Abstract
Background: Humans encounter disturbances like slips, pushes, and trips while walking, mainly from external forces. Technological advances have improved methods to study these impacts on gait, with split-belt treadmills being particularly effective. This scoping review aims to examine the types of perturbations used during split-belt treadmill gait, explore the methods used to induce them, and consolidate current knowledge on the effects of split-belt treadmill-induced gait perturbations. Methods: The review included publications from January 2015 to May 2024, as searched via PubMed, EBSCO, and ScienceDirect. Results: The review examined 33 studies on split-belt treadmills, focusing on perturbations like slip-like, trip-like, lateral displacements, and tilts, with speed changes being the most common. Perturbations were mainly applied during initial contact. The results show that young, healthy adults adapt quickly to anticipatory and reactive adjustments, while older adults and those with neurological impairments use less efficient strategies like increased muscular co-contraction. Asymmetrical gait adaptations persist after perturbations, highlighting motor learning and the role of the central nervous system and sensory feedback. Conclusions: Despite their precision, split-belt and tilting treadmills may not fully replicate real-world walking complexities. The review highlights the strengths and limitations of split-belt treadmills, emphasizing the need to integrate diverse methods to enhance rehabilitation and improve gait stability.
1. Introduction
Walking is a fundamental human activity that allows for movement and the performance of daily tasks, playing a vital role in maintaining independence and enhancing the quality of life. Walking involves the coordinated, alternating movements of the lower and upper limbs, constantly responding to stimuli processed by the nervous system. Consequently, gait analysis has become a critical area of research within biomechanics and neuroscience, offering insights into the intricate processes that govern human movement [1]. Understanding how individuals maintain stability during walking, especially when subjected to unexpected disturbances, is essential for developing strategies to prevent falls and improve overall mobility [2,3,4].
Perturbations, defined as unexpected disturbances, are used across various scientific fields and contexts. In physics, perturbation refers to a sudden change or disruption in the equilibrium state of a system, affecting its motion, structure, or properties [5,6]. In biology, perturbations include sudden environmental modifications that affect function, adaptation, or health. In biomechanics, perturbation refers to sudden changes in movement conditions or loads that affect the mechanical behavior of the organism. These perturbations can arise from various sources, such as changes in terrain [7,8], obstacles [9], or internal conditions like balance disorders [3].
Over the years, researchers have employed various methods to induce perturbations and study their effects on human gait. Traditional methods include changes in speeds on single-belt treadmills and the stimulation of lower limb nerves, as seen in Berger et al.’s [10] study. Other techniques involve pushing or pulling subjects using hydraulic systems [11], simulating slips through floor friction modulation (e.g., by pouring oil on the path) [12,13], introducing trips by placing obstacles in the subject’s path, and manipulating the entire treadmill with lateral shifts or sudden tilting [14,15]. Additionally, perturbations had been triggered by manipulating sensory inputs such as light, sound, and temperature, further broadening the scope of gait stability research [16]. With advancements in technology, virtual reality (VR) has also been used to simulate various terrain conditions and induce perturbations in a controlled manner [17]. VR allows researchers to create immersive environments that mimic real-world challenges, providing a versatile and highly controlled method for studying gait adaptation and balance recovery.
Each type of disturbance offers valuable insights into an individual’s ability to maintain balance and adapt to different walking conditions. These studies are essential for developing effective interventions and devices to improve safety and quality of life, particularly for those at higher risk of falls, such as older adults and individuals with neurological impairments [18,19,20]. Traditional methods of inducing gait perturbations, such as manual pushes or pulls, sudden changes in treadmill speed, and the introduction of obstacles, each have advantages and limitations. Manual pushes or pulls can provide direct perturbations but of-ten lack precision and reproducibility [21]. Sudden changes in treadmill speed can simulate real-world challenges but may not accurately reflect the nuanced disturbances encountered during daily activities. Introducing obstacles can create realistic scenarios, though controlling the timing and nature of these perturbations can be challenging. Despite their effectiveness, these methods often do not provide the control and specificity required for detailed gait analysis.
In contrast, the split-belt treadmill offers a more sophisticated approach by operating its belts at different speeds, thus introducing specific and controlled asymmetrical perturbations to an individual’s gait [2,4]. This advanced setup allows researchers to dissect the adaptive mechanisms of gait in response to asymmetrical walking conditions. The split-belt treadmill’s ability to independently adjust the speed of each belt provides a nuanced understanding of how individuals respond to these conditions. By simulating real-world challenges in a controlled environment, this method proves invaluable for studying gait stability.
The split-belt treadmill enables the examination of various adaptive strategies, such as altering step length, timing, and coordination between limbs, which are crucial for maintaining balance and preventing falls [4]. These treadmills offer precise control of perturbation timing, magnitude, and direction, offering detailed insight into adaptive responses during walking. It is particularly relevant for populations vulnerable to gait instability, including older adults and individuals with neurological impairments. For example, older adults often exhibit slower and less adaptable responses to perturbations, making them more susceptible to falls [22]. Individuals with neurological impairments, such as stroke survivors, may have asymmetric gait patterns and reduced adaptive capacity, which can be effectively studied using the split-belt treadmill [23]. This scoping review aims to examine the types of perturbations used during split-belt treadmill gait, explore the methods used to induce them, and consolidate current knowledge on the effects of split-belt treadmill-induced gait perturbations. By examining various studies, we seek to understand the strategies employed by individuals to maintain balance and adapt their gait. Understanding these strategies can significantly improve the development of fall prevention programs for older adults and inform gait reeducation in post-traumatic rehabilitation. Research on gait perturbations has practical value in refining rehabilitation protocols, such as split-belt treadmill training for stroke survivors [23,24], to improve balance and coordination. It also supports the development of assistive devices like exoskeletons [25] for those with mobility impairments and strengthens fall prevention strategies. These advancements improve mobility, reduce injury risks, and enhance the quality of life for vulnerable populations.
2. Materials and Methods
This review was not registered in the PROSPERO Register of Systematic Reviews or the Open Science Framework. However, it was conducted and reported following the PRISMA 2020 guidelines [26,27,28].
2.1. Search Strategy
This review focused on studies that used a two-lane treadmill to induce gait perturbations. Two authors (R.B. and K.C.) independently conducted an electronic search of PubMed, Science-Direct, and EBSCO databases in April/May 2024. The search was limited to papers published between January 2015 and 2024 and included the following terms: “perturbation AND split-belt treadmill”; “slip AND gait AND adult”; “trip AND walk AND split-belt”; “perturbation AND walk AND dual-belt treadmill”; “slip-like AND gait AND adult”.
2.2. Eligibility
Only full-text articles in English, published from 2015 onwards, were selected from the electronic databases. The inclusion criteria contained (1) studies involving human adult participants; (2) research focusing on various mechanical perturbations during walking; (3) usage of a split-belt treadmill; (4) peer-reviewed full scientific articles; and (5) availability in the English language. Exclusion criteria were as follows: (1) publications in languages other than English; (2) conference materials; (3) reviews and meta-analyses; (4) studies involving minors; (5) perturbations induced by visual displays or body part vibrations; and (6) mechanical perturbations occurring under static conditions or during activities other than walking, such as running or jumping. In addition, studies involving treadmill perturbations, in which the treadmill belt speed did not return to the initial value but persisted for several steps after the change, were excluded. Studies were excluded if they involved perturbations, such as pull or push, that were not treadmill related. Additionally, publications focusing solely on individuals with disabilities were excluded. However, studies comparing individuals with disabilities to a control group of healthy individuals were retained.
2.3. Review Process
Duplicate articles from different sources were removed. Titles, abstracts, and full texts of retrieved documents were sequentially reviewed by two authors (KC and RB) to determine their relevance to the topic. Furthermore, the reference lists of all studies included for review were searched manually for additional studies of relevance. In case of doubt, the MB resolved the issue and decided whether to include or exclude the paper in the review. The publications finally included in the review were checked and approved by author M.B. M.B. compiled all articles using reference management software (EndNote X7.7, Clarivate Analytics, Philadelphia, PA, USA).
2.4. Quality Assessment
KC assessed the methodological quality of each eligible paper. MB revised the process. A checklist for both randomized and non-randomized studies was used [29]. This checklist encompassed five sub-scales: (1) Reporting (questions 1–10), with 10 items evaluating the adequacy of information provided to facilitate an unbiased assessment of study outcomes; (2) External validity (questions 11–13), with 3 items assessing the extent to which findings could be extrapolated to the broader population; (3) Internal validity—Bias (questions 14–20), encompassing 7 items addressing potential biases in intervention and outcome measurement; (4) Internal validity—Confounding (selection bias: questions 21–26), consisting of 6 items for detecting biases in participant selection; and (5) Power, featuring 1 item (question 27) designed to determine if adverse study outcomes might be attributable to chance.
Therefore, the checklist included the following items [29]: 1. Is the hypothesis/aim/objective of the study clearly described? 2. Should the main outcomes be measured and clearly described in the Introduction or Methods section? 3. Are the characteristics of the patients included in the study clearly described? 4. Are the interventions of interest clearly described? 5. Are the descriptions of the distributions of principal confounders in each group of subjects clear? 6. Are the main findings of the study clearly described? 7. Does the study provide estimates of the random variability in the data for the main outcomes? 8. Have all the important adverse events that may be a consequence of the intervention been reported? 9. Have the characteristics of patients lost to follow-up been described? 10. Have actual probability values been reported (e.g., 0.035 rather than <0.05) for the main outcomes except where the probability value is less than 0.001? 11. Were the subjects asked to participate in the study representative of the entire population from which they were recruited? 12. Were those subjects prepared to participate representative of the entire population from which they were recruited? 13. Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? 14. Was an attempt made to blind study subjects to the intervention they have received? 15. Was an attempt made to blind those measuring the main outcomes of the intervention? 16. If any of the study results were based on “data dredging”, was this made clear? 17. In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or in case-control studies, is the period between the intervention and outcome the same for cases and controls ? 18. Were the statistical tests used to assess the main outcomes appropriate? 19. Was compliance with the intervention/s reliable? 20. Were the main outcome measures used accurate (valid and reliable)? 21. Were the patients in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited from the same population? 22. Were study subjects in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited over the same period? 23. Were study subjects randomized to intervention groups? 24. Was the randomized intervention assignment concealed from patients and health care staff until recruitment was complete and irrevocable? 25. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? 26. Were losses of patients to follow-up taken into account? 27. Did the study have sufficient power to detect a clinically important effect where the probability value for a difference due to chance is less than 5%? Answers were scored 0 or 1, except for one item no. 5 in the Reporting subscale, which scored 0 to 2, and the single item on power, which was scored 0 to 5. The maximum possible score was 32.
3. Results
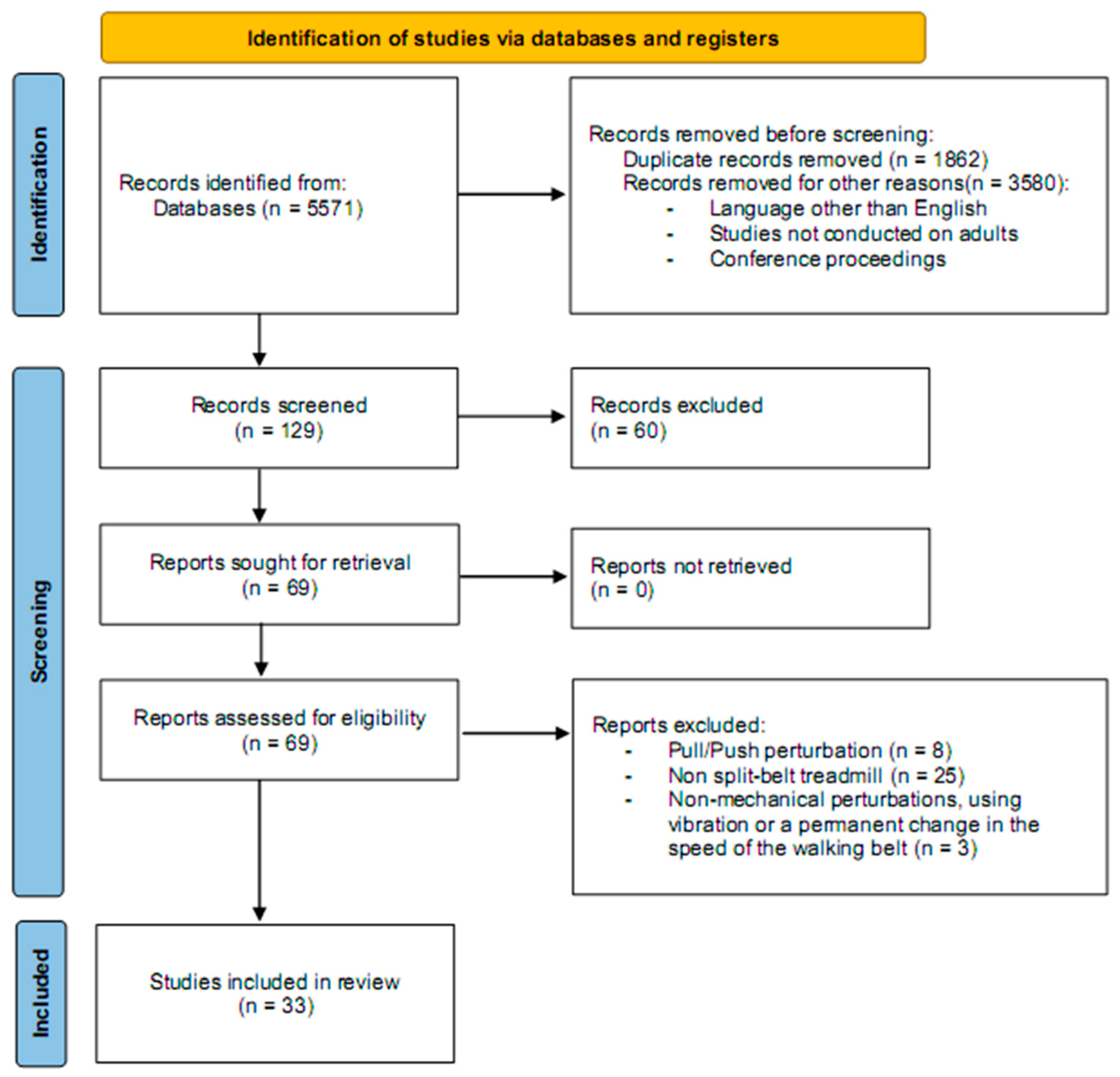
The initial search of electronic databases yielded 5571 articles. A total of 5442 articles were excluded in the first approach. These included 1862 duplicates and 3580 removed for the following reasons: papers in languages other than English, studies not conducted on adults, and conference proceedings. Following this process, 129 documents remained for further analysis. Ninety-six articles were excluded from this pool because the perturbations were not performed on a split-belt treadmill, involved movements other than walking, or were induced by vibrations or pull/push forces. Studies were also excluded if the treadmill speed did not return to the initial value following the perturbation. In total, 33 articles were selected for the review process (Figure 1).
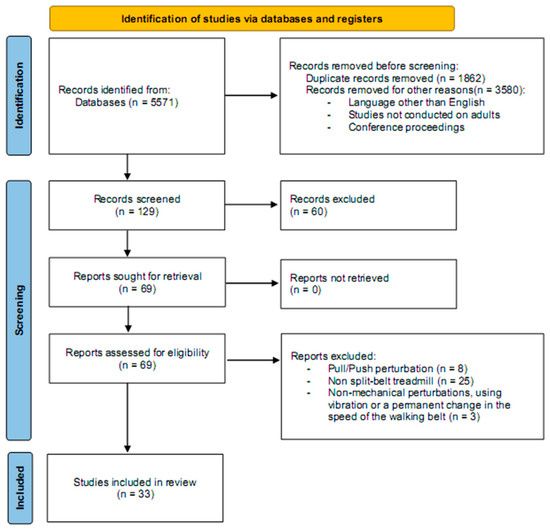
Figure 1.
A flowchart demonstrating the selection of articles through the review process [26,27].
The following items were selected from the papers included in this review: participant characteristics, study objectives, participant tasks, and result descriptions. Additionally, the review provided detailed information about the equipment used, the timing of perturbation application, and the characteristics of these perturbations, including their intensity, duration, and the specific lower limb targeted. The papers were categorized based on the direction of the perturbations: Table 1 includes 18 papers describing anterior–posterior (AP) perturbations, while Table 2 focuses on mediolateral (ML) perturbations, comprising 15 manuscripts. The articles were organized chronologically within each table, from the oldest to the most recent.

Table 1.
Papers reporting the results of perturbations in the anterior–posterior (AP) direction.
The quality assessment scores of the included papers ranged from 11 to 18 in Table 1 and from 13 to 17 in Table 2. The mean score for papers from Table 1 was 15.61 ± 1.72, while articles from Table 2 had a mean score of 15.47 ± 1.36. These values were mainly affected by receiving no points for two questions in the Internal Validity—Bias section (questions 15 and 16) and questions 21 to 26 in the Internal Validity—Confounding section.
3.1. Perturbations in the Anterior–Posterior (AP) Direction
Table 1 features 18 studies where perturbations were induced in the AP direction. The papers in this table were divided into three groups. The first group included nine articles where perturbations were caused by the acceleration of one treadmill belt. The second group comprised three studies where perturbations were induced by decelerating a treadmill belt. The third group contained six papers where both the acceleration and deceleration of the treadmill belt were used to perturb the subjects.
Working on a split-belt treadmill enabled the generation of perturbations, which the authors described as slipping-like (9 papers) or tripping-like (3 papers). In most studies [30,31,32,33,34,35,36], slip-like perturbations were induced by unexpectedly accelerating one belt during the IC phase. This sudden acceleration caused the foot to slide forward rapidly, leading to a backward loss of balance. A trip-like perturbation was induced by treadmill belt deceleration [19,38], causing forward balance loss as the foot unexpectedly slowed down.
3.1.1. Characteristics of Participants
Most studies were conducted on young adults, accounting for 13 publications. Two studies focused on older adults [38,43], with one comparing older adults with knee osteoarthritis (KOA) to those without KOA [43]. Ren, et al. [38] studied slip-like perturbations. While Ren, et al. [43] examined responses to both slip- and trip-like perturbations. Three publications compared responses elicited by unexpected slip-like perturbations in older adults and young adults [31,32,42]. In addition, Ren, et al. [42] investigated the first recovery step following tripping.
The number of subjects varied across the studies. Aprigliano, et al. [45] studied only five young people, and this was the smallest group. On the other hand, Swart, et al. [34] and Ren, et al. [42] had the largest groups, with 30 participants each. Most studies included both men and women, but some focused exclusively on one gender: Hirata, et al. [36] and Shokouhi, et al. [19] studied only men, while Ciunelis, et al. [4] and Błażkiewicz and Hadamus [2] studied only women.
Each paper provided information on the subjects’ characteristics, including age, height, and weight. However, half of the manuscripts did not specify the dominance of the lower limb. In the remaining nine studies, the right limb was dominant. In ten papers, the authors perturbed the right side. Błażkiewicz and Hadamus [2], Ciunelis, et al. [4], and Lee, et al. [41] chose to perturb the left side of the body. In contrast, in five papers [31,36,37,40,45], the authors perturbed two lower limbs.
3.1.2. Measurement Tools
Various tools were used to capture data during perturbations, including high-frequency treadmills (e.g., 1000 Hz), motion capture systems (e.g., Vicon, Nexus 2.2), and electromyography (EMG). Sixteen studies used motion capture, mostly Vicon systems at 100 Hz. However, two studies did not use motion capture systems: Swart, et al. [34] relied on GRF data, and Mueller, et al. [40] utilized EMG. Additionally, EMG was used by Lee, et al. [41].
Seven types of treadmills were used for measurements and inducing perturbations. The most frequently used was the Motek Grail treadmill [2,4,33,38,42,43]. Ciunelis, et al. [4] and Van den Bogaart, et al. [33] introduced slipping-like perturbations. Ren, et al. [38] used it for trip-like perturbations. Three studies examined both perturbation types. The Caren Motek [19,37,44], Senly [30,31,32], and Bertec [36,39,41] treadmills were each used in three studies. Bertec and Caren treadmills generated slip-like [36,37], trip-like [19,39], and both types of perturbations [41,44]. The Senly treadmill was only used for slip-like perturbations. The M-gait [34] and unspecified Motek [35] treadmill were used for slip-like perturbations, while the Woodway treadmill [40] was used for all perturbations. Each of these treadmills was used in a single study.

Table 2.
Papers reporting the results of perturbations in the mediolateral (ML) direction.
Table 2.
Papers reporting the results of perturbations in the mediolateral (ML) direction.
| Study/ Quality | Study Group Age [Years]; Body Mass [kg]; Body Height [cm]; Leg Dominance | Aim | Equipment/ Perturbed Limb/ Perturbed Moment/ Walking Speed/ Perturbation Intensity/ Perturbation Characteristics | Results |
|---|---|---|---|---|
| Mediolateral (ML) shifts of the treadmill (N = 6) | ||||
| Sheehan, et al. [46] 15/32 | Post-transtibial amputation Y: 9M Age: 30.7 ± 6.8; Weight: 90.2 ± 16.1; Height: 176 ± 11 Leg dominance: nd. Control group 13 (3F, 10M) Age: 24.8 ± 6.9; Weight: 79.3 ± 11.6; Height: 175 ± 8; Leg dominance: nd. | To determine how lateral walking surface perturbations affect the regulation of whole-body and individual leg angular momentum in able-bodied controls and individuals with unilateral transtibial amputation. | Treadmill Caren Motek: nd.; 24-cameras MoCap Vicon: 60 Hz (full-body model, 57 markers). Perturbed limb: nd.; Perturbation moment: nd.; Walking speed: 1.22 ± 0.28 m/s. Perturbation intensity: 4 incommensurate sine waves; 5 trials with 3 min unperturbed walking; 5 trials with 3 min continuous, pseudorandom ML platform oscillations. | The range and variability of angular momentum for the whole body and legs were significantly higher during platform oscillations. There were no significant differences between groups in whole-body angular momentum during unperturbed walking. In the frontal plane, individuals with amputation had greater angular momentum ranges than controls across all segments. While patients with amputation had higher angular momentum ranges for the whole body and intact leg, they had lower ranges for the prosthetic leg compared to controls. Overall, patients with amputation were more affected by the perturbations. |
| Afschrift, et al. [47] 14/32 | Y: 18 Age: 21 ± 2; Weight: nd.; Height: nd.; Leg dominance: nd. | To determine the contribution of the gluteus medius muscle of the stance and swinging limb in response to mediolateral perturbations at different phases of the gait cycle. | Treadmill Grail Motek: 1000 Hz; 12-cameras MoCap Vicon: 200 Hz; (full-body model, 48 markers); EMG Bortec: 1000 Hz; bilaterally: gluteus medius; OpenSim: gait2392_model. Perturbed limb: left; Perturbation moments: LR (7.5% gait cycle), MS (22.5% gait cycle), TS (37.5% gait cycle), PSw (52.5% gait cycle); Walking speed: 1.1 m/s. Perturbation intensity: 48 perturbations: 3 magnitudes (small, medium, large) and 4 directions (left/right platform translation, increase/decrease in belt speed). | Step width increased during perturbations at 7.5% and 22.5% of the gait cycle and decreased during the second double support phase. Gluteus medius activity significantly increased at 7.5% of the gait cycle and was higher in the stance limb at 22.5%, 37.5%, and 52.5%. |
| Rosenblum, et al. [48] 17/32 | Y: 20 (10F, 10M) Age: 27 ± 2.8; Weight: 62.54 ± 10.65; Height: 167 ± 8; Leg dominance: nd. | To investigate balance recovery differences between single-support and double-support phases in biomechanical behavior and lower limb muscle activation. | Treadmill Caren Motek; nd. 18-cameras Vicon MoCap; nd. EMG: 2048 Hz; bilaterally: vastus lateralis, tibialis anterior. Perturbed limb: nd.; Perturbation moment: single or double-support phase; Walking speed: self-selected. Perturbation intensity: randomly induced platform shifts of 15 cm for 0.92 s, occurring in various directions and timings (25–35 s). | Following a perturbation, lower extremity muscle spectral power significantly increased during the first three seconds. In the double-support phase, different muscle fiber recruitment patterns were observed between the vastus lateralis and tibialis anterior. No significant differences were found in muscle fiber recruitment during single-support phases. |
| Kao and Pierro [49] 13/32 | Y: 18 (8F, 10M) Age: 20.4 ± 1.5; Weight: 69.2 ± 11.7; Height: 172 ± 10; Leg dominance: nd. | To examine:
| Treadmill M-Gait Motek; nd. MoCap Motion Analysis Corporation: 100 Hz; (full-body model). Perturbed limb: nd.; Perturbation moment: Walking speed: ~1.25 m/s. Perturbation intensity: ML translation distance ranged from −0.05 m to 0.05 m. Participants walked under 2 conditions: with and without continuous ML sways (perturbed vs. unperturbed) and under 5 task conditions: PASAT (Paced Auditory Serial Addition Test), Clock, V-Stroop, A-Stroop, and Walk Only. | Participants showed greater local instability and variability in gait with perturbations. They increased average MoS in the ML direction during Clock and PASAT tasks compared to Walk Only, regardless of perturbations. While participants prioritized walking under challenging conditions, adjustments were insufficient to maintain balance. Cognitive tasks affecting working memory, visuospatial recognition, or attention had a greater impact on gait, especially with perturbations. |
| Castano, et al. [50] 16/32 | Y: 10 (5F, 5M) Age: 23 ± 4.2; Weight: nd.; Height: nd; Leg dominance: nd. E: 10 (4F, 6M) Age: 70 ± 6.6 Weight: nd.; Height: nd; Leg dominance: nd. | To investigate how healthy young and older adults adjust their gait strategies when responding to ML perturbations of varying unpredictability. | Treadmill M-Gait Motek; nd.; MoCap OptiTrack: nd.; (lower body model). Perturbed limb: left; Perturbation moment: LR, TS, MSw; Walking speed: self-selected, (Y: 1.27 ± 0.13 m/s; E: 1.45 ± 0.16 m/s). Perturbation intensity: ML treadmill shifts of 1 cm, 3 cm, or 5 cm. | During perturbations, participants took faster, wider, and longer steps. Older individuals walked faster than younger ones. Gait kinematic variability, including step width, increased with perturbation unpredictability. |
| Molina, et al. [51] 15/32 | Y: 15 (8F, 7M) Age: 25 ± 4; Weight: 69 ± 12; Height: 169 ± 13; Leg dominance: nd. |
| Treadmill Motek: 960 Hz; 10-cameras MoCap Vicon: 120 Hz; (full-body model, 56 markers). EMG Motion Labs Systems: 2160 Hz; bilaterally: medial gastrocnemius, soleus, tibialis anterior and gluteus medius. Perturbed limb: nd.; Perturbation moment: IC; Walking speed: self-selected. Perturbation intensity: ML treadmill shifts of 2.5 cm, lasting 0.25 s. Walking at 3 widths: narrow (25% narrower), SS (self-selected), wide (50% wider), and extra-wide (100% wider) step widths. | During steady-state walking, wider steps led to decreased balance control increased gluteus medius activity and reduced hip abduction and ankle inversion moments, indicating a reliance on lateral ankle strategies. Plantarflexion moments were unchanged. During perturbed walking, only lateral surface translations affected balance. Wider steps did not alter balance response strategies, suggesting consistent responses to perturbations across different step widths. |
| Mediolateral (ML) shifts of the treadmill and Acceleration/Deceleration of one belt in anterior–posterior (AP) direction (N = 6) | ||||
| Punt, et al. [52] 16/32 | 38 stroke survivors: Non fallers: 23 (13F, 10M) Age: 55.0 ± 12.2; Weight: 87 ± 19; Height: 172 ± 10; Leg dominance: nd. Fallers: 15 (7F, 8M) Age: 65.4 ± 6.7; Weight: 83 ± 20.1; Height: 171 ± 13; Leg dominance: nd. | To examine the differences in walking perturbation responses between post-stroke individuals who have experienced falls and those who have not. | Treadmill Grail Motek; nd.; 10-cameras MoCap Vicon; nd.; (full-body model, 47 markers). Perturbed limb: nd.; Perturbation moment: IC; Walking speed: 0.41 m/s; Perturbation intensity: ML treadmill shifts of 4.5 cm; deceleration to 0 m/s, acceleration: −3.9 m/s2. | During steady walking, individuals who fell had shorter step duration and length with the affected limb. During ML perturbations, they reacted faster and took shorter initial steps. |
| Chien and Hsu [53] 16/32 | E: 17 (12F, 5M) Age: 68.33 ± 5.80; Weight: 58.92 ± 7.69; Height: 157.09 ± 5.35; Leg dominance: nd. | To investigate balance control in static and dynamic conditions in older adults after eight weeks of perturbation training focused on both AP and ML sway perturbations. | Treadmill custom-made, AMTI force plates: 960 Hz; 10-cameras MoCap Vicon: 120 Hz; (full-body model, 14 markers). Perturbed limb: both randomly; Perturbation moment: nd.; Walking speed: self-selected. Perturbation intensity: 2 sessions per week, 1 h each, for 8 weeks. Walking perturbations: AP 20 forward (0.5–0.6 m/s) and 20 backward (0.4–0.6 m/s); ML 20 left-to-right and 20 right-to-left in random order (0.09–0.18 m/s). Standing perturbations: forward (0.15–0.2 m/s), backward (0.20–0.25 m/s), lateral (0.09–0.18 m/s). | After training, older adults showed significant improvement in CoM control during quiet standing with perturbations, but no change in CoP control during unperturbed standing. These findings suggest that perturbation-based balance training enhances dynamic control in older adults. |
| Roeles, et al. [9] 17/32 | Y: 9 (3F, 6M) Age: 25.1 ± 3.4; Weight: 76.6 ± 15.1; Height: 176 ± 9; Leg dominance: nd. E: 9 (7F, 2M) Age: 70.1 ± 8.1; Weight: 77.9 ± 10.5; Height: 170 ± 11; Leg dominance: nd. |
| Treadmill Caren Motek: nd.; 12-cameras MoCap Vicon: 100 Hz; (full-body model, 47 markers). Perturbed limb: non-dominant; Perturbation moment: IC; Walking speed: self-selected. Perturbations intensity: ipsilateral: 5 cm platform translation to the non-dominant side (0.7 s, 2.04 m/s2). Contra-lateral: same as ipsilateral but to the dominant side. Unilateral belt acceleration of the non-dominant side to 160% of the comfortable speed (0.4 s, 2.43–5.13 m/s2). Unilateral belt deceleration to 40% of the comfortable speed (0.4 s, 2.43–5.13 m/s2). Visual: rapid room darkening for 5 s to < 1 lux. Auditory: 0.5 s air horn at 82 dB. | The perturbation effect, measured by MoS deviation over six post-perturbation steps, showed that contra-lateral sway and deceleration caused the largest ML and AP effects, 1.9 to 5.6 times greater than other perturbations. Participants responded with wider, shorter, and faster steps, with no differences between young and older adults. |
| Aprigliano, et al. [54] 16/32 | E: 6M Age: 68.7 ± 5.2; Weight: 76.9 ± 7.9; Height: 176 ± 10; Leg dominance: nd. | Investigation of the effectiveness of balance recovery strategies following unexpected, multi-directional slips using an active pelvis orthosis (APO) robot. | Treadmill Senly: nd.; 6-cameras MoCap Vicon: 250 Hz; (full-body model, 34 markers). Perturbed limb: right; Perturbation timing: IC; Walking speed: self-selected (0.89 ± 0.12 m/s); Perturbations intensity: sudden forward or lateral movement of the right belt. | The APO was effective in helping restore stability in the sagittal plane after perturbations in both the AP and ML directions but was not helpful for perturbations in the frontal plane. |
| Rieger, et al. [55] 17/32 | Treatment group 15 (8F, 7M): Age: 70.33 ± 3.99; Weight: 74.93 ± 9.22; Height: 172.93 ± 10.48; Leg dominance: nd. Control group 15 (7F, 8M): Age: 71.67 ± 4.98; Weight: 75.40 ± 11.17; Height: 172.33 ± 8.77; Leg dominance: nd. | To evaluate the transfer and retention effects of gait training with treadmill perturbations in AP direction to ML reactive recovery. | Treadmill Grail Motek: 1000 Hz; 10-cameras MoCap Vicon: 100 Hz; (full-body model, 26 markers). Perturbed limb: both randomly; Perturbation moment: IC; Walking speed: 1 m/s; Perturbation intensity: 4 ML shifts to the opposite side (5 cm, 0.31 s); 4 AP belt accelerations/decelerations (9 m/s2 for 0.12 s). Training: Treadmill belt speed changes (low: 8 m/s2, 0.11 s; high: 10 m/s2, 0.13 s). | Both groups showed improved balance recovery after AP and ML perturbations immediately and one week post-intervention, with no differences between groups. Short-term training may effectively enhance dynamic trunk stabilization. |
| Rosenblum, et al. [56] 16/32 | Y: 12 (5F, 7M) Age: 26.92 ± 3.40; Weight: 63.67 ± 10.26; Height: 168.42 ± 7.32; Leg dominance: nd. E: 12 (6F, 6M) Age: 69.50 ± 5.20; Weight: 78.34 ± 16.22; Height: 169.67 ± 6.68; Leg dominance: nd. |
| Treadmill Caren Motek: nd.; 18-cameras Vicon MoCap: 120 Hz (full-body model, 41 markers). Perturbed limb: both randomly; Perturbation moment: IC, MS, TS; Walking speed: self-selected; Perturbation intensity: ML shifts (15 cm; 0.92 s); AP (Level 12—reducing the speed by 1.2 m/s with a deceleration of 5 m/s2). | A novel algorithm was developed to determine total recovery time for regaining stable step length and width after perturbations, using PCA. Both older and younger individuals took 4–6 s to return to free walking, regardless of perturbation type. |
| Mediolateral (ML) shifts of the treadmill, Acceleration/Deceleration of one belt in anterior–posterior (AP) direction and tilt (N = 3) | ||||
| Aprigliano, et al. [57] 13/32 | Y: 15 (5F, 10M) Age: 26.1 ± 1.3; Weight: 68.8 ± 12.3; Height: 178 ± 6; Leg dominance: nd. | To investigate how multi-directional slipping-like perturbations affect inter-segmental coordination, as described by the planar covariation law. | Treadmill Senly: nd.; 6-camera MoCap Vicon: 100 Hz (full-body model, 46 markers). Perturbed limb: both randomly; Perturbation moment: IC; Walking speed: Fr = 0.15. Perturbation intensity: displacement of each treadmill belt (forward, sideways, forward–sideways, sideways–backward, backward). | In response to perturbations, step time decreased from 1.21 ± 0.07 s to 0.75 ± 0.22 s, and stance phase reduced from 59.5 ± 1% to 53.7 ± 12.9%. Hip joint range of motion decreased from 37.8 ± 3.5° to 29.1 ± 8.5°, while knee joint motion reduced from 60.9 ± 5° to 48.2 ± 8.9°. Ankle joint motion increased from 27 ± 4.7° to 38.8 ± 27.6° on the perturbed side and 32.8 ± 8.1° on the non-perturbed side. |
| Onushko, et al. [58] 15/32 | Y: 15 (7F, 8M) Age: 21.3 ± 1.4; Weight: 68.8 ± 10.7; Height: 170 ± 10; Leg dominance: nd. | Examine changes in spatiotemporal gait parameters and mediolateral stability in response to sinusoidal perturbations of different amplitudes, types, and directions. | Treadmill Woodway: nd.; 14-cameras MoCap OptiTrack: 120 Hz; (lower body model). Perturbed limb: nd.; Perturbation moment: IC; Walking speed: 0.78 ±0.19 m/s; Perturbation intensity: the same speed and acceleration were for ML and AP perturbations and the roll and pitch rotational trials. 13 perturbation conditions: for 12 conditions, continuous sinusoidal oscillations (0.12 Hz) were with pitch and roll (±5°, ±10°, ±15°); ML and AP (±8 cm, ±16.5 cm, ±25 cm). The 13th condition involved a combination of roll, pitch, and yaw oscillations at frequencies of 0.15, 0.16, and 0.17 Hz, with an amplitude of ±8°. Participants walked for 80 s with 60 s of rest between trials. | In response to perturbations, participants increased step width and decreased step length while simultaneously increasing ML MoS, especially during oscillations that were in the frontal plane. Surface rotations induced the greatest changes in spatiotemporal parameters of gait. |
| Gerards, et al. [59] 17/32 | Treatment group 39 (31F, 8M): Age: 73 ± 10; Weight: 71.1 ± 19; Height: 161.0 ± 11.6; Leg dominance: nd. Control group 43 (34F, 9M) Age: 73 ± 8; Weight: 69.7 ± 18.5; Height: 164 ± 10; Leg dominance: nd. | To evaluate the effect of adding a Perturbation Training Protocol (PTP) to standard care on balance control and fall-related fear in older adults at higher risk of falls. | Treadmill Caren Motek: nd.; MoCap: nd.; Fear of falling assessment: FES-I questionnaire. Balance control assessment: Mini-BESTest tool. Perturbed limb: nd.; Perturbation moment: nd.; Walking speed: self-selected. Perturbation intensity: PBT involved three 30 min sessions over 3 weeks with unilateral treadmill belt accelerations/decelerations and platform shifts/tilts. Perturbations lasted 0.2–0.7 s. | Post-intervention, the median Mini-BESTest scores showed no clinically significant improvement and did not differ between groups. Similarly, FES-I test results remained unchanged in both groups. |
Abbreviations: M—men; F—women; Y—young; E—elderly; N—number of studies; nd.—no data; CoM—center of mass; CoP—center of pressure; MoS—margin of stability; GRF—ground reaction force; IC—Initial Contact gait phase; LR—Loading Response gait phase, MS—Mid Stance gait phase, TS—Terminal Stance gait phase; PSw—Pre-Swing gait phase; MSw—Mid Swing gait phase; APO—active pelvis orthosis.
3.1.3. Characteristics of Perturbations
Before perturbation, walking speeds were often set to participants’ preferred speed—five studies [38,39,41,42,43] or specific values, such as 1 m/s [34,40], 1.2 m/s [2,33,35], and 1.25 m/s [37,44], to the rhythm of a metronome (slow—80 or fast—140 BPM) [36] or corresponding to a Froude number [30,31,32].
The timing of perturbations varied, with some occurring at fixed intervals: every 10 s [2,4], every 15–20 s [38], or randomly [33,36] every 10–15 strides [33]. Similar variability was observed for the length of each session and the number of perturbations. Van den Bogaart, et al. [33] registered five trials, each containing 15 perturbations. Hirata, et al. [36] had trials with four perturbations per leg. Golyski, et al. [37] and Liss, et al. [39] induced 80 perturbations per participant. Ciunelis, et al. [4] applied five perturbations for the three trials. The authors also varied in their methods of analyzing the parameters. In some cases, the results were based on responses to the first perturbation [4,33,36], while in others, they were obtained from the average of all trials containing responses to the perturbations [2,30,31,34,35]. Sometimes, the description was not clear [44].
Perturbations were most often triggered during heel strike, i.e., the IC phase. For slip-like perturbations, seven authors targeted only the IC phase [30,31,32,33,34,35,36]. Ciunelis, et al. [4] considered perturbations in the IC, MS, and PSw phases. Golyski, et al. [37] set the onset of belt accelerations at 10%, 15%, 20%, and 30% of the gait cycle.
For trip-like perturbations, all three papers [19,38,39] targeted only the IC phase with one-belt deceleration.
Among studies considering both slip- and trip-like perturbations, four authors chose only perturbations in the IC phase. Lee, et al. [41] specified perturbations in the PSw phase, while Błażkiewicz and Hadamus [2] analyzed perturbations in the IC, MS, and PSw phases.
The duration and intensity of perturbations varied based on equipment. Authors using the Senly treadmill [30,31,32] set perturbation intensity with a Froude number of 0.1 to 0.4 and an acceleration of 8 m/s2 for a slip-like effect. There was no information about their duration. For the Grail Motek, perturbation magnitude ranged from 1 (0.1 m/s speed change) to 5 (0.5 m/s speed change) [2,4,33]. Ciunelis, et al. [4] reported a slip-like perturbation lasting 0.82 s, with speed changing from 1.2 to 1.7–1.8 m/s, then back to 1.2 m/s. Golyski, et al. [37] used the Caren Motek system to accelerate from 1.25 to 2.5 m/s and back, with a 15 m/s2 acceleration/deceleration over 340 ms (30% of the gait cycle). Swart, et al. [34] used the M-Gait Motek to accelerate belts to 0.35 m/s, then return to regular speed, with perturbation lasting up to 0.5 s. Hirata, et al. [36] applied a Bertec treadmill acceleration of 1.6 m/s at 5.3 m/s2 for 0.3 s, then decelerated to 0 m/s at 5.3 m/s2 for 0.3 s, with a GRF threshold of 5 N on the slipping side.
Two authors described a trip-like perturbations setting. Liss, et al. [39] used the Bertec treadmill to slow the belt by an increment of 0 to 0.4 m/s during walking. Shokouhi, et al. [19] set the Caren Motek system to decelerate the belt to 0.5 m/s for 0.5 s with a maximum acceleration of 3 m/s2, then to rapidly accelerate back to the baseline speed.
In the papers investigating both slip- and trip-like perturbations, the settings varied significantly. Mueller, et al. [40] used a Woodway treadmill to apply perturbations lasting 50 ms, with forward accelerations of +20 m/s2 (velocity +2 m/s) and +40 m/s2 (velocity +3 m/s) and backward accelerations of −20 m/s2 (0 m/s) and −40 m/s2 (−1 m/s). Lee, et al. [41] set the Bertec treadmill to decelerate at −10 m/s2 for trips and accelerate at 20 m/s2 for slips. Ren et al. [42,43] configured the Grail Motek treadmill with a perturbation intensity of 3 m/s2 and 1.2 m/s baseline speed for 300 ms perturbations, featuring posterior acceleration for slips and anterior deceleration for trips.
3.1.4. Summary of Results and Measurement Outcomes
Nine papers extensively studied the slipping-like effect caused by accelerating one treadmill belt. Aprigliano, et al. [30] found strong perturbations reduced dynamic stability, increased compensatory step time, and decreased the margin of stability (MoS) in young subjects. They also noted significant reductions in step time, stance phase, step length, and width during slip-like perturbations across age groups [31], though aging did not affect intra-limb coordination. Martelli, et al. [32] showed older subjects had longer recovery times and steps, indicating greater destabilization. Van den Bogaart, et al. [33] highlighted the critical role of the CoP mechanism in adjusting the CoM acceleration post-perturbation, particularly during the initial stages in young subjects. Swart, et al. [34] observed young participants took shorter, wider steps after a perturbation warning, with significant gait adjustments. Debelle, et al. [35] found balance recovery involved a few corrective steps with larger hip and knee moments across young adults. Hirata, et al. [36] noted that slower walking velocities resulted in more backward or wide corrective steps presented by the young. Golyski, et al. [37] reported that earlier perturbations led to longer and wider recovery steps. Ciunelis, et al. [4] detailed significant impacts on gait parameters, especially knee extension and flexion torques, depending on the gait cycle phase in young women.
Three studies examined the trip-like effect of treadmill belt deceleration. Ren, et al. [38] found that for the elderly, barefoot walking increased stability during trip-like perturbations and significantly decreased walking speed compared to wearing shoes. Shokouhi, et al. [19] noted increased positive and negative leg work during trip recovery, with the knee contributing significantly to negative work and the hip to positive work for the young. Liss, et al. [39] emphasized the importance of ankle proprioception and whole-body feedback in slip perception among young individuals.
Six studies investigated the combined effects of acceleration and deceleration of one treadmill belt in the AP direction, focusing on neuromuscular responses and gait compensatory mechanisms. Mueller, et al. [40] found significantly higher muscle activity, especially in ventral muscles, with rapid neuromuscular responses among young adults. Lee, et al. [41] reported faster compensatory reactions to slip-related perturbations, increasing trunk, arm, and CoM movements, and higher muscle activity in key leg muscles of young participants. Ren, et al. [42] showed that slipping and tripping increased step width and joint moments, using ankle and hip strategies for compensation. Also, despite the fact that aging did not alter overall gait, it affected hip extension moments during slipping. Another study by Ren, et al. [43] found that patients with knee osteoarthritis (KOA) had lower step lengths and gait speeds, indicating higher fall risk during backward slips compared to healthy older adults. Shokouhi, et al. [44] showed that for young adults, trips were more destabilizing than slips, requiring significant adjustments in recovery steps and whole-body angular momentum. Błażkiewicz and Hadamus [2] noted that CoM displacement regularity of young women varied with perturbation type and phase, with specific patterns in both AP and ML directions. These studies highlight the varied effects of perturbations on gait stability and the complex compensatory mechanisms needed during split-belt treadmill walking. In summary, the observed disturbances, such as slip-like and trip-like perturbations, had varying impacts depending on the sample population. Healthy young adults quickly adapted their gait to regain stability, while older adults and those with neurological impairments exhibited less efficient compensatory strategies, such as increased muscular co-contraction. These differences highlight the role of age and neurological health in determining the effectiveness of adaptive gait mechanisms during disturbances.
3.2. Perturbations in the Mediolateral (ML) Direction
Table 2 encompasses a broader range of perturbation directions and techniques, including lateral shifts (side to side), forward and backward movements, and adjustments in treadmill incline (tilting).
Table 2 presents 15 studies categorized into three groups: (1) 6 studies focusing solely on perturbations in the ML direction [46,47,48,49,50,51], (2) 6 studies examining perturbations in both the ML and AP directions [9,52,53,54,55,56], and (3) 3 studies that investigated perturbations in both directions, along with treadmill movements or inclines [57,58,59].
3.2.1. Characteristics of Participants
Most studies were conducted on young adults, accounting for seven publications [46,47,48,49,51,57,58], including one by Sheehan, et al. [46], who compared a group of individuals with amputations to a healthy control group. Five studies focused on older adults [52,53,54,55,59], including one by Punt, et al. [52], which examined stroke survivors. In three papers [9,50,56], the authors compared how healthy young and older adults adjust their gait strategies when responding to varying perturbations.
The number of subjects varied across the studies. Aprigliano, et al. [54] studied only six men, and this was the smallest group. On the other hand, Gerards, et al. [59] had the largest group, with 82 participants.
Most studies included men and women, but Aprigliano, et al. [54] focused exclusively on men. Only Afschrift, et al. [47] did not specify the participants’ gender, providing only age information. All other articles included detailed subject characteristics, such as age, height, and weight. However, none of the studies specified lower limb dominance.
3.2.2. Measurement Tools
As in Table 1, Table 2 demonstrated that different tools were used to capture data during perturbations. The motion capture system was employed in fourteen studies, predominantly using a Vicon system operating on a full-body model and recording kinematic data at 60 Hz [46], 100 Hz [9,55], 120 Hz [51,53,56], 200 Hz [47], or 250 Hz [54]. Two studies [48,52] did not specify the data recording frequency.
EMG data were recorded in three studies [47,48,51], measuring muscle activation bilaterally in response to ML platform translation. Afschrift, et al. [47] registered gluteus medius muscle activity, Rosenblum, et al. [48] analyzed tibialis anterior and vastus lateralis muscles, and Molina, et al. [51] had signals from medial gastrocnemius, soleus, tibialis anterior, and gluteus medius.
As in the case of slip- and trip-like perturbation, seven types of treadmills were used to induce perturbations in the studies listed in Table 2. The Caren Motek treadmill was the most frequently used (appearing in five studies [9,46,48,56,59]), followed by the Grail Motek in three papers [47,52,55]. The Senly [54,57] and M-gait Motek [49,50] treadmills were each used in two studies. Single studies used the Woodway [58], an unspecified Motek [51], and a custom-made AMTI treadmill [53]. In the first group, which investigated perturbations solely in the ML direction, the Caren Motek and M-gait Motek treadmills were used most commonly, and each of them appeared in two studies. In the group studying perturbations in both ML and AP directions, the Grail and Caren Motek treadmills were used most frequently, each in two studies. The last group exhibited diversity, including Woodway, Senly, and Caren Motek treadmills.
3.2.3. Characteristics of Perturbations
Before perturbation, walking speeds were typically set to participants’ preferred speeds in six studies [9,48,51,53,56,59] or specific values: 0.41 m/s [52], 0.78 ± 0.19 m/s [58], 0.89 ± 0.12 m/s [54], 1 m/s [55], 1.1 m/s [47], 1.22 ± 0.28 m/s [46], and 1.25 m/s [49]. Castano, et al. [50] used different preferred speeds for young and older participants (1.27 ± 0.13 m/s vs. 1.45 ± 0.16 m/s).
Similar to the studies in Table 1, perturbations were most frequently applied only during the IC phase of gait, as observed in seven studies. In the first group, there was one paper [51]. In the second, there were four papers [9,52,54,55], and in the third, there were two [57,58]. Some authors did not specify when the perturbation occurred [46,49,53,59]. Perturbations were applied at various gait cycle moments in three papers from the first group [47,48,50] and one from the second group [56]. Afschrift, et al. [47] applied perturbations immediately after IC, during early and late MS (22.5%, 37.5% gait cycle), and PSw (52.5% gait cycle). Similarly, Castano, et al. [50] shifted the treadmill during the LR, TS, and MSw phases. Rosenblum, et al. [48] induced perturbations randomly during single- or double-support phases. Rosenblum, et al. [56] introduced perturbations at IC, MS, and PSw.
Perturbations causing significant ML instability were typically administered in a pseudorandom or balanced random order. Most studies involved lateral shifts or oscillations of the treadmill platform, but the intensity and timing of these perturbations varied across studies. Sheehan, et al. [46] used the sum of four sine waves for perturbations, with participants completing trials of unperturbed and pseudorandom ML oscillations. Kao and Pierro [49] programmed platform sways with sine wave patterns, limited to ±0.05 m. Molina, et al. [51] applied 2.5 cm medial and lateral translations lasting 0.25 s during a single-leg stance. Afschrift, et al. [47] designed perturbations with three different magnitudes (small, medium, and large) and four directions (left/right translation, belt speed increase/decrease). Rosenblum, et al. [48] implemented unannounced 15 cm platform shifts lasting 0.92 s. Castano, et al. [50] varied ML shifts to 1 cm, 3 cm, or 5 cm.
Studies in the second group included additional AP displacements or combined ML and AP perturbations. Punt, et al. [52] applied ML and AP perturbations beginning 80–90 ms after IC, with ML displacements of 0.045 m and AP decelerations and accelerations at IC. Aprigliano, et al. [54] triggered right-side perturbations at the IC with sudden forward or lateral movements. Chien and Hsu [53] implemented a protocol involving perturbations during standing and walking, with various speeds for forward, backward, and lateral movements. Rieger, et al. [55] investigated perturbed walking using four AP belt decelerations and four ML perturbations. In the case of the ML perturbation, the treadmill moved 5 cm in the opposite direction in 0.31 s, likely inducing a cross-stepping strategy. The AP disturbance caused the treadmill to decelerate by 9 m/s2 for 0.12 s at the IC point. The order of perturbations, the perturbed leg, and the intervals between perturbations (10–60 s) were randomized but consistent for all participants. Rosenblum, et al. [56] classified perturbations by direction, gait phase, and reference foot, using 15 cm ML displacements and 1.2 m/s AP decelerations. Roeles, et al. [9] used six perturbation types triggered at non-dominant IC: (1) ipsilateral sway with a 5 cm platform translation over 0.7 s (max acceleration 2.04 m/s2); (2) contra-lateral sway to the dominant side with similar parameters; (3) unilateral belt acceleration to 160% of comfortable walking speed in 0.4 s (max acceleration 2.43 to 5.13 m/s2); (4) unilateral belt deceleration to 40% of comfortable walking speed; (5) visual perturbation by darkening the room for 5 s; and (6) auditory perturbation with a 0.5 s air horn blast at 82 dB.
In the third group, advanced protocols were developed. Aprigliano, et al. [57] created ten types of perturbations combining longitudinal and transversal belt movements but did not provide specific details. Gerards, et al. [59] developed a training regimen with unexpected balance perturbations, including unilateral treadmill belt accelerations or decelerations, platform translations, and rotations. The treadmill perturbations lasted 0.2–0.7 s, but specific details were not provided. Onushko, et al. [58] used thirteen experimental conditions: twelve with continuous sinusoidal oscillations (0.12 Hz) on the treadmill in pitch, roll, ML, and AP directions, each at three amplitudes (±5°, ±10°, and ±15° for pitch and roll and ±8, ±16.5, and ±25 cm for ML and AP translations), and one combining roll, pitch, and yaw oscillations at different frequencies (0.15, 0.16, and 0.17 Hz) at an amplitude ± 8°. Subjects walked for 80 s per trial with 60 s of rest between them.
3.2.4. Summary of Results and Measurement Outcomes
The studies from Table 2 examined the effects of gait perturbations in the ML direction combined with AP perturbations, revealing several common findings and significant differences.
Across various studies, it was commonly observed that perturbations significantly impact gait stability. Sheehan, et al. [46] reported greater ranges and variability in angular momentum during platform oscillations, especially in amputees. Similarly, Afschrift, et al. [47] observed increased step width and gluteus medius muscle activity during different gait phases in young subjects. Rosenblum, et al. [48] found that young adults increase the total spectral power of lower extremity muscles immediately following a perturbation, indicating distinct muscle fiber recruitment patterns during different gait phases. This suggests that muscle activity rapidly adapts to maintain stability. Kao and Pierro [49] demonstrated for the young greater local instability and variability in gait parameters under perturbations. Castano, et al. [50] noted that participants took faster, wider, and longer steps during perturbations, with older individuals walking faster than younger ones and displaying increased variability in gait kinematics. Molina, et al. [51] indicated that wider steps were associated with decreased balance control, increased GM activity, and reliance on a lateral ankle strategy to maintain balance without changes in the plantarflexion moment during perturbed walking in young participants.
When examining ML shifts and AP direction changes, Punt, et al. [52] found that post-stroke individuals who experienced falls had shorter step durations and lengths during steady-paced walking and responded to ML perturbations with faster reactions and shorter initial steps. Chien and Hsu [53] showed a significant improvement in the control of the CoM during quiet standing post-perturbation in young adults after training. Roeles, et al. [9] measured the perturbation effect by changes in the MoS over six steps after perturbation. Contra-lateral sway and deceleration caused the largest ML and AP perturbation effects. Participants increased their MoS with wider, shorter, and faster steps, showing a common adaptive strategy. Changes were similar for both the elderly and the young. Aprigliano, et al. [54] found that assistance from an active pelvis orthosis was helpful for recovery balance in the sagittal plane but not in the frontal plane for older participants. Rieger, et al. [55] reported improved balance recovery after AP and ML perturbations immediately and one-week post-intervention of older participants. Rosenblum, et al. [56] developed an algorithm to determine total recovery time, finding that older and younger individuals rapidly returned to stable walking post-perturbation.
The last three studies from Table 2 focused on the effects of ML shifts, AP acceleration/deceleration of one belt, and tilt perturbations on gait and balance. Aprigliano, et al. [57] observed decreased step time, stance phase percentage, and hip/knee range of motion, with increased ankle joint motion on both the perturbed and non-perturbed sides in young adults. Onushko, et al. [58] found that young participants responded to perturbations by increasing step width and decreasing step length, especially during frontal plane oscillations. Surface rotations had the greatest impact on gait parameters, suggesting that young, healthy adults use lateral steps to maintain balance during perturbations. Lastly, Gerards, et al. [59] reported that perturbation-based balance training for the elderly did not significantly differ from usual care in improving balance control or reducing fear of falling.
4. Discussion
Gait adaptability and symmetry are crucial for efficient and safe locomotion, making the study of gait perturbations increasingly important. Developments within methods and techniques to induce gait perturbations, especially on split-belt treadmills where each belt can move at different speeds, offer a unique environment to study neuromuscular adaptive responses. This review aimed to consolidate knowledge on how these perturbations affect gait dynamics, focusing on adaptive mechanisms, neural responses, and potential therapeutic applications. Based on the 33 papers included in the review, split-belt treadmills effectively generated controlled gait perturbations, allowing for a detailed study of adaptive responses. However, the small number of studies (33 out of 5571 initially identified) highlights the limited use of split-belt treadmills in perturbation research compared to other methods, such as single-belt treadmills or manual push–pull perturbations. This limited adoption may be due to the higher cost, increased complexity, and limited accessibility of split-belt systems.
This section was divided into four subsections covering essential factors for analyzing perturbations during gait: treadmill types; terminology for slip-like and trip-like perturbations; the effects of side-to-side, pitch, roll, and yaw perturbations; and study limitations.
4.1. Differences in Used Treadmills
In studies that used split-belt treadmills, the Grail Motek treadmill is the most frequently used, allowing for perturbations in AP and ML directions, tilting, and offering a realistic simulation of real-life walking conditions [2,4,33,38,42,43,47,52,55]. The Caren Motek treadmill, the second most implemented, features 6 degrees of freedom for complex movement simulations, benefiting rehabilitation, sports, military, and aviation training [9,19,37,44,46,48,56,59]. The Senly treadmill, though less common [30,31,32,54,57], is valued for its independently moving sections and advanced sensors, providing precise control and detailed analysis of gait dynamics. A notable feature of the Senly treadmill is its use of the Froude number (Fr) to determine walking speed and intensity.
The Froude number is a ratio of kinetic-to-potential energy used to characterize natural movements of animals that are geometrically similar but of different sizes. It is defined as Fr = v2/(gL), where v is velocity [m/s], g is the acceleration due to gravity [9.81 m/s2], and L is the leg length of the participant [60]. According to Vaughan and O’Malley [61], Fr = 0.25 represents optimal walking speed, Fr = 0.5 denotes the walk-to-run transition, and Fr = 1.0 indicates the physical walking limit. For most studies, the initial velocity level was calculated using the following formula: with a typical Fr of 0.15 for a leisurely walk. It allows for personalized walking speeds based on leg length [32]. Perturbation intensity is categorized as soft (Fr = 0.10), medium (Fr = 0.20), and strong (Fr = 0.30), with higher Fr values increasing treadmill speed and perturbation intensity [54,57].
In the case of the Grail and Caren Motek treadmills, perturbation intensity depends on the treadmill’s acceleration and the duration of the perturbation. Variations in these parameters across different studies complicate direct comparisons. Thus, the choice of treadmill will depend on research needs. The Grail Motek is the best for simulating single-leg slips/trips and tri-axial perturbations, the Caren Motek excels in advanced multi-directional simulations and complex rehabilitation, and the Senly treadmill is preferred for precise perturbation control and a detailed force analysis. Each treadmill’s unique capabilities are crucial for advancing gait biomechanics research, rehabilitation, and fall prevention strategies.
4.2. Terminology of Slip-Like and Trip-Like Perturbations
Van Dieën, et al. [62] explained that trips occur when the swinging leg collides with an external object, hindering its forward movement. This collision creates a destabilizing scenario because the CoM is ahead of the CoP and outside the base of support during single support [63]. According to Winter [64], individuals are most vulnerable to trips during the MSw phase due to minimum toe clearance, increasing the risk of hitting obstacles. However, trips can also occur during the early swing phase and cause forward destabilization [62].
Another event that can lead to a fall due to a loss of balance is a slip. Lockhart [65] explained that slips happen when the coefficient of friction between the foot and the floor is too low, such as on wet or icy surfaces. Slips are usually classified based on the direction of foot movement, like forward or backward [66,67]. A forward slip occurs when the backward horizontal frictional force is less than the forward horizontal reactive force at IC [66], causing the foot to slip forward and the CoM to fall backward [68]. Conversely, backward slips occur when the horizontal propulsive force at push-off exceeds the surface’s coefficient of friction [67], causing the foot to slip backward and the CoM to fall forward [69].
To simulate tripping and slipping, researchers use split-belt treadmills or manipulate ground surfaces [41,66,67]. Ground protocols use obstacles to induce trips or lubricants to create slippage, while treadmills offer a safe environment. On split-belt treadmills, trips are simulated by suddenly decelerating or momentarily stopping one belt during the IC phase, unlike natural trips that occur during the swing phase [70,71]. In contrast, slips on treadmills are triggered by accelerating one belt forward or backward [32,35,71]. For a forward slip, the belt under the foot in the IC phase accelerates forward, causing the foot to slide rapidly forward. For a backward slip, the belt under the foot in the push-off phase decelerates or stops, causing the foot to slide backward. Therefore, it is crucial to precisely define the treadmill belt’s actions and the gait cycle phase [4] rather than using general terms like slips or tripping. Additionally, differences between treadmill and over-ground perturbations can impact reactive stepping and balance responses. Understanding these variations is essential for comprehending fall etiology and improving intervention strategies.
This paper takes a narrower approach, linking treadmill acceleration solely with forward slips [31,32,33,34,35,36,37,45] and deceleration with trips [19,38,39]. Slip-like perturbations increased step width while decreasing step length and time. Participants exhibited increased muscle activation, particularly of the tibialis anterior, gastrocnemius, rectus femoris, biceps femoris, and ventral muscles. Slip-like perturbations also reduced the MoS, indicating decreased stability and necessitating gait adjustments.
Trip-like perturbations caused a significant increase in step width, prolonged step time, and altered joint angles, especially at the knee and hip. These perturbations led to higher muscle activation and a greater MoS, indicating a higher risk of falls. Consequently, slip-like perturbations resulted in faster reactions and less destabilization, while trip-like perturbations were more destabilizing and required broader gait adjustments.
4.3. Studies on Mediolateral Perturbations and Treadmill Tilts
Responses to ML perturbations during gait varied with age and perturbation specifics. Participants showed increased variability in gait parameters like step width and length. Younger adults responded faster and more effectively than older adults. Older adults adopted a strategy that increased stability but faced higher balance challenges. Muscle activation patterns also changed depending on the gait phase during perturbation [48,51]. For example, gluteus medius activity increased during specific gait phases, helping to stabilize the pelvis.
Additionally, muscles like the vastus lateralis and tibialis anterior showed heightened activity, particularly during the double-support phase. The intensity and direction of perturbations affected recovery. Larger, unpredictable perturbations required more significant gait adjustments and muscle activity, indicating a higher demand on the neuromuscular system for balance restoration. In summary, mediolateral perturbations caused notable changes in gait and muscle activation, with younger adults typically responding more effectively. The phase of the gait cycle and perturbation characteristics were crucial in shaping these responses.
Perturbations caused by pitch, roll, and yaw during treadmill gait introduce distinct directional disturbances that impact balance and gait dynamics. However, their effect on gait is the least studied form of perturbation on a two-lane treadmill. In this review, there are only two papers [44,58]. Pitch perturbations involve tilting the treadmill forward or backward, changing the angle of the walking surface. This simulates walking on an incline (forward tilt) or decline (backward tilt), affecting the forward or backward movement of the body and influencing gait dynamics and stability as the body adjusts to the new angle. These perturbations can cause changes in step length, step frequency, and muscle activation to maintain balance and accommodate the altered slope [58,72]. Roll perturbations involve tilting the treadmill sideways, creating a lateral incline or decline. This simulates walking on a slope that tilts left or right, affecting side-to-side balance and stability. The perturbation challenges the body’s ability to maintain an upright posture, potentially leading to changes in step width and adjustments in lateral muscle activation to counteract the sideways tilt and maintain stability [58,73]. Yaw perturbations involve rotating the treadmill around its vertical axis, causing the walking surface to shift direction. This simulates unexpected changes in direction or turning while walking, affecting the body’s orientation and balance. The rotation requires adjustments to gait direction and stability, resulting in changes in step orientation, step length, and increased muscle activation to manage the sudden direction change and maintain forward progression [58].
Onushko, et al. [58] explored how sinusoidal oscillations of various amplitudes, types, and directions during walking impact spatiotemporal gait parameters and ML dynamic stability. Their research demonstrated that pitch perturbations resulted in a 25% increase in activation of the gluteus medius and a 20% increase in the tibialis anterior. Participants responded by adjusting their step length by approximately 8% and step width by about 10% to maintain balance. Furthermore, there was an increase in whole-body angular momentum of up to 12% as they adapted to the tilts. Roll perturbations, characterized by side-to-side tilts, led to a 30% increase in activation of lateral muscles, particularly the hip abductors and adductors. To stabilize their stance, participants widened their step width by about 15% and corrected lateral shifts in their CoM with a 20% adjustment in gait dynamics. Yaw perturbations caused a 15% increase in core muscle activation to counteract the rotational forces. Participants adjusted their stepping patterns, modifying step length by approximately 7% and step width by 9% to accommodate the rotational movements. The angular velocity of yaw perturbations resulted in a 10% increase in whole-body angular momentum, requiring effective gait adjustments to maintain forward progression. Shokouhi, et al. [44] analyzed only pitch perturbations, which included three slope angles (downhill: − 8°; level: 0°; uphill: + 8°). Participants demonstrated increased whole-body angular momentum as they adjusted their posture to counteract the tilt. Muscle activation increased significantly to manage the perturbation. Participants exhibited up to a 20% increase in activation of the quadriceps and hamstring muscles and a 25% increase in core stabilizing muscles such as the rectus abdominis and obliques. Moreover, participants modified their gait to cope with the tilt. They adjusted their step length by approximately 10% and increased step width by about 12%. These changes helped maintain balance and adapt to the altered treadmill orientation.
Overall, these studies demonstrated that different types of perturbations (pitch, roll, and yaw) required specific muscle activation and gait adjustments, highlighting the intricate nature of maintaining dynamic stability and the importance of targeted rehabilitation strategies for gait and balance training.
4.4. Limitations of the Reviewed Studies and Suggestions for Future Research
A crucial limitation of included studies is the controlled laboratory setting, which does not replicate the complexity of walking in the real world. Thus, the observed adaptive responses may differ from those in everyday situations. Another limitation is the ability to anticipate change due to the recurrent nature of perturbations. Anticipating perturbations may cause individuals to adopt a cautious gait or prepare in advance [34], skewing results and not accurately reflecting natural, spontaneous responses.
Participant demographics in the included studies also present limitations. Most studies focused on young, healthy adults, with fewer studies examining older adults or individuals with neurological impairments. Moreover, the varied methodologies of the included studies further complicate synthesizing the results. Additionally, the relatively small sample sizes in many studies may limit the statistical power and robustness of the findings.
These limitations highlight several key areas where further research is needed. First, there is a notable lack of studies focusing on older adults and individuals with neurological impairments, i.e., populations that are particularly vulnerable to gait instability and falls. Only a few studies included these groups, limiting the generalizability of findings.
Second, the methods used to induce perturbations vary significantly across studies. Differences in treadmill settings, perturbation timing, and intensity make it difficult to compare outcomes. Standardizing these parameters would facilitate more robust comparisons and help identify the most effective approaches for improving gait stability.
Additionally, while motion capture and electromyography are commonly used to analyze gait, emerging technologies such as virtual reality (VR) have been underutilized. Integrating new technologies with split-belt treadmill perturbations could provide a more comprehensive understanding of real-world gait challenges.
Finally, in most studies, follow-up duration was limited or absent. Future research should prioritize longitudinal studies to examine the long-term effects of perturbation-based training. Comparative studies are also needed to explore how different perturbations influence gait adaptation and fall prevention. These efforts will advance the field by providing clearer guidance for rehabilitation protocols and assistive device development.
5. Conclusions
Through an in-depth analysis of 33 studies included in this scoping review, we could identify the types of perturbations rarely investigated in the literature and highlight the inherent flaws and limitations of these studies that may impact the interpretation of results and future research directions in this field. It is worth noting that the current body of research focusing on pitch, roll, and yaw disturbances is limited, with only two studies addressing these types of perturbations on dual-belt treadmills. This knowledge gap highlights the need for further investigation to fully understand how pitch, roll, and yaw perturbations influence gait and stability. Future research should aim to expand on these initial findings, exploring a broader range of perturbation types, intensities, and individual responses. Enhanced knowledge in this area will be crucial for developing more effective gait rehabilitation strategies and improving balance training programs, ultimately advancing our understanding of locomotion and fall prevention. Moreover, all findings suggest that split-belt treadmill training can significantly influence gait symmetry, adaptability, and neural plasticity, highlighting its potential for rehabilitation, particularly in populations with gait abnormalities.
Author Contributions
Conceptualization, M.B.; methodology, K.C., R.B. and M.B.; software, K.C., R.B. and M.B.; validation, M.B.; formal analysis, K.C. and R.B.; investigation, K.C. and R.B.; resources, K.C., R.B. and M.B.; data curation, K.C., R.B. and M.B.; writing—original draft preparation, K.C. and R.B.; writing—review and editing, K.C. and M.B.; visualization, K.C. and M.B.; supervision, M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Józef Piłsudski University of Physical Education in Warsaw, grant number UPB no. 2 (114/12/PRO/2023).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bartsch-Jimenez, A.; Błażkiewicz, M.; Azadjou, H.; Novotny, R.; Valero-Cuevas, F.J. “Fine synergies” describe motor adaptation in people with drop foot in a way that supplements traditional “coarse synergies”. Front. Sports Act. Living 2023, 5, 1080170. [Google Scholar] [CrossRef] [PubMed]
- Błażkiewicz, M.; Hadamus, A. Influence of Perturbation’s Type and Location on Treadmill Gait Regularity. Appl. Sci. 2024, 14, 493. [Google Scholar] [CrossRef]
- Błażkiewicz, M.; Wiszomirska, I.; Kaczmarczyk, K.; Brzuszkiewicz-Kuźmicka, G.; Wit, A. Mechanisms of compensation in the gait of patients with drop foot. Clin. Biomech. 2017, 42, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Ciunelis, K.; Borkowski, R.; Błażkiewicz, M. The Impact of Induced Acceleration Perturbations in Selected Phases of the Gait Cycle on Kinematic and Kinetic Parameters. Appl. Sci. 2024, 14, 4849. [Google Scholar] [CrossRef]
- Bender, C.; Orszag, S. Advanced Mathematical Methods for Scientists and Engineers: Asymptotic Methods and Perturbation Theory; Springer: Berlin/Heidelberg, Germany, 1999; Volume 1. [Google Scholar]
- Holmes, M.H. Introduction to Perturbation Methods; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar] [CrossRef]
- Rogers, M.W.; Mille, M.-L. Chapter 5—Balance perturbations. In Handbook of Clinical Neurology; Day, B.L., Lord, S.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; Volume 159, pp. 85–105. [Google Scholar]
- McCrum, C.; Epro, G.; Meijer, K.; Zijlstra, W.; Brüggemann, G.P.; Karamanidis, K. Locomotor stability and adaptation during perturbed walking across the adult female lifespan. J. Biomech. 2016, 49, 1244–1247. [Google Scholar] [CrossRef] [PubMed]
- Roeles, S.; Rowe, P.J.; Bruijn, S.M.; Childs, C.R.; Tarfali, G.D.; Steenbrink, F.; Pijnappels, M. Gait stability in response to platform, belt, and sensory perturbations in young and older adults. Med. Biol. Eng. Comput. 2018, 56, 2325–2335. [Google Scholar] [CrossRef]
- Berger, W.; Dietz, V.; Quintern, J. Corrective reactions to stumbling in man: Neuronal co-ordination of bilateral leg muscle activity during gait. J. Physiol. 1984, 357, 109–125. [Google Scholar] [CrossRef]
- Forbes, P.A.; Happee, R.; van der Helm, F.C.; Schouten, A.C. EMG feedback tasks reduce reflexive stiffness during force and position perturbations. Exp. Brain Res. 2011, 213, 49–61. [Google Scholar] [CrossRef]
- Kim, S.; Joo, K.S.; Liu, J.; Sohn, J.H. Lower extremity kinematics during forward heel-slip. Technol. Health Care Off. J. Eur. Soc. Eng. Med. 2019, 27, 345–356. [Google Scholar] [CrossRef]
- Arena, S.L.; Davis, J.L.; Grant, J.W.; Madigan, M.L. Tripping Elicits Earlier and Larger Deviations in Linear Head Acceleration Compared to Slipping. PLoS ONE 2016, 11, e0165670. [Google Scholar] [CrossRef]
- Boerger, T.F.; McGinn, L.; Wang, M.C.; Schmit, B.D.; Hyngstrom, A.S. Degenerative cervical myelopathy delays responses to lateral balance perturbations regardless of predictability. J. Neurophysiol. 2022, 127, 673–688. [Google Scholar] [CrossRef] [PubMed]
- Zadravec, M.; Olenšek, A.; Matjačić, Z. The comparison of stepping responses following perturbations applied to pelvis during overground and treadmill walking. Technol. Health Care Off. J. Eur. Soc. Eng. Med. 2017, 25, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Pasma, J.H.; Boonstra, T.A.; Campfens, S.F.; Schouten, A.C.; Van der Kooij, H. Sensory reweighting of proprioceptive information of the left and right leg during human balance control. J. Neurophysiol. 2012, 108, 1138–1148. [Google Scholar] [CrossRef] [PubMed]
- Torres-Oviedo, G.; Bastian, A.J. Seeing is believing: Effects of visual contextual cues on learning and transfer of locomotor adaptation. J. Neurosci. 2010, 30, 17015–17022. [Google Scholar] [CrossRef]
- Schrijvers, J.C.; van den Noort, J.C.; van der Esch, M.; Harlaar, J. Responses in knee joint muscle activation patterns to different perturbations during gait in healthy subjects. J. Electromyogr. Kinesiol. 2021, 60, 102572. [Google Scholar] [CrossRef]
- Shokouhi, S.; Mokhtarzadeh, H.; Lee, P.V.-S. Lower extremity joint power and work during recovery following trip-induced perturbations. Gait Posture 2024, 107, 1–7. [Google Scholar] [CrossRef]
- Siragy, T.; Russo, Y.; Young, W.; Lamb, S.E. Comparison of over-ground and treadmill perturbations for simulation of real-world slips and trips: A systematic review. Gait Posture 2023, 100, 201–209. [Google Scholar] [CrossRef]
- Borkowski, R.; Błażkiewicz, M. Postural Reactions to External Mediolateral Perturbations: A Review. Appl. Sci. 2023, 13, 1696. [Google Scholar] [CrossRef]
- Bruijn, S.M.; Meijer, O.G.; Beek, P.J.; van Dieën, J.H. Assessing the stability of human locomotion: A review of current measures. J. R. Soc. Interface 2013, 10, 20120999. [Google Scholar] [CrossRef]
- Reisman, D.S.; Block, H.J.; Bastian, A.J. Interlimb coordination during locomotion: What can be adapted and stored? J. Neurophysiol. 2005, 94, 2403–2415. [Google Scholar] [CrossRef]
- Reisman, D.S.; McLean, H.; Bastian, A.J. Split-belt treadmill training poststroke: A case study. J. Neurol. Phys. Ther. JNPT 2010, 34, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Sado, T.; Nielsen, J.; Glaister, B.; Takahashi, K.Z.; Malcolm, P.; Mukherjee, M. A passive exoskeleton can assist split-belt adaptation. Exp. Brain Res. 2022, 240, 1159–1176. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Aprigliano, F.; Martelli, D.; Tropea, P.; Micera, S.; Monaco, V. Effects of slipping-like perturbation intensity on the dynamical stability. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5295–5298. [Google Scholar]
- Aprigliano, F.; Martelli, D.; Tropea, P.; Pasquini, G.; Micera, S.; Monaco, V. Aging does not affect the intralimb coordination elicited by slip-like perturbation of different intensities. J. Neurophysiol. 2017, 118, 1739–1748. [Google Scholar] [CrossRef]
- Martelli, D.; Aprigliano, F.; Tropea, P.; Pasquini, G.; Micera, S.; Monaco, V. Stability against backward balance loss: Age-related modifications following slip-like perturbations of multiple amplitudes. Gait Posture 2017, 53, 207–214. [Google Scholar] [CrossRef]
- van den Bogaart, M.; Bruijn, S.M.; van Dieën, J.H.; Meyns, P. The effect of anteroposterior perturbations on the control of the center of mass during treadmill walking. J. Biomech. 2020, 103, 109660. [Google Scholar] [CrossRef]
- Swart, S.B.; den Otter, R.; Lamoth, C.J.C. Anticipatory control of human gait following simulated slip exposure. Sci. Rep. 2020, 10, 9599. [Google Scholar] [CrossRef]
- Debelle, H.; Harkness-Armstrong, C.; Hadwin, K.; Maganaris, C.N.; O’Brien, T.D. Recovery From a Forward Falling Slip: Measurement of Dynamic Stability and Strength Requirements Using a Split-Belt Instrumented Treadmill. Front. Sports Act. Living 2020, 2, 82. [Google Scholar] [CrossRef] [PubMed]
- Hirata, K.; Kokubun, T.; Taku, M.; Hanawa, H.; Kubota, K.; Yokoyama, M.; Fujino, T.; Kanemura, N. Relationship Between the Walking Velocity Relative to the Slip Velocity and the Corrective Response. J. Med. Biol. Eng. 2020, 41, 25–33. [Google Scholar] [CrossRef]
- Golyski, P.R.; Vazquez, E.; Leestma, J.K.; Sawicki, G.S. Onset timing of treadmill belt perturbations influences stability during walking. J. Biomech. 2022, 130, 110800. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Kebbach, M.; Bruhn, S.; Yang, Q.; Lin, H.; Bader, R.; Tischer, T.; Lutter, C. Barefoot walking is more stable in the gait of balance recovery in older adults. BMC Geriatr. 2022, 22, 904. [Google Scholar] [CrossRef] [PubMed]
- Liss, D.J.; Carey, H.D.; Allen, J.L. Young adults use whole-body feedback and ankle proprioception to perceive small locomotor disturbances. Hum. Mov. Sci. 2023, 89, 103084. [Google Scholar] [CrossRef]
- Mueller, J.; Engel, T.; Mueller, S.; Kopinski, S.; Baur, H.; Mayer, F. Neuromuscular response of the trunk to sudden gait disturbances: Forward vs. backward perturbation. J. Electromyogr. Kinesiol. 2016, 30, 168–176. [Google Scholar] [CrossRef]
- Lee, B.C.; Kim, C.S.; Seo, K.H. The Body’s Compensatory Responses to Unpredictable Trip and Slip Perturbations Induced by a Programmable Split-Belt Treadmill. IEEE Trans. Neural Syst. Rehabil. Eng. A Publ. IEEE Eng. Med. Biol. Soc. 2019, 27, 1389–1396. [Google Scholar] [CrossRef]
- Ren, X.; Lutter, C.; Kebbach, M.; Bruhn, S.; Bader, R.; Tischer, T. Lower extremity joint compensatory effects during the first recovery step following slipping and stumbling perturbations in young and older subjects. BMC Geriatr. 2022, 22, 656. [Google Scholar] [CrossRef]
- Ren, X.; Lutter, C.; Kebbach, M.; Bruhn, S.; Yang, Q.; Bader, R.; Tischer, T. Compensatory Responses During Slip-Induced Perturbation in Patients with Knee Osteoarthritis Compared with Healthy Older Adults: An Increased Risk of Falls? Front. Bioeng. Biotechnol. 2022, 10, 893840. [Google Scholar] [CrossRef]
- Shokouhi, S.; Sritharan, P.; Lee, P.V. Recovering whole-body angular momentum and margin of stability after treadmill-induced perturbations during sloped walking in healthy young adults. Sci. Rep. 2024, 14, 4421. [Google Scholar] [CrossRef]
- Aprigliano, F.; Martelli, D.; Kang, J.; Kuo, S.-H.; Kang, U.J.; Monaco, V.; Micera, S.; Agrawal, S.K. Effects of repeated waist-pull perturbations on gait stability in subjects with cerebellar ataxia. J. NeuroEng. Rehabil. 2019, 16, 50. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, R.C.; Beltran, E.J.; Dingwell, J.B.; Wilken, J.M. Mediolateral angular momentum changes in persons with amputation during perturbed walking. Gait Posture 2015, 41, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Afschrift, M.; Pitto, L.; Aerts, W.; van Deursen, R.; Jonkers, I.; De Groote, F. Modulation of gluteus medius activity reflects the potential of the muscle to meet the mechanical demands during perturbed walking. Sci. Rep. 2018, 8, 11675. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, U.; Melzer, I.; Zeilig, G.; Plotnik, M. Muscle activation profile is modulated by unexpected balance loss in walking. Gait Posture 2022, 93, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Kao, P.-C.; Pierro, M.A. Motor adaptation to cognitive challenges and walking perturbations in healthy young adults. Gait Posture 2022, 92, 167–175. [Google Scholar] [CrossRef]
- Castano, C.R.; Lee, L.D.; Huang, H.J. Speeding up: Discrete mediolateral perturbations increased self-paced walking speed in young and older adults. Gait Posture 2023, 102, 198–204. [Google Scholar] [CrossRef]
- Molina, L.K.; Small, G.H.; Neptune, R.R. The influence of step width on balance control and response strategies during perturbed walking in healthy young adults. J. Biomech. 2023, 157, 111731. [Google Scholar] [CrossRef]
- Punt, M.; Bruijn, S.M.; Roeles, S.; van de Port, I.G.; Wittink, H.; van Dieën, J.H. Responses to gait perturbations in stroke survivors who prospectively experienced falls or no falls. J. Biomech. 2017, 55, 56–63. [Google Scholar] [CrossRef]
- Chien, J.E.; Hsu, W.L. Effects of Dynamic Perturbation-Based Training on Balance Control of Community-Dwelling Older Adults. Sci. Rep. 2018, 8, 17231. [Google Scholar] [CrossRef]
- Aprigliano, F.; Monaco, V.; Tropea, P.; Martelli, D.; Vitiello, N.; Micera, S. Effectiveness of a Robot-Mediated Strategy While Counteracting Multidirectional Slippages. Robotica 2019, 37, 2119–2131. [Google Scholar] [CrossRef]
- Rieger, M.M.; Papegaaij, S.; Pijnappels, M.; Steenbrink, F.; van Dieën, J.H. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin. Biomech. 2020, 75, 104988. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, U.; Kribus-Shmiel, L.; Zeilig, G.; Bahat, Y.; Kimel-Naor, S.; Melzer, I.; Plotnik, M. Novel methodology for assessing total recovery time in response to unexpected perturbations while walking. PLoS ONE 2020, 15, e0233510. [Google Scholar] [CrossRef] [PubMed]
- Aprigliano, F.; Martelli, D.; Micera, S.; Monaco, V. Intersegmental coordination elicited by unexpected multidirectional slipping-like perturbations resembles that adopted during steady locomotion. J. Neurophysiol. 2016, 115, 728–740. [Google Scholar] [CrossRef] [PubMed]
- Onushko, T.; Boerger, T.; Van Dehy, J.; Schmit, B.D. Dynamic stability and stepping strategies of young healthy adults walking on an oscillating treadmill. PLoS ONE 2019, 14, e0212207. [Google Scholar] [CrossRef] [PubMed]
- Gerards, M.; Marcellis, R.; Senden, R.; Poeze, M.; de Bie, R.; Meijer, K.; Lenssen, A. The effect of perturbation-based balance training on balance control and fear of falling in older adults: A single-blind randomised controlled trial. BMC Geriatr. 2023, 23, 305. [Google Scholar] [CrossRef]
- Monaco, V.; Rinaldi, L.A.; Macrì, G.; Micera, S. During walking elders increase efforts at proximal joints and keep low kinetics at the ankle. Clin. Biomech. 2009, 24, 493–498. [Google Scholar] [CrossRef]
- Vaughan, C.L.; O’Malley, M.J. Froude and the contribution of naval architecture to our understanding of bipedal locomotion. Gait Posture 2005, 21, 350–362. [Google Scholar] [CrossRef]
- van Dieën, J.H.; Pijnappels, M.; Bobbert, M.F. Age-related intrinsic limitations in preventing a trip and regaining balance after a trip. Saf. Sci. 2005, 43, 437–453. [Google Scholar] [CrossRef]
- Winter, D.A. Human balance and posture control during standing and walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Winter, D.A. Foot Trajectory in Human Gait: A Precise and Multifactorial Motor Control Task. Phys. Ther. 1992, 72, 45–53. [Google Scholar] [CrossRef]
- Lockhart, T. Biomechanics of Human Gait—Slip and Fall Analysis; Elsevier: Amsterdam, The Netherlands, 2013; pp. 466–476. [Google Scholar]
- Liu, J.; Lockhart, T.E. Age-related joint moment characteristics during normal gait and successful reactive-recovery from unexpected slip perturbations. Gait Posture 2009, 30, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, C.M.; Hunt, N.H. Unconstrained slip mechanics and stepping reactions depend on slip onset timing. J. Biomech. 2021, 125, 110572. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, T.E.; Woldstad, J.C.; Smith, J.L.; Ramsey, J.D. Effects of age related sensory degradation on perception of floor slipperiness and associated slip parameters. Saf. Sci. 2002, 40, 689–703. [Google Scholar] [CrossRef] [PubMed]
- Nagano, H.; Sparrow, W.A.; Begg, R.K. Biomechanical characteristics of slipping during unconstrained walking, turning, gait initiation and termination. Ergonomics 2013, 56, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Pijnappels, M.; Bobbert, M.F.; van Dieën, J.H. How early reactions in the support limb contribute to balance recovery after tripping. J. Biomech. 2005, 38, 627–634. [Google Scholar] [CrossRef]
- Vilensky, J.A.; Cook, J.A.; Cooper, J.L. Stumbling corrective responses in healthy human subjects to rapid reversal of treadmill direction. J. Electromyogr. Kinesiol. 1999, 9, 161–171. [Google Scholar] [CrossRef]
- Kim, W.H.; Kim, W.B.; Yun, C.K. The effects of forward and backward walking according to treadmill inclination in children with cerebral palsy. J. Phys. Ther. Sci. 2016, 28, 1569–1573. [Google Scholar] [CrossRef][Green Version]
- Sinitski, E.; Terry, K.; Wilken, J.; Dingwell, J. Effects of perturbation magnitude on dynamic stability when walking in destabilizing environments. J. Biomech. 2012, 45, 2084–2091. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).