Breast Cancer Detection Using a High-Performance Ultra-Wideband Vivaldi Antenna in a Radar-Based Microwave Breast Cancer Imaging Technique
Abstract
1. Introduction
2. Materials and Methods
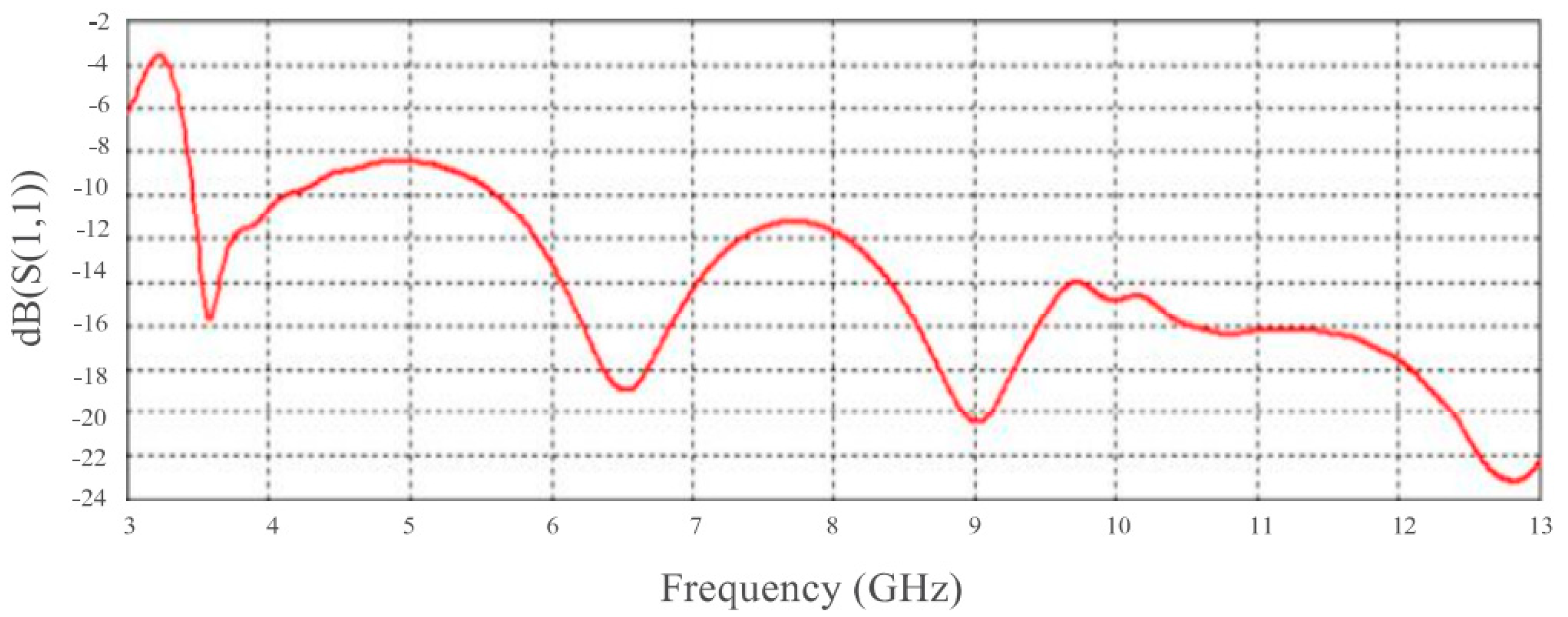
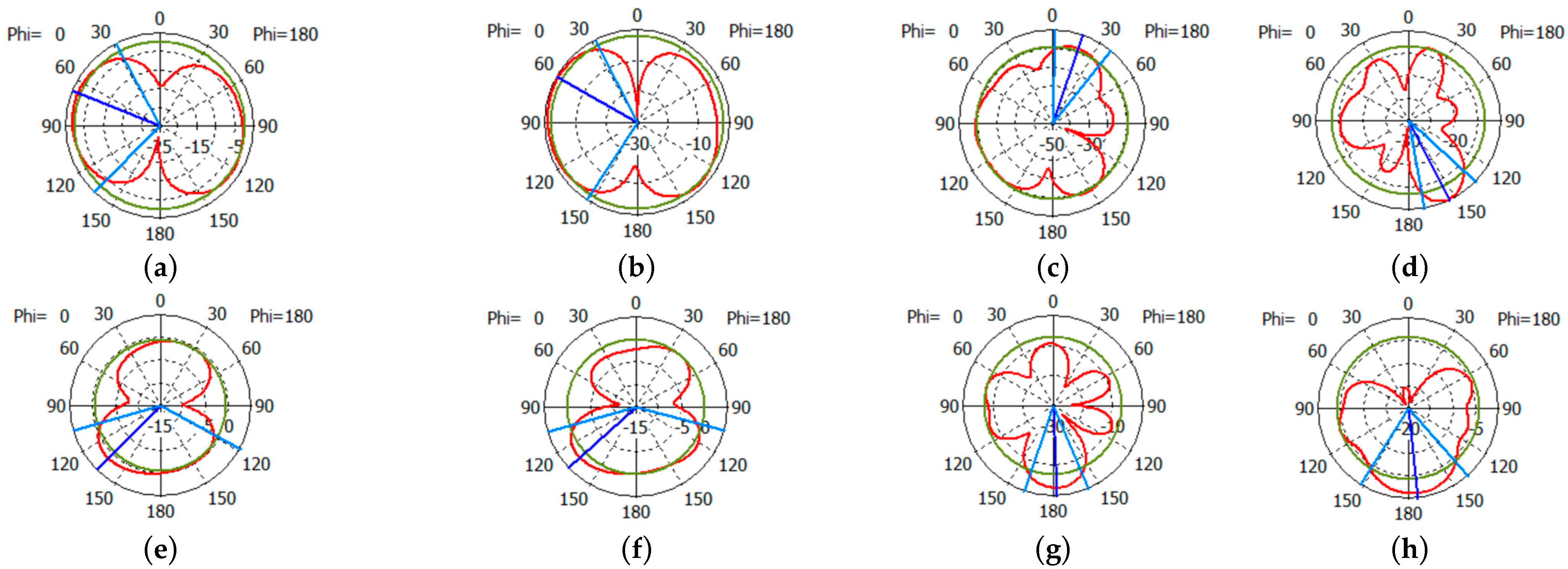
Antenna Design
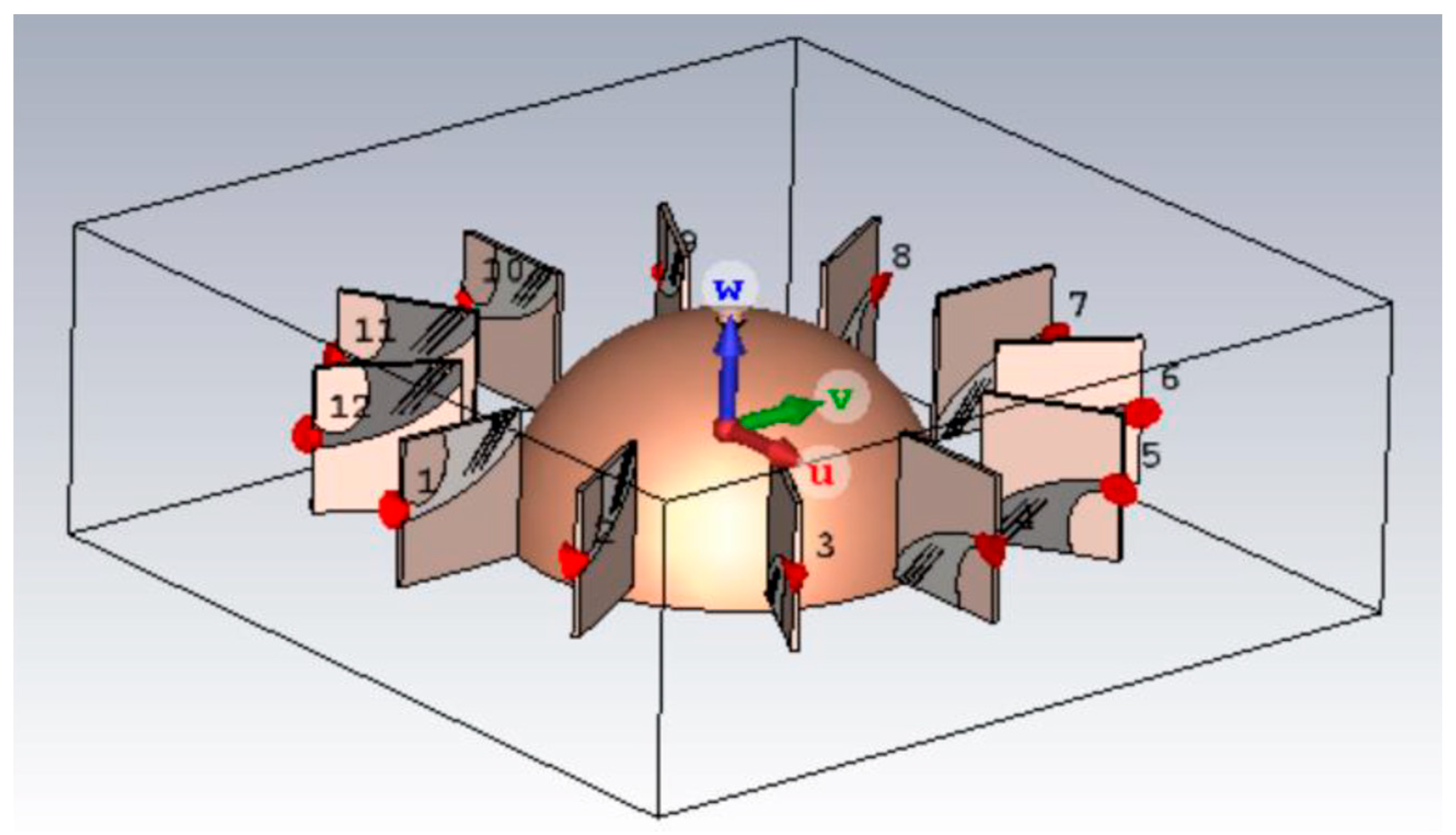
3. Simulation Environment and RMWBI System
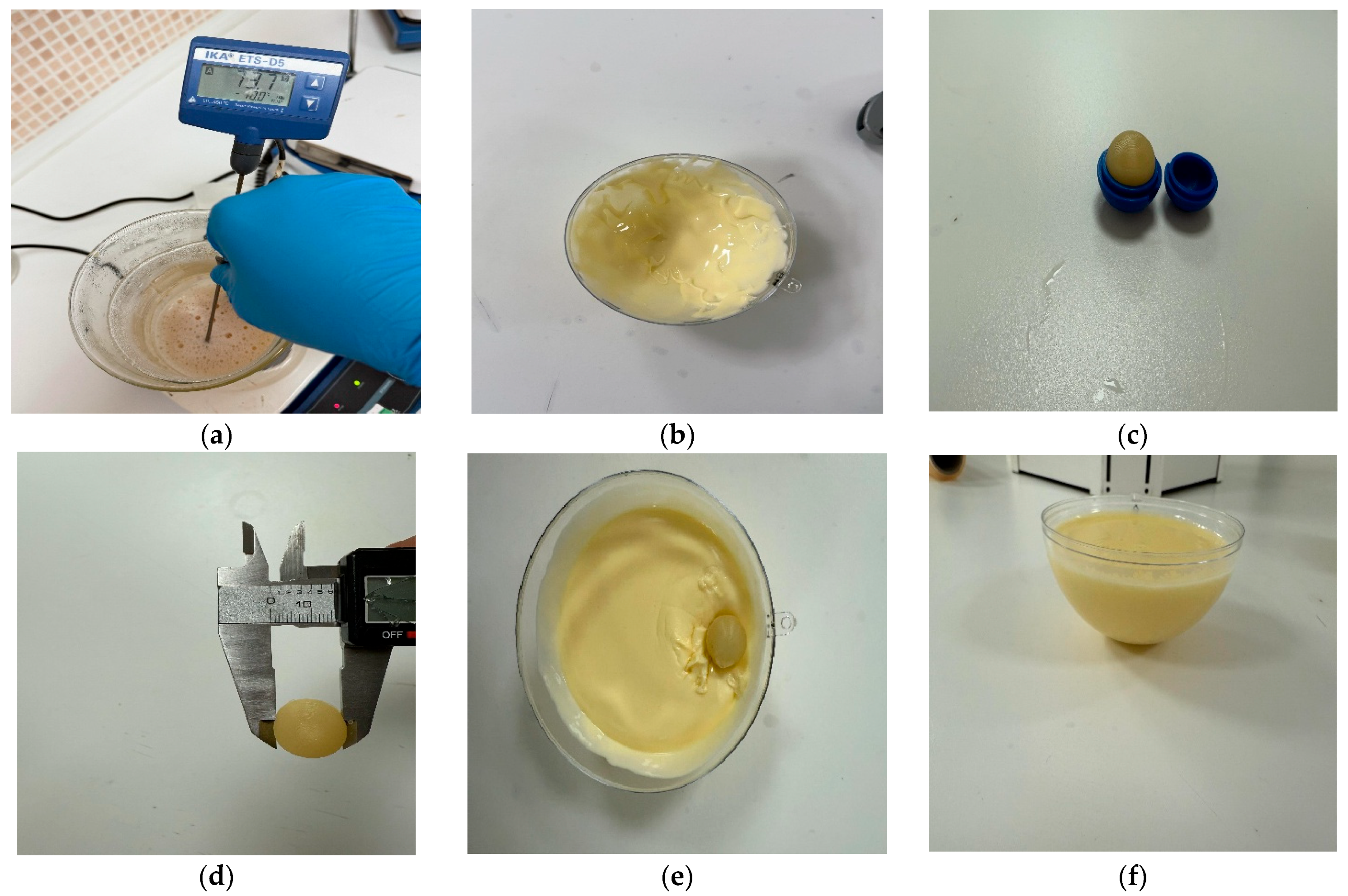
3.1. Breast Model
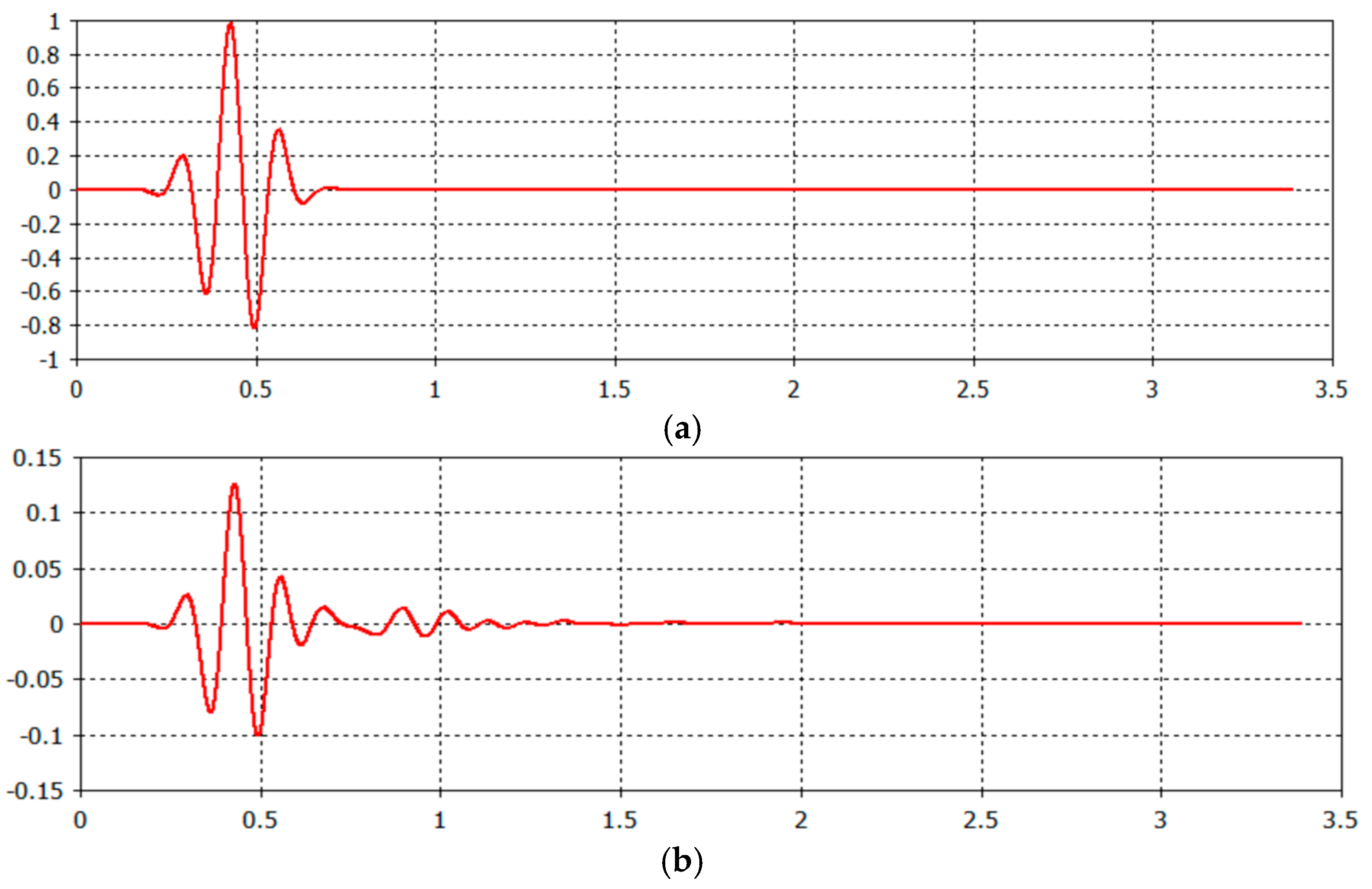
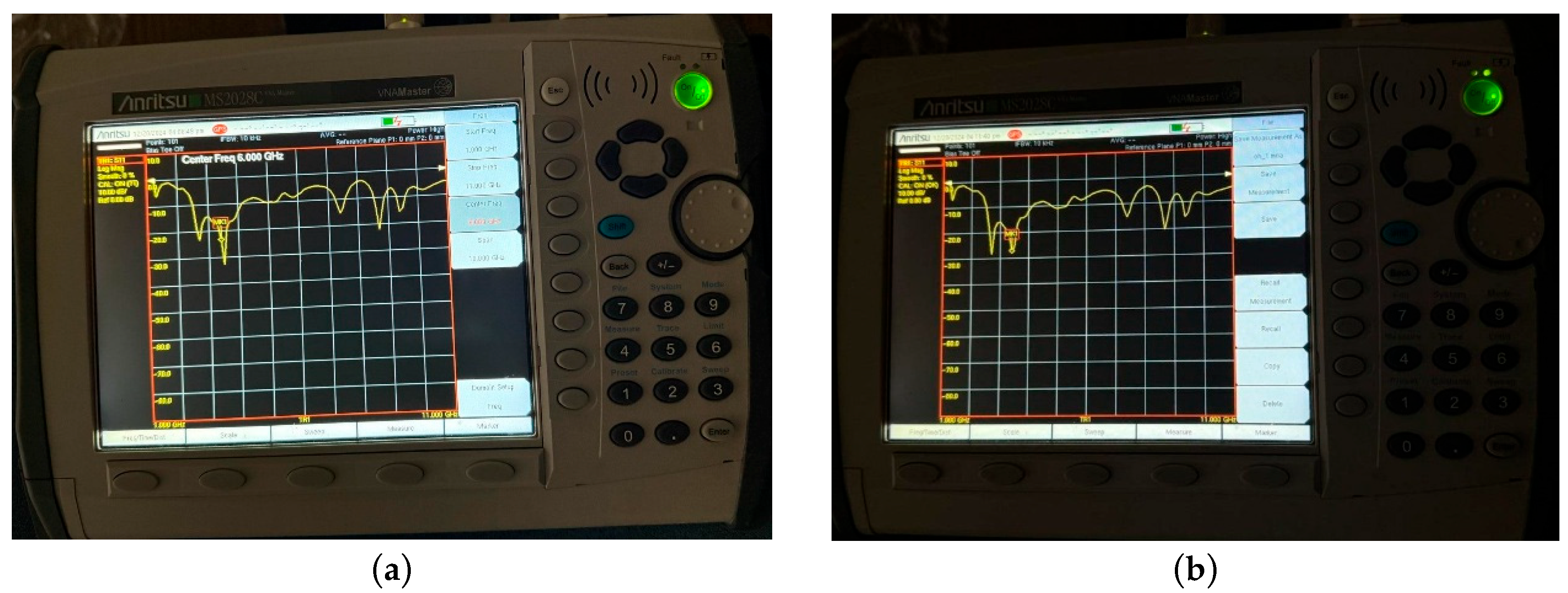
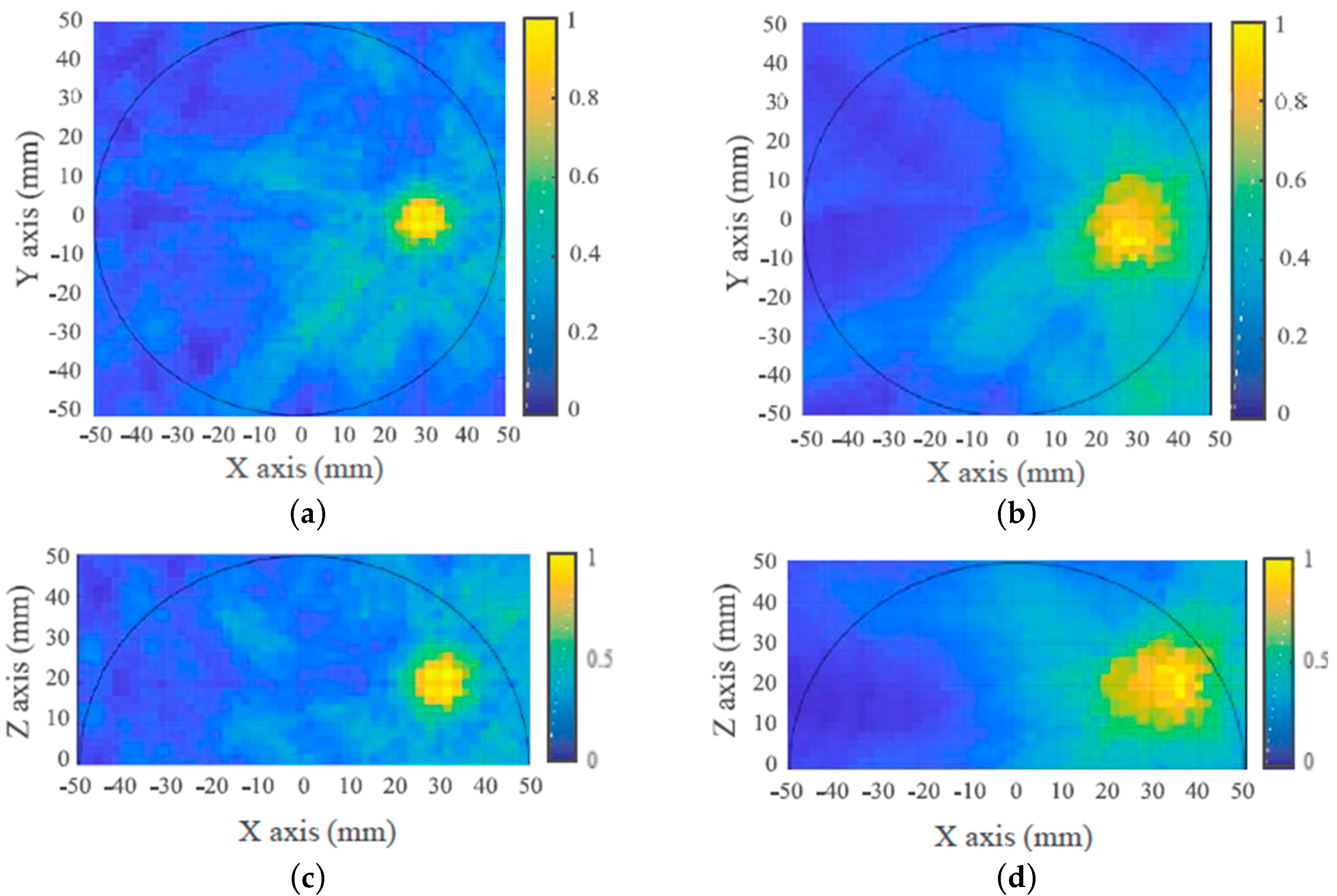
3.2. RMWBI System and Visualization in the Simulation Environment
4. Results and Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chhikara, B.S.; Parang, K. Global Cancer Statistics 2022: The trends projection analysis. Chem. Biol. Lett. 2023, 10, 451. [Google Scholar]
- American Cancer Society. Available online: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html (accessed on 12 January 2023).
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 13 March 2024).
- Mittal, P.; Singh, S.; Singh, A.; Singh, I.K. Current advances in drug delivery systems for treatment of Triple negative breast cancer (TNBC). Chem. Biol. Lett. 2020, 7, 1–12. [Google Scholar]
- Chaurasia, A.S.; Shankhwar, A.K.; Singh, A. Design and analysis of the Flexible Antenna behavior for Microwave Imaging of breast cancer. J. Integr. Sci. Technol. 2024, 12, 727. [Google Scholar] [CrossRef]
- Aldhaeebi, M.A.; Almoneef, T.; Bamatraf, S.; Aldhaibain, A.O.; Bakhalah, O.; Alhdad, S.; Bakhalah, S.; Saleem, M.K. Near-field metasurface sensor for an early-stage breast cancer detection. Sens. Int. 2025, 6, 100305. [Google Scholar] [CrossRef]
- Pomerantz, B.J. Imaging and Interventional Radiology for Cancer Surgical Oncology for the General Surgeon. Issue Surg. Clin. 2020, 100, 499. [Google Scholar]
- Kaiser, C.G.; Dietzel, M.; Vag, T.; Rübenthaler, J.; Froelich, M.F.; Tollens, F. Impact of specificity on cost-effectiveness of screening women at high risk of breast cancer with magnetic resonance imaging, mammography and ultrasound. Eur. J. Radiol. 2021, 137, 109576. [Google Scholar] [CrossRef] [PubMed]
- Hernández, M.L.; Osorio, S.; Florez, K.; Ospino, A.; Díaz, G.M. Abbreviated magnetic resonance imaging in breast cancer: A systematic review of literature. Eur. J. Radiol. Open 2021, 8, 100307. [Google Scholar] [CrossRef]
- Sueoka, S.; Sasada, S.; Masumoto, N.; Emi, A.; Kadoya, T.; Okada, M. Performance of dedicated breast positron emission tomography in the detection of small and low-grade breast cancer. Breast Cancer Res. Treat. 2021, 187, 125–133. [Google Scholar] [CrossRef]
- Aldhaeebi, M.A.; Alzoubi, K.; Almoneef, T.S.; Bamatraf, S.M.; Attia, H.; Ramahi, O.M. Review of microwaves techniques for breast cancer detection. Sensors 2020, 20, 2390. [Google Scholar] [CrossRef]
- AlSawaftah, N.; El-Abed, S.; Dhou, S.; Zakaria, A. Microwave imaging for early breast cancer detection: Current state, challenges, and future directions. J. Imaging 2022, 8, 123. [Google Scholar] [CrossRef]
- Elsheakh, D.N.; Mohamed, R.A.; Fahmy, O.M.; Ezzat, K.; Eldamak, A.R. Complete breast cancer detection and monitoring system by using microwave textile based antenna sensors. Biosensors 2023, 13, 87. [Google Scholar] [CrossRef] [PubMed]
- Adachi, M.; Nakagawa, T.; Fujioka, T.; Mori, M.; Kubota, K.; Oda, G.; Kikkawa, T. Feasibility of portable microwave imaging device for breast cancer detection. Diagnostics 2021, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Chiarelli, A.M.; Blackmore, K.M.; Muradali, D.; Done, S.J.; Majpruz, V.; Weerasinghe, A.; Mirea, L.; Eisen, A.; Rabeneck, L.; Warner, E. Performance Measures of Magnetic Resonance Imaging Plus Mammography in the High Risk Ontario Breast Screening Program. J. Natl. Cancer Inst. 2020, 112, 136–144. [Google Scholar] [CrossRef]
- Saeidi, T.; Mahmood, S.N.; Saleh, S.; Timmons, N.; Al-Gburi, A.J.A.; Razzaz, F. Ultra-Wideband (UWB) Antennas for Breast Cancer Detection with Microwave Imaging: A Review. Results Eng. 2025, 25, 104167. [Google Scholar] [CrossRef]
- Crișan, G.; Moldovean-Cioroianu, N.S.; Timaru, D.G.; Andrieș, G.; Căinap, C.; Chiș, V. Radiopharmaceuticals for PET and SPECT imaging: A literature review over the last decade. Int. J. Mol. Sci. 2022, 23, 5023. [Google Scholar] [CrossRef]
- Bhargava, D.; Rattanadecho, P.; Jiamjiroch, K. Microwave imaging for breast cancer detection-a comprehensive review. Eng. Sci. 2024, 30, 1116. [Google Scholar] [CrossRef]
- He, Z.; Chen, Z.; Tan, M.; Elingarami, S.; Liu, Y.; Li, T. A review on methods for diagnosis of breast cancer cells and tissues. Cell Prolif. 2020, 53, e12822. [Google Scholar] [CrossRef]
- Kirtania, S.G.; Elger, A.W.; Hasan, M.R.; Wisniewska, A.; Sekhar, K.; Karacolak, T.; Sekhar, P.K. Flexible Antennas: A Review. Micromachines 2020, 11, 847. [Google Scholar] [CrossRef]
- Singh, G.; Kaur, J. Skin and Brain Implantable Inset-Fed Antenna at ISM Band for Wireless Biotelemetry Applications. Microwave. Microw. Opt. Technol. Lett. 2020, 63, 510–515. [Google Scholar]
- Mahmood, S.N.; Ishak, A.J.; Saeidi, T.; Soh, A.C.; Jalal, A.; Imran, M.A.; Abbasi, Q.H. Full Ground Ultra-Wideband Wearable Textile Antenna for Breast Cancer and Wireless Body Area Network Applications. Micromachines 2021, 12, 322. [Google Scholar] [CrossRef]
- Arezoomandan, M.; Mohanna, S.; Bakhtiari Shahri, A. Compact Ultra-Wideband Arch Shaped Wide-Slot Antenna with High fidelity Factor and Bandwidth Enhancement for Microwave Imaging of Breast Cancer. Int. J. Ind. Electron. Control Optim. 2025, 205–215. Available online: https://ieco.usb.ac.ir/article_9146.html (accessed on 1 April 2025).
- Lalitha, K.; Manjula, J. Non-invasive microwave head imaging to detect tumors and to estimate their size and location. Phys. Med. 2022, 13, 100047. [Google Scholar] [CrossRef]
- Wang, L.; Peng, H.; Ma, J. Microwave breast imaging techniques and measurement systems. In New Perspectives in Breast Imaging; IntechOpen Limited: London, UK, 2017; p. 73. [Google Scholar]
- Alwan, M.; Sadek, S.; Katbay, Z. Investigation of tumor using an antenna scanning system. In Proceedings of the 2014 Mediterranean Microwave Symposium (MMS2014), Marrakech, Morocco, 12–14 December 2014; pp. 1–4. [Google Scholar]
- Lazebnik, M.; Watkins, C.B.; Hagness, S.C.; Booske, J.H.; Popovic, D.; McCartney, L.; Ogilvie, T. The dielectric properties of normal and malignant breast tissue at microwave frequencies: Analysis, conclusions, and implications from the Wisconsin/Calgary study. In Proceedings of the 2007 IEEE Antennas and Propagation Society International Symposium, Honolulu, HI, USA, 9–15 June 2007; pp. 2172–2175. [Google Scholar]
- Akram, M.; Iqbal, M.; Daniyal, M.; Khan, A.U. Awareness and current knowledge of breast cancer. Biol. Res. 2017, 50, 33. [Google Scholar] [CrossRef] [PubMed]
- Guliato, D.; Rangayyan, R.M.; Carvalho, J.D.; Santiago, S. Polygonal modeling of contours of breast tumors with the preservation of spicules. IEEE Trans. Biomed. Eng. 2008, 55, 14–20. [Google Scholar] [CrossRef]
- Naghibi, A.; Attari, A.R. Near-field radar-based microwave imaging for breast cancer detection: A study on resolution and image quality. IEEE Trans. Antennas Propag. 2020, 69, 1670–1680. [Google Scholar] [CrossRef]
- Liang, H.; Xing, L.; Lin, J. Application and algorithm of ground-penetrating radar for plant root detection: A review. Sensors 2020, 20, 2836. [Google Scholar] [CrossRef]
- Mohammed, B.J.; Abbosh, A.M.; Mustafa, S.; Ireland, D. Microwave system for head imaging. IEEE Trans. Instrum. Meas. 2013, 63, 117–123. [Google Scholar] [CrossRef]
- Nizam-Uddin, N.; Abdulkawi, W.M.; Elshafiey, I.; Sheta, A.F.A. Towards an efficient system for hyperthermia treatment of breast tumors. Biomed. Signal Process. Control 2022, 71, 103084. [Google Scholar] [CrossRef]
- Gas, P.; Miaskowski, A.; Subramanian, M. In silico study on tumor-size-dependent thermal profiles inside an anthropomorphic female breast phantom subjected to multi-dipole antenna array. Int. J. Mol. Sci. 2020, 21, 8597. [Google Scholar] [CrossRef]
- Miaskowski, A.; Gas, P. Numerical estimation of SAR and temperature distributions inside differently shaped female breast tumors during radio-frequency ablation. Materials 2022, 16, 223. [Google Scholar] [CrossRef]
- Álvarez Sánchez-Bayuela, D.; Ghavami, N.; Romero Castellano, C.; Bigotti, A.; Badia, M.; Papini, L.; Raspa, G.; Palomba, G.; Ghavami, M.; Loretoni, R.; et al. A multicentric, single arm, prospective, stratified clinical investigation to confirm MammoWave’s ability in breast lesions detection. Diagnostics 2023, 13, 2100. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Dhayal, M.; Dwivedi, S. Breast cancer detection by terahertz UWB microstrip patch antenna loaded with 6x6 SRR array. IETE J. Res. 2024, 70, 5295–5310. [Google Scholar] [CrossRef]
- Moll, J.; Slanina, T.; Stindl, J.; Maetz, T.; Nguyen, D.H.; Krozer, V. Temperature-induced contrast enhancement for radar-based breast tumor detection at k-band using tissue mimicking phantoms. IEEE J. Electromagn. R F Microw. Med. Biol. 2023, 7, 251–257. [Google Scholar] [CrossRef]
- Asok, A.O.; Shukoor, M.A.; Dey, S. Breast cancer detection with metamerial enabled monopole antennas using microwave imaging. In Proceedings of the 2022 IEEE International Conference on Emerging Electronics (ICEE), Bangalore, India, 11–14 December 2022; pp. 1–4. [Google Scholar]
- Bhaij, A.; Haddad, A.; Jouali, R.; Sabri, K.; Aoutoul, M. Design and optimization of a vivaldi antenna for early cancer detection: Sar and current density analysis. Int. J. Tech. Phys. Probl. Eng. 2024, 16, 85–92. [Google Scholar]
- Lazaro, A.; Villarino, R.; Girbau, D. Design of tapered slot Vivaldi antenna for UWB breast cancer detection. Microw. Opt. Technol. Lett. 2011, 53, 639–643. [Google Scholar] [CrossRef]
- Abbak, M.; Çayören, M.; Akduman, İ. Microwave breast phantom measurements with a cavity-backed Vivaldi antenna. IET Microw. Antennas Propag. 2014, 8, 1127–1133. [Google Scholar] [CrossRef]
- Salimi, M.; Gheitarani Sehrigh, S.; Rajebi, S. Design and analysis of Microstrip Patch Antenna for hyperthermia applications in breast cancer. Int. J. Tech. Phys. Probl. Eng. 2019, 41, 71–76. [Google Scholar]
- Rajput, J.L.; Nandgaonkar, A.B.; Nalbalwar, S.L.; Wagh, A.E.; Huilgol, N.G. Performance evaluation of compact rectangular microstrip antenna for breast hyperthermia. Int. J. Tech. Phys. Probl. Eng. 2021, 48, 87–94. [Google Scholar]
- Aldhaeebi, M.A.; Almoneef, T.S. Dipole array sensor for microwave breast cancer detection. IEEE Access 2023, 11, 91375–91384. [Google Scholar] [CrossRef]
- Hossain, A.; Pancrazio, S.; Kelley, T.; Pham, A.V. A Compact and Low-Profile High-Gain Multilayer Vivaldi Antenna Based on Gradient Metasurface Superstrates. IEEE Antennas Wirel. Propag. Lett. 2025, 1–5. [Google Scholar] [CrossRef]
- Harel, J.; Himdi, M.; Lafond, O.; Clauzier, O.; Vivares, O. A compact Vivaldi-shaped array using antipodal Vivaldi antennas to stabilize the high-frequency radiation pattern. IEEE Access 2025, 13, 29983–29993. [Google Scholar] [CrossRef]
- Islam, M.T.; Mahmud, M.Z.; Misran, N.; Takada, J.; Cho, M. Microwave breast phantom measurement system with compact side slotted directional antenna. IEEE Access 2017, 5, 5321–5330. [Google Scholar] [CrossRef]
- Natarajan, R.; George, J.V.; Kanagasabai, M.; Lawrance, L.; Moorthy, B. Modified antipodal Vivaldi antenna for ultra-wideband communications. IET Microw. Antennas Propag. 2016, 10, 401–405. [Google Scholar] [CrossRef]
- Islam, M.T.; Mahmud, M.Z.; Islam, M.T.; Kibria, S.; Samsuzzaman, M. A low cost and portable microwave imaging system for breast tumor detection using UWB directional antenna array. Sci. Rep. 2019, 9, 15491. [Google Scholar] [CrossRef]
- Katbay, Z.; Le, R.M.; Olleik, C.; Pérennec, A.; Sadek, S.; Lababidi, R. Bi-Static Time Domain Study for Microwave Breast Imaging. In Proceedings of the 2018 18th Mediterranean Microwave Symposium (MMS), Istanbul, Turkey, 31 October–2 November 2018; pp. 411–414. [Google Scholar]
- Samsuzzaman, M.; Islam, M.T.; Shovon, A.A.S.; Faruque, R.I. A 16-modified antipodal Vivaldi antenna array for microwave-based breast tumor imaging applications. Microw. Opt. Technol. Lett. 2019, 61, 2110–2118. [Google Scholar] [CrossRef]
- Özmen, H.; KURT, M.B. Radar-based microwave breast cancer detection system with a high-performanceultrawide band antipodal Vivaldi antenna. Turk. J. Electr. Eng. Comput. Sci. 2021, 29, 2326–2345. [Google Scholar] [CrossRef]
- Christydass, S.; Navaneethakrishnan, G.; Palanisamy, R.; Saleel, C.A.; Arputharaj, B.S. Split ring resonators and composite FR4 substrate for analysis and design of tri-band monopole antenna. Appl. Phys. Lett. 2024, 125, 183903. [Google Scholar] [CrossRef]
- Ali, S.Z.; Ahsan, K.; ul Khairi, D.; Alhalabi, W.; Anwar, M.S. Advancements in FR4 dielectric analysis: Free space approach and measurement validation. PLoS ONE 2024, 19, e0305614. [Google Scholar] [CrossRef]
- Kwe, N.B.; Yadav, V.; Kumar, M.; Savilov, S.V.; Yahya, M.Z.A.; Singh, S.K. A comparative study of dielectric substrate materials effects on the performance of microstrip patch antenna for 5G/6G application. J. Mater. Sci. Mater. Electron. 2024, 35, 1617. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, M.; Bai, Y.; Xu, H.; Fan, Y. Distance compensation-based dual adaptive artifact removal algorithm in microwave breast tumor imaging system. Biomed. Signal Process. Control 2024, 88, 105598. [Google Scholar] [CrossRef]
- Fear, E.; Li, X.; Hagness, S.; Stuchly, M. Confocal microwave imaging for breast cancer detection: Localization of tumors in three dimensions. IEEE Trans. Biomed. Eng. 2002, 49, 812–822. [Google Scholar] [CrossRef] [PubMed]
- Bond, E.J.; Li, X.; Hagness, S.C.; Van, V.B.D. Microwave imaging via spacetime beamforming for early detection of breast cancer. IEEE Trans. Antennas Propag. 2003, 51, 1690–1705. [Google Scholar] [CrossRef]
- Ranjitha, K.V.; Pushphavathi, T.P. Analysis on improved Gaussian-Wiener filtering technique and GLCM based feature extraction for breast cancer diagnosis. Procedia Comput. Sci. 2024, 235, 2857–2866. [Google Scholar] [CrossRef]
- Saini, R. Modified weiner filter for improving quality of MRI image for detection of diseases. Int. J. Adv. Res. Comput. Sci. 2017, 8, 64. [Google Scholar] [CrossRef]
- Chakraborty, R.; Bairagi, A.; Samui, P.; Das, S. Noise removal from digital mammogram. Eur. J. Pharm. Med. Res. 2019, 6, 312–319. [Google Scholar]
- Liu, G.; Xiao, X.; Song, H.; Lu, M.; Kikkawa, T. An adaptive window-based hybrid artifact removal method for ultra-wide band imaging enhancement of early breast cancer detection. Biomed. Signal Process. Control 2021, 70, 102980. [Google Scholar] [CrossRef]
- Ruvio, G.; Solimene, R.; Cuccaro, A.; Gaetano, D.; Browne, J.E.; Ammann, M.J. Breast cancer detection using interferometric MUSIC: Experimental and numerical assessment. Med. Phys. 2014, 41, 103101. [Google Scholar] [CrossRef]
- Felício, J.M.; Bioucas-Dias, J.M.; Costa, J.R.; Fernandes, C.A. Microwave Breast Imaging using a Dry Setup. IEEE Trans. Comput. Imaging 2020, 6, 167–180. [Google Scholar] [CrossRef]
- Elahi, M.A.; Shahzad, A.; Glavin, M.; Jones, E.; O’Halloran, M. Hybrid Artifact Removal for Confocal Microwave Breast Imaging. IEEE Antennas Wirel. Propag. Lett. 2014, 13, 149–152. [Google Scholar] [CrossRef]
- Pato, M.; Eleutério, R.; Conceição, R.C.; Godinho, D.M. Evaluating the performance of algorithms in axillary microwave imaging towards improved breast cancer staging. Sensors 2023, 23, 1496. [Google Scholar] [CrossRef]
- Reimer, T.; Solis-Nepote, M.; Pistorius, S. The Application of an Iterative Structure to the Delay-and-Sum and the Delay-Multiply-and-Sum Beamformers in Breast Microwave Imaging. Diagnostics 2020, 10, 411. [Google Scholar] [CrossRef] [PubMed]
- KaramFard, S.S.; Asl, B.M. Fast delay-multiply-and-sum beamformer: Application to confocal microwave imaging. IEEE Antennas Wirel. Propag. Lett. 2019, 19, 14–18. [Google Scholar] [CrossRef]
- Islam, M.T.; Samsuzzaman, M.; Kibria, S.; Islam, M.T. Experimental breast phantoms for estimation of breast tumor using microwave imaging systems. IEEE Access 2018, 6, 78587–78597. [Google Scholar] [CrossRef]
- Woodard, H.Q.; White, D.R. The composition of body tissues. Br. J. Radiol. 1986, 59, 1209–1218. [Google Scholar] [CrossRef]
- Lazebnik, M.; Madsen, E.; Frank, G.; Hagness, S. Tissue-mimicking phantom materials for narrowband and ultrawideband microwave applications. Phys. Med. Biol. 2005, 50, 4245–4258. [Google Scholar] [CrossRef]
- Zhang, H.; Arslan, T.; Flynn, B. A single antenna-based microwave system for breast cancer detection: Experimental results. In Proceedings of the 2013 Loughborough Antennas & Propagation Conference (LAPC), Loughborough, UK, 11–12 November 2013; pp. 477–481. [Google Scholar]
- Tiang, S.S.; Hathal, M.S.; Anwar, N.N.; Ain, M.F.; Abdullah, M.Z. Development of a Compact Wide-Slot Antenna for Early Stage Breast Cancer Detection Featuring Circular Array Full-View Geometry. Int. J. Antennas Propag. 2014, 2014, 309321. [Google Scholar] [CrossRef]
- Sasikala, S.; Karthika, K.; Arunkumar, S.; Anusha, K.; Adithya, S.; Al-Gburi, A.J.A. Design and analysis of a low-profile tapered slot UWB Vivaldi antenna for breast cancer diagnosis. Prog. Electromagn. Res. M 2024, 124, 43–51. [Google Scholar] [CrossRef]
- Qashlan, A.M.; Aldhaheri, R.W.; Alharbi, K.H. A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection. Appl. Sci. 2022, 12, 4908. [Google Scholar] [CrossRef]
- Slimi, M.; Jmai, B.; Dinis, H.; Gharsallah, A.; Mendes, P.M. Metamaterial vivaldi antenna array for breast cancer detection. Sensors 2022, 22, 3945. [Google Scholar] [CrossRef]
- Saleh, S.; Saeidi, T.; Timmons, N. Simple compact UWB Vivaldi antenna arrays for breast cancer detection. Telecom 2024, 5, 312–332. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, W.X.; Tang, S.J. Improved tapered slot-sine antennas loaded by grating. J. Electromagn. Waves Appl. 2009, 23, 1039–1048. [Google Scholar] [CrossRef]
- Lim, H.B.; Nhung, N.T.T.; Li, E.P.; Thang, N.D. Confocal microwave imaging for breast cancer detection: Delay-multiplyand-sum image reconstruction algorithm. IEEE Trans. Biomed. Eng. 2008, 55, 1697–1704. [Google Scholar] [PubMed]
- Zhou, B.; Li, H.; Zou, X.; Cui, T.J. Broadband and high-gain planar Vivaldi antennas based on inhomogeneous anisotropic zero-index metamaterials. Prog. Electromagn. Res. 2011, 120, 235–247. [Google Scholar] [CrossRef]
- Liu, Y.; Drew, M.G.; Li, H.; Liu, Y. A theoretical analysis of the relationships shown from the general experimental results of scattering parameters s 11 and s 21—Exemplified by the film of BaFe12−iCeiO19/polypyrene with i = 0.2, 0.4, 0.6. J. Microw. Power Electromagn. Energy 2021, 55, 197–218. [Google Scholar]
- Liu, Y.; Drew, M.G.; Li, H.; Liu, Y. An experimental and theoretical investigation into methods concerned with “reflection loss” for microwave absorbing materials. Mater. Chem. Phys. 2020, 243, 122624. [Google Scholar] [CrossRef]
- Sun, J.; Wang, L.; Yang, Q.; Shen, Y.; Zhang, X. Preparation of copper-cobalt-nickel ferrite/graphene oxide/polyaniline composite and its applications in microwave absorption coating. Prog. Org. Coat. 2020, 141, 105552. [Google Scholar] [CrossRef]
- Pandey, G.K.; Meshram, M.K. A printed high gain UWB vivaldi antenna design using tapered corrugation and gratingelements. Int. J. RF Microw. Comput.-Aided Eng. 2015, 25, 610–618. [Google Scholar] [CrossRef]
- Fei, P.; Jiao, Y.; Hu, W.; Zhang, F. A miniaturized antipodal Vivaldi antenna with improved radiation characteristics. IEEE Antennas Wirel. Propag. Lett. 2011, 10, 127–130. [Google Scholar]
- Pandey, G.; Verma, H.; Meshram, M. Compact antipodal Vivaldi antenna for UWB applications. Electron. Lett. 2015, 51, 308–310. [Google Scholar] [CrossRef]
- Chamaani, S.; Mirtaheri, S.A.; Abrishamian, M.S. Improvement of time and frequency domain performance of antipodal Vivaldi antenna using multi-objective particle swarm optimization. IEEE Trans. Antennas Propag. 2011, 59, 1738–1742. [Google Scholar] [CrossRef]
- Furat, A.; Pascal, F. A customized reduced size antipodal Vivaldi antenna used in wireless baseband transmission for short-range communication. AEU-Int. J. Electron. Commun. 2016, 70, 1684–1691. [Google Scholar]
- Tasnim, F.; Jannat, F.; Kibria, S.; Alam, M.S.; Ahsan, T.; Alam, T.; Islam, M.T. Electromagnetic performances analysis of a microwave imaging system (MIS) for breast tumor detection. In Proceedings of the 2018 International Conference on Innovations in Science, Engineering and Technology (ICISET), Chittagong, Bangladesh, 27–28 October 2018; pp. 442–446. [Google Scholar]
- Bidhendi, H.K.; Jafari, H.M.; Genov, R. Ultra-wideband imaging systems for breast cancer detection. In Ultra-Wideband and 60 GHz Communications for Biomedical Applications; Springer: Boston, MA, USA, 2014; pp. 83–103. [Google Scholar]
- Aydın, E.A.; Aydın, A.; Sarıbaş, G. Designs of three different octagonal-shaped antennas for microwave-based breast cancer detection. J. Instrum. 2023, 18, P09013. [Google Scholar] [CrossRef]
- Kaur, G.; Kaur, A. Breast tissue tumor detection using “S” parameter analysis with an UWB stacked aperture coupled microstrip patch antenna having a “+” shaped defected ground structure. Int. J. Microw. Wirel. Technol. 2020, 12, 635–651. [Google Scholar] [CrossRef]
- Klemm, M.; Craddock, I.J.; Leendertz, J.A.; Preece, A.; Benjamin, R. Radar-based breast cancer detection using a hemispherical antenna array—Experimental results. IEEE Trans. Antennas Propag. 2009, 57, 1692–1704. [Google Scholar] [CrossRef]
- Kaur, G.; Kaur, A. Monostatic radar-based microwave imaging of breast tumor detection using a compact cubical dielectric resonator antenna. Microw. Opt. Technol. Lett. 2021, 63, 196–204. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, H.; Lee, S. Image enhancement with Gaussian filtering in time-domain microwave imaging system for breast cancer detection. Electron. Lett. 2016, 52, 342–344. [Google Scholar] [CrossRef]
- Porter, E.; Fakhoury, J.; Oprisor, R.; Coates, M.; Popović, M. Improved tissue phantoms for experimental validation of microwave breast cancer detection. In Proceedings of the Fourth European Conference on Antennas and Propagation, Barcelona, Spain, 12–16 April 2010; pp. 1–5. [Google Scholar]
- Rahayu, Y.; Hilmi, M.F.; Masdar, H. A novel design rectangular UWB antenna array for microwave breast tumor detection. In Proceedings of the 2019 IEEE 16th International Conference on Quality in Research (QIR): International Symposium on Electrical and Computer Engineering, Padang, Indonesia, 22–24 July 2019; pp. 1–5. [Google Scholar]
- Slimi, M.; Jmai, B.; Mendes, P.; Gharsallah, A. Breast cancer detection based on CPW antenna. In Proceedings of the 2019 IEEE 19th Mediterranean Microwave Symposium (MMS), Hammamet, Tunisia, 31 October–2 November 2019; pp. 1–4. [Google Scholar]
- Junaid, K.M.; Sheela, J.J.J.; Logeshwaran, M. Design and Analysis of Novel Face Shaped Microstrip Array Antenna of UWB for Early Breast Tumor Detection. In Proceedings of the 2022 Sixth International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Dharan, Nepal, 10–12 November 2022; pp. 424–429. [Google Scholar]
- Amsaveni, A.; Kaiser, A.; Harish, L.; Rashmi, S. Double Layered Hexagonal Slot Antenna for Breast Cancer Detection using Microwave Imaging. In Proceedings of the 2023 2nd International Conference on Advancements in Electrical, Electronics, Communication, Computing and Automation (ICAECA), Coimbatore, India, 16–17 June 2023; pp. 1–5. [Google Scholar]
- Aziza, N.; Samad, F. Early Breast Cancer Detection with Microwave Imaging Technique by Using Spiral PIFA Antenna. In Proceedings of the 2021 5th International Conference on Electrical Information and Communication Technology (EICT), Khulna, Bangladesh, 17–19 December 2021; pp. 1–5. [Google Scholar]
- Jahan, I.; Kabir, A. Microstrip patch antenna for breast cancer detection. In Proceedings of the 2021 5th International Conference on Electrical Information and Communication Technology (EICT), Khulna, Bangladesh, 17–19 December 2021; pp. 1–6. [Google Scholar]
- Dey, G.K.; Nuzhat, T.; Das, K.P.; Ali, F. Microwave Imaging: CPW Fed Microstrip Patch Antenna with Defected Ground Plane Operating in ISM Band for Breast Tumor Detection. In Proceedings of the 2022 27th Asia Pacific Conference on Communications (APCC), Jeju Island, Republic of Korea, 19–21 October 2022; pp. 390–394. [Google Scholar]
- Chowdhury, N.A.; Wang, L.; Islam, M.S.; Gu, L.; Kaya, M. Microstrip patch antenna with an inverted T-type notch in the partial ground for breast cancer detections. Comput. Model. Eng. Sci. 2024, 138, 1301–1322. [Google Scholar] [CrossRef]
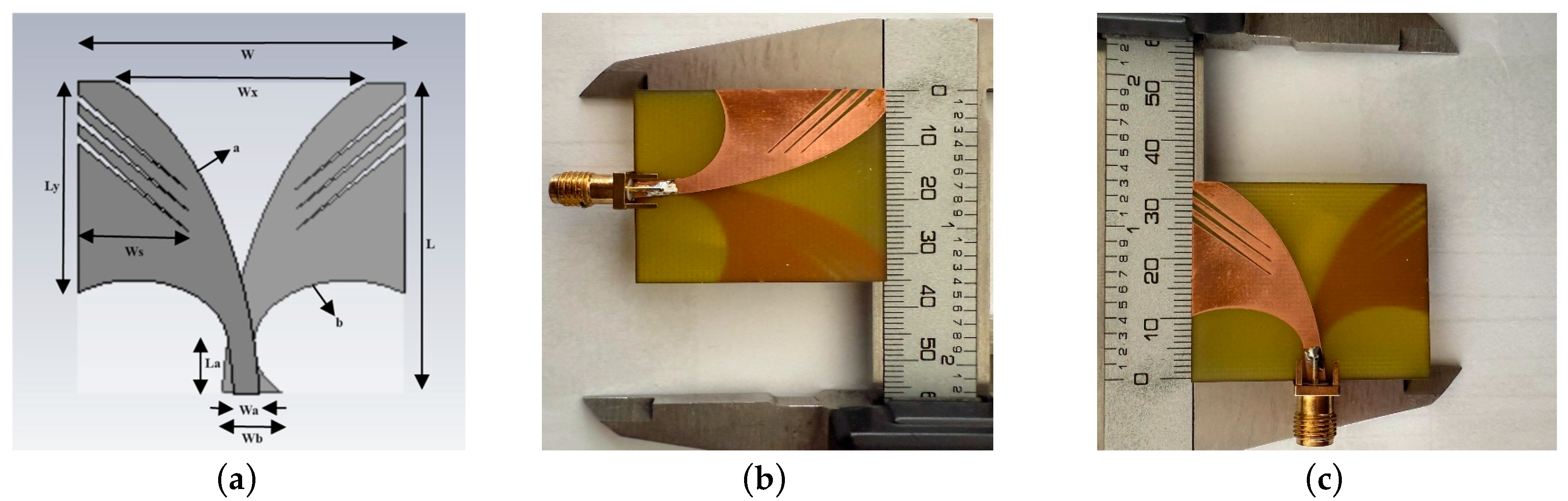





| Parameter | Vivaldi Antenna Value (mm) |
|---|---|
| W (Antenna width) | 34.6 |
| L (Antenna length) | 33 |
| Wx (Spacing width) | 26.6 |
| Ly (Flap length) | 22.4 |
| Ws (Slot width) | 11.7 |
| Wa (Port width) | 2.75 |
| Wb (Port width) | 6.25 |
| La (Port length) | 6 |
| a (Elliptical edge) | 0.085 |
| b (Circular diameter) | 11.25 |
| Ref. No. | Size (mm2) | Material | Bandwidth (GHz) | Gain (dB) | Directivity (dB) |
|---|---|---|---|---|---|
| [32] | 90 × 95 | Rogers RO3010 | 1–4 | - | - |
| [40] | 96.5 × 51.5 | FR-4 | 3.87–4.49 | 6.06 | 6.44 |
| [48] | 88 × 75 | RT/Duroid 5870 | 1.54–7 | 9.8 | - |
| [49] | 60 × 60 | FR-4 | 2.4–14 | 8.1 | - |
| [50] | 51 × 42 | RT/Duroid 5870 | 2.8–7 | 7.8 | - |
| [51] | 39.2 × 44 | RT/Duroid 6010 | 3.1–10.6 | - | - |
| [52] | 40 × 40 | FR-4 | 2.5–11 | 7.2 | 7.2 |
| [53] | 36 × 36 | FR-4 | 3.05–12.2 | 8.2 | 10.5 |
| [74] | 73.4 × 42 | FR-4 | 5–10 | 10 | - |
| [76] | 45 × 40 | FR-4 | 2.79–16.66 | 4.77 | 5.84 |
| [77] | 25 × 20 | Polyimide flexible | 4–9.4 | 2.33 | 4.06 |
| [78] | 67 × 46 | Rogers RO3010 | 1–8 | 5.8 | - |
| [79] | 88 × 44.75 | Rogers RO4003C | 2.42–11.52 | 8.14 | - |
| [80] | 84 × 48 | RT/Duroid 5870 | 5.3–9.6 | 12 | - |
| [85] | 40 × 45 | FR-4 | 2.9–12 | 8.2 | - |
| [86] | 48 × 60 | FR-4 | 2.4–14 | 10 | - |
| [87] | 56 × 50 | FR-4 | 2.0–12 | 5.2 | - |
| [88] | 96 × 86.2 | RF35 | 2.6–11 | 9 | - |
| [89] | 37 × 21 | FR-4 | 3.6–12 | 4.5 | - |
| [90] | 60.77 × 34.98 | FR-4 | 3.04–3.30 | 4 | 4.44 |
| Proposed | 34.6 × 33 | FR-4 | 3.6–13 | 9.27 | 11 |
| Tissue | Dielectric Property (εr) | Tangent Loss |
|---|---|---|
| Skin | 17.7 | 0.930 |
| Oil | 3.4 | 0.160 |
| Glandular | 16 | 0.940 |
| Tumor | 18 | 1.050 |
| Material | Fat | Gland | Skin | Tumor |
|---|---|---|---|---|
| p-toluic acid (g) | 0. 133 | 0.253 | 0.294 | 0.346 |
| n-propanol (mL) | 6.96 | 12.71 | 28.69 | 17.0 |
| Deionized water (mL) | 132.7 | 241.9 | 279.5 | 328.0 |
| 200 Bloom gelatin (g) | 24.32 | 43.27 | 50.02 | 58.67 |
| Formaldehyde (37% by weight) (g) | 1.53 | 2.74 | 3.33 | 3.72 |
| oil (mL) | 265.6 | 141.5 | 98.6 | 8.4 |
| Washing detergent (mL) | 12.00 | 6.79 | 5.86 | 2.0 |
| Ref. No. | Simulation Study (Tumor Diameter) | Breast Model | Experimental Study (Tumor Diameter) | Breast Model |
|---|---|---|---|---|
| [40] | 5 | Heterogeneous | - | - |
| [48] | 10 | Heterogeneous | 30 | Heterogeneous |
| [50] | - | - | 20 | Heterogeneous |
| [52] | 1.8 | Heterogeneous | - | - |
| [53] | 2 | Heterogeneous | 20 | Homogeneous |
| [73] | - | - | 25 | Heterogeneous |
| [75] | 6.5 | Heterogeneous | - | - |
| [76] | 5 | Heterogeneous | - | - |
| [77] | - | - | 25 | Homogeneous |
| [78] | 10 | Heterogeneous | - | - |
| [90] | 10 | Heterogeneous | - | - |
| [98] | 8 | Heterogeneous | - | - |
| [99] | 10 | Heterogeneous | - | - |
| [100] | 5 | Heterogeneous | - | - |
| [74] | 5 | Heterogeneous | 40 | Heterogeneous |
| [101] | 3 | Heterogeneous | - | - |
| [102] | 6 | Heterogeneous | - | - |
| [103] | 10 | Heterogeneous | - | - |
| [104] | 5 | Heterogeneous | - | - |
| [105] | 5 | Heterogeneous | - | - |
| Proposed | 0.9 | Heterogeneous | 16 | Heterogeneous and Homogeneous |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yıldız, Ş.; Kurt, M.B. Breast Cancer Detection Using a High-Performance Ultra-Wideband Vivaldi Antenna in a Radar-Based Microwave Breast Cancer Imaging Technique. Appl. Sci. 2025, 15, 6015. https://doi.org/10.3390/app15116015
Yıldız Ş, Kurt MB. Breast Cancer Detection Using a High-Performance Ultra-Wideband Vivaldi Antenna in a Radar-Based Microwave Breast Cancer Imaging Technique. Applied Sciences. 2025; 15(11):6015. https://doi.org/10.3390/app15116015
Chicago/Turabian StyleYıldız, Şahin, and Muhammed Bahaddin Kurt. 2025. "Breast Cancer Detection Using a High-Performance Ultra-Wideband Vivaldi Antenna in a Radar-Based Microwave Breast Cancer Imaging Technique" Applied Sciences 15, no. 11: 6015. https://doi.org/10.3390/app15116015
APA StyleYıldız, Ş., & Kurt, M. B. (2025). Breast Cancer Detection Using a High-Performance Ultra-Wideband Vivaldi Antenna in a Radar-Based Microwave Breast Cancer Imaging Technique. Applied Sciences, 15(11), 6015. https://doi.org/10.3390/app15116015






