1. Background
Dental implants with implant-supported prostheses represent an effective and reliable treatment option for replacing natural teeth [
1]. Advances in surgical techniques and implant components have significantly improved success rates, achieving over 90% for up to eight years [
2]. However, despite these advancements, mechanical failures and biological complications continue to affect peri-implant soft tissues, presenting ongoing challenges in dental implantology [
3,
4].
Mechanical complications associated with dental implants often include the loosening and fracture of prosthetic or abutment screws, as well as wear and fracture of the prosthesis or other system components [
5]. Mechanical complications in dental implants often arise from excessive occlusal forces, material fatigue, or improper prosthetic design. These factors can lead to screw loosening, fractures, and wear of implant components. Additionally, inadequate maintenance or poor alignment of the implant–abutment connection may exacerbate these issues [
6]. Although the occurrence of abutment screw fractures is relatively low, ranging from 0.5% to 8%, they are more frequently observed in fixed partial dentures compared to fixed complex prostheses. The extraction of fractured screw fragments remains a significant challenge in clinical practice, primarily depending on the degree of screw fracture and its engagement with the implant threads [
2,
3,
4,
5].
In instances where extraction proves difficult or could potentially harm the internal threads of the implant, the options typically include either leaving the fragment in place or opting for implant removal, both of which carry considerable risks, high morbidity, and uncertain prognosis [
6,
7,
8,
9,
10].
Moreover, removal techniques can generate heat due to the high thermal diffusivity of metals, which can adversely affect the bone–implant interface and compromise osseointegration. Fractured screw fragments can be extracted using conventional or drilling techniques. Agustin-Panadero et al. reported that conventional methods, through the use of an explorer and an ultrasound device, showed a success rate of 73.3%, while the mechanical technique achieved a success rate of 96.7% by precisely drilling into and extracting the fragment. Both techniques have a similar impact on implant–abutment connection integrity [
7].
This study aimed to analyze and compare the retrievability of fractured abutment screws and damage to the implant–abutment connections using conventional and drilling techniques. The null hypothesis (H0) posits that there is no difference in the retrievability and connection damage between the conventional and drilling techniques for fractured abutment screws.
2. Methods
2.1. Study Design
Forty abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) were randomly assigned to forty dental implants (dimensions: 4.6 × 12 mm: TLX4612, BioHorizons, Birmingham, AL, USA) using the Epidat v.4.1 software (Galicia, Spain). The screws were intentionally fractured within the conical internal hex connection of the dental implants. The implants with the fractured abutment screws (PGHYBN, BioHorizons, Birmingham, AL, USA) were then randomly allocated into one of four removal technique groups using the Epidat 4.1 software. Group A underwent a conventional removal method using an exploration probe and an ultrasonic device without irrigation (ProUltra®, Dentsply Maillefer®, Ballaigues, Switzerland) (n = 10) (conventional). Group B used the Phibo drilling removal system without irrigation (Phibo, Barcelona, Spain) (n = 10) (Phibo). Group C employed the Rhein83® drilling system without irrigation (Broken Screw Extractor Kit, Rhein83®, Bologna, Italy) (n = 10) (Rhein83), and Group D applied the Sanhigia® drilling removal system without irrigation (FSRK-01; Sanhigia®, Saragossa, Spain) (n = 10) (Sanhigia).
This study, a randomized controlled experimental trial, took place between April and November 2023 at the Dental Centre of Innovation and Advanced Specialties at Alfonso X El Sabio University (Madrid, Spain). The sample size was determined based on a power effect of 87.2, with a threshold of 80 considered acceptable. To achieve a power effect of at least 80.00% for identifying statistically significant differences, forty abutment screws were included in the study. The bilateral Student’s t-test, with a 5% significance level, was employed to test the null hypothesis, H0: µ1 = µ2, for two independent samples.
2.2. Experimental Procedure
Twenty dental implants (4.6 × 12 mm: TLX4612, BioHorizons, Birmingham, AL, USA) were positioned in nylon tubes using epoxy resin (Exakto-Form
®, Bredent GmbH & Co.KG, Senden, Germany), with a cast key employed to ensure consistent placement according to the ISO 14801 guidelines [
11]. Before fracturing the abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) within the conical internal hex implant–abutment connection, micro-computed tomography (micro-CT) scans were conducted using the Super Argus MicroCT scanner (SEDECAL, Algete, Madrid, Spain) at the Molecular Imaging Laboratory, which is part of the NUCLEUS lab at the University of Salamanca. The scan parameters were set to 45.0 kilovolt peak, 900.0 microamperes, and 720 projections, generating precise Standard Tessellation Language (STL) digital files of the unaltered dental implants (STL1).
Subsequently, the abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) were intentionally fractured within the internal threads of the conical internal hex connection. This was achieved by using a diamond burr (S6881 314 012, Komet Medical, Lemgo, Germany) to sever two-thirds of the abutment screw diameter between the shank and the threads. The screws were then tightened into the dental implants (TLX4612, BioHorizons) with a torque that exceeded the manufacturer’s recommended 30 Ncm. After this, the screws were extracted from the dental implants following the assigned removal technique for each case.
2.3. Phibo Drilling Removal System
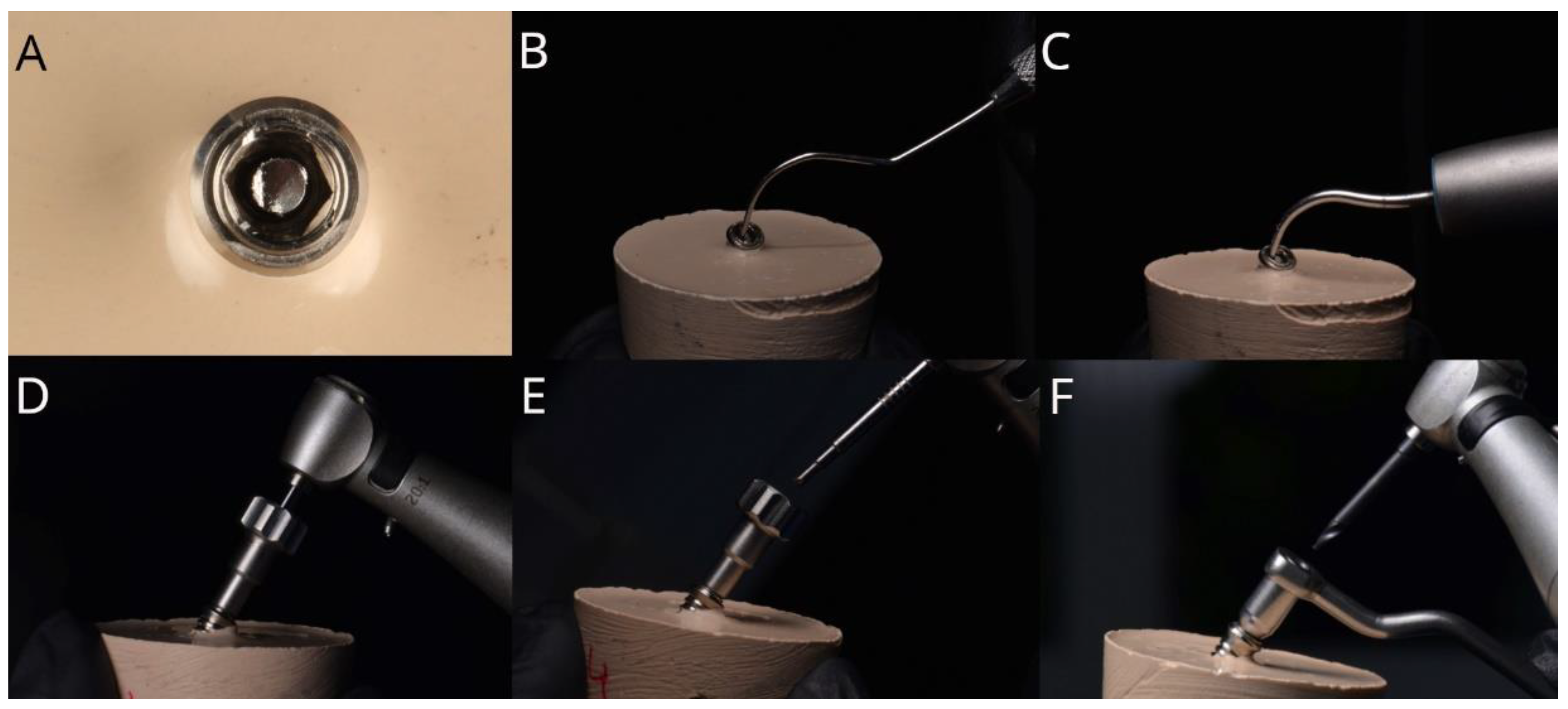
The abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) randomly assigned to the Phibo drilling removal system without irrigation (Phibo, Barcelona, Spain) were removed using a tungsten carbide bur with an implantology handpiece at 850 revolutions per minute (rpm) using a 20:1 reduction in a clockwise movement without irrigation to perforate the coronal surface of the fractured abutment screw (
Figure 1). Afterwards, a stainless-steel pyramid-shaped drill was used with an implantology handpiece at 15 rpm in a 20:1 reduction in counterclockwise movement without irrigation (
Figure 1). The drill was placed in the hole created by the previous drill to grab the fragment and remove it by unscrewing it.
2.4. Rhein83® Drilling Removal System
The abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) assigned to the Rhein83
® drilling removal system (Broken Screw Extractor Kit; Rhein83
®, Bologna, Italy) were extracted by first securing the centering device on the implant connection (
Figure 2). A claw reamer bur (680 FA; Rhein83
®) was then used with an implantology handpiece, operating at 1000–2000 rpm with a 20:1 reduction in counterclockwise rotation (WS-75 LG; W&H, Hawthorne Drive, MI, USA) without irrigation (
Figure 2). If any part of the fractured abutment screw remained in the implant, a special reverse-cut bur was utilized at 500–600 rpm, also with a 20:1 reduction in the counterclockwise motion and without irrigation.
2.5. Sanhigia® Drilling Removal System
The abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) allocated to the Sanhigia
® drilling removal system (FSRK-01; Sanhigia
®, Saragossa, Spain) were extracted by first placing and securing the guide (TSV 3.7/4.7; Sanhigia
®, Saragossa, Spain) over the implant–abutment connection. A drill was then used with an implantology handpiece at a speed of 1200–2000 rpm, with a 20:1 reduction in the clockwise direction and without irrigation, to perforate the coronal portion of the fractured screw (
Figure 3). In the final step, a second drill was employed with an implantology handpiece at 50–80 rpm, with a 20:1 reduction in the counterclockwise motion and without irrigation, to fully extract the fractured screw (
Figure 3).
2.6. Conventional Technique with Exploration Probe and Ultrasonic Appliance
The abutment screws (PXAS, BioHorizons, Birmingham, AL, USA) randomly assigned to the conventional study group were removed using the conventional technique with an exploration probe and an ultrasonic tip (Start-X3, Dentsply SIRONA, Baillagues, Switzerland) placed in an ultrasonic appliance (ProUltra
®, Dentsply Maillefer
®, Ballaigues, Switzerland). The exploration probe with counterclockwise circular movements and the ultrasonic tip were used to tap the center of the broken fragment with 30 VA power and 50 Hz frequency; no irrigation was used (
Figure 4).
2.7. Measurement Procedure
After the abutment screws were removed (PGHYBN, BioHorizons, Birmingham, AL, USA), or after 5 min had passed, a postoperative micro-CT scan (Super Argus MicroCT, SEDECAL, Algete, Madrid, Spain) (STL2) was taken under the aforementioned exposure parameters. Next, the STL1 and STL2 digital files were imported into the reverse engineering morphometric software (3D Geomagic Capture Wrap v.2024, 3D Systems
©, Rock Hill, SC, USA), and the best-fit algorithm was used to align the digital STL files. The differences in volume between the STL1 and STL2 digital files were then analyzed to assess the wear volume. The tolerance between the alignment of the digital files was set at ±10 µm and the spectrum at ±100 µm. A maximum of 5 min of working time was allowed for recording the removal of the abutment screws from the dental implants. A unique operator with over 10 years of experience in prosthetic dentistry performed the various techniques for removing the abutment screws (P.M.-A.), and the measurement procedures were performed by another operator (A.Z.-M.), who was calibrated and blinded to the randomization process of the samples and who had performed the same digital measurement procedure in a previous study [
8].
The wear on the internal threads of the conical internal hex implant–abutment connection (4.6 × 12 mm, TLX4612 BioHorizons, Birmingham, AL, USA) was analyzed by comparing the pre- and postoperative STL digital files after aligning the STL1 and STL2 digital files and calculating the volumetric differences (mm
3) of the conventional technique (
Figure 5B and video 1,
https://youtu.be/eR76VAanLt0 (“(accessed on 23 September 2024)”)) and the Phibo (
Figure 5C and video 2, (
https://youtu.be/Bgb2wMQHF_E “ (accessed on 23 September 2024)”), Rhein83 (
Figure 5D and video 3, (
https://youtu.be/Ra61jd8cNYs, (“(accessed on 23 September 2024)”)), and Sanhigia (
Figure 5E and video 4,
https://youtu.be/va9fL47p-HE, (“(accessed on 23 September 2024)”)) drilling removal systems.
2.8. Statistical Tests
Tables were created with summary statistics for each of the response variables according to the group, including number of observations, mean, median, standard deviation, and minimum and maximum values. These statistics were presented graphically using box diagrams.
Normality tests were performed using the Shapiro–Wilk test. For variables with a normal distribution, the comparison of means between groups was performed using an analysis of variance (ANOVA); if statistically significant differences between the groups were detected, 2-by-2 comparisons were performed, and the p-values were adjusted using the Tukey method to correct for type I errors. For variables with a non-normal distribution, the comparison between groups was performed using a non-parametric analysis (Kruskal–Wallis test); if statistically significant differences between the groups were detected, 2-by-2 comparisons were performed, and the p-values were adjusted using the Bonferroni method.
The statistical analysis was performed with the SAS v9.4 software, SAS Institute Inc., Cary, NC, USA. Statistical decisions were made taking the value of 0.05 as the significance level.
3. Results
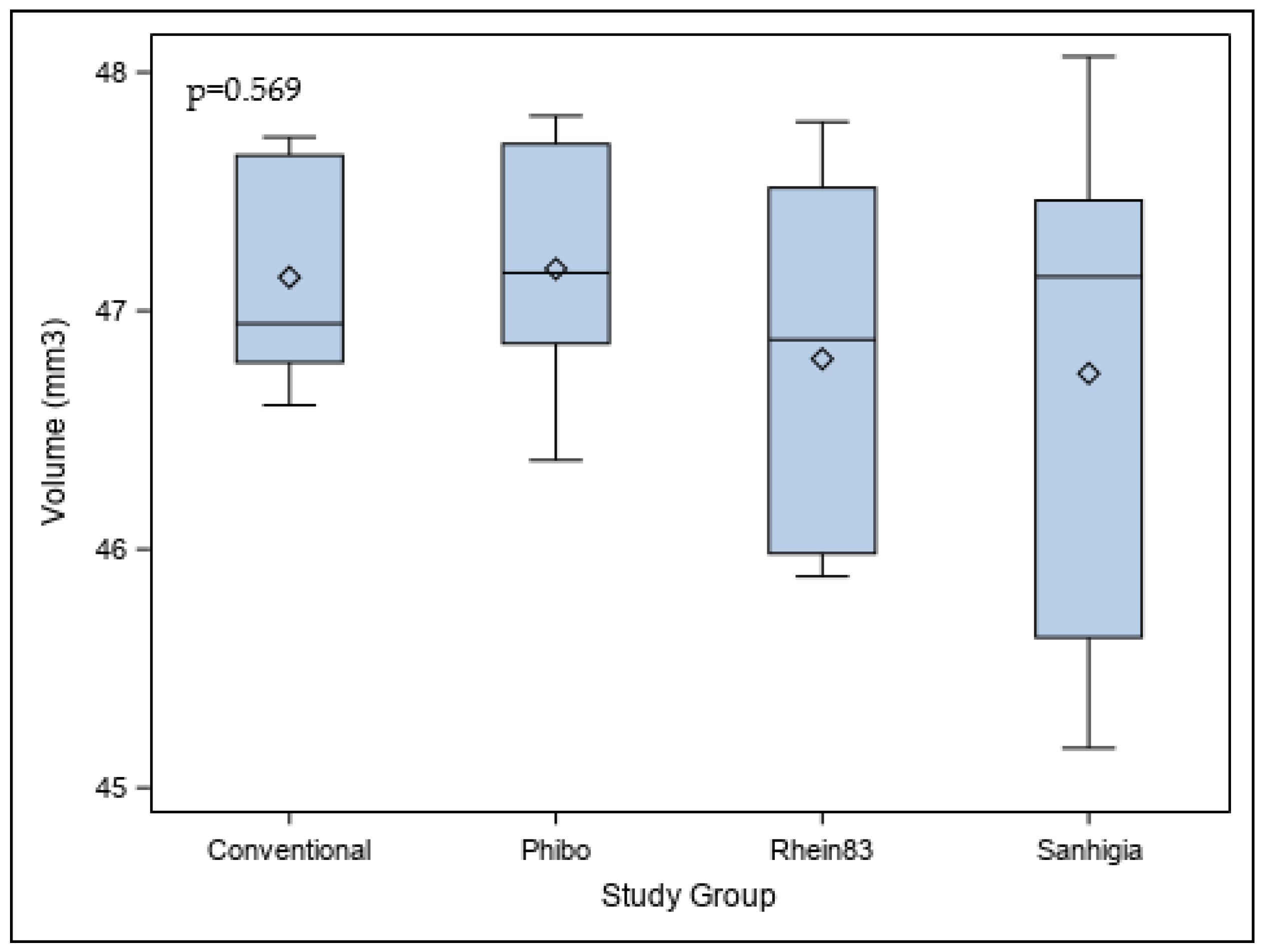
Table 1 and
Figure 6 display the means and SD values for the postoperative volumetric differences (mm
3) of the internal threads at the conical internal hex implant–abutment connection among the study groups.
The ANOVA results did not show statistically significant differences (
p = 0.569) in the postoperative volumetric differences of the internal threads at the conical internal hex implant–abutment connection between the conventional, Phibo, Rhein83, and Sanhigia study groups (
Figure 6).
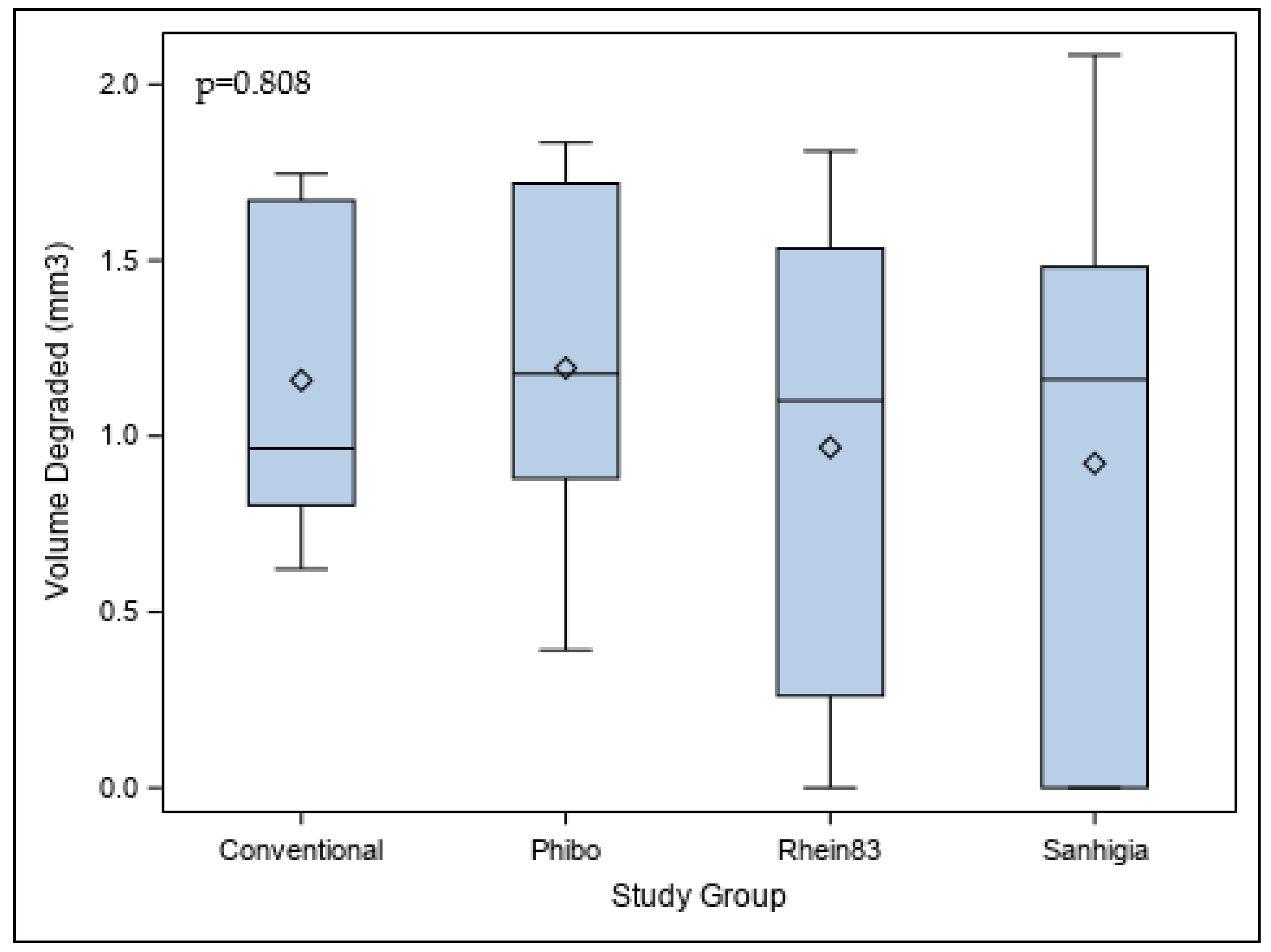
Table 2 and
Figure 7 display the means and SD values for the volumetric differences (mm
3) between the pre- and postoperative volumes of the internal threads at the conical internal hex implant–abutment connection among the study groups.
The ANOVA results did not show statistically significant differences (
p = 0.808) in the pre- and postoperative volumes of the internal threads at the conical internal hex implant–abutment connection between the conventional, Phibo, Rhein83, and Sanhigia study groups (
Figure 7).
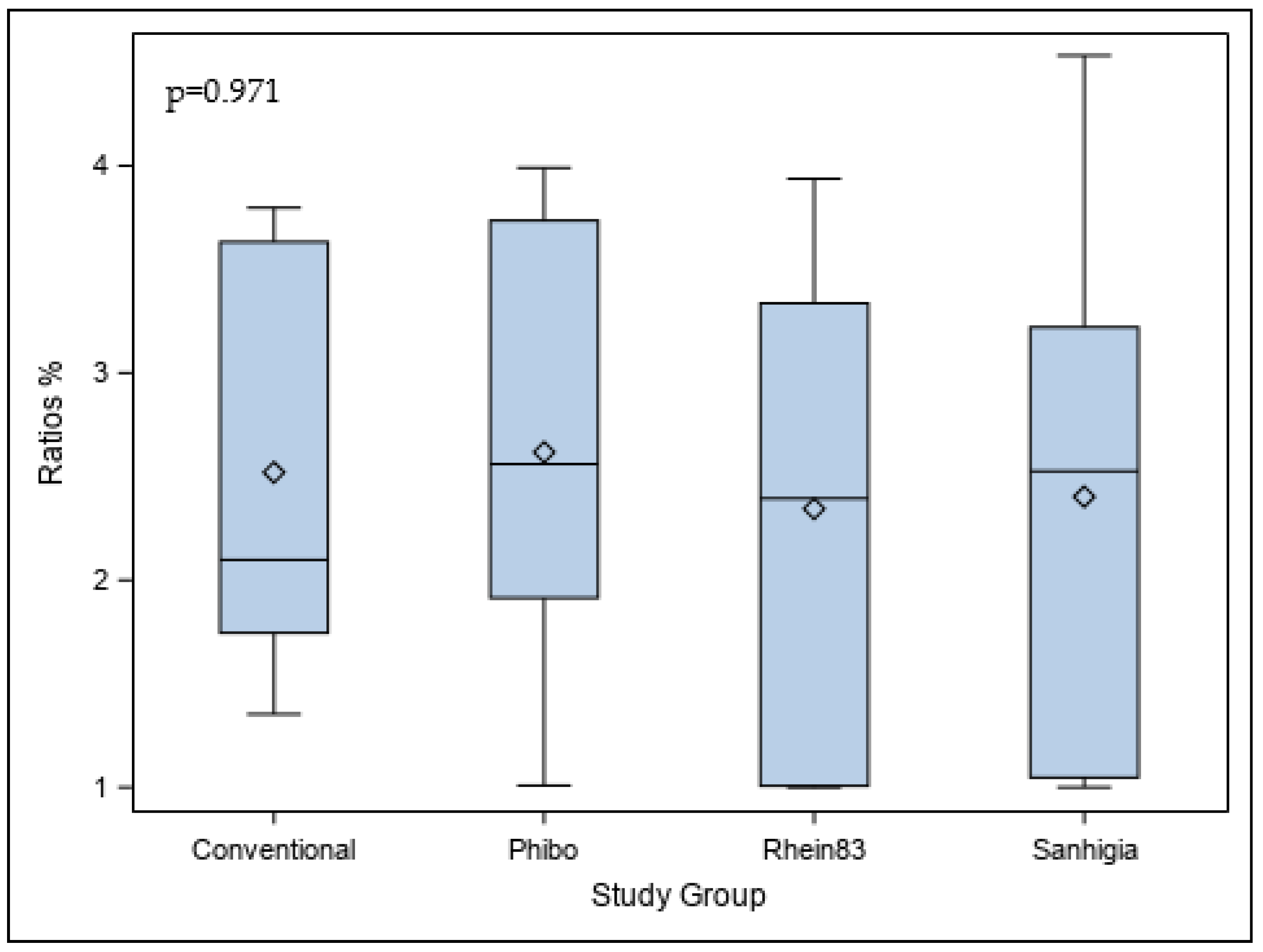
Table 3 and
Figure 8 display the means and SD values for the volumetric ratio (%) between the pre- and postoperative volumes of the internal threads at the conical internal hex implant–abutment connection among the study groups.
The ANOVA results did not show statistically significant differences (
p = 0.971) in the volumetric ratio (%) between the pre- and postoperative volumes of the internal threads at the conical internal hex implant–abutment connection between the conventional, Phibo, Rhein83, and Sanhigia study groups (
Figure 8).
Additionally, the success rate for retrieval of the fractured abutment screws from the conical internal hex implant–abutment connection was analyzed. The results showed that 90% of the fractured abutment screws were successfully removed using the Phibo, Rhein83, and Sanhigia drilling removal systems, whereas 50% of the fractured abutment screws were successfully removed using the conventional technique with an exploration probe and an ultrasonic appliance.
4. Discussion
The results of the present study reject the null hypothesis (H0) that there is no difference in the retrievability and damage to the implant–abutment connection of fractured abutment screws between the conventional and drilling techniques. While various techniques were employed, no statistically significant differences were found among them. However, the non-irrigation drilling techniques with the Phibo, Rhein83, and Sanhigia drilling systems demonstrated a higher retrieval success rate of 90% for fractured screws, compared to only 50% for the conventional technique. This raises questions about the practical efficacy of less invasive approaches.
The scientific literature has yet to establish an efficient and predictable protocol for the removal of fractured abutment screw fragments from within dental implants. Current studies on managing these fractures are limited, and no scientific evidence is currently available to guide clinicians in choosing the most effective or manageable technique [
7,
10]. Additionally, there is no documentation on the volumetric impact at the implant–abutment interface following fractured screw removal. Ideally, an effective extraction of a fractured screw within an implant should avoid damage to the internal threading to prevent adverse outcomes, such as implant removal [
12,
13]. If the internal threading remains intact, only a new screw would be necessary, allowing the reuse of both the implant and the prosthesis.
A previous study emphasized the importance of avoiding damage to the implant connection and access channel during fractured screw removal, particularly with internal connection implants [
9]. Additionally, fractured screw removal is crucial to maintaining implant functionality [
14]. Moreover, it has been highlighted that abutment screw fractures could increase the gap at the implant–abutment interface, leading to peri-implantitis development [
15]. This underscores the clinical importance of removing fractured abutment screws. However, maintaining the integrity of an implant’s internal thread is challenging, with damage rates of 9.8% reported, which sometimes prevents subsequent prosthetic placement. In addition, an internal thread damage rate of 13.33% has been reported [
7,
10].
These drilling techniques have emerged in response to the mechanical complications associated with implants, such as screw fractures. Potential mechanical complications include loosening, screw fractures, wear, prosthesis fractures, and damage to other system components [
6]. Despite numerous clinical and in vitro studies, the exact causes of these complications remain unclear and may stem from improper prosthesis fitting [
16]. Notably, experienced clinicians have been reported to tighten screws at 30–50% less than necessary [
17]. The torque applied to the implant prosthetic screw is crucial for achieving the ideal load at the screw joint and preventing loosening [
3,
5,
18]. Undetected loosening is a primary cause of screw fractures, with potential contributing factors including bruxism, unfavorable superstructure design, overload, rehabilitation malfunction, inadequate abutment seating, occlusal interferences, and manufacturing errors [
1,
3,
6].
Screw loosening can occur when the forces acting to separate the screw joint, such as off-axis occlusal loads, exceed the forces holding the abutment and implant together. Additionally, screw fractures can arise from superstructure misalignment, overload, or malfunction [
5]. Research has indicated that screw fractures are often associated with the external hexagon prosthetic connection [
19], while implant systems equipped with anti-rotational features, such as an internal hex, tend to exhibit improved strength [
19,
20]. These systems, along with those where the abutment is deeply integrated into the implant body, have shown lower rates of complications [
21]. Consequently, implant manufacturers have begun designing more robust internal connections to reduce the risk of loosening and subsequent screw fractures [
19].
Various techniques for extracting fractured screw fragments have been developed, each dependent on the initial condition of the fragment [
20]. Conventional, conservative methods are often recommended as the first line of treatment. For instance, a dental explorer can be rotated counterclockwise to recover the remaining screw fragments, as suggested by previous studies [
22]. Other effective techniques include the use of an ultrasonic tip, which has a reported success rate of 73.3% [
7], cotton swabs [
23], and Er-YAG lasers [
24]. In cases where conservative methods fail, more invasive techniques, such as specialized rescue instruments designed by different implant manufacturers, may be employed. One such example is the IMZ TwinPlus Repair Set K 3.3 (Dentsply Friadent, Mannheim, Germany) [
2,
21]. This method typically involves drilling the fragment to ensure retention before unscrewing it, as described by other researchers [
25]. However, this procedure can be complicated and time-consuming for routine clinical use, as it risks damaging the threads within the implant [
21,
25].
Previous research suggested the use of two burs: the first is a serrated #557 bur, which is used counterclockwise when the fragment is deep, and the second is a #33 ½ bur, which is used clockwise when the fragment is coronal for complete fragment extraction to avoid implant damage [
26].
The use of these techniques can not only damage the implant but also compromise osseointegration, altering the implant–bone interface due to heat production [
27,
28].
Overheating of osseous tissues can lead to irreversible damage. When bone is subjected to temperatures of around 47 °C for 1 min, this sometimes causes lesions in adipose cells and inconsistent tissue damage [
29].
In cases of failure to remove the fractured screw fragment, other less invasive methods have been proposed to save the implant and avoid explantation. In addition, a previous study introduced a custom metal abutment into the implant, repositioning the implant-supported rehabilitation [
30]. One study used shorter abutment screws as a replacement without prior removal of the remaining broken screw fragment [
31], and another also used a shorter second screw to fix the implant-supported prosthesis, attaching it to the remaining fractured fragment without prior extraction [
32].
Despite the use of these methods for fragment extraction, irreversible damage to implants can occur [
25]. One study recommended that clinicians must be especially careful to avoid damaging the dental–implant connection, in addition to the implant access channel, when extracting the fractured screw [
27].
This study shows that the use of the conventional and drilling techniques for the extraction of fractured abutment screws did not result in statistically significant differences in the morphometric wear volume of the implant–abutment connection (p = 0.569), or the wear volume (p = 0.808) or ratio (p = 0.971) of the internal hexagonal threads at the implant–abutment connection.
An accurate morphometric analysis (tolerance at ±10 µm) of the wear volume of the dental conical internal hex implant–abutment connection after fractured abutment screw extraction validates this measurement procedure, which can be used in future studies to analyze volumetric changes. However, the accuracy of this measurement procedure is dependent on the resolution of the compared STL digital files; it is, therefore, prudent to use digital files with a high tessellation density, such as those obtained with micro-CT. In any case, further studies are needed to establish the clinical relevance of implant–abutment damage and heat generation and their effect on dental implant prognosis.