1. Introduction
With the advent of digital dentistry, orthodontics has ushered in a more diverse patient population seeking more esthetic treatment options. More specifically, clear aligner therapy (CAT) has sparked the interest of patients pursuing the correction of their smiles without the use of brackets and wires [
1,
2]. Clear aligner therapy has been shown to be an effective treatment modality in the correction of malocclusion. Through advancements in technology and materials, CAT has expanded its application from its initial stages of only the correction of simple anterior crowding to comprehensive orthodontic treatment [
3,
4,
5]. These advancements have enabled possible tooth movements of nearly any desired vector and has established an esthetic and effective treatment option.
Through its increased use in orthodontics, limitations have been noted in CAT’s ability to correct malocclusions. These limitations have been brought to light through recent comparisons in the literature of ClinCheck predictions and expressed post-treatment tooth movement [
6,
7,
8]. Blundell et al. demonstrated that Align ClinCheck software greatly overpredicts its ability to correct an anterior deep bite. This finding shows that ClinCheck software cannot accurately predict the clinical expression of intrusive movements with clear aligners. The deficiency in clinical expression was seen in 95.3% of the cases evaluated [
6]. This finding comes with great clinical relevance as more and more patients are requesting this treatment modality. The issues with predicted tooth movement in CAT was even further highlighted in research by Al-Balaa et al., where anterior intrusive movements were specifically evaluated [
7]. Again, the predictability of CAT was questioned as it was found to have significant insufficiencies in its ability to intrude the dentition. One must question how and why these large discrepancies exist so that more accurate treatment planning and increased efficiency in tooth movement can take place.
In mandibular anterior intrusion, the inaccuracy of ClinCheck’s predictions in the vertical dimension should also prompt the questioning of its accuracy in a horizontal plane as well. Intrusive movements of lower incisors have historically been accompanied by the tipping or flaring of the lower incisors, also known as relative intrusion, as demonstrated by Burstone in the 1970s [
8]. The intrusion accomplished with Invisalign CAT should be investigated for the presence of relative intrusion and an increased incisor mandibular plane angle (IMPA). This holds great clinical importance as incisor position can have a significant impact on facial esthetics and profile [
9]. There has also been evidence to suggest that IMPA can play a crucial role in long-term post-orthodontic treatment stability; thus, controlling such proclination can improve the predictability of treatment [
10].
Furthermore, all existing studies evaluating ClinCheck prediction have only evaluated orthodontic movements in non-growing adult patients. As CAT is being used more frequently in growing patients, it is imperative that an evaluation of efficacy in this patient population be completed. One might assume that a closer adherence to ClinCheck prediction would be observed based on the increased velocity of orthodontic tooth movement seen in younger subjects [
11]. However, that has yet to be demonstrated in clinical studies related to CAT. Thus, further investigation of the efficacy of CAT in children must be conducted.
The aim of this current study is to evaluate the predictability of mandibular incisor bodily intrusion in both growing and non-growing patients using CAT and ClinCheck software and evaluating the angular control of mandibular incisors during intrusive movements.
The following hypotheses will be tested: the primary hypothesis—there is no difference between projected ClinCheck mean intrusion and angular control and clinically expressed mean intrusion and angular control of mandibular incisor in patients with CAT; the secondary hypothesis—there is no difference in ClinCheck predictions and clinical expression between growing and non-growing patients.
2. Materials and Methods
This retrospective study received Institutional Review Board exemption (STUDY00007083) at the University of Rochester Eastman Institute for Oral Health.
The samples consisted of 48 patients who started and completed orthodontic treatment at the private office of ABO-certified orthodontist Dr. Robert Tarby, in NJ, USA between the dates of 1 January 2012 and 18 July 2019 using Invisalign CAT.
The following inclusion criteria was applied: (1) patients with no systemic diseases/conditions and/or craniofacial syndromes, (2) non-smoking patients, (3) patients who do not require extractions or surgery, (4) patients presenting with a mild to moderate overbite at the initiation of orthodontic treatment (>2 mm), (5) patients with at least 1 mm of planned mandibular incisor intrusion in the ClinCheck software, (6) radiographs of adequate diagnostic quality, (7) patients with no history of previous orthodontic treatment, (8) patients with mild to moderate dental crowding (<5 mm).
The following excluding criteria was applied: (1) patients with systemic diseases and/or craniofacial syndromes, (2) patients with severe skeletal Class III (ANB < −2°) or Class II malocclusion (ANB > 5°), (3) patients exhibiting anterior open bite, impacted/missing teeth, and/or severe crowding requiring OT with extractions and/or orthognathic surgery.
All eligible patients possessed pre-treatment (T1) and post-treatment (T2) lateral cephalometric radiographs, an iTero (Align Technologies, San Jose, CA, USA) digital scan, and an initial ClinCheck with all desired tooth movements in millimeters (mm) and degrees.
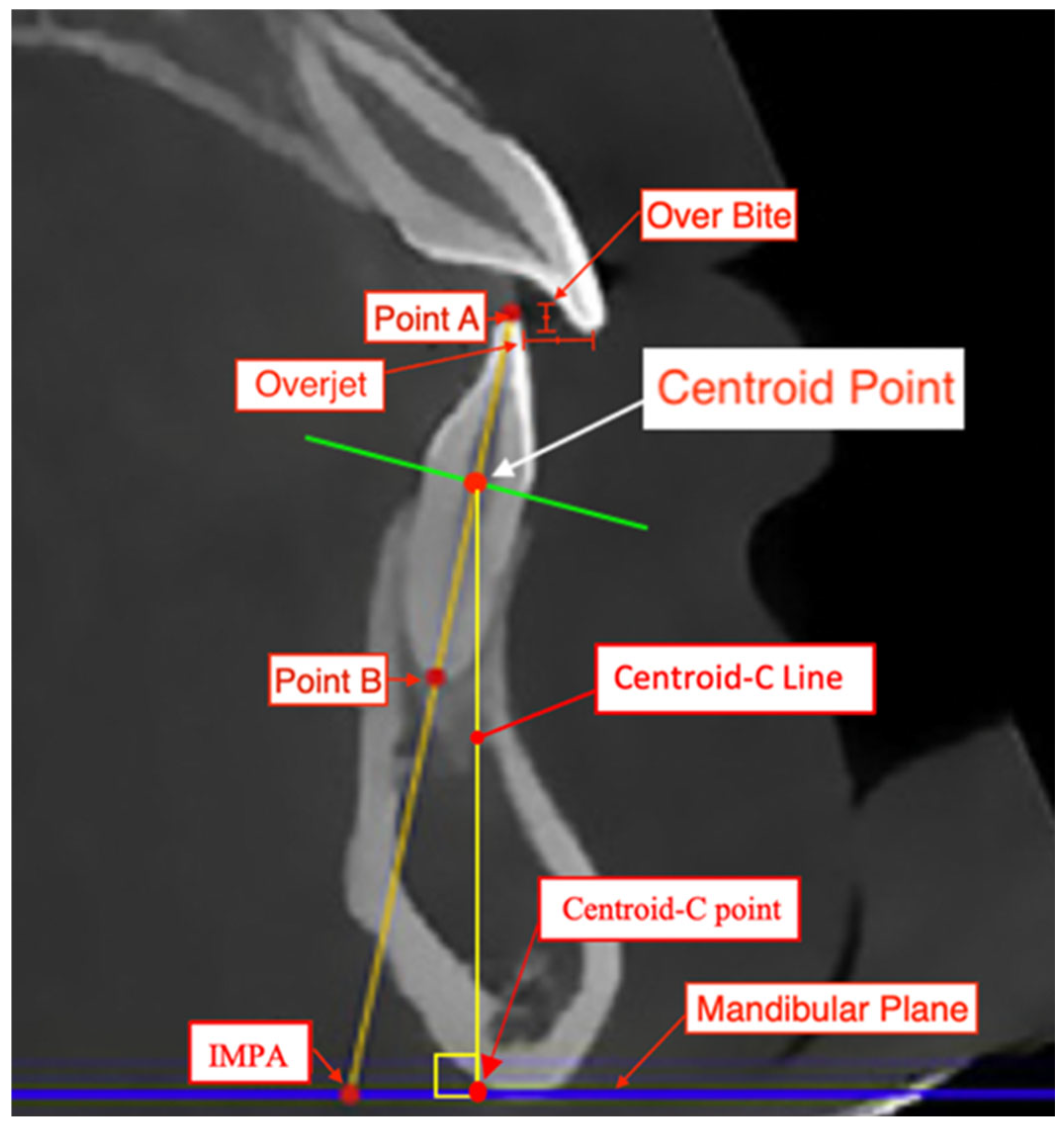
All measurements were conducted by one examiner (CB) who was pre-calibrated and trained in cephalometric assessment. The same examiner (CB) remeasured records from 10 randomly selected patients to assess intra-observer reliability. A second calibrated examiner (AG) measured records from 10 randomly selected patients to assess inter-observer reliability. The methodology for assessment will be similar to that in the study by Al-Balaa et al. [
7] in determining the total intrusive movement of mandibular central incisors. First, the landmarks of a centroid point were established at the intersection of a horizontal line constructed from the cementoenamel junction (CEJ) of the facial and lingual surfaces of the lower central incisor and the vertical axis of the lower central incisor on a lateral cephalogram (
Figure 1). The IMPA, L1 to APo, and L1 to NB were established using Dolphin software version 11.95 and the Steiner [
12], Tweed [
13], and Ricketts [
14] cephalometric analyses (
Figure 2). These measurements were made on pre-treatment (T1) and on post-treatment (T2) lateral cephalograms. A tooth’s total intrusion was determined by the decrease in distance from the centroid point to the mandibular plane (Centroid-C Line) in T1 to T2. IMPA, L1 to APo, and L1 to NB were also recorded for T1 and T2. The total intrusion of each tooth was then contrasted with the total intrusive movement predicted in the ClinCheck software [
15,
16,
17,
18]. The change in inclination of IMPA, L1 to APo, and L1 to NB from T1 to T2 were also contrasted with the predicted degree of change in the ClinCheck software.
Statistical Analysis
To analyze cephalometric changes before and after CAT, and to assess the consistency between the projected ClinCheck mean intrusion and angular control compared to the actual clinical CAT-based mean intrusion and angular control of mandibular incisors on lateral cephalometric images, paired sample t-tests were employed. Differences between the growing and non-growing groups were evaluated using a repeated measures ANOVA with Tukey post hoc analysis. For statistical significance, an alpha level of 0.05 and a power of 80% were applied. With a pooled standard deviation of 1 mm, a sample size of 48 ClinCheck-based intrusion predictions and 48 pre–post sets of cephalometric images would be necessary to detect a 0.58 mm difference between the two groups. The statistical software utilized was SAS Release: 3.81 (Enterprise Edition), Copyright © 2012–2020, SAS Institute Inc., Cary, NC, USA.
3. Results
3.1. Inter- and Intra-Observer Error
The intra-observer reliability test was conducted by instructing the investigator (CB) to retrace 10 randomly chosen radiographs. Additionally, for the inter-observer reliability test, a second examiner (AG) retraced 10 randomly selected radiographs, and Cronbach’s Alpha test was utilized to assess the reliability between measurements. Evidence of high reliability was established with the alpha levels of α = 0.995 (T1) and α = 0.998 (T2).
3.2. Characteristics of the Study Sample
A total of 48 patients (12 male and 36 female) with a mean age of 19.79 ± 11.78 years were included. The total group was divided into growing and non-growing subgroups. The growing group included 30 patients (19 male and 11 female) with a mean age of 13.5 ± 2.08 years. The non-growing group included 18 patients (1 male and 17 female) with a mean age of 30.28 ± 13.79 years. All included patients were treated using Invisalign with ClinCheck software where treatment mechanics did not include surgery or extractions. Throughout the Invisalign treatment, the overall mean number of refinements was 7.44 ± 2.31; the growing group had 6.87 ± 1.74, and the non-growing group had 8.39 ± 2.85 refinements (
Table 1).
The ClinCheck-predicted tooth movement characteristics included showed an overall mean lower incisor intrusion of 2.32 ± 1.82 mm; the growing group was 2.27 ± 1.16 mm, and the non-growing group was 2.4 ± 1.24 mm. The overall lower incisor change in inclination was 4.6 ± 6.3 degrees; the growing group was 4.27 ± 6.25 degrees, and the non-growing group was 5.13 ± 6.25 degrees (
Table 2).
3.3. Comparison of the Main Treatment Variable/Outcome Across Time Points and Among Groups
Table 3 summarizes the descriptive values of Centroid-C, IMPA, L1-NB, L1-APo, OB, and OJ at T1 and T2 for the overall, growing, and non-growing groups. The overall, growing, and non-growing groups showed no significant difference in mean intrusion from T1 to T2 using Centroid-C (
p = 0.27,
p = 0.31,
p = 0.67, respectively). The overall, growing, and non-growing groups showed no significant difference in mean change in lower incisor angulation from T1 and T2 using IMPA (
p = 0.37,
p = 0.51,
p = 0.56, respectively). The overall, growing, and non-growing groups showed no significant difference in mean change in lower incisor angulation between T1 and T2 using L1-NB (
p = 0.62,
p = 0.98,
p = 0.28, respectively). The overall, growing, and non-growing groups showed no significant difference in mean change in lower incisor angulation between T1 and T2 using L1-APo (
p = 0.09,
p = 0.095,
p = 0.57, respectively). The overall and growing groups showed a significant difference in mean change in OB and OJ between T1 and T2 where
p < 0.001. The non-growing group showed no significant change in OB between T1 and T2 where
p = 0.09; however, there was a significant change in OJ where
p = 0.02.
Table 4 summarizes the comparison of predicted ClinCheck tooth movements to the clinical expression of subsequent CAT using the variables of Centroid-C, IMPA, L1-NB, L1-APo. For all variables, there was a significant difference observed between predicted values and clinical expression. The Centroid-C comparison value was significant with
p < 0.001, the IMPA comparison was significant with
p = 0.003, the L1-NB was significant with
p = 0.009, and the L1-APo comparison was significantly different with
p = 0.005.
3.4. Repeated Measures ANOVA with Tukey Post Hoc
Table 5 summarizes the comparison of discrepancies between the ClinCheck prediction and clinical expression between the groups of growing and non-growing patients. There was no significant difference found between any of the included variables of Centroid-C (
p = 0.87), IMPA (
p = 0.58), L1-NB (
p = 0.72), and L1-APo (
p = 0.886).
4. Discussion
Invisalign and ClinCheck software were adopted in the current study for its acceptance and prevalence among practitioners. The findings of this study coincide with previous research in that the predictions in ClinCheck software significantly overpredict orthodontic tooth movement. This was evident in both angular control and bodily intrusion, where clinical expression was significantly less than predictions made in ClinCheck. The current study showed a mean bodily intrusion of only 9.5% of that of the software prediction, a finding similar to that in the study by Al-Balaa et al. [
7], where lower incisor intrusion was under expressed clinically. An analogous result was seen with angular control, where the planned correction that was achieved was 17.2% for IMPA, 12% for L1-NB, and 26.3% for L1-APo. Despite the lack of homogeneity between clinical expression and software prediction, OB and OJ were both significantly improved following CAT. This finding would suggest that significant improvement of deep bite can still be achieved with CAT and is a result of cumulative tooth movements outside of the variables evaluated in this study. In the current study, as well as previous research, overcorrection of malocclusions in pre-treatment software planning is indicated, as only a fraction of planned movements are achieved clinically [
19,
20]. This approach may allow for final tooth positions following CAT to more closely parallel ideal desired tooth positions. A more comprehensive study is needed to fully understand the required percent of overcorrection of all desired tooth movements using CAT.
The current study, unlike previous research, has also investigated and compared the efficacy of CAT in both growing and non-growing populations in terms of variables related to anterior deep bite correction. All parameters of tooth movement were assessed collectively within the patient population, as well as individually within the growing and non-growing subgroups. The results of the current study failed to show statistical differences in any of the tooth movement variables included in this study. Angular control and bodily lower incisor intrusion were comparable for both the growing and non-growing groups. This study demonstrated comparable outcomes across both growing and non-growing groups, highlighting the potential effectiveness of CAT in diverse patient demographics [
19].
In summary, this study sheds light on the critical role of Invisalign and ClinCheck software in contemporary orthodontic practice, particularly in the context of correcting anterior deep bite. Consistent with previous research, the current study reveals a tendency for ClinCheck software to overpredict orthodontic tooth movement, notably in angular control and bodily intrusion variables. However, despite these discrepancies, the results demonstrate significant improvements in OB and OJ following CAT, indicating the potential effectiveness of this approach in achieving clinically meaningful outcomes [
20]. Furthermore, the investigation into the efficacy of CAT in both growing and non-growing populations reinforces its versatility and applicability across patient demographics. While statistical differences were not observed in the tooth movement variables analyzed, the comparable outcomes between these groups highlight the potential of CAT as a viable treatment option. Moving forward, the findings suggest the importance of overcorrection in pre-treatment software planning to better align final tooth positions with ideal desired outcomes [
20]. Nevertheless, further comprehensive studies are warranted to elucidate the optimal degree of overcorrection required for all desired tooth movements using CAT.
Limitations
This study has a number of limitations that should be acknowledged. Firstly, there is the factor of patient compliance when utilizing CAT. The study included subjects that completed initial series of aligners without major signs of fitment issues in efforts to minimize the effects of non-compliance in the study. Additionally, the treating orthodontist only provided subjects who demonstrated attendance to all scheduled appointments. This study also was reliant on two-dimensional radiography. More accurate three-dimensional imaging is now available in clinical practice and should be considered in future assessments. Finally, this study did not evaluate the inclusion or type of attachments used. CAT is typically accompanied by a number of resin composite attachments to aid in tooth movement, where location and shape are optimized through software algorithms. The inclusion of attachment type may influence the efficacy of some related tooth movements and results achieved.
5. Conclusions
Clinical expression of Invisalign aligners were significantly less than the predictions made in the ClinCheck software in lower incisor bodily intrusion and angular control.
No significant difference was observed between growing and non-growing populations in anterior deep bite correction with CAT.
The primary hypothesis, “There is no difference between projected ClinCheck mean intrusion and angular control and clinically expressed mean intrusion and angular control of mandibular incisor in patients with CAT”, was rejected.
The secondary hypothesis, “There is no difference in ClinCheck predictions and clinical expression between growing and non-growing patients”, was accepted.
Overcorrection in pre-treatment software planning is recommended.
Author Contributions
Conceptualization, P.E.R., C.B. and R.T.; methodology, C.B., P.E.R. and D.M.; validation, P.E.R., C.B. and D.M.; formal analysis, C.B. and A.B.B.; investigation, C.B.; resources, R.T.; data curation, C.B. and R.T. writing—original draft preparation, C.B.; writing—review and editing, P.E.R. and D.M.; supervision, P.E.R.; project administration, P.E.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The RSRB office determined that the proposed study activity (retrospective cephalometric) is not research involving human subjects as defined by DHHS and FDA regulations. The Institutional Review Board determined that study 00007083 does not require ethical approval. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of The University of Rochester (protocol code 00007083 approval 10 May 2022).
Informed Consent Statement
Not applicable.
Data Availability Statement
All research data applicable to the project has been presented in the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| DHHS | Department of Health and Human Services |
| FDA | US Food and Drug Administration |
References
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–276.e12; discussion 76–77. [Google Scholar] [CrossRef]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62 (Suppl. S1), 58–62. [Google Scholar] [CrossRef] [PubMed]
- Bawaskar, N.S. Anterior Crossbite and Crowding Correction with a Series of Clear Aligners Involving Lower Incisor Extraction: “The Clear Way” Case Report. Int. J. Orthod. Milwaukee 2015, 26, 29–33. [Google Scholar] [PubMed]
- Frongia, G.; Castroflorio, T. Correction of severe tooth rotations using clear aligners: A case report. Aust. Orthod. J. 2012, 28, 245–249. [Google Scholar] [PubMed]
- Houle, J.P.; Piedade, L.; Todescan, R., Jr.; Pinheiro, F.H. The predictability of transverse changes with Invisalign. Angle Orthod. 2017, 87, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Blundell, H.L.; Weir, T.; Kerr, B.; Freer, E. Predictability of overbite control with the Invisalign appliance. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Al-Balaa, M.; Li, H.; Ma Mohamed, A.; Xia, L.; Liu, W.; Chen, Y.; Omran, T.; Li, S.; Hua, X. Predicted and actual outcome of anterior intrusion with Invisalign assessed with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e275–e280. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.R. Deep overbite correction by intrusion. Am. J. Orthod. 1977, 72, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Baumrind, S.; Korn, E.L.; Boyd, R.L. Apical root resorption in orthodontically treated adults. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Yared, K.F.; Zenobio, E.G.; Pacheco, W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 6.e1–6.e8. [Google Scholar] [CrossRef] [PubMed]
- Puttaravuttiporn, P.; Wongsuwanlert, M.; Charoemratrote, C.; Leethanakul, C. Volumetric evaluation of root resorption on the upper incisors using cone beam computed tomography after 1 year of orthodontic treatment in adult patients with marginal bone loss. Angle Orthod. 2018, 88, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Tweed, C.H. The Application of the Principles of the Edge-wise Arch in the Treatment of Malocclusions: I. Angle Orthod. 1941, 11, 5–11. [Google Scholar]
- Ricketts, R.M. A foundation for cephalometric communication. Am. J. Orthod. 1960, 46, 330–357. [Google Scholar] [CrossRef]
- Liu, W.; Shao, J.; Li, S.; Al-Balaa, M.; Xia, L.; Li, H.; Hua, X. Volumetric cone-beam computed tomography evaluation and risk factor analysis of external apical root resorption with clear aligner therapy. Angle Orthod. 2021, 91, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Aman, C.; Azevedo, B.; Bednar, E.; Chandiramami, S.; German, D.; Nicholson, E.; Nicholson, K.; Scarfe, W.C. Apical root resorption during orthodontic treatment with clear aligners: A retrospective study using cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 842–851. [Google Scholar] [CrossRef] [PubMed]
- Linkous, E.R.; Trojan, T.M.; Harris, E.F. External apical root resorption and vectors of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Segal, G.R.; Schiffman, P.H.; Tuncay, O.C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofac. Res. 2004, 7, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.A.; Miethke, H.R. Invisalign, an innovative invisible orthodontic appliance to correct malocclusions: Advantages and limitations. Dent. Update 2012, 39, 254–256, 258–260. [Google Scholar] [CrossRef] [PubMed]
- de la Cruz, A.; Sampson, P.; Little, R.M.; Artun, J.; Shapiro, P.A. Long-term changes in arch form after orthodontic treatment and retention. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 518–530. [Google Scholar]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).