Abstract
This study aims to present the development of a wearable prototype device consisting of soft robotic gloves (SRGs), its integration into a wearable robotics platform for sensorimotor rehabilitation, and the device’s validation experiments with individuals suffering from impaired hand motor function due to neurological lesions. The SRG is tested and evaluated by users with spinal cord injury (SCI) and stroke. The proposed system combines multiple-sensor arrays with pneumatic actuation to assist finger movement during grasping tasks. Evaluations on SCI and stroke patients revealed that the gloves consistently improved finger and grip performance. Detailed analyses indicated observable differences in sensor-derived features during actuation versus non-actuation, with statistically significant modifications appearing in both time-domain and frequency-domain metrics. Although the stroke participants exhibited greater variability, all participants were able to use the system reporting low discomfort and effort. The findings underscore the potential for personalized calibration to further optimize therapeutic outcomes. In summary, the study validates the utility of these gloves as assistive and rehabilitative modalities, and future research will focus on refining the device in the context of multimodal wearable robotics and individualized neurorehabilitation strategies.
1. Introduction
The human hand’s intrinsic biomechanical complexity and it’s overlying multi-level neuronal integration [1] enables precise voluntary movement [2,3], allows for detailed interaction with the surrounding world [4], plays a crucial role in multisensory integration in the brain [5], and is integral in the execution of many activities of daily living (ADLs) [6]. Loss of hand function is a traumatic consequence of many neurological conditions [7], including SCI and stroke, that significantly affects patient quality of life (QoL) [8,9], acting as a major barrier to patient independence [10,11].
Over 15 million people worldwide live with spinal cord injury—most resulting from preventable trauma such as falls, traffic collisions, or violence—and younger age groups are disproportionately affected [12]. Stroke afflicts more than 100 million individuals globally, with over 15 million new cases each year, and remains the third leading cause of death and disability, accounting for some 160 million disability-adjusted life years lost [13,14]. Both SCI and stroke survivors face elevated risks of secondary complications, increased morbidity and premature mortality, and reduced educational and economic participation. Addressing this dual burden demands integrated strategies for prevention, acute care, rehabilitation, and long-term support to enhance outcomes and societal well-being [15].
Rehabilitation and restoration of hand function after neural damage can be challenging due to the aforementioned biomechanical and neural complexity. Therefore, addressing the challenge requires innovative strategies, among which lies the vision of creating robotic systems that mimic the functionality of human hand physiology [16]. In this context, soft robotics (SR) presents a promising solution by offering improved adaptability and harmony with the hand’s dynamic movements [17]. Exercise-based treatments that attempt to stimulate affected muscles’ activation while training the patient to perform specific activities have improved the neurologic recovery of the upper extremity in SCI and stroke [18]. The success of these treatments warrants further exploration of their relevance to hand function [19]. In addition, SCI and stroke survivors display a diverse range of phenotypes from complete paralysis to partial weakness and varied degrees of spasticity [20]. Although many patients retain some degree of hand function after SCI or stroke, performing ADLs [21] remains a significant challenge. Achieving complete recovery is often difficult and, in many cases, impossible [22].
To enhance rehabilitation—even in cases of partial recovery—it is essential to employ targeted motor exercises that both quantify patient progress and gauge therapeutic efficacy [23]. Conventional physical therapy is labor-intensive and costly [24], motivating the development of portable, user-friendly orthotic and robotic devices that simplify donning and doffing while remaining affordable [25]. Soft robotic gloves (SRGs) leverage compliant materials and advanced control systems to augment hand function and support sensorimotor retraining [26], yet optimal protocols for their clinical integration remain undefined [27]. We hypothesize that embedding SRGs within neurorehabilitation regimens will enhance motor recovery and drive neuroplastic changes, ultimately improving outcomes for individuals with hand deficits due to SCI or stroke. This study therefore aims to identify and evaluate strategies for effective SRG implementation in therapeutic settings, thereby maximizing their rehabilitative impact and quality-of-life benefits.
In this manuscript, we present the design, development, and evaluation experiments integrating ADL features of a wearable prototype device consisting of soft robotic gloves (SRGs). The SRG is tested and evaluated by users with spinal cord injury (SCI) and stroke with impaired hand function. Data from a multiple-sensor array are utilized to drive pneumatic actuation to assist finger movement during grasping tasks. Analyses are performed on physiological signals to evaluate actuated against non-actuated performance by users, while the user experience and the perception of robotics are also presented.
2. Materials and Methods
2.1. Body-Area-Distributed Sensor and Actuator System and the NeuroSuitUp Platform
The SRG system was developed as part of a larger assistive wearable robotics suite, designed to enable neuroplasticity-induced neurorehabilitation for patients post-spinal cord injury and stroke (Figure 1). The platform records the kinematic and dynamic response of users during serious game-mediated training regimens, and generates the corresponding control response, through the use of lightweight, flexible, and dedicated actuation techniques [28]. The complementary wearable modalities of the suite include an upper and lower-body cloth-based exoskeleton, ensuring ease of use and minimal impact on the participants while providing a multi-segmental view of movement. Kinematic data are provided by 9 degrees of freedom (DoF) inertial measurement units (IMUs) placed on the primary kinematic segments of the corresponding body region (5 for the upper body, 4 for the lower body) to enable real-time recording of motion. In order to evaluate the underlying dynamics of the motor system, surface electromyography (sEMG) units are employed in the major muscle groups actuating the corresponding monitored kinematic joints (14 for the upper, 4 for the lower body).
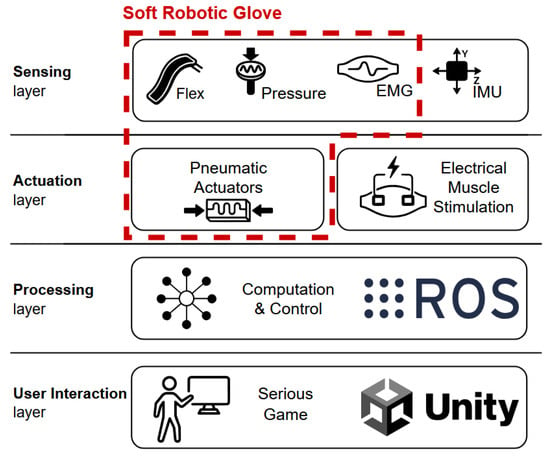
Figure 1.
NeuroSuitUp - HEROES suite architecture.
Given the extensive impact of these pathologies on movement, the modalities are equipped with an electrical muscle stimulation (EMS) subsystem, providing assistance when the desired range-of-motion and ambient force generation capabilities of each user are insufficient for the task. The control strategies focus on providing stimulation in response to accumulated kinematic errors, specifically when participants fail to achieve target joint angles (position errors) or desired movement velocities (velocity errors) during task execution [29].
Sensor data acquisition, processing, and control strategies employed by the suite are managed through a dedicated set of robot operating system (ROS) packages. This modular ROS stack enables reliable communication between operational nodes, including sensors, data processing filters, and control algorithms, whilst facilitating experimentation with different control strategies, under repeatable conditions. The processed sensor data are subsequently integrated into a custom serious game application, developed in Unity. The platform delivers interactive task-based training regimens, designed by healthcare professionals after a comprehensive physical evaluation, to ensure full adaptability to the patient’s functional status and rehabilitation goals [29]. The continuous interaction between sensor data acquisition, real-time visual feedback through the serious gaming application, and the control actuation strategies aims to establish a robust biofeedback loop. This loop is designed to promote neuroplasticity and enable a highly personalized, motivating, and immersive neurorehabilitation program.
The Wearable SRG
Wearable SRGs have emerged as a game-changing invention in the rehabilitation of people with hand impairments, providing new opportunities for regaining hand function and improving overall QoL [30]. These devices are intended to help patients undertake therapeutic regimens while also fostering brain neuroplasticity and motor skill development via interactive, user-friendly interfaces. The wearable SRGs presented in this manuscript incorporate modern technologies such as sensors, SR actuators, and adaptive control software systems, which can give individualized assistance and feedback during rehabilitation sessions.
2.2. Design, Development, and Integration of SRGs
The SRGs presented in this manuscript leverage a combination of multi-sensor data and SR exoskeleton actuation for sensorimotor rehabilitation of the human hand (Table 1) [31]. The emphasis on wearability, portability, and power autonomy is key to this effort, as it aligns with the practical needs of rehabilitation settings and the requirement for user-friendly therapies. The proposed system consists of three interrelated subsystems designed to synergistically facilitate rehabilitation and produce the best possible therapeutic outcomes: (a) The multi-sensor subsystem (MSS) encompasses a suite of sensors strategically integrated into the SRG, enabling data acquisition essential for monitoring hand movements and muscle activity for assessing the user’s hand motor performance and physiological responses. Complementing this sensing capability is (b) the soft robotic pneumatic actuation subsystem (SRPAS), featuring a PneuNet-based [32] flexible soft-shell robotic exoskeleton engineered to apply targeted forces and stimuli to the user’s hand [33]. Crucially, the SRPAS operates in tandem with a (c) microcontroller-based Communication Software Subsystem (ComSS), orchestrating near-real-time processing of the sensor data collected by the MSS, enabling precise control over the SRPAS movements and interactions with the user’s hand. This approach has the potential to advance the area of neurorehabilitation by providing a dynamic and adaptable platform for tailored therapy interventions aimed at restoring and improving hand motor function.

Table 1.
SRG system architecture.
2.2.1. SRG Prototype for SCI Participants
The initial prototype was designed and developed for the right hand of individuals with SCI. This SRG is designed to monitor, evaluate, and facilitate the challenges faced by SCI patients, including reduced muscle control and sensory deficits. A Qwiic Flex Glove Controller [34] attached to the index and middle fingers is connected with the Qwiic Flex Glove Controller attached to the ring and little fingers. The Qwiic Flex Glove Controller is connected to the microcontroller via the SparkFun Qwiic Shield’s Qwiic connection ports. One of the leads of each pressure sensor is connected to the power (3.3 V) and the other leads to the analog in of the microcontroller while a 10 kOhm pulldown resistor is connected between GND and the analog in. An sEMG Myoware Muscle Sensor’s (+) lead is connected to the power (3.3 V), the (−) lead is connected to ground and the signal lead is connected to the analog in of the microcontroller. In addition to the MSS suite, the system incorporates the SRPAS subsystem based on a PneuNet [32] flexible exoskeleton that applies controlled forces to the hand. The sensor and actuation technologies involved are sewn, attached and wired on the surface of an F.F. Group Antistatic Glove [35] as illustrated in Figure 2.
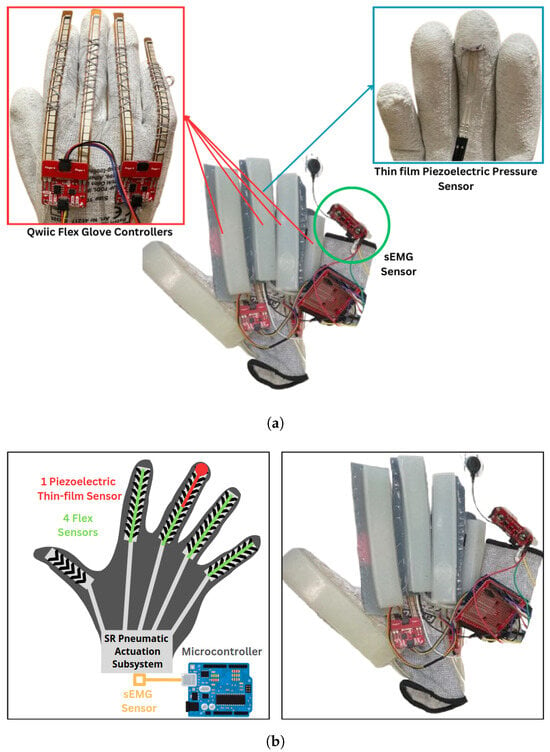
Figure 2.
SCI SRG prototype architecture: (a) MSS subsystem and (b) SRPAS subsystem.
2.2.2. SRG Prototype for Post-Stroke Participants
A revised prototype was developed to monitor the kinematics of both hands in post-stroke individuals while also providing targeted pneumatic assistance. These SRGs, integrate ten flex sensors positioned above and along the five fingers of each hand and four thin-film piezoelectric sensors mounted on each thumb and middle finger. The sensors are powered by a 5 V supply, with their output connected to the microcontroller’s analog inputs and stabilized by a 10 kOhm pulldown resistor between the ground and the analog input. Additionally, two sEMG Myoware Muscle Sensors are incorporated in each SRG, with each sensor’s positive terminal connected to 5 V, the negative terminal to ground, and the signal terminal linked to the corresponding microcontroller analog input. Furthermore, these SRG prototypes include two ADXL345 accelerometers interfaced with an Arduino Mega via the I2C bus (pins 20 and 21). To ensure proper communication, both sensors are wired in parallel on the SDA and SCL lines while sharing the same power and ground connections. Unique I2C addresses were assigned by connecting the AD0 pin of the first sensor to the ground (yielding the default address 0x53) and the AD0 pin of the second sensor to VCC (yielding the address 0x1D).
Complementing the MSS suite, the system also features the SRPAS subsystem, which employs a PneuNet flexible exoskeleton to apply controlled forces to the middle, index, and thumb fingers of each hand. The pneumatic actuation is provided by a single 2.5 lpm air pump that supplies the necessary pressure and a solenoid valve that regulates the airflow for inflation and deflation of the exoskeletons. The valve is controlled by a simple TIP120 transistor circuit—with an accompanying flyback diode for inductive load protection—and its operation is triggered either via the CoMSS or manually via an integrated push button. Power for the actuation components is derived from a regulated 6 V supply, ensuring stable and reliable operation. All sensor and actuation components are integrated into antistatic gloves, as illustrated in Figure 3.
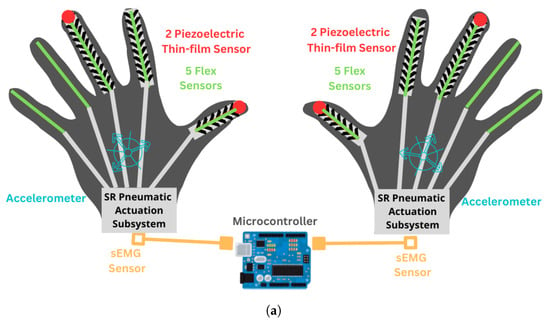
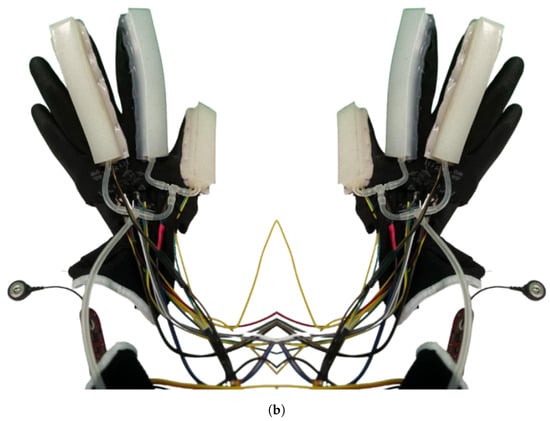
Figure 3.
Post-stroke SRGs: (a) architecture and (b) prototype.
2.3. Experimental Setup and Protocol
Three (3) male chronic SCI patients (ages 21, 62, 53) and three (3) male chronic stroke patients (ages 51, 54, 23) were recruited in the clinical trial protocols [36,37] and, after having obtained informed consent in accordance with the institutionally approved and published study protocol [28], they participated in the validation experiments during March 2024-March 2025. The participants, in addition to basic medical history, were evaluated using an array of clinical measures, which included (a) for SCI patients: the International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI) [38] and the Spinal Cord Independence Measure (g-SCIM-III) [39,40], and (b) for stroke patients: the Oxford Muscle Scale, the Stroke Impact Scale, version 3.0 (SIS) [41], the Modified Rankin Score-9Q (mRS-9Q) [42], the Timed Up and Go Test at 3 m (TUG) [43] and the Timed 10-Meter Walk Test [44]. Both groups of patients were administered the Modified Ashworth Scale (MAS) [45] and an array of neuropsychological questionnaires that included the Beck Anxiety Index (BAI) [46], the Beck’s Depression Inventory (BDI) [47,48], the Rosenberg Self-Esteem Scale (RSE) [49,50], the Apathy Evaluation Scale (AES) [51], the Vividness of Visual Imagery Questionnaire (VVIQ) [52] and the Kinesthetic and Visual Imagery Questionnaire (KVIQ [53]). The SCI participant evaluation is presented in Table 2 and the post-stroke participant evaluation is presented in Table 3.

Table 2.
Demographic, clinical, and neuropsychological evaluation of the SCI patient participants in the NeuroSuitUp protocol trials.

Table 3.
Demographic, clinical, and neuropsychological evaluation of the stroke patient participants in the HEROES protocol trials.
Participants reported no prior experience with wearable robotics or with serious game applications. They completed the experimental tasks as described below, taking place in the Thess-AHALL Living Lab [54] of the Medical Physics and Digital Innovation Laboratory. Afterward, they completed an array of questionnaires aiming to evaluate user experience (UX), which included perception of robotics through the GODSPEED Robotics Questionnaire [55,56], mental effort through the Subjective Mental Effort Questionnaire (SMEQ) [57], and discomfort through the Locally Experienced Discomfort Questionnaire (LED) [58]. Statistical analysis of the answers to the above questionnaires consisted of calculating medians (Mdns) and interquartile ranges (IQRs) for the SCI, stroke, and total participants, which are presented in Table 4 and reported as Mdn(IQR). The number of participants in each leg (3 SCI, 3 stroke, 6 in total) does not allow for further meaningful statistical comparisons, so discussion of those results was based on qualitative observations.

Table 4.
Perception of robotics, mental effort, discomfort and mental image capacity reported by the patient participants.
2.4. Data Acquisition and Analysis
Data for the SCI participants group were collected using the ComSS subsystem of the SRG measuring voltage outputs for flexion, pressure, and muscle activity while participants executed 6 repetitions of the Grasping exercises. Each session was timestamped, allowing for the correlation of events with specific time intervals. Categorical data indicating specific events during the exercise, including grasp events (e.g., “Grasp 0”, “Grasp 1”, etc.) and PAS subsystem valve states (e.g., “Valve OPEN”, “Valve CLOSED”) were also annotated. Similarly, data for the post-stroke participants were acquired using the ComSS subsystem integrated into dual SRGs, capturing voltage outputs from the MSS on both hands. Each data file adheres to a standardized format beginning with a timestamp in milliseconds and a phase indicator, followed by sensor readings for each hand. For example, the right-hand data include channels for finger flexion—renamed for clarity as RH_Flex_Thumb, RH_Flex_Index, RH_Flex_Middle, RH_Flex_Ring, and RH_Flex_Little—along with RH_Pressure_Thumb and RH_Pressure_Middle for pressure, RH_EMG_Raw for muscle activity, and acceleration channels (RH_AccelX, RH_AccelY, RH_AccelZ). The left-hand data mirror this structure with corresponding LH channels. During each session, participants performed three distinct grasping exercises, and the sessions were meticulously timestamped to allow precise correlation between sensor data and specific exercise intervals. In addition, categorical annotations were incorporated to mark key events, such as the initiation and completion of each exercise and the activation of the PAS subsystem, thereby enabling a detailed analysis of motor performance and recovery in post-stroke patients. All recorded data are stored in CSV files, ensuring standardized formatting and ease of access.
2.4.1. Data Preprossesing
The raw data were parsed from a text file and organized into a structured format (DataFrame) using the Python (version 3.10.12) Pandas library (version 2.2.3). Each entry included relevant fields, such as timestamp, event, valve state, sensor voltages, pressure, and EMG readings. The raw time data were converted to numeric values using Python’s (version 3.10.12) Pandas library (version 2.2.3). Any rows with missing or non-numeric time values were subsequently removed to ensure a continuous and reliable time base. Data were filtered by each exercise for each condition (non-actuated, right hand actuation, and left hand actuation). In order to facilitate comparison across conditions, the time series were synchronized by aligning the onset of the phase to t = 0. Due to potential variability between sensor channels and across participants, each sensor signal was normalized using z-score normalization. Specifically, for each sensor channel, the mean was subtracted and the result was divided by the channel’s standard deviation. For channels with zero variance, only the mean was subtracted. This normalization step ensured that differences in scale and sensor drift were minimized, thereby enabling a fair comparison of sensor responses across conditions.
2.4.2. Data Analysis
Data analysis was carried out in Python (version 3.10.12) using Pandas (version 2.2.3) for data handling and Seaborn (version 0.13.2) and Matplotlib (version 3.10.1) for all visualizations. Descriptive statistics—computing mean voltages for each sensor across all grasp events—were used to characterize overall trends and variability in the SCI cohort. Time-series line plots were then produced to depict flex and pressure sensor readings and EMG activity over the course of each exercise; these plots incorporated annotations for individual grasp events and vertical markers indicating valve state transitions, thereby improving interpretability. Finally, a comparative analysis of sensor outputs across successive grasp events was performed to evaluate the SRG’s influence on grasp performance and muscle activation.
Variations in sensor outputs across repeated ball-grasping exercises were first examined to evaluate the SRG’s effect on grasp performance and muscle activation in the SCI cohort. In the post-stroke group, we extended this analysis by extracting both temporal and spectral features from the recorded signals. Time-domain metrics for the flex sensors included peak amplitude—the maximum voltage attained during each grasp phase—while oscillatory recordings from the sEMG and accelerometer channels were subjected to Fast Fourier Transform to yield frequency-domain descriptors: the dominant frequency (Hz) at which spectral magnitude peaked and the total power () summed across the spectrum, providing a quantitative measure of overall signal energy.
Principal Component Analysis (PCA) was performed on the flex peak amplitude and sEMG/accelerometer frequency-domain features. This multivariate approach allowed the exploration of the overall sensor response space and the assessment of whether the frequency profiles of post-stroke participants differed across conditions. PCA facilitated visualization of potential clustering by condition in a reduced dimensional space.
3. Results
The participants’ perceptions of the robotics, mental effort, and discomfort are presented in Table 4.
3.1. SCI Participants
Table 5, Table 6 and Table 7 summarize the mean sensor readings collected during the ball-grasping exercises illustrated in Figure 4, Figure 5, Figure 6, Figure 7 and Figure 8, as performed by participants wearing the SRG. For each grasp event—labeled sequentially in the “Event” column—the mean values were calculated over a 25s interval while the pneumatic valve remained in the “OPEN” state. Each table reports the following variables: the exact recording time (“Timestamp”), the grasp event identifier (“Event”), and the valve’s operational status (“Valve State”); four digit-specific sensor voltages (“Index,” “Middle,” “Ring,” and “Pinky”); the mean pressure voltage applied by the middle finger (“Pressure”); and the average sEMG amplitude reflecting underlying muscle activity (“EMG”).

Table 5.
Ball grasping exercise—mean NSU-01-001.

Table 6.
Ball grasping exercise—mean NSU-02-001.

Table 7.
Ball grasping exercise—mean NSU-02-002.
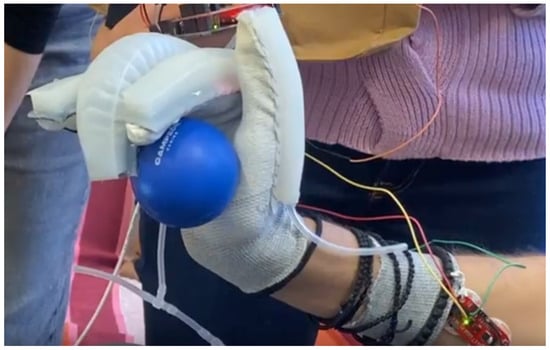
Figure 4.
Ball grasping exercise NSU-01-001.
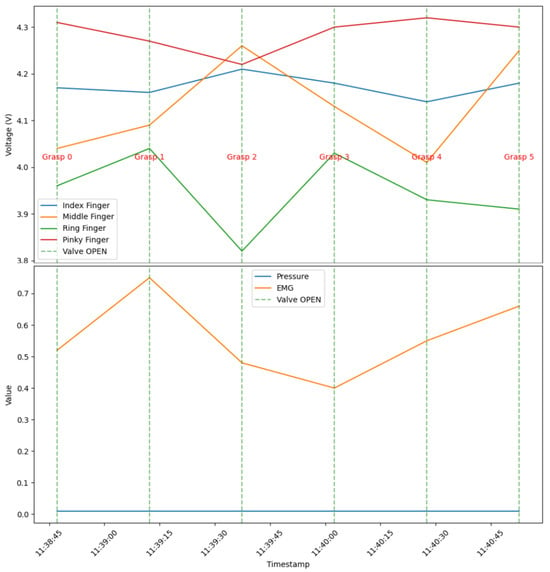
Figure 5.
Ball grasping exercise—mean NSU-01-001.

Figure 6.
Ball grasping exercise NSU-02-001.
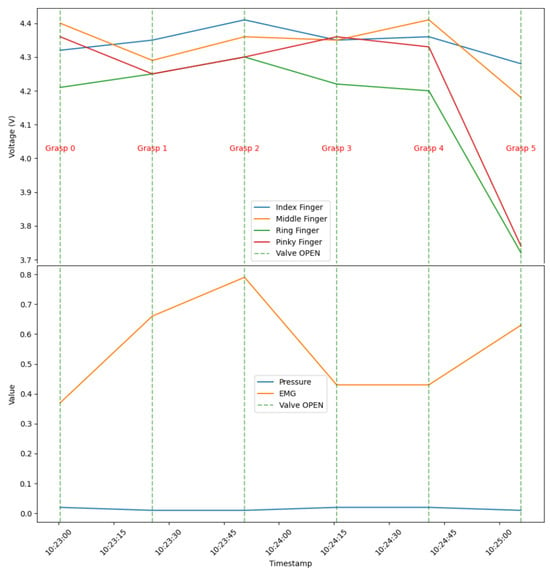
Figure 7.
Ball grasping exercise—mean NSU-02-001.
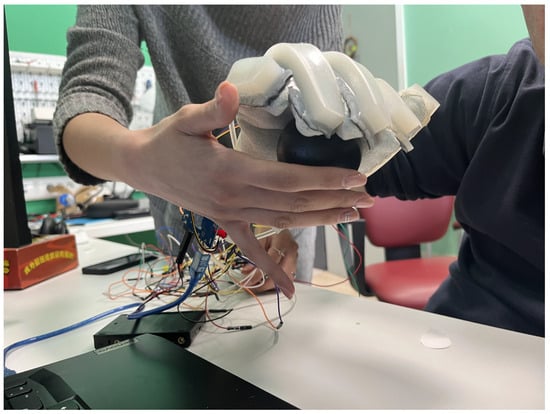
Figure 8.
Ball grasping exercise NSU-02-002.
These mean values provide critical insights into the performance and functionality of the soft robotic glove during the exercises, allowing for a comprehensive assessment of each finger’s response while the valve was open. By illustrating these averages (Figure 5, Figure 7, Figure 9), the study aims to evaluate the effectiveness of robotic assistance in enhancing grasping ability among participants.
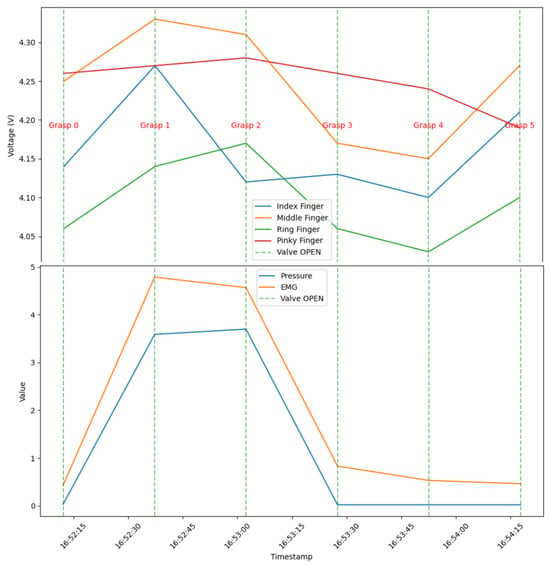
Figure 9.
Ball grasping exercise—mean NSU-02-002.
3.2. Post-Stroke Participants
In the post-stroke cohort, sensor data were analyzed across three conditions—non-actuated, left-actuated, and right-actuated—to evaluate how the SRPAS assistance modulates hand function during the three grasping tasks: Ball grasping (Figure 10, Figure 11, Figure 12, Figure 13 and Figure 14; Table 8, Table 9 and Table 10), glass grip (Figure 15, Figure 16, Figure 17, Figure 18 and Figure 19; Table 11, Table 12 and Table 13), paper grip (Figure 20, Figure 21, Figure 22, Figure 23, Figure 24 and Figure 25; Table 14, Table 15 and Table 16). Figures of flex sensor peak amplitude for all participants and exercises (Figure 10, Figure 15 and Figure 21) illustrate distinct patterns of grip strength, while FFT spectral plots (Figure 11, Figure 12 and Figure 13, Figure 16, Figure 17 and Figure 18, Figure 22, Figure 23 and Figure 24) reveal differences in the frequency content of the signals, indicating shifts in dominant frequencies and power distributions under actuated conditions. Additionally, for each exercise time and frequency domain features were calculated (Table 8, Table 9, Table 10, Table 11, Table 12, Table 13, Table 14, Table 15 and Table 16) and PCA plots (Figure 14, Figure 19 and Figure 25) performed demonstrating that the overall sensor response space separates the conditions, further supporting the observation that actuation alters neuromuscular activation. Collectively, these results underscore the potential of the SRG system to improve motor performance in post-stroke individuals by modulating both the temporal and spectral characteristics of the collected MSS signals.
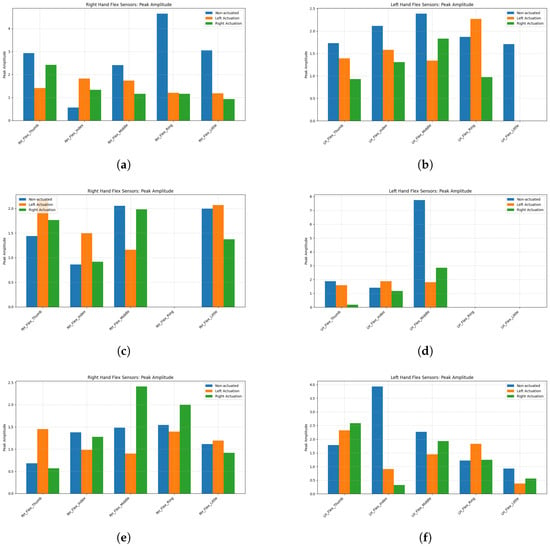
Figure 10.
Flex peak amplitude—ball grasping: (a) HER-01-001 right hand; (b) HER-01-001 left hand; (c) HER-02-001 right hand; (d) HER-02-001 left hand; (e) HER-02-002 right hand; (f) HER-02-002 left hand.
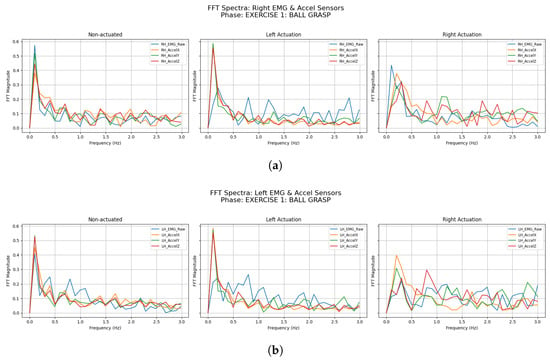
Figure 11.
HER-01-001—EMG and accelerometer data FFT spectra—ball grasping: (a) right hand and (b) left hand.
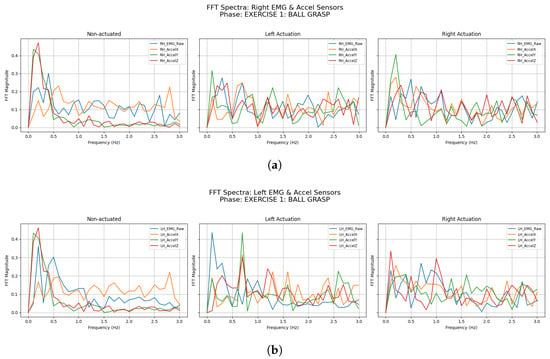
Figure 12.
HER-02-001—EMG and accelerometer data FFT spectra—ball grasping: (a) right hand and (b) left hand.
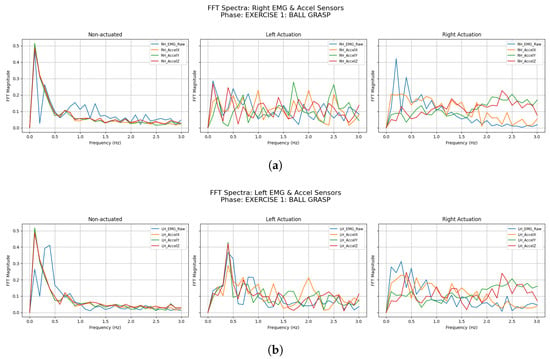
Figure 13.
HER-02-002—EMG and accelerometer data FFT spectra—ball grasping: (a) right hand and (b) left hand.
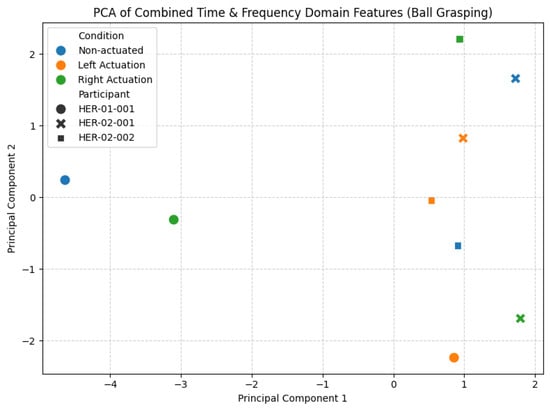
Figure 14.
Ball grasping exercise—PCA time and frequency domain features.

Table 8.
Time-domain peak amplitude features for flex and pressure sensors—ball grasping exercise.

Table 9.
Frequency-domain features for accelerometer sensors—ball grasping exercise.

Table 10.
Frequency-domain features for EMG sensors—ball grasping exercise.
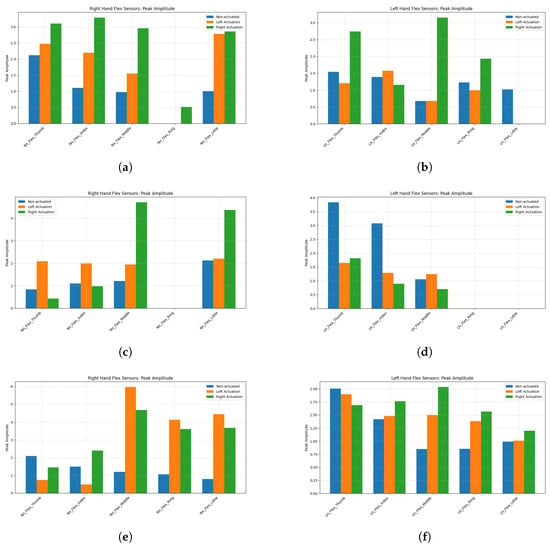
Figure 15.
Flex peak amplitude—glass grip: (a) HER-01-001 right hand; (b) HER-01-001 left hand; (c) HER-02-001 right hand; (d) HER-02-001 left hand; (e) HER-02-002 right hand; (f) HER-02-002 left hand.
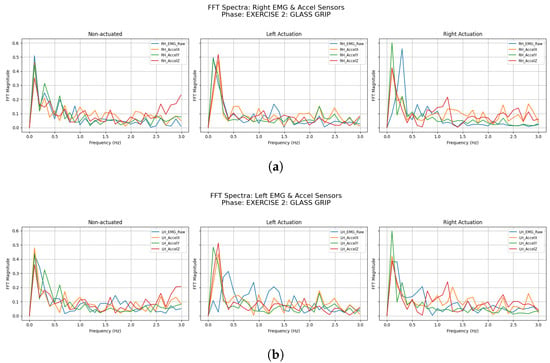
Figure 16.
HER-01-001—EMG and accelerometer data FFT spectra—glass grip: (a) right hand and (b) left hand.
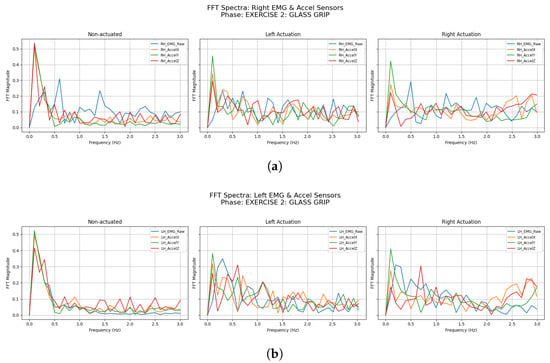
Figure 17.
HER-02-001—EMG and accelerometer data FFT spectra—glass grip: (a) right hand and (b) left hand.
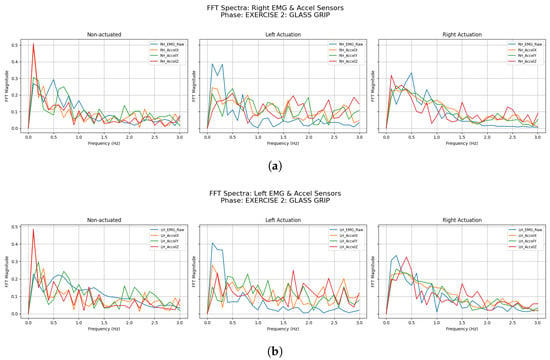
Figure 18.
HER-02-002—EMG and accelerometer data FFT spectra—glass grip: (a) right hand and (b) left hand.
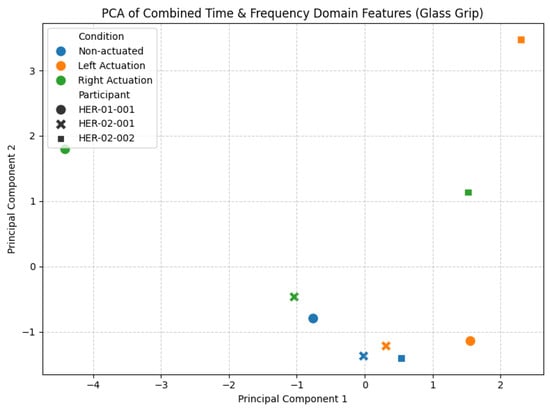
Figure 19.
Glass grip exercise—PCA time and frequency domain features.

Table 11.
Time-domain peak amplitude feature for flex sensors—glass grip.

Table 12.
Frequency-domain features for accelerometer sensors—glass grip.

Table 13.
Frequency-domain features for EMG sensors—glass grip.
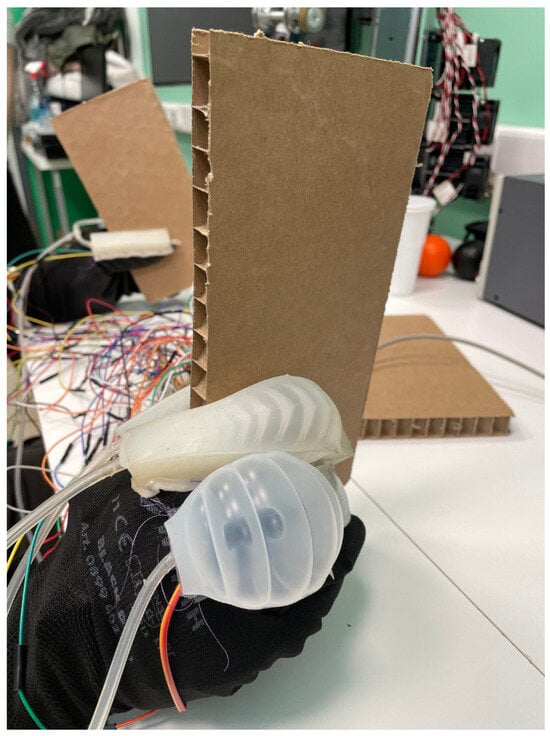
Figure 20.
Paper grip—exercise example.
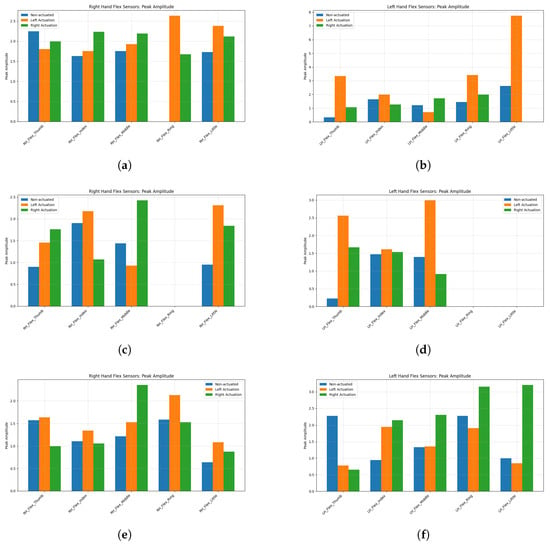
Figure 21.
Flex peak amplitude—paper grip: (a) HER-01-001 right hand; (b) HER-01-001 left hand; (c) HER-02-001 right hand; (d) HER-02-001 left hand; (e) HER-02-002 right hand; (f) HER-02-002 left hand.
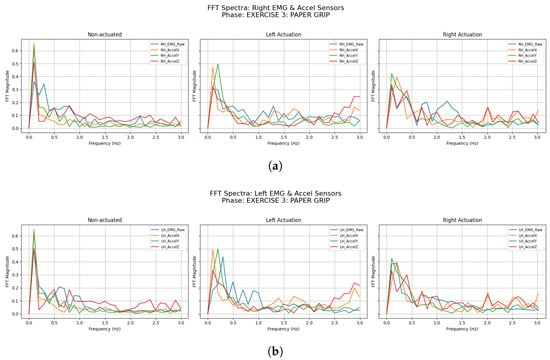
Figure 22.
HER-01-001—EMG and accelerometer data FFT spectra—paper grip: (a) right hand and (b) left hand.
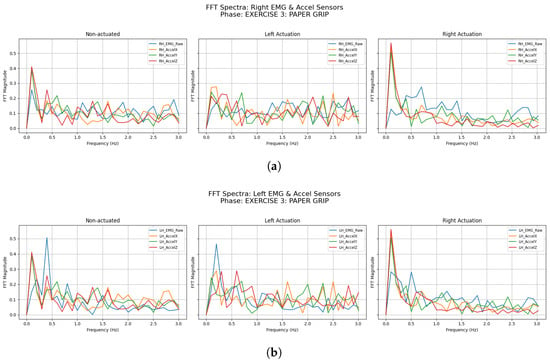
Figure 23.
HER-02-001—EMG and accelerometer data FFT spectra—paper grip: (a) right hand and (b) left hand.
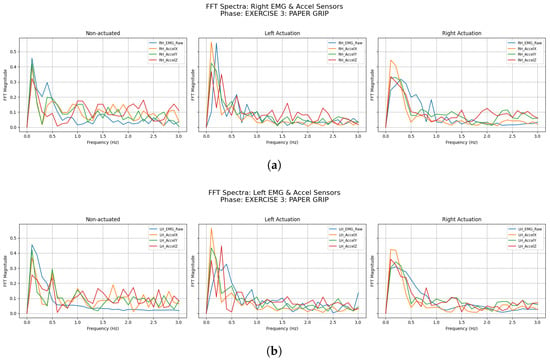
Figure 24.
HER-02-002—EMG and accelerometer data FFT spectra—paper grip: (a) right hand and (b) left hand.
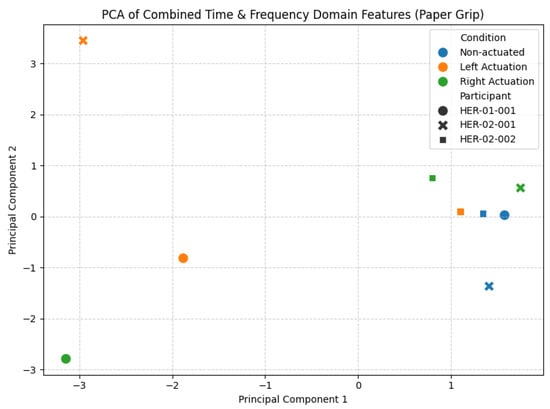
Figure 25.
Paper grip exercise—PCA time and frequency domain features.

Table 14.
Flex sensor time-domain features for flex sensors—paper grip.

Table 15.
Frequency-domain features for accelerometer sensors—paper grip.

Table 16.
Frequency-domain features for EMG sensors—paper grip.
3.2.1. Ball Grasping
The ball grasping exercise was designed to assess the participant’s ability to generate and modulate grip force in a simple, spherical object manipulation. During each trial, subjects reached for and closed their hand around a standardized 5-cm diameter soft ball, allowing measurement of flex-sensor peak amplitude as an index of maximal voluntary contraction. By comparing non-actuated, left-actuated, and right-actuated conditions, we quantified how the SRPAS assistance affects the grasping generation. Time-domain features and frequency-domain characteristics were extracted from each trial and subsequently projected into PCA plots to visualize shifts in the sensor response under different actuation states. This introductory analysis lays the groundwork for understanding the neuromuscular adaptations induced by SRG assistance in post-stroke hand function rehabilitation.
3.2.2. Glass Grip
The glass grip exercise measured how well participants flex their fingers around a cylindrical object resembling a drinking glass. Participants reached out and wrapped their fingers around a 6 cm–diameter, 10 cm–tall cardboard tube engineered to simulate the feel and weight of a filled glass. We compared trials without actuation to those with left-side and right-side assistance from the SRPAS to see if and how the device alters grip coordination. From each trial, we extracted both time-domain and frequency-domain features, then used PCA to reveal clear groupings of sensor patterns under each condition.
3.2.3. Paper Grip
In the paper grip exercise, participants used their fingers as visualized in Figure 20 to lift and hold two cardboard papers. We ran this under three conditions—no actuation, left-side SRPAS assistance, and right-side assistance—to explore how the device influences the performance of this grip. From each trial, we extracted time-domain measures and frequency-domain descriptors. A PCA of these features then revealed clear grouping of sensor responses by condition, highlighting how actuation assists the hand coordination in this grip.
Finally, to explore the monotonic relationships between participants’ subjective ratings and their biomechanical signals, we computed Spearman rank-order correlations across all six participants, the the results of which are presented in Figure 26 below.
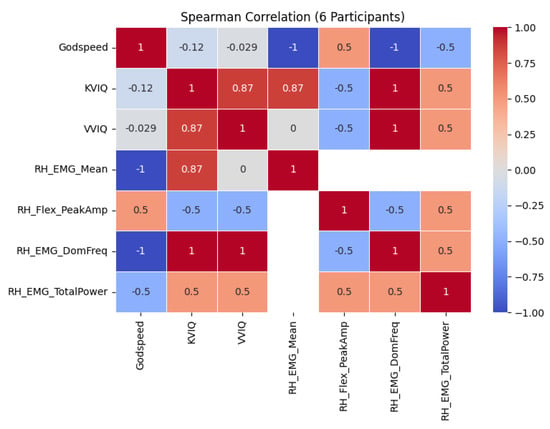
Figure 26.
Spearman correlation of participant data.
4. Discussion
The findings presented in this manuscript provide a thorough investigation of grasping task performance among SCI and stroke patients, with the SRPAS that we developed assisting with each task. All participants in our study had established chronic impaired function of the hands (at least 18 months old) and plateaued during their rehabilitation process. SCI participants had impaired function of both hands with UEMS ranging from 22/50 to 40/50 and one among them demonstrated a complete injury. Similarly, stroke participants had their affected hand’s muscle function evaluated with the Oxford scale from 0 to 4+, with one participant being left-side plegic. Due to their lesions, the patients demonstrated varied levels of spasticity of the affected hands, ranging from 1 to 4 in the MAS, further impairing their achievable ROM during hand-related activities and SRPAS-assisted tasks.
The tasks involved in our investigation were designed to resemble ADLs [6,29,59,60], such as repeated and intermittent performing of spherical, cylindrical, and lumbrical gripping, using objects such as balls, glass and paper. Our SCI participants’ disability was documented through the SCIM questionnaire, where their scores in the self-care category indicated severe to moderate disability [61,62], ranging from 7 to 16 out of 20. Similarly, the disability of our stroke participants was validated through SIS [63,64], where their cores in the hand domain ranged from 0% to 70% and their scores in the ADL domain ranged from 37.5% to 57.5%. As a result of their impaired motor function, these individuals would not have been able to complete the activities using their affected hands, without the mechanical assistance provided by the SRPAS. The finger flexion values that we acquired for the index, middle, ring, and pinky fingers demonstrate a stable and consistent grip performance, which was made feasible using pneumatic actuation. The relatively uniform flexion across different fingers emphasizes the necessity of this external mechanical help in allowing coordinated finger motions in order to compensate for the lack of individual motor control and reduced ROM.
The piezoelectric pressure and sEMG measurements demonstrate the relevance of pneumatic actuation in grasping performance. The increased pressure values recorded, notably during Events 1 and 2, suggest that the SRPAS was actively aiding the SCI participants’ grasp. This increased pressure shows that the actuation delivered the necessary mechanical force, allowing participants to execute a task that would otherwise be impossible for them to achieve unaided. The sEMG data, which correlate to muscle activation, demonstrate that, while the patients exerted some muscular activity, the robotic aid took on a significant portion of the effort, as reflected in the low-to-moderate sEMG values in relation to the task’s mechanical demands.
Figure 14, Figure 15, Figure 16, Figure 17, Figure 18, Figure 19, Figure 20, Figure 21, Figure 22, Figure 23, Figure 24 and Figure 25 present PCA projections of combined time-domain (flex peak amplitude) and frequency-domain (sEMG/accelerometer dominant frequency, total power) features for each exercise and actuation condition. In all plots, PC1 and PC2 capture the largest and second-largest portions of variance, respectively. Color coding denotes non-actuated, left-actuated, and right-actuated trials, while marker shapes distinguish participants. In the ball-grasping PCA (Figure 14), actuated conditions generally form clusters distinct from non-actuated trials, indicating that pneumatic assistance alters both neuromuscular and kinematic signatures—though separation varies by participant. The glass-grip PCA (Figure 19) shows similar patterns: some participants’ actuated data shift clearly along PC axes, while others overlap, reflecting individual grasp strategies. Finally, the paper-grip PCA (Figure 25) again reveals that actuation shifts sensor profiles for certain participants but not others. Together, these results demonstrate that assistive actuation consistently modifies sensor--feature space, yet the magnitude and direction of those changes are highly participant-specific.
As we aim to get more patients enrolled in the NeuroSuitUp and HEROES studies, we will attempt to investigate the effect of the patients’ measured neuropsychological properties on the performance during robotic use and on the neural rehabilitation process. A total of 15 SCI patients and 35 stroke patients are expected to be recruited by the end of the clinical trials, when the development of the final versions of robotic devices is concluded, allowing for meaningful statistical investigations. In this evaluation study, both the SCI and stroke patients demonstrated no apathy, anxiety, depression, or low-self-esteem traits. SCI patients reported a high degree of capacity for mental imagery with VVIQ scores of 80 (0.5) and KVIQ scores of 50 (0). On the other hand, stroke patients reported a decrease in vividness (55 (9)) and in kinesthetic/visual motor imagery (39 (17)) that was, interestingly, uniform with regard to their affected and unaffected hands. The only measurable comparable clinical difference between the two groups can be explored through spasticity levels. The SCI patients scored lower MAS UE levels (1, 1+, 2) in relation to the stroke patients who exhibited higher UE spasticity (MAS 4, 2, 3). The difference was evident during the SRPAS fitting, where it was notably more difficult to fit the device on the spastic-affected hands of the stroke participants. Spasticity has been traditionally documented to be a maladaptive plastic [65] compensation and an important target of mitigation through rehabilitation [66], but newer evidence does not necessarily correlate it to worse functional outcomes [67,68]. The relation of spasticity and poor visualization of movement is even less well understood, but the restriction of movement caused by spasticity should be further investigated as potentially harmful to movement visualization and recovery [69].
The groups of patients that participated in our study commented favorably upon their experience and interaction with the robotics [70,71], both qualitatively and through quantitative scales. Participants experienced very low discomfort levels (most 0 at LED) and reported generally low mental effort (0-10, with only one stroke patient reporting 70 at SMEQ). With regards to their perception of the robotics’ characteristics, SCI and stroke participants both reported high Likeability (20 (3) and 17 (6.5), respectively), high perceived intelligence (15 (3.5) and 17 (8), respectively) and maximum perceived safety (15 (0) both groups) at the Godspeed Robotics Questionnaire [72]. They also reported the SRPAS as moderately anthropomorphic (9 (2) and 13 (1.5), respectively), showing moderate animosity (13 (2.5) and (15 (3.5), respectively) and, in general, Godspeed scores comparable to our previous investigations [28,29].
Spearman rank-order correlations (Figure 26) showed that imagery scales (KVIQ, VVIQ) were strongly and positively associated with EMG features—participants with higher imagery vividness exhibited greater mean EMG activity and higher EMG dominant frequencies—whereas Godspeed scores flipped the sign, correlating negatively with EMG but positively with flex peak amplitude, such that better robot perception accompanied larger peak flexion yet lower sustained muscle activity. However, with this limited number of participants, even “perfect” values are almost certainly driven by this binary grouping rather than a continuous, generalizable sensor–questionnaire relationship.
5. Conclusions
The study presented in this manuscript demonstrates that the proposed SRG prototypes can modify sensor-derived features during grasping tasks, ultimately enhancing hand function in individuals with severe motor impairments. In participants with SCI, the SRG facilitated coordinated finger movements by providing consistent and stable pneumatic support. Analyses of finger flexion in the time domain revealed uniform and reliable grip performance across the index, middle, ring, and pinky fingers—a crucial outcome for individuals with compromised motor control.
For the post-stroke participant group, although baseline sensor readings and feature values differed from those in the SCI cohort, the SRPAS similarly induced significant changes in both time- and frequency-domain metrics. Actuation influenced key time-domain features, such as peak amplitude, while frequency-domain measures—namely dominant frequency and total power—revealed changes in the energy distribution of EMG and accelerometer signals. PCA illustrated systematic differences between non-actuated and actuated conditions. Despite greater variability among post-stroke participants, these outcomes underscore the potential of SRGs to modulate neuromuscular and kinematic patterns even in cases of heterogeneous motor deficits.
Overall, the proposed SRGs offer a promising approach to enhance hand function by dynamically altering the sensor profiles associated with grasping tasks. The marked improvements observed in the SCI group, along with the encouraging yet individualized responses in the post-stroke group, highlight the importance of personalized device calibration. We should carefully place the importance of our findings on the feasibility and usability of the SRG under the scope of limiting factors, especially the small number of subjects (three SCI and three stroke patients) that participated in this preliminary study. While some conclusions regarding the promise of the approach can be drawn, no sub-group analysis, including gender analysis, no extensive statistical analysis with regards to injury severity, chronicity, side or level of lesion, and few meaningful comparisons between the two groups of patients can be conducted, except for qualitative observations. Similarly, the current work focused on preliminary analyses of feasibility, usability, and user experience rather than statistical analysis of efficacy and performance against healthy control subjects.
Furthermore, the post-stroke results indicate that although each participant exhibits unique sensor “signatures,” a noticeable shift in feature space occurs between different actuation states—particularly when both time- and frequency-domain features are considered together. Future work of the proposed project’s development will include integration of kinematic and dynamic modeling of human hand and glove complex into the control scheme, use of normative sEMG [73] value ranges [74] for thresholding assistive levels, and integrating and optimizing electrical stimulation in a hybrid actuation scheme for the arm and hand, integrating sensor-derived metrics with clinical performance measures—such as grip strength and task success rates—to further optimize the device’s therapeutic impact across diverse patient populations. More importantly, the conduction and conclusion of the two registered clinical trials, involving SCI and stroke patients, as well as age- and sex-matched healthy control participants will allow for meaningful statistical analyses with regards to the patient demographics, clinical information, neuropsychological evaluations and extensive performance metrics. Only such analyses will allow us to accurately evaluate and discuss the rehabilitative effect of the platform of devices, and the SRG.
Author Contributions
Conceptualization, V.F., K.M. and A.A. (Alkinoos Athanasiou); Data curation, V.F., K.M., K.K., V.M. and V.P.; Formal analysis, V.F., K.M. and A.A. (Alkinoos Athanasiou); Funding acquisition, P.D.B. and A.A. (Alkinoos Athanasiou); Investigation, V.F., K.M., K.N., K.K, V.M., V.P., P.A., K.T., A.A. (Alexander Astaras) and A.A. (Alkinoos Athanasiou); Methodology, V.F., K.M. and A.A. (Alkinoos Athanasiou); Project administration, P.D.B. and A.A. (Alkinoos Athanasiou); Resources, A.A. (Alexander Astaras), P.D.B. and A.A. (Alkinoos Athanasiou); Software, V.F., K.M., P.A. and K.T.; Supervision, P.D.B., A.A. (Alexander Astaras) and A.A. (Alkinoos Athanasiou); Validation, V.F., K.M. and A.A. (Alkinoos Athanasiou); Visualization, V.F. and K.M.; Writing—original draft, V.F., K.M., K.N., V.P. and A.A. (Alkinoos Athanasiou); Writing—review and editing, V.F., K.M., K.N., V.M., V.P., P.A., K.T., M.G.T., A.A. (Alexander Astaras), P.D.B. and A.A. (Alkinoos Athanasiou). All authors have read and agreed to the published version of the manuscript.
Funding
This research project was supported by the Hellenic Foundation for Research and Innovation (H.F.R.I.) https://www.elidek.gr (accessed on 30 April 2024) under the “2nd Call for H.F.R.I. Research Projects to support Faculty Members & Researchers” (Project Number: 4391).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The NeuroSuitUp protocol was approved by the Committee for Bioethics and Ethics of the School of Medicine, Aristotle University of Thessaloniki with the protocol number 188117/2022 in the Committee sitting 68/13-7-2022 following the application with the protocol number 165080/2022. The HEROES protocol was approved by the Committee for Bioethics and Ethics of the School of Medicine, Aristotle University of Thessaloniki with the protocol number 266604/2022 in the Committee sitting 73/12-10-2022 following the application with the protocol number 243371/2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data from the NeuroSuitUp and HEROES studies will be made publicly available after the completion of the projects and will be accessible through their respective institutional project web pages under an Attribution-NonCommercial-NoDerivatives 4.0 International license. Data of the analysis presented in the current manuscript and the related code can be made available via a request to the authors following a Memorandum of Understanding (MoU) in the context of Open Research Initiative.
Acknowledgments
We would like to thank the following members of the Biomedical Electronics Robotics and Devices (BERD) research group of the Medical Physics and Digital Innovation Laboratory, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki (Athanasios Arvanitidis, Maria Giouvanoglou, Alexandros Moraitopoulos, Niki Pandria, Theodore Savvidis and Magda Anastasiadou) who are collaborators in the NeuroSuitUp and HEROES projects but were not listed as authors in this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest. The funding body had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| ADLs | Activities of Daily Living |
| AES | Apathy Evaluation Scale |
| BAI | Beck Anxiety Index |
| BDI | Beck’s Depression Inventory |
| ComSS | Communication Software Subsystem |
| DoF | Degrees of Freedom |
| EMS | Electrical Muscle Stimulation |
| g-SCIM-III | Spinal Cord Independence Measure |
| IMUs | Inertial Measurement Units |
| ISNCSCI | International Standard for Neurological Classification of Spinal Cord Injury |
| KVIQ | Kinesthetic and Visual Imagery Questionnaire |
| MAS | Modified Ashworth Scale |
| MSS | Multi-Sensor Subsystem |
| PCA | Principal Component Analysis |
| QoL | Quality of Life |
| ROS | Robot Operating System |
| RSE | Rosenberg Self-Esteem Scale |
| SCI | Spinal Cord Injury |
| sEMG | Surface Electromyography |
| SR | Soft Robotics |
| SRG(s) | Soft Robotic Glove(s) |
| SRPAS | Soft Robotic Pneumatic Actuation Subsystem |
| VVIQ | Vividness of Visual Imagery Questionnaire |
References
- Fuglevand, A.J. Mechanical properties and neural control of human hand motor units. J. Physiol. 2011, 589, 5595–5602. [Google Scholar] [CrossRef] [PubMed]
- Metcalf, C.D.; Irvine, T.A.; Sims, J.L.; Wang, Y.L.; Su, A.W.; Norris, D.O. Complex hand dexterity: A review of biomechanical methods for measuring musical performance. Front. Psychol. 2014, 5, 414. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Qi, Y.; Wu, X.; Zhu, J.; Zhang, J.; Wang, Y. Decoding Joint-Level Hand Movements With Intracortical Neural Signals in a Human Brain–Computer Interface. IEEE Trans. Cogn. Dev. Syst. 2024, 16, 2100–2109. [Google Scholar] [CrossRef]
- Vanderkolff, S.M.; Maibauer, I.; Amin, N. Beyond sight: Environmental interaction with the hands or feet? J. Neurophysiol. 2025, 133, 622–624. [Google Scholar] [CrossRef]
- Paraskevopoulos, E.; Herholz, S. Multisensory integration and neuroplasticity in the human cerebral cortex. Transl. Neurosci. 2013, 4, 337–348. [Google Scholar] [CrossRef]
- Dollar, A.M. Classifying human hand use and the activities of daily living. In The Human Hand as an Inspiration for Robot Hand Development; Springer International Publishing: Cham, Switzerland, 2014; pp. 201–216. [Google Scholar] [CrossRef]
- Wang, H.; Arceo, R.; Chen, S.; Ding, L.; Jia, J.; Yao, J. Effectiveness of interventions to improve hand motor function in individuals with moderate to severe stroke: A systematic review protocol. BMJ Open 2019, 9, e032413. [Google Scholar] [CrossRef]
- Nam, H.U.; Huh, J.S.; Yoo, J.N.; Hwang, J.M.; Lee, B.J.; Min, Y.S.; Kim, C.H.; Jung, T.D. Effect of dominant hand paralysis on quality of life in patients with subacute stroke. Ann. Rehabil. Med. 2014, 38, 450–457. [Google Scholar] [CrossRef]
- Rivers, C.S.; Fallah, N.; Noonan, V.K.; Whitehurst, D.G.; Schwartz, C.E.; Finkelstein, J.A.; Craven, B.C.; Ethans, K.; O’Connell, C.; Truchon, B.C.; et al. Health conditions: Effect on function, health-related quality of life, and life satisfaction after traumatic spinal cord injury. A prospective observational registry cohort study. Arch. Phys. Med. Rehabil. 2018, 99, 443–451. [Google Scholar] [CrossRef]
- Hmaied Assadi, S.; Barel, H.; Dudkiewicz, I.; Gross-Nevo, R.F.; Rand, D. Less-affected hand function is associated with independence in daily living: A longitudinal study poststroke. Stroke 2022, 53, 939–946. [Google Scholar] [CrossRef]
- Lili, L.; Sunnerhagen, K.S.; Rekand, T.; Alt Murphy, M. Independence and upper extremity functioning after spinal cord injury: A cross-sectional study. Sci. Rep. 2023, 13, 3148. [Google Scholar] [CrossRef]
- World Health Organization. Spinal Cord Injury: Fact Sheets. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury (accessed on 29 September 2024).
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.O.; Pandian, J.; Lindsay, P.; Grupper, M.; Rautalin, I. World Stroke Organization: Global Stroke Fact Sheet 2025. Int. J. Stroke 2025, 20, 132–144. [Google Scholar] [CrossRef] [PubMed]
- WHO EMRO | Stroke, Cerebrovascular Accident | Health Topics — emro.who.int. Available online: https://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html (accessed on 3 April 2025).
- CDC. Stroke Facts — cdc.gov. Available online: https://www.cdc.gov/stroke/data-research/facts-stats/index.html (accessed on 3 April 2025).
- Gherman, B.; Zima, I.; Vaida, C.; Tucan, P.; Pisla, A.; Birlescu, I.; Machado, J.; Pisla, D. Robotic Systems for Hand Rehabilitation—Past, Present and Future. Technologies 2025, 13, 37. [Google Scholar] [CrossRef]
- Perera, O.; Liyanapathirana, R.; Gargiulo, G.; Gunawardana, U. A Review of Soft Robotic Actuators and Their Applications in Bioengineering, with an Emphasis on HASEL Actuators’ Future Potential. Actuators 2024, 13, 524. [Google Scholar] [CrossRef]
- Hong, R.; Li, B.; Bao, Y.; Liu, L.; Jin, L. Therapeutic robots for post-stroke rehabilitation. Med Rev. 2024, 4, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.; Sierro, T.; Niu, T.; Sarino, M.E.; Sarrafzadeh, M.; McArthur, D.; Edgerton, V.R.; Lu, D.C. Rehabilitation of hand function after spinal cord injury using a novel handgrip device: A pilot study. J. Neuroeng. Rehabil. 2017, 14, 22. [Google Scholar] [CrossRef]
- Marek, K.; Redlicka, J.; Miller, E.; Zubrycki, I. Objectivizing Measures of Post-Stroke Hand Rehabilitation through Multi-Disciplinary Scales. J. Clin. Med. 2023, 12, 7497. [Google Scholar] [CrossRef] [PubMed]
- Edemekong, P.F.; Bomgaars, D.L.; Sukumaran, S.; Schoo, C. Activities of Daily Living; StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Ragnarsson, K.T. Functional electrical stimulation after spinal cord injury: Current use, therapeutic effects and future directions. Spinal Cord 2007, 46, 255–274. [Google Scholar] [CrossRef]
- Maggio, M.G.; Bonanno, M.; Manuli, A.; Calabrò, R.S. Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway. Brain Sci. 2024, 14, 140. [Google Scholar] [CrossRef]
- Smith, S.N.; Crocker, A.F. Experiential learning in physical therapy education. Adv. Med. Educ. Pract. 2017, 8, 427–433. [Google Scholar] [CrossRef]
- Osuagwu, B.A.; Timms, S.; Peachment, R.; Dowie, S.; Thrussell, H.; Cross, S.; Shirley, R.; Segura-Fragoso, A.; Taylor, J. Home-based rehabilitation using a soft robotic hand glove device leads to improvement in hand function in people with chronic spinal cord injury:a pilot study. J. Neuroeng. Rehabil. 2020, 17, 40. [Google Scholar] [CrossRef]
- Polygerinos, P.; Wang, Z.; Galloway, K.C.; Wood, R.J.; Walsh, C.J. Soft robotic glove for combined assistance and at-home rehabilitation. Robot. Auton. Syst. 2015, 73, 135–143. [Google Scholar] [CrossRef]
- Proulx, C.E.; Beaulac, M.; David, M.; Deguire, C.; Haché, C.; Klug, F.; Kupnik, M.; Higgins, J.; Gagnon, D.H. Review of the effects of soft robotic gloves for activity-based rehabilitation in individuals with reduced hand function and manual dexterity following a neurological event. J. Rehabil. Assist. Technol. Eng. 2020, 7, 205566832091813. [Google Scholar] [CrossRef]
- Athanasiou, A.; Mitsopoulos, K.; Praftsiotis, A.; Astaras, A.; Antoniou, P.; Pandria, N.; Petronikolou, V.; Kasimis, K.; Lyssas, G.; Terzopoulos, N.; et al. Neurorehabilitation Through Synergistic Man–Machine Interfaces Promoting Dormant Neuroplasticity in Spinal Cord Injury: Protocol for a Nonrandomized Controlled Trial. JMIR Res. Protoc. 2022, 11, e41152. [Google Scholar] [CrossRef] [PubMed]
- Mitsopoulos, K.; Fiska, V.; Tagaras, K.; Papias, A.; Antoniou, P.; Nizamis, K.; Kasimis, K.; Sarra, P.D.; Mylopoulou, D.; Savvidis, T.; et al. NeuroSuitUp: System Architecture and Validation of a Motor Rehabilitation Wearable Robotics and Serious Game Platform. Sensors 2023, 23, 3281. [Google Scholar] [CrossRef]
- Fardipour, S.; Hadadi, M. Investigation of therapeutic effects of wearable robotic gloves on improving hand function in stroke patients: A systematic review. Curr. J. Neurol. 2022, 21, 125. [Google Scholar] [CrossRef]
- Fiska, V. Development of a Wearable Exoskeletal Device Based on Multi-Sensor Data Fusion & Soft Robotics for Neural Rehabilitation of the Human Hand. Master’s Thesis, Aristotle University of Thessaloniki, Thessaloniki, Greece, 2022. [Google Scholar]
- Polygerinos, P.; Lyne, S.; Wang, Z.; Nicolini, L.F.; Mosadegh, B.; Whitesides, G.M.; Walsh, C.J. Towards a soft pneumatic glove for hand rehabilitation. In Proceedings of the 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems, Tokyo, Japan, 3–7 November 2013; pp. 1512–1517. [Google Scholar] [CrossRef]
- Manns, M.; Morales, J.; Frohn, P. Additive manufacturing of silicon based PneuNets as soft robotic actuators. Procedia CIRP 2018, 72, 328–333. [Google Scholar] [CrossRef]
- SparkFun Electronics. SparkFun Qwiic Flex Glove Controller. Available online: https://www.sparkfun.com/products/14666 (accessed on 29 September 2024).
- FF Group. Antistatic PU Coated Gloves with Polyester Carbon Fiber Knitting. Available online: https://products.ffgroup-toolindustries.com/product/4888/antistatic-pu-coated-gloves-with-polyester-carbon-fiber-knitting (accessed on 29 September 2024).
- ClinicalTrials.gov, I.N. NeuroSuitUp: Neurorehabilitation through Synergistic Man–Machine Interfaces. 2022. Available online: https://clinicaltrials.gov/study/NCT05465486 (accessed on 3 April 2024).
- ClinicalTrials.gov, I.N. HEROES: Human Extremity Robotic Rehabilitation and Outcome Enhancement for Stroke (HEROES). 2024. Available online: https://clinicaltrials.gov/study/NCT06160453 (accessed on 3 April 2025).
- Kirshblum, S.C.; Burns, S.P.; Biering-Sorensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Johansen, M.; Jones, L.; Krassioukov, A.; Mulcahey, M.; et al. International standards for neurological classification of spinal cord injury (revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef]
- Athanasiou, A.; Alexandrou, A.; Paraskevopoulos, E.; Foroglou, N.; Prassas, A.; Bamidis, P.D. Towards a Greek adaptation of the Spinal Cord Independence Measure (SCIM). In Proceedings of the 15th European Congress of Neurosurgery, Prague, Czech Republic, 12–17 October 2014; pp. 184–187. [Google Scholar] [CrossRef]
- Michailidou, C.; Marston, L.; De Souza, L.H. Translation into Greek and initial validity and reliability testing of a modified version of the SCIM III, in both English and Greek, for self-use. Disabil. Rehabil. 2016, 38, 180–188. [Google Scholar] [CrossRef]
- Duncan, P.W.; Bode, R.K.; Lai, S.M.; Perera, S.; Glycine Antagonist in Neuroprotection Americas Investigators. Rasch analysis of a new stroke-specific outcome scale: The Stroke Impact Scale. Arch. Phys. Med. Rehabil. 2003, 84, 950–963. [Google Scholar] [CrossRef]
- Patel, N.; Rao, V.A.; Heilman-Espinoza, E.R.; Lai, R.; Quesada, R.A.; Flint, A.C. Simple and reliable determination of the modified rankin scale score in neurosurgical and neurological patients: The mRS-9Q. Neurosurgery 2012, 71, 971–975. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Bohannon, R.W. Comfortable and maximum walking speed of adults aged 20—79 years: Reference values and determinants. Age Ageing 1997, 26, 15–19. [Google Scholar] [CrossRef]
- Meseguer-Henarejos, A.B.; Sánchez-Meca, J.; López-Pina, J.A.; Carles-Hernández, R. Inter-and intra-rater reliability of the Modified Ashworth Scale: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2017, 54, 576–590. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893. [Google Scholar] [CrossRef]
- At, B. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Rosenberg, M. Rosenberg self-esteem scale. In PsycTESTS Dataset; American Psychological Association: Washington, DC, USA, 1965. [Google Scholar] [CrossRef]
- Galanou, C.; Galanakis, M.; Alexopoulos, E.; Darviri, C. Rosenberg self-esteem scale Greek validation on student sample. Psychology 2014, 5, 819. [Google Scholar] [CrossRef]
- Marin, R.S.; Biedrzycki, R.C.; Firinciogullari, S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res. 1991, 38, 143–162. [Google Scholar] [CrossRef]
- Isaac, A.; Marks, D.F.; Russell, D.G. An instrument for assessing imagery of movement: The Vividness of Movement Imagery Questionnaire (VMIQ). J. Ment. Imag. 1986, 10, 23–30. [Google Scholar]
- Malouin, F.; Richards, C.L.; Jackson, P.L.; Lafleur, M.F.; Durand, A.; Doyon, J. The Kinesthetic and Visual Imagery Questionnaire (KVIQ) for assessing motor imagery in persons with physical disabilities: A reliability and construct validity study. J. Neurol. Phys. Ther. 2007, 31, 20–29. [Google Scholar] [CrossRef]
- Konstantinidis, E.I.; Billis, A.; Bratsas, C.; Siountas, A.; Bamidis, P.D. Thessaloniki Active and Healthy Ageing Living Lab: The roadmap from a specific project to a living lab towards openness. In Proceedings of the 9th ACM International Conference on PErvasive Technologies Related to Assistive Environments, Corfu Island, Greece, 29 June–1 July 2016; pp. 1–4. [Google Scholar] [CrossRef]
- Bartneck, C.; Kulić, D.; Croft, E.; Zoghbi, S. Measurement instruments for the anthropomorphism, animacy, likeability, perceived intelligence, and perceived safety of robots. Int. J. Soc. Robot. 2009, 1, 71–81. [Google Scholar] [CrossRef]
- Astaras, A.; Athanasiou, A.; Alexandrou, A.; Kartsidis, P.; Moustakas, N.; Bamidis, P. Double-blind greek translation and online implementation of the Godspeed robotics questionnaire. In Proceedings of the 6th Panhellenic Conference on Biomedical Technology Conference, Athens, Greece, 6–8 May 2015; p. 34. [Google Scholar]
- Zijlstra, F.; Van Doorn, L. The Construction of a Scale to Measure Perceived Effort; University of Technology: Delft, The Netherlands, 1985. [Google Scholar]
- Sauro, J.; Dumas, J.S. Comparison of three one-question, post-task usability questionnaires. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Boston, MA, USA, 4–9 April 2009; pp. 1599–1608. [Google Scholar] [CrossRef]
- Song, X.; Van De Ven, S.S.; Liu, L.; Wouda, F.J.; Wang, H.; Shull, P.B. Activities of daily living-based rehabilitation system for arm and hand motor function retraining after stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Jarque-Bou, N.J.; Gracia-Ibáñez, V.; Vergara, M.; Sancho-Bru, J.L. The BE-UJI Hand Function Activity Set: A reduced set of activities for the evaluation of the healthy and pathological hand. J. Neuroeng. Rehabil. 2023, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- Rudhe, C.; Van Hedel, H.J. Upper extremity function in persons with tetraplegia: Relationships between strength, capacity, and the spinal cord independence measure. Neurorehabilit. Neural Repair. 2009, 23, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Scivoletto, G.; Tamburella, F.; Laurenza, L.; Molinari, M. The spinal cord independence measure: How much change is clinically significant for spinal cord injury subjects. Disabil. Rehabil. 2013, 35, 1808–1813. [Google Scholar] [CrossRef]
- Kogan, E.; Twyman, K.; Heap, J.; Milentijevic, D.; Lin, J.H.; Alberts, M. Assessing stroke severity using electronic health record data: A machine learning approach. BMC Med. Inform. Decis. Mak. 2020, 20, 1–8. [Google Scholar] [CrossRef]
- Balasch i Bernat, M.; Balasch i Parisi, S.; Sebastián, E.N.; Moscardó, L.D.; Ferri Campos, J.; Lopez Bueno, L. Determining cut-off points in functional assessment scales in stroke. NeuroRehabilitation 2015, 37, 165–172. [Google Scholar] [CrossRef]
- Mills, P.B.; Holtz, K.A.; Szefer, E.; Noonan, V.K.; Kwon, B.K. Early predictors of developing problematic spasticity following traumatic spinal cord injury: A prospective cohort study. J. Spinal Cord Med. 2020, 43, 315–330. [Google Scholar] [CrossRef]
- Pundik, S.; Falchook, A.D.; McCabe, J.; Litinas, K.; Daly, J.J. Functional brain correlates of upper limb spasticity and its mitigation following rehabilitation in chronic stroke survivors. Stroke Res. Treat. 2014, 2014, 306325. [Google Scholar] [CrossRef]
- Dionne, A.; Mac-Thiong, J.M.; Alsofyani, M.A.; Richard-Denis, A. Are early onset spasms predictive of poor neurological recovery after traumatic spinal cord injury? J. Spinal Cord Med. 2024, 47, 566–572. [Google Scholar] [CrossRef]
- Sangari, S.; Chen, B.; Grover, F.; Salsabili, H.; Sheth, M.; Gohil, K.; Hobbs, S.; Olson, A.; Eisner-Janowicz, I.; Anschel, A.; et al. Spasticity predicts motor recovery for patients with subacute motor complete spinal cord injury. Ann. Neurol. 2024, 95, 71–86. [Google Scholar] [CrossRef] [PubMed]
- Poveda-García, A.; Moret-Tatay, C.; Gómez-Martínez, M. The association between mental motor imagery and real movement in stroke. Healthcare 2021, 9, 1568. [Google Scholar] [CrossRef] [PubMed]
- Banyai, A.D.; Brișan, C. Robotics in physical rehabilitation: Systematic Review. Healthcare 2024, 12, 1720. [Google Scholar] [CrossRef] [PubMed]
- Beckerle, P.; Salvietti, G.; Unal, R.; Prattichizzo, D.; Rossi, S.; Castellini, C.; Hirche, S.; Endo, S.; Amor, H.B.; Ciocarlie, M.; et al. A human–robot interaction perspective on assistive and rehabilitation robotics. Front. Neurorobotics 2017, 11, 24. [Google Scholar] [CrossRef]
- Weiss, A.; Bartneck, C. Meta analysis of the usage of the godspeed questionnaire series. In Proceedings of the 2015 24th IEEE International Symposium on Robot and Human Interactive Communication (RO-MAN), Kobe, Japan, 31 August–September 2015; pp. 381–388. [Google Scholar]
- Arvanitidis, A.; Mitsopoulos, K.; Fiska, V.; Athanasiou, A.; Bamidis, P.D. Design of A Normative sEMG Database for Biometric Comparison in Rehabilitation Research. Glob. Clin. Eng. J. 2024, 6, 96–101. [Google Scholar] [CrossRef]
- Arsenidis, A.; Moraitopoulos, A.; Athanasiou, A.; Vildiridis, A.; Bamidis, P.; Stefaneas, P.; Astaras, A. Novel Functional Electrical Stimulation Parameter Optimization for Neurorehabilitation Using Both Conventional and AI Techniques. Glob. Clin. Eng. J. 2024, 6, 45–50. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).