Featured Application
The hardware and software VR complex was created based on a new scientific technique for cognitive rehabilitation—multitasking cognitive training.
Abstract
Background: The use of virtual reality (VR) has great potential for medical research and practice, which can help expand rehabilitation activities. This study aimed to evaluate the acceptability and feasibility of the original protocol VR multitasking cognitive training (CT) in both a healthy group and cardiac surgery patients. Methods: A specialized hardware and software complex was developed and tested on both a group of 25 practically healthy individuals, mean age 22.9 years (SD 2.57), and 25 cardiac surgery patients, mean age 62.2 years (SD 7.35). The participants were instructed to complete one session of multitasking CT within the VR complex. Psychometric testing and EEG studies were conducted. Results: All participants were highly accepting of the intended future use, attitude, and pleasure of the training. The healthy subjects demonstrated a statistically significant improvement in attention and spatial skills after VR (p ˂ 0.05). The EEG data revealed a significant increase in alpha power compared to pre-experiment levels (p ˂ 0.0001). The theta/alpha ratio significantly decreased after the VR multitasking CT as compared to the baseline (p ˂ 0.0001). Conclusions: The data obtained indicate that the original training protocol for multitasking CT using VR is acceptable and easy to use for both healthy individuals and cardiac surgery patients.
1. Introduction
The aging population has presented health professionals with new and complex challenges, not only in extending life expectancy but also in preserving its quality. Maintaining one’s intellectual abilities is essential for achieving a high quality of life [1,2]. Normal aging is characterized by psychomotor slowing, poorer divided attention, difficulty learning new information, and poor verbal fluency, while sustained attention, simple copy, remote, and procedural memory are preserved [3]. Moreover, the development of cardiovascular disease in older people can have specific features that can lead to cognitive decline [4,5]. Atherosclerosis causes more severe cognitive impairments than age-related cognitive changes. It has been suggested that brain dysfunction can be accelerated due to the atherosclerotic remodeling of brain vessels [6,7]. Cognitive deficits are now regarded as a sign of a poor quality of life and a decrease in life expectancy for patients. The progression and worsening of cardiovascular diseases can occur as a result of cognitive health deterioration and decreased medication compliance [8].
The patients with cognitive impairment who undergo cardiac surgery are considered a distinct and challenging group [9,10]. The risk of ischemic brain injury increases as a result of global or local ischemia during cardiopulmonary bypass during cardiac surgery. This procedure is not always complicated by stroke, but other consequences can lead to less pronounced, diffuse lesions that eventually lead to cognitive decline [10,11]. There is an increase in the likelihood of postoperative cognitive dysfunction (POCD) in these patients [9]. POCD is a deterioration of higher-grade cognitive skills, attention, executive function, and memory [12]. Postoperative cognitive deficit manifestations can complicate the recovery process and decrease the efficacy of rehabilitation measures [13]. All of the above increases the financial burden on the healthcare system, which explains the need to find new approaches to cognitive recovery and prevent the progression of cognitive deficits.
Cognitive rehabilitation aims to enhance cognitive reserve or stimulate plastic processes in the brain through various training methods. Recent studies have reported improved cognitive performance following combined physical and cognitive activities [14,15,16]. The simultaneous execution of cognitive and motor tasks or dual tasks requires significant cognitive control of attentional and executive functions [17]. Thus, the preliminary data show that a multimodal approach using cognitive training (CT) interventions can provide effective cognitive recovery. In the study by Syrova and colleagues, cognitive–motor training reduced the frequency of POCD during the early postoperative period of coronary surgery. The indicators of executive functions, attention, and short-term memory showed positive changes [18]. According to the authors, multitasking training can increase the involvement of different brain regions in the recovery process and slow down the progression of cognitive decline. The study used a computer-based version of the multitask training. However, new clinical practice options are available due to the development of emerging technologies.
Virtual reality (VR) could be a possible approach for multimodal cognitive training. The manipulation of experimental parameters in VR apps has a great potential to develop new forms of cognitive intervention and treatment [19,20]. Recent studies suggest that VR-based training interventions can be utilized to enhance well-being, cognition, and physical fitness in individuals with cognitive deficits [21,22,23]. In the study by Kang et al. [21], the VR group demonstrated improvements in psychiatric symptoms, including apathy, affect for positive affect, and quality of life, when compared to the control group. According to Eleni Baldimtsi and colleagues, patients with cognitive impairment who participated in 32 VR training sessions had no or negligible declines in their basic cognitive function, verbal memory, executive functions, and mental flexibility [23]. In another study, 12 weeks of VR rehabilitation were compared to conventional physical therapy for patients with Parkinson’s disease. VR training contributed to a major improvement in the balance and gait of the patients as compared to the conventional physical therapy [24].
A systematic review by Saeedi and colleagues showed that VR training is one of the most advanced motor rehabilitation methods for stroke patients [25]. The trainings were mainly aimed at improving balance and mobility of the limbs and demonstrated their effectiveness. The research on the impact of virtual reality on cognitive function recovery following cardiac surgery is still in its infancy. The studies mentioned above were not focused on POCD in patients who have ischemic brain damage or have undergone cardiac surgery. In order to successfully perform cognitive recovery in cardiac surgery patients, innovative techniques and approaches are necessary. Multitasking can be used in VR as one of these approaches.
It should be noted that the physiological reserves in cardiac surgery patients are very limited, so it is important to take this into consideration when choosing VR as a rehabilitation procedure. Immersion in a virtual information environment can lead to a number of negative consequences that depend on such factors as the individual characteristics of the users of VR systems, technical characteristics of the system, and specificity of the tasks performed [26]. The research on the effects of VR on the human brain has not produced conclusive results. It was demonstrated that presence in VR is often accompanied by the observation of subjects moving, with their position being immobile, which creates the illusion of human body movement in space (vection) [27]. This produces a set of adverse effects, such as dizziness and disorientation in space [28].
To search for new approaches to the recovery of cognitive functions, it is necessary to understand the neurophysiological changes associated with VR cognitive rehabilitation. Digital electroencephalography (EEG) is widely used to control brain activity without invasive intervention and to study the fundamental mechanisms of brain functioning [29,30]. The neurophysiological effects of VR training were studied by Gangemi and colleagues in patients with ischemic stroke. The authors showed a significant increase in both the alpha band power in the occipital areas and the beta band power in the frontal areas. There were no significant changes in the theta band power [31]. In another study, it was demonstrated that VR-based rehabilitation in patients with chronic stroke caused the mirror neuron system to be involved, which resulted in enhanced motor performance [32].
Therefore, our literature review suggests that multitasking in virtual reality will be the most productive approach for cognitive rehabilitation of cardiac patients. However, it is necessary to consider the negative effects of VR on brain and cognitive functioning, which consequently affect the effectiveness of multitasking CT. Thus, the aim of our study is to investigate the neurophysiological effects of VR during multitasking CT in healthy subjects and evaluate the acceptability and feasibility of the original protocol VR multitasking CT in both a healthy group and cardiac surgery patients.
2. Materials and Methods
2.1. Participants
This sample study was conducted between February 2024 and June 2024. Twenty-five practically healthy subjects aged between 20 and 25 years participated in this study. The healthy participants had college or higher education, normal or corrected to normal vision, and experience using a computer. The health status of the participants was assessed using the questionnaire by V.P. Vojtenko [33] (see Table 1).

Table 1.
Demographic and clinical characteristics of the healthy participants and cardiac surgery patients.
The cardiac surgery group consisted of 25 participants who signed an informed consent form. The exclusion criteria for the patients were any abnormal changes in the brain, as evidenced by computed tomography; depressive symptoms; dementia; life-threatening arrhythmia; heart failure functional class IV according to the guidelines of the New York Heart Association (NYHA); chronic obstructive pulmonary disease; malignant pathology; diseases of the central nervous system; and brain damage. This study did not include patients who received anxiolytic therapy. The demographic and clinical details are presented in Table 1.
2.2. Design and Development of the Original Multitasking CT VR System
We created the original VR system to test a new scientifically based technique for cognitive rehabilitation in ischemic brain damage that used a multitasking approach and virtual environment. Our expert multidisciplinary team included physiologists, computer scientists, engineers, and healthcare professionals. The implementation of a virtual environment was created by the software company “LABIMMERTEX”, Kemerovo, Russia. The multitasking CT VR system was created using personalized design (User Experience Design), a systematic approach to creating usable products, systems, or services that are specifically designed for target users. During the postoperative period after a cardiac surgery, patients often exhibit cognitive impairments, such as reduced executive function, short-term memory, and attention [10]. Our proposal is that the VR system can be a useful tool for multitasking training, where motor and cognitive tasks are executed simultaneously. The VR program should include tasks like object selection, counting, memorization, motor activity, and immersion in a natural virtual environment. Cardiac surgery patients can activate their cognitive reserves through the use of the VR program.
2.2.1. Hardware Components
The technical requirements for a multitasking CT VR system were established. The developed VR complex should provide 3D content playback in a VR display with a frequency of not less than 90 Hz and a field of view of at least 110 degrees. Minimal resistance is necessary for the device to perform the motor task. The maximum gripping radius of the device for performing the motor task was selected experimentally at 280 mm. The following hardware devices were selected for this purpose: a PC with GeForce RTX™ 4070 VENTUS 3X E 12G OC (MSI, Shenzhen, China) graphics card and Intel Core i7-13700F BOX (Intel, Santa Clara, CA, USA) chip, VR headmounted display (the HP Reverb G2 (HP, Palo Alto, CA, USA)), and the Hori Racing Wheel Apex (Hori, Torrance, CA, USA) (see Figure 1). A complete list of the hardware devices composing the training system is in Appendix B.
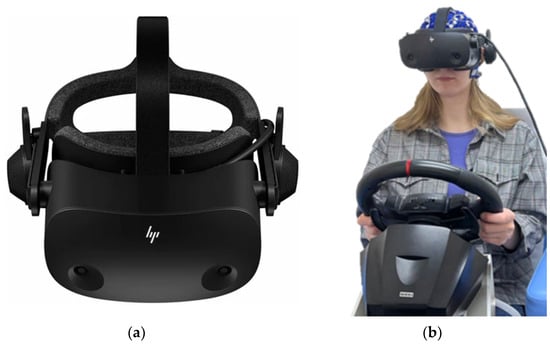
Figure 1.
The hardware devices composing the VR training system. (a) VR headmounted display. (b) The wheel.
2.2.2. Software Components
The VR application was developed on the Unity Real-Time Development Platform, version 2021.3.10f1 [34]. All 3D models used in the application were created in the free and open-source 3D computer graphics software tool Blender 3.6 LTS [35]. A virtual environment was created that is enjoyable and resembles a large fruit garden. At the start of every session, the user observed the fruit garden through the window of a tractor. The user was tasked with keeping the trajectory of the tractor’s movement on the track by driving (motor task) and counting different colored apples on a tree from when it was passing the tree (cognitive task). Only the number of red and green apples should be counted; yellow apples should be ignored. Ten apples must be remembered in total (see Figure 2). A cognitive task’s answer was displayed on the screen after 30 s. Pressing the appropriate key on the wheel, either incorrectly or correctly, is necessary for the user to indicate the number of red and green apples in the answer field. At the end of the session, the display displayed the performance data of each participant, which included the number of correct or incorrect answers and a visual reward (Video S1: VR Apple. https://disk.yandex.ru/i/GEFaLv4BmfqjYg).


Figure 2.
The virtual multitasking cognitive training. (a) A cognitive task; (b) A cognitive task’s answer. In this case, a participant should press the key on the wheel to indicate an incorrect answer to a cognitive task; (c) End of the session; (d) General view of experiment.
2.3. Neurophysiological Assessment
The healthy subjects were examined through an extensive neuropsychological battery to evaluate psychomotor and executive function, selective attention, short-term memory, and mental rotation. The neuropsychological battery has been described in detail previously [36]. The testing was conducted before and after completing one session of multitasking CT within the VR complex. Alternate versions of the neuropsychological tests were used in repeated measurements to minimize practice effects. In addition, the participants were assessed by a neurologist to determine whether they had any signs of vection.
The EEGs were recorded in the eyes-closed condition in a dimly lit, soundproof, electrically shielded room via a 62-channel Quik-cap using a NEUVO-64 system (Compumedics, El Paso, TX, USA) before and after VR [37]. The recording lengths were approximately 5 min. To place the electrodes on the scalp, a modified 10/10 system was employed [38]. On the tip of the nose and at the center of the forehead were placed the reference and ground electrodes. Bipolar eye movement electrodes were used to observe eye movement artifacts on the canthus and cheek bone. The amplifiers had bandwidth ranges ranging from 1.0 to 50.0 Hz, and the EEGs were recorded at 1000 Hz. The data were analyzed offline using automatic algorithms performed by the Neuroscan 4.5 software program (Compumedics, El Paso, TX, USA). Eye movements, electro-myographic signals, and other artifacts were visually inspected. Artifact-free EEG fragments were divided into 2 s epochs and underwent Fourier transformation [37]. For each subject, the EEG power values (in µV2/Hz) were averaged within the six standard ranges: theta 1 (4–6 Hz), theta 2 (6–8 Hz), alpha 1 (8–10 Hz), alpha 2 (10–13 Hz), beta 1 (13–20 Hz), and beta 2 (20–30 Hz). The average power ratio between the theta and alpha rhythms was calculated as given in Equation (1):
Power ratio = (theta1 + theta2)/(alpha1 + apha2),
The groups of cardiac surgery patients were assessed using modified Russian versions of the Montreal Cognitive Assessment Scale (MoCA) before study inclusion. Subjects with MoCA scores ≥ 18 were excluded from this study. The baseline cognitive testing was carried out 2–3 days before cardiac surgery. The session of multitasking CT within the VR complex was conducted at 7–10 days after cardiac surgery. Before and after VR training, the patients were assessed by a neurologist. The extensive neuropsychological testing and EEG recording were not conducted to avoid any complications for the patients.
All participants (healthy subjects and cardiac surgery patients) were also asked to complete a series of questionnaires concerning the functionality and friendliness of the system. The System Usability Scale (SUS) was used to evaluate the usability of the products and services. The questionnaire consists of 10 questions with a five-point scale, and the respondents rate their impressions of the system, product, or service [39]. Also, the subjective mental effort questionnaire (SMEQ) was used as a single-item measure of the mental effort required to complete a task (VR training). The SMEQ was created as a vertical slider scale that had a range from 0 to 150. Each participant had to rate using the scale how easy and convenient it was to perform the task [40].
2.4. Statistical Analysis
The variables were analyzed using the Statistica 10.0 software package (StatSoft, Tulsa, OK, USA). The clinical and demographic data are presented as means (M), standard deviation (SD), range, and percentages (%). The Shapiro–Wilk test was used to assess the normality of the distribution. Using the non-parametric Wilcoxon test, quantitative cognitive indicators were analyzed for the pre- and post-VR periods. The log10 transformation was used to normalize the distribution of the EEG data. A paired sample t-test was used to conduct the statistical analyses of the pre- and post-VR EEG power data. The level of significance was set at p < 0.05.
3. Results
3.1. Study 1 (Practically Healthy Subjects)
The neurologist’s examination revealed that a few participants (6/25) experienced dizziness and nausea at the beginning of the experiment. They had minor vection effects after VR.
3.1.1. Cognitive Test Indicators
The results indicate that the healthy subjects after completing one session of VR multitasking CT had significant differences at baseline in the indicators of psychomotor speed and executive function. There was an increase in the psychomotor speed and a decrease in the missed signals in the test of the functional mobility of nervous processes (see Table 2). At the same time, the number of errors increased in the test of the brain’s responses to feedback that is more complex than the previous test. Additionally, the attention indicators were higher after VR, as well as the clock-turn test scores.

Table 2.
Cognitive tests indicators in the healthy participants before and after completing one session of multitasking CT within the VR complex.
3.1.2. EEG Data
The changes in EEG indicators before and after the experiment are presented in Table 3. According to the analysis, the theta 1 power decreased compared to the baseline values. It should be noted that alpha 1 and alpha 2 rhythm power increased, but beta activity did not change significantly.

Table 3.
EEG indicators in the healthy participants before and after completing one session of multitasking CT within the VR complex.
The average power ratio between the theta and alpha rhythms decreased after completing one session of multitasking CT within the VR complex (see Figure 3).
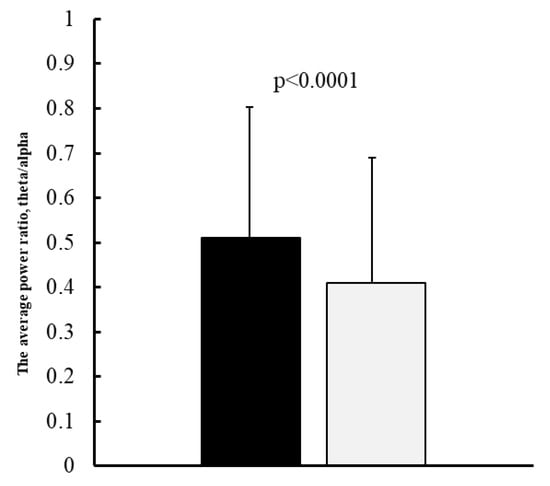
Figure 3.
The average power ratio between the theta and alpha rhythms: dark columns—the indicators before multitasking CT within the VR complex, light columns—the indicators after completing one session of multitasking CT within the VR complex, error bars denote SE.
3.1.3. SUS and SMEQ Scales Data
The healthy group was highly accepting of the intended future use, attitude, and pleasure of the training. The average SUS score was 72.6 ± 11.9, which means a good level of usability of VR multitasking training. The results of the SMEQ scale were surprisingly small (mean score was 13.7; minimum was 1, and maximum was 55) (see Figure 4). We can assume that the healthy participants rated the difficulty of completing the task low due to the lack of competition and social desirability.
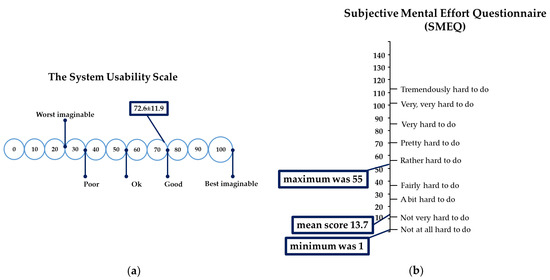
Figure 4.
The results of the SUS (a) and SMEQ (b) scales in the healthy group: in the subfigures, the mean scores and minimum-maximum of appropriate scales are shown.
3.2. Study 2 (Cardiac Surgery Patients)
No complications or pathological symptoms were found in the neurological examination immediately after the VR system was applied. No vection effects after VR were revealed. The survey of cardiac surgery patients revealed that they were enthusiastic about their future use, attitude, and enjoyment of the VR program.
The SUS score of 74.3 ± 6.7 indicated that the cardiac surgery patients considered VR training to be user-friendly (good level) (see Figure 5). The results of the SMEQ scale were also small (mean score 9.6, minimum was 1, maximum was 35). Thus, the difficulty of performing the training was also considered low. We proposed that the likely reason for this was a high level of social desirability.
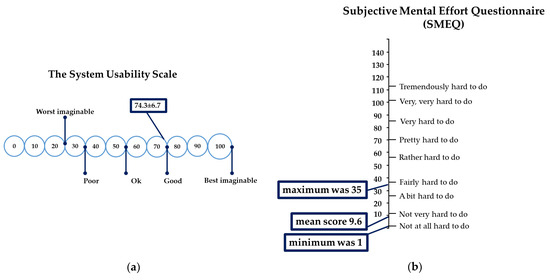
Figure 5.
The results of the SUS (a) and SMEQ (b) scales in the cardiac surgery patients: in the subfigures, the mean scores and minimum-maximum of appropriate scales are shown.
4. Discussion
The purpose of this study was to evaluate the neurophysiological effects of VR during multitasking CT in healthy subjects and the acceptability and feasibility of the original protocol VR multitasking CT in both a healthy group and cardiac surgery patients. Our findings indicated that the healthy individuals demonstrated an increase in psychomotor speed, higher attention indicators, as well as higher mental rotation test scores after completing one session of VR multitasking CT. Additionally, there was a decrease in the missed signals in the executive function test.
The assessment of the influence of VR on the human psychophysiological state is ambiguous, and the data obtained by different authors are often contradictory [23,41,42]. According to J.M. Juliano and her co-authors [41], a higher cognitive load in VR is linked to reduced long-term motor memory formation. In another study, it was shown that healthy individuals were able to successfully adapt to visual-motor rotation [43].
According to our data, healthy subjects can easily adapt to virtual environments because their psychometric indicators improved after VR training. In addition, the healthy subjects considered the task to be easy to complete. Thus, the developed VR paradigm demonstrated acceptable subjective difficulty and tolerability among these participants.
The analysis of the changes in the EEG indicators after the VR experiment revealed that the theta 1 power decreased compared to the baseline values. It should be noted that the alpha 1 and alpha 2 rhythm power increased. Therefore, the theta/alpha ratio decreased.
EEG patterns are among the current methods of neuroimaging that directly reflect the electrical activity of the brain at the level of synapses in real-time. The rhythmic activity in the brain is divided into five main types: delta rhythm, theta rhythm, alpha rhythm, beta rhythm, and gamma rhythm [44]. In the context of this study, the changes in theta and alpha rhythmic activity provided the most important information about the status of the participants in the VR experiment.
Theta rhythm can be detected in the waking state and increases with emotional arousal, fatigue, and drowsiness [45,46]. The power increase in theta activity in the resting-state condition may be considered as a correlate of brain dysfunction [4,37]. A recent study showed that fatigued participants with brain damage who performed a VR balance task demonstrated an increase in the theta power [46]. As demonstrated by our data, VR multitasking training resulted in a decrease in theta power in the healthy subjects. We suggested that the cognitive workload was acceptable, with low subjective difficulty, and caused activation of adaptive processes in the brain.
Alpha rhythm (8–13 Hz) is the main rhythm of the brain, which is recorded in healthy people in the occipital–parietal regions of the brain with closed eyes in a state of calm wakefulness and rest. A decrease in the power of the alpha rhythm is an indicator of cognitive impairment [44]. Previous studies using the EEG method to estimate brain correlations of cognitive load reported that multitasking activity can lead to an increase in alpha power [47]. An increase in alpha power is also caused by monotonous activity. The younger participants showed markedly increased alpha activity during a short (4–5 h) working shift in the post office [48].
The EEG changes in the subjects after VR in our study are in line with previous investigations. A decrease in the theta/alpha ratio is a sign of domination of the alpha activity and reduced levels of theta power [44]. All of this together corresponds to patterns of the optimization of brain activity under the influence of monotonous mental activity.
A positive evaluation of VR multitasking training in cardiac surgery patients was another significant result of our study. It should be noted that the vection effects after VR were not revealed in this group. The VR program’s future use, attitude, and enjoyment were highly rated by the cardiac surgery patients. In addition, the cardiac surgery patients considered VR training to be user-friendly, and the difficulty was also low.
VR is still not widely used in the rehabilitation of cardiac surgery patients. Several studies have demonstrated the positive effects of VR procedures on the mood and functional activity of cardiac surgery patients [49,50,51]. VR motor exercises have been shown to improve functional performance in cardiac surgery patients [49]. Rousseaux and colleagues studied the effects of virtual reality on anxiety, pain, fatigue, and relaxation in cardiac surgery patients [50]. Gerber et al. demonstrated a relaxing effect of VR in critically ill cardiac surgery patients [51]. However, all of these studies were not aimed at cognitive rehabilitation in cardiac surgery patients. In this regard, the developed VR training protocol that was tested on healthy individuals and cardiac surgery patients may be considered an effective tool for preventing POCD in this difficult category of patients.
Study Limitations
First of all, we conducted this study with a small sample. These results should not be considered as definitive data on the impact of the virtual environment on the condition of the trained subjects. Nevertheless, it should be regarded as confirmation of the quality of the VR training paradigm that was developed. Therefore, a replication of this study with a larger sample is necessary for estimating and evaluating the efficacy of rehabilitation. Future research should involve a more comprehensive evaluation of the VR system’s effectiveness through a randomized controlled trial with larger sample sizes and different intervention periods.
5. Conclusions
The results of this study showed that healthy individuals improved their psychomotor speed, attention, and spatial perception after experiencing VR multitasking CT. The increase in alpha activity with a decrease in theta activity can be regarded as a reflection of the optimal brain activity under the monotonic mental load. Also, the original protocol VR multitasking CT showed acceptable subjective difficulty and tolerability in the healthy subjects and cardiac surgery patients. In order to confirm the availability of VR-based multitasking CT for patients with postoperative cognitive dysfunction, further studies are required.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app142310893/s1, Video S1: VR Apple.
Author Contributions
Conceptualization, I.T. and O.T.; methodology, I.T. and O.T.; validation, I.T. and O.T.; formal analysis, I.T.; investigation, D.K., I.K. and A.S.; data curation, D.K., I.K. and A.S.; writing—original draft preparation, I.T.; writing—review and editing, O.T.; project administration, O.T.; funding acquisition, O.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Russian Science Foundation No. 23-15-00379, https://rscf.ru/en/project/23-15-00379/, accessed on 15 May 2023.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the Research Institute for Complex Issues of Cardiovascular Diseases (protocol No. 5 dated 16 May 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author.
Acknowledgments
We gratefully acknowledge the assistance and expert advice from Olga Razumnikova, Novosibirsk State Technical University, Novosibirsk, Russia, as well as the technical support from Sergej Kizilov, the representative of the software company “LABIMMERTEX”, Kemerovo, Russia.
Conflicts of Interest
The authors declare no conflicts of interest. The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A
Cognitive impairment is a deterioration in the activity of higher brain functions and ranges from mild to moderate disorders to more severe ones such as dementia. There are impairments in memory, executive functions, thinking, attention, and visual-spatial perception compared to individual norms [52].
Postoperative cognitive dysfunction (POCD) is a disorder characterized by deterioration of cognitive functions (memory and executive functions) in the early postoperative period and can persist for 3–6 months and 1 year. It occurs mainly in elderly patients due to the influence of several factors of surgery: anesthesia, local and global ischemia, and microembolism [53].
Plastic processes in the brain are the ability of the brain to change and adapt under the influence of experience and learning and create new connections between neurons or modify existing connections [54].
Practically healthy subjects are persons with functional abnormalities in organs and systems that do not affect activity and ability to work. In the context of this study, practically healthy subjects are young people aged 18–30 years who do not have severe concomitant diseases, which is confirmed by the results of the questionnaire “Self-assessment of health status” by V. P. Voitenko [33,55].
Functional class NYHA is a classification of heart failure depending on exercise tolerance. There are four classes: I—there are no symptoms, II—a slight restriction of activity, III—a noticeable restriction, IV—the inability to perform any loads without discomfort. Symptoms of heart failure may include shortness of breath, fatigue, leg swelling, and others [56].
Ejection fraction of left ventricle (LVEF) is an indicator that reflects the volume of blood ejected by the left ventricle of the heart with each contraction. It is calculated as the ratio of stroke volume (the amount of blood that is ejected from the ventricle in one contraction) to the final diastolic volume (the volume of blood in the ventricle before contraction). The normal LVEF value is 50–70%. A decrease in this indicator may indicate heart failure or other heart diseases [57].
Arterial hypertension is a steady increase in blood pressure above 140/90 mm Hg. Art. [58].
Type 2 diabetes mellitus is a chronic endocrine disease that develops due to insulin resistance and impaired function of pancreatic beta cells, characterized by a state of hyperglycemia [59].
Carotid artery stenoses is a condition in which there is a narrowing (stenosis) or complete closure (occlusion) of the carotid artery, which can lead to an increased risk of cerebrovascular events, such as cognitive impairment and stroke [60].
Antiplatelet therapy is a treatment method aimed at preventing the formation of blood clots in blood vessels [61].
Beta-blocker therapy is a treatment method that involves the use of drugs that block beta—adrenergic receptors. These receptors are found in various tissues of the body and respond to adrenaline and norepinephrine, which are stress hormones. They help to lower the heart rate and reduce the myocardial oxygen demand, which leads to lower blood pressure and improved heart function [62].
ACEi therapy (angiotensin-converting-enzyme inhibitors) is a treatment method that involves the use of drugs to treat cardiovascular diseases. They block the enzyme that converts the hormone angiotensin I into angiotensin II, which leads to a decrease in blood pressure and a decrease in the load on the heart [63].
Statin therapy is a group of medications that are used to lower cholesterol levels in the blood. They block an enzyme that is involved in the production of cholesterol in the liver [64].
Cardiopulmonary bypass time is the time during which the patient’s heart and lungs are replaced by a heart–lung machine during cardiac surgery. The artificial blood circulation device circulates blood throughout the body, saturating it with oxygen and removing carbon dioxide. This allows for surgeons to work on a stopped heart. The duration of artificial blood circulation depends on the complexity of the operation, the patient’s condition, and other factors [65].
Electrical activity in the brain is reflected in brain rhythms. Brain rhythms are a regular type of electrical activity that corresponds to a specific brain state and is associated with certain brain mechanisms. There are five main types: delta rhythm, theta rhythm, alpha rhythm, beta rhythm, and gamma rhythm. Electroencephalography (EEG) is the tool used for measuring brain rhythms [44].
Theta rhythm (4–8 Hz) is registered in the waking state and increases with emotional arousal and during drowsiness, mainly in the frontal–central parts of the brain. It is crucial for cognitive processing, in particular learning and memory. An increase in the power of low-frequency activity is a correlate of postoperative brain dysfunction [45,66].
Alpha rhythm (8–13 Hz) is the main rhythm of the brain, which is recorded in healthy people in the occipital–parietal regions of the brain with closed eyes in a state of calm wakefulness and rest. A decrease in the power of the alpha rhythm is an indicator of cognitive impairment [44,67].
Appendix B
| No. | Item | Amount |
| 1 | 27” display MSI G27C4 E2 | 1 |
| 2 | Hori Racing Wheel Apex | 1 |
| 3 | Speakers DEXP R350 | 1 |
| 4 | VR Cover для HP Reverb G2 | 2 |
| 5 | VR headmounted display HP Reverb G2 | 1 |
| 6 | DDR5 ADATA XPG Lancer [AX5U5200C3816G-DCLABK] 32 ГБ | 1 |
| 7 | DEEPCOOL CH560 DIGITAL [R-CH560-BKAPE4D-G-1] system unit | 1 |
| 8 | MSI GeForce RTX 4070 VENTUS 3X E 12G OC graphics card | 1 |
| 9 | MSI MAG Z790 TOMAHAWK WIFI motherboard | 1 |
| 10 | Intel Core i7-13700F chip | 1 |
| 11 | 1000GB SSD M.2 Samsung 980 PRO drive | 1 |
| 12 | OS Microsoft Windows 11 pro, 64 bit | 1 |
References
- Pan, C.W.; Wang, X.; Ma, Q.; Sun, H.P.; Xu, Y.; Wang, P. Cognitive dysfunction and health-related quality of life among older Chinese. Sci. Rep. 2015, 5, 17301. [Google Scholar] [CrossRef] [PubMed]
- Pavel, A.; Paun, R.; Matei, V.; Rosca, A.; Tudose, C. Quality of life in people with subjective cognitive decline. Alpha Psychiatry 2023, 24, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Jongsiriyanyong, S.; Limpawattana, P. Mild cognitive impairment in clinical practice: A review article. Am. J. Alzheimers Dis. Dement. 2018, 33, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Tarasova, I.V.; Trubnikova, O.A.; Barbarash, O.L. EEG and clinical factors associated with mild cognitive impairment in coronary artery disease patients. Dement. Geriatr. Cogn. Disord. 2018, 46, 275–284. [Google Scholar] [CrossRef]
- Lu, Y.; Zhu, Y.; Ma, Y.; Li, C.; Hua, R.; Zhong, B.; Wang, H.; Xie, W. Association of subclinical atherosclerosis and cognitive decline: A community-based cross-sectional study. BMJ Open 2022, 12, e059024. [Google Scholar] [CrossRef]
- Bangen, K.J.; Werhane, M.L.; Weigand, A.J.; Edmonds, E.C.; Delano-Wood, L.; Thomas, K.R.; Nation, D.A.; Evangelista, N.D.; Clark, A.L.; Liu, T.T.; et al. Reduced regional cerebral blood flow relates to poorer cognition in older adults with type 2 diabetes. Front. Aging Neurosci. 2018, 10, 270. [Google Scholar] [CrossRef]
- Rundek, T.; Tolea, M.; Ariko, T.; Fagerli, E.A.; Camargo, C.J. Vascular cognitive impairment (VCI). Neurotherapeutics 2022, 19, 68–88. [Google Scholar] [CrossRef]
- Chudiak, A.; Uchmanowicz, I.; Mazur, G. Relation between cognitive impairment and treatment adherence in elderly hypertensive patients. Clin. Interv. Aging 2018, 13, 1409–1418. [Google Scholar] [CrossRef]
- Indja, B.; Seco, M.; Seamark, R.; Kaplan, J.; Bannon, P.G.; Grieve, S.M.; Vallely, M.P. Neurocognitive and psychiatric issues post cardiac surgery. Heart Lung Circ. 2017, 26, 779–785. [Google Scholar] [CrossRef]
- Tarasova, I.V.; Trubnikova, O.A.; Syrova, I.D.; Barbarash, O.L. Long-term neurophysiological outcomes in patients undergoing coronary artery bypass grafting. Braz. J. Cardiovasc. Surg. 2021, 36, 629–638. [Google Scholar] [CrossRef]
- Weimar, C.; Bilbilis, K.; Rekowski, J.; Holst, T.; Beyersdorf, F.; Breuer, M.; Dahm, M.; Diegeler, A.; Kowalski, A.; Martens, S.; et al. Safety of simultaneous coronary artery bypass grafting and carotid endarterectomy versus isolated coronary artery bypass grafting: A randomized clinical trial. Stroke 2017, 48, 2769–2775. [Google Scholar] [CrossRef] [PubMed]
- Suraarunsumrit, P.; Pathonsmith, C.; Srinonprasert, V.; Sangarunakul, N.; Jiraphorncharas, C.; Siriussawakul, A. Postoperative cognitive dysfunction in older surgical patients associated with increased healthcare utilization: A prospective study from an upper-middle-income country. BMC Geriatr. 2022, 22, 213. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Chen, Y.; Zhang, P.; Chen, G.; Zhou, Y.; Yu, X. The potential mechanism of postoperative cognitive dysfunction in older people. Exp. Gerontol. 2020, 130, 110791. [Google Scholar] [CrossRef]
- Phirom, K.; Kamnardsiri, T.; Sungkarat, S. Beneficial effects of interactive physical-cognitive game-based training on fall risk and cognitive performance of older adults. Int. J. Environ. Res. Public. Health 2020, 17, 6079. [Google Scholar] [CrossRef]
- Gavelin, H.M.; Dong, C.; Minkov, R.; Bahar-Fuchs, A.; Ellis, K.A.; Lautenschlager, N.T.; Mellow, M.L.; Wade, A.T.; Smith, A.E.; Finke, C.; et al. Combined physical and cognitive training for older adults with and without cognitive impairment: A systematic review and network meta-analysis of randomized controlled trials. Ageing Res. Rev. 2021, 66, 101232. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Zou, G.; Speechley, M.; Almeida, Q.J.; Liu-Ambrose, T.; Middleton, L.E.; Camicioli, R.; Bray, N.W.; Li, K.Z.H.; Fraser, S.; et al. Effects of exercise alone or combined with cognitive training and vitamin d supplementation to improve cognition in adults with mild cognitive impairment: A randomized clinical trial. JAMA Netw. Open. 2023, 6, e2324465. [Google Scholar] [CrossRef]
- Lin, Y.P.; Lin, I.I.; Chiou, W.D.; Chang, H.C.; Chen, R.S.; Lu, C.S.; Chang, Y.J. The executive-function-related cognitive-motor dual task walking performance and task prioritizing effect on people with Parkinson’s disease. Healthcare 2023, 11, 567. [Google Scholar] [CrossRef]
- Syrova, I.D.; Tarasova, I.V.; Trubnikova, O.A.; Kupriyanova, D.S.; Sosnina, A.S.; Temnikova, T.B.; Barbarash, O.L. A multitask approach to prevention of the cognitive decline after coronary artery bypass grafting: A prospective randomized controlled study. J. Xiangya Med. 2023, 8, 2. [Google Scholar] [CrossRef]
- Hassandra, M.; Galanis, E.; Hatzigeorgiadis, A.; Goudas, M.; Mouzakidis, C.; Karathanasi, E.M.; Petridou, N.; Tsolaki, M.; Zikas, P.; Evangelou, G.; et al. A virtual reality app for physical and cognitive training of older people with mild cognitive impairment: Mixed methods feasibility study. JMIR Serious Games 2021, 9, e24170. [Google Scholar] [CrossRef]
- Bosch-Barceló, P.; Climent-Sanz, C.; Martínez-Navarro, O.; Masbernat-Almenara, M.; Pakarinen, A.; Ghosh, P.K.; Fernández-Lago, H. A treadmill training program in a gamified virtual reality environment combined with transcranial direct current stimulation in Parkinson’s Disease: Study protocol for a randomized controlled trial. PLoS ONE 2024, 19, e0307304. [Google Scholar] [CrossRef]
- Kang, J.M.; Kim, N.; Lee, S.Y.; Woo, S.K.; Park, G.; Yeon, B.K.; Park, J.W.; Youn, J.H.; Ryu, S.H.; Lee, J.Y.; et al. Effect of cognitive training in fully immersive virtual reality on visuospatial function and frontal-occipital functional connectivity in predementia: Randomized controlled trial. J. Med. Internet Res. 2021, 23, e24526. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Park, J.H. Ecological effects of VR-based cognitive training on ADL and IADL in MCI and AD patients: A systematic review and meta-analysis. Int. J. Environ. Res. Public. Health 2022, 19, 15875. [Google Scholar] [CrossRef] [PubMed]
- Baldimtsi, E.; Mouzakidis, C.; Karathanasi, E.M.; Verykouki, E.; Hassandra, M.; Galanis, E.; Hatzigeorgiadis, A.; Goudas, M.; Zikas, P.; Evangelou, G.; et al. Effects of virtual reality physical and cognitive training intervention on cognitive abilities of elders with mild cognitive impairment. J. Alzheimers Dis. Rep. 2023, 7, 1475–1490. [Google Scholar] [CrossRef]
- Feng, H.; Li, C.; Liu, J.; Wang, L.; Ma, J.; Li, G.; Gan, L.; Shang, X.; Wu, Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: A randomized controlled trial. Med. Sci. Monit. 2019, 25, 4186–4192. [Google Scholar] [CrossRef]
- Saeedi, S.; Ghazisaeedi, M.; Rezayi, S. Applying game-based approaches for physical rehabilitation of poststroke patients: A systematic review. J. Healthcare Eng. 2021, 2021, 9928509. [Google Scholar] [CrossRef]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.D.; Rizzo, A.; Loetscher, T. Factors associated with virtual reality sickness in head-mounted displays: A systematic review and meta-analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef]
- Kooijman, L.; Berti, S.; Asadi, H.; Nahavandi, S.; Keshavarz, B. Measuring vection: A review and critical evaluation of different methods for quantifying illusory self-motion. Behav. Res. Methods 2024, 56, 2292–2310. [Google Scholar] [CrossRef]
- Luu, W.; Zangerl, B.; Kalloniatis, M.; Kim, J. Effects of stereopsis on vection, presence and cybersickness in head-mounted display (HMD) virtual reality. Sci. Rep. 2021, 11, 12373. [Google Scholar] [CrossRef]
- Khoo, S.Y.; Lai, W.H.; On, S.H.; On, Y.Y.; Adam, B.M.; Law, W.C.; Ng, B.H.S.; Fong, A.Y.Y.; Anselm, S.T. Resting-state electroencephalography (EEG) microstates of healthy individuals following mild sleep deprivation. Sci. Rep. 2024, 14, 16820. [Google Scholar] [CrossRef]
- Shivdat, S.; Zhan, T.; De Palma, A.; Zheng, W.L.; Krishnamurthy, P.; Paneerselvam, E.; Snider, S.; Bevers, M.; O’Reilly, U.M.; Lee, J.W.; et al. Early burst suppression similarity association with structural brain injury severity on MRI after cardiac arrest. Neurocrit. Care 2024. online ahead of print. [Google Scholar] [CrossRef]
- Gangemi, A.; De Luca, R.; Fabio, R.A.; Lauria, P.; Rifici, C.; Pollicino, P.; Marra, A.; Olivo, A.; Quartarone, A.; Calabrò, R.S. Effects of virtual reality cognitive training on neuroplasticity: A quasi-randomized clinical trial in patients with stroke. Biomedicines 2023, 11, 3225. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Leo, A.; De Luca, R.; Balletta, T.; Buda, A.; La Rosa, G.; Bramanti, A.; Bramanti, P. The role of virtual reality in improving motor performance as revealed by EEG: A randomized clinical trial. J. Neuroeng. Rehabil. 2017, 14, 53. [Google Scholar] [CrossRef] [PubMed]
- Vojtenko, V.P. Health of Healthy People: Introduction to Sanology; Health: Kyiv, Ukraine, 1991; 245p. [Google Scholar]
- Papandrea, M.; Peternier, A.; Frei, D.; La Porta, N.; Gelsomini, M.; Allegri, D.; Leidi, T. V-Cockpit: A Platform for the design, testing, and validation of car infotainment systems through virtual reality. Appl. Sci. 2024, 14, 8160. [Google Scholar] [CrossRef]
- Guyer, G.; Mueller, S.; Wyss, Y.; Bertholet, J.; Schmid, R.; Stampanoni, M.F.M.; Manser, P.; Fix, M.K. Technical note: A collision prediction tool using Blender. J. Appl. Clin. Med. Phys. 2023, 24, e14165. [Google Scholar] [CrossRef]
- Trubnikova, O.A.; Tarasova, I.V.; Moskin, E.G.; Kupriyanova, D.S.; Argunova, Y.A.; Pomeshkina, S.A.; Gruzdeva, O.V.; Barbarash, O.L. Beneficial effects of a short course of physical prehabilitation on neurophysiological functioning and neurovascular biomarkers in patients undergoing coronary artery bypass grafting. Front. Aging Neurosci. 2021, 13, 699259. [Google Scholar] [CrossRef]
- Tarasova, I.; Trubnikova, O.; Kupriyanova, D.; Kukhareva, I.; Syrova, I.; Sosnina, A.; Maleva, O.; Barbarash, O. Effect of carotid stenosis severity on patterns of brain activity in patients after cardiac surgery. Appl. Sci. 2023, 13, 20. [Google Scholar] [CrossRef]
- Jurcak, V.; Tsuzuki, D.; Dan, I. 10/20, 10/10, and 10/5 systems revisited: Their validity as relative head-surface-based positioning systems. NeuroImage 2007, 34, 1600–1611. [Google Scholar] [CrossRef]
- Lloréns, R.; Noé, E.; Colomer, C.; Alcañiz, M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2015, 96, 418–425.e2. [Google Scholar] [CrossRef]
- Metzemaekers, J.; Haazebroek, P.; Smeets, M.J.G.H.; English, J.; Blikkendaal, M.D.; Twijnstra, A.R.H.; Adamson, G.D.; Keckstein, J.; Jansen, F.W. EQUSUM: Endometriosis QUality and grading instrument for SUrgical performance: Proof of concept study for automatic digital registration and classification scoring for r-ASRM, EFI and Enzian. Hum. Reprod. Open. 2020, 2020, hoaa053. [Google Scholar] [CrossRef]
- Juliano, J.M.; Schweighofer, N.; Liew, S.L. Increased cognitive load in immersive virtual reality during visuomotor adaptation is associated with decreased long-term retention and context transfer. J. Neuroeng. Rehabil. 2022, 19, 106. [Google Scholar] [CrossRef]
- Jeong, S.; Kim, J.; Lee, J. The differential effects of multisensory attentional cues on task performance in VR depending on the level of cognitive load and cognitive capacity. IEEE Trans. Vis. Comput. Graph. 2024, 30, 2703–2712. [Google Scholar] [CrossRef]
- Anglin, J.M.; Sugiyama, T.; Liew, S.L. Visuomotor adaptation in head-mounted virtual reality versus conventional training. Sci. Rep. 2017, 7, 45469. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Barry, R.J.; Başar, E.; Blinowska, K.J.; Cichocki, A.; Drinkenburg, W.H.; Klimesch, W.; Knight, R.T.; da Silva, F.L.; Nunez, P.; et al. International Federation of Clinical Neurophysiology (IFCN)—EG research workgroup: Recommendations on frequency and topographic analysis of resting state EEG rhythms. Part 1: Applications in clinical research studies. Clin. Neurophysiol. 2020, 131, 285–307. [Google Scholar] [CrossRef] [PubMed]
- Soltani Zangbar, H.; Ghadiri, T.; Seyedi Vafaee, M.; Ebrahimi Kalan, A.; Fallahi, S.; Ghorbani, M.; Shahabi, P. Theta oscillations through hippocampal/prefrontal pathway: Importance in cognitive performances. Brain Connect. 2020, 10, 157–169. [Google Scholar] [CrossRef]
- Sandri Heidner, G.; O’Connell, C.; Domire, Z.J.; Rider, P.; Mizelle, C.; Murray, N.P. Concussed neural signature is substantially different than fatigue neural signature in non-concussed controls. J. Mot. Behav. 2023, 55, 302–312. [Google Scholar] [CrossRef]
- Puma, S.; Matton, N.; Paubel, P.V.; Raufaste, É.; El-Yagoubi, R. Using theta and alpha band power to assess cognitive workload in multitasking environments. Int. J. Psychophysiol. 2018, 123, 111–120. [Google Scholar] [CrossRef]
- Wascher, E.; Heppner, H.; Kobald, S.O.; Arnau, S.; Getzmann, S.; Möckel, T. Age-sensitive effects of enduring work with alternating cognitive and physical load. A study applying mobile EEG in a real-life working scenario. Front. Hum. Neurosci. 2016, 9, 711. [Google Scholar] [CrossRef]
- Cacau, L.d.A.; Oliveira, G.U.; Maynard, L.G.; Araújo Filho, A.A.; Silva, W.M., Jr.; Cerqueria Neto, M.L.; Antoniolli, A.R.; Santana-Filho, V.J. The use of the virtual reality as intervention tool in the postoperative of cardiac surgery. Rev. Bras. Cir. Cardiovasc. 2013, 28, 281–289. [Google Scholar] [CrossRef]
- Rousseaux, F.; Faymonville, M.E.; Nyssen, A.S.; Dardenne, N.; Ledoux, D.; Massion, P.B.; Vanhaudenhuyse, A. Can hypnosis and virtual reality reduce anxiety, pain and fatigue among patients who undergo cardiac surgery: A randomised controlled trial. Trials 2020, 21, 330. [Google Scholar] [CrossRef]
- Gerber, S.M.; Jeitziner, M.M.; Knobel, S.E.J.; Mosimann, U.P.; Müri, R.M.; Jakob, S.M.; Nef, T. Perception and Performance on a Virtual Reality Cognitive Stimulation for Use in the Intensive Care Unit: A Non-randomized Trial in Critically Ill Patients. Front. Med. 2019, 6, 287. [Google Scholar] [CrossRef]
- Pérez Palmer, N.; Trejo Ortega, B.; Joshi, P. Cognitive Impairment in Older Adults: Epidemiology, Diagnosis, and Treatment. Psychiatr. Clin. North. Am. 2022, 45, 639–661. [Google Scholar] [CrossRef]
- Varpaei, H.A.; Farhadi, K.; Mohammadi, M.; Khafaee Pour Khamseh, A.; Mokhtari, T. Postoperative cognitive dysfunction: A concept analysis. Aging Clin. Exp. Res. 2024, 36, 133. [Google Scholar] [CrossRef] [PubMed]
- Kaleev, O.F.; Kaleva, N.G.; Yashin, D.A. QUALITY OF HUMAN HEALTH//Contemporary Problems of Science and Education. 2016. Available online: https://science-education.ru/en/article/view?id=25004 (accessed on 10 October 2024).
- Innocenti, G.M. Defining neuroplasticity. Handb. Clin. Neurol. 2022, 184, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Bredy, C.; Ministeri, M.; Kempny, A.; Alonso-Gonzalez, R.; Swan, L.; Uebing, A.; Diller, G.P.; Gatzoulis, M.A.; Dimopoulos, K. New York Heart Association (NYHA) classification in adults with congenital heart disease: Relation to objective measures of exercise and outcome. Eur. Heart J. Qual. Care Clin. Outcomes 2018, 4, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Kosaraju, A.; Goyal, A.; Grigorova, Y.; Makaryus, A.N. Left Ventricular Ejection Fraction; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Al Ghorani, H.; Götzinger, F.; Böhm, M.; Mahfoud, F. Arterial hypertension—Clinical trials update 2021. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 21–31. [Google Scholar] [CrossRef]
- Tinajero, M.G.; Malik, V.S. An Update on the Epidemiology of Type 2 Diabetes: A Global Perspective. Endocrinol. Metab. Clin. North. Am. 2021, 50, 337–355. [Google Scholar] [CrossRef]
- Ismail, A.; Ravipati, S.; Gonzalez-Hernandez, D.; Mahmood, H.; Imran, A.; Munoz, E.J.; Naeem, S.; Abdin, Z.U.; Siddiqui, H.F. Carotid Artery Stenosis: A Look Into the Diagnostic and Management Strategies, and Related Complications. Cureus 2023, 15, e38794. [Google Scholar] [CrossRef]
- Chandiramani, R.; Spirito, A.; Johnson, J.W.; Mehta, A.; Vogel, B.; Faillace, R.T.; Mehran, R. Antiplatelet therapy for coronary artery disease in 2023: Current status and future prospects. Expert Rev. Cardiovasc. Ther. 2023, 21, 311–328. [Google Scholar] [CrossRef]
- Ogrodowczyk, M.; Dettlaff, K.; Jelinska, A. Beta-Blockers: Current State of Knowledge and Perspectives. Mini Rev. Med. Chem. 2016, 16, 40–54. [Google Scholar] [CrossRef]
- Turner, J.M.; Kodali, R. Should Angiotensin-Converting Enzyme Inhibitors ever Be Used for the Management of Hypertension? Curr. Cardiol. Rep. 2020, 22, 95. [Google Scholar] [CrossRef]
- Koch, C.G. Statin therapy. Curr. Pharm. Des. 2012, 18, 6284–6290. [Google Scholar] [CrossRef]
- Hessel, E.A., 2nd. What’s New in Cardiopulmonary Bypass. J. Cardiothorac. Vasc. Anesth. 2019, 33, 2296–2326. [Google Scholar] [CrossRef] [PubMed]
- Girardeau, G.; Lopes-Dos-Santos, V. Brain neural patterns and the memory function of sleep. Science 2021, 374, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Lopez, S.; Hampel, H.; Chiesa, P.A.; Del Percio, C.; Noce, G.; Lizio, R.; Teipel, S.J.; Dyrba, M.; González-Escamilla, G.; Bakardjian, H.; et al. The association between posterior resting-state EEG alpha rhythms and functional MRI connectivity in older adults with subjective memory complaint. Neurobiol. Aging 2024, 137, 62–77. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).