Okada, H.; Kaneda, T. Age affects alveolar bone height and width in patients undergoing dental implant treatment: Findings from computed tomography imaging. J. Hard Tissue Biol. 2021, 30, 383–388. [Google Scholar] [CrossRef]
- Georgieva, I.; Damyanova, D.M.; Miteva, M. Interdental area in the aesthetic zone of maxilla—Variations of distance between interdental alveolar crest and interdental contact point in relation with age and sex. Int. J. Sci. Res. (IJSR) [Internet] 2017, 6, 566–569. [Google Scholar]
- Bittencourt, L.P.; Raymundo, M.V.; Mucha, J.N. The optimal position for insertion of orthodontic miniscrews. Rev. Odontol. 2011, 26, 133–138. [Google Scholar]
- Lee, K.J.; Joo, E.; Kim, K.D.; Lee, J.S.; Park, Y.C.; Yu, H.-S. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 486–494. [Google Scholar] [CrossRef]
- Milanovic, P.; Selakovic, D.; Vasiljevic, M.; Jovicic, N.U.; Milovanović, D.; Vasovic, M.; Rosic, G. Morphological Characteristics of the Nasopalatine Canal and the Relationship with the Anterior Maxillary Bone-A Cone Beam Computed Tomography Study. Diagnostics 2021, 11, 915. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.L.; Rustico, L.; Longo, M.; Oteri, G.; Papadopoulos, M.A.; Nucera, R. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J. Orthod. 2021, 51, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Rai, A.J.; Datarkar, A.N.; Borle, R.M. Customised screw for intermaxillary fixation of maxillofacial injuries. Br. J. Oral Maxillofac. Surg. 2009, 47, 325–326. [Google Scholar] [CrossRef]
- Elkolaly, M.A.; Hasan, H.S. MH cortical screws, a revolution aryorthodontic TADs design. J. Orthod. Sci. 2022, 11, 53. [Google Scholar] [CrossRef] [PubMed]
- Cozzani, M.; Nucci, L.; Lupini, D.; Dolatshahizand, H.; Fazeli, D.; Barzkar, E.; Naeini, E.; Jamilian, A. The ideal insertion angle after immediate loading in Jeil, Storm, and Thunder miniscrews: A 3D-FEM study. Int. Orthod. 2020, 18, 503–508. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Algabri, R.; Ibrahim, W.I.; Alhajj, M.N.; Elawady, D. Dental implant planning using artificial intelligence: A systematic review and meta-analysis. J. Prosthet. Dent. 2024; in press. [Google Scholar]
- Deglow, R.; Schröder, A.; Wriedt, S.; Wiechens, B.; Nahles, S. Augmented reality-assisted orthodontic mini-implant placement: A randomized clinical trial. BMC Oral Health 2023, 23, 77. [Google Scholar]
- Kim, S.H.; Choi, Y.S.; Hwang, E.H.; Chung, K.R.; Kook, Y.A.; Nelson, G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2007, 131 (Suppl. 4), S82–S89. [Google Scholar] [CrossRef]
- Longo, B.C.; Aquaroni, L.; Zimiani, G.S.; Cléverson, S.O. Black Ethnicity Influences Gingival and Bone Thickness: A Cross-Sectional Study. Int. J. Periodontics Restor. Dent. 2024, 44, 534–543. [Google Scholar] [CrossRef]








| Interclass Correlation | 95% Confidence Interval | Mean Difference Between Examiner 1 and Examiner 2 | Standard Deviation Between Examiner 1 and Examiner 2 | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| CP | 0.981 | 0.966 | 0.989 | −0.086 | 0.166 |
| IPP | 0.990 | 0.984 | 0.994 | −0.041 | 0.121 |
| IDW | 0.946 | 0.913 | 0.967 | 0.011 | 0.167 |
| BPD | 0.975 | 0.959 | 0.984 | −0.053 | 0.174 |
| Gender | ||||
|---|---|---|---|---|
| Frequency | Percent | Valid Percent | Cumulative Percent | |
| Male | 23 | 35.4 | 35.4 | 35.4 |
| Female | 42 | 64.6 | 64.6 | 100.0 |
| Total | 65 | 100.0 | 100.0 | |
| Age groups | ||||
| 15–20 | 17 | 26.2 | 26.2 | 26.2 |
| 21–30 | 19 | 29.2 | 29.2 | 55.4 |
| 31–40 | 13 | 20.0 | 20.0 | 75.4 |
| 40+ | 16 | 24.6 | 24.6 | 100.0 |
| Total | 65 | 100.0 | 100.0 | |
| N | Mean | Std. Deviation | 95% Confidence Interval for Mean | Sig. | |||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Regio 1 CP-IPP | 15–20 | 17 | 12.49 | 1.11 | 11.92 | 13.06 | 0.002 |
| 21–30 | 19 | 13.67 | 1.15 | 13.11 | 14.22 | ||
| 31–40 | 13 | 13.99 | 1.08 | 13.34 | 14.64 | ||
| 40+ | 16 | 13.15 | 1.18 | 12.52 | 13.78 | ||
| Total | 65 | 13.30 | 1.24 | 12.99 | 13.60 | ||
| Regio 2 CP-IPP | 15–20 | 17 | 11.73 | 1.43 | 11.00 | 12.47 | 0.004 |
| 21–30 | 19 | 13.43 | 1.27 | 12.82 | 14.05 | ||
| 31–40 | 13 | 13.08 | 1.08 | 12.43 | 13.73 | ||
| 40+ | 16 | 12.71 | 1.61 | 11.85 | 13.57 | ||
| Total | 65 | 12.74 | 1.49 | 12.37 | 13.11 | ||
| Regio 1 C1-IPP | 15–20 | 17 | 15.22 | 0.86 | 14.78 | 15.66 | 0.016 |
| 21–30 | 19 | 15.87 | 1.06 | 15.36 | 16.38 | ||
| 31–40 | 13 | 15.84 | 1.07 | 15.19 | 16.48 | ||
| 40+ | 16 | 15.27 | 0.97 | 14.75 | 15.78 | ||
| Total | 65 | 15.55 | 1.02 | 15.29 | 15.80 | ||
| Regio 1 C2-IPP | 15–20 | 17 | 13.38 | 0.86 | 12.93 | 13.82 | 0.000 |
| 21–30 | 19 | 14.83 | 0.98 | 14.35 | 15.30 | ||
| 31–40 | 13 | 14.72 | 0.96 | 14.14 | 15.30 | ||
| 40+ | 16 | 14.24 | 1.38 | 13.51 | 14.97 | ||
| Total | 65 | 14.28 | 1.19 | 13.99 | 14.58 | ||
| Regio 3 CP-IPP | 15–20 | 17 | 12.15 | 1.14 | 11.56 | 12.73 | 0.026 |
| 21–30 | 19 | 12.80 | 0.96 | 12.34 | 13.26 | ||
| 31–40 | 13 | 13.22 | 0.82 | 12.73 | 13.72 | ||
| 40+ | 16 | 12.62 | 0.83 | 12.18 | 13.06 | ||
| Total | 65 | 12.67 | 1.00 | 12.42 | 12.92 | ||
| Regio 2 C1—IPP | 15–20 | 17 | 15.23 | 0.87 | 14.78 | 15.67 | 0.028 |
| 21–30 | 19 | 15.98 | 0.95 | 15.52 | 16.43 | ||
| 31–40 | 13 | 15.98 | 0.94 | 15.41 | 16.55 | ||
| 40+ | 16 | 15.31 | 0.94 | 14.81 | 15.80 | ||
| Total | 65 | 15.62 | 0.97 | 15.38 | 15.86 | ||
| Regio 2′ CP-IPP | 15–20 | 17 | 11.88 | 1.37 | 11.18 | 12.59 | 0.003 |
| 21–30 | 19 | 13.57 | 1.14 | 13.02 | 14.12 | ||
| 31–40 | 13 | 12.84 | 1.28 | 12.06 | 13.61 | ||
| 40+ | 16 | 12.68 | 1.37 | 11.95 | 13.41 | ||
| Total | 65 | 12.76 | 1.41 | 12.42 | 13.11 | ||
| Regio 2′ C1-IPP | 15–20 | 17 | 14.97 | 1.07 | 14.42 | 15.52 | 0.003 |
| 21–30 | 19 | 16.19 | 1.07 | 15.67 | 16.71 | ||
| 31–40 | 13 | 15.91 | 1.28 | 15.14 | 16.68 | ||
| 40+ | 16 | 15.16 | 1.75 | 14.23 | 16.10 | ||
| Total | 65 | 15.56 | 1.38 | 15.22 | 15.90 | ||
| Regio 2′ C2-IPP | 15–20 | 17 | 13.38 | 1.07 | 12.83 | 13.94 | 0.003 |
| 21–30 | 19 | 14.94 | 1.06 | 14.42 | 15.45 | ||
| 31–40 | 13 | 14.65 | 0.89 | 14.11 | 15.19 | ||
| 40+ | 16 | 14.46 | 1.70 | 13.55 | 15.36 | ||
| Total | 65 | 14.35 | 1.34 | 14.02 | 14.69 | ||
| Regio 3′ CP-IPP | 15–20 | 17 | 12.37 | 0.73 | 12.00 | 12.75 | 0.043 |
| 21–30 | 19 | 12.57 | 0.96 | 12.11 | 13.04 | ||
| 31–40 | 13 | 13.07 | 0.84 | 12.57 | 13.58 | ||
| 40+ | 16 | 12.26 | 0.56 | 11.96 | 12.56 | ||
| Total | 65 | 12.54 | 0.83 | 12.34 | 12.75 | ||
| Regio 3′ C1-IPP | 15–20 | 17 | 14.76 | 0.86 | 14.32 | 15.20 | 0.023 |
| 21–30 | 19 | 15.65 | 1.33 | 15.01 | 16.29 | ||
| 31–40 | 13 | 15.81 | 1.14 | 15.12 | 16.50 | ||
| 40+ | 16 | 14.97 | 1.03 | 14.42 | 15.51 | ||
| Total | 65 | 15.28 | 1.17 | 14.99 | 15.57 | ||
| Regio 1 IDW Level D | 15–20 | 17 | 2.02 | 0.53 | 1.75 | 2.30 | 0.025 |
| 21–30 | 19 | 2.60 | 0.63 | 2.29 | 2.91 | ||
| 31–40 | 13 | 2.57 | 0.71 | 2.14 | 3.00 | ||
| 40+ | 16 | 2.52 | 0.31 | 2.35 | 2.68 | ||
| Total | 65 | 2.42 | 0.60 | 2.27 | 2.57 | ||
| Regio 2′ IDW Level C | 15–20 | 17 | 1.80 | 0.58 | 1.50 | 2.10 | 0.039 |
| 21–30 | 19 | 2.24 | 0.62 | 1.94 | 2.54 | ||
| 31–40 | 13 | 2.25 | 0.62 | 1.88 | 2.63 | ||
| 40+ | 16 | 1.85 | 0.44 | 1.62 | 2.09 | ||
| Total | 65 | 2.03 | 0.60 | 1.88 | 2.18 | ||
| Regio 2′ IDW Level D | 15–20 | 17 | 1.44 | 0.58 | 1.15 | 1.74 | 0.014 |
| 21–30 | 19 | 1.99 | 0.63 | 1.68 | 2.29 | ||
| 31–40 | 13 | 1.93 | 0.64 | 1.55 | 2.32 | ||
| 40+ | 16 | 1.52 | 0.45 | 1.28 | 1.76 | ||
| Total | 65 | 1.72 | 0.62 | 1.57 | 1.87 | ||
| Regio 1 IDW Level D | Male | 23 | 2.54 | 0.47 | 2.34 | 2.74 | 0.048 |
| Female | 42 | 2.36 | 0.66 | 2.16 | 2.57 | ||
| Total | 65 | 2.42 | 0.59 | 2.27 | 2.57 | ||
| Regio 2′ BPD Level D | 15–20 | 17 | 7.77 | 1.96 | 6.76 | 8.78 | 0.041 |
| 21–30 | 19 | 6.37 | 1.33 | 5.73 | 7.01 | ||
| 31–40 | 13 | 6.85 | 1.00 | 6.25 | 7.45 | ||
| 40+ | 16 | 7.05 | 1.15 | 6.43 | 7.66 | ||
| Total | 65 | 7.00 | 1.49 | 6.63 | 7.37 | ||
| Regio 1 BPD Level A | Male | 23 | 7.90 | 0.97 | 7.49 | 8.33 | 0.022 |
| Female | 42 | 7.38 | 0.82 | 7.12 | 7.63 | ||
| Total | 65 | 7.57 | 0.91 | 7.34 | 7.79 | ||
| Regio 1 BPD Level B | Male | 23 | 7.56 | 0.92 | 7.16 | 7.96 | 0.031 |
| Female | 42 | 7.10 | 0.74 | 6.87 | 7.33 | ||
| Total | 65 | 7.26 | 0.83 | 7.05 | 7.47 | ||
| Regio 1 BPD Level C | Male | 23 | 7.07 | 0.85 | 6.70 | 7.44 | 0.032 |
| Female | 42 | 6.69 | 0.69 | 6.48 | 6.91 | ||
| Total | 65 | 6.83 | 0.77 | 6.64 | 7.02 | ||
| Regio | Level | % |
|---|---|---|
| 1 | A | 87.7 |
| B | 73.8 | |
| C | 40.0 | |
| D | 15.4 | |
| 2 | A | 24.6 |
| B | 18.5 | |
| C | 10.8 | |
| D | 9.2 | |
| 3 | A | 70.8 |
| B | 53.8 | |
| C | 16.9 | |
| D | 9.2 | |
| 2′ | A | 21.5 |
| B | 10.8 | |
| C | 4.6 | |
| D | 4.6 | |
| 3′ | A | 70.8 |
| B | 58.5 | |
| C | 24.6 | |
| D | 10.8 |
| IDW and BPD | P. Correlation | Sig. | 95% Confidence Interval (CI) | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Regio 1 Level C | 0.250 | 0.045 | −0.027 | 0.399 |
| Regio 1 Level D | 0.262 | 0.035 | 0.118 | 0.508 |
| Regio 2 Level B | 0.258 | 0.038 | −0.013 | 0.522 |
| Regio 2 Level C | 0.268 | 0.031 | 0.019 | 0.469 |
| Regio 3 Level A | 0.637 | 0.000 | 0.418 | 0.782 |
| Regio 3 Level B | 0.512 | 0.000 | 0.267 | 0.711 |
| Regio 3 Level C | 0.469 | 0.000 | 0.229 | 0.673 |
| Regio 3 Level D | 0.456 | 0.000 | 0.166 | 0.668 |
| Regio 3′ Level A | 0.363 | 0.003 | 0.116 | 0.564 |
| Regio 3′ Level B | 0.363 | 0.003 | 0.068 | 0.652 |
| Regio 3′ Level C | 0.271 | 0.029 | −0.039 | 0.532 |
| Regio 3′ Level D | 0.271 | 0.029 | −0.022 | 0.529 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakovljevic, I.; Vasiljevic, M.; Milanovic, J.; Stevanovic, M.Z.; Jovicic, N.; Stepovic, M.; Ristic, V.; Selakovic, D.; Rosic, G.; Milanovic, P.; et al. Importance of CBCT Analysis in the Preoperative Planning of TAD Placement in the Anterior Maxillary Region. Appl. Sci. 2025, 15, 6866. https://doi.org/10.3390/app15126866
Jakovljevic I, Vasiljevic M, Milanovic J, Stevanovic MZ, Jovicic N, Stepovic M, Ristic V, Selakovic D, Rosic G, Milanovic P, et al. Importance of CBCT Analysis in the Preoperative Planning of TAD Placement in the Anterior Maxillary Region. Applied Sciences. 2025; 15(12):6866. https://doi.org/10.3390/app15126866
Chicago/Turabian StyleJakovljevic, Iva, Milica Vasiljevic, Jovana Milanovic, Momir Z. Stevanovic, Nemanja Jovicic, Milos Stepovic, Vladimir Ristic, Dragica Selakovic, Gvozden Rosic, Pavle Milanovic, and et al. 2025. "Importance of CBCT Analysis in the Preoperative Planning of TAD Placement in the Anterior Maxillary Region" Applied Sciences 15, no. 12: 6866. https://doi.org/10.3390/app15126866
APA StyleJakovljevic, I., Vasiljevic, M., Milanovic, J., Stevanovic, M. Z., Jovicic, N., Stepovic, M., Ristic, V., Selakovic, D., Rosic, G., Milanovic, P., & Arnaut, A. (2025). Importance of CBCT Analysis in the Preoperative Planning of TAD Placement in the Anterior Maxillary Region. Applied Sciences, 15(12), 6866. https://doi.org/10.3390/app15126866








