Abstract
This study aimed to formulate and characterize experimental dental adhesives charged with different concentrations of nanofillers. Different concentrations (0, 7.5 wt%, and 15 wt%) of nanosized silica (50 nm) were added to the bond of a two-bottle experimental etch-and-rinse adhesive system (EA0, EA7.5, and EA15). The following physicomechanical properties were evaluated: degree of conversion (DC%), ultimate tensile strength (UTS), flexural strength (FS), static modulus of elasticity (SME), dynamic modulus of elasticity (DME), and glass transition temperature (Tg). Marginal integrity (%MG) was evaluated in standardized class I cavities hybridized with the EAs and restored using two dental composites (CON-conventional and OBF-bulk-fill): EA0CON, EA7.5CON, EA15CON, EA0OBF, EA7.5OBF, and EA15OBF. Gap formation was measured in the occlusal and mesial tooth-restoration interfaces using a 3D laser confocal microscope. Microtensile bond strength (µTBS) was evaluated using dentin-composite beams (1 × 1 mm) obtained from restorations. Data were submitted to ANOVA and Tukey’s test (α = 0.05). For DC% and Tg, EA15 < EA0 = EA7.5 (p < 0.05). For UTS, EA0 < EA7.5 < EA15. For FS, SME, and DME, EA0 < EA7.5 = EA15 (p < 0.05). For the gap formation analysis, there were statistical differences only for the conventional composite (EA0CON > EA7.5CON = EA15CON). The lowest values (p < 0.05) of µTBS were observed for the groups restored with EAs without inorganic content. In conclusion, charging dental adhesives with nanofillers may be a suitable strategy for improving their properties as well as their interaction with dental substrates.
1. Introduction
Adhesive dentistry has been greatly improved in the past few years as a result of several factors such as better knowledge of the morphology of the dental substrates that are adhered to dental composites, greater development of dental materials, and improvement of restorative techniques. However, the tooth–composite interface is still one of the most challenging and least predictable areas of restoration, mainly due to the great variability of the composition of the dental substrate; moreover, it is well-known that dentin exerts a pivotal role in this chain of events.
In this context, the ability of restorative materials to adhere to the dentin surface is affected by several factors [1], which include the dentin heterogeneity regarding morphology, orientation, quantity, and size of dentinal tubules, all of them influencing the dentin degree of humidity [2,3,4,5,6]. Since humidity plays a crucial role in the dentin bond phenomenon, all these factors may jeopardize the establishment of an effective and long-lasting bond strength between the tooth and the dental composite used for restoring the tooth. Besides, the bonded interface should be able to resist the stresses caused by the shrinkage produced during dental composite polymerization, which is related to gap formation at the tooth–composite interface [7,8,9].
In order to reduce the effect of the polymerization shrinkage stress, bulk-fill dental composites have been used. According to the manufacturers, these special types of restorative materials develop a lower polymerization shrinkage, theoretically inducing lower stress at the tooth–dental composite interface [10,11]. From this perspective, bulk-fill composites might help with preserving the adhesive interface through less gap formation [12,13]; however, there are controversial results regarding the shrinkage of these materials, showing that this low-shrinkage characteristic is highly dependent on the composition of each bulk-fill dental composite [14,15].
Another factor that enormously affects the adhesive interface integrity is the bond strength provided by the adhesive system to the dentin, which should be able to counterattack the shrinkage stress at the tooth–composite interface. Adhesive systems consist mainly of monomers, solvents, and photoinitiators [16]. It has been noticed that adhesives containing inorganic fillers lead to improved mechanical properties such as the ultimate tensile strength [17,18], flexural strength [19,20], and elastic modulus [18,21], besides improving bond strength to dentin [18,20,22]. Particularly, the enhancement of the bond strength is attributed to the greater ultimate tensile strength of the adhesive and to the better stress distribution at the bond interface [20,23]. On the other hand, it is questioned if the high modulus of elasticity—due to the higher content of inorganic fillers—could compromise the bonding interface since it could reduce its flow in the face of the contraction stresses generated [24]. In fact, studies that used flow composites without fillers [25] or a thick layer of unfilled adhesive as a liner in cavities restored with high modulus composites [26] produced better marginal sealing of restorations. According to the authors, they attribute this finding to the lower stresses generated by materials with a lower elastic modulus, generally due to the higher flow capacity in the early stages of polymerization.
Therefore, aiming to verify whether charging dental adhesives with nanofillers could influence the gap formation at the tooth–dental composite interface when bulk-fill or conventional composites are used in dental restorations with a high C-factor, the purpose of the present study was to formulate and characterize dental adhesives charged with different concentrations of nanofillers. Physicomechanical properties, gap formation, and microtensile bond strength were evaluated. The null hypothesis tested was that there would not be differences in physicomechanical properties, gap formation, and microtensile bond strength among all of the experimental dental adhesives.
2. Materials and Methods
2.1. Preparation of the Experimental Adhesives
The organic matrix of the adhesives was formulated in accordance with the composition shown in Table 1 (wt%), and then the nanosized silica particles (50 nm, Esstech, Inc., Essington, PA, USA) were added in different concentrations (0%, 7.5%, and 15%) in the bond, performing the three experimental two-bottle etch-and-rinse adhesives. All the components were weighed on an analytical balance with 0.01 mg precision (XP 205, Mettler Toledo, Greinfensee, Switzerland) and centrifuged using three cycles of 1400 rpm for 1 min (dual DAC 150.1 FVZ, FlackTeK Inc., Landrum, SC, USA). Camphorquinone (0.5% and N,N-dimethyl-4aminobenzoate (0.5%), both from Sigma Aldrich (Milwaukee, WI, USA), were incorporated as the photosensitizer and the reducing agent, respectively.

Table 1.
Composition of the experimental adhesives.
2.2. Physical Properties
2.2.1. Degree of Conversion (DC%)
Amounts of 0.6 μL of the primer and 0.6 μL of the bond of each experimental adhesive (n = 5) were mixed and the solvent evaporation from these mixtures was monitored using an analytical balance (XP 205, Mettler Toledo, Greinfensee, Switzerland) in a dark environment until a mass equilibrium was reached. Afterward, the mixtures were inserted into a mold (Top Dam Blue, FGM, Joinville, SC, Brazil) positioned onto the ATR crystal of the FT-IR spectrometer (Alpha-P/Platinum ATR Module, Bruker Optics GmbH, Ettlingen, Germany) and the spectra between 1500 and 1800 cm−1 were recorded, with the spectrometer operating with 40 scans and at a resolution of 4 cm−1. After light-curing for 20 s (Radii-cal, SDI Inc., Bayswater, VIC, Australia, 1200 mW/cm−2) the spectra were recorded exactly as performed for the unpolymerized mixture. The DC% was calculated from the ratio between the integrated area of absorption bands of the aliphatic C=C bond (1638 cm−1) to that of the C=O bond (1608 cm−1), used as an internal standard, which was obtained from the polymerized and unpolymerized increments using the following equation:
where R = integrated area at 1638 cm−1/integrated area at 1608 cm−1.
DC% = [1 − (R polymerized/R unpolymerized)] × 100,
2.2.2. Ultimate Tensile Strength (UTS)
For the ultimate tensile strength analysis, the primer and bond of each experimental adhesive (n = 5) were mixed and the solvent was evaporated, as described before. Then, each mixture was carefully inserted into a metallic hourglass-shaped mold (10 mm × 3 mm × 1.5 mm, with central constriction measuring 2.25 mm2), and placed over a glass plate. The mold was covered with a 0.3 mm glass laminate, and a 0.5 kg mass was placed over it for 30 s to extrude excesses. Then, the specimens were light-cured for 20 s (Radii-cal, SDI Inc., Victoria, Austrália, 1200 mW/cm−2), removed from the metallic mold, and observed under a stereomicroscope (40×, SZ61TR, Olympus, Center Valley, PA, USA). All specimens were incubated in deionized water at 37 °C for 24 h, and then fixed on a JIG with cyanoacrylate (Tekbond gel, São Paulo, Brazil) for evaluation with a universal testing machine (DL 2000, EMIC, São Paulo, Brazil) at a crosshead speed of 1 mm/min. The load required to fracture the specimen was recorded in MPa.
2.2.3. Flexural Strength (FS) and Static Modulus of Elasticity (SME)
For this analysis, specimens were prepared as described for the UTS test, using a barshaped metallic matrix (10 mm × 2 mm × 1 mm). After storage in distilled water for 24 h at 37 °C, specimens were submitted to a three-point bending test, with a span distance of 6 mm, using a universal testing machine (DL 2000, EMIC) at a crosshead speed of 1 mm/min. The static modulus was obtained based on the linear portion of the stress–strain curve and the flexural strength, based on the load recorded at the moment of the fracture of the specimens using the following equations, respectively:
where l is the span distance, F is the applied load, w is the specimen width, h is the specimen thickness, and d is the deflection corresponding to the F load during the elastic regimen.
SME = l3F/4wh3d,
FS = 3lF/2wh2,
2.2.4. Dynamic Modulus of Elasticity (DME) and Glass Transition Temperature (Tg)
For the dynamic modulus of elasticity analysis, the specimens of each adhesive system (n = 5) were made as described before, using a barshaped metallic matrix (35 mm × 10 mm × 4 mm) and light-cured with four overlapped irradiations for 20 s each, along the sample on both sides. After storage in distilled water for 24 h at 37 °C, the specimens were submitted to the DMTA test (Dynamic Mechanical Thermal Analyzer/DMA Q800 TA Instruments, New Castle, DE, USA), using a 3-point dynamic flexural compression load, with a frequency of 1 Hz, a force of 4 N, a temperature range of 0 to 200 °C, and a heating rate of 5 °C/min. In this dynamic test, the recorded response is divided into an in-phase component called storage modulus (E′), and an out-of-phase component called viscous modulus (E″). The relationship between the viscous modulus and the elastic modulus is determined as the tangent delta (Tan δ) value, a measure of energy dissipation as heat. The peak of the Tan δ curve is commonly referred to as the glass transition temperature (Tg) of the material. During the test, as the temperature increases, there is a point where there is enough vibrational energy for the polymer chains to move together to become a unit. Thereafter, the behavior of the polymer rapidly changes from vitreous to very rigid when the Tg of material [27] is determined. Data collected from DME at 37 °C and Tg were recorded.
2.3. Adhesive Interface Analysis
For this analysis, forty-two caries-free human third molars (Ethics Committee Approval HUAP CAAE: 52273421.20000.5243) were disinfected in 0.5% chloramine-T solution at 4 °C for 7 days, stored in distilled water, and used within one month after extraction.
The tooth’s occlusal surfaces were flattened with the aid of a polisher (DPU 10, Struers, Copenhagen, Denmark) using 600-grit SiC papers, leading to a flat enamel surface. Occlusal cavities were prepared with a diamond bur (#4103, KG Sorensen, São Paulo, SP, Brazil) under water cooling (6 mm in mesio-distal width, 5 mm in bucco-lingual width, and 4 mm in depth) using a high-speed hand piece. Then, the teeth were randomly distributed into 6 experimental groups (n = 7), according to Table 2.

Table 2.
Experimental groups.
The primer was actively applied on the tooth structure for 20 s, gently air dried for 5 s followed by the active application of the bond, and light-cured for 20 s. Afterward, the cavities were restored with each dental composite: the bulk-fill composite was inserted in a single increment and light-cured for 40 s (Radii Cal, SDI), and the conventional composite was inserted with the incremental technique using increments of up to 2 mm light-curing for 20 s (Radii Cal, SDI). The occlusal surfaces were sequentially polished using SiC paper (#600, 800, 1200, 3000, and 4000) for 1 min each, in order to remove excesses and allow microscopic analysis. The teeth were placed in an ultrasonic bath (750 USC, Quimis, Rio de Janeiro, Brazil) for 10 min to remove any debris.
Then, the analysis of the adhesive interface on the occlusal surface was performed, recording the perimeter of the tooth–restoration interface, and the sum of the gaps found along the entire length of the occlusal interface (Occlusal gaps-OG) with the aid of a confocal laser scanning microscope (CSLM-LEXT 3D OLS4100, Olympus, USA) at 5X magnification (Figure 1). Subsequently, a longitudinal cut in the bucco-lingual direction, close to the mesial surface of the cavity was performed using a slow-speed diamond saw (Isomet 1000 precision saw Buëhler, Lake Bluff, IL, USA) so that the adhesive interface of the mesial adhesive interface was exposed for analysis (Figure 1). After sequential polishing using SiC paper and cleaning in an ultrasonic bath, as previously described, the perimeter of the mesial adhesive interface and the sum of the gaps found along the entire length of the mesial interface (mesial gaps-MG) were recorded. The presence of gaps was calculated in percentage, according to the following formulas:
where OG is the sum of the length of the gaps found across the tooth–restoration interface from the occlusal surface, BW is the width of the buccal adhesive interface, LW is the width of the lingual adhesive interface, MW is the width of the mesial adhesive interface, and DW is the width of the distal adhesive interface.
where MG is the sum of the length of the gaps found across the tooth–restoration interface of the mesial surface, BW is the width of the buccal adhesive interface, CW is the width of the cervical adhesive interface, and LW is the width of the lingual adhesive interface.
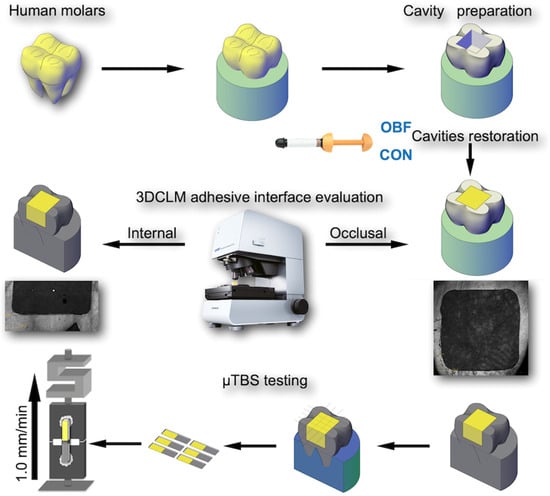
Figure 1.
Schematic representation of specimen preparation for analysis under the confocal microscope and microtensile test.
2.4. Microtensile Bond Strength (µTBS) and Failure Pattern
After measuring the gaps, the specimens were longitudinally sectioned (IsoMet) in both the mesial-distal and buccal-lingual directions across the bonded interfaces to produce beams with a cross-sectional area of approximately 1.0 mm2. After measuring the cross-sectional area with a digital caliper (MPI/E101, Mytutoyo, Tokyo, Japan), each beam was fixed with cyanoacrylate glue (Tekbond gel, Saint Gobain, São Paulo, Brazil) to the microtensile device and loaded under tension in a universal testing machine (DL 2000, EMIC, São Paulo) at a crosshead speed of 1.0 mm/min until failure occurred (Figure 1). The µTBS (MPa) was calculated (MPa) by the following formula:
where F = the load at failure (N) and A = cross-sectional area of the adhesive area (mm2).
The failure mode of the tested beams was evaluated at 80× magnification under stereomicroscope (SZ61TR, Olympus, Tokyo, Japan) and classified as adhesive (failures at the adhesive interface), cohesive (failures occurring mainly within dentin or composite), or mixed (mixture of adhesive and cohesive failure on the same fractured surface).
2.5. Statistical Analysis
The data were analyzed using Statgraphics Centurion XVI software (STATPOINT Technologies, Warrenton, VA, USA). Initially, the normal distribution of errors and the homogeneity of variances were checked using Shapiro–Wilk and Levene tests. Data on the degree of conversion, ultimate tensile strength, flexural strength, static modulus of elasticity, dynamic modulus of elasticity, Tan δ, and Tg were subjected to one-way ANOVA. The data from the analysis of the gaps of the adhesive interface and the bond strength were submitted to two-way ANOVA. Tukey’s HSD was employed as a post hoc test. The analyses were performed at a confidence level of 95% (α = 0.05). Failure pattern was analyzed as percentage.
3. Results
3.1. Physical Properties
The values obtained for the degree of conversion (DC%), ultimate tensile strength (UTS), flexural strength (FS), static modulus of elasticity (SME), dynamic modulus of elasticity (DME), and Tg are shown in Table 3. EA15 presented lower DC% and Tg than EA0 and EA7.5 (p < 0.05), which were statistically similar to each other. The adhesives containing inorganic fillers showed higher UTS, FS, SME, and DME than the control group EA0 (p < 0.05), and only for UTS, EA7.5 was lower than EA15 (p < 0.05).

Table 3.
Mean and standard deviation of physical properties for the experimental adhesives.
3.2. Adhesive Interface Analysis
The percentages of occlusal and mesial gaps found in the study are described in Table 4. Regarding the occlusal and mesial gaps, it can be observed that there was no statistical difference between the experimental adhesives for the bulk-fill composite. When using the conventional composite, EA0 showed a higher percentage of occlusal and mesial gaps than EA7.5 and EA15 (p < 0.05), which were statistically similar to each other. The experimental adhesive containing 7.5% of inorganic fillers (EA7.5) showed a similar percentage of occlusal and mesial gaps for the two restorative composites, while EA0 and EA15 showed a higher percentage of gaps for the conventional composite (p < 0.05).

Table 4.
Mean and standard deviation of marginal gaps (µm) for the experimental groups.
3.3. Bond Strength
The mean and standard deviation of bond strength for each experimental group are described in Table 5. Two-way analysis of variance showed statistical significance only for the adhesive factor. The composite factor and the interaction between adhesive and composite were not statistically significant. EA0 showed lower bond strength than EA7.5 and EA15 (p < 0.05), which were similar to each other.

Table 5.
Mean and standard deviation of microtensile bond strength (Mpa) for the experimental groups.
The distribution of failure patterns after the microtensile test is shown in Figure 2. A smaller number of cohesive failures can be observed for the groups in which the E0 adhesive was used, and there was a predominance of mixed failures for all groups.
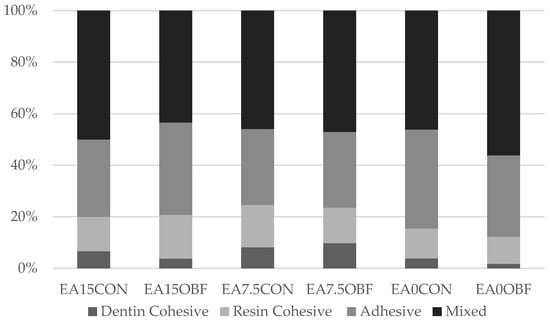
Figure 2.
Failure pattern (%) for each experimental group.
4. Discussion
In the present study, the incorporation of 7.5 or 15% of inorganic fillers in the experimental adhesive system increased some of the mechanical properties analyzed, such as elastic modulus, flexural strength, and ultimate tensile strength, and produced a slight decrease in the degree of conversion, specifically for the adhesive containing 15% of silica nanoparticles. It is speculated that this increase in the mechanical properties leads to the increase in the bond strength values to dentin, irrespective of the type of composite employed (conventional or bulk-fill). Furthermore, greater marginal gaps were observed for the adhesive system without inorganic content when used in association with the conventional composite. Based on these results, the null hypothesis of the present study was rejected.
The achievement of a high degree of conversion is desirable for the longevity of the adhesive layer since it guarantees a proper conversion of the monomers that have been polymerized, consequently reducing the chances of leaching oligomers from the hybrid layer [28] and ensuring a better quality of the tooth–composite bonded interface [29]. In the present study, all experimental adhesive systems achieved similar or higher values of degree of conversion than those found in the literature for commercial [30,31] and experimental materials [17,19] ranging between 78% and 84%. Despite this, a statistically significant reduction was detected for the DC% of the adhesive systems containing 15% of inorganic particles compared to the control group (EA0), which agrees with Alhenaki et al. [32] who found lower DC% for adhesives with concentrations of nanoparticles of silica greater than 10%. Filler particles can be responsible for promoting light scattering, making light more difficult to reach deeper regions, especially when the filler size is half of the photoactivator light wavelength [33]. The worst performance of the adhesive system with 15% of inorganic content may be associated with greater light scattering due to a higher concentration of silica nanoparticles, negatively impacting its DC%. The addition of 7.5% did not affect the DC%, which is in agreement with a previous study [17], in which increasing the concentration of silica nanoparticles up to 10% did not change the DC%.
The lower degree of conversion observed for EA15 was not able to interfere with the mechanical properties studied since all experimental adhesives containing silica nanoparticles at concentrations of 7.5 and 15% reached higher values of UTS, FS, SME, and DME than the control group; moreover, the UTS was higher for EA15 than for EA7.5. This finding agrees with previous studies that also observed that the addition of a certain amount of filler particles can promote an improvement in these mechanical properties [17,18,19,20,21]. In the studies by Azad et al. [20] and Mazloon-Jalali et al. [34], the positive effect of the addition of silica nanoparticles on the flexural strength occurred only when up to 0.2% of inorganic content was present, being attributed to the good interfacial adhesion between resin matrix and fillers, which would facilitate the transfer of stresses from the matrix to the fillers, avoiding the propagation of cracks and, consequently, leading to greater mechanical strength. At higher concentrations, these authors believe that an agglomeration of the filler particles occurred, generating fragility points where the cracks would start, thus reducing the mechanical strength. In these studies, the smaller particle size (12 nm) used may have contributed to this agglomeration, which may not have occurred in the present study where larger particles (50 nm) were used. In fact, the presence of spherical silica particles of 40–120 nm in composites, as well as the good interfacial relationship between filler and matrix, were considered essential for increasing the mechanical strength of polymers [35]. In the study by Belli et al. [18], the presence of larger SiO2-BaO particles (180/500 nm) in concentrations up to 15% increased the ultimate tensile strength and elastic modulus.
The improvement of the mechanical properties studied for the experimental adhesives containing inorganic particles was expected since the use of silanized particles would allow a chemical union between the functional group of methacrylates and the silane (γ-MPS), preventing the propagation of the fracture along the matrix-–load interface, increasing the cohesive and flexural strength, and the elastic modulus [18]. Also, as the elastic modulus of a polymer is associated with the elastic properties of its components, it was expected that the greater stiffness presented by the filler particles would lead to an increase in this property in experimental adhesives with inorganic content [36].
The dynamic mechanical analysis proves to be quite suitable for the analysis of viscoelastic materials, being used to predict the cross-link density and the heterogeneous structure of the polymer chain since the method allows recording both the elastic and viscous response [27]. In the present study, higher values of dynamic elastic modulus were observed than the static one, in agreement with other studies [37,38], which also showed a strong correlation between these tests and was related to the high frequency of applied force since the stiffest component of the material is then stimulated [39]. The lower Tg of the EA15 is in line with its lower degree of conversion since the greater amount of unreacted monomers would be free to move at lower temperatures, causing the peak of tan δ recorded at lower temperatures. In fact, although the cross-link density had a higher influence on the Tg of the materials, the lower degree of material conversion can determine a lower glass transition temperature, as found in a previous study [40,41].
In addition to the positive results achieved in relation to the mechanical properties with the incorporation of inorganic particles in the experimental adhesive systems, the bond strength to dentin using these adhesives also showed an improvement regardless of the type of composite used, in agreement with previous studies [18,20,22,32]. The increase in the mechanical properties of the adhesive system can improve the distribution of stresses resulting from the contraction of polymerization of the composite, which would lead to greater bond strength [23]. At the same time, a greater number of adhesive failures was observed for the groups in that the adhesive without inorganic content was used, which may be associated with the lower bond strength associated with these groups. In fact, the higher number of adhesive or cohesive failures has been explained by the lower or higher bond strength observed, respectively, in previous studies [42,43]. The high percentage of mixed failures for all groups could indicate, as in a previous study [44], a strong union of the experimental adhesives with dentin.
In the present study, the silica nanoparticles (50 nm) were not incorporated into the primer in order to ensure that an adequate hybrid layer was obtained since the primer could freely penetrate the spaces between the collagen fibrils, which are an average of 12nm wide [45]. When the adhesive–dentin bonding interface is strong, the defects responsible for the fracture can preferentially start in the adhesive and propagate from there; the filler particles can act as obstacles for this propagation [46]. Alhenaki et al. [32] also found better bond strength for adhesives containing filler particles (150 nm) up to 15%. Azad et al. [23], using smaller particles (12 nm) at a concentration of up to 0.5%, found a significant increase in bond strength. In the study by Di Hipolito et al. [22], higher bond strength was found only for the commercial adhesive that contained a smaller size of filler particles (5 nm), justified by the increase in the resistance of the hybrid layer, and associated with the penetration of the particles of charge together with the monomers between the collagen fibrils (12 nm).
Contrary to the present study, other adhesives with larger particles were not able to promote an increase in bond strength, in agreement with other authors who did not find better bonding results for adhesives containing filler particles [47,48]. In the study by Di Hipolito et al. [22], it was observed that larger-sized cargo particles or cargo agglomerates would be trapped only in the adhesive layer, which would not have been sufficient to increase the bond strength. It is important to note that these contradictory studies [22], refs. [47,48] analyzed commercial materials and there may be differences in the composition of the tested adhesives, in addition to not having any reference regarding the amount of filler particles present in them, which could have influenced the different results found.
The use of bulk-fill and conventional composites in this study was based on differences regarding the polymerization shrinkage [49] of both and, consequently, on the behavior that they could develop related to the shrinkage stresses generated at the bonding interface in cavities of high cavity configuration factor (Class I). Regarding the bond strength, the different types of composites did not influence the results obtained. It is noteworthy that both were applied according to the manufacturers’ recommendations, that is, the conventional one by the incremental technique and the bulk-fill by the single-increment technique, which may have compensated for the fact that the conventional composite presented a very high polymerization shrinkage, higher than bulk-fill [49]. Other studies [50,51] also found similar bond strength values between bulk-fill and conventional composites when applied by the recommended techniques.
Regarding the occlusal and mesial marginal gaps observed at the tooth–restoration interface, it was found that the conventional composite showed a higher percentage of cracks when the adhesive without filler particles was used, while for the bulk-fill composite, the type of adhesive used did not influence the results. As verified in previous studies, the increase in the inorganic content in polymeric materials could reduce the polymerization shrinkage [52]. Although it was not the focus of the present study to verify the polymerization shrinkage of the materials used, it can be assumed that the greater shrinkage of the adhesives without filler particles, added to the one that occurred with the conventional composite even when the incremental technique was used, has been a determining factor for the increase in tensions at the bonding interface, leading, consequently, to the occurrence of larger marginal gaps that have culminated in the statistical difference in this analysis, although this fact did not influence the bond strength. In fact, greater material polymerization shrinkage has been associated with greater adhesive failures and maladaptation at the bonding interface between composite and tooth structure [12,53]. Although no statistical significance was observed for the bulk-fill composite, a gradual decrease in the percentage of marginal cracks was also observed as the inorganic content of the adhesive increased.
In the present study, it is convenient to emphasize that only two composites and one filler particle size were studied, and it is essential to carry out additional studies with other experimental conditions to certify the benefits of the presence of inorganic particles in commercial adhesive systems.
Within the limitations of this study, it can be verified that the addition of up to 15% of 50 nm silica nanoparticles in experimental three-step adhesive systems is capable of increasing their mechanical properties, as well as promoting better bond strength, regardless of the type of composite used. In addition, a better adaptation at the tooth–restoration interface was observed with the use of adhesives containing filler particles for the conventional composite, being indifferent to the bulk-fill composite. Thus, silica nanoparticles indicate components that can potentially be included during the formulation of new adhesive systems.
5. Conclusions
It can be concluded from the results of the present study that charging dental adhesives with nanofillers can be a suitable strategy for improving their properties, as well as their interaction with the dental substrates, as better bond strength and adaptation to the dental cavity walls can be reached depending on the type of composite used.
Author Contributions
Conceptualization, L.T.P., C.R.P.C. and E.M.d.S.; methodology, C.R.P.C. and R.F.d.S.M.; formal analysis, L.T.P. and C.M.A.; data curation, J.G.A.G.; writing—original draft preparation, C.R.P.C. and R.F.d.S.M.; writing—review and editing, L.T.P., C.M.A., E.M.d.S. and A.G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brazil), Grant number 001, and FAPERJ (Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro), Grant numbers E-26 210.636/2019 and E-26 210.069-2021.
Institutional Review Board Statement
This study was approved by the Ethics Committee Approval from the HUAP (Hospital Universitário Antônio Pedro), number CAAE: 52273421.20000.5243; date of approval: 23 March 2022.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.
Acknowledgments
The authors thank the Instituto de Macromoléculas Eloisa Mano (IMA) from the UFRJ (Universidade Federal do Rio de Janeiro, Brazil) for making available the Dynamic Mechanical Thermal Analyser.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Perdigão, J. Current perspectives on dental adhesion: (1) Dentin adhesion—Not there yet. Jpn. Dent. Sci. Rev. 2020, 56, 190–207. [Google Scholar] [CrossRef]
- Garcés-Ortíz, M.; Ledesma-Montes, C.; Reyes-Gasga, J. Scanning Electron Microscopic Study on the Fibrillar Structures within Dentinal Tubules of Human Dentin. J. Endod. 2015, 41, 1510–1514. [Google Scholar] [CrossRef]
- Giannini, M.; Carvalho, R.M.; Martins, L.R.; Dias, C.T.; Pashley, D.H. The influence of tubule density and area of solid dentin on bond strength of two adhesive systems to dentin. J. Adhes. Dent. 2001, 3, 315–324. [Google Scholar]
- Perdigão, J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent. Mater. 2010, 26, e24–e37. [Google Scholar] [CrossRef]
- Carvalho, R.M.; Tjäderhane, L.; Manso, A.P.; Carrilho, M.R.; Carvalho, C.A.R. Dentin as a bonding substrate. Endod. Topics. 2012, 21, 62–88. [Google Scholar] [CrossRef]
- Weerakoon, A.T.; Cooper, C.; Meyers, I.A.; Condon, N.; Sexton, C.; Thomson, D.; Ford, P.J.; Symons, A.L.J. Does dentine mineral change with anatomical location, microscopic site and patient age? Struct. Biol. X 2022, 23, 100060. [Google Scholar] [CrossRef]
- Braga, R.R.; Ballester, R.Y.; Ferracane, J.L. Factors involved in the development of polymerization shrinkage stress in resin-composites: A systematic review. Dent. Mater. 2005, 21, 962–970. [Google Scholar] [CrossRef]
- Rodrigues, F.P.; Lima, R.G.; Muench, A.; Watts, D.C.; Ballester, R.Y. A method for calculating the compliance of bonded-interfaces under shrinkage: Validation for Class I cavities. Dent. Mater. 2014, 30, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Park, S.H. Incremental and bulk-fill techniques with bulk-fill resin composite in different cavity configurations. Oper. Dent. 2018, 43, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Boaro, L.C.C.; Gonçalves, F.; Guimarães, T.C.; Ferracne, J.L.; Versluis, V.; Braga, R.R. Polymerization stress, shrinkage and elastic modulus of current lowshrinkage restorative composites. Dent. Mater. 2010, 26, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Zorzin, J.; Maier, E.; Harre, S.; Fey, T.; Belli, R.; Lohbauer, U.; Taschner, M. Bulk-fill resin composites: Polymerization properties and extended light curing. Dent. Mater. 2015, 31, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Park, S.H. Measurement of the internal adaptation of resin composites using micro-CT and its correlation with polymerization shrinkage. Oper. Dent. 2014, 39, E57–E70. [Google Scholar] [CrossRef]
- Paganini, A.; Attin, T.; Tauböck, T.T. Margin integrity of bulk-fill composite restorations in primary teeth. Materials 2020, 13, 3802. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Van Landuyt, K.; Van Meerbeek, B. Effect of bulk-filling on the bonding efficacy in occlusal Class I cavities. J. Adhes. Dent. 2016, 18, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A review of the current literature. J. Adhes. Dent. 2017, 9, 95–109. [Google Scholar] [CrossRef]
- Van Landuyt, K.L.; Snauwaert, J.; De Munck, J.; Peumans, M.; Yoshida, Y.; Poitevin, A.; Van Meerbeek, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef]
- Conde, M.C.; Zanchi, C.H.; Rodrigues-Junior, S.A.; Carreño, N.L.; Ogliari, F.A.; Piva, E. Nanofiller loading level: Influence on selected properties of an adhesive resin. J. Dent. 2009, 37, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Belli, R.; Kreppel, S.; Petschelt, A.; Hornberger, H.; Boccaccini, A.R.; Lohbauer, U. Strengthening of dental adhesives via particle reinforcement. J. Mech. Behav. Biomed. Mater. 2014, 37, 100–108. [Google Scholar] [CrossRef]
- Kim, S.; Cho, B.; Lee, I.; Um, C.; Lim, B.; Oh, M.; Chang, C.; Son, H. Effect of the hydrophilic nanofill loading on the mechanical properties and the microtensile bond strength of an ethanol-based one-bottle dentin adhesive. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 72, 284–291. [Google Scholar] [CrossRef]
- Azad, E.; Atai, M.; Zandi, M.; Shokrollahi, P.; Solhi, L. Structure–properties relationships in dental adhesives: Effect of initiator, matrix monomer structure, and nano-filler incorporation. Dent. Mater. 2018, 34, 1263–1270. [Google Scholar] [CrossRef]
- Giannini, M.; Mettenburg, D.; Arrais, C.A.; Rueggeberg, F.A. The effect of filler addition on biaxial flexure strength and modulus of commercial dentin bonding systems. Quintessence Int. 2011, 42, e39–e43. [Google Scholar] [PubMed]
- Di Hipólito, V.; Reis, A.F.; Mitra, S.B.; de Goes, M.F. Interaction morphology and bond strength of nanofilled simplified-step adhesives to acid etched dentin. Eur. J. Dent. 2012, 6, 349–360. [Google Scholar] [CrossRef]
- Solhi, L.; Atai, M.; Nodehi, A.; Imani, M. A novel dentin bonding system containing poly (methacrylic acid) grafted nanoclay: Synthesis, characterization and properties. Dent. Mater. 2012, 28, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Braga, R.R.; Ferracane, J.L. Alternatives in polymerization contraction stress management. J. Appl. Oral. Sci. 2004, 15, 176–184. [Google Scholar] [CrossRef]
- Kemp-Scholte, C.M.; Davidson, C.L. Complete marginal seal of class V resin composite restorations effected by increased flexibility. J. Dent. Res. 1990, 69, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.K.; Condon, J.R.; Ferracane, J.L. The effects of adhesive thickness on polymerization contraction stress of composite. J. Dent. Res. 2000, 79, 812–817. [Google Scholar] [CrossRef]
- Mesquita, R.V.; Geis-Gerstorfer, J. Influence of temperature on the visco-elastic properties of direct and indirect dental composite resins. Dent. Mater. 2008, 24, 623–632. [Google Scholar] [CrossRef]
- Maktabi, H.; Ibrahim, M.; Alkhubaizi, Q.; Weir, M.; Xu, H.; Strassler, H.; Fugolin, A.P.P.; Pfeifer, C.S.; Melo, M. Underperforming light curing procedures trigger detrimental irradiance-dependent biofilm response on incrementally placed dental composites. J. Dent. 2019, 88, 103110. [Google Scholar] [CrossRef]
- Tichy, A.; Hosaka, K.; Abdou, A.; Nakajima, M.; Tagami, J. Degree of Conversion Contributes to Dentin Bonding Durability of Contemporary Universal Adhesives. Oper. Dent. 2020, 45, 556–566. [Google Scholar] [CrossRef]
- Faria-e-Silva, A.L.; Lima, A.F.; Moraes, R.R.; Piva, E.; Martins, L.R. Degree of conversion of etch-and-rinse and self-etch adhesives light-cured using QTH or LED. Oper. Dent. 2010, 35, 649–655. [Google Scholar] [CrossRef]
- Pongprueksa, P.; Miletic, V.; Janssens, H.; Van Landuyt, K.L.; De Munck, J.; Godderis, L.; Van Meerbeek, B. Degree of conversion and monomer elution of CQ/amine and TPO adhesives. Dent. Mater. 2014, 30, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Alhenaki, A.M.; Attar, E.A.; Alshahrani, A.; Farooq, I.; Vohra, F.; Abduljabbar, T. Dentin bond integrity of filled and unfilled resin adhesive enhanced with silica nanoparticles-An SEM, EDX, micro-raman, FTIR and micro-tensile bond strength study. Polymers 2021, 13, 1093. [Google Scholar] [CrossRef]
- Ruyter, I.E.; Oysaed, H. Conversion in different depths of ultraviolet and visible light activated composite materials. Acta Odontol. Scand. 1982, 40, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Mazloom-Jalali, A.; Taromi, F.A.; Atai, M.; Solhi, L. Dual modified nanosilica particles as reinforcing fillers for dental adhesives: Synthesis, characterization, and properties. J. Mech. Behav. Biomed. Mater. 2020, 110, 103904. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.S.; Lee, Y.D.; Nicolella, D.P.; Furman, B.R.; Wellinghoff, S.; Rawls, H.R. Improving fracture toughness of dental nanocomposites byinterface engineering and micromechanics. Eng. Fract. Mech. 2007, 74, 1857–1871. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.; Feng, X.; Lauke, B.; Mai, Y. Effects of particle size, particle/matrix interface adhesion and particle loading on mechanical properties of particulate-polymer composites. Compos. B Eng. 2008, 39, 933–961. [Google Scholar] [CrossRef]
- Sabbagh, J.; Vreven, J.; Leloup, G. Dynamic and static moduli of elasticity of resin-based materials. Dent. Mater. 2002, 18, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Leprince, J.; Palin, W.M.; Mullier, T.; Devaux, J.; Vreven, J.; Leloup, G. Investigating filler morphology and mechanical properties of new low-shrinkage resin composite types. J. Oral. Rehabil. 2010, 37, 364–376. [Google Scholar] [CrossRef]
- Braem, M.; Lambrechts, P.; Van Doren, V.; Vanherle, G. The impact of composite structure on its elastic response. J. Dent. Res. 1986, 65, 648–653. [Google Scholar] [CrossRef]
- Brandt, W.C.; Silva, C.G.; Frollini, E.; Souza-Junior, E.J.; Sinhoreti, M.A. Dynamic mechanical thermal analysis of composite resins with CQ and PPD as photo-initiators photoactivated by QTH and LED units. J. Mech. Behav. Biomed. Mater. 2013, 24, 21–29. [Google Scholar] [CrossRef]
- Pomès, B.; Behin, P.; Jordan, L.; Legoff, S.; Stoclet, G.; Richaud, E.; Nguyen, J.F. Influence of polymerization pressure and post-cure treatment on conversion degree and viscoelastic properties of polymer infiltrated ceramic network. J. Mech. Behav. Biomed. Mater. 2021, 115, 104286. [Google Scholar] [CrossRef]
- Nima, G.; Cavalli, V.; Bacelar-Sá, R.; Ambrosano, G.M.B.; Giannini, M. Effects of sodium hypochlorite as dentin deproteinizing agent and aging media on bond strength of two conventional adhesives. Microsc. Res. Tech. 2020, 83, 186–195. [Google Scholar] [CrossRef]
- Augusto, M.G.; Torres, C.; Pucci, C.R.; Schlueter, N.; Borges, A.B. Bond Stability of a Universal Adhesive System to Eroded/Abraded Dentin After Deproteinization. Oper. Dent. 2018, 43, 291–300. [Google Scholar] [CrossRef]
- Saikaew, P.; Matsumoto, M.; Chowdhury, A.; Carvalho, R.M.; Sano, H. Does Shortened Application Time Affect Long-Term Bond Strength of Universal Adhesives to Dentin? Oper. Dent. 2018, 43, 549–558. [Google Scholar] [CrossRef]
- Osorio, E.; Toledano, M.; Aguilera, F.S.; Tay, F.R.; Osorio, R. Ethanol wet-bonding technique sensitivity assessed by AFM. J. Dent. Res. 2010, 89, 1264–1269. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Ferracane, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Braga, R.R.; Cesar, P.F.; Gonzaga, C.C. Tensile bond strength of filled and unfilled adhesives to dentin. Am. J. Dent. 2000, 13, 73–76. [Google Scholar] [PubMed]
- Can Say, E.; Nakajima, M.; Senawongse, P.; Soyman, M.; Ozer, F.; Ogata, M.; Tagami, J. Microtensile bond strength of a filled vs unfilled adhesive to dentin using self-etch and total-etch technique. J. Dent. 2006, 34, 283–291. [Google Scholar] [CrossRef]
- Silva, J.D.S.; Freitas, L.A.S.; Silva, V.A.S.E.; Firmiano, T.C.; Tantbirojn, D.; Versluis, A.; Veríssimo, C. Using a professional DSLR camera to measure total shrinkage of resin composites. Braz. Oral. Res. 2022, 36, e009. [Google Scholar] [CrossRef] [PubMed]
- França, F.M.; Tenuti, J.G.; Broglio, I.P.; Paiva, L.E.; Basting, R.T.; Turssi, C.P.; do Amaral, F.L.; Reis, A.F.; Vieira-Junior, W.F. Low- and high-viscosity bulk-fill resin composites: A comparison of microhardness, microtensile bond strength, and fracture strength in restored molars. Acta Odontol. Latinoam. 2021, 34, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Mandava, J.; Vegesna, D.P.; Ravi, R.; Boddeda, M.R.; Uppalapati, L.V.; Ghazanfaruddin, M.D. Microtensile bond strength of bulk-fill restorative composites to dentin. J. Clin. Exp. Dent. 2017, 9, e1023–e1028. [Google Scholar] [CrossRef] [PubMed]
- Meereis, C.T.W.; Münchow, E.A.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization shrinkage stress of resin-based dental materials: A systematic review and meta-analyses of composition strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.J.; Kim, Y.J.; Choi, N.S.; Lee, I.B. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J. Dent. 2015, 43, 430–439. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).