Digital Health Technology for Stroke Rehabilitation in Canada: A Scoping Review
Abstract
1. Introduction
- How are DHTs used in stroke rehabilitation across Canada?
- What key gaps exist in the current use of DHTs for stroke rehabilitation in this context?
- How can findings from Canadian research inform funding decisions, resource allocation, and clinical improvements in stroke rehabilitation?
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Inclusion & Exclusion Criteria
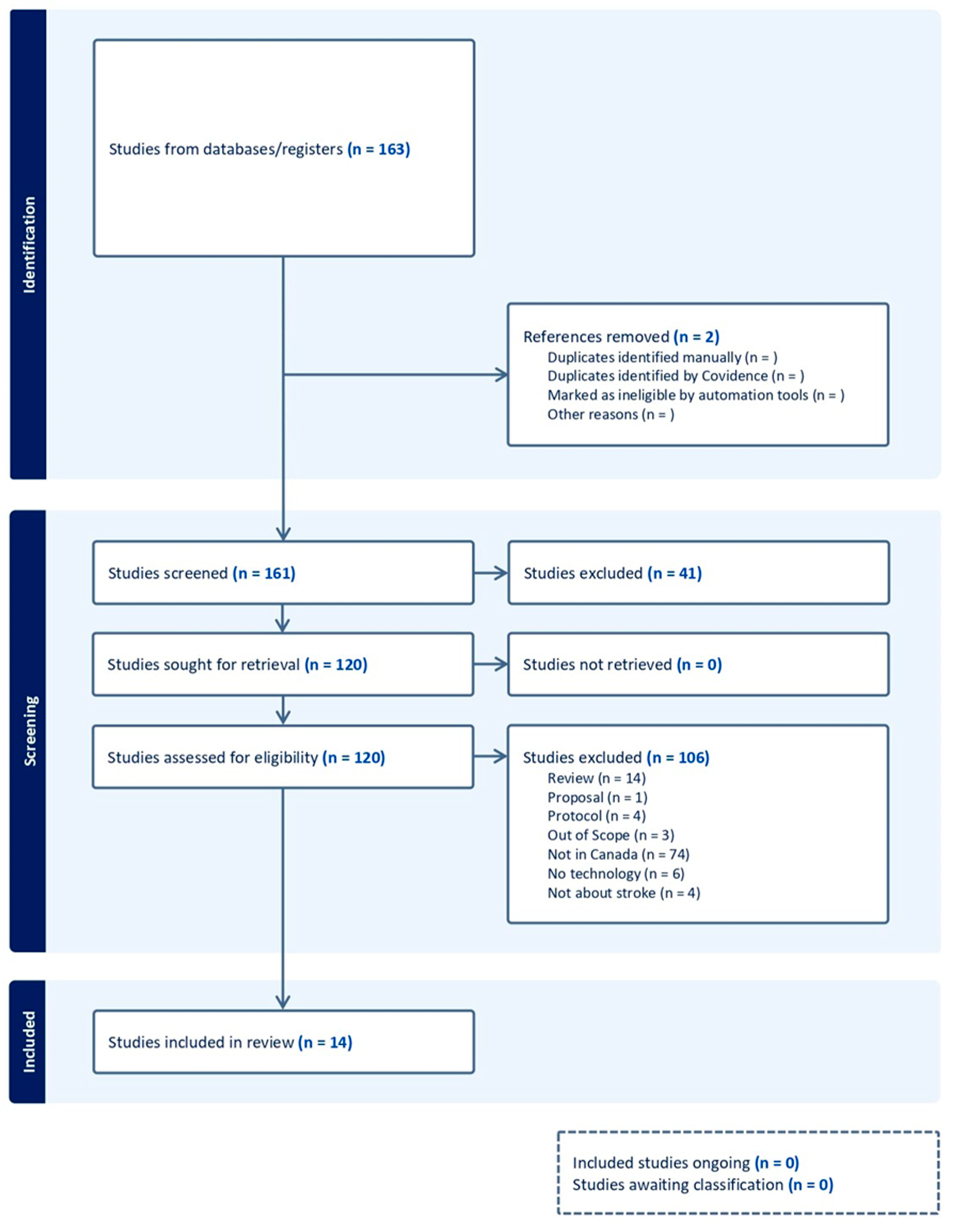
2.4. Study Selection Process
2.5. Data Extraction and Analysis
3. Results
3.1. VR and Telerehabilitation
3.2. Robotic Devices
3.3. Gaming Systems
3.4. Mobile and Sensor-Based Training
4. Discussion
4.1. Interpretations of Study Characteristics on the Use of DHTs in Stroke Rehabilitation in Canada
4.2. Findings on the Feasibility and Effectiveness of Technology Use in Stroke Rehabilitation in Canada
4.3. Determinants of DHT Adoption for Stroke Rehabilitation
4.4. Strengths and Limitations of This Review
5. Conclusions and Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ADLs | Activities of Daily Living |
| AI | Artificial Intelligence |
| DHT | Digital Health Technology |
| EMG | Electromyogram |
| FMA-UE | Fugl-Meyer Assessment for Upper Extremity |
| H-GRASP | Home-Graded Repetitive Arm Supplementary Program |
| UE | Upper Extremity |
| LE | Lower Extremity |
| RCT | Randomized Controlled Trial |
| VR | Virtual Reality |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews |
Appendix A
- exp stroke/
- exp Cerebral Hemorrhage/
- (stroke or strokes or cva* or poststroke* or apoplexy).tw,kw.
- ((cerebro* or brain or brainstem or cerebral*) adj3 (infarct* or accident*)).tw,kf.
- brain attack*.tw,kw.
- exp artificial intelligence/
- exp Monitoring, Physiologic/
- exp Monitoring, Ambulatory/
- Biofeedback, psychology/
- Self-Help Devices/
- exp Man-Machine Systems/
- automation/
- exp Computer Simulation/
- exp Video Games/
- exp wearable electronic devices/
- exp Cell Phone/ or Mobile Applications/ or Computers, Handheld/
- Electronic Mail/
- exp Touch Perception/
- wireless technology/
- (artificial intelligen* or AI or neural network* or (automat* adj2 recogni*) or machine learning).tw,kf.
- robot*.tw,kw.
- (video gam* or videogam* or exergam* or exer gam*).tw,kw.
- ambient assisted living.tw,kw.
- ambient intelligen*.tw,kw.
- (assistive adj3 (device* or technolog* or self-help)).tw,kf.
- ((ambient or smart or intelligent) adj2 (environment* or home* or house*)).tw,kf.
- (intelligent adj2 system*).tw,kf.
- ((technolog* or comput*) adj5 (ambient or non-wearable* or nonwearable* or unobtrusiv* or non-intrusive or nonintrusive or pervasive or ubiquitous or non-contact or noncontact or smart or intelligen* or passive)).tw,kf.
- (home adj2 (automation or device or module)).tw,kw.
- (digital technolog* or smart technolog*).tw,kw.
- ((monitor* or track*) adj2 (biomedical or medical or personal or home* or patient* or health or activit* or ambulat* or physiolog*)).tw,kf.
- (robot* or automat* or computer aided or computer assisted or power assist*).tw,kw.
- (virtual realit* or VR or simulat*).tw,kw.
- ((interactiv* or virtual) adj2 (environment or technolog*)).tw,kf.
- augmented realit*.tw,kw.
- (smartphone or smart-phone*).tw,kw.
- ((mobile or cell or smart or handheld) adj2 (device or phone*)).tw,kf.
- (iphone* or android* or ipad*).tw,kw.
- (personal digital assistant* or handheld computer* or handheld device*).tw,kw.
- mobile app*.tw,kw.
- haptic*.tw,kw.
- biofeedback.tw,kw.
- ((force or tactile or touch or tactual or electr*) adj2 (feedback or perception)).tw,kf.
- sensory substitution.tw,kw.
- piezoelectric*.tw,kw.
- (vibrotactile or vibration).tw,kw.
- wearable*.tw,kw.
- sensory aids/
- ((intelligent or smart) adj1 (home* or technolog* or sensor? or environment)).tw,kw.
- (rehabilitat* or rehab or “occupational therap*” or physiotherap* or “physical therap*”).tw,kw.
- rehabilitation/ or “activities of daily living”/ or neurological rehabilitation/ or stroke rehabilitation/ or telerehabilitation/
- exp Physical Therapy Modalities/
- Occupational Therapy/
- or/1–5 [Stroke Search]
- or/6–49 [Digital Technology Search]
- or/50–53 [Rehab Search]
- exp Canada/ or canada.cp. or canad*.tw,kw.
- 54 and 55 and 56 and 57 (129)
- limit 58 to english (128)
References
- Barracca, A.; Ledda, S.; Mancosu, G.; Pintore, G.; Quintaliani, G.; Ronco, C.; Kashani, K.B. Digital Health: A New Frontier. J. Transl. Crit. Care Med. 2023, 5, e00018. [Google Scholar] [CrossRef]
- Pawar, D.K.; Gujarathi, S.; Gupta, R.; Khan, A.; Tiwari, A. A Detail Review on Digital Health Technologies. Int. J. Res. Appl. Sci. Eng. Technol. 2024, 12, 2. [Google Scholar] [CrossRef]
- Perakslis, E.D.; Ginsburg, G.S. Digital Health-The Need to Assess Benefits, Risks, and Value. JAMA 2020, 325, 127–128. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.Y. Current status and future direction of digital health in Korea. Korean J. Physiol. Pharmacol. Off. J. Korean Physiol. Soc. Korean Soc. Pharmacol. 2019, 23, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Meskó, B. COVID-19’s Impact on Digital Health Adoption: The Growing Gap Between a Technological and a Cultural Transformation. JMIR Hum. Factors 2022, 9, e38926. [Google Scholar] [CrossRef]
- van Hattem, N.E.; Silven, A.V.; Bonten, T.N.; Chavannes, N.H. COVID-19’s impact on the future of digital health technology in primary care. Fam. Pract. 2021, 38, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Choukou, M.-A.; Taha, A.; Qadeer, A.; Monnin, C. Digital health technology for remote care in response to the COVID-19 pandemic: A scoping review. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 3386–3394. [Google Scholar]
- Alfian, S.D.; Insani, W.N.; Puspitasari, I.M.; Wawruch, M.; Abdulah, R. Effectiveness and Process Evaluation of Using Digital Health Technologies in Pharmaceutical Care in Low- and Middle-Income Countries: A Systematic Review of Quantitative and Qualitative Studies. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2023, 29, 1289–1303. [Google Scholar] [CrossRef]
- Dave, P. How Digital Health is Revolutionizing Healthcare and Contributing to Positive Health Outcomes. J. Drug Deliv. Ther. 2024, 14, 287–293. [Google Scholar] [CrossRef]
- Backman, C.; Papp, R.; Tonjock Kolle, A.; Papp, S.; Visintini, S.; Schaefer Ferreira de Mello, A.L.; de Melo Lanzoni, G.M.; Harley, A. Platform-Based Patient-Clinician Digital Health Interventions for Care Transitions: Scoping Review. J. Med. Internet Res. 2024, 26, e55753. [Google Scholar] [CrossRef]
- Hestetun-Mandrup, A.M.; Toh, Z.A.; Oh, H.X.; He, H.-G.; Martinsen, A.C.T.; Pikkarainen, M. Effectiveness of digital home rehabilitation and supervision for stroke survivors: A systematic review and meta-analysis. Digit. Health 2024, 10, 20552076241256861. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.; Cau, A.; Semakula, M.; Lodokiyiia, P.; Abdullahi, O.A.; Bullock, M.; Hayward, A.; Lester, R.T. Digital mHealth and Virtual Care Use During COVID-19 in 4 Countries: Rapid Landscape Review. JMIR Form. Res. 2020, 6, e26041. [Google Scholar] [CrossRef]
- Hughes, C.M.L.; Padilla, A.; Hintze, A.; Raymundo, T.M.; Sera, M.; Weidner, S.; Ontiveros, J.; Peng, T.; Encarcion, A.; Cruz, Z.A. Developing an mHealth app for post-stroke upper limb rehabilitation: Feedback from US and Ethiopian rehabilitation clinicians. Health Inform. J. 2020, 26, 1104–1117. [Google Scholar] [CrossRef]
- Krueger, H.; Koot, J.; Hall, R.E.; O’callaghan, C.; Bayley, M.T.; Corbett, D. Prevalence of Individuals Experiencing the Effects of Stroke in Canada: Trends and Projections. Stroke 2015, 46, 2226–2231. [Google Scholar] [CrossRef] [PubMed]
- Teasell, R.; Foley, N.; Bhogal, S.; Bagg, S.; Jutai, J. Evidence-based practice and setting basic standards for stroke rehabilitation in Canada. Top. Stroke Rehabil. 2006, 13, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Buyting, R.; Melville, S.; Chatur, H.; White, C.; Légaré, J.-F.; Lutchmedial, S.; Brunt, K.R. Virtual care with digital technologies for rural and remote Canadians living with cardiovascular disease. CJC Open 2020, 4, 133–147. [Google Scholar] [CrossRef]
- Choukou, M.-A.; Maddahi, A.; Polyvyana, A.; Monnin, C. Digital health technology for Indigenous older adults: A scoping review. Int. J. Med. Inform. 2021, 148, 104408. [Google Scholar] [CrossRef]
- Richards, C.L.; Malouin, F.; Nadeau, S. Stroke rehabilitation: Clinical picture, assessment, and therapeutic challenge. Prog. Brain Res. 2015, 218, 253–280. [Google Scholar]
- McIntyre, A.; Viana, R.; Cao, P.; Janzen, S.; Saikaley, M.; Harnett, A.; Teasell, R. A national survey of evidence-based stroke rehabilitation intervention use in clinical practice among Canadian occupational therapists. NeuroRehabilitation 2023, 52, 463–475. [Google Scholar] [CrossRef]
- Bayley, M.T.; Hurdowar, A.; Richards, C.L.; Korner-Bitensky, N.; Wood-Dauphinee, S.; Eng, J.J.; McKay-Lyons, M.; Harrison, E.; Teasell, R.; Harrison, M.B.; et al. Barriers to implementation of stroke rehabilitation evidence: Findings from a multi-site pilot project. Disabil. Rehabil. 2012, 34, 1633–1638. [Google Scholar] [CrossRef]
- Meyer, M.J.; Meyer, J.-P.; Foley, N.C.; Salter, K.L.; McClure, J.A.; Teasell, R. Stroke Rehabilitation in Ontario: An Opportunity for Health Care Transformation. Can. J. Neurol. Sci. J. Can. Des. Sci. Neurol. 2011, 38, 810–814. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Elnady, A.; Mortenson, W.B.; Menon, C. Perceptions of existing wearable robotic devices for upper extremity and suggestions for their development: Findings from therapists and people with stroke. JMIR Rehabil. Assist. Technol. 2018, 5, e9535. [Google Scholar] [CrossRef]
- Vollebregt, B.; Reinikka, K.; Vasiliu, D.; Pepe, A.; Prasanna, S.S.; Jain, A.; Lawrence-Dewar, J.; Johnson, V.B. The Impact of a Hand Training Programme in Chronic Stroke Survivors: A Qualitative Analysis of Participant Perceived Benefits. In Proceedings of the 2019 International Conference on Virtual Rehabilitation (ICVR), Tel Aviv, Israel, 21–24 July 2019; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar]
- Paquin, K.; Crawley, J.; Harris, J.E.; Horton, S. Survivors of chronic stroke–participant evaluations of commercial gaming for rehabilitation. Disabil. Rehabil. 2016, 38, 2144–2152. [Google Scholar] [CrossRef]
- Tatla, S.K.; Shirzad, N.; Lohse, K.R.; Virji-Babul, N.; Hoens, A.M.; Holsti, L.; Li, L.C.; Miller, K.J.; Lam, M.Y.; Van der Loos, H.M. Therapists’ perceptions of social media and video game technologies in upper limb rehabilitation. JMIR Serious Games 2015, 3, e3401. [Google Scholar] [CrossRef]
- Hernandez, A.; Bubyr, L.; Archambault, P.S.; Higgins, J.; Levin, M.F.; Kairy, D. Virtual reality–based rehabilitation as a feasible and engaging tool for the management of chronic poststroke upper-extremity function recovery: Randomized controlled trial. JMIR Serious Games 2022, 10, e37506. [Google Scholar] [CrossRef]
- Bouchard, A.E.; Corriveau, H.; Milot, M.-H. A single robotic session that guides or increases movement error in survivors post-chronic stroke: Which intervention is best to boost the learning of a timing task? Disabil. Rehabil. 2017, 39, 1607–1614. [Google Scholar] [CrossRef]
- Sheehy, L.; Taillon-Hobson, A.; Sveistrup, H.; Bilodeau, M.; Fergusson, D.; Levac, D.; Finestone, H. Does the addition of virtual reality training to a standard program of inpatient rehabilitation improve sitting balance ability and function after stroke? Protocol for a single-blind randomized controlled trial. BMC Neurol. 2016, 16, 42. [Google Scholar] [CrossRef]
- Paquin, K.; Ali, S.; Carr, K.; Crawley, J.; McGowan, C.; Horton, S. Effectiveness of commercial video gaming on fine motor control in chronic stroke within community-level rehabilitation. Disabil. Rehabil. 2015, 37, 2184–2191. [Google Scholar] [CrossRef]
- Salbach, N.M.; MacKay-Lyons, M.; Solomon, P.; Howe, J.-A.; McDonald, A.; Bayley, M.T.; Veitch, S.; Sivarajah, L.; Cacoilo, J.; Mihailidis, A. The role of theory to develop and evaluate a toolkit to increase clinical measurement and interpretation of walking speed and distance in adults post-stroke. Disabil. Rehabil. 2022, 44, 3719–3735. [Google Scholar] [CrossRef] [PubMed]
- Allegue, D.R.; Kairy, D.; Higgins, J.; Archambault, P.S.; Michaud, F.; Miller, W.C.; Sweet, S.N.; Tousignant, M. A personalized home-based rehabilitation program using exergames combined with a telerehabilitation app in a chronic stroke survivor: Mixed methods case study. JMIR Serious Games 2021, 9, e26153. [Google Scholar] [CrossRef]
- Saposnik, G.; Mamdani, M.; Bayley, M.; Thorpe, K.E.; Hall, J.; Cohen, L.G.; Teasell, R. Effectiveness of Virtual Reality Exercises in STroke Rehabilitation (EVREST): Rationale, design, and protocol of a pilot randomized clinical trial assessing the Wii gaming system. Int. J. Stroke 2010, 5, 47–51. [Google Scholar] [CrossRef]
- Allegue, D.R.; Higgins, J.; Sweet, S.N.; Archambault, P.S.; Michaud, F.; Miller, W.; Tousignant, M.; Kairy, D. Rehabilitation of upper extremity by telerehabilitation combined with exergames in survivors of chronic stroke: Preliminary findings from a feasibility clinical trial. JMIR Rehabil. Assist. Technol. 2022, 9, e33745. [Google Scholar] [CrossRef] [PubMed]
- Allegue, D.R.; Sweet, S.N.; Higgins, J.; Archambault, P.S.; Michaud, F.; Miller, W.C.; Tousignant, M.; Kairy, D. Lessons Learned from Clinicians and Stroke Survivors About Using Telerehabilitation Combined with Exergames: Multiple Case Study. JMIR Rehabil. Assist. Technol. 2022, 9, e31305. [Google Scholar] [CrossRef]
- Simpson, L.A.; Eng, J.J.; Chan, M. H-GRASP: The feasibility of an upper limb home exercise program monitored by phone for individuals post stroke. Disabil. Rehabil. 2017, 39, 874–882. [Google Scholar] [CrossRef]
- Kapral, M.K.; Hall, R.; Gozdyra, P.; Amy, Y.; Jin, A.Y.; Martin, C.; Silver, F.L.; Swartz, R.H.; Manuel, D.G.; Fang, J. Geographic access to stroke care services in rural communities in Ontario, Canada. Can. J. Neurol. Sci. 2020, 47, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.M.; Mawson, S.J.; Brownsell, S. Telerehabilitation: Enabling the remote delivery of healthcare, rehabilitation, and self management. Stud. Health Technol. Inform. 2009, 145, 231–248. [Google Scholar]
- Putrino, D. Telerehabilitation and emerging virtual reality approaches to stroke rehabilitation. Curr. Opin. Neurol. 2014, 27, 631–636. [Google Scholar] [CrossRef]
- Altilio, R.; Liparulo, L.; Panella, M.; Proietti, A.; Paoloni, M. Multimedia and Gaming Technologies for Telerehabilitation of Motor Disabilities [Leading Edge]. IEEE Technol. Soc. Mag. 2015, 34, 23–30. [Google Scholar] [CrossRef]
- Arienti, C.; Armijo-Olivo, S.; Ferriero, G.; Peter, F.; Hoogeboom, T.; Kiekens, C.; Lazzarini, S.G.; Minozzi, S.; Negrini, S.; Aydan, O. The influence of bias in randomized controlled trials on rehabilitation intervention effect estimates: What we have learned from meta-epidemiological studies. Eur. J. Phys. Rehabil. Med. 2023, 60, 135. [Google Scholar] [CrossRef] [PubMed]
- Wang, F. Recent research advances in upper-extremity rehabilitation. Adv. Robot. Autom. 2012, 1, e110. [Google Scholar] [CrossRef]
- Abdullahi, A.; Wong, T.W.; Ng, S.S. Variation in the rate of recovery in motor function between the upper and lower limbs in patients with stroke: Some proposed hypotheses and their implications for research and practice. Front. Neurol. 2023, 14, 1225924. [Google Scholar] [CrossRef]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef] [PubMed]
- Draaisma, L.R.; Wessel, M.J.; Hummel, F.C. Neurotechnologies as tools for cognitive rehabilitation in stroke patients. Expert Rev. Neurother. 2020, 20, 1249–1261. [Google Scholar] [CrossRef]
- Malik, A.N.; Tariq, H.; Afridi, A.; Rathore, F.A. Technological advancements in stroke rehabilitation. J. Pak. Med. Assoc. 2022, 72, 1672–1674. [Google Scholar]
- Domínguez, A.A.; Periñán, M.J.Z.; González, C.G. Aportación de la rehabilitación a la prevención y manejo de las complicaciones de la fase aguda del ictus. Rehabilitación 2000, 34, 400–411. [Google Scholar]
- Brandstater, M.E.; Shutter, L.A. Rehabilitation Interventions During Acute Care of Stroke Patients. Top. Stroke Rehabil. 2002, 9, 48–56. [Google Scholar] [CrossRef]
- Siekierka, E.; Eng, K.; Bassetti, C.; Blickenstorfer, A.; Cameirao, M.; Dietz, V.; Duff, A.; Erol, F.; Ettlin, T.; Hermann, D. New technologies and concepts for rehabilitation in the acute phase of stroke: A collaborative matrix. Neurodegener. Dis. 2007, 4, 57–69. [Google Scholar] [CrossRef]
- Thommessen, B.; Wyller, T.B. Hospital-based rehabilitation after stroke. Tidsskr. Nor. Laegeforen. Tidsskr. Prakt. Med. Ny Raekke 2007, 127, 1224–1227. [Google Scholar]
- Caughlin, S.; Mehta, S.; Corriveau, H.; Eng, J.J.; Eskes, G.A.; Kairy, D.; Meltzer, J.A.; Sakakibara, B.M.; Teasell, R. Implementing Telerehabilitation After Stroke: Lessons Learned from Canadian Trials. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2020, 26, 710–719. [Google Scholar] [CrossRef]
- Schuster-Amft, C.; Kool, J.; Möller, J.C.; Schweinfurther, R.; Ernst, M.J.; Reicherzer, L.; Ziller, C.; Schwab, M.E.; Wieser, S.; Wirz, M.; et al. Feasibility and cost description of highly intensive rehabilitation involving new technologies in patients with post-acute stroke—A trial of the Swiss RehabTech Initiative. Pilot Feasibility Stud. 2022, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Choukou, M.-A.; He, E.; Moslenko, K. Feasibility of a Virtual-Reality-Enabled At-Home Telerehabilitation Program for Stroke Survivors: A Case Study. J. Pers. Med. 2023, 13, 1230. [Google Scholar] [CrossRef]
- Shek, A.; Biondi, A.; Ballard, D.; Wykes, T.; Simblett, S.K. Technology-based interventions for mental health support after stroke: A systematic review of their acceptability and feasibility. Neuropsychol. Rehabil. 2019, 31, 432–452. [Google Scholar] [CrossRef]
- Ballantyne, R.; Rea, P.M. A Game Changer: ‘The Use of Digital Technologies in the Management of Upper Limb Rehabilitation’. Adv. Exp. Med. Biol. 2019, 1205, 117–147. [Google Scholar] [PubMed]
- Toh, S.F.M.; Chia, P.F.; Fong, K.N. Effectiveness of home-based upper limb rehabilitation in stroke survivors: A systematic review and meta-analysis. Front. Neurol. 2022, 13, 964196. [Google Scholar] [CrossRef] [PubMed]
- Saposnik, G.; Levin, M.F. Virtual Reality in Stroke Rehabilitation: A Meta-Analysis and Implications for Clinicians. In Ischemic Stroke Therapeutics; Springer: Cham, Switzerland, 2011; Volume 42, pp. 1380–1386. [Google Scholar]
- Kerr, A.; Smith, M.; Reid, L.; Baillie, L. Adoption of Stroke Rehabilitation Technologies by the User Community: Qualitative Study. JMIR Rehabil. Assist. Technol. 2018, 5, e9219. [Google Scholar] [CrossRef]
- Morrow, C.; Johnson, E.E.; Simpson, K.N.; Seo, N.J. Determining Factors that Influence Adoption of New Post-Stroke Sensorimotor Rehabilitation Devices in the USA. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 1213–1222. [Google Scholar] [CrossRef]
- Klaic, M.; Galea, M.P. Using the Technology Acceptance Model to Identify Factors That Predict Likelihood to Adopt Tele-Neurorehabilitation. Front. Neurol. 2020, 11, 580832. [Google Scholar] [CrossRef]
| Author | Study Type | Goals | Participants | Stroke Phase | Setting | Type of Technology | Main Findings | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Description | Main Goal | Outcome Focus | N | Age | Male/Female | |||||||
| 1 | Dorra Rakia Allegue (2022) [37] | Multiple Case Study Design | Identify behavioral and motivational techniques used by clinicians during the virtele intervention. Explore indicators of empowerment among stroke survivors. Investigate the determinants of VirTele use among stroke survivors and clinicians. | Client Perception, Clinician Perception | UE | 3 | Mean Age of 58.8 (SD 19.4) | F (2) M (1) | Chronic | Home | VR and Telerehabilitation | 5 major determinants of virtele use emerged from the qualitative analyses:
|
| 2 | Dorra Rakia Allegue (2022) [36] | Feasibility Clinical Trial | Determine the feasibility of using virtele in survivors of chronic stroke at home and explore the impact of VirTele on UE motor function, quantity and quality of use, quality of life, and motivation in survivors of chronic stroke compared with conventional therapy. | Feasibility | UE | 11 | Mean Age 57.8 | Both Genders | Chronic | Home | VR and Telerehabilitation | The VirTele intervention constitutes another therapeutic alternative, in addition to the GRASP, to deliver an intense personalized rehabilitation program to survivors of chronic stroke (at least 8 years since the stroke) with UE deficits. The highest scores for autonomous motivation were achieved in the experimental group, which achieved a high frequency of use of the exergames and a very high number of repetitions. |
| 3 | Nancy M. Salbach (2022) [33] | Quantitative (Case Study) & Qualitative | Describe how authors used a process model, a determinant framework, and two classic theories to guide the design and process evaluation of the implementation of the iWalk toolkit. | Clinician Perception | Walking Speed | Pre-Intervention: 49 Post-Intervention: 37 Focus Group: 33 | Pre-Intervention: Mean Age of 38.7 Post-Intervention: Mean Age of 38.1 Focus Group: Mean Age of 38.5 | Pre-Intervention: F (45) M (4) Post-Intervention: F (33) M (4) Focus Group: F (29) M (4) | Chronic | Home | Mobile and Sensor Based Training | Self-efficacy ratings for recommended practices increased and were significant for the 10 mwt. Theory-based toolkit features and implementation strategies likely facilitated engagement with toolkit components, contributing to observed improvements in pts’ knowledge, attitudes, skill, self-efficacy, and clinical practice. |
| 4 | Alejandro Hernandez (2022) [29] | RCT | (Determine the extent to which a 1-month intervention using a VR-based serious game is effective in improving UE function compared with an evidence-based home exercise program. Assess the feasibility of implementing the intervention for chronic stroke rehabilitation in participants’ homes. | Intervention Effectiveness | UE | 51 | Treatment: Mean Age 59.8 (Sd 13.1) Standard Care: Mean Age 56.7 (Sd 11.2) | F (14) M (37) | Chronic | Institution | Vr and Telerehabilitation | UE training for chronic stroke survivors using virtual rehabilitation in their home may be as effective as a gold standard home exercise program and those who used the system the most achieved the greatest improvement in UE function, indicating its relevance to being included as part of ongoing rehabilitation services |
| 5 | Dorra Rakia Allegue (2021) [34] | Mix Method Case Study | To determine the feasibility of VirTele for remote UE rehabilitation in a chronic stroke survivor Explore the preliminary efficacy of virtele on UE motor function, the amount and quality of UE use, and impact on quality of life and motivation Explore the determinants of behavioral intention and use behavior of VirTele along with indicators of empowerment. | Feasibility | UE | 1 | 63 | Male | Chronic | Home | Vr and Telerehabilitation | Results suggest that the virtele intervention and the study protocol could be feasible for stroke survivors. |
| 6 | Brontë Vollebregt (2019) [26] | Qualitative | Determine the perceived benefits of the participants in a hand training program using a haptic indirect-feedback hand function device (HIFHFD) | Client Perception | UE | 8 | 55–82 (M = 69.38) | F (3) M (5) | Chronic | Institution | Mobile and Sensor-Based Training | This study provided insight into the response of stroke survivors to a community-based hand training program using this novel HIFHFD and examined its impact on their QOL. In addition to functional improvements, participants experienced a sense of community, companionship, and motivation. |
| 7 | Lisa A. Simpson (2019) [38] | Pre-Post Double Baseline Repeated Measures Design | Investigate the feasibility of a phone-monitored home exercise program for the UE following stroke. | Feasibility | UE | 8 | Mean 66.4 | Female 4 Male 4 | >2 Months and <12 Months Post-Stroke | home | Mobile and Sensor Based Training | The H-GRASP was feasible for participants when they were sufficiently challenged by the exercise program. Participants showed sustainable improvements in UE function, UE use, grip strength and occupational performance following the H-GRASP program. |
| 8 | Ahmed Elnady (2018) [25] | Qualitative | Describe users’ perceptions about existing wearable robotic devices for the ue education and information technologies Identify if there is a need to develop new devices for the ue and the desired features Explore obstacles that would influence the utilization of these new devices. | Client Perception, Clinician Perception | UE | 10 | 50–60 (13%) 61–70 (62%) >70 (25%) | F (13%) M (87%) | Chronic | Home and Institution | Robotic Devices | “They exist, but…” A. Existing devices and technologies B. Cost-effectiveness C. Doubts on efficiency D. Compromise the independence Indeed, we need more. Can we have it all? A. Assistance vs. rehabilitation B. Distal vs. proximal C. Portability vs. complexity D. Activation and motivation Bumps on the road A. Single solution is challenging B. Ensure accessibility C. Setup time and learning curve |
| 9 | Amy E. Bouchard (2017) [30] | RCT | The goal of the study was to evaluate the impact of a single session of haptic guidance (HG) and error amplification (EA) robotic training interventions on the improvement of post-stroke timing accuracy. | Intervention Effectiveness | UE | 34 | Haptic Guidance Group: 67 ± 7, Error Amplification Group: 67 ± 6 | NA | Chronic | Institution | Robotic Devices | The results of this innovative study have demonstrated that HG robotic training helps improve the immediate timing accuracy of Survivors’ post-chronic stroke, and that the side of the stroke lesion can influence timing accuracy following EA training. Knowing that Timing deficits can have a detrimental impact on the performance of daily activities |
| 10 | Kate Paquin (2016) [27] | Qualitative | Gather end-user data from chronic stroke participants who engaged with an off-the-shelf CG device in a community-level rehabilitation setting. | Client Perception | UE | 10 | Mean Age 72.1 | Male (10) | Chronic | Home | Gaming Systems | Participants illustrated the positive impact that VR training had on their functional abilities as well as their confidence towards completing activities of daily living (ADL). Participants also expressed the need for increased rehabilitation opportunities within the community. |
| 11 | L. Sheehy (2016) [31] | RCT | Determine if supplemental VRT-based sitting balance exercises improve sitting balance ability and function in stroke rehabilitation inpatients. | Intervention Effectiveness | Sitting Balance | 76 | NA | NA | Acute | Institution | VR and Telerehabilitation | Provide important evidence for the use of low-cost, accessible VRT as an adjunct intervention to increase sitting balance in lower-functioning patients receiving inpatient rehabilitation. The motivating and enjoyable attributes of VRT may increase exercise dosage, leading to improved function and optimal results from rehabilitation. |
| 12 | Kate Paquin (2015) [32] | RCT | Investigate the effectiveness of commercial gaming as an intervention for fine motor recovery in chronic stroke. | Intervention Effectiveness | UE | 10 | Mean Age 72.1 | M (10) | Chronic | Home | Gaming Systems | Illustrating an increase in fine motor ability as well as an increase in the participants’ perceived ability to complete ADL. |
| 13 | Sandy K Tatla (2015) [28] | Qualitative | Explore clinicians’ perceptions of how young people and adults with hemiplegia use gaming and social media technologies in daily life and rehabilitation Identify barriers to using these technologies in rehabilitation. | Clinician Perception | UE | 10 | 20–34 Years Old: 5 (50%) 35–49 Years Old: 4 (40%) 50–64 Years Old: 1 (10%) | F (8) M (2) | NA | Institution | Gaming Systems | Therapists were using technology in a limited capacity. They identified barriers to using social media and gaming technology with their clients, including a lack of age appropriateness, privacy issues with social media, limited transfer of training, and a lack of accessibility of current systems. Therapists also questioned their role in the context of technology-based interventions. The opportunity for social interaction was perceived as a major benefit of integrated gaming and social media |
| 14 | G. Saposnik (2010) [35] | Pilot RCT | ComparE VRWII versus recreational therapy in patients receiving standard rehabilitation within six months of stroke with a motor deficit of ≥3 on the Chedoke-McMaster Scale (arm) | Effectiveness of the Intervention | UE | 21 | Mean Age: 61 [41–83] Years | NA | Acute | Institution | Gaming Systems | The results of secondary endpoints will serve to calculate the necessary sample size for a potentially larger multicentre trial. The initial step in understanding of the potential benefit of interactive rehabilitation using Wii gaming technology post-stroke with potential implications for daily patient care. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kheirollahzadeh, M.; Sarvghadi, P.; Azizkhani, S.; Bani Hani, J.; Monnin, C.; Choukou, M.-A. Digital Health Technology for Stroke Rehabilitation in Canada: A Scoping Review. Appl. Sci. 2025, 15, 5340. https://doi.org/10.3390/app15105340
Kheirollahzadeh M, Sarvghadi P, Azizkhani S, Bani Hani J, Monnin C, Choukou M-A. Digital Health Technology for Stroke Rehabilitation in Canada: A Scoping Review. Applied Sciences. 2025; 15(10):5340. https://doi.org/10.3390/app15105340
Chicago/Turabian StyleKheirollahzadeh, Mahsa, Pooria Sarvghadi, Sarah Azizkhani, Jasem Bani Hani, Caroline Monnin, and Mohamed-Amine Choukou. 2025. "Digital Health Technology for Stroke Rehabilitation in Canada: A Scoping Review" Applied Sciences 15, no. 10: 5340. https://doi.org/10.3390/app15105340
APA StyleKheirollahzadeh, M., Sarvghadi, P., Azizkhani, S., Bani Hani, J., Monnin, C., & Choukou, M.-A. (2025). Digital Health Technology for Stroke Rehabilitation in Canada: A Scoping Review. Applied Sciences, 15(10), 5340. https://doi.org/10.3390/app15105340








