The Influence of Functional Rehabilitation Braces with Resistance on Joint Coordination and ACL Force in Martial Artists Following ACL Reconstruction
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Study Design
2.3. Rehabilitation Program
- Standardized Physical Therapy Program: Conducted 5 times a week for 8 consecutive weeks. The specific content covers passive joint movement training, straight-leg raising training, quadriceps femoris electrical stimulation treatment, and knee joint range-of-motion restoration training.
- Standardized Walking Program: Conducted 2–3 times a week, spanning from the 3rd to the 8th week, for a total of 6 weeks. Walk on a treadmill at a speed of 1 m/s, rest for 2 min after every 3 min of walking, and complete 6 rounds in total. Warm up the knee joints for 5 min before walking, and take appropriate rest after the end. The total duration of each session was 40 min (see Figure 2).
2.4. Evaluation Time Points
- Pre-operation (T0): Before the operation, baseline data were comprehensively collected from all subjects, including basic physical indicators (height, weight, BMI, etc.), knee joint function evaluation, and joint range-of-motion measurement.
- 15 days after operation (T1): Evaluation of changes in knee joint range of motion. At the same time, a comprehensive joint coordination assessment was carried out on the subjects.
- 30 days after operation (T2): Evaluation of changes in knee joint range of motion was carried out again.
- 60 days after operation (T3): Evaluation of changes in knee joint range of motion. At the same time, a comprehensive joint coordination assessment was carried out on the subjects, and the joint forces and ACL forces were estimated with the help of a musculoskeletal model.
2.5. Data Collection and Analysis
2.5.1. Knee Joint Range-of-Motion Measurement
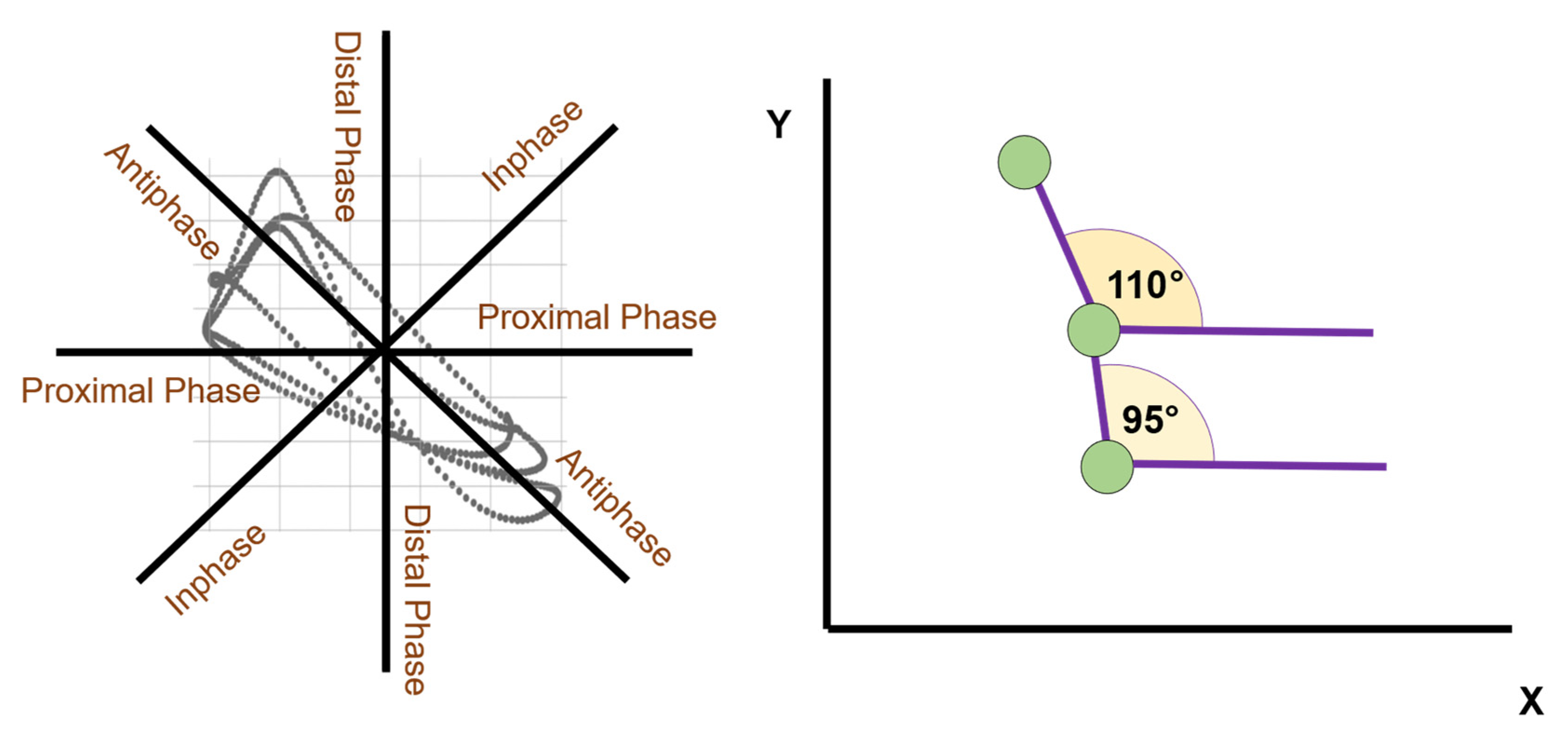
2.5.2. Joint Coordination Analysis
- In-Phase Coordination: When the coupling angle is in the range of 22.5° to 67.5° or 202.5° to 247.5°, it indicates that the two segments rotate synchronously in the same direction.
- Antiphase Coordination: When the coupling angle is in the range of 112.5° to 157.5° or 292.5° to 337.5°, it indicates that the two segments rotate in opposite directions.
- Proximal Phase Coordination: When the coupling angle is in the range of 157.5° to 202.5° or 337.5° to 360°, it indicates that the movement mainly occurs in the proximal segment.
- Distal Phase Coordination: When the coupling angle is in the range of 67.5° to 112.5° or 247.5° to 292.5°, it indicates that the movement mainly occurs in the distal segment.
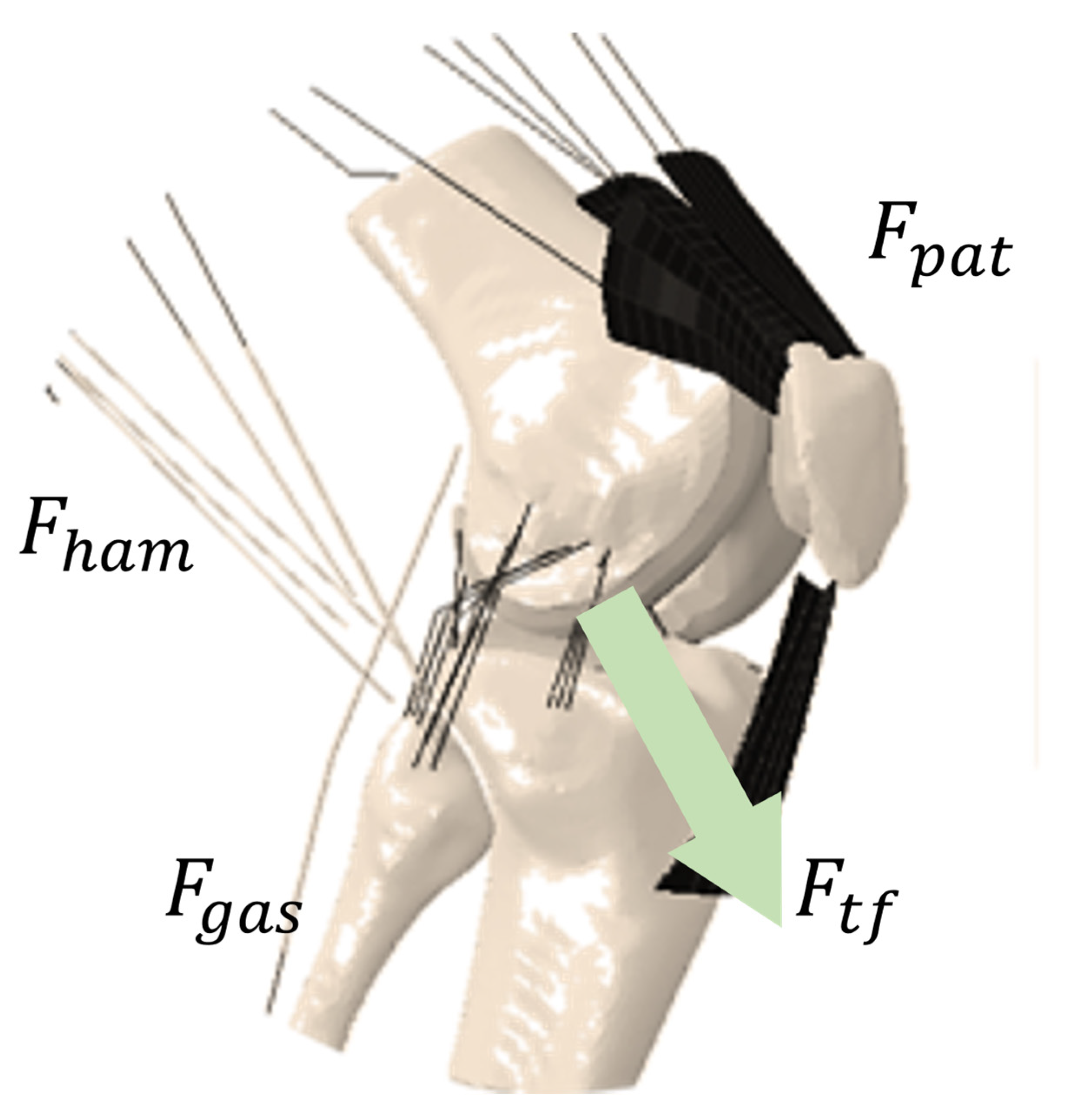
2.5.3. Musculoskeletal Model
- 1.
- Calculation of Tibiofemoral Contact Force (Ftf)
- 2.
- Calculation of the Anterior–Posterior Shear Force on the Knee Ligament (Fligament)
- 3.
- Calculation of ACL Force (FACL)
2.6. Statistical Analysis
3. Results
4. Discussion
4.1. Analysis of ACL Recovery
4.2. Joint Coordination Analysis
4.3. Force Simulation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Musahl, V.; Engler, I.D.; Nazzal, E.M.; Engler, I.D.; Nazzal, E.M.; Dalton, J.F.; Lucidi, G.A.; Hughes, J.D.; Zaffagnini, S.; Della Villa, F.; et al. Current trends in the anterior cruciate ligament part II: Evaluation, surgical technique, prevention, and rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2022, 30, 34–51. [Google Scholar] [CrossRef] [PubMed]
- Naeger, P.A.; Weatherby, P.J.; Nsekpong, T.; Naeger, P.A.; Weatherby, P.J.; Weiss, W. Simultaneous Bilateral Anterior Cruciate Ligament Revision Reconstruction. Cureus 2023, 15, e41092. [Google Scholar] [CrossRef] [PubMed]
- Dawkins, J.; Teel, J.; Kitziger, R.; Khair, M. Anterior Cruciate Ligament Injury Prevention and Rehabilitation. HSS J. Musculoskelet. J. Hosp. Spec. Surg. 2023, 19, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Della Villa, F.; Hagglund, M.; Della Villa, S.; Hägglund, M.; Ekstrand, J.; Waldén, M. Infographic. High rate of second ACL injury following ACL reconstruction in male professional footballers: An updated longitudinal analysis from 118 players in the UEFA Elite Club Injury Study. Br. J. Sports Med. 2021, 55, 1379–1380. [Google Scholar] [CrossRef] [PubMed]
- Gianakos, A.L.; Arias, C.; Batailler, C.; Gianakos, A.L.; Servien, E.; Mulcahey, M.K. Sex specific considerations in anterior cruciate ligament injuries in the female athlete: State of the art. J. ISAKOS 2024, 9, 100325. [Google Scholar] [CrossRef]
- Prodromidis, A.D.; Drosatou, C.; Thivaios, G.C.; Prodromidis, A.D.; Thivaios, G.C.; Zreik, N.; Charalambous, C.P. Timing of Anterior Cruciate Ligament Reconstruction and Relationship With Meniscal Tears: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2021, 49, 2551–2562. [Google Scholar] [CrossRef]
- Garmasheva, Z.A.; Kasimov, V.; Russkikh, A.N. Histological Analysis of Injured Anterior Cruciate Ligament in Male Athletes from Team Sports and Martial Arts. Human. Sport. Med. 2021, 21, 107–110. [Google Scholar]
- Pawlik, D.; Szyszko, M. Social and psychological conditions of pain in martial arts. In Proceedings of the 3rd Imacsss International Conference/3RD World Scientific Congress of Combat Sports and Martial Arts, Rzeszów, Poland, 15–17 October 2014; pp. 44–52. [Google Scholar]
- Kaarre, J.; Zsidai, B.; Winkler, P.W.; Zsidai, B.; Winkler, P.W.; Narup, E.; Horvath, A.; Svantesson, E.; Senorski, E.H.; Musahl, V.; et al. Different patient and activity-related characteristics result in different injury profiles for patients with anterior cruciate ligament and posterior cruciate ligament injuries. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2023, 31, 308–315. [Google Scholar] [CrossRef]
- Eggerding, V.; Reijman, M.; Meuffels, D.E.; van Es, E.; van Arkel, E.; van den Brand, I.; van Linge, J.; Zijl, J.; Bierma-Zeinstra, S.M.; Koopmanschap, M. ACL reconstruction for all is not cost-effective after acute ACL rupture. Br. J. Sports Med. 2021, 56, 24–28. [Google Scholar] [CrossRef]
- Piussi, R.; Brandt, E.; Johansson, A.; Snaebjörnsson, T.; Thomeé, R.; Samuelsson, K.; Hamrin Senorski, E. The Patient-Physiotherapist Tango: A Personalized Approach to ACL Recovery—A Qualitative Interview Study. Int. J. Sports Phys. Ther. 2024, 19, 1589–1599. [Google Scholar] [CrossRef]
- Mokhtarmanand, J.S.; Moradi, A.; Moharrami, M. Preventive Effects of Knee Brace on Anterior Cruciate Ligament Injuries in Susceptible Individuals: A Systematic Review. Trauma Mon. 2021, 26, 340–348. [Google Scholar] [CrossRef]
- Jalali, M.; Farahmand, F.; Esfandiarpour, F.; Golestanha, S.A.; Akbar, M.; Eskandari, A.; Mousavi, S.E. The effect of functional bracing on the arthrokinematics of anterior cruciate ligament injured knees during lunge exercise. Gait Posture 2018, 63, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Palmieri-Smith, R.M.; Brown, S.R.; Wojtys, E.M.; Palmieri-Smith, R.M.; Brown, S.R.; Wojtys, E.M.; Krishnan, C. Functional Resistance Training Improves Thigh Muscle Strength after ACL Reconstruction: A Randomized Clinical Trial. Med. Sci. Sports Exerc. 2022, 54, 1729–1737. [Google Scholar] [CrossRef]
- Kadlec, D.; Jordan, M.J.; Alderson, J.; Jordan, M.J.; Nimphius, S. Examining the Effects of Dynamic and Isometric Resistance Training on Knee Joint Kinetics During Unplanned Sidesteps in Elite Female Athletes. J. Strength Cond. Res. 2024, 38, 2079–2087. [Google Scholar] [CrossRef] [PubMed]
- Nyland, J.; Pyle, B.; Richards, J.; Yoshida, K.; Brey, J.; Carter, S. A clinical practice review of therapeutic movement-based anterior cruciate ligament reconstruction return to sports bridge program: The biological, biomechanical and behavioral rationale. Ann. Jt. 2023, 8, 23. [Google Scholar] [CrossRef]
- Forman, D.A.; Alizadeh, S.; Button, D.C.; Forman, D.A.; Button, D.C.; Holmes, M.W. The Use of Elastic Resistance Bands to Reduce Dynamic Knee Valgus in Squat-Based Movements: A Narrative Review. Int. J. Sports Phys. Ther. 2023, 18, 1206–1217. [Google Scholar] [CrossRef]
- Smith, J.A.; Popovich, J.M., Jr.; Kulig, K. The influence of hip strength on lower-limb, pelvis, and trunk kinematics and coordination patterns during walking and hopping in healthy women. J. Orthop. Sports Phys. Ther. 2014, 44, 525–531. [Google Scholar] [CrossRef]
- Kernozek, T.W.; Ragan, R.J. Estimation of anterior cruciate ligament tension from inverse dynamics data and electromyography in females during drop landing. Clin. Biomech. 2008, 23, 1279–1286. [Google Scholar] [CrossRef]
- Salles, J.I.; Velasques, B.; Cossich, V.; Nicoliche, E.; Ribeiro, P.; Amaral, M.V.; Motta, G. Strength training and shoulder proprioception. J. Athl. Train. 2015, 50, 277–280. [Google Scholar] [CrossRef]
- Sheikhi, B.; Letafatkar, A.; Hadadnezhad, M.; Hogg, J. Effectiveness of Injury Prevention Program Using a Global Systems Approach on High-Risk Movement Mechanics for Noncontact ACL Injury. Sports Health. 2024. [Google Scholar] [CrossRef]
- Sutor, T.W.; Kura, J.; Mattingly, A.J.; Otzel, D.M.; Yarrow, J.F. The Effects of Exercise and Activity-Based Physical Therapy on Bone after Spinal Cord Injury. Int. J. Mol. Sci. 2022, 23, 608. [Google Scholar] [CrossRef] [PubMed]
- Hewlett, J.; Kenney, J. Innovations in functional and rehabilitative knee bracing. Ann. Transl. Med. 2019, 7 (Suppl. 7), S248. [Google Scholar] [CrossRef] [PubMed]
- Focke, A.; Steingrebe, H.; Moehler, F.; Möhler, F.; Ringhof, S.; Sell, S.; Potthast, W.; Stein, T. Effect of Different Knee Braces in ACL-Deficient Patients. Front. Bioeng. Biotechnol. 2020, 8, 964. [Google Scholar] [CrossRef]
- Beynnon, B.; Good, L.; Risberg, M.; Beynnon, B.D.; Good, L.; Risberg, M.A. The Effect of Bracing on Proprioception of Knees with Anterior Cruciate Ligament Injury. J. Orthop. Sports Phys. Ther. 2002, 32, 11–15. [Google Scholar] [CrossRef]
- Chaves, T.S.; Scarpelli, M.C.; Bergamasco, J.G.A.; Silva, D.G.D.; Medalha Junior, R.A.; Dias, N.F.; Bittencourt, D.; Carello Filho, P.C.; Angleri, V.; Nóbrega, S.R.; et al. Effects of Resistance Training Overload Progression Protocols on Strength and Muscle Mass. Int. J. Sports Med. 2024, 45, 504–510. [Google Scholar] [CrossRef]
- Ewing, K.A.; Begg, R.K.; Galea, M.P.; Ewing, K.A.; Begg, R.K.; Galea, M.P.; Lee, P.V. Effects of Prophylactic Knee Bracing on Lower Limb Kinematics, Kinetics, and Energetics During Double-Leg Drop Landing at 2 Heights. Am. J. Sports Med. 2016, 44, 1753–1761. [Google Scholar] [CrossRef]
- Koester, K.; Troeller, H.; Panter, S.; Winter, E.; Patel, J.J. Overview of Intensive Care Unit-Related Physical and Functional Impairments and Rehabilitation-Related Devices. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2018, 33, 177–184. [Google Scholar] [CrossRef]
- Goerger, B.M.; Marshall, S.W.; Beutler, A.I.; Goerger, B.M.; Marshall, S.W.; Beutler, A.I.; Troy Blackburn, J.; Wilckens, J.H.; Padua, D.A. Asymmetry Of Joint Coordination And Variability In Those With Prior ACL Injury. Med. Sci. Sports Exerc. 2014, 46, 960. [Google Scholar] [CrossRef]
- Antoni, M.H.; Schneiderman, N.; Fletcher, M.A.; Goldstein, D.A.; Ironson, G.; Laperriere, A. Psychoneuroimmunology and HIV-1. J. Consult. Clin. Psychol. 1990, 58, 38–49. [Google Scholar] [CrossRef]
- Blache, Y.; de Fontenay, B.P.; Argaud, S.; Pairot de Fontenay, B.; Monteil, K. Asymmetry of Inter-joint Coordination during Single Leg Jump after Anterior Cruciate Ligament Reconstruction. Int. J. Sports Med. 2017, 38, 159–167. [Google Scholar] [CrossRef]
- Bogardus, M.A. Best Practices and Self-Care to Support Women in Living Well with Human Immunodeficiency Virus/AIDS. Nurs. Clin. North Am. 2018, 53, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Palm, H.-G.; Brattinger, F.; Stegmueller, B.; Achatz, G.; Riesner, H.-J.; Friemert, B. Effects of knee bracing on postural control after anterior cruciate ligament rupture. Knee 2012, 19, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Rocchi, J.E.; Labanca, L.; Luongo, V.; Rum, L. Innovative rehabilitative bracing with applied resistance improves walking pattern recovery in the early stages of rehabilitation after ACL reconstruction: A preliminary investigation. BMC Musculoskelet. Disord. 2020, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ramos, L.E.; Zell, J.P. Rehabilitation program for children with brachial plexus and peripheral nerve injury. Semin. Pediatr. Neurol. 2000, 7, 52–57. [Google Scholar] [CrossRef]
- Mohseni, S.S.; Farahmand, F.; Karimi, H. Arthrometric evaluation of stabilizing effect of knee functional bracing at different flexion angles. J. Sports Sci. Med. 2009, 8, 247–251. [Google Scholar]
- Riffitts, M.; Cook, H.; McClincy, M.; Bell, K. Evaluation of a Smart Knee Brace for Range of Motion and Velocity Monitoring during Rehabilitation Exercises and an Exergame. Sensors 2022, 22, 9965. [Google Scholar] [CrossRef]
- Myong, Y.; Park, S.; Cho, M.; Cho, S.Y.; Lee, W.H.; Oh, B.M.; Kim, S. Development and validation of a portable articulated dynamometry system to assess knee extensor muscle strength. Sci. Rep. 2023, 13, 11887. [Google Scholar] [CrossRef]
- Wu, G.; Ng, G.; Mak, A.; Wu, G.K.; Ng, G.Y.; Mak, A.F. Effects of knee bracing on the functional performance of patients with anterior cruciate ligament reconstruction. Arch. Phys. Med. Rehabil. 2001, 82, 282–285. [Google Scholar] [CrossRef]
- Washabaugh, E.P.; Brown, S.R.; Palmieri-Smith, R.M.; Washabaugh, E.P.; Brown, S.R.; Palmieri-Smith, R.M.; Krishnan, C. Functional Resistance Training Differentially Alters Gait Kinetics After Anterior Cruciate Ligament Reconstruction: A Pilot Study. Sports Health. 2023, 15, 372–381. [Google Scholar] [CrossRef]
- Sinclair, J.; Taylor, P.J.; Taylor, P.J. Effects of a Prophylactic Knee Sleeve on Anterior Cruciate Ligament Loading During Sport-Specific Movements. J. Sport Rehabil. 2019, 28, 1–7. [Google Scholar] [CrossRef]



| Experimental Group (n = 22) | Control Group (n = 22) | |
|---|---|---|
| Gender | 50% female | 50% female |
| Age (years) | 26.4 ± 6.3 | 27.3 ± 5.9 |
| Height (cm) | 170.7 ± 7.9 | 171.3 ± 8.1 |
| Weight (kg) | 66.2 ± 8.7 | 67.1 ± 8.5 |
| Training Experience (years) | 12.1 ± 5.9 | 13.3 ± 6.7 |
| Muscle Diameter—Rectus Femoris (cm) | 2.1 ± 0.9 | 2.2 ± 0.8 |
| Muscle Diameter—Vastus Lateralis (cm) | 1.6 ± 0.2 | 1.7 ± 0.3 |
| Muscle Diameter—Vastus Medialis (cm) | 1.3 ± 0.3 | 1.4 ± 0.4 |
| EG | CG | p | ES | Group × Time | |
|---|---|---|---|---|---|
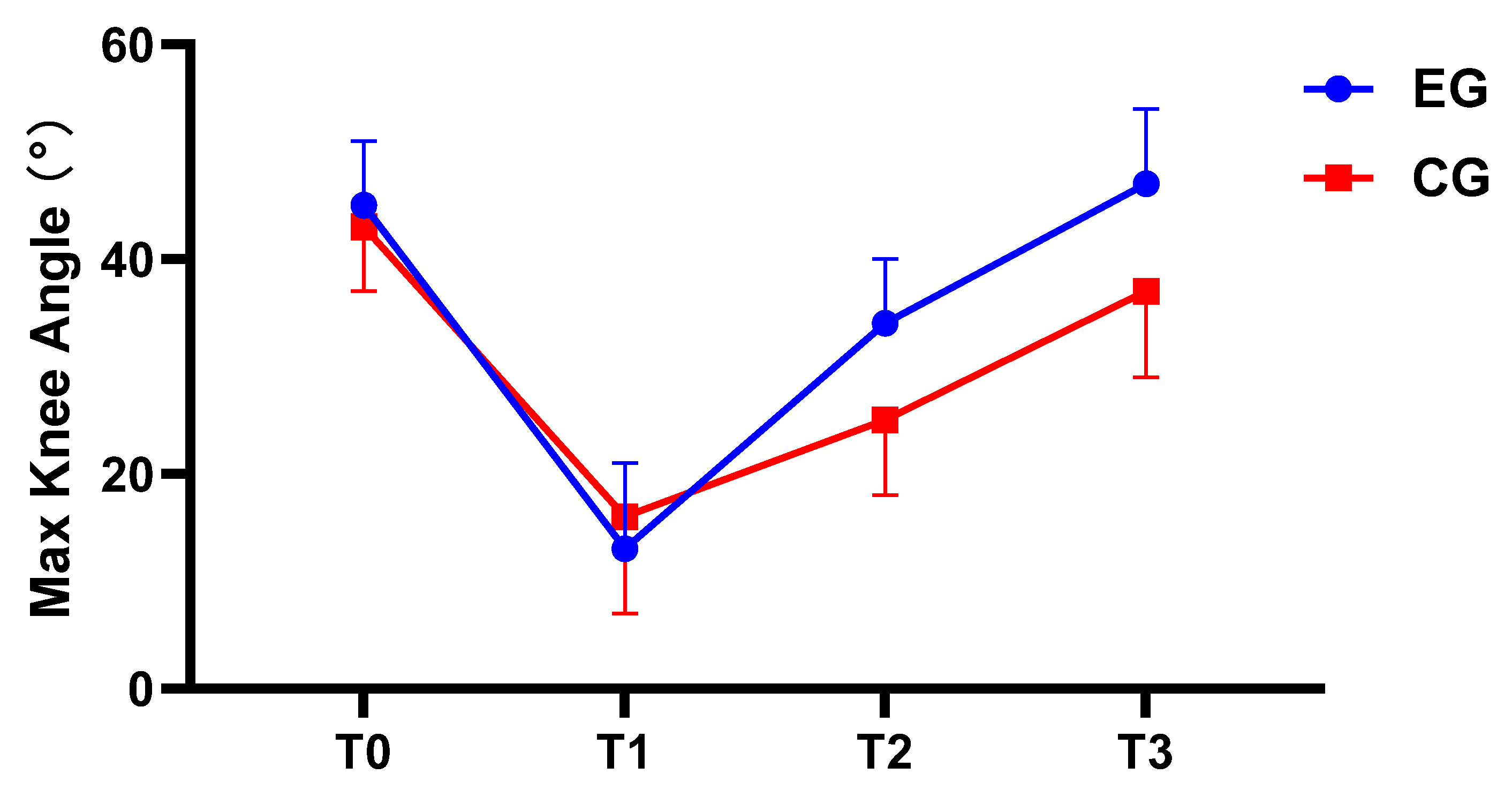
| T0 | 45.6 ± 6.9 | 43.2 ± 6.2 | 1.000 | 0.063 | p = 0.005 ES = 0.275 |
| T1 | 13.2 ± 8.8 | 16.1 ± 9.0 | 0.297 | 0.026 | |
| T2 | 34.4 ± 6.6 | 25.4 ± 7.4 | 0.000 | 0.292 | |
| T3 | 47.1 ± 7.3 | 37.7 ± 8.8 | 0.001 | 0.253 | |
| p | 0.000 | 0.000 | |||
| ES | 0.830 | 0.775 |
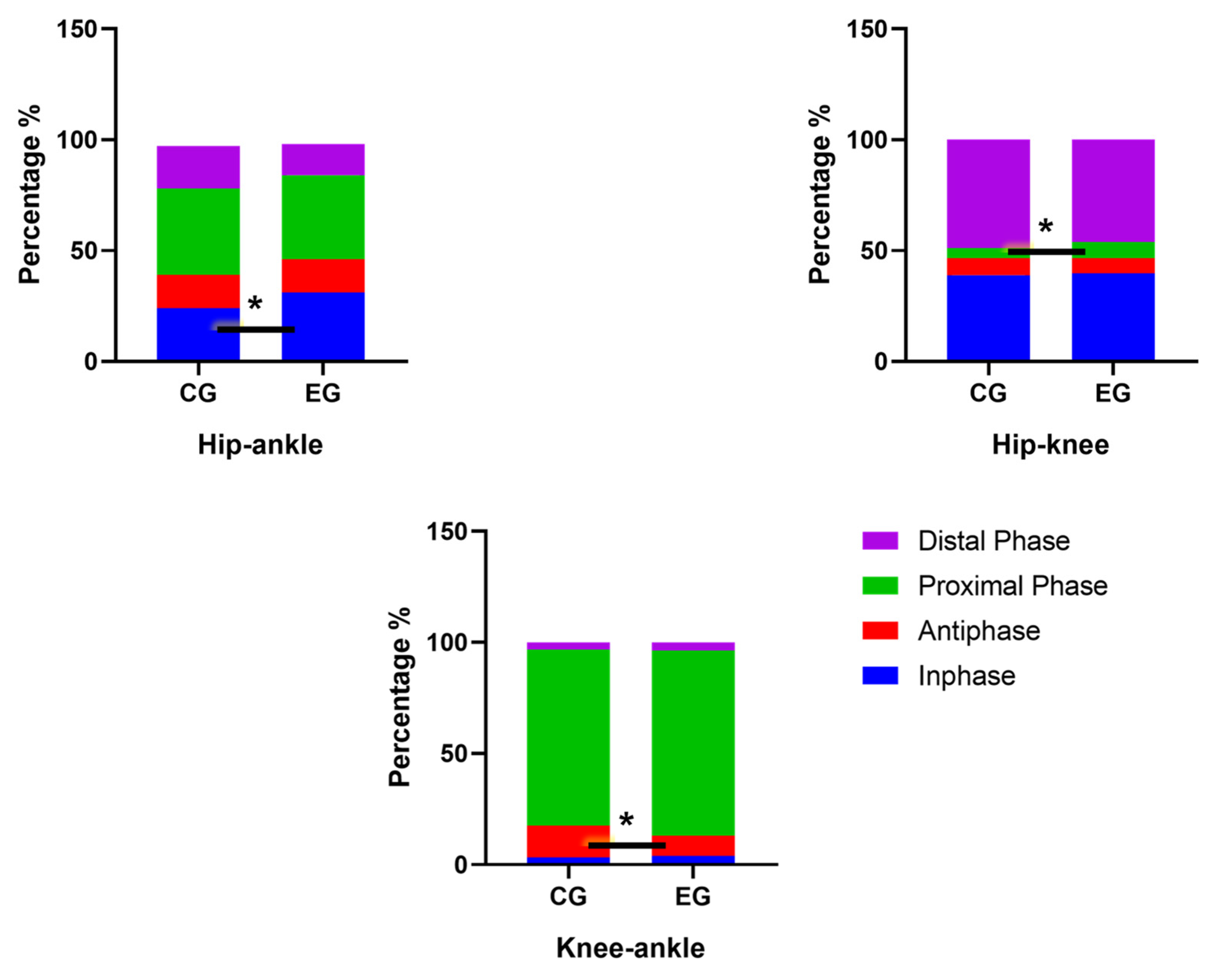
| In-Phase | Antiphase | Proximal Phase | Distal Phase | |
|---|---|---|---|---|
| Hip–ankle | ||||
| CG | 14.55 ± 10.31 | 25.51 ± 5.68 | 39.74 ± 12.53 | 20.20 ± 9.99 |
| EG | 15.32 ± 10.52 | 23.43 ± 5.18 | 39.51 ± 14.84 | 22.74 ± 9.88 |
| p | 0.705 | 0.060 | 0.423 | 0.862 |
| Hip–knee | ||||
| CG | 25.77 ± 11.63 | 17.70 ± 5.72 | 14.47 ± 5.58 | 42.02 ± 15.84 |
| EG | 26.64 ± 11.43 | 17.74 ± 5.85 | 14.67 ± 6.63 | 40.95 ± 15.73 |
| p | 0.728 | 0.537 | 0.492 | 0.587 |
| Knee–ankle | ||||
| CG | 4.34 ± 3.65 | 13.27 ± 5.89 | 58.66 ± 9.37 | 23.73 ± 12.64 |
| EG | 3.41 ± 2.64 | 14.43 ± 5.79 | 59.95 ± 8.29 | 22.21 ± 12.39 |
| p | 0.160 | 0.926 | 0.979 | 0.467 |
| In-Phase | Antiphase | Proximal Phase | Distal Phase | |
|---|---|---|---|---|
| Hip–ankle | ||||
| CG | 24.63 ± 10.12 | 15.85 ± 5.35 | 39.96 ± 6.98 | 19.56 ± 10.76 |
| EG | 31.51 ± 6.13 | 15.25 ± 5.72 | 38.63 ± 6.69 | 14.61 ± 10.72 |
| p | 0.013 | 0.292 | 0.202 | 0.483 |
| Hip–knee | ||||
| CG | 38.89 ± 12.35 | 7.69 ± 4.64 | 4.44 ± 2.85 | 48.98 ± 16.48 |
| EG | 39.77 ± 10.51 | 6.79 ± 4.49 | 7.26 ± 1.47 | 46.18 ± 15.70 |
| p | 0.164 | 0.958 | <0.001 | 0.968 |
| Knee–ankle | ||||
| CG | 3.26 ± 2.91 | 14.25 ± 5.75 | 79.28 ± 8.17 | 3.21 ± 2.33 |
| EG | 3.93 ± 2.96 | 9.16 ± 5.76 | 83.27 ± 9.15 | 3.64 ± 2.53 |
| p | 0.280 | 0.015 | 0.096 | 0.236 |
| EG | CG | t | p | ES | |
|---|---|---|---|---|---|
| FACL | 0.51 ± 0.13 | 0.63 ± 0.17 | −2.24 | 0.030 | 0.69 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Li, H. The Influence of Functional Rehabilitation Braces with Resistance on Joint Coordination and ACL Force in Martial Artists Following ACL Reconstruction. Appl. Sci. 2025, 15, 6265. https://doi.org/10.3390/app15116265
Wang X, Li H. The Influence of Functional Rehabilitation Braces with Resistance on Joint Coordination and ACL Force in Martial Artists Following ACL Reconstruction. Applied Sciences. 2025; 15(11):6265. https://doi.org/10.3390/app15116265
Chicago/Turabian StyleWang, Xiaoyan, and Haojie Li. 2025. "The Influence of Functional Rehabilitation Braces with Resistance on Joint Coordination and ACL Force in Martial Artists Following ACL Reconstruction" Applied Sciences 15, no. 11: 6265. https://doi.org/10.3390/app15116265
APA StyleWang, X., & Li, H. (2025). The Influence of Functional Rehabilitation Braces with Resistance on Joint Coordination and ACL Force in Martial Artists Following ACL Reconstruction. Applied Sciences, 15(11), 6265. https://doi.org/10.3390/app15116265




