A New Automatic Process Based on Generative Design for CAD Modeling and Manufacturing of Customized Orthosis
Abstract
1. Introduction
2. Materials and Methods
2.1. 3D Acquisition by Photogrammetry
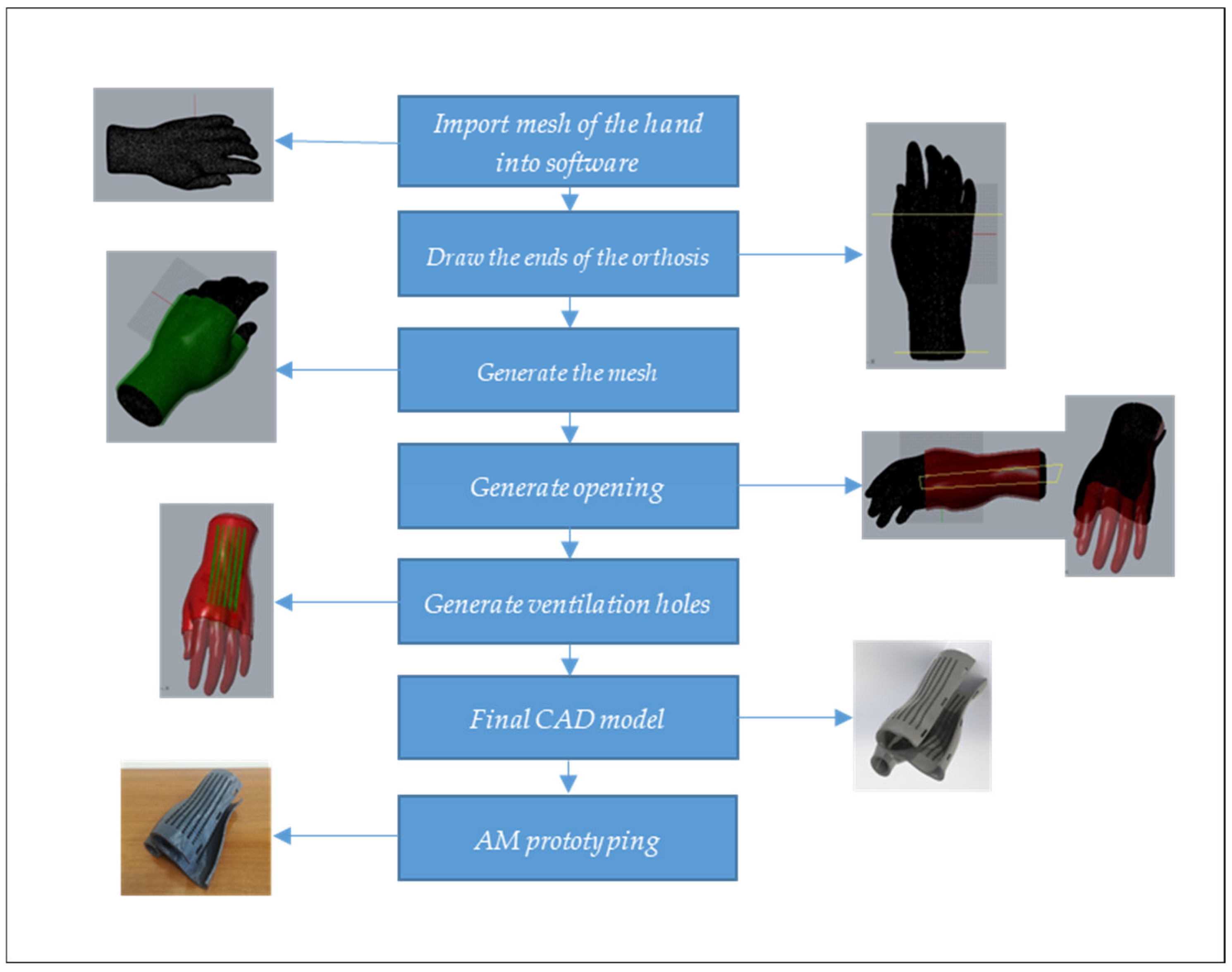
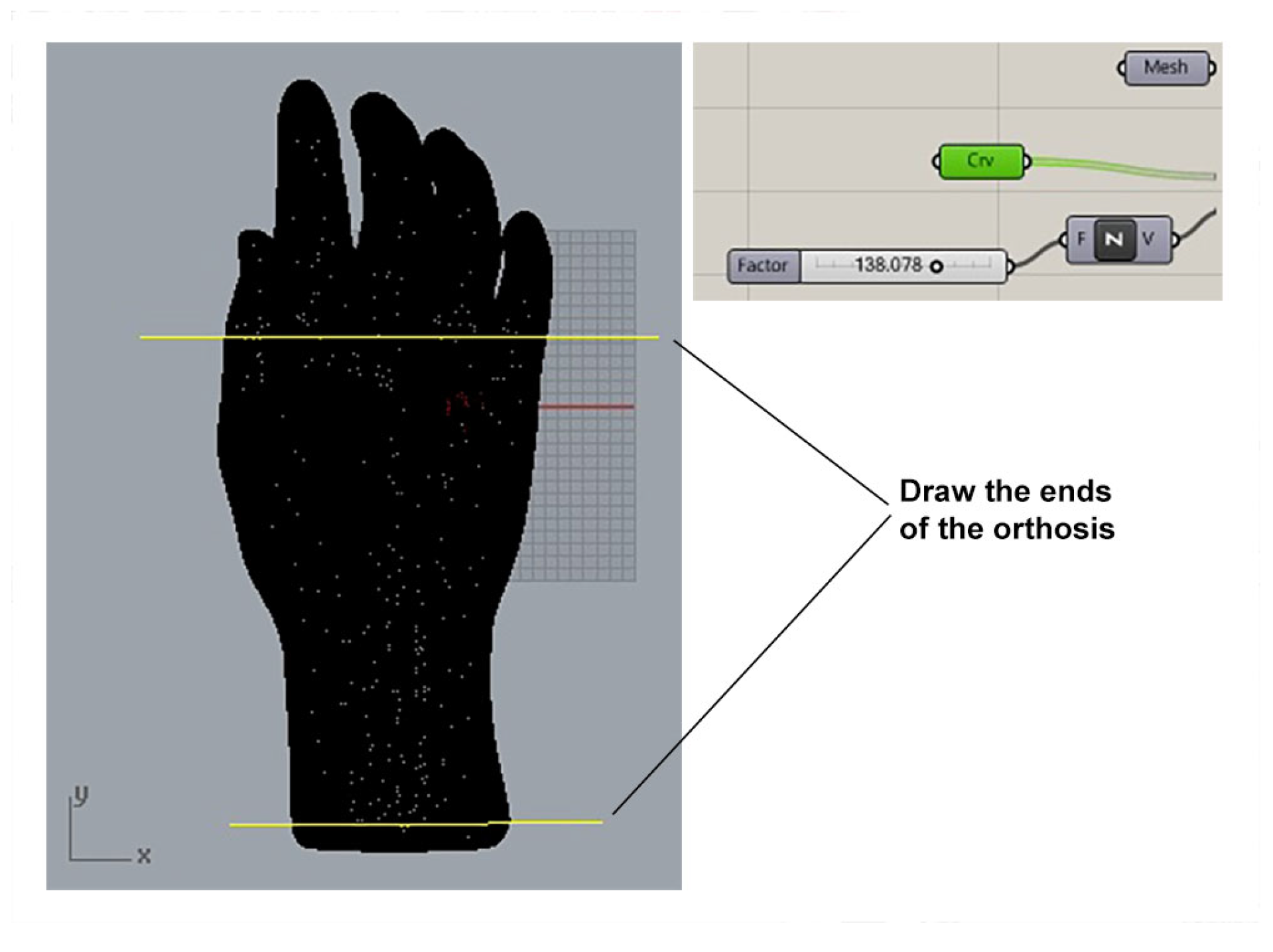
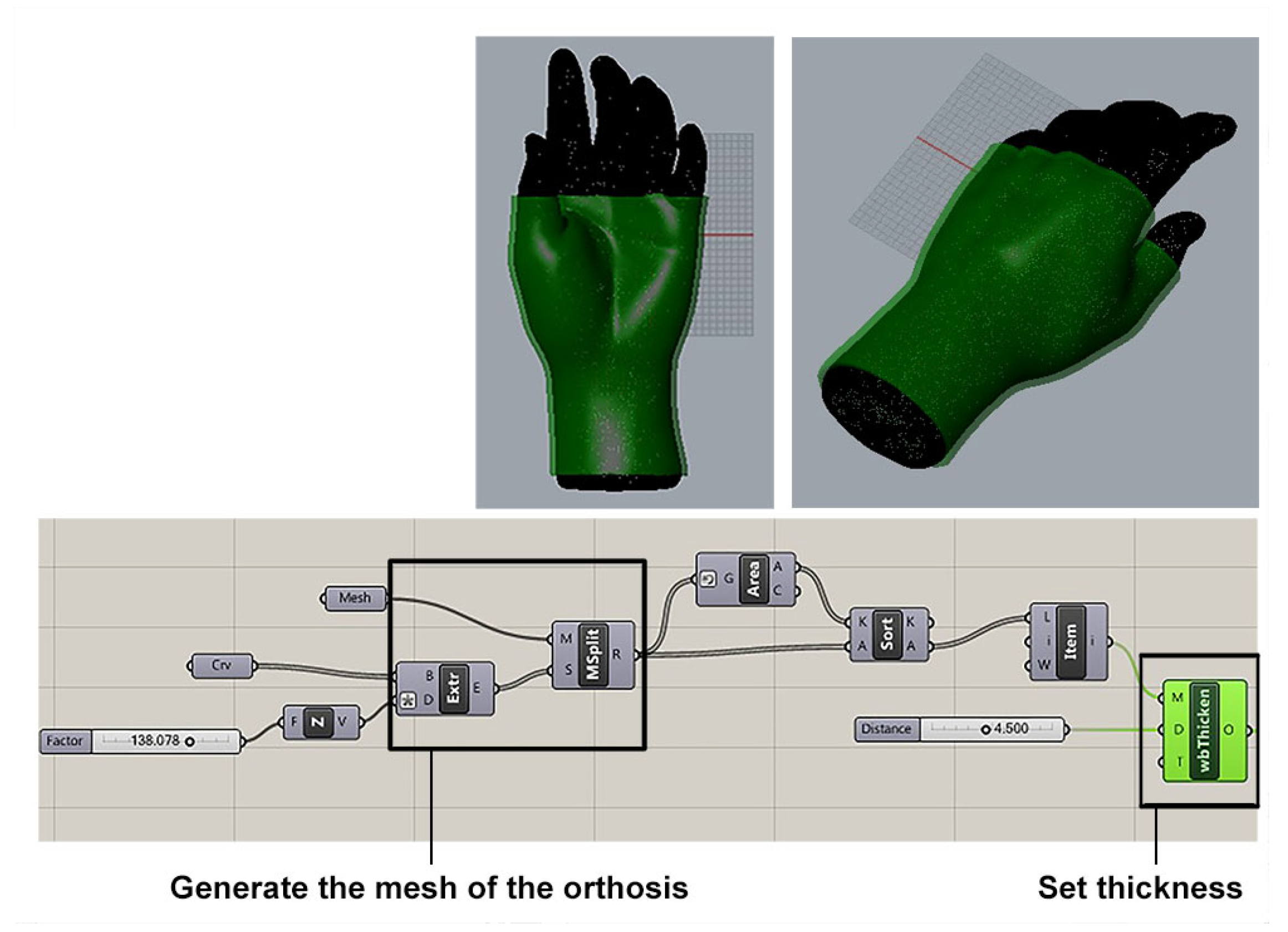
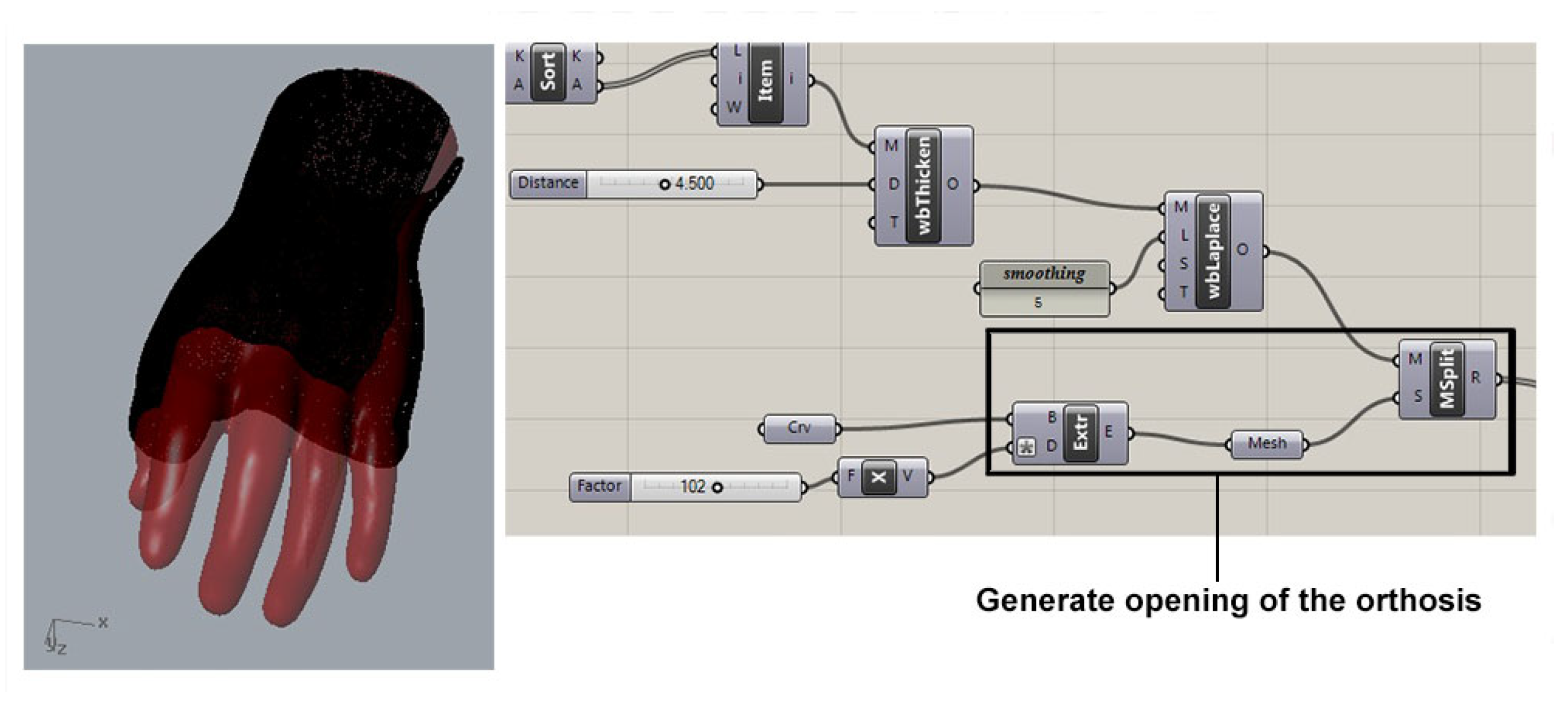
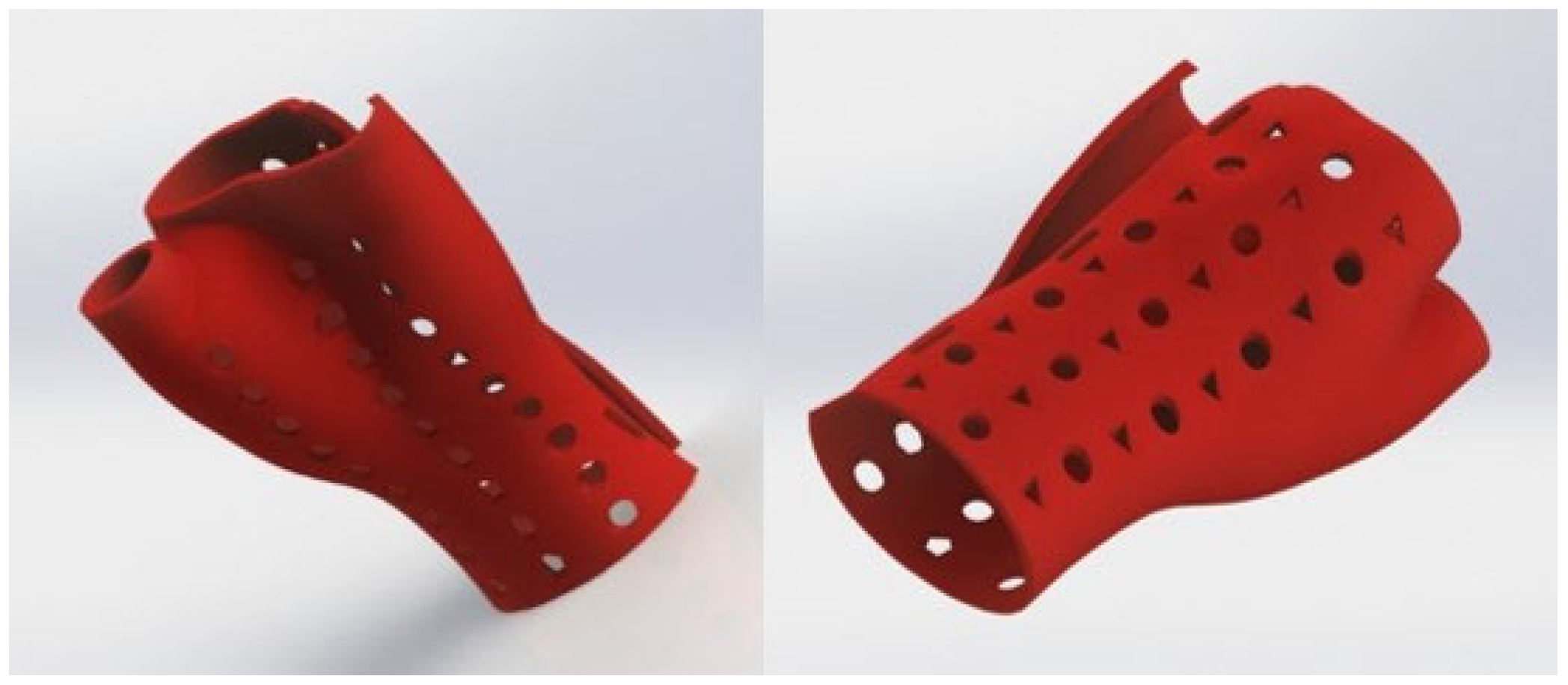
2.2. CAD Modeling of the Orthosis by Generative Algorithms
- ✓
- N is the number of adjacent vertices to node i;
- ✓
- is the position of the j-th adjacent vertex; and
- ✓
- is the new position for node i.
3. Orthosis Additive 3D Rapid Prototyping
- ✓
- the printing process avoids the presence of potentially dangerous residuals in medical environments;
- ✓
- the mechanical performances of the printed parts are generally compliant with the application requirements;
- ✓
- FDM printing by using ABS material has already been used for orthoses manufacturing and approved for medical applications [7].
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leite, M.; Soares, B.; Lopes, V.; Santos, S.; Silva, M.T. Design for personalized medicine in orthotics and prosthetics. Procedia CIRP 2019, 84, 457–461. [Google Scholar] [CrossRef]
- Ingrassia, T.; Nigrelli, V.; Ricotta, V.; Tartamella, C. Process parameters influence in additive manufacturing. In Advances on Mechanics, Design Engineering and Manufacturing; Lecture Notes in Mechanical Engineering; Springer International Publishing: Cham, Switzerland, 2017; pp. 261–270. [Google Scholar]
- Li, C.; Pisignano, D.; Zhao, Y.; Xue, J. Advances in Medical Applications of Additive Manufacturing. Engineering 2020, 6, 1222–1231. [Google Scholar] [CrossRef]
- Lal, H.; Patralekh, M.K. 3D printing and its applications in orthopaedic trauma: A technological marvel. J. Clin. Orthop. Trauma 2018, 9, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Sheoran, A.J.; Kumar, H.; Arora, P.K.; Moona, G. Bio-Medical applications of Additive Manufacturing: A Review. Procedia Manuf. 2020, 51, 663–670. [Google Scholar] [CrossRef]
- Halem, A.; Javaid, M. 3D printed medical parts with different materials using additive manufacturing. Clin. Epidemiol. Glob. Health 2020, 8, 215–223. [Google Scholar] [CrossRef]
- Buonamici, F.; Furferi, R.; Governi, L.; Lazzeri, S.; McGreevy, K.S.; Servi, M.; Talanti, E.; Uccheddu, F.; Volpe, Y. A CAD-based Procedure for Designing 3D Printable Arm-Wrist-Hand Cast. Comput.-Aided Des. Appl. 2019, 16, 25–34. [Google Scholar]
- Chen, R.K.; Jin, Y.; Wensman, J.; Shih, A. Additive manufacturing of custom orthoses and prostheses—A review. Addit. Manuf. 2016, 12, 77–89. [Google Scholar] [CrossRef]
- Paterson, A.M.; Bibb, R.; Campbell, R.I.; Bingham, G. Comparing additive manufacturing technologies for customized wrist splints. Rapid Prototyp. J. 2015, 21, 230–243. [Google Scholar] [CrossRef]
- Zhou, M.; Sun, C.; Naghavi, S.A.; Wang, L.; Tamaddon, M.; Wang, J.; Liu, C. The design. and manufacturing of a Patient-Specific wrist splint for rehabilitation of rheumatoid arthritis. Mater. Des. 2024, 238, 112704. [Google Scholar] [CrossRef]
- Fang, J.-J.; Lin, C.-L.; Tsai, J.-Y.; Lin, R.-M. Clinical Assessment of Customized 3D-PrintedWrist Orthoses. Appl. Sci. 2022, 12, 11538. [Google Scholar] [CrossRef]
- Patel, P.; Gohil, P. Custom orthotics development process based on additive manufacturing. Mater. Today Proc. 2022, 59, A52–A63. [Google Scholar] [CrossRef]
- Sabyrov, N.; Sotsial, Z.; Abilgaziyev, A.; Adair, D.; Ali, M.H. Design of a flexible neck orthosis on Fused Deposition Modeling printer for rehabilitation on regular usage. Procedia Comput. Sci. 2021, 179, 63–71. [Google Scholar] [CrossRef]
- Beyene Mamo, H.; Adamiak, M.; Kunwar, A. 3D printed biomedical devices and their applications: A review on state-of-the-art technologies, existing challenges, and future perspectives. J. Mech. Behav. Biomed. Mater. 2023, 143, 105930. [Google Scholar]
- Amaya-Rivas, J.L.; Perero, B.S.; Helguero, C.G.; Hurel, J.L.; Peralta, J.M.; Flores, F.A.; Alvarado, J.D. Future trends of additive manufacturing in medical applications: An overview. Heliyon 2024, 10, e26641. [Google Scholar] [CrossRef]
- Sala, F.; Carminati, M.; D’Urso, G.; Giardini, C. A feasibility analysis of a 3D customized upper limb orthosis. Procedia CIRP 2022, 110, 207–212. [Google Scholar] [CrossRef]
- Sala, F.; D’Urso, G.; Giardini, C. Customized Wrist Immobilization Splints Produced via Additive Manufacturing—A Comprehensive Evaluation of the Viable Configurations. Prosthesis 2023, 5, 792–808. [Google Scholar] [CrossRef]
- Mirulla, A.I.; Marcheggiani Muccioli, G.M.; Fratini, S.; Zaffagnini, S.; Ingrassia, T.; Bragonzoni, L.; Innocenti, B. Analysis of different geometrical features to achieve close-to-bone stiffness material properties in medical device: A feasibility numerical study. Comput. Methods Programs Biomed. 2022, 221, 106875. [Google Scholar] [CrossRef] [PubMed]
- Ricotta, V.; Campbell, R.; Ingrassia, T.; Nigrelli, V. Additively manufactured textiles and parametric modelling by generative algorithms in orthopaedic applications. Rapid Prototyp. J. 2020, 26, 827–834. [Google Scholar] [CrossRef]
- Palousek, D.; Rosicky, J.; Koutny, D.; Stoklásek, P.; Navrat, T. Pilot study of the wrist orthosis design process. Rapid Prototyp. J. 2014, 20, 27–32. [Google Scholar] [CrossRef]
- Kim, H.; Jeong, S. Case study: Hybrid model for the customized wrist orthosis using 3D printing. J. Mech. Sci. Technol. 2015, 29, 5151–5156. [Google Scholar] [CrossRef]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Żukowska, M.; Lulkiewicz, M.; Zawadzki, P. Experimental Studies on 3D Printing of Automatically Designed Customized Wrist-Hand Orthoses. Materials 2020, 13, 4091. [Google Scholar] [CrossRef] [PubMed]
- Buonamici, F.; Furferi, R.; Governi, L.; Lazzeri, S.; McGreevy, K.S.; Servi, M.; Talanti, E.; Uccheddu, F.; Volpe, Y. A practical methodology for computer-aided design of custom 3D printable casts for wrist fractures. Vis. Comput. 2020, 36, 375–390. [Google Scholar] [CrossRef]
- Fernandez-Vicente, M.; Escario Chust, A.; Conejero, A. Low cost digital fabrication approach for thumb orthoses. Rapid Prototyp. J. 2017, 23, 1020–1031. [Google Scholar] [CrossRef]
- Ingrassia, T.; Nigrelli, V.; Pecorella, D.; Bragonzoni, L.; Ricotta, V. Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach. Appl. Sci. 2020, 10, 4941. [Google Scholar] [CrossRef]
- Bikas, H.; Stavropoulos, P.; Chryssolouris, G. Additive manufacturing methods and modelling approaches: A critical review. Int. J. Adv. Manuf. Technol. 2016, 83, 389–405. [Google Scholar] [CrossRef]
- Huang, S.H.; Liu, P.; Mokasdar, A.; Hou, L. Additive manufacturing and its societal impact: A literature review. Int. J. Adv. Manuf. Technol. 2013, 67, 1191–1203. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, Y.; Ramanujan, D.; Ramania, K.; Chen, Y.; Williams, C.B.; Wang, C.C.L.; Shin, Y.C.; Zhang, S.; Zavattieri, P.D. The status, challenges, and future of additive manufacturing in engineering. Comput.-Aided Des. 2015, 69, 65–89. [Google Scholar] [CrossRef]
- Ingrassia, T.; Lombardo, B.; Nigrelli, V.; Ricotta, V.; Nalbone, L.; D’Arienzo, A.; D’Arienzo, M.; Porcellini, G. Influence of sutures configuration on the strength of tendon-patch joints for rotator cuff tears treatment. Injury 2019, 50, S18–S23. [Google Scholar] [CrossRef]
- Campbell, R.I.; Ingrassia, T.; Nigrelli, V.; Ricotta, V. New customized elbow orthosis made by additive manufacturing. In Advances on Mechanics, Design Engineering and Manufacturing II; Lecture Notes in Mechanical Engineering (LNME); Springer International Publishing: Cham, Switzerland, 2019; pp. 473–483. [Google Scholar]
- Mirulla, A.I.; Bragonzoni, L.; Zaffagnini, S.; Ingrassia, T.; Zinno, R. Assessment of paradoxical anterior translation in a CR total knee prosthesis coupling dynamic RSA and FE techniques. J. Exp. Ortop. 2021, 8, 50. [Google Scholar] [CrossRef]
- Cirello, A.; Ingrassia, T.; Mancuso, A.; Nigrelli, V.; Tumino, D. Improving the downwind sail design process by means of a novel FSI approach. J. Mar. Sci. Eng. 2021, 9, 624. [Google Scholar] [CrossRef]
- Dal Maso, A.; Cosmi, F. 3D-printed ankle-foot orthosis: A design method. Mater. Today Proc. 2019, 12, 252–261. [Google Scholar] [CrossRef]
- Munhoz, R.; Da Costa Moraes, C.A.; Tanaka, H.; Kunkel, M.E. A digital approach for design and fabrication by rapid prototyping of orthosis for developmental dysplasia of the hip. Res. Biomed. Eng. 2016, 32, 63–73. [Google Scholar] [CrossRef]
- Silva, R.; Silva, B.; Fernandes, C.; Morouco, P.; Alves, N.; Veloso, A. A Review on 3D Scanners Studies for Producing Customized Orthoses. Sensors 2024, 24, 1373. [Google Scholar] [CrossRef] [PubMed]
- Brognara, L.; Fantini, M.; Morellato, K.; Graziani, G.; Baldini, N.; Cauli, O. Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials 2022, 15, 4064. [Google Scholar] [CrossRef] [PubMed]
- Fantini, M.; De Crescenzio, F.; Brognara, L.; Baldini, N. Design and Rapid Manufacturing of a customized foot orthosis: A first methodological study. In Advances on Mechanics, Design Engineering and Manufacturing; Lecture Notes in Mechanical Engineering; Springer International Publishing: Cham, Switzerland, 2017; pp. 457–467. [Google Scholar]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirello, A.; Ingrassia, T.; Marannano, G.; Mirulla, A.I.; Nigrelli, V.; Petrucci, G.; Ricotta, V. A New Automatic Process Based on Generative Design for CAD Modeling and Manufacturing of Customized Orthosis. Appl. Sci. 2024, 14, 6231. https://doi.org/10.3390/app14146231
Cirello A, Ingrassia T, Marannano G, Mirulla AI, Nigrelli V, Petrucci G, Ricotta V. A New Automatic Process Based on Generative Design for CAD Modeling and Manufacturing of Customized Orthosis. Applied Sciences. 2024; 14(14):6231. https://doi.org/10.3390/app14146231
Chicago/Turabian StyleCirello, Antonino, Tommaso Ingrassia, Giuseppe Marannano, Agostino Igor Mirulla, Vincenzo Nigrelli, Giovanni Petrucci, and Vito Ricotta. 2024. "A New Automatic Process Based on Generative Design for CAD Modeling and Manufacturing of Customized Orthosis" Applied Sciences 14, no. 14: 6231. https://doi.org/10.3390/app14146231
APA StyleCirello, A., Ingrassia, T., Marannano, G., Mirulla, A. I., Nigrelli, V., Petrucci, G., & Ricotta, V. (2024). A New Automatic Process Based on Generative Design for CAD Modeling and Manufacturing of Customized Orthosis. Applied Sciences, 14(14), 6231. https://doi.org/10.3390/app14146231










