Surgical Treatment of Distal Radius Fractures Using Minimally Invasive Plate Osteosynthesis or Open Reduction and Internal Fixation: A Five-Year Comparative Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Aspects
2.2. Eligibility Criteria
2.3. Description of the Experimental Stage
2.4. Scores
- DASH (Disabilities of the Arm, Shoulder, and Hand): A self-administered 30-item questionnaire designed to measure upper limb disability and symptom severity. Each item assesses difficulty in performing various daily activities, with responses ranging from 1 (no difficulty) to 5 (unable to perform the activity). The final score is scaled from 0 to 100, where 0 represents no disability, and 100 indicates severe impairment. Lower scores reflect better functional ability and less disability;
- PRWE (Patient-Rated Wrist Evaluation): A condition-specific tool designed to assess pain and functional impairment in wrist injuries. It consists of 15 items divided into two subscales: pain (5 items) and function (10 items). Each item is scored on a scale from 0 (no pain or difficulty) to 10 (severe pain or difficulty), with a total score ranging from 0 to 100. Higher scores indicate greater pain and functional limitation;
- Mayo Wrist Score: A clinician-administered assessment tool used to evaluate overall wrist function. It includes four components: pain intensity, functional status (ability to work and perform daily activities), range of motion (ROM), and grip strength. Each component contributes to a total score ranging from 0 to 100, with higher scores indicating better wrist function and minimal impairment. This score is widely used to provide an objective measure of recovery following wrist fractures and surgical interventions (Table 1).
2.5. Statistical Analysis
2.6. Limitations and Bias
3. Results
4. Discussion
Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MIPO | Minimally Invasive Plate Osteosynthesis |
| ORIF | Open Reduction and Internal Fixation |
| DRF | Distal Radius Fracture |
| PKW | Percutaneous Kirschner Wire |
| VLP | Volar Locking Plate |
| DASH | Disabilities of the Arm, Shoulder, and Hand |
| PRWE | Patient-Rated Wrist Evaluation |
| MAYO | Mayo Wrist Score |
| ROM | Range of Motion |
| CRPS | Complex Regional Pain Syndrome |
| FPL | Flexor Pollicis Longus |
| EPL | Extensor Pollicis Longus |
| IRB | Institutional Review Board |
| RCT | Randomized Controlled Trial |
| SD | Standard Deviation |
References
- Court-Brown, C.M.; Caesar, B. Epidemiology of adult fractures: A review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Mattila, V.M.; Huttunen, T.T.; Sillanpää, P.; Niemi, S.; Pihlajamäki, H.; Kannus, P. Significant Change in the Surgical Treatment of Distal Radius Fractures: A Nationwide Study Between 1998 and 2008 in Finland. J. Trauma Inj. Infect. Crit. Care 2011, 71, 939–943. [Google Scholar] [CrossRef]
- Gopal, N.; Anil, A.; Gopal, M.; Bhat, A.K. A Comparison Between Volar Locking Plates and Percutaneous Pinning in the Treatment of Distal Radius Fractures: A Systematic Review. J. Hand Surg. 2025, 50, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Candela, V.; Di Lucia, P.; Carnevali, C.; Milanese, A.; Spagnoli, A.; Villani, C.; Gumina, S. Epidemiology of distal radius fractures: A detailed survey on a large sample of patients in a suburban area. J. Orthop. Traumatol. 2022, 23, 43. [Google Scholar] [CrossRef] [PubMed]
- Karl, J.W.; Olson, P.R.; Rosenwasser, M.P. The Epidemiology of Upper Extremity Fractures in the United States, 2009. J. Orthop. Trauma 2015, 29, e242. [Google Scholar] [CrossRef]
- Mauck, B.M.; Swigler, C.W. Evidence-Based Review of Distal Radius Fractures. Orthop. Clin. N. Am. 2018, 49, 211–222. [Google Scholar] [CrossRef]
- Garcia-Elias, M.; Folgar, M.Á.V. The management of wrist injuries: An international perspective. Injury 2006, 37, 1049–1056. [Google Scholar] [CrossRef]
- Porrino, J.A.; Maloney, E.; Scherer, K.; Mulcahy, H.; Ha, A.S.; Allan, C. Fracture of the Distal Radius: Epidemiology and Premanagement Radiographic Characterization. Am. J. Roentgenol. 2014, 203, 551–559. [Google Scholar] [CrossRef]
- MacIntyre, N.J.; Dewan, N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J. Hand Ther. 2016, 29, 136–145. [Google Scholar] [CrossRef]
- Franceschi, F.; Franceschetti, E.; Paciotti, M.; Cancilleri, F.; Maffulli, N.; Denaro, V. Volar locking plates versus K-wire/pin fixation for the treatment of distal radial fractures: A systematic review and quantitative synthesis. Br. Med. Bull. 2015, 115, 91–110. [Google Scholar] [CrossRef]
- Costa, M.L.; Achten, J.; Rangan, A.; Lamb, S.E.; Parsons, N.R. Percutaneous fixation with Kirschner wires versus volar locking-plate fixation in adults with dorsally displaced fracture of distal radius: Five-year follow-up of a randomized controlled trial. Bone Jt. J. 2019, 101-B, 978–983. [Google Scholar] [CrossRef]
- Peng, F.; Liu, Y.; Wan, Z. Percutaneous pinning versus volar locking plate internal fixation for unstable distal radius fractures: A meta-analysis. J. Hand Surg. Eur. Vol. 2018, 43, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, H.; Kleinlugtenbelt, Y.V.; Mundi, R.; Ristevski, B.; Goslings, J.C.; Bhandari, M. Are Volar Locking Plates Superior to Percutaneous K-wires for Distal Radius Fractures? A Meta-analysis. Clin. Orthop. 2015, 473, 3017–3027. [Google Scholar] [CrossRef]
- Zyluk, A.; Janowski, P.; Szlosser, Z.; Puchalski, P. Percutaneous K-wires vs palmar locking plate fixation for different types of distal radial fractures: A comparison of the outcomes of two methods to controll our guidelines. Handchir. Mikrochir. Plast. Chir. 2018, 50, 319–325. [Google Scholar] [CrossRef]
- Khan, J.I.; Hussain, F.N.; Mehmood, T.; Adil, O. A comparative study of functional outcome of treatment of intra articular fractures of distal radius fixed with percutaneous Kirschner’s wires vs T-plate. Pak. J. Med. Sci. 2017, 33, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Egund, L.; McGuigan, F.E.; Egund, N.; Besjakov, J.; Åkesson, K.E. Patient-related outcome, fracture displacement and bone mineral density following distal radius fracture in young and older men. BMC Musculoskelet. Disord. 2020, 21, 816. [Google Scholar] [CrossRef]
- Nellans, K.W.; Kowalski, E.; Chung, K.C. The Epidemiology of Distal Radius Fractures. Hand Clin. 2012, 28, 113–125. [Google Scholar] [CrossRef]
- Chung, K.C.; Shauver, M.J.; Birkmeyer, J.D. Trends in the United States in the Treatment of Distal Radial Fractures in the Elderly. J. Bone Jt. Surg. 2009, 91, 1868–1873. [Google Scholar] [CrossRef] [PubMed]
- Wilcke, M.K.T.; Hammarberg, H.; Adolphson, P.Y. Epidemiology and changed surgical treatment methods for fractures of the distal radius: A registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop. 2013, 84, 292–296. [Google Scholar] [CrossRef]
- Labbe, F.; Daoulas, T.; Letissier, H.; Liverneaux, P.; Ducournau, F. Distal radius fracture osteosynthesis by volar locking plate: Influence of epiphyseal screw positioning on risk of loss of reduction. Hand Surg. Rehabil. 2024, 43, 101743. [Google Scholar] [CrossRef]
- Floquet, A.; Druart, T.; Lavantes, P.; Vendeuvre, T.; Delaveau, A. Flexor tendon rupture after volar plating of distal radius fracture: A systematic review of the literature. Hand Surg. Rehabil. 2021, 40, 535–546. [Google Scholar] [CrossRef]
- Zelenski, N.A.; Schmidt, E.; Chin, M.; Gittings, D.; Steinberg, D.; Hast, M.W. Flexor Pollicis Longus Tendon Wear Associated with Volar Plating: A Cadaveric Study. J. Hand Surg. 2021, 46, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Caruso, G.; Aquino, A.; Preziuso, L.; Martini, L.; Vitali, A.; Petrini, A. Il Trattamento Delle Fratture del Radio Distale Nell’anziano. Riv Chir Mano 2010, 47, 22–30. [Google Scholar]
- Pacchiarini, L.; Massimo Oldrini, L.; Feltri, P.; Lucchina, S.; Filardo, G.; Candrian, C. Complications after volar plate synthesis for distal radius fractures. EFORT Open Rev. 2024, 9, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Kamal, R. Enhanced Approaches to the Treatment of Distal Radius Fractures. Hand Clin. 2023, 39, 515–521. [Google Scholar] [CrossRef]
- Gullborg, E.J.; Kim, J.H.; Ward, C.M.; Simcock, X.C. Optimizing Treatment Strategies for Distal Radius Fractures in Osteoporosis: A Comparative Review. Med. Kaunas Lith. 2024, 60, 1848. [Google Scholar] [CrossRef]
- Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE) Study Group; Lawson, A.; Naylor, J.M.; Buchbinder, R.; Ivers, R.; Balogh, Z.J.; Smith, P.; Xuan, W.; Howard, K.; Vafa, A.; et al. Surgical Plating vs Closed Reduction for Fractures in the Distal Radius in Older Patients: A Randomized Clinical Trial. JAMA Surg. 2021, 156, 229–237. [Google Scholar] [CrossRef]
- Patiño, J.M.; Rullan Corna, A.F.; Michelini, A.; Abdon, I. Distal radius fractures—Treatment with volar locking plates—Functional results according to fracture type. Rev. Fac. Cienc. Medicas Cordoba Argent. 2020, 77, 272–275. [Google Scholar] [CrossRef]
- Karantana, A.; Downing, N.D.; Forward, D.P.; Hatton, M.; Taylor, A.M.; Scammell, B.E.; Moran, C.G.; Davis, T.R.C. Surgical Treatment of Distal Radial Fractures with a Volar Locking Plate Versus Conventional Percutaneous Methods: A Randomized Controlled Trial. J. Bone Jt. Surg. 2013, 95, 1737–1744. [Google Scholar] [CrossRef]
- Tariq, M.A.; Ali, U.; Uddin, Q.S.; Altaf, Z.; Mohiuddin, A. Comparison between Volar Locking Plate and Kirschner Wire Fixation for Unstable Distal Radius Fracture: A Meta-Analysis of Randomized Controlled Trials. J. Wrist Surg. 2024, 13, 469–480. [Google Scholar] [CrossRef]
- Youlden, D.J.; Sundaraj, K.; Smithers, C. Volar locking plating versus percutaneous Kirschner wires for distal radius fractures in an adult population: A meta-analysis. ANZ J. Surg. 2019, 89, 821–826. [Google Scholar] [CrossRef]
- Brennan, S.A.; Kiernan, C.; Beecher, S.; O’Reilly, R.T.; Devitt, B.M.; Kearns, S.R.; O’Sullivan, M.E. Volar plate versus k-wire fixation of distal radius fractures. Injury 2016, 47, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.R.K.; Kundu, N.K. Evaluation of Functional Outcome of Unstable Distal Radial Fracture Treatment: A Comparison between Internal & External Fixations. Int. J. Med. Sci. Clin. Res. Stud. 2022, 2, 56–72. [Google Scholar] [CrossRef]
- Testa, G.; Panvini, F.M.C.; Vaccalluzzo, M.S.; Cristaudo, A.G.; Sapienza, M.; Pavone, V. Surgical Treatment of Periarticular Distal Radius Fracture in Elderly: A Systematic Review. Medicina 2024, 60, 1671. [Google Scholar] [CrossRef]
- Alter, T.H.; Ilyas, A.M. Complications Associated with Volar Locking Plate Fixation of Distal Radial Fractures. JBJS Rev. 2018, 6, e7. [Google Scholar] [CrossRef]
- Soong, M.; Van Leerdam, R.; Guitton, T.G.; Got, C.; Katarincic, J.; Ring, D. Fracture of the Distal Radius: Risk Factors for Complications After Locked Volar Plate Fixation. J. Hand Surg. 2011, 36, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Fulchignoni, C.; Alessandri Bonetti, M.; Rovere, G.; Ziranu, A.; Maccauro, G.; Pataia, E. Wide awake surgery for flexor tendon primary repair: A literature review. Orthop. Rev. 2020, 12, 8668. [Google Scholar] [CrossRef]
- Alessandri Bonetti, M.; Rovere, G.; Fulchignoni, C.; De Santis, V.; Ziranu, A.; Maccauro, G.; Pataia, E. Autologous fat transplantation for the treatment of trapeziometacarpal joint osteoarthritis. Orthop. Rev. 2020, 12, 8666. [Google Scholar] [CrossRef]





| Category | Score | Findings |
|---|---|---|
| 25 | No pain |
| 20 | Mild, occasional | |
| 15 | Moderate, tolerable | |
| 0 | Severe to intolerable | |
| 25 | Returned to regular employment |
| 20 | Restricted employment | |
| 15 | Able to work, unemployed | |
| 0 | Unable to work because of pain | |
| 25 | 100% or 120° or more |
| 15 | 75–100% or 90–120° | |
| 10 | 50–75% or 60–90° | |
| 5 | 25–50% or 30–60° | |
| 0 | 0–25% or 30° or less | |
| 25 | 100% |
| 15 | 75–100% | |
| 10 | 50–75% | |
| 5 | 25–50% | |
| 0 | 0–25% |
| Groups | Number of Patients | Mean Age (SD) | Men | Women |
|---|---|---|---|---|
| 18 | 65 (9.59) | 5 | 13 |
| 9 | 66.2 (8.18) | 2 | 7 |
| 6 | 49.1 (11.81) | 4 | 2 |
| 9 | 60.8 (12.18) | 4 | 5 |
| Treatment | Number of Patients | Mean Age (SD) | Men | Women |
|---|---|---|---|---|
| PKW | 27 | 65.4 (9.17) | 7 | 20 |
| VLP | 15 | 56.2 (13.33) | 8 | 7 |
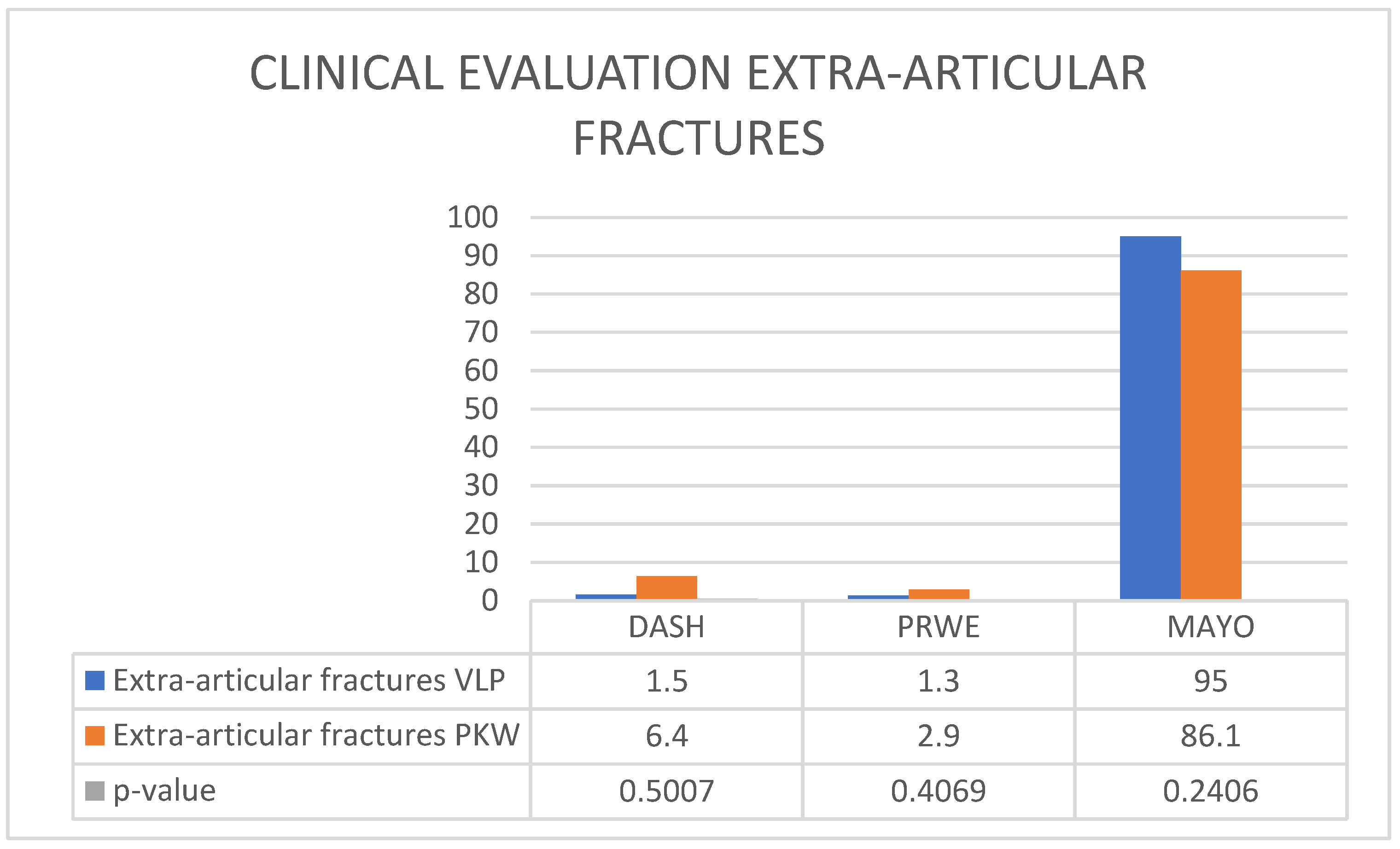
| Extra-Articular Fractures | DASH (SD) | PRWE (SD) | MAYO (SD) |
|---|---|---|---|
| VLP | 1.5 (0.8) | 1.3 (0.6) | 95 (4.5) |
| PKW | 6.4 (2.1) | 2.9 (1.5) | 86.1 (6.2) |
| p value | 0.5007 | 0.4069 | 0.2406 |
| Intra-Articular Fractures | DASH (SD) | PRWE (SD) | MAYO (SD) |
|---|---|---|---|
| VLP | 6.6 (3.2) | 12.9 (5.1) | 78.9 (7.8) |
| PKW | 19.7 (4.9) | 21.1 (6.3) | 72.2 (8.5) |
| p value | 0.0981 | 0.3661 | 0.4503 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rovere, G.; Pirri, P.; Murgante, G.; De Luna, V.; Testa, A.; Fidone, G.; Liuzza, F.; Farsetti, P.; De Maio, F. Surgical Treatment of Distal Radius Fractures Using Minimally Invasive Plate Osteosynthesis or Open Reduction and Internal Fixation: A Five-Year Comparative Follow-Up Study. Appl. Sci. 2025, 15, 6235. https://doi.org/10.3390/app15116235
Rovere G, Pirri P, Murgante G, De Luna V, Testa A, Fidone G, Liuzza F, Farsetti P, De Maio F. Surgical Treatment of Distal Radius Fractures Using Minimally Invasive Plate Osteosynthesis or Open Reduction and Internal Fixation: A Five-Year Comparative Follow-Up Study. Applied Sciences. 2025; 15(11):6235. https://doi.org/10.3390/app15116235
Chicago/Turabian StyleRovere, Giuseppe, Pierfrancesco Pirri, Gianmarco Murgante, Vincenzo De Luna, Aurelio Testa, Giovanna Fidone, Francesco Liuzza, Pasquale Farsetti, and Fernando De Maio. 2025. "Surgical Treatment of Distal Radius Fractures Using Minimally Invasive Plate Osteosynthesis or Open Reduction and Internal Fixation: A Five-Year Comparative Follow-Up Study" Applied Sciences 15, no. 11: 6235. https://doi.org/10.3390/app15116235
APA StyleRovere, G., Pirri, P., Murgante, G., De Luna, V., Testa, A., Fidone, G., Liuzza, F., Farsetti, P., & De Maio, F. (2025). Surgical Treatment of Distal Radius Fractures Using Minimally Invasive Plate Osteosynthesis or Open Reduction and Internal Fixation: A Five-Year Comparative Follow-Up Study. Applied Sciences, 15(11), 6235. https://doi.org/10.3390/app15116235







