Abstract
Background: Temporary anchorage devices (TADs) have reduced the need for anterior segmental osteotomy (ASO) in Class I patients; however, ASO remains relevant in Class II patients. As previous studies were conducted before the usage of TADs, updated guidelines are required to determine the relationship between surgery and orthodontic treatment. We aimed to evaluate the hard tissue changes following ASO versus non-ASO (NASO) orthodontic treatment utilizing TADs with premolar extraction. Methods: This retrospective clinical study involved 67 patients diagnosed with skeletal Class II malocclusion. The patients were categorized into the ASO (n = 31) and NASO (n = 36) groups. Cephalometric analyses were conducted to compare initial and final records to assess the treatment effects. Results: Pre- and post-treatment changes in the ASO and NASO groups exhibited significant differences in ΔSNA, ΔSNB, ΔANB, ΔA to N-perp, ΔB to N-perp, ΔPog to N-perp, and ΔA to FH (p < 0.05). Both groups demonstrated normalized ANB, indicating significant skeletal improvement in Class II malocclusion. Specifically, the change in FMIA (ΔL1 to FH [°]) was 4.98° greater in the NASO group than in the ASO group (p < 0.05). Conclusions: Considering the IMPA change, NASO was recommended for treatment choice when a reduction of more than 10° was achievable.
1. Introduction
Bimaxillary protrusion is prevalent among individuals of African and Asian descent, prompting them to seek orthodontic treatment [1,2]. The introduction of orthodontic temporary anchorage devices (TADs) has broadened the scope of non-extraction tooth alignment by improving anchorage. However, these orthodontic treatment methods may have limitations in terms of enhancing facial esthetics due to risks of root resorption, excessive posterior inclination of the anterior teeth, and reduction in the alveolar bone in the palatal region [3].
Anterior segmental osteotomy (ASO) with premolar extraction was developed to effectively address these adverse effects while efficiently correcting protrusions [4]. However, despite its ability to overcome several limitations of orthodontic treatment, ASO may lead to various postoperative complications and impose economic and psychological burdens on patients. According to a comparative study conducted by Lee et al. [5] on ASO versus nonsurgical extraction orthodontics (NASO), the ASO group exhibited a lower Orthodontic Discrepancy Index than the NASO group did. Additionally, the ASO group showed posterior movement of the anterior maxilla [sella–nasion–point A (SNA), point A to nasion (N)-perpendicular] and a more significant reduction in the point A–nasion–point B (ANB) angle. Regarding the dentition, previous research has indicated that the changes in the angle of the maxillary anterior teeth were less pronounced in the ASO group compared to those in the NASO group [5]. Moreover, Hwang et al. [6] reported significant differences in incisal angle changes between the ASO and NASO groups, with values of 7.18° and 11.93°, respectively. Furthermore, a recent comparative study by Yong et al. [7] demonstrated that patients who underwent ASO were more likely to achieve an interincisal angle of 135 ± 5° after treatment compared to those who underwent NASO, and long-term follow-up of patients who underwent ASO revealed that adverse effects were rare. However, so far, no studies have comprehensively compared the treatment outcomes between Class II ASO and NASO employing TADs. While previous studies have compared these modalities, most have focused only on ASO cases or lacked consistent adjunctive anchorage protocols. This study was distinguished by its focus on skeletal Class II patients treated with ASO or NASO while incorporating TADs in the NASO. In addition, a subgroup analysis was performed for patients with comparable baseline ANB values, allowing for a more refined comparison of treatment effects under similar skeletal conditions in borderline cases.
Therefore, this study aimed to analyze and compare the skeletal and dental changes resulting from ASO with those of treatment with TADs in NASO. The clinical significance of this research was hypothesized to lie in its potential to assist in determining the most effective treatment outcome based on the patient’s initial characteristics and concerns, thereby aiding in the formulation of an appropriate treatment plan.
In this study, particular attention was given to the incisor mandibular plane angle (IMPA) due to its diagnostic and therapeutic significance in cases of bimaxillary protrusion, considering treatment stability or esthetic outcomes [8]. When the posterior movement of the lower incisors can be achieved by changing the IMPA—primarily through crown retraction—NASO may be sufficient to obtain the desired outcome. However, when the bodily movement of the entire tooth, including root apex retraction, is required, ASO becomes essential. Therefore, IMPA may serve as a key decision-making parameter in evaluating the appropriateness and limits of each treatment modality in this cohort.
2. Materials and Methods
2.1. Study Sample
The study sample size was determined using G*Power (version 3.1; Heinrich-Heine University, Düsseldorf, Germany). Briefly, sample size calculation entailed two independent sample t-tests, assuming a two-tailed distribution, an effect size of 0.5 (indicating a medium effect), a significance level of 0.05, and a power of 0.8. The calculation indicated that a minimum of 63 patients would be necessary for a comparative analysis between the ASO and NASO groups. This retrospective study was conducted between 1 September 2016 and 1 September 2021. Among 562 patients diagnosed with skeletal Class II malocclusion, 67 (ASO: 31, NASO: 36) aged 19–40 years, who visited the Department of Orthodontics at Ajou University Dental Hospital, were selected based on the study’s inclusion and exclusion criteria. Pre- and post-treatment lateral cephalometric radiographs were obtained and analyzed. Notably, patients with an ANB greater than 7.33° were excluded to avoid including cases that would require orthognathic surgery or more complex interventions, as suggested in a recent study by Lee et al. [9], where patients with ANB ≥ 7.33° showed unsuccessful skeletal normalization after ASO. The decision to undergo anterior segmental osteotomy (ASO) or non-surgical orthodontic camouflage treatment (NASO) was made based on thorough consultation. Patients were provided with comprehensive explanations regarding the risks, benefits, and costs of both treatment options. The final group allocation was determined according to the patients’ informed preferences after understanding all relevant information.
The inclusion criteria were as follows:
A diagnosis of skeletal class II malocclusion (3° < ANB < 7.33°);
Adults aged ≥ 18 years;
Patients who underwent orthodontic treatment;
Those who underwent extraction of the premolars;
Those seeking treatment for lip protrusion.
The exclusion criteria encompassed:
Patients with congenital dental anomalies;
Those with congenital conditions such as craniosynostosis and cleft palate;
Those with systemic diseases affecting bone metabolism;
Those with severe facial asymmetry (chin displacement < 4 mm relative to the facial midline);
Those who discontinued orthodontic treatment;
Cases in which posterior TADs were used for further anterior teeth and lip retraction after ASO.
This study received approval from and adhered to the guidelines of the Institutional Review Board of Ajou University. The IRB Committee waived the requirement for obtaining patient consent from both institutions. The demographic data are described in Table 1.

Table 1.
Baseline characteristics of the study participants.
2.2. Variables
Cephalometric Measurement (Table 2)
Lateral cephalometric radiographs were obtained with the patients positioned in their natural head posture, with instructions to keep their lips closed to ensure accurate assessments of lip incompetence per Burstone’s guidelines [10]. Cephalometric measurements and analyses were performed by a single examiner (PR Hong) using the V-ceph 8.4 software (Osstem, Seoul, Republic of Korea). To assess measurement precision, cephalometric analyses of ten randomly selected patients were repeated at 4-week intervals. The reproducibility of these measurements was confirmed by calculating the intraclass correlation coefficient, which exceeded 0.9, indicating a high level of measurement reliability.

Table 2.
Skeletal and dental measurements to compare ASO with NASO group.
Table 2.
Skeletal and dental measurements to compare ASO with NASO group.
| Explanation | |
|---|---|
| Skeletal Measurements | |
| SNA (°) | Angle of nasion–sella to nasion–A point |
| SNB (°) | Angle of nasion–sella to nasion–B point |
| ANB (°) | Angle of A point–nasion to nasion–B point |
| FMA (°) | Angle of Frankfort horizontal plane (FH) and the mandibular plane |
| SN–GoMe (°) | Angle of sella–nasion to gonion–menton |
| A to N-perp (mm) | Distance between A point and N-perpendicular |
| B to N-perp (mm) | Distance between B point and N-perpendicular |
| Pog to N-perp (mm) | Distance between Pogonion point and N-perpendicular |
| A to FH (mm) | Distance between A point and FH plane |
| B to FH (mm) | Distance between B point and FH plane |
| FABA (°) | Angle of Frankfort horizontal plane (FH) to AB plane |
| Dental measurements | |
| U1 to FH (°) | Angle of FH to U1 axis |
| U1 to FH (mm) | Distances between U1 tip and FH |
| L1 to FH (°) | Angle of FH to L1 axis |
| L1 to FH (mm) | Distance between L1 tip and FH |
| U1 C_N-perp (mm) | Distance between U1 tip and N-perpendicular |
| U1 R_N-perp (mm) | Distance between U1 apex and N-perpendicular |
| L1 C_N-perp (mm) | Distance between L1 tip and N-perpendicular |
| L1 R_N-perp (mm) | Distance between L1 apex and N-perpendicular |
| FOP (Functional occlusal plane) | Angle of FH to line joins the midpoint of U6 and L6 with the midpoint of upper and lower premolars |
| BOP (Bisected occlusal plane) | Angle of FH to line that bisects the vertical distance between the upper and lower incisal tips (U1 tip, L1 tip) and the upper and lower first molar occlusal surface (U6 occlusal, L6 occlusal) |
| Interincisal angle (°) | Angle of U1 axis to L1 axis |
Twenty-two specific measurements were made to assess the cephalometric changes before and after treatment. These measurements were analyzed on the X-axis, defined by the Frankfort horizontal (FH) line, and on the Y-axis, determined by the line perpendicular to point N (N-perpendicular line), enabling both vertical and horizontal comparisons (Figure 1 and Figure 2). In this study, the FH to N-perpendicular coordinate system was adopted based on the McNamara analysis [11]. While it is known that the SN plane with a −7° adjustment is also commonly used as an alternative reference to better simulate the natural head position, this concern was examined by measuring the angular difference between the FH and SN planes in our dataset. The analysis revealed a mean difference of 6.47° with a standard deviation of 2.85°, which is close to the commonly accepted 7° approximation. The relatively small standard deviation suggests that the FH plane deviation in our sample was minimal and consistent, thus supporting the validity of using the FH plane as a horizontal reference line in this study.
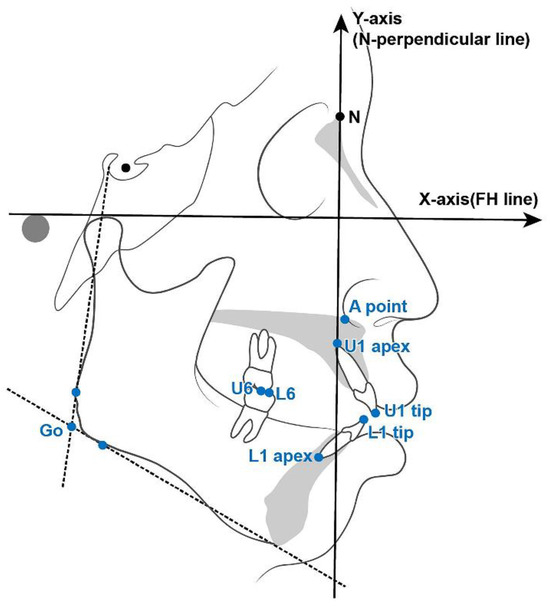
Figure 1.
Key landmarks and reference lines utilized in cephalometric analysis. Axes of coordinates are represented, with the Frankfort horizontal (FH) line defining the X-axis and the nasion–perpendicular line (N-perp) defining the Y-axis.
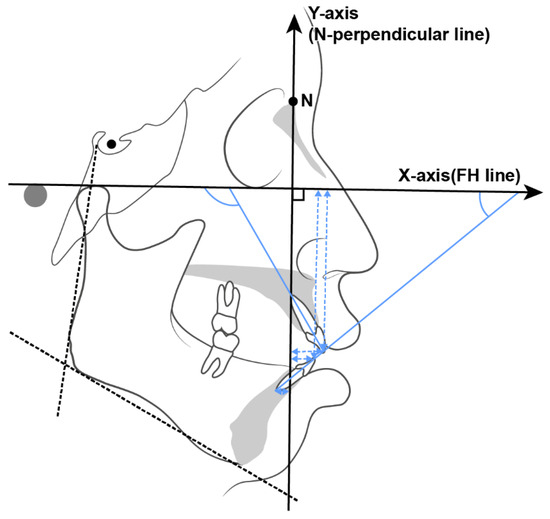
Figure 2.
Reference lines used in cephalometric analysis and dental measurements.
ASO procedures were exclusively performed by a single surgeon (YJ Choi), while all orthodontic treatments were administered by a single American Board of Orthodontics-certified orthodontist (HS Chae) using a 022-slot bracket system with MBT prescription.
2.3. Data Collection Techniques
2.3.1. Surgical Procedures
ASO and/or genioplasty were performed under general anesthesia. The first premolars were extracted during surgery to facilitate posterior translation of the anterior segment. Owing to the superior vascular supply of the mandible compared with the maxilla, mandibular osteotomy was prioritized to minimize the ischemic duration for the maxillary region. Briefly, osteotomy was performed using a 4 mm diameter round burr and a reciprocating saw. For the mandible, an incision was made below the mucogingival junction, extending from canine to canine, to protect the bilateral mental nerves. In the maxilla, a minor Le Fort I incision spanning the right and left canines was made on the labial side. The palatal incision involved a central stab incision coupled with a crevicular incision extending from the canine to the second premolar. These maxillary incisions were specifically designed to preserve blood supply to the palatal area. After repositioning the maxillary and mandibular segments to their intended locations, they were secured using miniplates and screws. Additionally, genioplasty guided by intraoperative evaluation was performed.
2.3.2. TAD Placement Procedures
TADs were employed to reinforce anchorage and were typically placed in the interradicular region between the first and second premolars. The TADs used in the maxilla measured 1.6 mm in diameter and 8 mm in length, while those in the mandible were 6 mm in length. Placement was performed at the mucogingival junction under topical anesthesia. In cases of failure or inadequate primary stability, alternative sites such as the palatal slope or retromolar area were selected. Immediate loading was applied using elastomeric chains, delivering a consistent retraction force of approximately 150–200 g per side.
2.4. Data Analyses
All statistical analyses were conducted using the SPSS software (IBM, Armonk, New York, NY, USA, version 29.0). A Shapiro–Wilk test was employed to assess the normality of data distribution for both pre- and post-treatment measurements. An independent t-test was utilized to compare measurements obtained before treatment, changes observed between pre- and post-treatment, and measurements recorded after treatment between the ASO and NASO groups.
3. Results
3.1. Pretreatment Comparison Between the ASO and NASO Groups (Table 3)
3.1.1. Skeletal Differences Before Treatment
Significant differences were observed before treatment between the ASO and NASO groups in the following measurements: SNA, ANB, B-to-N-perpendicular, B-to-FH, and angle formed by the FH plane and the line joining points A and B (AB) (FABA) (p < 0.05). Notably, the ASO group showed a higher tendency toward skeletal Class II malocclusion compared with the NASO group, and the SNA was 2.31° higher in the ASO group than in the NASO group, indicating greater maxillary protrusion. However, no significant difference was noted between the two groups in the absolute evaluation of the anteroposterior position of the maxilla measured using A to N-perpendicular.

Table 3.
Comparison of skeletal and dental measurements between the ASO and NASO groups before treatment.
Table 3.
Comparison of skeletal and dental measurements between the ASO and NASO groups before treatment.
| ASO Group | Non-ASO Group | |||||
|---|---|---|---|---|---|---|
| Measurements | Mean | SD | Mean | SD | Difference | p |
| SNA | 82.17 | 4.16 | 79.85 | 3.07 | 2.31 | 0.01 ** |
| SNB | 76.69 | 4.01 | 76.08 | 3.12 | 0.60 | 0.49 |
| ANB | 5.48 | 1.13 | 3.77 | 1.41 | 1.71 | 0.00 ** |
| FMA | 29.51 | 6.03 | 29.22 | 4.46 | 0.29 | 0.82 |
| SN-GoMe | 38.13 | 6.47 | 39.47 | 4.84 | −1.34 | 0.35 |
| A to N-perp | 0.87 | 3.13 | 0.11 | 2.91 | 0.76 | 0.31 |
| A to FH | 35.77 | 3.35 | 34.65 | 4.22 | 1.11 | 0.24 |
| B to N-perp | −9.35 | 5.78 | −6.67 | 4.89 | −2.68 | 0.04 * |
| B to FH | 72.85 | 6.58 | 73.16 | 6.47 | 9.69 | 0.00 |
| Pog to N-perp | −10.41 | 6.80 | −8.84 | 5.94 | −1.56 | 0.32 |
| FABA | 77.79 | 3.64 | 80.13 | 3.80 | −2.33 | 0.01 * |
| U1 to FH (°) | 114.81 | 6.50 | 116.51 | 6.58 | −1.70 | 0.29 |
| U1 to FH (mm) | 63.50 | 4.17 | 57.50 | 5.87 | 6.00 | 0.00 ** |
| L1 to FH (°) | 45.68 | 4.84 | 51.83 | 7.23 | −6.15 | 0.00 ** |
| L1 to FH (mm) | 61.31 | 4.11 | 55.89 | 5.36 | 5.42 | 0.00 ** |
| U1 C to N-perp | 8.52 | 4.95 | 6.24 | 4.24 | 2.28 | 0.046 * |
| U1 R to N-perp | −2.99 | 3.99 | −4.19 | 2.93 | 1.20 | 0.16 |
| L1 C to N-perp | 5.16 | 4.89 | 2.87 | 4.17 | 2.29 | 0.04 * |
| L1 R to N-perp | −10.77 | 5.81 | −9.49 | 4.31 | −1.27 | 0.31 |
| Interincisal angle | 110.87 | 7.70 | 115.32 | 10.70 | −4.45 | 0.053 |
| BOP | 11.19 | 3.04 | 10.30 | 3.58 | 0.89 | 0.28 |
| FOP | 11.74 | 3.50 | 11.43 | 4.07 | 0.31 | 0.74 |
| IMPA | 104.81 | 6.95 | 98.94 | 7.46 | 5.87 | 0.00 ** |
Independent t-tests were performed to compare variables between the two groups before treatment. * p < 0.05, ** p < 0.01. IMPA, incisor mandibular plane angle; ASO, anterior segmental osteotomy; SD, standard deviation; FH, Frankfort Horizontal.
3.1.2. Dental Differences Before Treatment
Significant differences were also present before treatment between the ASO and NASO groups in measurements such as upper central incisor (U1) to FH (mm), lower central incisor (L1) to FH (°), L1 to FH (mm), U1 C to N-perpendicular, L1 C to N-perpendicular, and incisor–mandibular plane angle (IMPA) (p < 0.05). While no significant differences were evident in U1 to FH (°) between the two groups, the ASO group exhibited a significantly larger IMPA (5.87°) than the NASO group. Additionally, the horizontal positions of the upper and lower incisors (U1 C to N-perpendicular, L1 C to N-perpendicular) were significantly different between the ASO group versus the NASO group, being positioned 2.28 mm and 2.29 mm more forward, respectively.
3.2. Post-Treatment Comparison Between the ASO and NASO Groups (Table 4)
3.2.1. Post-Treatment Skeletal Differences
Following treatment, significant skeletal differences were observed between the ASO and NASO groups in measurements such as A to N-perpendicular, B to N-perpendicular, B to FH, and pogonion (Pog) to N-perpendicular (p < 0.05). Specifically, point A in the ASO group was positioned 3.13 mm further back than that in the NASO group after treatment (A to N-perpendicular). Similarly, point B in the ASO group was positioned 6.06 mm posterior to that in the NASO group after treatment (B to N-perpendicular). Additionally, Pog to N-perpendicular in the ASO group was positioned 2.97 mm further back than that in the NASO group after treatment. However, significant differences were not evident in the SNA, sella–nasion–point B (SNB), and ANB post-treatment. The respective ANB values of 3.22 and 3.28 in the ASO and NASO groups implied that the proportions between the maxilla and mandible in the sagittal dimension was normalized in each group.

Table 4.
Comparison of skeletal and dental measurements between the ASO and NASO groups after treatment.
Table 4.
Comparison of skeletal and dental measurements between the ASO and NASO groups after treatment.
| ASO Group | Non-ASO Group | |||||
|---|---|---|---|---|---|---|
| Measurements | Mean | SD | Mean | SD | Difference | p |
| SNA | 78.04 | 4.14 | 79.15 | 3.32 | −1.11 | 0.23 |
| SNB | 74.82 | 3.92 | 75.88 | 2.98 | −1.05 | 0.22 |
| ANB | 3.22 | 1.22 | 3.28 | 1.37 | −0.06 | 0.85 |
| FMA | 28.79 | 3.84 | 28.46 | 4.42 | 0.33 | 0.75 |
| SN-GoMe | 37.33 | 4.65 | 38.67 | 4.95 | −1.34 | 0.26 |
| A to N-perp | −3.86 | 2.76 | −0.72 | 2.78 | −3.13 | 0.00 ** |
| A to FH | 34.22 | 3.47 | 35.30 | 4.16 | −1.09 | 0.13 |
| B to N-perp | −13.10 | 5.29 | −7.05 | 4.36 | −6.06 | 0.00 ** |
| B to FH | 82.57 | 5.94 | 72.98 | 6.80 | 9.59 | 0.00 ** |
| Pog to N-perp | −11.13 | 5.80 | −8.16 | 5.52 | −2.97 | 0.04 * |
| FABA | 79.15 | 3.67 | 80.50 | 3.60 | −1.34 | 0.14 |
| U1 to FH (°) | 110.31 | 6.06 | 110.00 | 7.53 | 0.31 | 0.86 |
| U1 to FH (mm) | 62.90 | 4.42 | 57.26 | 5.60 | 5.65 | 0.00 ** |
| L1 to FH (°) | 51.86 | 6.34 | 62.99 | 7.97 | −11.13 | 0.00 ** |
| L1 to FH (mm) | 60.23 | 4.34 | 55.08 | 5.67 | 5.14 | 0.00 ** |
| U1 C to N-perp | 1.95 | 4.66 | 2.13 | 3.86 | −0.18 | 0.86 |
| U1 R to N-perp | −7.58 | 3.81 | −5.64 | 3.00 | −1.93 | 0.02 * |
| L1 C to N-perp | −1.16 | 4.75 | −1.00 | 3.75 | −0.16 | 0.88 |
| L1 R to N-perp | −15.23 | 5.36 | −9.71 | 4.27 | −5.52 | 0.00 ** |
| Interincisal angle | 121.56 | 9.49 | 132.99 | 11.88 | −11.44 | 0.00 ** |
| BOP | 12.17 | 3.69 | 10.88 | 4.09 | 1.29 | 0.18 |
| FOP | 12.29 | 3.87 | 10.68 | 4.67 | 1.61 | 0.13 |
| IMPA | 99.34 | 7.39 | 88.54 | 7.54 | 10.80 | 0.00 ** |
Independent t-tests were performed to compare variables between the two groups after treatment * p < 0.05, ** p < 0.01. IMPA, incisor mandibular plane angle; ASO, anterior segmental osteotomy; SD, standard deviation; FH, Frankfort horizontal.
3.2.2. Dental Differences Post-Treatment
After treatment, significant dental differences were noted between the ASO and NASO groups in measurements such as U1 to FH (mm), L1 to FH (°), L1 to FH (mm), U1 R to N-perpendicular, L1 R to N-perpendicular, interincisal angle, and IMPA (p < 0.05). After treatment, U1 R to N-perpendicular and L1 R to N-perpendicular in the ASO group were positioned 1.93 mm and 5.52 mm further back, respectively, compared to those in the NASO group. The interincisal angle was 11.44° smaller in the ASO group than in the NASO group after treatment. Furthermore, the IMPA was 10.80° greater in the ASO group than in the NASO group after treatment.
3.3. Comparison of Pre- and Post-Treatment Changes in the ASO and NASO Groups (Table 5)
To account for the differences between the initial conditions of the ASO and NASO groups, the pre- and post-treatment changes within each group were examined. This analysis facilitated evaluation of the skeletal and dental effects based on the treatment method.

Table 5.
Comparison of pre- and post-treatment changes between the ASO and NASO groups.
Table 5.
Comparison of pre- and post-treatment changes between the ASO and NASO groups.
| (T1–T0) | (Δ ASO Group–Δ NASO Group) | ||||
|---|---|---|---|---|---|
| Measurements | ΔASO Mean | Δ NASO Mean | Mean Difference | SD Difference | p |
| SNA diff | −4.13 | −0.70 | −3.43 | 0.34 | 0.00 ** |
| SNB diff | −1.87 | −0.21 | −1.66 | 0.23 | 0.00 ** |
| ANB diff | −2.26 | −0.49 | −1.77 | 0.35 | 0.00 ** |
| FMA diff | −0.72 | −0.76 | 0.04 | 0.94 | 0.48 |
| SN-GoMe diff | −0.80 | −0.80 | 0.00 | 0.91 | 0.50 |
| A to N-perp diff | −4.73 | −0.84 | −3.89 | 0.48 | 0.00 ** |
| A to FH diff | −1.55 | 0.65 | −2.20 | 0.46 | 0.00 ** |
| B to N-perp diff | −3.76 | −0.38 | −3.38 | 0.62 | 0.00 ** |
| B to FH diff | −0.29 | −0.18 | −0.11 | 0.64 | 0.43 |
| Pog to N-perp diff | −0.73 | 0.68 | −1.41 | 0.83 | 0.048 * |
| FABA diff | 1.36 | 0.37 | 0.99 | 0.66 | 0.07 |
| U1 to FH (°) diff | −4.50 | −6.51 | 2.01 | 1.49 | 0.09 * |
| U1 to FH (mm) diff | −0.60 | −0.24 | −0.36 | 0.56 | 0.27 |
| L1 to FH (°) diff | 6.18 | 11.16 | −4.98 | 1.83 | 0.00 ** |
| L1 to FH (mm) diff | −1.08 | −0.81 | −0.27 | 0.55 | 0.31 |
| U1 C to N-perp diff | −6.57 | −4.11 | −2.46 | 0.79 | 0.00 ** |
| U1 R to N-perp diff | −4.58 | −1.45 | −3.14 | 0.53 | 0.00 ** |
| L1 C to N-perp diff | −6.31 | −3.87 | −2.44 | 0.75 | 0.00 ** |
| L1 R to N-perp diff | −4.47 | −0.22 | −4.25 | 0.60 | 0.00 ** |
| Interincisal angle diff | 10.69 | 17.67 | −6.98 | 2.71 | 0.01 ** |
| BOP diff | 0.98 | 0.58 | 0.40 | 0.58 | 0.25 |
| FOP diff | 0.54 | −0.76 | 1.30 | 0.82 | 0.06 |
| U1 movement diff | 6.76 | 5.80 | 0.97 | 0.62 | 0.06 |
| L1 movement diff | 6.59 | 5.55 | 1.04 | 0.60 | 0.04 * |
| IMPA diff | −5.46 | −10.40 | 4.93 | 2.12 | 0.01 * |
Independent t-tests were performed to compare variables between Δ ASO and Δ MI non-surgery. * p < 0.05, ** p < 0.01. IMPA, incisor mandibular plane angle; ASO, anterior segmental osteotomy; SD, standard deviation; MI.
3.3.1. Skeletal Changes Pre- and Post-Treatment
The pre- and post-treatment changes in the ASO and NASO groups revealed significant differences in ΔSNA, ΔSNB, ΔANB, ΔA to N-perpendicular, ΔB to N-perpendicular, ΔPog to N-perpendicular, and ΔA to FH (p < 0.05). While the reduction in ANB in the ASO group compared with that in the NASO group was clinically significant at 1.77, both groups exhibited normalized ANB values, indicating substantial skeletal improvement in Class II malocclusion. Similarly, significant differences were observed between the two groups in the sagittal changes in points A and B, as measured by ΔA to N-perpendicular and ΔB to N-perpendicular (p < 0.05). Point A moved 3.89 mm and point B moved 3.38 mm further back in the ASO group compared to the NASO group. Additionally, the difference in Pog to N-perp change between the ASO and NASO groups was −1.41 mm.
3.3.2. Dental Changes Pre- and Post-Treatment
The pre- and post-treatment changes in the ASO and NASO groups exhibited significant differences in ΔL1 to FH (°), ΔU1 C to N-perpendicular, ΔU1 R to N-perpendicular, ΔL1 C to N-perpendicular, ΔL1 R to N-perpendicular, Δinterincisal angle, ΔL1 movement, and ΔIMPA (p < 0.05). Specifically, the change in the Frankfort–mandibular incisor angle (FMIA) [ΔL1 to FH (°)] was 4.98° greater in the NASO group than in the ASO group (p < 0.05), and the change in the IMPA was 4.93° greater in the NASO group than in the ASO group (p < 0.05). Similarly, the change in U1 to FH (°) was 2.01° greater in the NASO group than in the ASO group, although the difference lacked statistical significance. Significant differences were evident between the two groups in the sagittal changes in the maxillary and mandibular incisors, as measured by ΔU1 C to N-perpendicular, ΔU1 R to N-perpendicular, ΔL1 C to N- perpendicular, and ΔL1 R to N-perpendicular (p < 0.01). In the ASO group, the crown of the maxillary incisors moved 2.46 mm, and the root moved 3.14 mm further back compared to the NASO group. Additionally, the crown of the mandibular incisors moved 2.44 mm, and the root moved 4.25 mm further back. The change in the interincisal angle was 6.98° less in the ASO group than in the NASO group.
3.3.3. Borderline Cases After Treatment Comparison (Supplementary Table S1)
To mitigate this confounding factor and ensure a fair comparison, we selected borderline cases with initial ANB values within the 3° < ANB < 4° range. This subset consisted of eight patients from the ASO group and nine from the NASO group. Among the 22 cephalometric variables analyzed, significant post-treatment differences were observed in the following: ANB, A to N-perpendicular, B to N-perpendicular, B to FH, L1 to FH (°), U1 to FH (mm), and L1 to FH (mm). A similar trend was observed when compared with the data in Table 4, which reports post-treatment data for the entire sample. The results suggested that the initial difference in ANB between the ASO and NASO groups within the current study range (Table 1) might not have had a substantial impact on the comparative outcomes in this study.
4. Discussion
Tweed [8] emphasized the importance of the position of mandibular incisors in determining esthetics after orthodontic treatment. However, despite being rooted in hard tissue analysis of the teeth and alveolar bone, Tweed’s diagnostic approach has been overshadowed by modern soft tissue-focused diagnostics [12,13]. The present study emphasizes the importance of mandibular incisor position and inclination in patients’ satisfaction with facial esthetics and occlusion after orthodontic correction of Class II malocclusion, particularly after ASO and NASO treatments resulting in ANB normalization. The study revealed that the ASO group exhibited significantly greater IMPA values than did the NASO group both before and after treatment. Additionally, mandibular incisor movement and IMPA changes were smaller in the ASO group than in the NASO group, suggesting that mandibular incisor inclination, camouflaged by severe skeletal disharmony pretreatment, persisted post-treatment, despite surgical intervention. However, unlike two-jaw surgeries, ASO preserves basal bone integrity, limiting the dentition’s camouflaging potential, as observed in this study. Table 3 demonstrates that the pretreatment FMIA values were 45.68° for the ASO group and 51.84° for the NASO group. After treatment, while the FMIA was 51.87° (Δ6.19°) in the ASO group, in the NASO group, it was 63° (Δ11.16°). This suggests that if mandibular incisor inclination falls within the range where normal FMIA values can be achieved through tooth movement and inclination adjustments with extraction orthodontics, NASO may yield esthetically pleasing and stable treatment outcomes, obviating the need for ASO. When comparing VTO/STO, achieving 5° more of incisor uprighting with orthodontic teeth movement may only suffice for nonsurgical treatment, given that the changes in FMIA were 4.98° greater in the NASO group than in the ASO group (p < 0.05); this serves as a clinical benchmark for deciding between ASO and NASO. Consequently, reevaluating the importance of the mandibular incisor inclination improvement in patients with Class II skeletal malocclusion while considering Tweed’s diagnostic method underscores the significance of both initial mandibular incisor inclination and achievable movement of the mandibular incisors.
In a comparative study by Baek and Kim [3], orthodontic treatment was found to be more effective than ASO, especially in cases where the maxillary teeth were inclined forward, the occlusal plane was less steep, the interlabial gap was large, and the lower nasolabial angle was acute. Conversely, Lee et al. [5] recommended ASO for cases with normal-range maxillary incisor inclination, relatively deficient chin growth, and a gummy smile. They also suggested that orthodontic treatment was preferable to ASO in patients with a skeletal Class I relationship and proclined upper and lower incisors. These recommendations were based on the assumption that orthodontic treatment with extraction is preferable for cases with maxillary or bimaxillary incisal proclination, whereas ASO is suitable for cases with skeletal issues or normal-range maxillary incisor inclination. However, this study found no significant difference in maxillary incisor inclination between the ASO and NASO groups before treatment. Specifically, it was noted that during orthodontic treatment, more controlled maxillary incisor movement can be achieved within the alveolar bone compared to that of the mandibular incisors due to the thicker medullary space of the palatal bone. Furthermore, advancements in orthodontic devices, such as TADs, have increased the scope of tooth movement in contemporary orthodontics.
While limited tooth movement has been attributed to NASO, studies reported the high risk of palatal bone resorption in high-angle Class II patients with normal incisal inclination and small medullary space in the palatal bone [14,15,16,17]. Additionally, articles cautioned against potential esthetic and bone-thickness-related issues on the labial side during extraction orthodontic treatment [14,18]. These studies highlight the importance of performing extraction orthodontic treatment (NASO) within a range that avoids functional problems with the dentition and maxillary alveolar bone, emphasizing that orthodontic treatment alone should not be pushed beyond limits to achieve a desirable outcome. Table 5 indicates that maxillary incisor retraction, measured by the U1 C to N-perpendicular value, was Δ −6.57 for the ASO group and Δ −4.11 for the NASO group. Similarly, the U1 R to N-perpendicular value was Δ −4.58 for the ASO group and Δ −1.45 for the NASO group. Thus, these findings suggest that NASO alone can provide sufficient movement with a root movement of Δ −1.45, achieving satisfactory results through controlled tipping to bodily movements.
In contrast, previous studies have often overlooked the importance of considering the inclination of the mandibular incisors in ASO diagnosis and treatment planning. This may be attributed to the varying thickness of the symphysis in the mandibular incisor area; generally, the amount of bone present in this area is lesser than that in the maxillary incisor area, limiting root movement. Consequently, bodily movement of the mandibular incisors is challenging, and efforts generally lead to only tipping movement. Nevertheless, the advantage of mandibular ASO lies in its ability to move the mandibular incisors. However, in Class II patients, where the roots are already positioned posteriorly, there are fewer indications for moving the root backwards through ASO.
According to Son et al. [17], even though the mandible is smaller in the anteroposterior dimension in Class II patients, lower lip protrusion can occur due to lip incompetence or protruding maxillary incisors pushing the lower lip downward and forward. In such cases, reducing maxillary protrusion alone may be sufficient to secure lower lip retraction. However, mandibular extraction orthodontics or posterior movement of point B through ASO in Class II patients may lead to excessive retrusion of the lower lip, resulting in an unesthetic outcome [9]. Mandibular ASO may be indicated in cases where the IMPA is not large, but the mandibular incisors exhibit severe extrusion despite being uprighted, requiring bodily movement and intrusion, or when there are concerns about gingival recession during retraction. However, in mandibular ASO for Class II patients with a large IMPA, counterclockwise rotation of point B is often necessary, which can make the surgical part difficult and potentially yield unsatisfactory outcomes [9]. The findings of the current study suggest that although the ANB was normalized, increased selective retraction of point A than that of point B was not observed in the ASO group, primarily due to technical difficulties in point B-oriented counterclockwise rotation of the mandibular anterior segment.
Therefore, in Class II patients with a normal curve of Spee in the mandibular incisors, where sufficient movement of the maxillary incisors through ASO is expected to enhance facial esthetics, it is advisable to consider orthodontic treatment in the mandible to improve IMPA while maximizing the preservation of point B, rather than opting for mandibular ASO (Figure 3A,B).
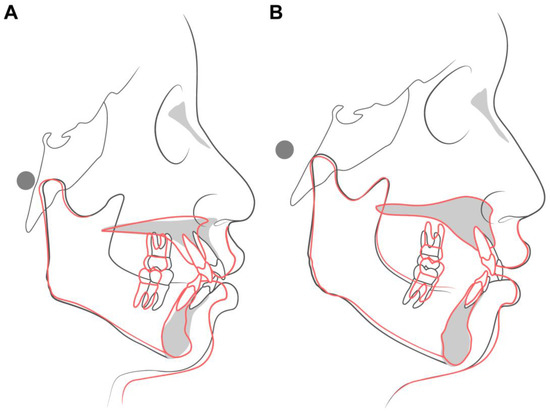
Figure 3.
(A) Superimposition of an ASO patient—initial (black line) and final (red line). (B) Superimposition of a NASO patient—initial (black line) and final (red line).
While this study did not include cases of ASO in the maxilla and lower full arch distalization, if the treatment plan requires retracting the maxillary incisor roots by approximately 4.6 mm (average in this study) and retroclining the mandibular incisors by approximately Δ −10.40° (average in this study), a suitable approach could entail ASO in the maxilla and total arch distalization using TADs in the mandible.
Several limitations must be acknowledged when interpreting the results of this study. One of the notable limitations of this study is that the pretreatment conditions of patients undergoing ASO and NASO did not completely align in terms of SNA, ANB, and IMPA. The ASO group exhibited a more pronounced skeletal Class II tendency, per the pretreatment measurements. For example, while both the ASO and NASO groups demonstrated skeletal Class II features primarily due to mandibular retrognathism, as evidenced by relatively normal SNA and decreased SNB values compared to Korean norms (SNA = 81.6 ± 3.10°, SNB = 79.1 ± 2.4°), it is noteworthy that the ASO group showed a significantly more retrusive B point as measured by B to N-perpendicular (−9.35 mm vs. −6.67 mm, p = 0.04). Therefore, we posit that with an increase in sample size and the inclusion of more borderline cases, a more comprehensive analysis of hard tissue changes in patients undergoing ASO compared to those undergoing NASO can be achieved. Moreover, this study investigated only hard tissue changes; therefore, further research is necessary to evaluate the corresponding soft tissue responses. The absence of long-term follow-up further restricted the ability to assess the durability and stability of the treatment outcomes over time. Relapse or delayed adverse effects may not have been captured within the observation period, potentially leading to an overestimation of treatment efficacy. Furthermore, the potential for clinician bias in treatment assignment cannot be overlooked. As treatment modalities were not randomly allocated, the decision to pursue ASO or NASO may have been influenced by subjective clinical judgment or patient-specific factors not fully accounted for in the analysis. Variability in patient compliance—such as the inconsistent use of elastics, poor oral hygiene, or missed appointments—may also have influenced treatment outcomes and contributed to inter-individual differences in responses, which could have introduced confounding variables and compromised the internal validity of the study. Lastly, the analyses were based on 2D cephalometric radiographs. Despite efforts to standardize the measurements, the 2D analysis may not have fully captured the complexity of skeletal and dental changes, especially in the transverse dimension.
5. Conclusions
It is often assumed that the amount of maxillary anterior retraction is the primary factor in determining whether ASO or NASO treatment is appropriate for Class II patients with lip protrusion. However, the results of this study indicated that non-surgical treatment achieved normal ANB, U1 to FH, and IMPA values postoperatively through 3.87 mm of posterior movement and 10.4° of retroclination of the lower incisors. Considering the change in IMPA, NASO was recommended as the treatment choice when a reduction of more than 10° in the IMPA was achievable. Therefore, when generating VTO/STO, achieving 5° more of incisor uprighting with orthodontic teeth movement may only suffice for nonsurgical treatment, serving as a clinical benchmark for deciding between ASO and NASO. In addition, since the mandibular incisors typically require less movement in patients with skeletal Class II, ASO treatment for the maxilla combined with total arch distalization using TADs in the mandible should be considered.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15094849/s1, Supplementary Table S1: Skeletal and dental measurements to compare ASO with NASO in borderline cases after treatment.
Author Contributions
P.H.: collection of data, analysis of data, interpretation of data, construction of manuscript. Y.H.K.: conception and design of the study, description of data results, construction of manuscript. H.C.: design and organization of the article. Y.-J.C.: Surgical information of the article. H.S.C.: conception and design of the article, analysis of data, interpretation of data, construction of manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013. This study was reviewed and approved by the Institutional Review Board (IRB) of Ajou University Hospital (IRB no.: AJIRB-MED-MDB-2022-354); Date of approval: 07 September 2023. The IRB Committee waived the requirement for obtaining patient informed consent.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
We would like to express my gratitude to Yujin Kwon for her support in composing the references.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Farrow, A.L.; Zarrinnia, K.; Azizi, K. Bimaxillary protrusion in black Americans—An esthetic evaluation and the treatment considerations. Am. J. Orthod. Dentofac. Orthop. 1993, 104, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Jayaratne, Y.S.; Zwahlen, R.A.; Lo, J.; Cheung, L.K. Facial soft tissue response to anterior segmental osteotomies: A systematic review. Int. J. Oral Maxillofac. Surg. 2010, 39, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Kim, B.H. Determinants of successful treatment of bimaxillary protrusion: Orthodontic treatment versus anterior segmental osteotomy. J. Craniofacial Surg. 2005, 16, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.G.; Mills, P.B.; Brenner, L.D. Maxillary and mandibular subapical osteotomies for the correction of anterior open-bite. Oral Surg. Oral Med. Oral Pathol. 1967, 23, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Chung, K.R.; Baek, S.H. Treatment outcomes of orthodontic treatment, corticotomy-assisted orthodontic treatment, and anterior segmental osteotomy for bimaxillary dentoalveolar protrusion. Plast. Reconstr. Surg. 2007, 120, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Hwang, B.Y.; Choi, B.J.; Lee, B.S.; Kwon, Y.D.; Lee, J.W.; Jung, J.; Ohe, J.Y. Comparison between anterior segmental osteotomy versus conventional orthodontic treatment in root resorption: A radiographic study using cone-beam computed tomography. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 34. [Google Scholar] [CrossRef] [PubMed]
- Yong, C.; Sng, T.; Quah, B.; Lee, C.; Lim, A.; Wong, R. The role of anterior segmental osteotomies in orthognathic surgery for protrusive faces in a Southeast Asian population: 10-year retrospective data of 51 patients treated in a single centre. Int. J. Oral Maxillofac. Surg. 2023, 52, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Tweed, C.H. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am. J. Orthod. Oral Surg. 1946, 32, 175–230. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lim, S.-W.; Chan, V.; Hong, P.; Han, S.-B.; Chae, H.S. The surgical outcomes of anterior segmental osteotomy in Asian skeletal class II patients. Oral Maxillofac. Surg. 2024, 28, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.C.; Burstone, C.J. Soft-tissue profile--fallacies of hard-tissue standards in treatment planning. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 52–62. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr. A method of cephalometric evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, J.L.; Proffit, W.R.; Sarver, D.M. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin. Orthod. Res. 1999, 2, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.T. Cephalometric soft tissue facial analysis. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 373–389. [Google Scholar] [CrossRef] [PubMed]
- Domingo-Clérigues, M.; Montiel-Company, J.-M.; Almerich-Silla, J.-M.; García-Sanz, V.; Paredes-Gallardo, V.; Bellot-Arcís, C. Changes in the alveolar bone thickness of maxillary incisors after orthodontic treatment involving extractions—A systematic review and meta-analysis. J. Clin. Exp. Dent. 2019, 11, e76. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.-W.; Moon, S.C.; Baek, S.-H. Morphometric evaluation of changes in the alveolar bone and roots of the maxillary anterior teeth before and after en masse retraction using cone-beam computed tomography. Angle Orthod. 2013, 83, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.-J.; Ge, Z.-P.; Ma, R.-H.; Hou, J.-X.; Li, G. A six-site method for the evaluation of periodontal bone loss in cone-beam CT images. Dentomaxillofac. Radiol. 2016, 45, 20150265. [Google Scholar] [CrossRef] [PubMed]
- Son, E.J.; Kim, S.J.; Hong, C.; Chan, V.; Sim, H.Y.; Ji, S.; Hong, S.Y.; Baik, U.B.; Shin, J.W.; Kim, Y.H.; et al. A study on the morphologic change of palatal alveolar bone shape after intrusion and retraction of maxillary incisors. Sci. Rep. 2020, 10, 14454. [Google Scholar] [CrossRef] [PubMed]
- Sarikaya, S.; Haydar, B.; Ciǧer, S.; Ariyürek, M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 15–26. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).