A Comprehensive Review of Virtual Reality Technology for Cognitive Rehabilitation in Patients with Neurological Conditions
Abstract
1. Introduction
2. Methodology
2.1. Search Strategy
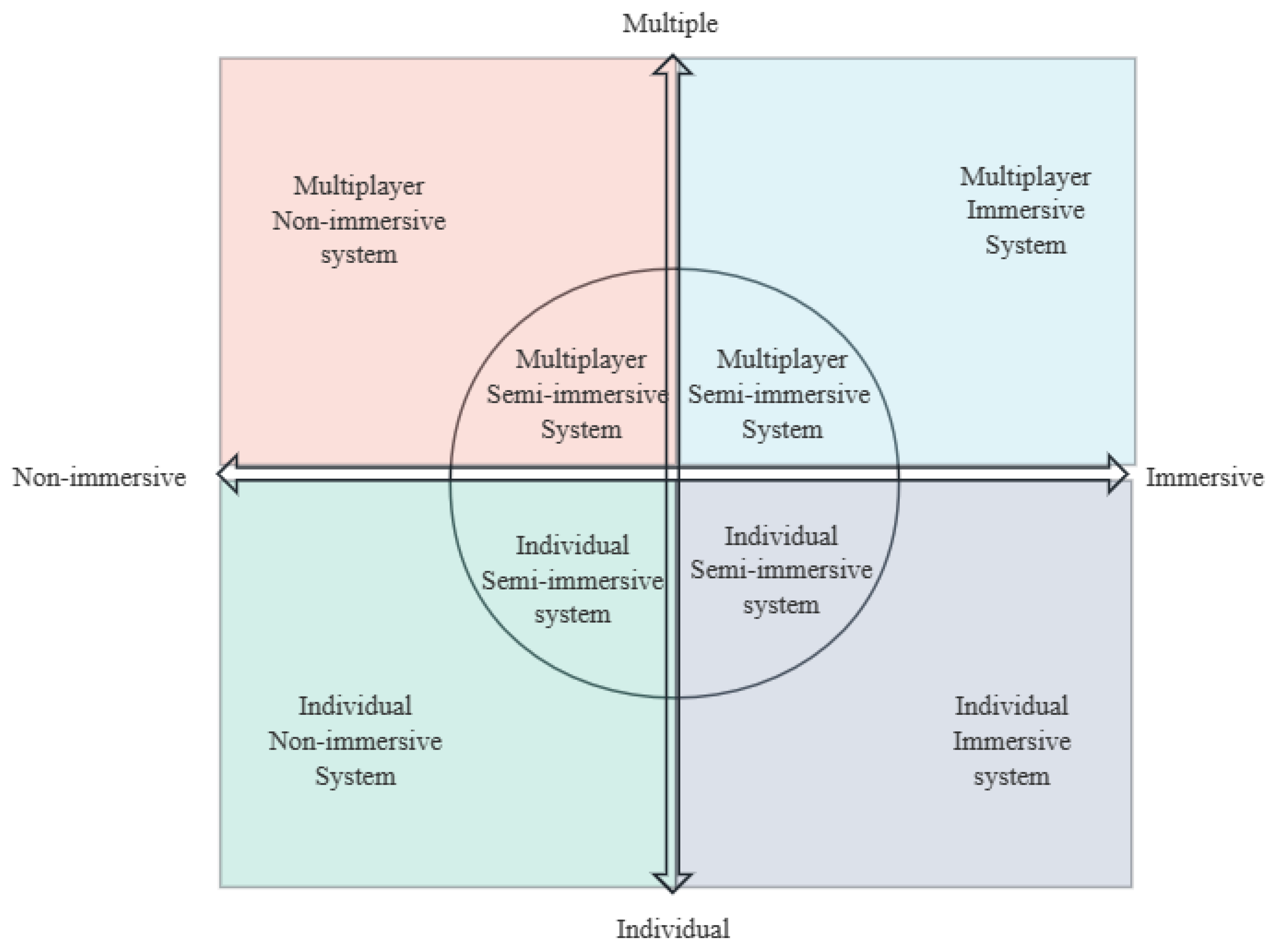
2.2. Model Construction
3. Practical Applications of VR in CR
3.1. Individual Immersive Systems
3.2. Individual Semi-Immersive Systems
3.3. Individual Non-Immersive Systems
3.4. Multiplayer Immersive Systems
3.5. Multiplayer Semi-Immersive Systems
3.6. Multiplayer Non-Immersive Systems
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hao, J.; Xie, H.; Harp, K.; Chen, Z.; Siu, K.C. Effects of virtual reality intervention on neural plasticity in stroke rehabilitation: A systematic review. Arch. Phys. Med. Rehabil. 2022, 103, 523–541. [Google Scholar] [CrossRef] [PubMed]
- Wiley, E.; Khattab, S.; Tang, A. Examining the effect of virtual reality therapy on cognition post-stroke: A systematic review and meta-analysis. Disabil. Rehabil. Assist. Technol. 2022, 17, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; De Bartolo, D.; Calabrò, R.S.; Ciancarelli, I.; Cerasa, A.; Tonin, P.; Di Iulio, F.; Paolucci, S.; Antonucci, G.; Morone, G.; et al. Computer-assisted cognitive rehabilitation in neurological patients: State-of-art and future perspectives. Front. Neurol. 2023, 14, 1255319. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Latella, D.; Maresca, G.; Sciarrone, F.; Manuli, A.; Naro, A.; De Luca, R.; Calabrò, R.S. Virtual reality and cognitive rehabilitation in people with stroke: An overview. J. Neurosci. Nurs. 2019, 51, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Cogollor, J.M.; Rojo-Lacal, J.; Hermsdörfer, J.; Ferre, M.; Waldmeyer, M.T.A.; Giachritsis, C.; Armstrong, A.; Martinez, J.M.B.; Loza, D.A.B.; Sebastián, J.M. Evolution of cognitive rehabilitation after stroke from traditional techniques to smart and personalized home-based information and communication technology systems: Literature review. JMIR Rehabil. Assist. Technol. 2018, 5, e8548. [Google Scholar] [CrossRef]
- Nie, P.; Liu, F.; Lin, S.; Guo, J.; Chen, X.; Chen, S.; Yu, L.; Lin, R. The effects of computer-assisted cognitive rehabilitation on cognitive impairment after stroke: A systematic review and meta-analysis. J. Clin. Nurs. 2022, 31, 1136–1148. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Téllez, P.; Moral-Muñoz, J.A.; Salazar, A.; Casado-Fernández, E.; Lucena-Antón, D. Game-based virtual reality interventions to improve upper limb motor function and quality of life after stroke: Systematic review and meta-analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Bergo, E.; Lombardi, G.; Pambuku, A.; Della Puppa, A.; Bellu, L.; D’avella, D.; Zagonel, V. Cognitive rehabilitation in patients with gliomas and other brain tumors: State of the art. BioMed Res. Int. 2016, 2016, 3041824. [Google Scholar] [CrossRef] [PubMed]
- Georgiev, D.D.; Georgieva, I.; Gong, Z.; Nanjappan, V.; Georgiev, G.V. Virtual reality for neurorehabilitation and cognitive enhancement. Brain Sci. 2021, 11, 221. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, A.S.; Fagundes, C.V.; dos Santos Mendes, F.A.; Leal, J.C. Effectiveness of virtual reality rehabilitation in persons with multiple sclerosis: A systematic review and meta-analysis of randomized controlled trials. Mult. Scler. Relat. Disord. 2021, 54, 103128. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Naro, A.; Colucci, P.V.; Pranio, F.; Tardiolo, G.; Billeri, L.; Le Cause, M.; De Domenico, C.; Portaro, S.; Rao, G.; et al. Improvement of brain functional connectivity in autism spectrum disorder: An exploratory study on the potential use of virtual reality. J. Neural Transm. 2021, 128, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Cisnal, A.; Martínez-Cagigal, V.; Alonso-Linaje, G.; Moreno-Calderón, S.; Pérez-Turiel, J.; Hornero, R.; Fraile, J. An Overview of M3Rob, a Robotic Platform for Neuromotor and Cognitive Rehabilitation Using Augmented Reality. In Proceedings of the Proc. XL Congreso Annual de la Sociedad Espa nola de Ingeniería Biomédica, Valladolid, Spain, 23–25 November 2022; pp. 180–183. [Google Scholar]
- Maggio, M.G.; De Luca, R.; Manuli, A.; Buda, A.; Foti Cuzzola, M.; Leonardi, S.; D’Aleo, G.; Bramanti, P.; Russo, M.; Calabrò, R.S. Do patients with multiple sclerosis benefit from semi-immersive virtual reality? A randomized clinical trial on cognitive and motor outcomes. Appl. Neuropsychol. Adult 2022, 29, 59–65. [Google Scholar] [CrossRef]
- Belger, J. DC: Clinical application of immersive VR in spatial cognition: The assessment of spatial memory and unilateral spatial neglect in neurological patients. In Proceedings of the 2021 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW), Lisbon, Portugal, 27 March–1 April 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 723–724. [Google Scholar]
- Rogers, J.M.; Duckworth, J.; Middleton, S.; Steenbergen, B.; Wilson, P.H. Elements virtual rehabilitation improves motor, cognitive, and functional outcomes in adult stroke: Evidence from a randomized controlled pilot study. J. Neuroeng. Rehabil. 2019, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef] [PubMed]
- Paulino, T.; Faria, A.L.; i Badia, S.B. Reh@ City v2. 0: A comprehensive virtual reality cognitive training system based on personalized and adaptive simulations of activities of daily living. In Proceedings of the 2019 5th Experiment International Conference (exp. at’19), Funchal, Portugal, 12–14 June 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 292–297. [Google Scholar]
- Feitosa, J.; Stefano Filho, C.A.; Casseb, R.; Camargo, A.; Martins, B.; Ballester, B.R.; Omedas, P.; Verschure, P.; Oberg, T.; Min, L.L.; et al. Complex network changes during a virtual reality rehabilitation protocol following stroke: A case study. In Proceedings of the 2019 9th International IEEE/EMBS Conference on Neural Engineering (NER), San Francisco, CA, USA, 20–23 March 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 891–894. [Google Scholar]
- Bagce, H.F.; Saleh, S.; Adamovich, S.V.; Tunik, E. Visuomotor gain distortion alters online motor performance and enhances primary motor cortex excitability in patients with stroke. Neuromodul. Technol. Neural Interface 2012, 15, 361–366. [Google Scholar] [CrossRef] [PubMed]
- San Luis, M.A.V.; Atienza, R.O.; San Luis, A.M. Immersive virtual reality as a supplement in the rehabilitation program of post-stroke patients. In Proceedings of the 2016 10th International Conference on Next Generation Mobile Applications, Security and Technologies (NGMAST), Cardiff, UK, 24–26 August 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 47–52. [Google Scholar]
- Pazzaglia, C.; Imbimbo, I.; Tranchita, E.; Minganti, C.; Ricciardi, D.; Monaco, R.L.; Parisi, A.; Padua, L. Comparison of virtual reality rehabilitation and conventional rehabilitation in Parkinson’s disease: A randomised controlled trial. Physiotherapy 2020, 106, 36–42. [Google Scholar] [CrossRef]
- Lamontagne, A.; Blanchette, A.K.; Fung, J.; McFadyen, B.J.; Sangani, S.; Robitaille, N.; Deblock-Bellamy, A.; Bühler, M.A.; Perez, C.; Anita, M. Development of a virtual reality toolkit to enhance community walking after stroke. In Proceedings of the 2019 International Conference on Virtual Rehabilitation (ICVR), Tel Aviv, Israel, 21–24 July 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1–3. [Google Scholar]
- Morone, G.; Spitoni, G.F.; De Bartolo, D.; Ghanbari Ghooshchy, S.; Di Iulio, F.; Paolucci, S.; Zoccolotti, P.; Iosa, M. Rehabilitative devices for a top-down approach. Expert Rev. Med. Devices 2019, 16, 187–195. [Google Scholar] [CrossRef]
- Burdea, G.C.; Defais, C. Repetitive bimanual integrative therapy (RABIT) virtual rehabilitation system. In Proceedings of the 2013 IEEE Virtual Reality (VR), Lake Buena Vista, FL, USA, 18–20 March 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 99–100. [Google Scholar]
- Kim, B.R.; Chun, M.H.; Kim, L.S.; Park, J.Y. Effect of virtual reality on cognition in stroke patients. Ann. Rehabil. Med. 2011, 35, 450. [Google Scholar] [CrossRef] [PubMed]
- Burdea, G.; Polistico, K.; Krishnamoorthy, A.; House, G.; Rethage, D.; Hundal, J.; Damiani, F.; Pollack, S. Feasibility study of the BrightBrainer™ integrative cognitive rehabilitation system for elderly with dementia. Disabil. Rehabil. Assist. Technol. 2015, 10, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, R.S.; Russo, M.; Naro, A.; De Luca, R.; Leo, A.; Tomasello, P.; Molonia, F.; Dattola, V.; Bramanti, A.; Bramanti, P. Robotic gait training in multiple sclerosis rehabilitation: Can virtual reality make the difference? Findings from a randomized controlled trial. J. Neurol. Sci. 2017, 377, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Kılıc, M.M.; Muratlı, O.C.; Catal, C. Virtual reality based rehabilitation system for Parkinson and multiple sclerosis patients. In Proceedings of the 2017 International Conference on Computer Science and Engineering (UBMK), Antalya, Turkey, 5–7 October 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 328–331. [Google Scholar]
- Pedraza-Hueso, M.; Martín-Calzón, S.; Díaz-Pernas, F.J.; Martínez-Zarzuela, M. Rehabilitation using kinect-based games and virtual reality. Procedia Comput. Sci. 2015, 75, 161–168. [Google Scholar] [CrossRef]
- Maggio, M.G.; De Cola, M.C.; Latella, D.; Maresca, G.; Finocchiaro, C.; La Rosa, G.; Cimino, V.; Sorbera, C.; Bramanti, P.; De Luca, R.; et al. What about the role of virtual reality in Parkinson disease’s cognitive rehabilitation? Preliminary findings from a randomized clinical trial. J. Geriatr. Psychiatry Neurol. 2018, 31, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Chun, M.H.; Son, Y.R. Effect of virtual reality on cognitive dysfunction in patients with brain tumor. Ann. Rehabil. Med. 2014, 38, 726. [Google Scholar] [CrossRef] [PubMed]
- Vourvopoulos, A.; Faria, A.L.; Cameirao, M.S.; i Badia, S.B. RehabNet: A distributed architecture for motor and cognitive neuro-rehabilitation. In Proceedings of the 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013), Lisbon, Portugal, 9–12 October 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 454–459. [Google Scholar]
- Kirner, C.; Kirner, T.G. Development of an interactive artifact for cognitive rehabilitation based on augmented reality. In Proceedings of the 2011 International Conference on Virtual Rehabilitation, Zurich, Switzerland, 27–29 June 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 1–7. [Google Scholar]
- Ko, L.W.; Stevenson, C.; Chang, W.C.; Yu, K.H.; Chi, K.C.; Chen, Y.J.; Chen, C.H. Integrated gait triggered mixed reality and neurophysiological monitoring as a framework for next-generation ambulatory stroke rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2435–2444. [Google Scholar] [CrossRef] [PubMed]
- González-Ortega, D.; Díaz-Pernas, F.J.; Martínez-Zarzuela, M.; Antón-Rodríguez, M. A Kinect-based system for cognitive rehabilitation exercises monitoring. Comput. Methods Programs Biomed. 2014, 113, 620–631. [Google Scholar] [CrossRef]
- Shapi’i, A.; Mat Zin, N.A.; Elaklouk, A.M. A game system for cognitive rehabilitation. BioMed Res. Int. 2015, 2015, 493562. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yi, S.H.; Ao, L.; Tang, X.; Xu, X.; Shim, D.; Yoo, B.; Park, E.S.; Rha, D.w. Virtual reality rehabilitation in children with brain injury: A randomized controlled trial. Dev. Med. Child Neurol. 2021, 63, 480–487. [Google Scholar] [CrossRef]
- Mondellini, M.; Arlati, S.; Pizzagalli, S.; Greci, L.; Sacco, M.; Ferrigno, G. Assessment of the usability of an immersive virtual supermarket for the cognitive rehabilitation of elderly patients: A pilot study on young adults. In Proceedings of the 2018 IEEE 6th International Conference on Serious Games and Applications for Health (SeGAH), Vienna, Austria, 16–18 May 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–8. [Google Scholar]
- Park, J.S.; Jung, Y.J.; Lee, G. Virtual reality-based cognitive–motor rehabilitation in older adults with mild cognitive impairment: A randomized controlled study on motivation and cognitive function. Healthcare 2020, 8, 335. [Google Scholar] [CrossRef] [PubMed]
- Torrisi, M.; Maresca, G.; De Cola, M.C.; Cannavò, A.; Sciarrone, F.; Silvestri, G.; Bramanti, A.; De Luca, R.; Calabrò, R.S. Using telerehabilitation to improve cognitive function in post-stroke survivors: Is this the time for the continuity of care? Int. J. Rehabil. Res. 2019, 42, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Bozgeyikli, L.; Bozgeyikli, E.; Raij, A.; Alqasemi, R.; Katkoori, S.; Dubey, R. Vocational rehabilitation of individuals with autism spectrum disorder with virtual reality. ACM Trans. Access. Comput. 2017, 10, 1–25. [Google Scholar] [CrossRef]
- Chatterjee, K.; Buchanan, A.; Cottrell, K.; Hughes, S.; Day, T.W.; John, N.W. Immersive virtual reality for the cognitive rehabilitation of stroke survivors. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 719–728. [Google Scholar] [CrossRef]
- Gabrielli, S.; Cristofolini, M.; Dianti, M.; Alvari, G.; Vallefuoco, E.; Bentenuto, A.; Venuti, P.; Ibarra, O.M.; Salvadori, E. Co-Design of a Virtual Reality Multiplayer Adventure Game for Adolescents With Autism Spectrum Disorder: Mixed Methods Study. JMIR Serious Games 2023, 11, e51719. [Google Scholar] [CrossRef]
- Tieri, G.; Morone, G.; Paolucci, S.; Iosa, M. Virtual reality in cognitive and motor rehabilitation: Facts, fiction and fallacies. Expert Rev. Med. Devices 2018, 15, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Cameirão, M.S.; Pereira, F.; i Badia, S.B. Virtual reality with customized positive stimuli in a cognitive-motor rehabilitation task. In Proceedings of the 2017 International Conference on Virtual Rehabilitation (ICVR), Montréal, QC, Canada, 19–22 June 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1–7. [Google Scholar]
- De Luca, R.; Maggio, M.G.; Maresca, G.; Latella, D.; Cannavò, A.; Sciarrone, F.; Lo Voi, E.; Accorinti, M.; Bramanti, P.; Calabrò, R.S.; et al. Improving cognitive function after traumatic brain injury: A clinical trial on the potential use of the semi-immersive virtual reality. Behav. Neurol. 2019, 2019, 9268179. [Google Scholar] [CrossRef] [PubMed]
- Dockx, K.; Bekkers, E.M.; Van den Bergh, V.; Ginis, P.; Rochester, L.; Hausdorff, J.M.; Mirelman, A.; Nieuwboer, A. Virtual reality for rehabilitation in Parkinson’s disease. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Pietrzak, E.; Pullman, S.; McGuire, A. Using virtual reality and videogames for traumatic brain injury rehabilitation: A structured literature review. Games Heal. Res. Dev. Clin. Appl. 2014, 3, 202–214. [Google Scholar] [CrossRef]
- Garcia-Betances, R.I.; Jiménez-Mixco, V.; Arredondo, M.T.; Cabrera-Umpiérrez, M.F. Using virtual reality for cognitive training of the elderly. Am. J. Alzheimer’s Dis. Other Dementias 2015, 30, 49–54. [Google Scholar] [CrossRef]
- Moro, S.B.; Carrieri, M.; Avola, D.; Brigadoi, S.; Lancia, S.; Petracca, A.; Spezialetti, M.; Ferrari, M.; Placidi, G.; Quaresima, V. A novel semi-immersive virtual reality visuo-motor task activates ventrolateral prefrontal cortex: A functional near-infrared spectroscopy study. J. Neural Eng. 2016, 13, 036002. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Reid, D. Using the virtual reality-cognitive rehabilitation approach to improve contextual processing in children with autism. Sci. World J. 2013, 2013, 716890. [Google Scholar] [CrossRef] [PubMed]
- Glegg, S.M.; Tatla, S.K.; Holsti, L. The GestureTek virtual reality system in rehabilitation: A scoping review. Disabil. Rehabil. Assist. Technol. 2014, 9, 89–111. [Google Scholar] [CrossRef] [PubMed]
- Bellani, M.; Fornasari, L.; Chittaro, L.; Brambilla, P. Virtual reality in autism: State of the art. Epidemiol. Psychiatr. Sci. 2011, 20, 235–238. [Google Scholar] [CrossRef]
- De La Guía, E.; Lozano, M.D.; Penichet, V.R. Cognitive rehabilitation based on collaborative and tangible computer games. In Proceedings of the 2013 7th International Conference on Pervasive Computing Technologies for Healthcare and Workshops, Venice, Italy, 5–8 May 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 389–392. [Google Scholar]
- Gandolfi, M.; Geroin, C.; Dimitrova, E.; Boldrini, P.; Waldner, A.; Bonadiman, S.; Picelli, A.; Regazzo, S.; Stirbu, E.; Primon, D.; et al. Virtual reality telerehabilitation for postural instability in Parkinson’s disease: A multicenter, single-blind, randomized, controlled trial. BioMed Res. Int. 2017, 2017, 7962826. [Google Scholar] [CrossRef] [PubMed]
- Faria, A.L.; Pinho, M.S.; Bermúdez i Badia, S. A comparison of two personalization and adaptive cognitive rehabilitation approaches: A randomized controlled trial with chronic stroke patients. J. Neuroeng. Rehabil. 2020, 17, 78. [Google Scholar] [CrossRef]
- Thumm, P.C.; Giladi, N.; Hausdorff, J.M.; Mirelman, A. Tele-rehabilitation with virtual reality: A case report on the simultaneous, remote training of two patients with Parkinson disease. Am. J. Phys. Med. Rehabil. 2021, 100, 435–438. [Google Scholar] [CrossRef]


| Study | Technology Type | Study Type | Sample Size | Patients | Results |
|---|---|---|---|---|---|
| Chatterjee et al., 2022 [45] | Multiplayer Immersive System | Double-Blind Phase 2b RCT 1 | 40 | Stroke | VR 2 can improve memory and resolution in stroke survivors. |
| Bagce et al., 2012 [22] | Individual Immersive System | Repeated Measures Design Experiment | 8 | Stroke | VR training is beneficial for the recovery of hand motor function after stroke. |
| San Luis et al., 2016 [23] | Individual Immersive System and Individual Non-immersive System | Repeated Measures Design Experiment | 8 | Stroke | VR training is beneficial for the recovery of hand motor function after stroke. |
| Lamontagne et al., 2019 [25] | Individual Immersive System | Prototype Development and User Feedback Experiment | 12 | Stroke | A toolkit using virtual reality technology could improve community walking rehabilitation for stroke survivors. |
| Kim et al., 2011 [28] | Individual Semi-immersive System | RCT | 18 | Stroke | The study found that patients with stroke cognitive impairment showed significant improvements in visual attention and short-term visuospatial memory when receiving a combination of computer-assisted and virtual reality therapy, compared with only receiving computer-assisted cognitive rehabilitation therapy. |
| Burdea et al., 2013 [27] | Individual Semi-immersive System | Feasibility Study | 10 | Stroke | Studies have shown that using the Razer Hydra gaming interface, patients can play a series of customized games that help improve focus, decision making (executive function), and short- and long-term memory. |
| Pazzaglia et al., 2020 [24] | Individual Immersive System and Individual Non-immersive System | RCT | 51 | PD 3 | Compared to the traditional group, the VR group showed greater improvements in the psychological aspects of balance, walking, arm function, and quality of life. |
| Lozano et al., 2013 [57] | Individual Immersive System and Individual Non-immersive System | Feasibility Study | 10 | AD 4 | Compared to the control group, the experimental group had greater improvements in cognitive function in terms of executive and visuospatial abilities. |
| Gandolfi et al., 2017 [58] | Multiplayer Non-immersive system | Multicenter, Single-Blind RCT | 76 | PD | VR balance training can reduce postural instability in PD patients. |
| Thumm et al., 2021 [60] | Multiplayer Semi-immersive Immersive System | Feasibility Study | 2 | PD | VR tele-rehabilitation therapy can improve patients’ confidence, gait speed, and mobility. Training multiple participants at the same time is feasible, enabling a personalized approach to therapy while saving the therapist time. |
| Choi et al., 2021 [40] | Individual Non-immersive System | RCT | 80 | TBI 5 | The VR treatment group showed more significant improvements in upper limb dexterity function, and children with more severe motor impairments showed significant improvements compared to children with less severe motor impairments. |
| Shapi’i et al., 2015 [39] | Individual Non-immersive System | Design and Evaluation Experiment | 10 | TBI and Stroke | The rehabilitation game system can improve the rehabilitation effect and ability by providing personalized rehabilitation game experience to improve patients’ enthusiasm. |
| González-Ortega et al., 2014 [38] | Individual Non-immersive System | System Development and Evaluation Experiment | 15 | TBI | This paper presents a real-time 3D computer vision aid system for psychomotor exercise monitoring, which is intended to help evaluate structural dysfunction and left–right disorder. |
| Maggio et al., 2023 [3] | Individual Non-immersive System | RCT | 60 | MS 6 | The VR rehabilitation approach not only improved cognitive and emotional outcomes in people with multiple sclerosis, but also improved motor function. |
| Calabrò et al., 2017 [30] | Individual Semi-immersive System | RCT | 40 | MS | RAGT(Robot-Assisted Gait Training) + VR can effectively improve walking ability and hip movement ability. |
| KıLıC et al., 2017 [31] | Individual Semi-immersive System | Multicenter, Single-Blind, RCT | 60 | MS and PD | VR-based rehabilitation system that provides active education and rehabilitation processes through gamification for people with Parkinson’s and multiple sclerosis. |
| De La Guia et al., 2013 [57] | Multiplayer Non-immersive system | Feasibility Study | 10 | AD | The system can enhance mental abilities such as perception, attention, reasoning, abstraction, memory, language, and orientation processes. |
| Burdea et a., 2017 [29] | Individual Semi-immersive System | Integrative Therapy and User Feedback Experiment | 36 | AD | BrightBrainer bimanual cognitive integrated simulation training improved participants’ executive function, processing speed, and auditory attention. |
| DE Luca et al., 2021 [14] | Individual Semi-immersive System | Clinical Trial | 100 | ASD 7 | VR therapy can improve patients’ cognitive and behavioral problems such as attention, visuospatial cognition, and anxiety. |
| Bozgeyikli et al., 2017 [44] | Multiplayer Immersive System | RCT | 18 | ASD | After VR4VR system training, the corresponding skills of ASD patients were improved to a certain extent. The VR4VR system can provide effective vocational training for ASD patients. |
| Wang et al., 2013 [54] | Multiplayer Non-immersive system | Experimental Study | 4 | ASD | After VR cognitive rehabilitation, the overall situation processing ability and cognitive flexibility of children with ASD were significantly improved. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quan, W.; Liu, S.; Cao, M.; Zhao, J. A Comprehensive Review of Virtual Reality Technology for Cognitive Rehabilitation in Patients with Neurological Conditions. Appl. Sci. 2024, 14, 6285. https://doi.org/10.3390/app14146285
Quan W, Liu S, Cao M, Zhao J. A Comprehensive Review of Virtual Reality Technology for Cognitive Rehabilitation in Patients with Neurological Conditions. Applied Sciences. 2024; 14(14):6285. https://doi.org/10.3390/app14146285
Chicago/Turabian StyleQuan, Wei, Shikai Liu, Meng Cao, and Jiale Zhao. 2024. "A Comprehensive Review of Virtual Reality Technology for Cognitive Rehabilitation in Patients with Neurological Conditions" Applied Sciences 14, no. 14: 6285. https://doi.org/10.3390/app14146285
APA StyleQuan, W., Liu, S., Cao, M., & Zhao, J. (2024). A Comprehensive Review of Virtual Reality Technology for Cognitive Rehabilitation in Patients with Neurological Conditions. Applied Sciences, 14(14), 6285. https://doi.org/10.3390/app14146285







