A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets
Abstract
1. Introduction
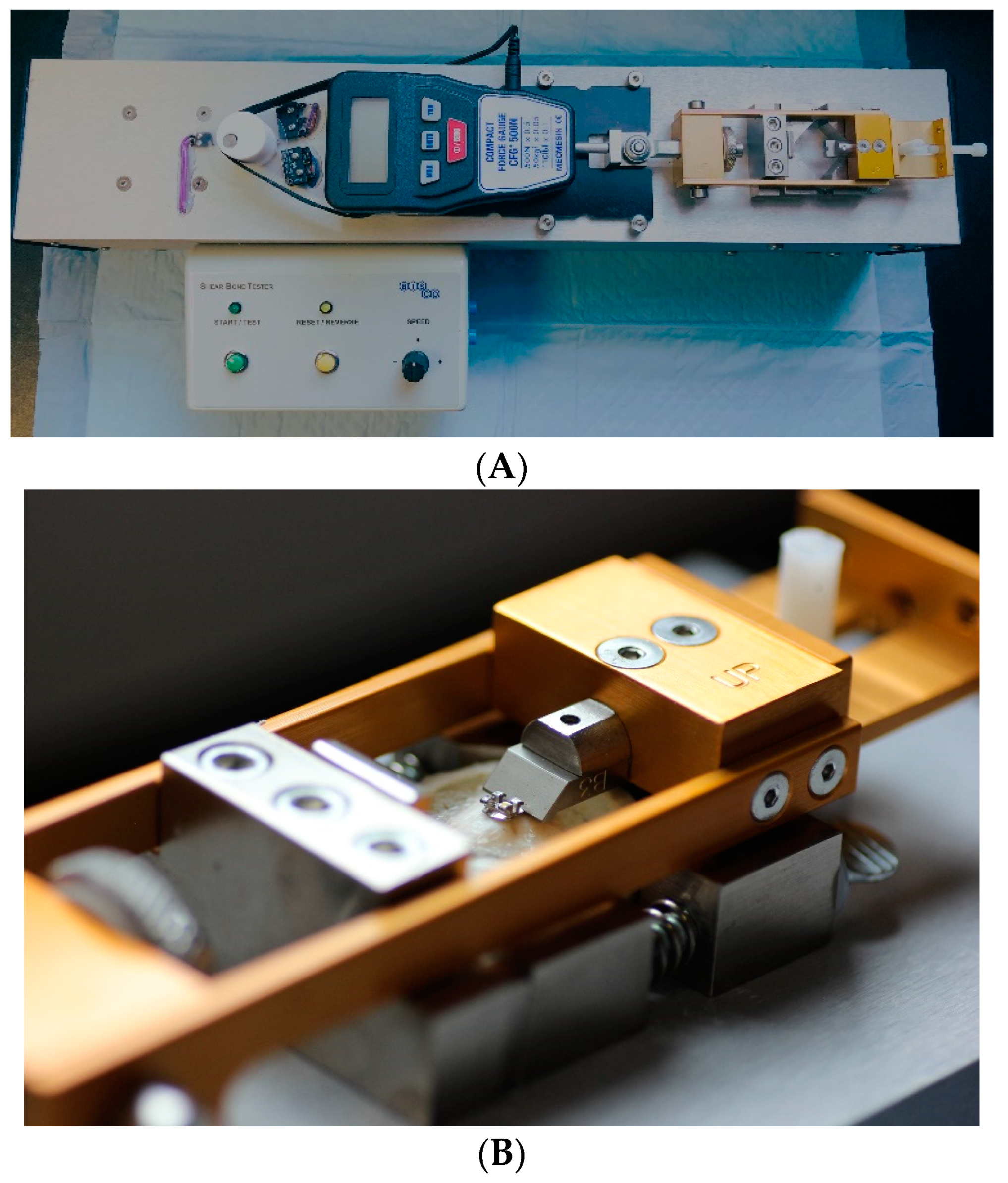
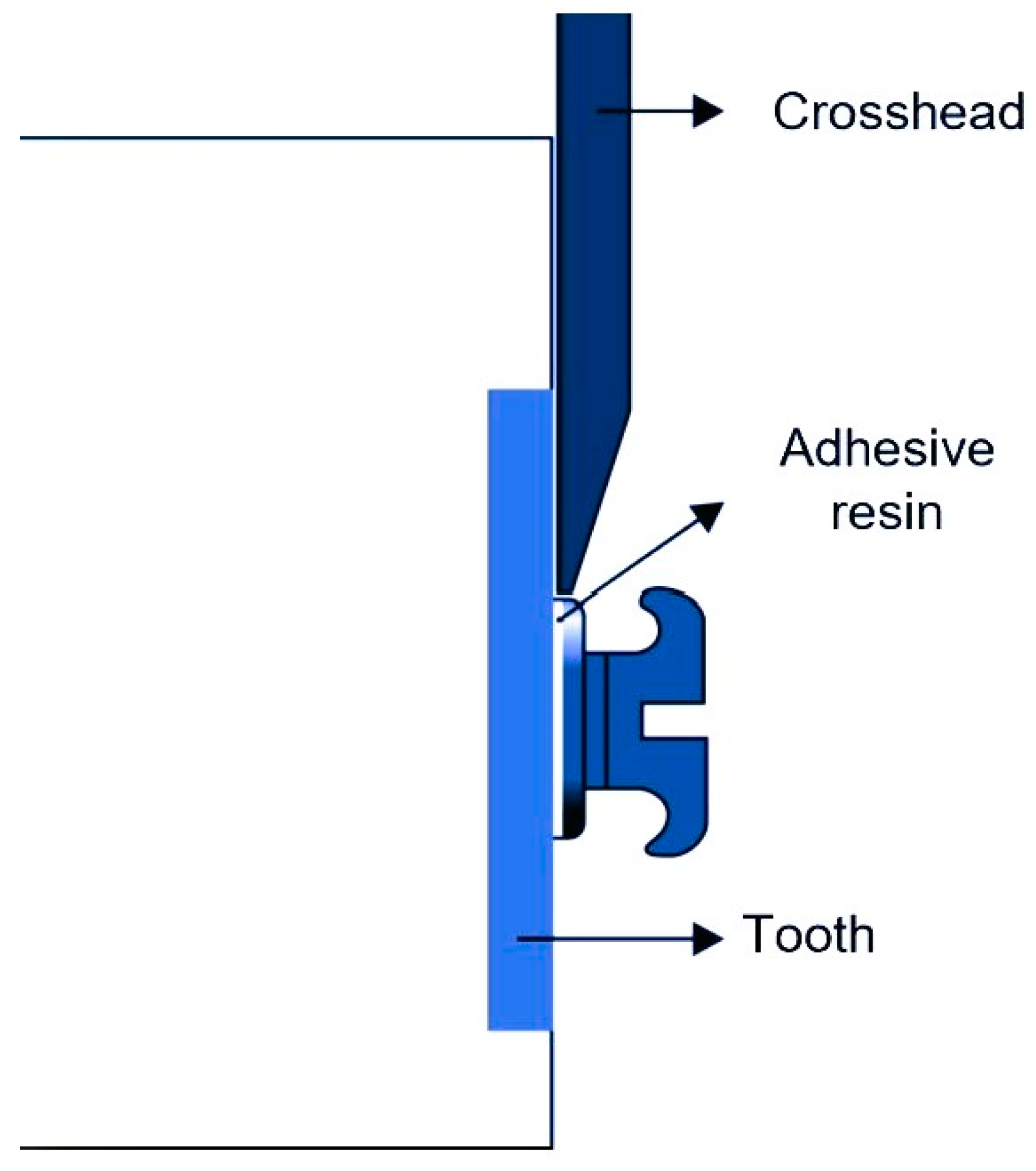
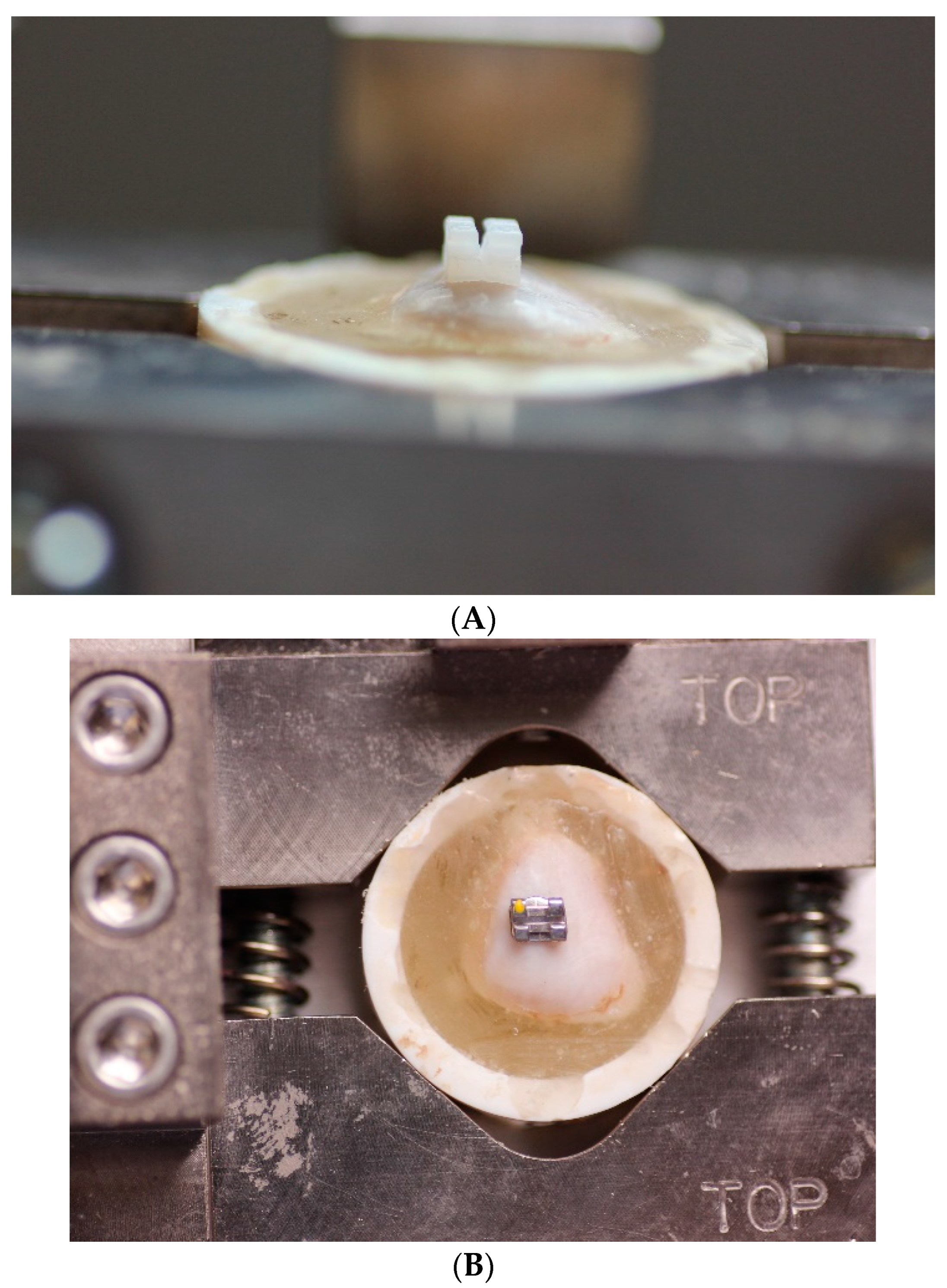
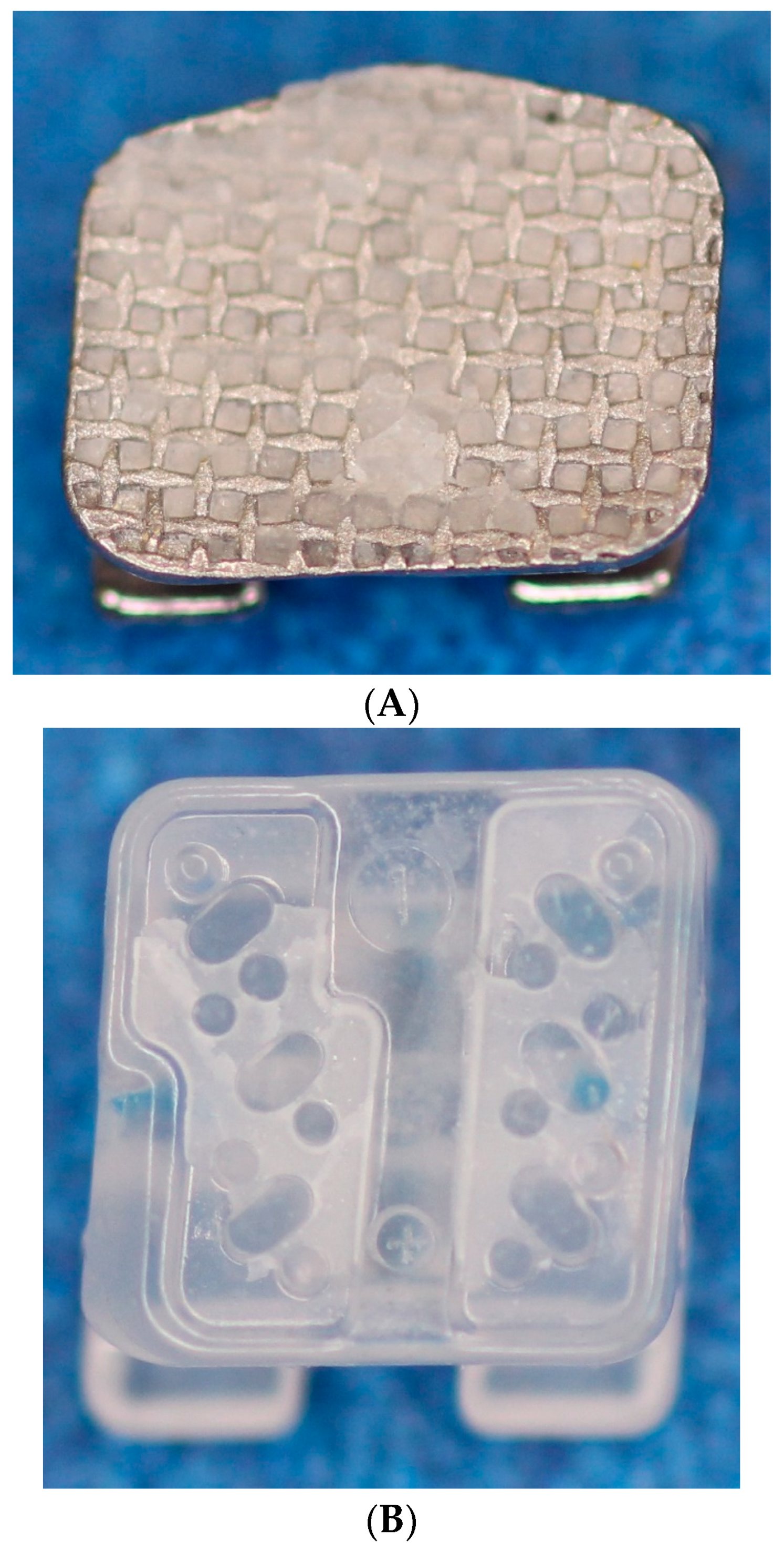
2. Materials and Methods
2.1. The Design and the Sample of This Study
2.2. Teeth and Bonding Procedures
2.3. Statistical Analysis
3. Results
3.1. Shear Bond Strength
3.2. Adhesive Remnant Index (ARI)
4. Discussion
5. Conclusions
- All the 3DB groups exhibited adequate SBSs that were lower compared to those for the conventional MB and CB groups.
- The majority of adhesive remnants for the 3DB groups remained on the bracket base, whereas, for conventional brackets, the majority remained on the enamel surfaces.
- The cleaning process following debonding appeared to be more efficient with 3D-printed brackets.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreira, F.C.; Jacob, H.B.; Vaz, L.G.; Guastaldi, A.C. Effect of Yd: YAG laser irradiation on the shear bond strength of orthodontic metal brackets. Dent. Press J. Orthasod. 2020, 25, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Huang, S.F.; Tsai, H.C.; Chang, W.J. Finite element sub-modeling analyses of damage to enamel at the incisor enamel/adhesive interface upon de-bonding for different orthodontic bracket bases. J. Biomech. 2011, 44, 134–142. [Google Scholar] [CrossRef]
- Kechagia, A.; Zinelis, S.; Pandis, N.; Athanasiou, A.E.; Eliades, T. The effect of orthodontic adhesive and bracket-base design in adhesive remnant index on enamel. J. World Fed. Orthod. 2015, 4, 18–22. [Google Scholar] [CrossRef]
- Sharma-Sayal, S.K.; Rossouw, P.E.; Kulkarni, G.V.; Titley, K.C. The influence of orthodontic bracket base design on shear bond strength. Am. J. Orthod. Dentofacial. Orthop. 2003, 124, 74–82. [Google Scholar] [CrossRef]
- Cozza, P.; Martucci, L.; De Toffol, L.; Penco, S.I. Shear bond strength of metal brackets on enamel. Angle Orthod. 2006, 76, 851–856. [Google Scholar] [PubMed]
- Sorel, O.; El Alam, R.; Chagneau, F.; Cathelineau, G. Comparison of bond strength between simple foil mesh and laser-structured base retention brackets. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 260–266. [Google Scholar] [CrossRef]
- Altmann, A.S.; Degrazia, F.W.; Celeste, R.K.; Leitune, V.C.; Samuel, S.M.; Collares, F.M. Orthodontic bracket bonding without previous adhesive priming: A meta-regression analysis. Angle Orthod. 2016, 86, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Rajesh, R.N.; Girish, K.S.; Sanjay, N.; Scindhia, R.D.; Kumar, S.G.; Rajesh, S. Comparison of Bond Strength of Brackets with Foil Mesh and Laser Structure Base using Light Cure Composite Resin: An in vitro Study. J. Contemp. Dent. Pract. 2015, 16, 963–970. [Google Scholar]
- Smith, D.C.; Maijer, R. Improvements in bracket base design. Am. J. Orthod. 1983, 83, 277–281. [Google Scholar] [CrossRef]
- Algera, T.J.; Kleverlaan, C.J.; Prahl-Andersen, B.; Feilzer, A.J. The influence of different bracket base surfaces on tensile and shear bond strength. Eur. J. Orthod. 2008, 30, 490–494. [Google Scholar] [CrossRef]
- Bishara, S.E.; Soliman, M.M.; Oonsombat, C.; Laffoon, J.F.; Ajlouni, R. The effect of variation in mesh-base design on the shear bond strength of orthodontic brackets. Angle Orthod. 2004, 74, 400–404. [Google Scholar] [PubMed]
- Elekdag-Türk, S. In vitro evaluation of a ceramic bracket with a laser-structured base. BMC Oral Health 2020, 20, 17. [Google Scholar] [CrossRef] [PubMed]
- Poorsattar-Bejeh Mir, A.; Rahmati-Kamel, M. Should the orthodontic brackets always be removed prior to magnetic resonance imaging (MRI)? J. Oral Biol. Craniofac. Res. 2016, 6, 142–152. [Google Scholar] [CrossRef]
- Russell, J.S. Aesthetic orthodontic brackets. J. Orthod. 2005, 32, 146–163. [Google Scholar] [CrossRef] [PubMed]
- Abend, R.; Dan, O.; Maoz, K.; Raz, S.; Bar-Haim, Y. Reliability, validity and sensitivity of a computerized visual analog scale measuring state anxiety. J. Behav. Ther. Exp. Psychiatry 2014, 45, 447–453. [Google Scholar] [CrossRef]
- Yang, L.; Yin, G.; Liao, X.; Yin, X.; Ye, N. A novel customized ceramic bracket for esthetic orthodontics: In vitro study. Prog. Orthod. 2019, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, P.E. A historical overview of the development of the acid-etch bonding system in orthodontics. In Seminars in Orthodontics; Elsevier: Amsterdam, The Netherlands, 2010; pp. 2–23. [Google Scholar]
- Wiechmann, D.; Rummel, V.; Thalheim, A.; Simon, J.S.; Wiechmann, L. Customized brackets and archwires for lingual orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 593–599. [Google Scholar] [CrossRef]
- Hodecker, L.D.; Scheurer, M.; Scharf, S.; Roser, C.J.; Fouda, A.M.; Bourauel, C.; Lux, C.J.; Bauer, C.A. Influence of Individual Bracket Base Design on the Shear Bond Strength of In-Office 3D Printed Brackets—An In Vitro Study. J. Funct. Biomater. 2023, 14, 289. [Google Scholar] [CrossRef]
- Bishara, S.E.; Soliman, M.; Laffoon, J.; Warren, J.J. Effect of changing a test parameter on the shear bond strength of orthodontic brackets. Angle Orthod. 2005, 75, 832–835. [Google Scholar]
- Artun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am. J. Orthod. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Soares, F.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.F.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef]
- Reynolds, I. A review of direct orthodontic bonding. Br. J. Orthod. 1975, 2, 171–178. [Google Scholar] [CrossRef]
- Sperber, R.L.; Watson, P.A.; Rossouw, P.E.; Sectakof, P.A. Adhesion of bonded orthodontic attachments to dental amalgam: In vitro study. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Mundstock, K.S.; Sadowsky, P.L.; Lacefield, W.; Bae, S. An in vitro evaluation of a metal reinforced orthodontic ceramic bracket. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Retief, D.H. Failure at the dental adhesive-etched enamel interface. J. Oral Rehabil. 1974, 1, 265–284. [Google Scholar] [CrossRef] [PubMed]
- Arash, V.; Naghipour, F.; Ravadgar, M.; Karkhah, A.; Barati, M.S. Shear bond strength of ceramic and metallic orthodontic brackets bonded with self-etching primer and conventional bonding adhesives. Electron. Physician 2017, 9, 3584–3591. [Google Scholar] [CrossRef] [PubMed]
- Mirzakouchaki, B.; Shirazi, S.; Sharghi, R.; Shirazi, S.; Moghimi, M.; Shahrbaf, S. Shear bond strength and debonding characteristics of metal and ceramic brackets bonded with conventional acid-etch and self-etch primer systems: An in-vivo study. J. Clin. Exp. Dent. 2016, 8, e38–e43. [Google Scholar] [CrossRef]
- Mirzakouchaki, B.; Kimyai, S.; Hydari, M.; Shahrbaf, S.; Mirzakouchaki-Boroujeni, P. Effect of self-etching primer/adhesive and conventional bonding on the shear bond strength in metallic and ceramic brackets. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e164–e170. [Google Scholar] [CrossRef][Green Version]
- Eminkahyagil, N.; Arman, A.; Cetinşahin, A.; Karabulut, E. Effect of resin-removal methods on enamel and shear bond strength of rebonded brackets. Angle Orthod. 2006, 76, 314–321. [Google Scholar]
- Tecco, S.; Traini, T.; Caputi, S.; Festa, F.; de Luca, V.; D’Attilio, M. A new one-step dental flowable composite for orthodontic use: An in vitro bond strength study. Angle Orthod. 2005, 75, 672–677. [Google Scholar]
- Gittner, R.; Müller-Hartwich, R.; Engel, S.; Jost-Brinkmann, P.-G. Shear bond strength and enamel fracture behavior of ceramic brackets Fascination® and Fascination®2. J. Orofac. Orthop. Fortschritte Kieferorthopadie 2012, 73, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Miller, A.; Orellana, M.F. Characterization of the porosity of human dental enamel and shear bond strength in vitro after variable etch times: Initial findings using the BET method. Angle Orthod. 2011, 81, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, L.J.; Shellhart, W.C.; Belanger, G.K. The use of bovine enamel in bonding studies. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, E.; Elsner, L.; Hirschfelder, U.; Ebert, T.; Hanke, S. Effects of enamel sealing on shear bond strength and the adhesive remnant index: Study of three fluoride-releasing adhesives in combination with metal and ceramic brackets. J. Orofac. Orthop. 2017, 78, 1–10. [Google Scholar] [CrossRef]
- Yassen, G.H.; Platt, J.A.; Hara, A.T. Bovine teeth as substitute for human teeth in dental research: A review of literature. J. Oral Sci. 2011, 53, 273–282. [Google Scholar] [CrossRef]
- Nakamichi, I.; Iwaku, M.; Fusayama, T. Bovine teeth as possible substitutes in the adhesion test. J. Dent. Res. 1983, 62, 1076–1081. [Google Scholar] [CrossRef]
- Pickett, K.L.; Sadowsky, P.L.; Jacobson, A.; Lacefield, W. Orthodontic in vivo bond strength: Comparison with in vitro results. Angle Orthod. 2001, 71, 141–148. [Google Scholar]
- Reimann, S.; Mezey, J.; Daratsianos, N.; Jäger, A.; Bourauel, C. The influence of adhesives and the base structure of metal brackets on shear bond strength. J. Orofac. Orthop. 2012, 73, 184–193. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]

| Bracket Type | Material | Base Size |
|---|---|---|
| 3D custom-printed (Lightforce, Cambridge, MA, USA) | Polycrystalline alumina | 12.06 mm2 |
| Chic Roth ceramic maxillary incisor brackets (GC Orthodontics America, Alsip, IL, USA) | Ceramic | 12.75 mm2 |
| Legend maxillary incisor brackets (GC Orthodontics America, Alsip, IL, USA) | Metal | 12.96 mm2 |
| Trade Name | Material | Bonding Procedures | Abbreviation |
|---|---|---|---|
| Lightforce | Polycrystalline alumina | 3DB + composite only (C) | 3DBC |
| Lightforce | Polycrystalline alumina | 3DB + composite (C) + Assure Plus (A) | 3DBCA |
| Lightforce | Polycrystalline alumina | 3DB + flowable only (F) | 3DBF |
| Lightforce | Polycrystalline alumina | 3DB + flowable (F) + Assure Plus (A) | 3DBFA |
| Chic Roth | Ceramic | CB + composite only (C) | CBC |
| Legend | Metal | MB + composite only (C) | MBC |
| Name of the Bracket | Number | Shear Bond Strength | ||||
|---|---|---|---|---|---|---|
| Mean | SD | SE | Median | IQR | ||
| 3DBC | 22 | 12.3 a | 1.53 | 0.326 | 11.9 | 2.54 |
| 3DBCA | 22 | 12.6 a | 1.85 | 0.395 | 12.6 | 2.43 |
| 3DBF | 22 | 12.3 a | 1.47 | 0.314 | 12.1 | 2.08 |
| 3DBFA | 22 | 11.0 a | 1.12 | 0.238 | 10.7 | 1.54 |
| CBC | 22 | 19.3 b | 5.54 | 1.180 | 20.0 | 10.00 |
| MBC | 22 | 16.9 b | 3.29 | 0.701 | 15.9 | 4.94 |
| Name of the Bracket | ARI of the Tooth * | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| 3DBC | 6 | 13 | 3 | 0 |
| 3DBCA | 4 | 15 | 2 | 1 |
| 3DBF | 13 | 8 | 1 | 0 |
| 3DBFA | 1 | 17 | 1 | 3 |
| CBC | 0 | 6 | 15 | 1 |
| MBC | 4 | 4 | 14 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jabr, L.; Rossouw, P.E.; Michelogiannakis, D.; Malik, S.; Wheeler, T.T.; Barmak, A.B. A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets. Appl. Sci. 2024, 14, 924. https://doi.org/10.3390/app14020924
Jabr L, Rossouw PE, Michelogiannakis D, Malik S, Wheeler TT, Barmak AB. A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets. Applied Sciences. 2024; 14(2):924. https://doi.org/10.3390/app14020924
Chicago/Turabian StyleJabr, Luay, P. Emile Rossouw, Dimitrios Michelogiannakis, Shaima Malik, Timothy T. Wheeler, and Abdul Basir Barmak. 2024. "A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets" Applied Sciences 14, no. 2: 924. https://doi.org/10.3390/app14020924
APA StyleJabr, L., Rossouw, P. E., Michelogiannakis, D., Malik, S., Wheeler, T. T., & Barmak, A. B. (2024). A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets. Applied Sciences, 14(2), 924. https://doi.org/10.3390/app14020924






