A Prototype Mechatronic Device for Upper Limb Rehabilitation and Analysis of Its Functionality
Abstract
1. Introduction
- –
- Paresis or complete paralysis;
- –
- Altered muscle tone (either increased or decreased);
- –
- Speech disorders or loss of speech;
- –
- Orofacial paralysis (e.g., swallowing and feeding difficulties);
- –
- Psychological issues such as emotional instability, depression, and personality changes;
- –
- Spasticity (exaggerated stretch reflex response).
2. Motivation and Contribution
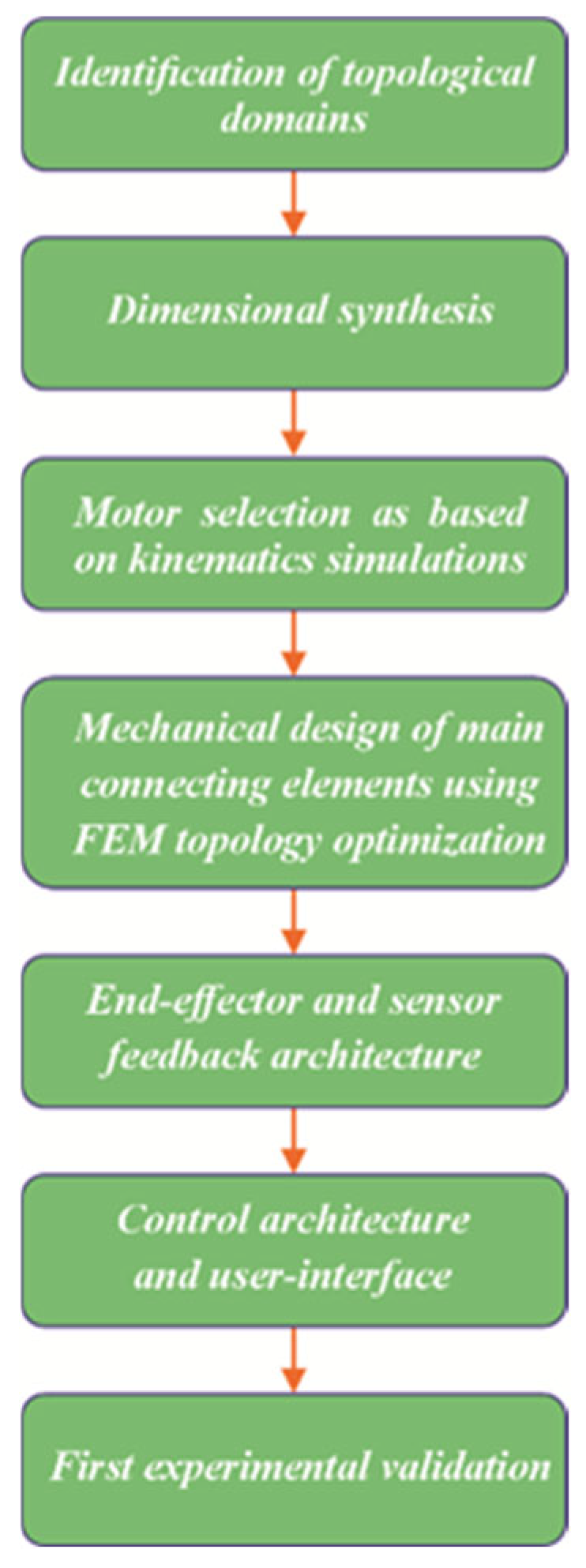
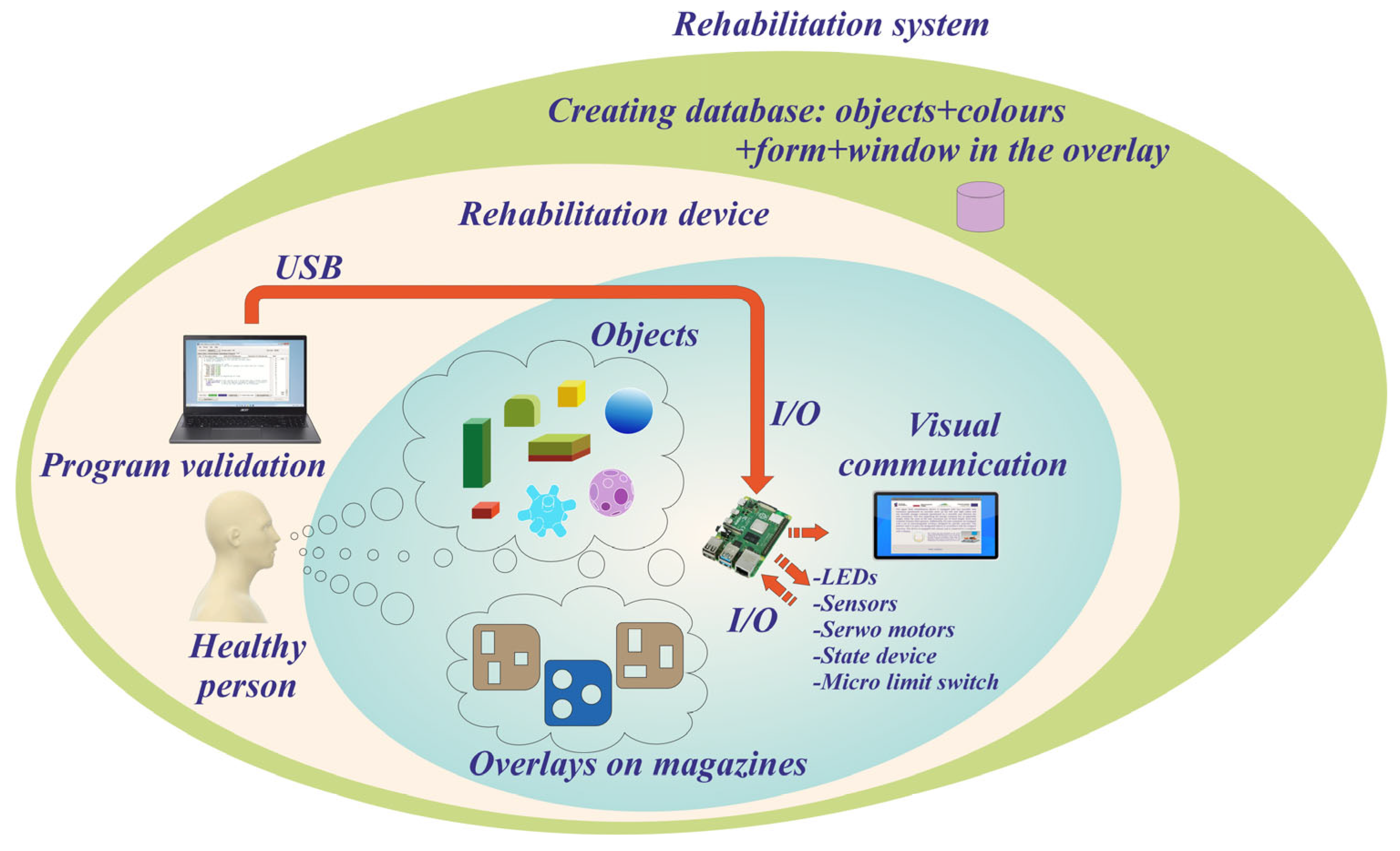
3. Concept and Design Solution for the Rehabilitation Device
3.1. Functional Assumptions of the Device
- The rehabilitation device must not require the installation of sensors or mechatronic components directly on the user’s limb.
- The solution should enable users to physically perceive the shape and texture of the manipulated objects and support the diagnosis of insufficient grip strength based on surface properties, shape, or weight. Additionally, colour coding may assist in object identification and ensure correct placement.
- The system should promote natural limb movement using real objects of varying shapes and weights. A mechatronic mechanism should facilitate the adjustable positioning of the arms and containers, thereby extending the range of motion and enhancing the rehabilitation process.
- The mechatronic system and accompanying software should incorporate diagnostic functionalities, including assessments of task completion time, object shape and weight, and the number of repetitions in cases of an incomplete or impaired task performance.
- The device should have a universal and adaptable design, allowing for adjustment to different limb lengths and configurations. It should be portable and suitable for use on tabletops or desks.
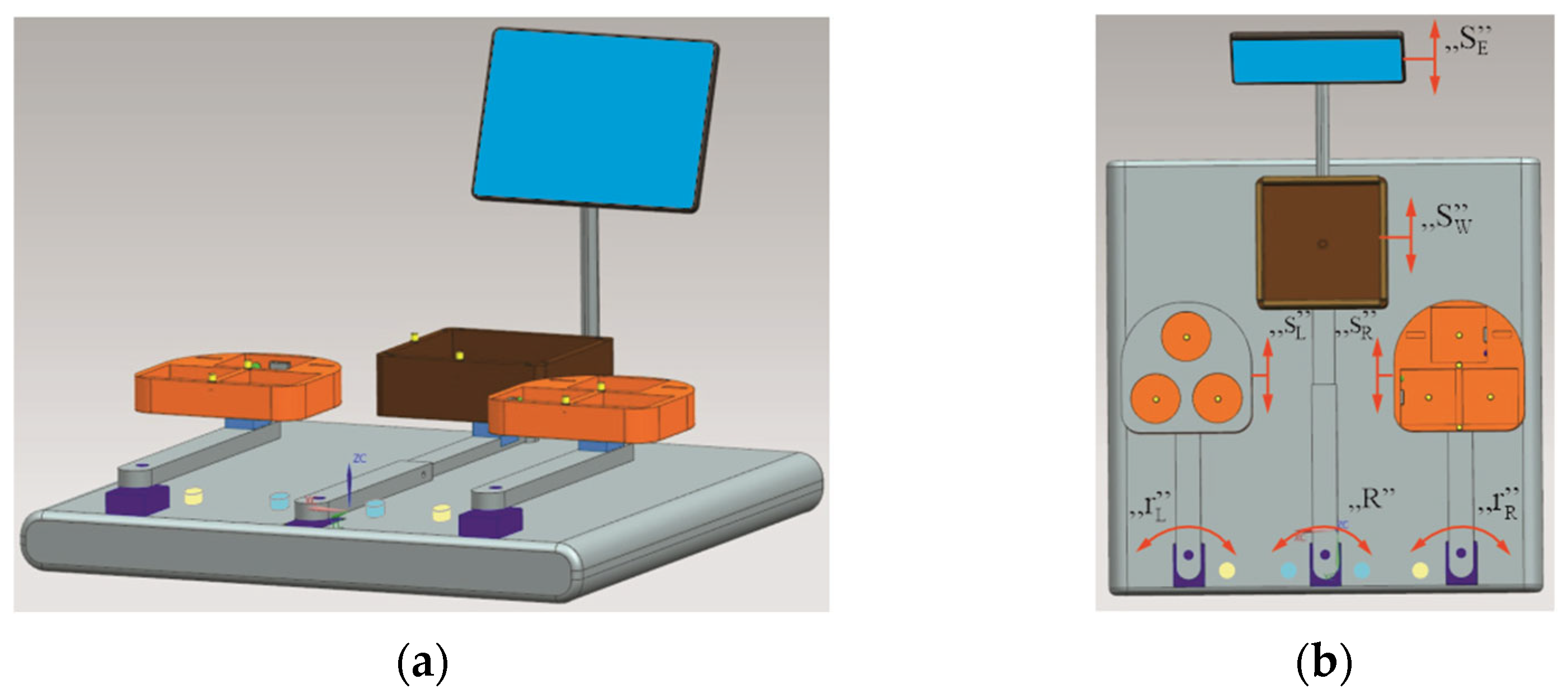
3.2. Concept
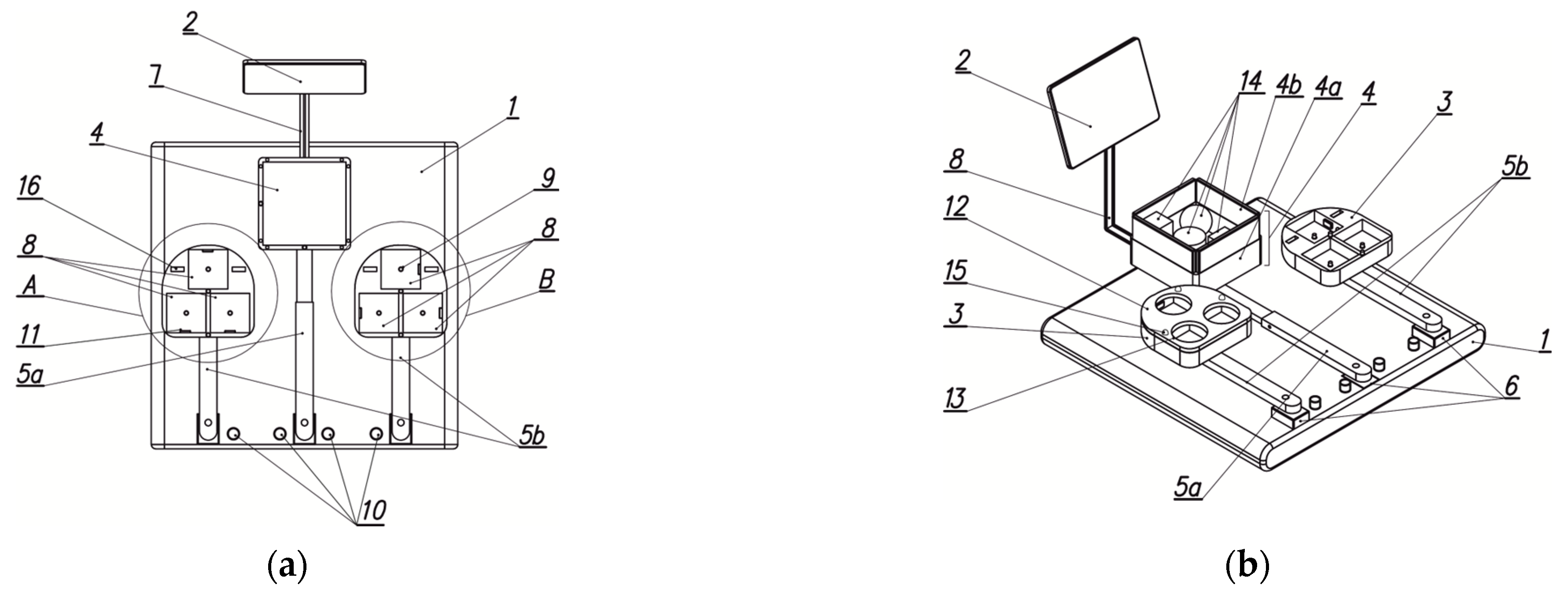
3.3. Prototype Solution of the Device
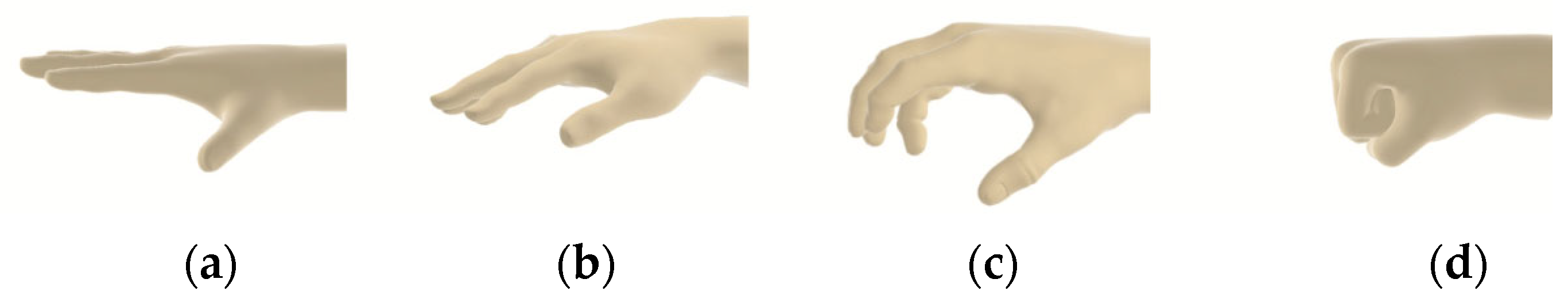
3.4. Objects Used for Exercises
- No. 1: Smooth and uniform surface;
- No. 2: Spherical indentations;
- No. 3: Variable-shaped surface protrusions;
- No. 4: Spherical protrusions;
- No. 5: Cylindrical protrusions.
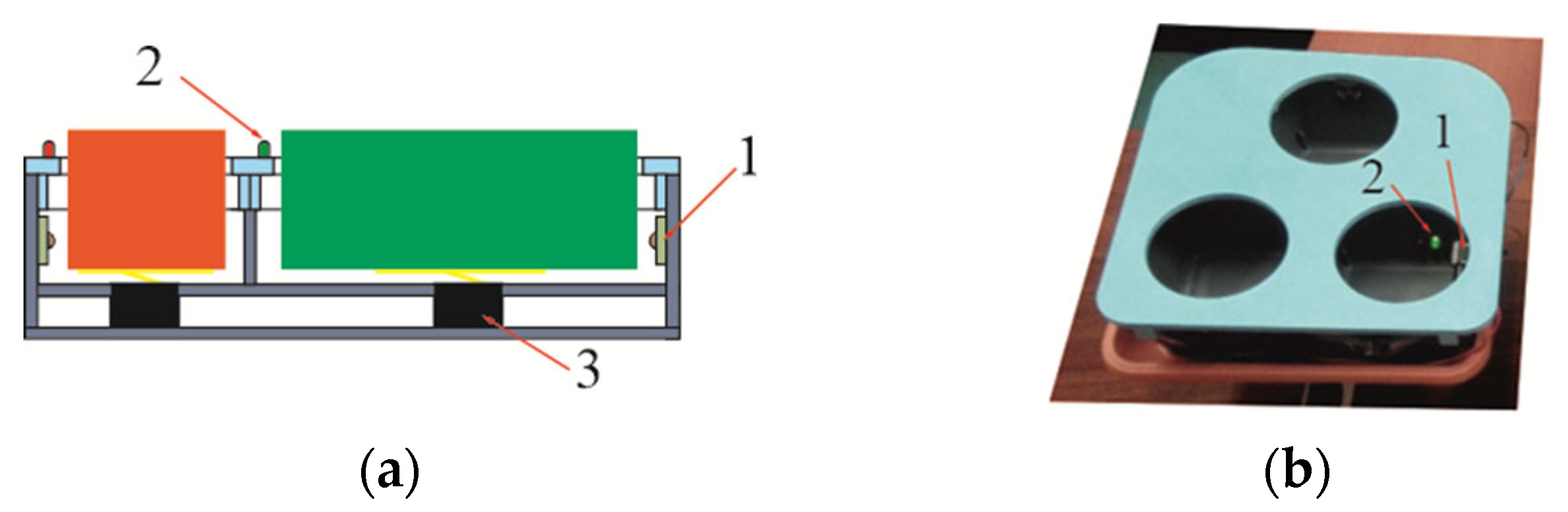
3.5. Overlays for Geometric Object Identification
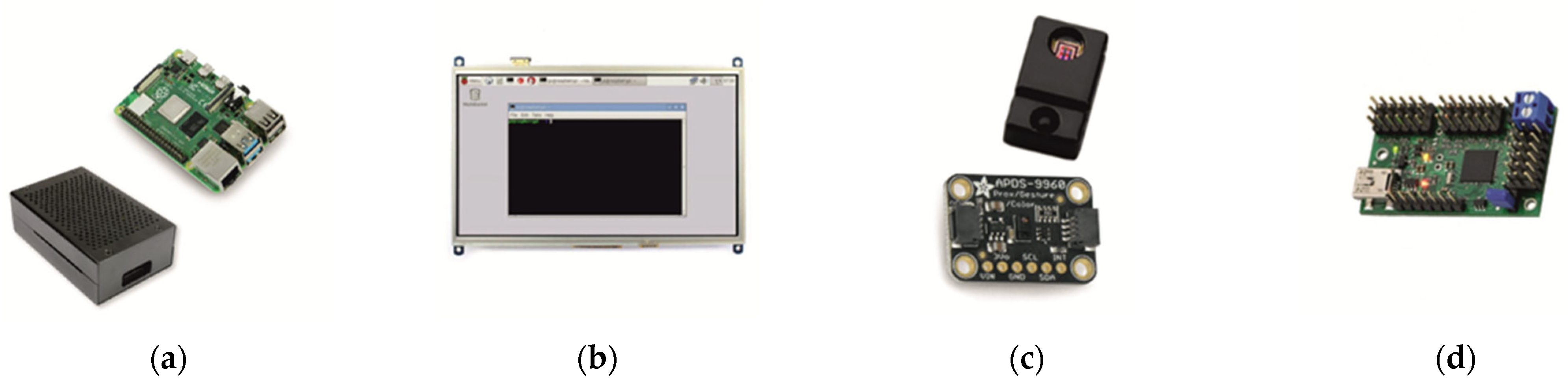
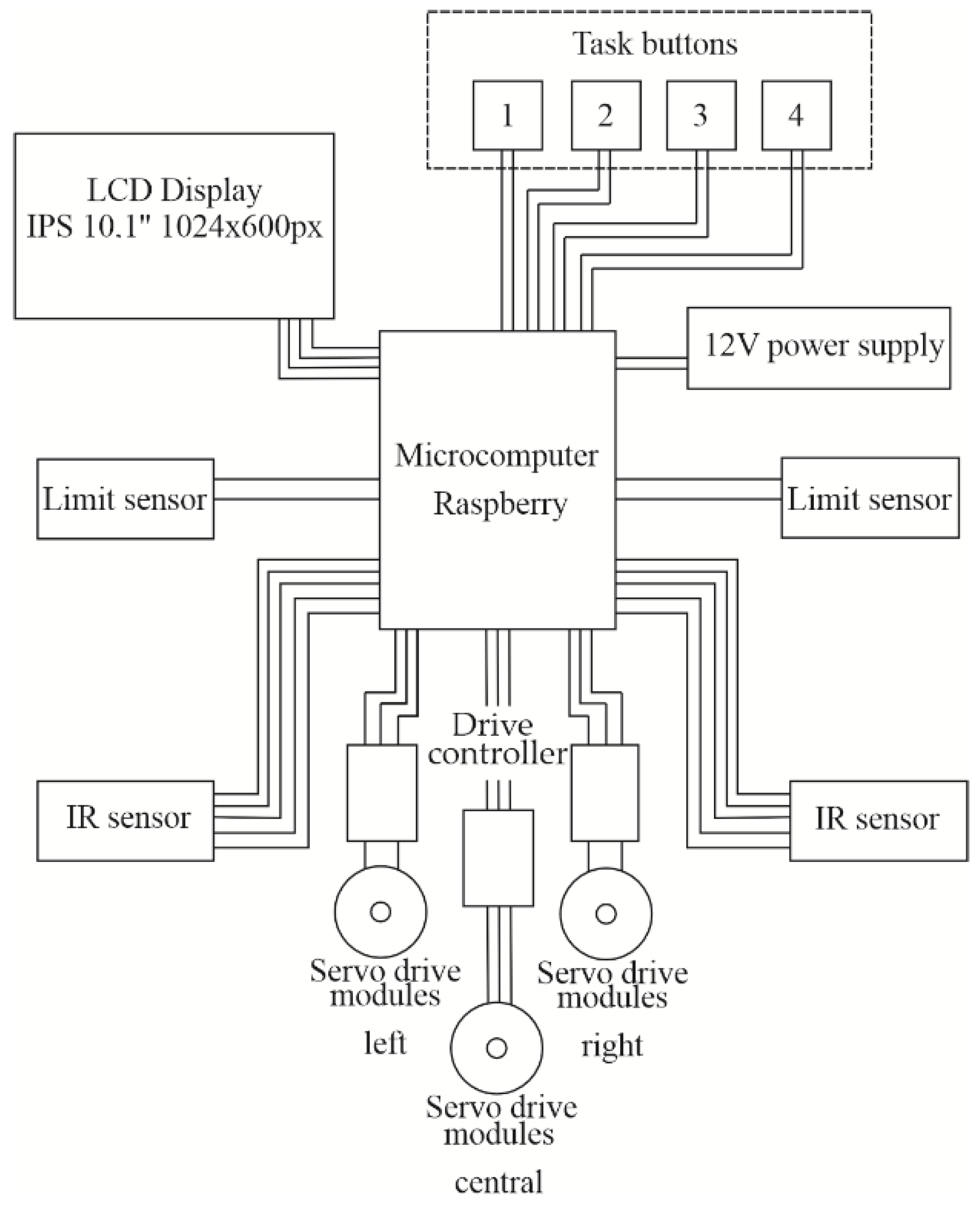
3.6. Characteristics of the Electronic System
- System-on-Chip: Broadcom 2711;
- Processor: Quad-core ARM Cortex-A72, 1.5 GHz;
- Memory: 8 GB LPDDR4 SDRAM;
- Graphics: Broadcom VideoCore VI.
4. Device Functionality
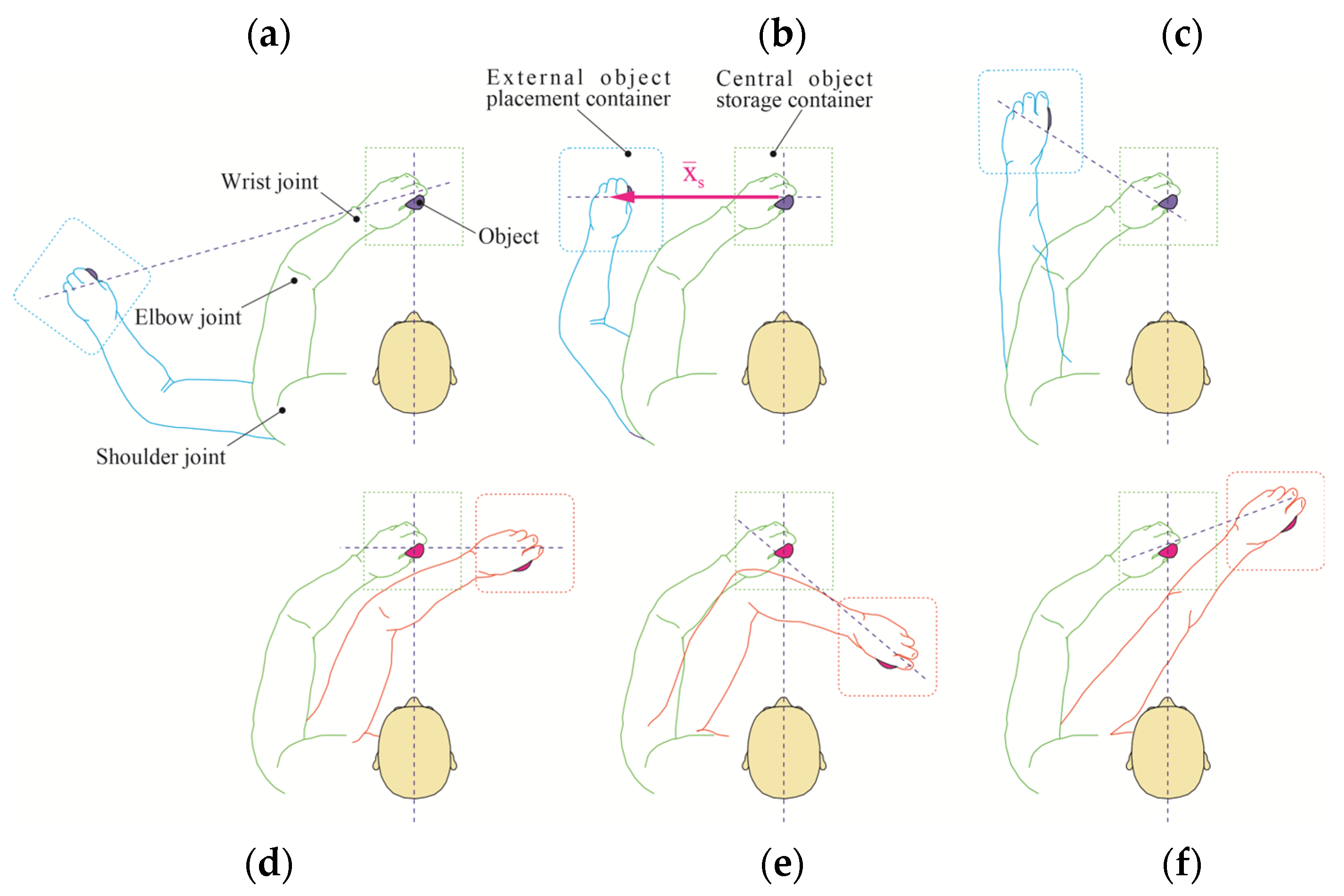
4.1. Execution of the BBT Task on the Rehabilitation Device
- Ipsilateral object placement (same side as the active limb; e.g., Figure 16a,c);
- Contralateral object placement (opposite side of the active limb; e.g., Figure 16b,f);
- Cross-body manipulations (right limb operating in the left-side field or vice versa);
- Combinations of manipulation zones and containers.
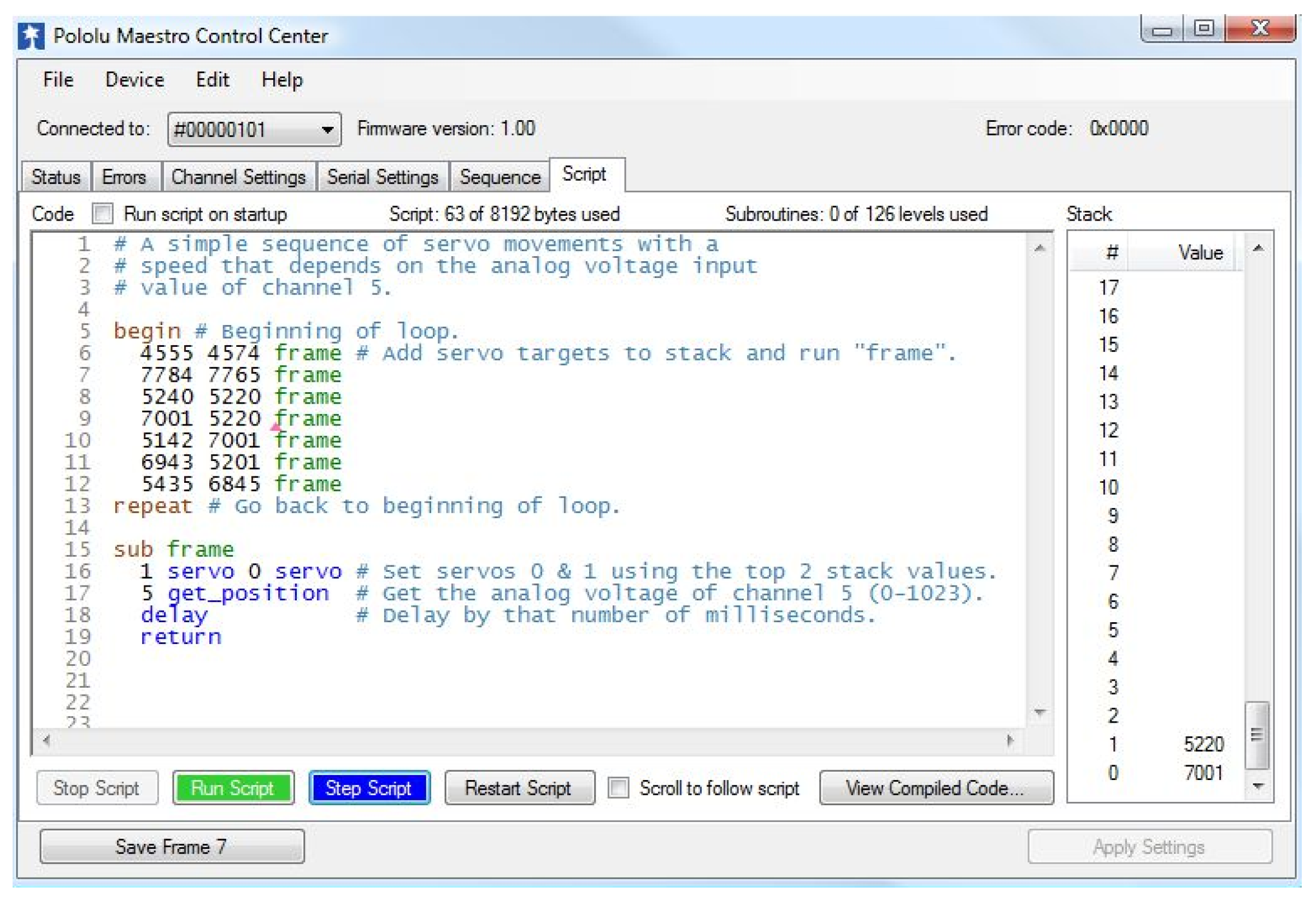
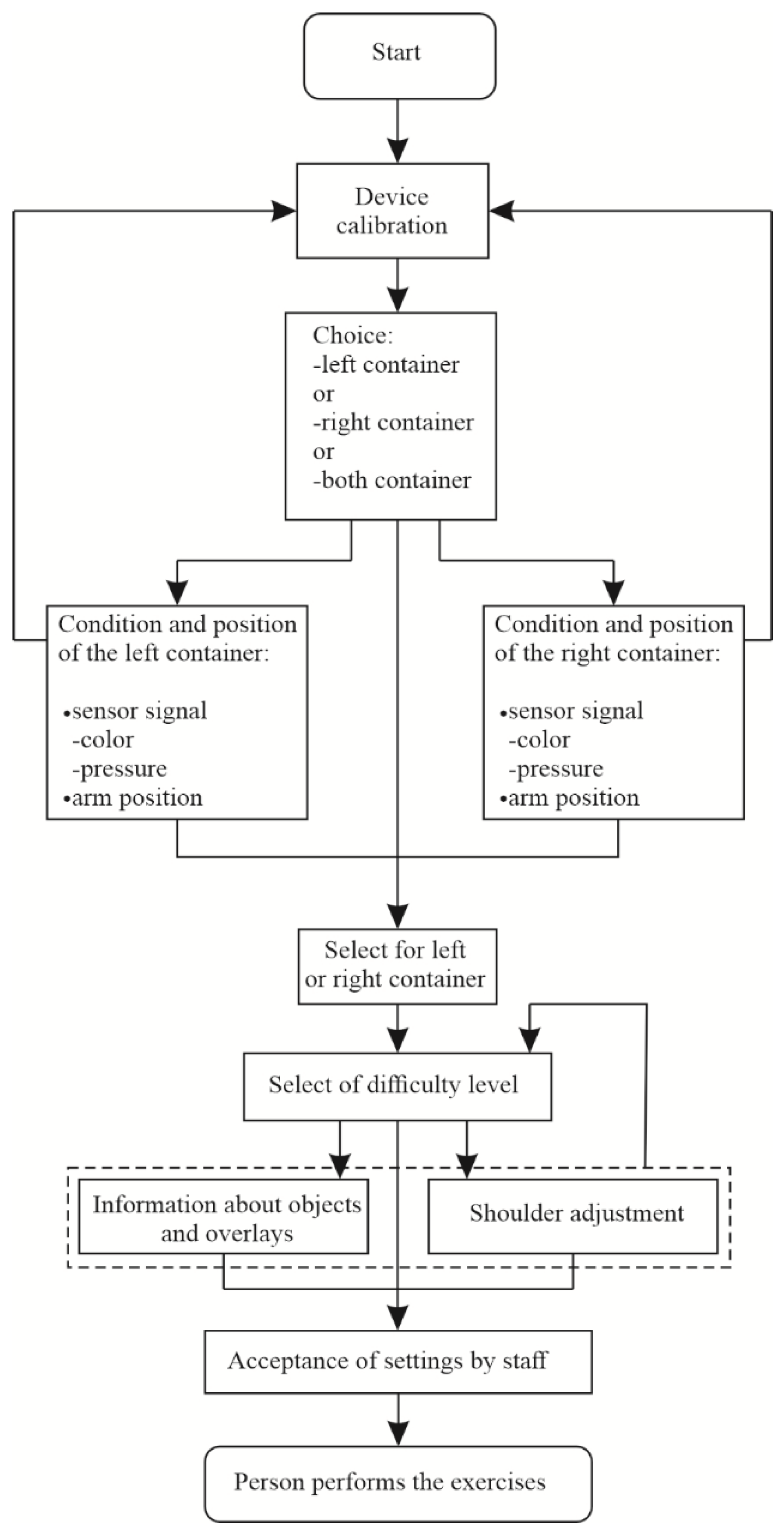
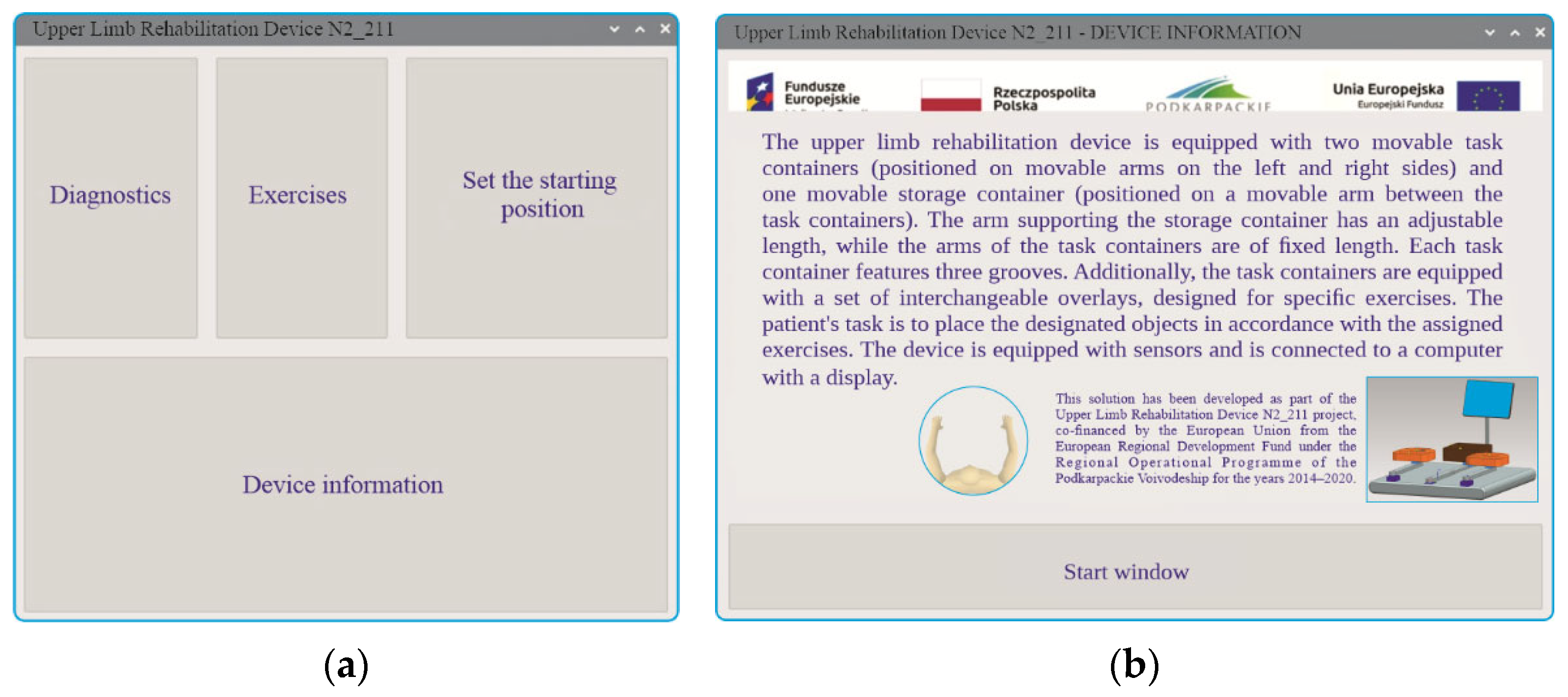
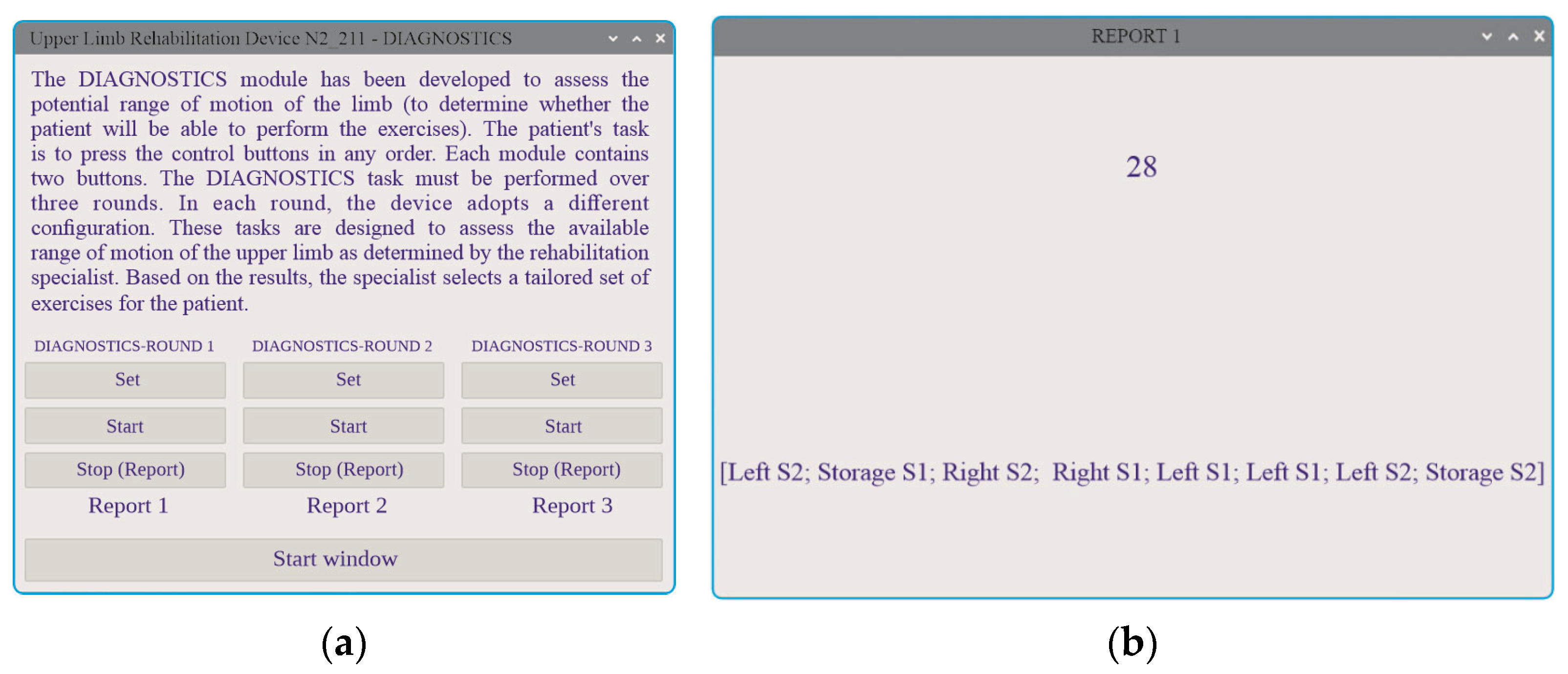
4.2. System Setup and Initialisation
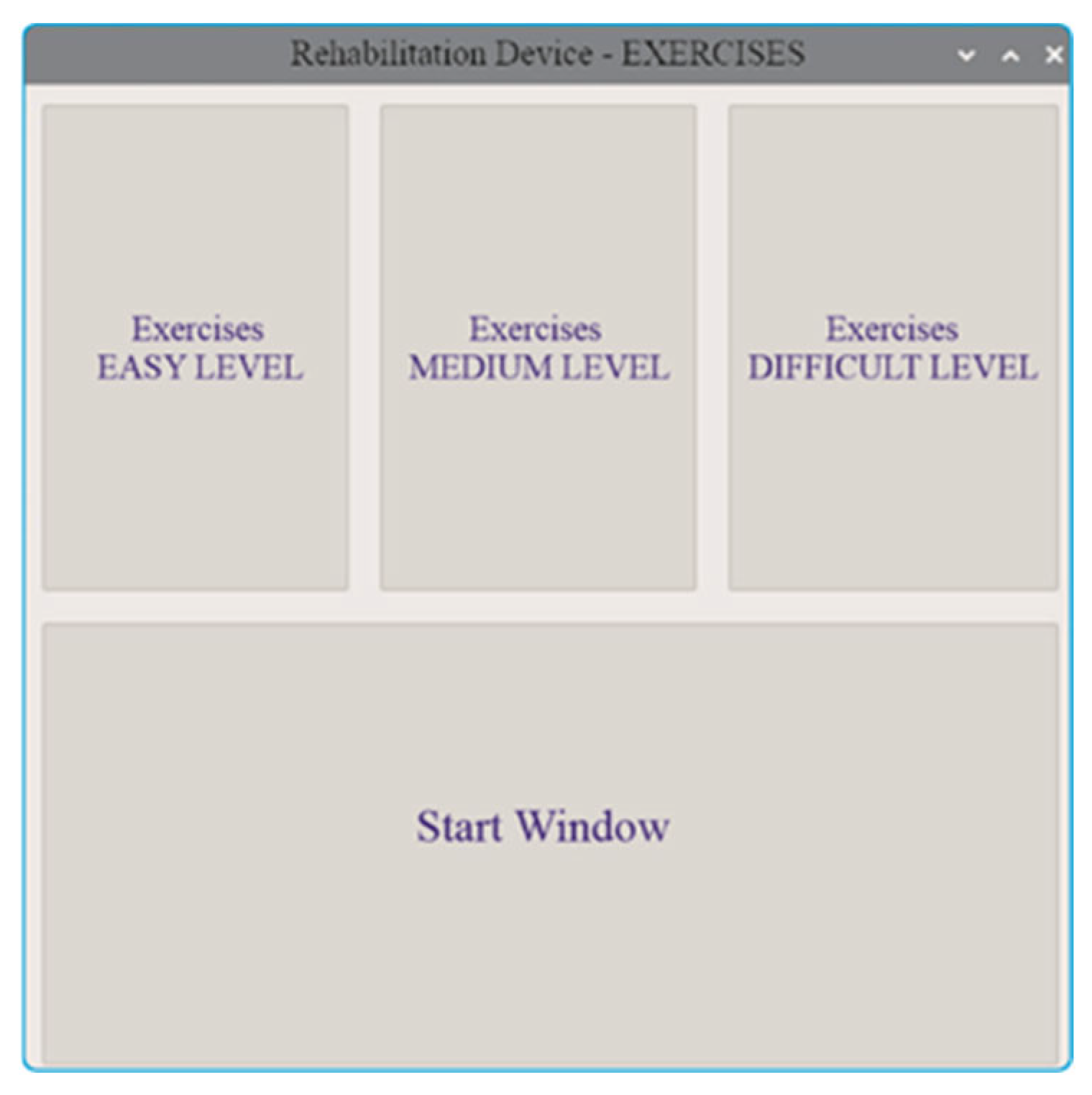
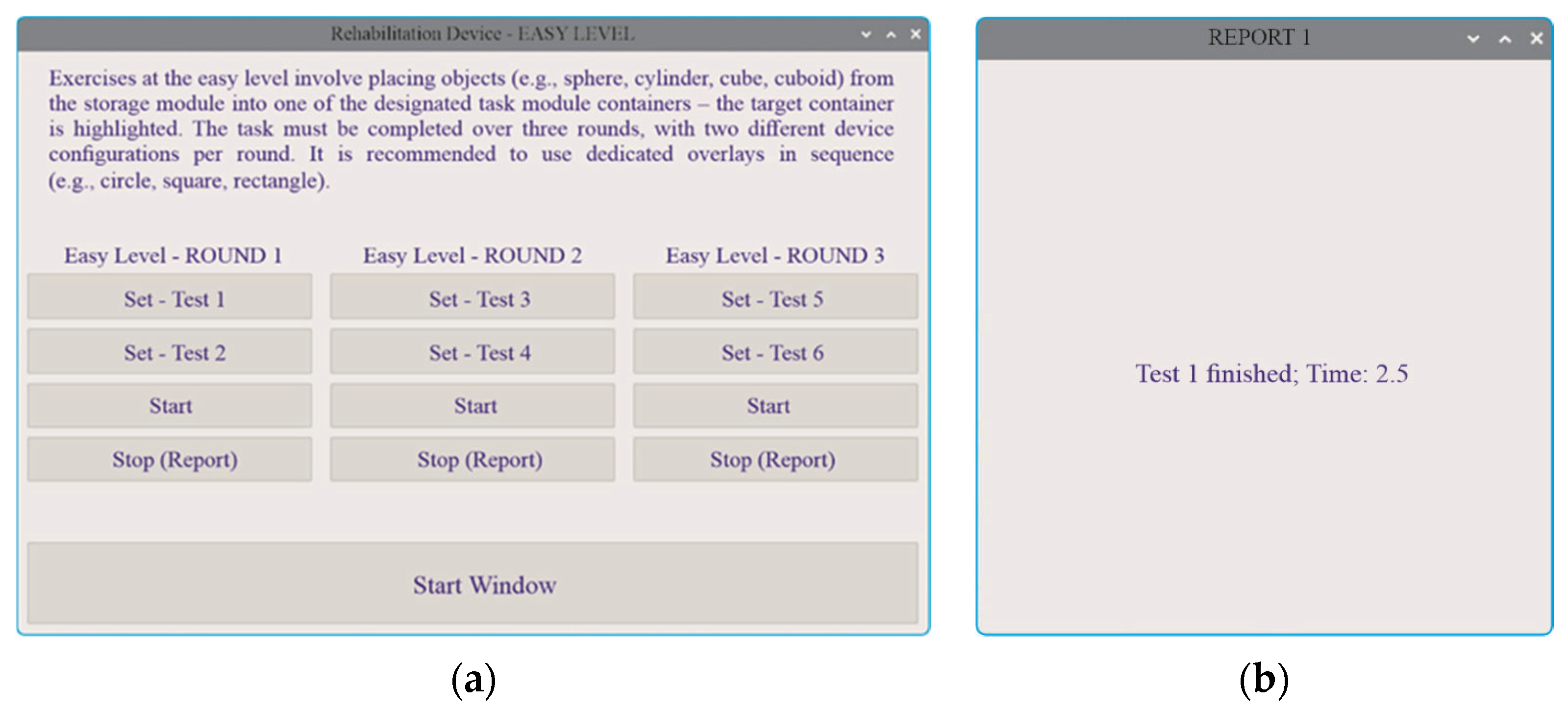
- Easy Level (Figure 22a)—In this introductory mode, the user selects from different arm configurations and completes object transfers from the central storage to the task modules. The evaluation criteria focus solely on the correct placement of objects in designated compartments. Upon completion of the task, a report and time record for the round are displayed (Figure 22b).
- Medium Level (Figure 23)—This level introduces an additional cognitive requirement by distinguishing objects based on colour, requiring the user to not only place the object correctly but also select it according to its visual features.
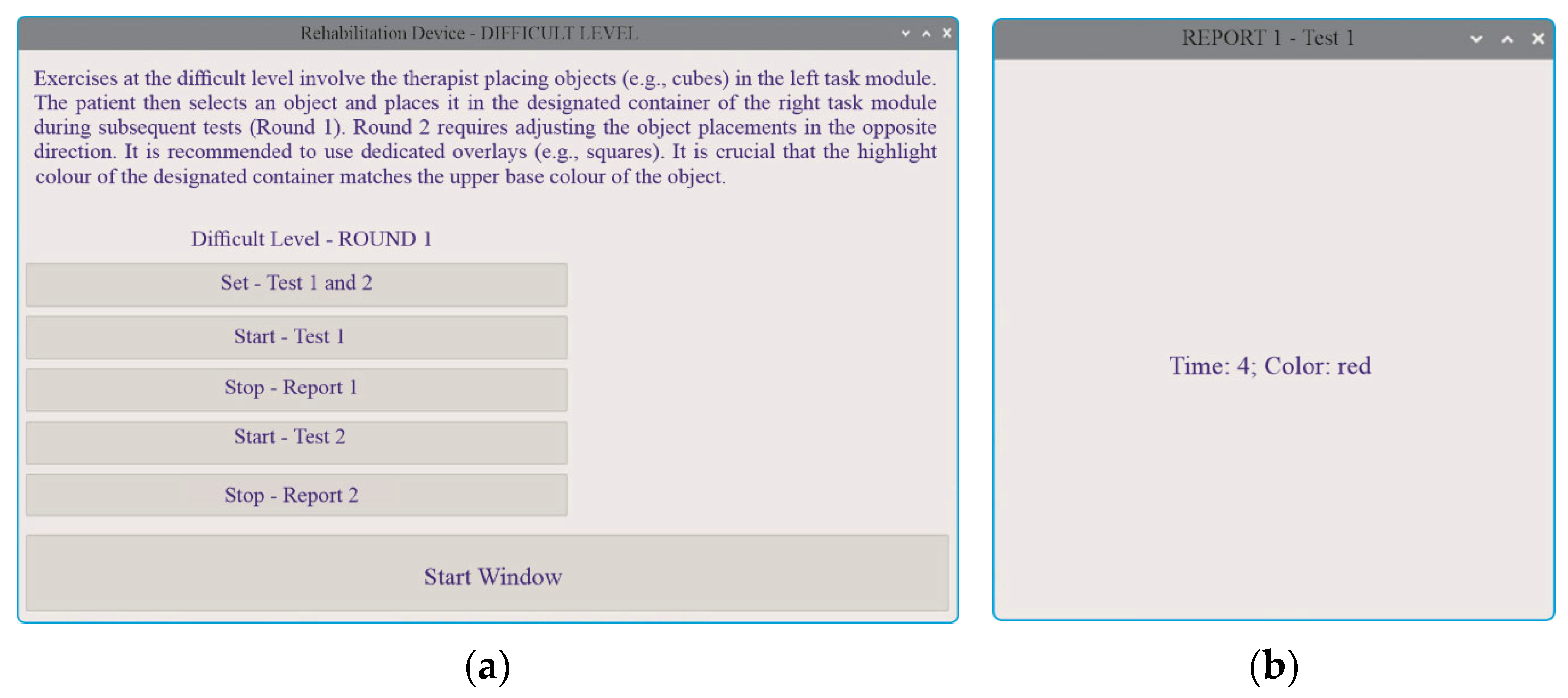
- Hard Level (Figure 24)—The most advanced mode includes object transfers between the left and right task modules, combined with the requirement to identify dual-coloured side surfaces. This setting challenges both spatial coordination and visual discrimination, offering a comprehensive training scenario.
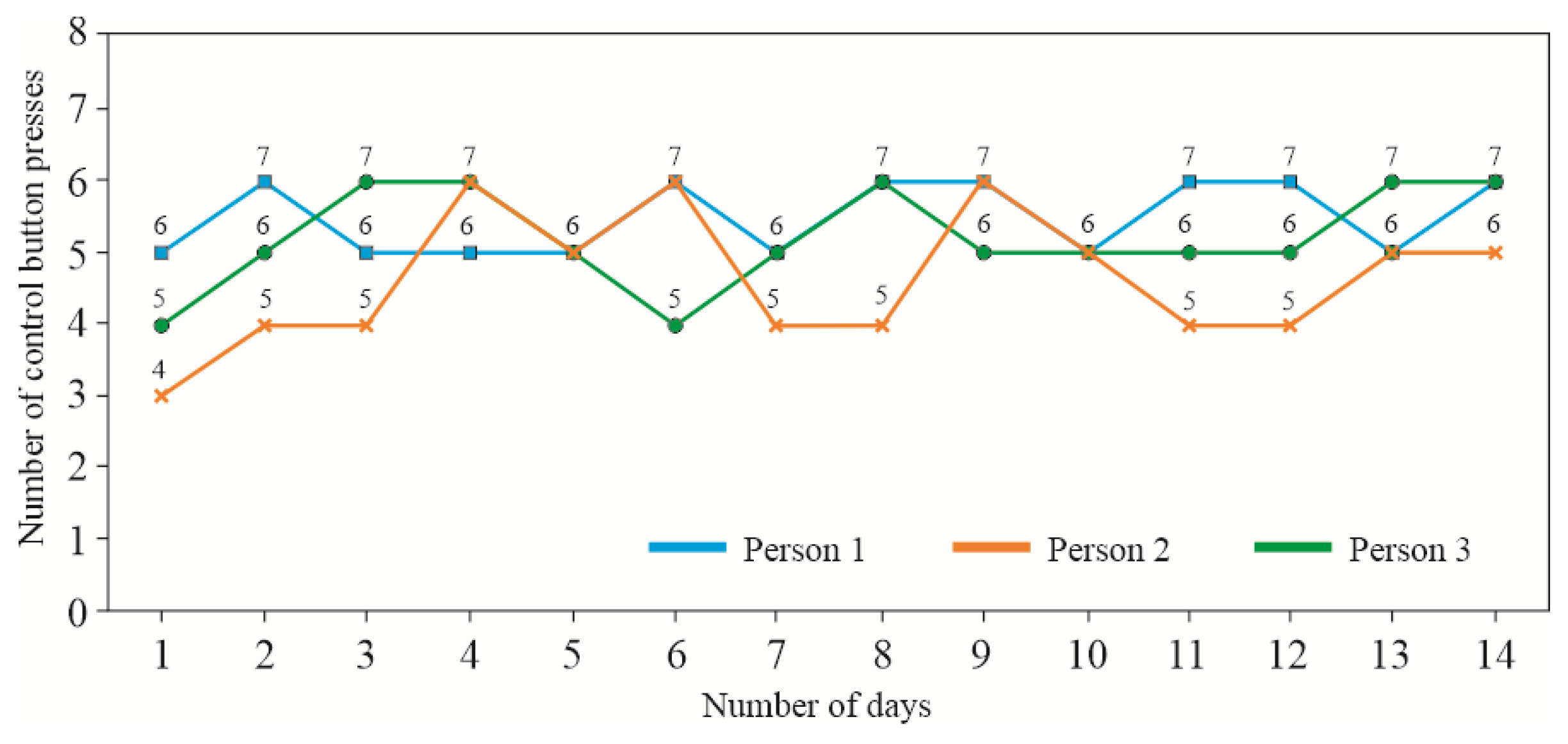
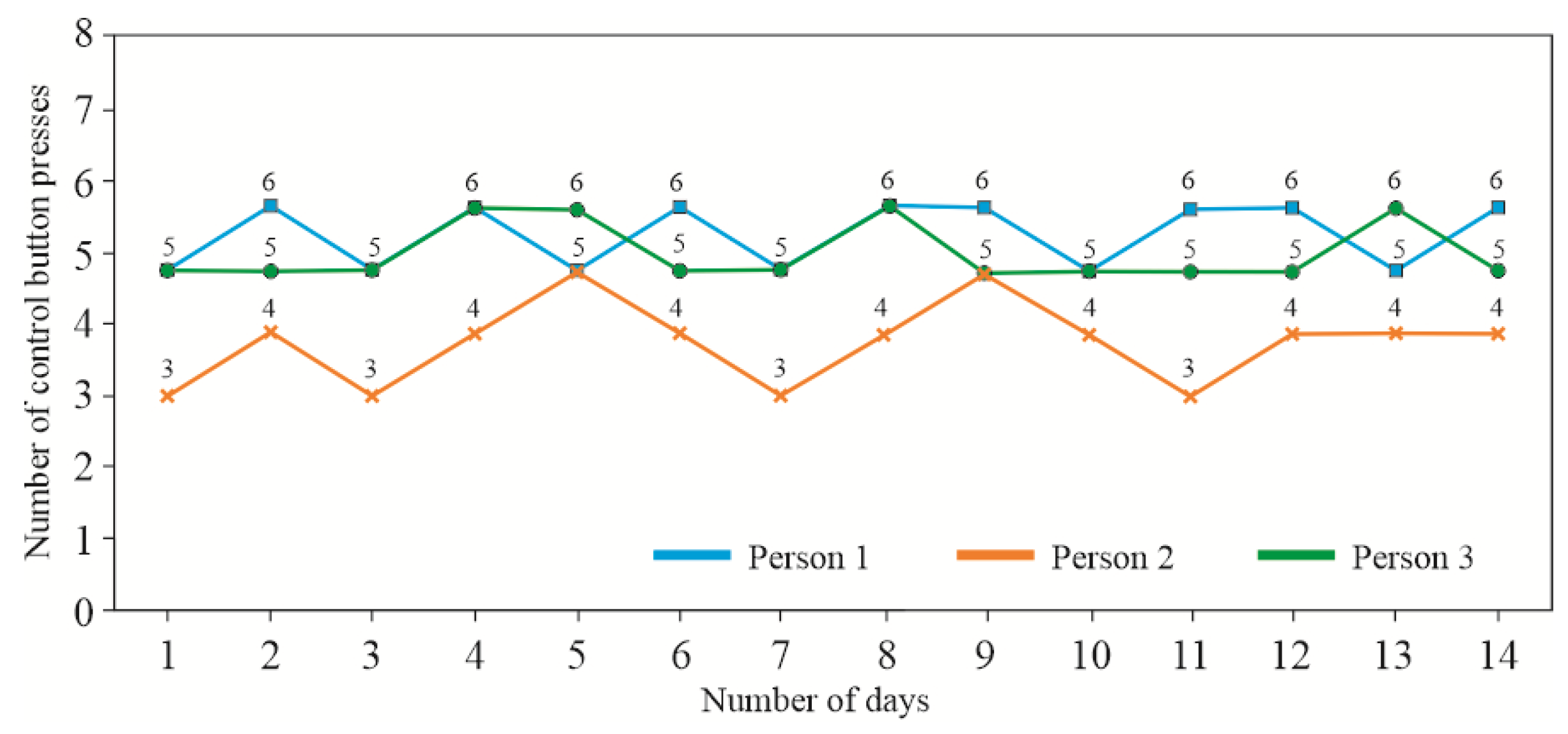
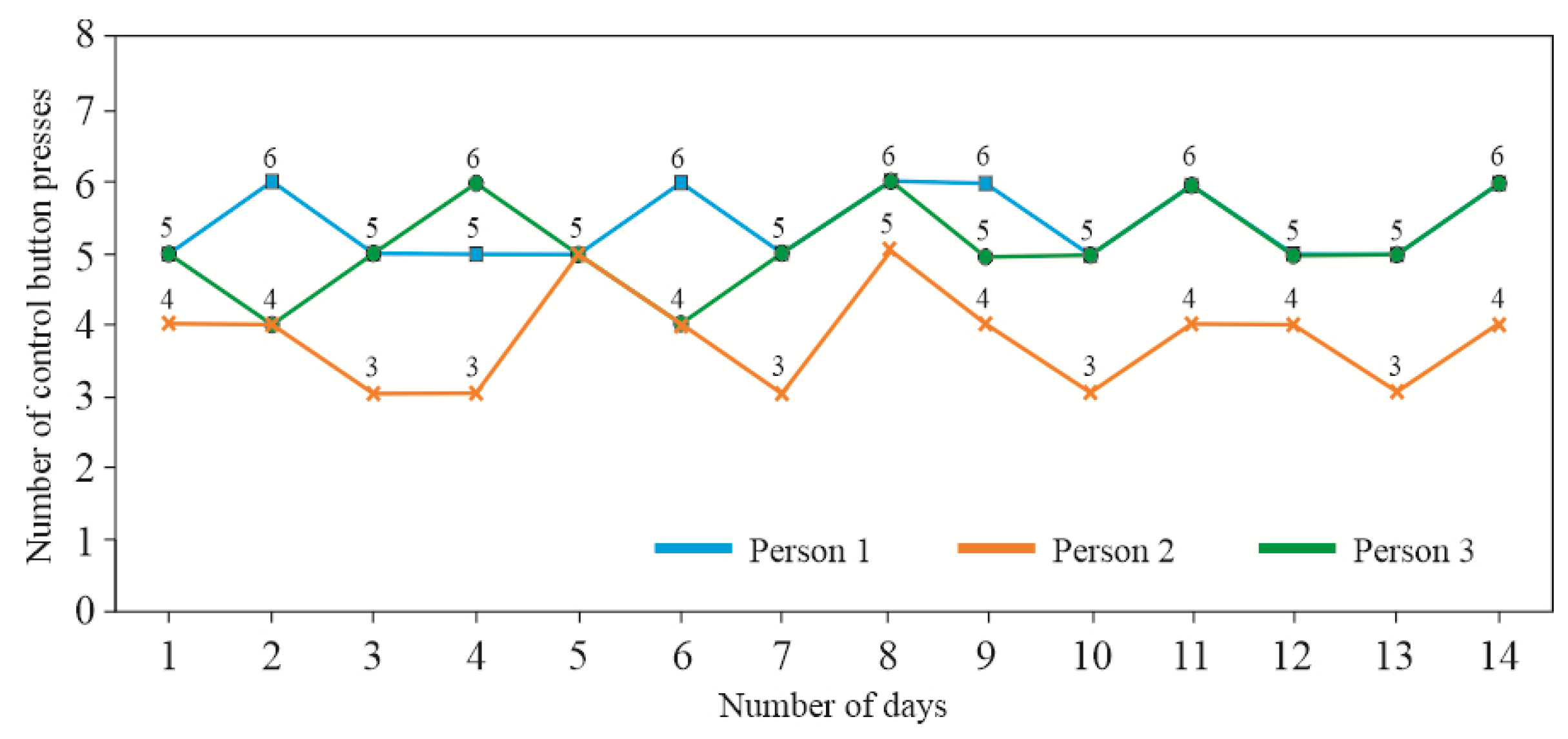
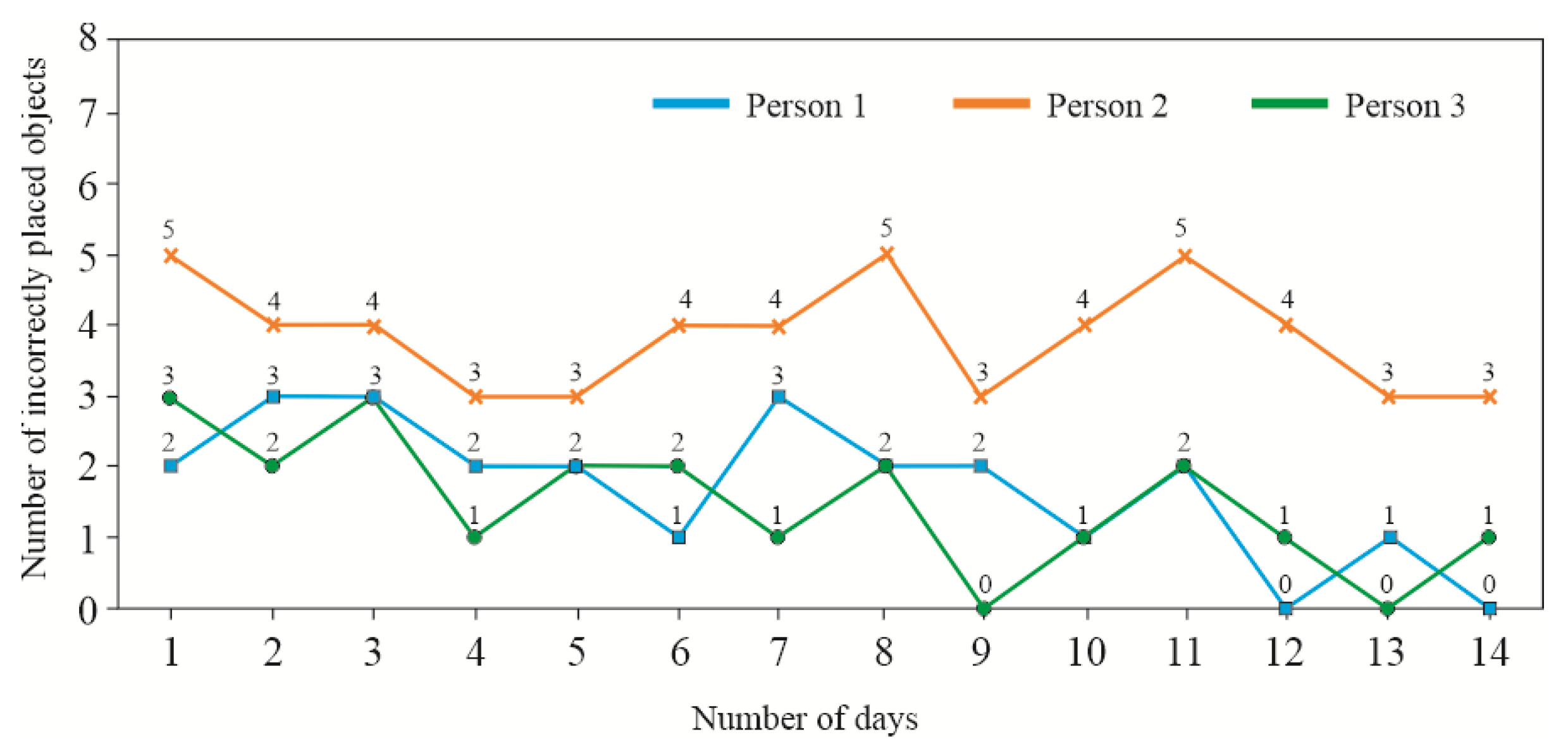
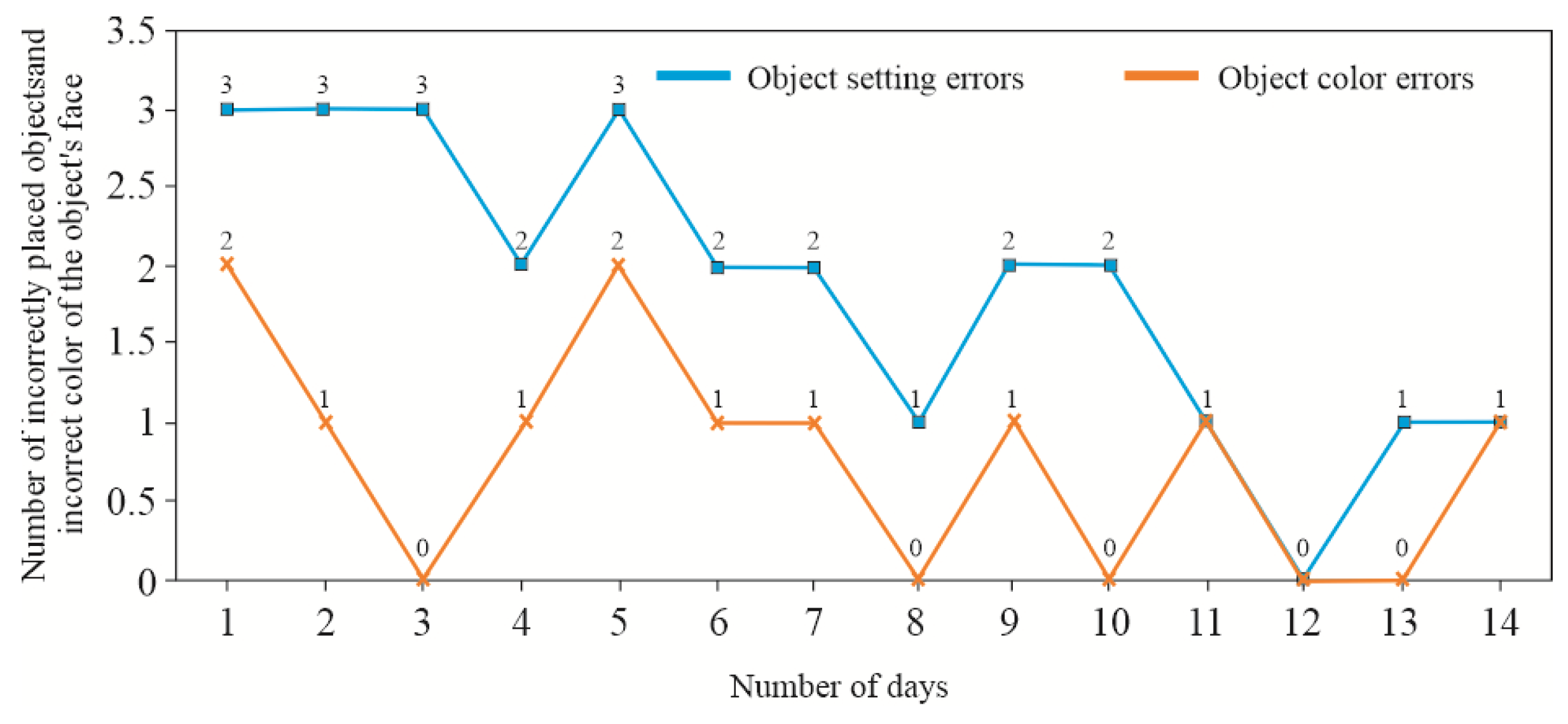
4.3. Results from Functional Testing of the Device
- Appraisement—Round 1: All three arms of the device (storage module, right task module, and left task module) were aligned at a 0° angle.
- Appraisement—Round 2: The storage module remained straight (0°), while the task modules were tilted outward at a 30° angle.
- Appraisement—Round 3: The storage module remained straight (0°), while the task modules were tilted outward at a 60° angle.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katan, M.; Luft, A. Global Burden of Stroke. Semin. Neurol. 2018, 38, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.world-stroke.org/ (accessed on 23 April 2025).
- Kwolek, A. Medical Rehabilitation, 2nd ed.; Elsevier Urban & Partner: Wrocław, Poland, 2003; ISBN 9788376093130. (In Polish) [Google Scholar]
- Grabowska-Fudala, B.; Jaracz, K.; Górna, K. Stroke incidence, case fatality and mortality—Current trends and future prognosis. Prz. Epidemiol. 2010, 64, 439–442. [Google Scholar]
- Bártlová, S.; Šedová, L.; Havierniková, L.; Hudáčková, A.; Dolák, F.; Sadílek, P. Quality of life of post-stroke patients. Slov. J. Public Health 2022, 61, 101–108. [Google Scholar] [CrossRef]
- Siger, A. (Ed.) The Situation of People After Stroke in Poland—A Report of the Stroke Foundation; The Stroke Foundation: Łódź, Poland, 2024; Available online: https://fum.info.pl/raport_osoby_po_udarze_e.pdf (accessed on 23 April 2025).
- Stroke Association. What We Think About: Rehabilitation. Rebuilding Lives After Stroke; Stroke Association: London, UK, 2023; Available online: https://www.stroke.org.uk/sites/default/files/new_pdfs_2019/our_policy_position/rehabilitation_policy_position.pdf (accessed on 23 April 2025).
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and regional bur den of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014, 383, 245–255. [Google Scholar] [CrossRef]
- Seshadri, S.; Wolf, A. Lifetime risk of stroke and dementia: Current concepts, and estimates from the framingham study. Lancet Neurol. 2017, 6, 1106–1114. [Google Scholar] [CrossRef]
- Mohan, K.M.; Wolfe, C.D.; Rudd, A.G.; Heuschmann, P.U.; Kolominsky-Rabas, P.L.; Grieve, A.P. Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke 2011, 42, 1489–1494. [Google Scholar] [CrossRef]
- National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health; National Center for Health Statistics: Hyattsville, MD, USA, 2012. Available online: https://www.cdc.gov/nchs/data/hus/hus11.pdf (accessed on 10 December 2024).
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Reeves, M.J.; Bushnell, C.D.; Howard, G.; Gargano, J.W.; Duncan, P.W.; Lynch, G.; Khatiwoda, A.; Lisabeth, L. Sex differences in stroke: Epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008, 7, 915–926. [Google Scholar] [CrossRef]
- Peterson, B.L.; Won, S.; Geddes, R.I.; Sayeed, I.; Stein, D.G. Sex-related differences in effects of progesterone following neonatal hypoxic brain injury. Behav. Brain Res. 2015, 286, 152–165. [Google Scholar] [CrossRef]
- Shahid, J.; Kashif, A.; Kashif-Shahid, M. A Comprehensive Review of Physical Therapy Interventions for Stroke Rehabilitation: Impairment-Based Approaches and Functional Goals. Brain Sci. 2023, 13, 717. [Google Scholar] [CrossRef]
- Pu, L.; Wang, L.; Zhang, R.; Zhao, T.; Jiang, Y.; Han, L. Projected Global Trends in Ischemic Stroke Incidence, Deaths and Disability-Adjusted Life Years From 2020 to 2030. Stroke 2023, 54, 1330–1339. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Lin, Y.; Shi, H.; Cheng, M.; Zhang, B.; Liu, X.; Shi, C.; Wang, Y.; Xia, C.; Xie, W. Projections of the Stroke Burden at the Global, Regional, and National Levels up to 2050 Based on the Global Burden of Disease Study 2021. J. Am. Heart Assoc. 2024, 13, e036142. [Google Scholar] [CrossRef] [PubMed]
- WHO. Stroke, Cerebrovascular Accident. 2025. Available online: https://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html (accessed on 20 April 2025).
- American Heart Association. Stroke Symptoms. 2025. Available online: https://www.stroke.org/en/about-stroke/stroke-symptoms (accessed on 17 April 2025).
- Andersson, J.; Rejnö, Å.; Jakobsson, S.; Hansson, P.-O.; Nielsen, S.J.; Björck, L. Symptoms at stroke onset as described by patients: A qualitative study. BMC Neurol. 2024, 24, 150. [Google Scholar] [CrossRef] [PubMed]
- Tater, P.; Pandey, S. Post-stroke Movement Disorders: Clinical Spectrum, Pathogenesis, and Management. Neurol. India 2021, 69, 272–283. [Google Scholar] [CrossRef]
- Lewek, M.D.; Bradley, C.E.; Wutzke, C.J.; Zinder, S.M. The relationship between spatiotemporal gait asymmetry and balance in individuals with chronic stroke. J. Appl. Biomech. 2014, 30, 31–36. [Google Scholar] [CrossRef]
- Lewek, M.D.; Randall, E.P. Reliability of spatiotemporal asymmetry during overground walking for individuals following chronic stroke. J. Neurol. Phys. Ther. 2011, 35, 116–121. [Google Scholar] [CrossRef]
- Patterson, K.K.; Gage, W.H.; Brooks, D.; Black, S.E.; McIlroy, W.E. Evaluation of gait symmetry after stroke: A comparison of current methods and recommendations for standardization. Gait Posture 2010, 31, 241–246. [Google Scholar] [CrossRef]
- Jamal, K.; Leplaideur, S.; Rousseau, C.; Chochina, L.; Moulinet-Raillon, A.; Bonan, I. Disturbances of spatial reference frame and postural asymmetry after a chronic stroke. Exp. Brain Res. 2018, 236, 2377–2385. [Google Scholar] [CrossRef]
- Hatem, S.M.; Saussez, G.; Della-Faille, M.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef]
- Kwakkel, G.; Stinear, C.; Essers, B.; Munoz-Novoa, M.; Branscheidt, M.; Cabanas-Valdés, R.; Lakičević, S.; Lampropoulou, S.; Luft, A.R.; Marque, R.; et al. Motor rehabilitation after stroke: European Stroke Organisation (ESO) consensus-based definition and guiding framework. Eur. Stroke J. 2023, 8, 880–894. [Google Scholar] [CrossRef]
- Lee, K.E.; Choi, M.; Jeoung, B. Effectiveness of Rehabilitation Exercise in Improving Physical Function of Stroke Patients: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 12739. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Zhang, W.; Kang, L.; Ma, Y.; Fu, L.; Jia, L.; Yu, H.; Chen, X.; Hou, L.; Wang, L.; et al. Clinical Evidence of Exercise Benefits for Stroke. Adv. Exp. Med. Biol. 2017, 1000, 131–151. [Google Scholar] [CrossRef]
- Chen, K.; Zhu, S.; Tang, Y.; Lan, F.; Liu, Z. Advances in balance training to prevent falls in stroke patients: A scoping review. Front. Neurol. 2024, 15, 1167954. [Google Scholar] [CrossRef]
- Lee, C.Y.; Howe, T.H. Effectiveness of Activity-Based Task-Oriented Training on Upper Extremity Recovery for Adults with Stroke: A Systematic Review. Am. J. Occup. Ther. 2024, 78, 7802180070. [Google Scholar] [CrossRef]
- Maciejasz, P.; Eschweiler, J.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 3. [Google Scholar] [CrossRef]
- Laut, J.; Porfiri, M.; Raghavan, P. The Present and Future of Robotic Technology in Rehabilitation. Curr. Phys. Med. Rehabil. Rep. 2016, 4, 312–319. [Google Scholar] [CrossRef]
- Colombo, R.; Pisano, F.; Micera, S.; Mazzone, A.; Delconte, C.; Carrozza, M.C.; Dario, P.; Minuco, G. Robotic Techniques for Upper Limb Evaluation and Rehabilitation of Stroke Patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2005, 13, 311–324. [Google Scholar] [CrossRef]
- Mazzoleni, S.; Dario, P.; Carrozza, M.; Guglielmelli, E. Application of Robotic and Mechatronic Systems to Neurorehabilitation. In Mechatronic Systems Applications, 1st ed.; Milella, A., Di Paola, D., Cicirelli, G., Eds.; IntechOpen: London, UK, 2010; pp. 99–116. [Google Scholar] [CrossRef][Green Version]
- Banyai, A.D.; Brisan, C. Robotics in Physical Rehabilitation: Systematic Review. Healthcare 2024, 12, 1720. [Google Scholar] [CrossRef]
- Martins, O.O.; Oosthuizen, C.C.; Desai, D.A. Exploring the import of mechatronics engineering in medicine: A review. Beni-Suef. Univ. J. Basic. Appl. Sci. 2025, 14, 26. [Google Scholar] [CrossRef]
- Dovat, L.; Lambercy, O.; Gassert, R.; Maeder, T.; Milner, T.; Leong, T.C.; Burdet, E. HandCARE: A cable-actuated rehabilitation system to train hand function after stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 16, 582–591. [Google Scholar] [CrossRef]
- Ramos-Murguialday, A.; Broetz, D.; Rea, M.; Laer, L.; Yilmaz, O.; Brasil, F.L.; Liberati, G.; Curado, M.R.; Garcia-Cossio, E.; Vyziotis, A.; et al. Brain-machine interface in chronic stroke rehabilitation: A controlled study. Ann. Neurol. 2013, 74, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Fazekas, G.; Horwath, M.; Toth, A. A novel robot training system designed to supplement upper limb physiotherapy on patient with spastic hemiparesis. Int. J. Rehabil. Res. 2006, 29, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.P. The exoskeletons are here. J. Neuroeng. Rehabil. 2009, 6, 17. [Google Scholar] [CrossRef] [PubMed]
- Pignolo, L.; Dolce, G.; Basta, G.; Lucca, L.F.; Serra, S.; Sannitam, W.G. Upper limb rehabilitation after stroke. ARAMIS a ‘robo-mechatronic’ innovative approach and prototype. In Proceedings of the 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 1410–1414. [Google Scholar] [CrossRef]
- Frisoli, A.; Borelli, L.; Montagner, A.; Marcheschi, S.; Procopio, C.; Salsedo, F.; Bergamasco, M.; Carboncini, M.C. Arm rehabilitation with a robotic exoskeleton in virtual reality. In Proceedings of the IEEE 10th International Conference on Rehabilitation and Robotics (ICORR), Noordwijk, The Netherlands, 13–15 June 2007; pp. 631–642. [Google Scholar] [CrossRef]
- Frolov, A.A.; Gusek, D.; Sil’chenko, A.V.; Tintera, Y.; Rydlo, Y. The Changes in the hemodynamic activity of the brain in motor imagery as a result of training subjects to control a brain-computer interface. Fiziol. Cheloveka 2016, 42, 5–18. [Google Scholar]
- Marchal-Crespo, L.; Reinkensmeyer, D.J. Review of control strategies for robotic movement training after neurologic injury. J. Neuroeng. Rehabil. 2009, 6, 20. [Google Scholar] [CrossRef]
- Desplenter, T.; Zhou, Y.; Edmonds, B.; Lidka, M.; Goldman, A.; Trejos, A.L. Rehabilitative and assistive wearable mechatronic upper-limb devices: A review. J. Rehabil. Assist. Technol. Eng. 2020, 7, 2055668320917870. [Google Scholar] [CrossRef]
- Just, F.; Baur, K.; Riener, R.; Klamroth-Marganska, V.; Rauter, G. Online adaptive compensation of the ARMin Rehabilitation Robot. In Proceedings of the 6th IEEE International Conference on IEEE 2016, Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 747–752. [Google Scholar] [CrossRef]
- Ren, H.; Liu, T.; Wang, J. Design and Analysis of an Upper Limb Rehabilitation Robot Based on Multimodal Control. Sensor 2023, 23, 8801. [Google Scholar] [CrossRef]
- Ventura, S.; Tessari, A.; Castaldini, S.; Magni, E.; Turolla, A.; Baños, R.; Lullini, G. Effectiveness of a Virtual Reality rehabilitation in stroke patients with sensory-motor and proprioception upper limb deficit: A study protocol. PLoS ONE 2024, 19, e0307408. [Google Scholar] [CrossRef]
- Ren, Y.; Park, H.S.; Zhang, L.Q. Developing a whole-arm exoskeleton robot with hand opening and closing mechanism for upper limb stroke rehabilitation. In Proceedings of the IEEE International Conference on Rehabilitation Robotics (ICORR), Kyoto, Japan, 23–26 June 2009; pp. 761–765. [Google Scholar] [CrossRef]
- Dipietro, L.; Ferraro, M.; Palazzolo, J.J.; Krebs, H.I.; Volpe, B.T.; Hogan, N. Customized interactive robotic treatment for stroke: EMG triggered therapy. IEEE Trans. Neur. Syst. Rehab. Eng. 2005, 13, 325–334. [Google Scholar] [CrossRef]
- Shih, J.; Krusienski, D.J.; Wolpaw, J.W. Brain-computer interfaces in medicine. Mayo Clin. Proc. 2012, 87, 268–279. [Google Scholar] [CrossRef]
- Hesse, S.; Kuhlmann, H.; Wilk, J.; Tomelleri, C.; Kirker, S.G.B. A new electromechanical trainer for sensorimotor rehabilitation of paralysed fingers: A case series in chronic and acute stroke patients. J. Neuroeng. Rehabil. 2008, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Frolov, A.A.; Mokienko, O.; Lyukmanov, R.; Biryukova, E.; Kotov, S.; Turbina, L.; Nadareyshvily, G.; Bushkova, Y. Post-stroke Rehabilitation Training with a Motor-Imagery-Based Brain-Computer Interface (BCI)-Controlled Hand Exoskeleton: A Randomized Controlled Multicenter Trial. Front. Neurosci. 2017, 11, 400. [Google Scholar] [CrossRef] [PubMed]
- Panny, M.; Mayr, A.; Nagiller, M.; Kim, Y. A domestic robotic rehabilitation device for assessment of wrist function for outpatients. J. Rehabil. Assist. Technol. Eng. 2020, 7, 2055668320961233. [Google Scholar] [CrossRef]
- Forbrigger, S.; DePaul, V.G.; Davies, T.C.; Morin, E.; Hashtrudi Zaad, K. Home based upper limb stroke rehabilitation mechatronics: Challenges and opportunities. Biomed. Eng. 2023, 22, 67. [Google Scholar] [CrossRef]
- Ruggiu, M.; Rea, P. Development of a Mechatronic System for the Mirror Therapy. Actuators 2022, 11, 14. [Google Scholar] [CrossRef]
- Akshay, M.; Latt, W.T.; Tan, H.G.; Tan, U.X.; Shee, C.Y.; Ang, W.T. Design and implementation of a mechatronic device for wrist and elbow rehabilitation. In Proceedings of the 1st International Convention on Rehabilitation Engineering & Assistive Technology: In Conjunction with 1st Tan Tock Seng Hospital Neurorehabilitation Meeting i-CREATe ‘07, Singapore, 23–26 April 2007; Association for Computing Machinery: New York, NY, USA, 2007; pp. 212–215. [Google Scholar] [CrossRef]
- Kyeong, S.; Na, Y.; Kim, J. A Mechatronic Mirror-Image Motion Device for Symmetric Upper-Limb Rehabilitation. Int. J. Precis. Eng. Manuf. 2020, 21, 947–956. [Google Scholar] [CrossRef]
- Averta, G.; Abbinante, M.; Orsini, P.; Felici, F.; Lippi, P.; Bicchi, A.; Catalano, M.G.; Bianchi, M. A novel mechatronic system for evaluating elbow muscular spasticity relying on Tonic Stretch Reflex Threshold estimation. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Montreal, QC, Canada, 20–24 July 2020; pp. 3839–3843. [Google Scholar] [CrossRef]
- Cavallaro, E.; Keller, T. Portable Device for Upper Limb Rehabilitation. U.S. Patent 8795207B2, 5 August 2014. [Google Scholar]
- Bimeo: An Award-Winning, Sensor-Based, Arm Rehabilitation System. Available online: https://kinestica.com/bimeo (accessed on 14 December 2024).
- Pablo: Functional Rehabilitation. Available online: https://tyromotion.com/en/products/pablo/ (accessed on 14 December 2024).
- Myro: Interactive and Task-Specific Therapy. Available online: https://tyromotion.com/en/products/myro (accessed on 14 December 2024).
- Annett, M.; Anderson, F.; Goertzen, D.; Halton, J.; Bischof, Q.R.W.F.; Boulanger, P. Using a Multi-touch Tabletop for Upper Extremity Motor Rehabilitation. In Proceedings of the 21st Annual Conference of the Australian Computer-Human Interaction Special Interest Group: Design: Open 24/7 (OZCHI ‘09), Melbourne Australia, 23–27 November 2009; Association for Computing Machinery: New York, NY, USA, 2009; pp. 261–264. [Google Scholar] [CrossRef]
- Kim, G.W.; Won, Y.H.; Seo, J.H.; Ko, M.H. Effects of newly developed compact robot-aided upper extremity training system (Neuro-X®) in patients with stroke: A pilot study. J. Rehabil. Med. 2018, 50, 607–612. [Google Scholar] [CrossRef]
- Kim, S.-Y.; Kim, Y.-M.; Koo, S.-W.; Park, H.-B.; Yoon, Y.-S. Effects of Therapist Intervention during Upper-Extremity Robotic Rehabilitation in Patients with Stroke. Healthcare 2023, 11, 1369. [Google Scholar] [CrossRef]
- Tunc, H.; Bakar, M.K.; Ozen, S.; Leblebici, G.; Tarakci, D. The effect of virtual reality applications on treatment outcomes in lower extremity rehabilitation: A systematic review. Adv. Rehabil. 2024, 38, 43–57. [Google Scholar] [CrossRef]
- Zahabi, M.; Abdul-Razak, A.M. Adaptive virtual reality-based training: A systematic literature review and framework. Virtual Real. 2020, 24, 725–752. [Google Scholar] [CrossRef]
- Vosinakis, S.; Koutsabasis, P. Evaluation of visual feedback techniques for virtual grasping with bare hands using Leap Motion and Oculus Rift. Virtual Real. 2018, 22, 47–62. [Google Scholar] [CrossRef]
- Dong, Y.; Liu, X.; Tang, M.; Huo, H.; Chen, D.; Wu, Z.; An, R.; Fan, Y. A haptic feedback virtual reality system to improve the Box and Block Test (BBT) for upper extremity motor function assessment. Virtual Real. 2023, 27, 1199–1219. [Google Scholar] [CrossRef]
- Alvarez-Rodríguez, M.; López-Dolado, E.; Salas-Monedero, M.; Lozano-Berrio, V.; Ceruelo-Abajo, S.; Gil-Agudo, A.; de los Reyes-Guzmán, A. Concurrent Validity of a Virtual Version of Box and Block Test for Patients with Neurological Disorders. World J. Neurosci. 2020, 10, 79–89. [Google Scholar] [CrossRef]
- Everard, G.; Otmane-Tolba, Y.; Rosselli, Z.; Pellissier, T.; Ajana, K.; Dehem, S.; Auvinet, E.; Edwards, M.G.; Lebleu, J.; Lejeune, T. Concurrent validity of an immersive virtual reality version of the Box and Block Test to assess manual dexterity among patients with stroke. J. Neuroeng. Rehabil. 2022, 19, 7. [Google Scholar] [CrossRef]
- Gieser, S.N.; Gentry, C.; LePage, J.; Makedon, F. Comparing objective and subjective metrics between physical and virtual tasks. In Virtual, Augmented and Mixed Reality, Proceedings of the VAMR 2016, Toronto, Canada, 17–22 July 2016; Lackey, S., Shumaker, R., Eds.; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2016; pp. 3–13. [Google Scholar] [CrossRef]
- Oña, E.D.; Jardón, A.; Balaguer, C. The Automated Box and Blocks Test an Autonomous Assessment Method of Gross Manual Dexterity in Stroke Rehabilitation. In Towards Autonomous Robotic Systems, Proceedings of the TAROS 2017, Guildford, UK, 19–21 July 2017; Gao, Y., Fallah, S., Jin, Y., Lekakou, C., Eds.; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2017; Volume 10454, pp. 3–13. [Google Scholar] [CrossRef]
- Oña, E.D.; Jardón, A.; Cuesta-Gómez, A.; Sánchez-Herrera-Baeza, P.; Canode-la-Cuerda, R.; Balaguer, C. Validity of a fully-immersive VR-based version of the box and blocks test for upper limb function assessment in Parkinson’s disease. Sensors 2020, 20, 2773. [Google Scholar] [CrossRef]
- Furmanek, M.P.; Schettino, L.F.; Yarossi, M.; Kirkman, S.; Adamovich, S.V.; Tunik, E. Coordination of reach-to-grasp in physical and haptic-free virtual environments. J. Neuroeng. Rehabil. 2019, 16, 78. [Google Scholar] [CrossRef]
- Oña, E.D.; Balaguer, C.; Jardón, A. Automatic Cube Counting System for the Box and Blocks Test Using Proximity Sensors: Development and Validation. Electronics 2023, 12, 914. [Google Scholar] [CrossRef]
- Temehy, B.; Rosewilliam, S.; Alvey, G.; Soundy, A. Exploring Stroke Patients’ Needs after Discharge from Rehabilitation Centres: Meta-Ethnography. Behav. Sci. 2022, 12, 404. [Google Scholar] [CrossRef]
- Mitchell, J.; Shirota, C.; Clanchy, K. Factors that influence the adoption of rehabilitation technologies: A multi-disciplinary qualitative exploration. J. Neuroeng. Rehabil. 2023, 20, 80. [Google Scholar] [CrossRef]
- Sivan, M.; Gallagher, J.; Holt, R.; Weightman, A.; Levesley, M.; Bhakta, B. Investigating the international classification of functioning, disability, and health (ICF) framework to capture user needs in the concept stage of rehabilitation technology development. Assist. Technol. 2014, 26, 164–173. [Google Scholar] [CrossRef]
- Sivan, M.; Gallagher, J.; Holt, R.; Weightman, A.; O’Connor, R.; Levesley, M. Employing the international classification of functioning, disability and health framework to capture user feedback in the design and testing stage of development of home-based arm rehabilitation technology. Assist Technol. 2016, 28, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Neibling, B.A.; Jackson, S.M.; Hayward, K.S.; Barker, R.N. Perseverance with technology-facilitated home-based upper limb practice after stroke: A systematic mixed studies review. J. Neuroeng. Rehabil. 2021, 18, 43. [Google Scholar] [CrossRef] [PubMed]
- Tutak, S.; Mucha, J.; Lew, L.; Jurka, M. Upper Limb Rehabilitation. Device. Patent Office of the Republic of Poland PL244088, 30 November 2021. [Google Scholar]
- Openshaw, S.; Taylor, E. Ergonomics and Design A Reference Guide. DIANE Publishing Company: Collingdale, PA, USA, 2007; ISBN 1422317048. [Google Scholar]
- Frenzel, A.; Binder, H.; Walter, N.; Wirkner, K.; Loeffler, M.; Loeffler-Wirth, H. The Aging human body shape. NPJ Aging Mech. Dis. 2020, 6, 5. [Google Scholar] [CrossRef] [PubMed]
- Valentin, J. Basic Anatomical and Physiological Data for Use in Radiological Protection: Reference Values. Ann. ICRP. 2002, 32, 1–277. [Google Scholar] [CrossRef]
- Pheasant, S.; Haslegrave, C.M. Bodyspace: Anthropometry, Ergonomics and the Design of Work, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2006. [Google Scholar] [CrossRef]
- Anthropometric-Detailed-Data-Tables. Available online: https://multisite.eos.ncsu.edu/www-ergocenter-ncsu-edu/wp-content/uploads/sites/18/2016/06/Anthropometric-Detailed-Data-Tables.pdf (accessed on 14 December 2024).
- EN 547-1:1996+A1:2008; Safety of machinery—Human body measurements—Part 1: Principles for Determining the Dimensions Required for Openings for Whole Body Access into Machinery. Technical Committee CEN/TC 122. European Committee for Standardization: Brussels, Belgium, 2008.
- EN 547-2:1996+A1:2008; Safety of Machinery—Human Body Measurements—Part 2: Principles for Determining the Dimensions Required for Access Openings. Technical Committee CEN/TC 122. European Committee for Standardization: Brussels, Belgium, 2008.
- EN 547-3:1996+A1:2008; Safety of Machinery—Human Body Measurements—Part 3: Anthropometric Data. Technical Committee CEN/TC 122. European Committee for Standardization: Brussels, Belgium, 2008.
- Saenen, L.; Orban de Xivry, J.-J.; Verheyden, G. Development and Validation of a Novel Robot-Based Assessment of Upper Limb Sensory Processing in Chronic Stroke. Brain Sci. 2022, 12, 1005. [Google Scholar] [CrossRef]
- Ballester, B.R.; Maier, M.; San Segundo Mozo, R.M.; Castañeda, V.; Duff, A.; Verschure, P.F.M.J. Counteracting learned non-use in chronic stroke patients with reinforcement-induced movement therapy. J. Neuroeng. Rehabil. 2016, 13, 74. [Google Scholar] [CrossRef]
- Han, C.E.; Kim, S.; Chen, S.; Lai, Y.-H.; Lee, J.-Y.; Osu, R.; Winstein, C.J.; Schweighofer, N. Quantifying Arm Nonuse in Individuals Poststroke. Neurorehabil. Neural Repair 2013, 27, 439–447. [Google Scholar] [CrossRef]
- Gentilucci, M.; Benuzzi, F.; Bertolani, L.; Daprati, E.; Gangitano, M. Recognising a hand by grasp. Cogn. Brain Res. 2000, 9, 125–135. [Google Scholar] [CrossRef]
- Dandekar, K.; Raju, B.I.; Srinivasan, M.A. 3-D Finite-Element Models of Human and Monkey Fingertips to Investigate the Mechanics of Tactile Sense. ASME J. Biomech. Eng. 2003, 5, 682–691. [Google Scholar] [CrossRef]
- O’Meara, D.M.; Smith, R.M. Static friction properties between human palmar skin and five grabrail materials. Ergonomics 2001, 44, 973–988. [Google Scholar] [CrossRef]
- Cruz, J.; Garcia, M.; Garza, C.; DeLucia, P.R.; Yang, J. Object shape affects hand grip function for heavy objects in younger and older adults. Ergonomics 2021, 64, 722–732. [Google Scholar] [CrossRef] [PubMed]
- Slota, G.P.; Enders, L.R.; Seo, N.J. Improvement of hand function using different surfaces and identification of difficult movement post stroke in the Box and Block Test. Appl. Ergon. 2014, 45, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.; Yick, K.-L.; Wong, S.-T. Analysis of length of finger segments with different hand postures to enhance glove design. Appl. Ergon. 2021, 94, 103409. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; van der Helm, F.C.T.; Veeger, H.E.J.D.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion–Part II: Shoul der, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]




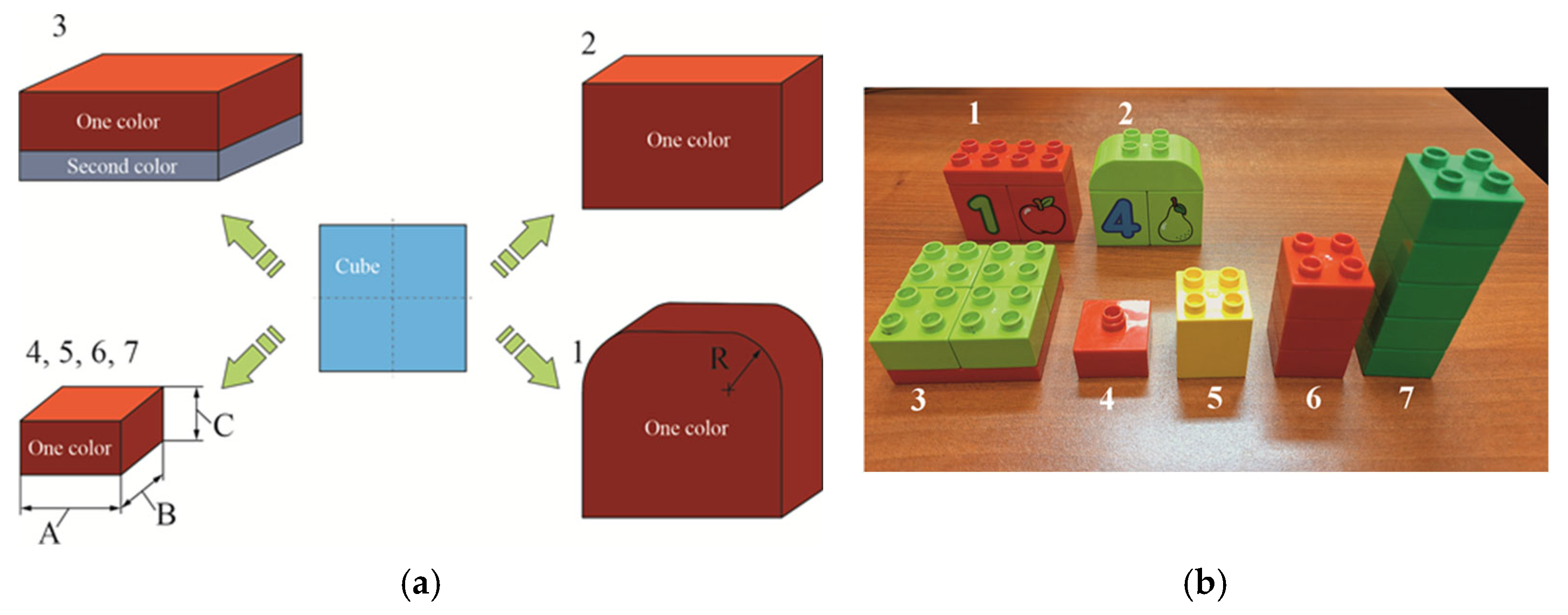





| Dimensions, [mm] | Object Number | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| D1 | 62 | 70 | 62 | 64 | 72 |
| D2 | - | - | - | - | 40 |
| d1 | - | 58 | 15 | 8 | 16 |
| d2 | - | 29 | 8 | - | 12 |
| h | - | 0.05 × d1,2 | - | - | - |
| e | - | - | 9 | - | - |
| Number of indentations/bulges | 0 | 9; 12 | 14 | 65 | 10 |
| Dimensions, [mm] | Object Number | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| A | 64 | 62 | 64 | 32 | 32 | 32 | 32 |
| B | 32 | 32 | 64 | 32 | 32 | 32 | 32 |
| C | 54 | 64 | 34 | 19 | 43 | 62 | 100 |
| R | - | 19 | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tutak, J.S.; Mucha, J. A Prototype Mechatronic Device for Upper Limb Rehabilitation and Analysis of Its Functionality. Appl. Sci. 2025, 15, 6613. https://doi.org/10.3390/app15126613
Tutak JS, Mucha J. A Prototype Mechatronic Device for Upper Limb Rehabilitation and Analysis of Its Functionality. Applied Sciences. 2025; 15(12):6613. https://doi.org/10.3390/app15126613
Chicago/Turabian StyleTutak, Jacek S., and Jacek Mucha. 2025. "A Prototype Mechatronic Device for Upper Limb Rehabilitation and Analysis of Its Functionality" Applied Sciences 15, no. 12: 6613. https://doi.org/10.3390/app15126613
APA StyleTutak, J. S., & Mucha, J. (2025). A Prototype Mechatronic Device for Upper Limb Rehabilitation and Analysis of Its Functionality. Applied Sciences, 15(12), 6613. https://doi.org/10.3390/app15126613







