Fit Accuracy of Cobalt–Chromium and Polyether Ether Ketone Prosthetic Frameworks Produced Using Digital Techniques: In Vitro Pilot Study
Abstract
1. Introduction
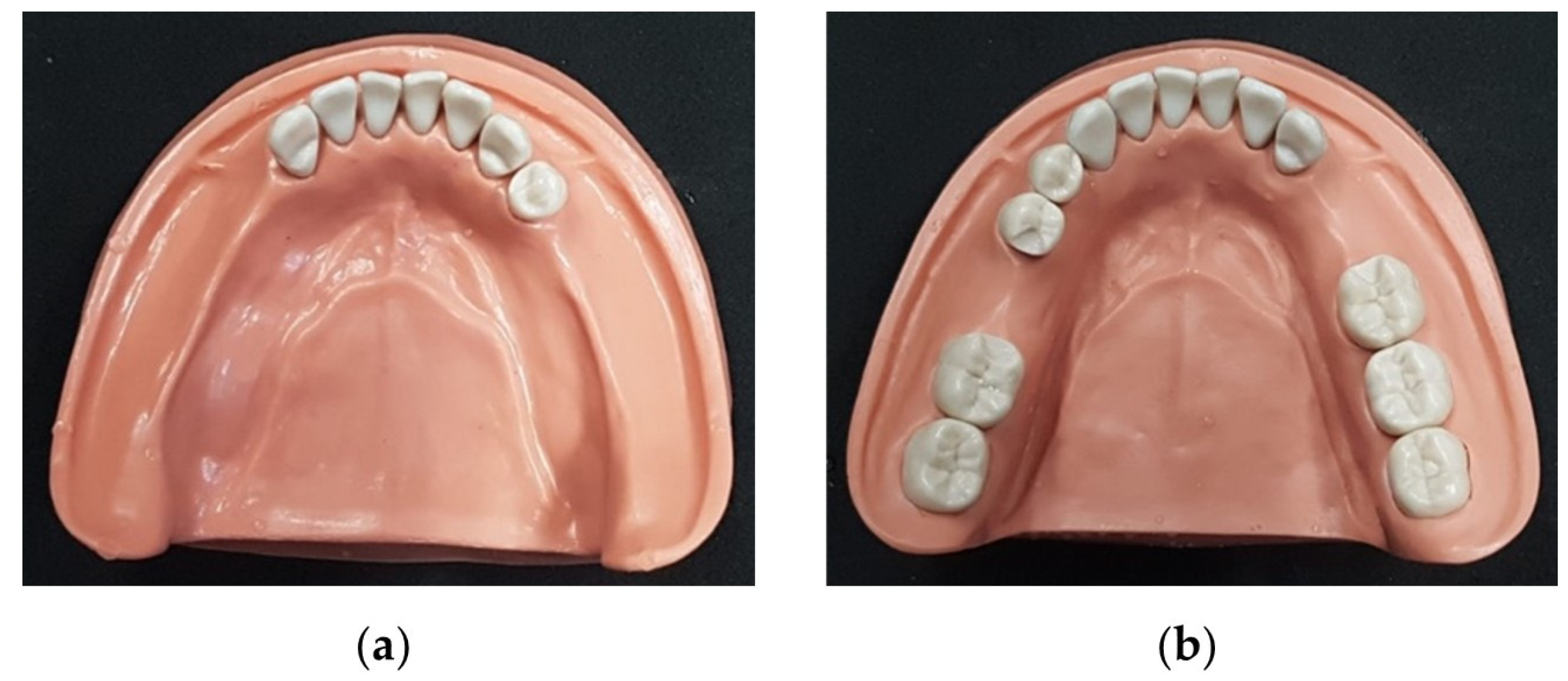
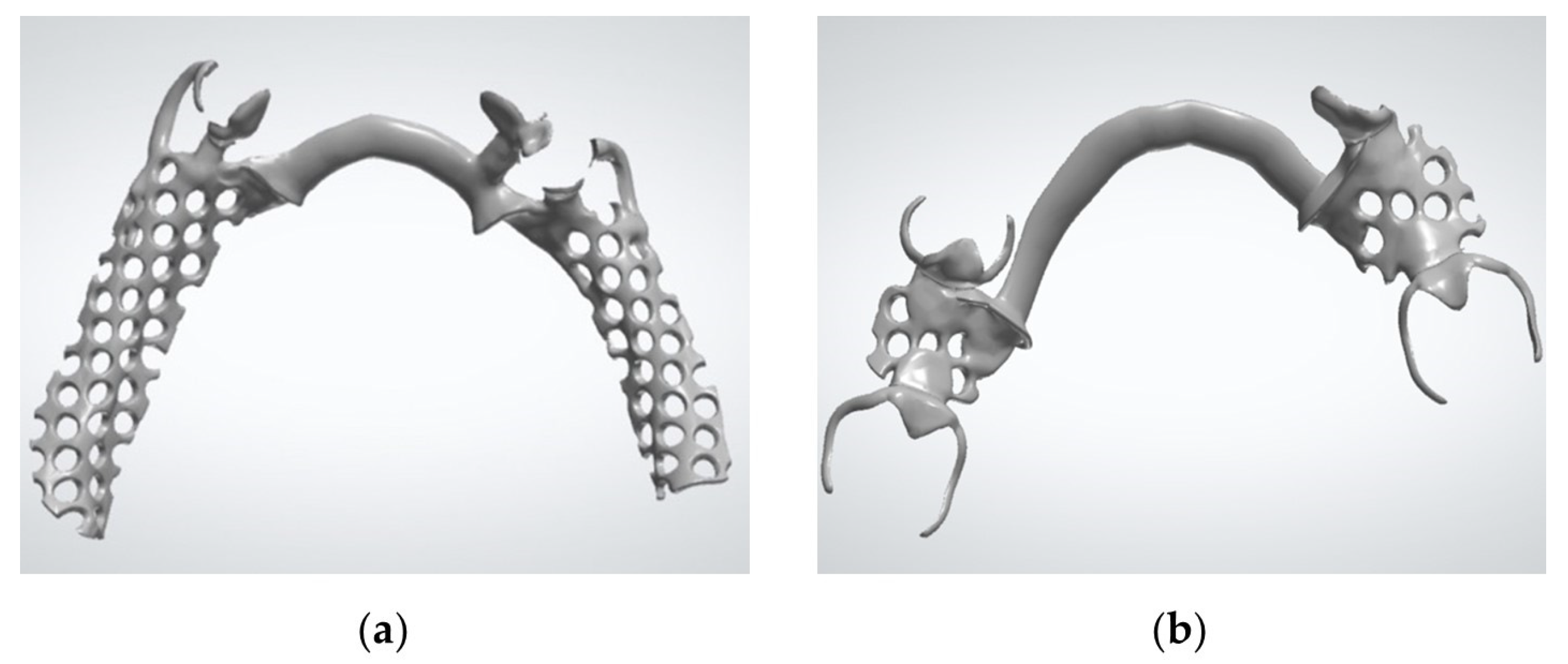
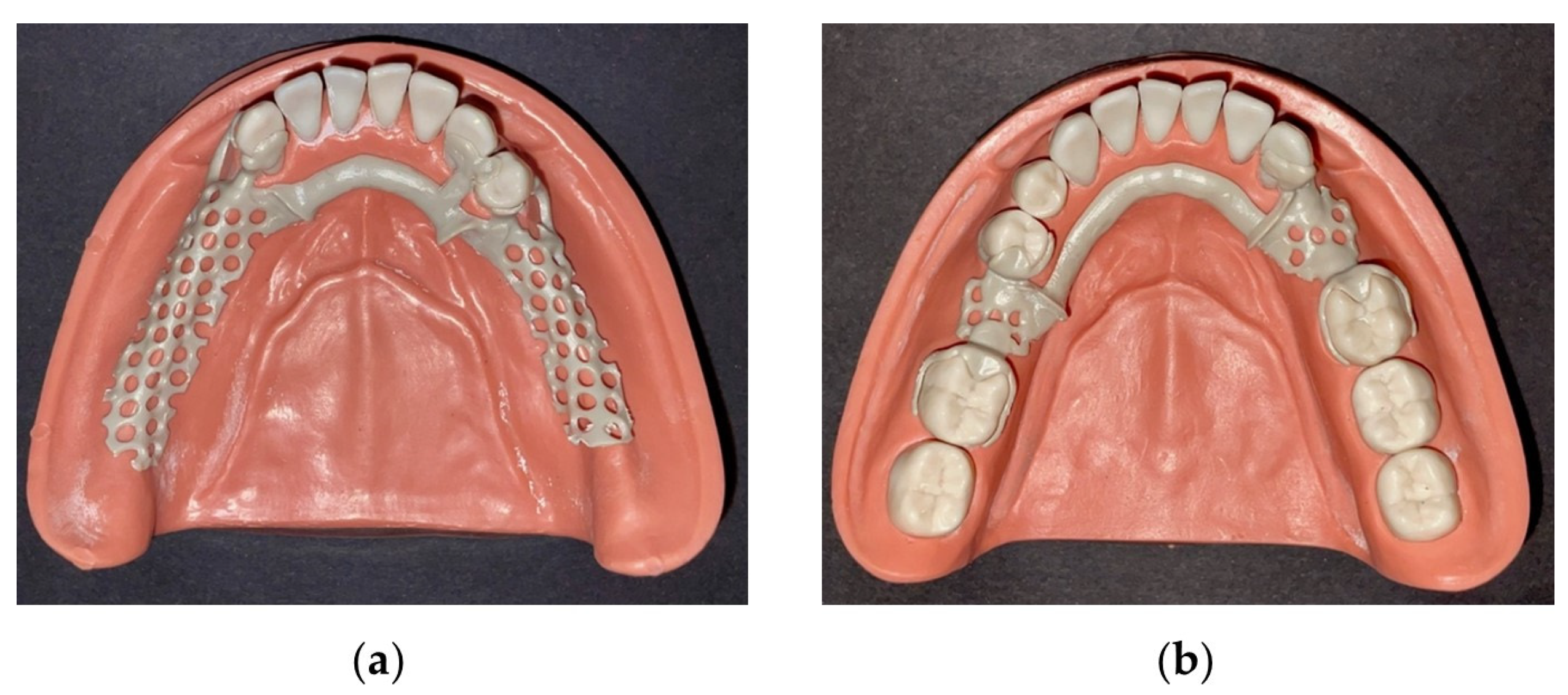
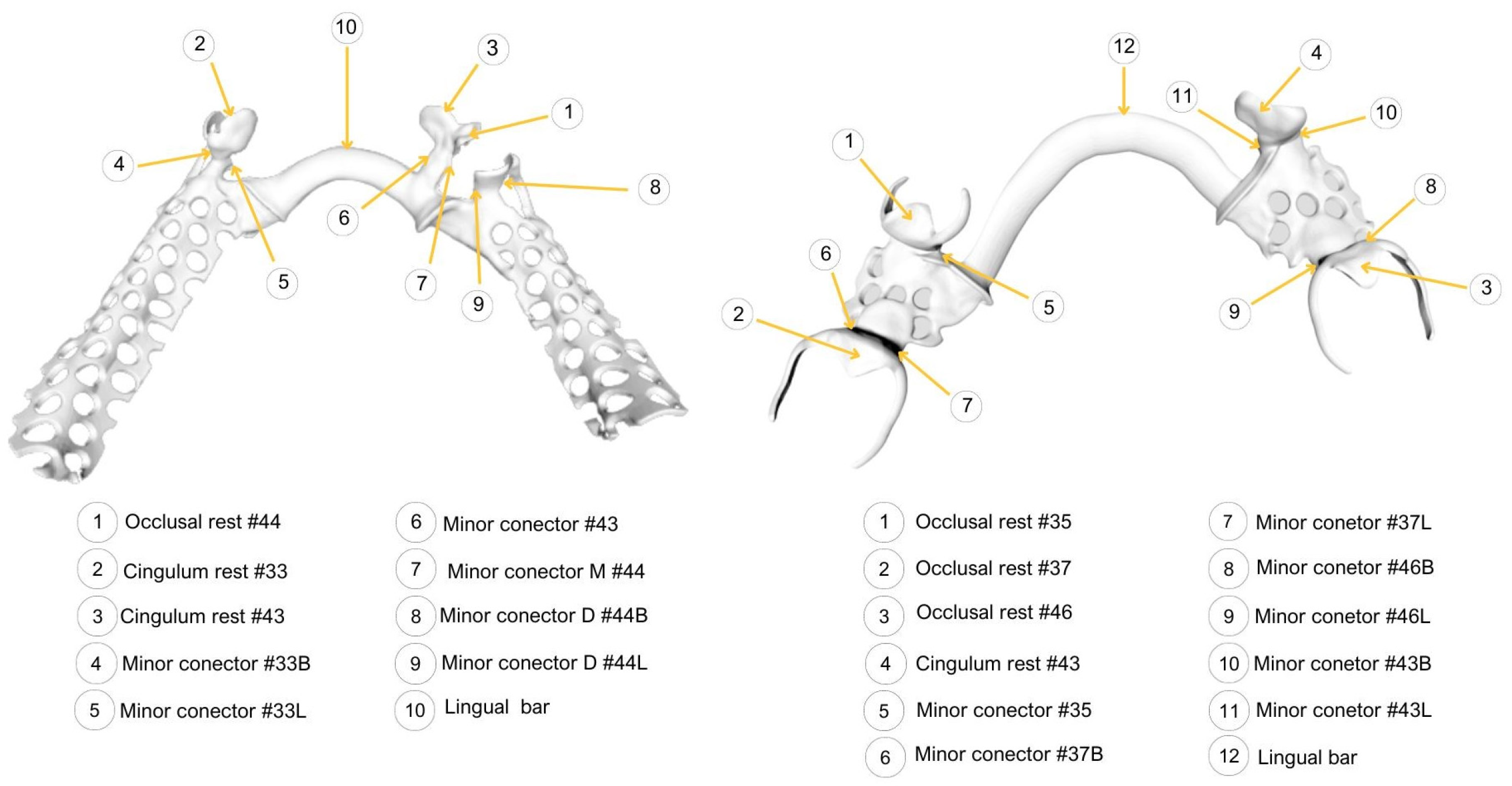
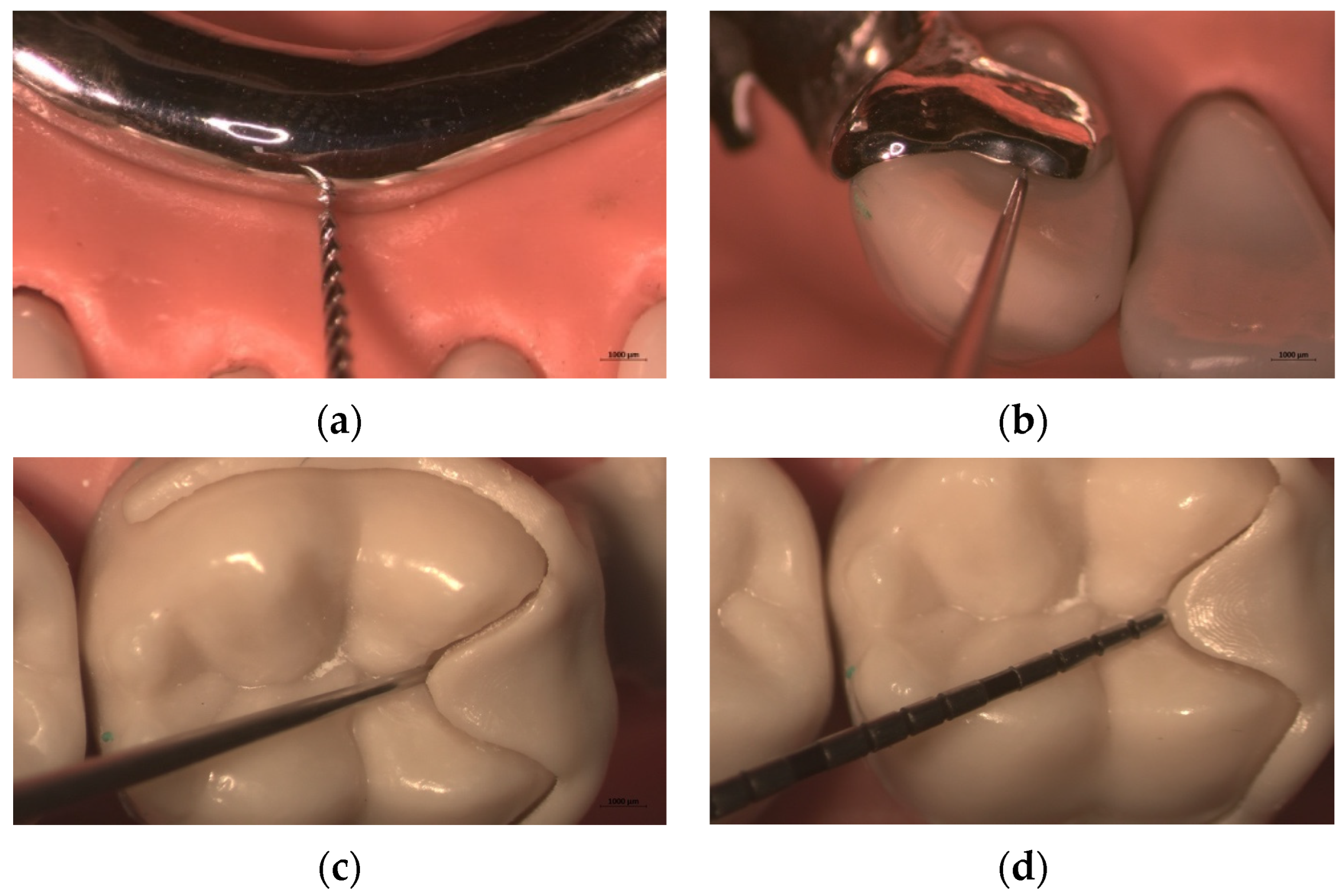
2. Materials and Methods
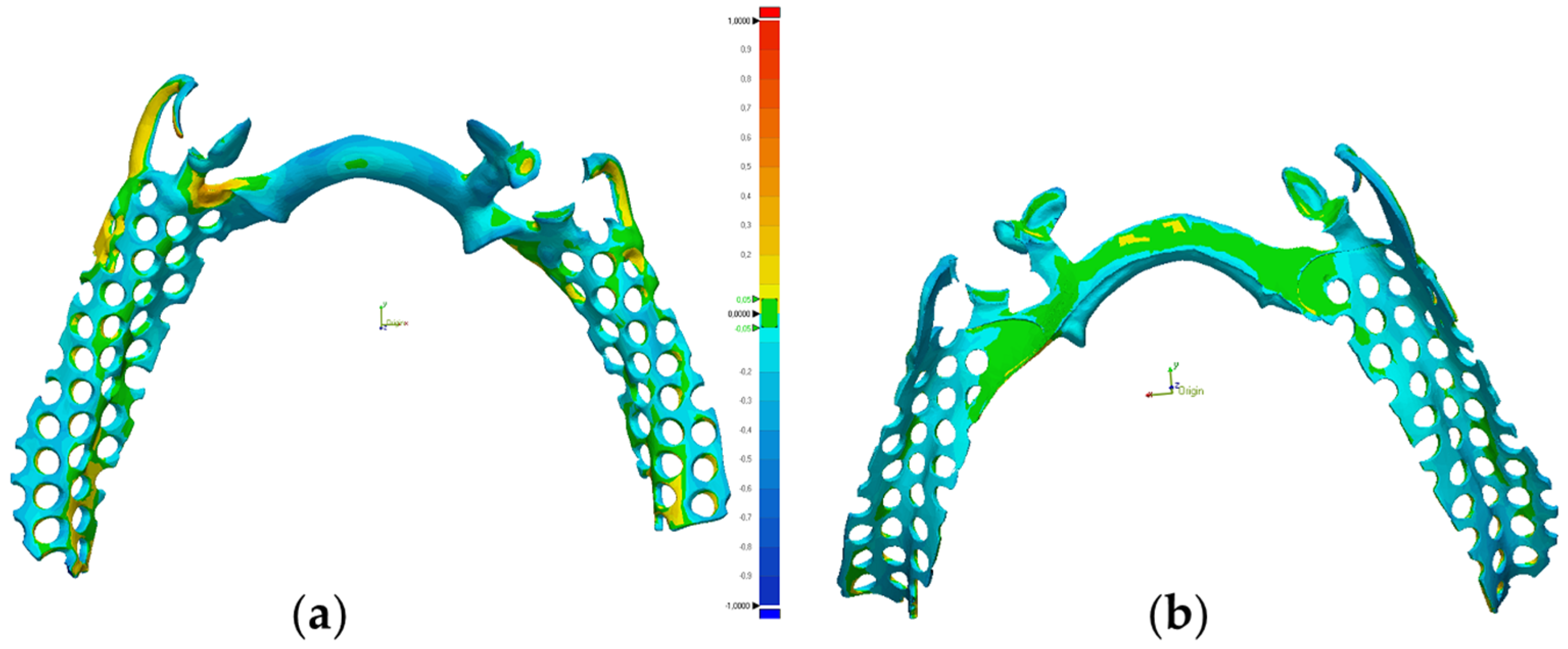
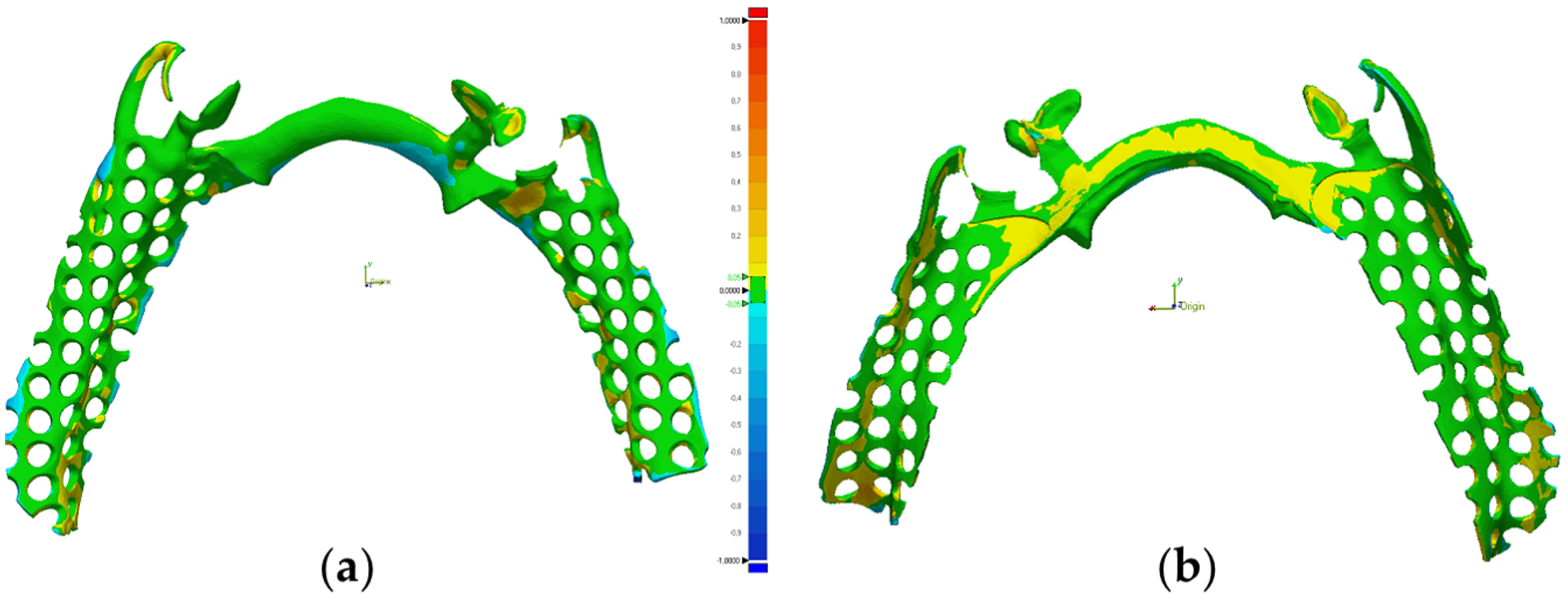
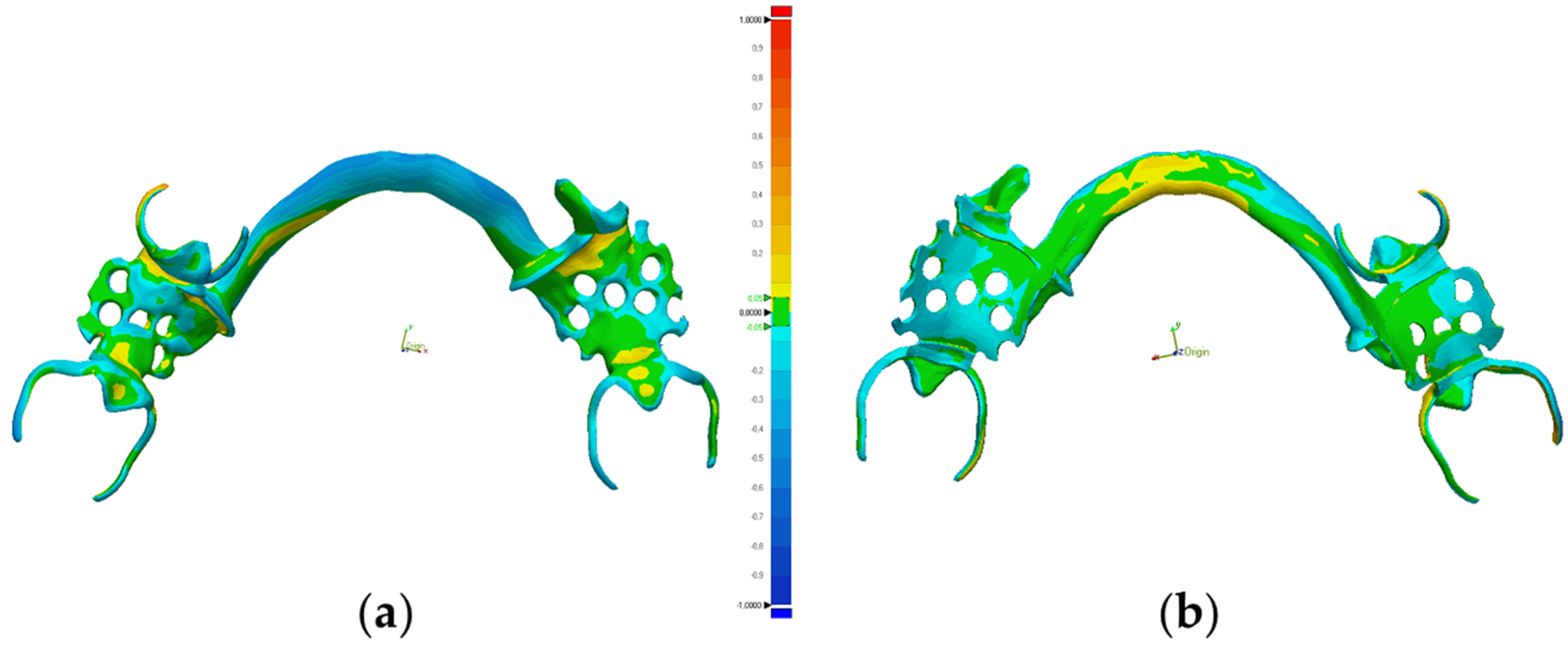
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, W.T.; Chen, Y.C. Digitally Fabricated Dentures for Full Mouth Rehabilitation with Zirconia, Polyetheretherketone and Selective Laser Melted Ti-6Al-4V Material. Int. J. Environ. Res. Public Health 2022, 19, 3021. [Google Scholar] [CrossRef] [PubMed]
- Peng, P.W.; Hsu, C.Y.; Huang, H.Y.; Chao, J.C.; Lee, W.F. Trueness of removable partial denture frameworks additively manufactured with selective laser melting. J. Prosthet. Dent. 2022, 127, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Bajunaid, S.O.; Altwaim, B.; Alhassan, M.; Alammari, R. The Fit Accuracy of Removable Partial Denture Metal Frameworks Using Conventional and 3D Printed Techniques: An In Vitro Study. J. Contemp. Dent. Pract. 2019, 20, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Almufleh, B.; Emami, E.; Alageel, O.; de Melo, F.; Seng, F.; Caron, E.; Nader, S.A.; Al-Hashedi, A.; Albuquerque, R.; Feine, J.; et al. Patient satisfaction with laser-sintered removable partial dentures: A crossover pilot clinical trial. J. Prosthet. Dent. 2018, 119, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Tregerman, I.; Renne, W.; Kelly, A.; Wilson, D. Evaluation of removable partial denture frameworks fabricated using 3 different techniques. J. Prosthet. Dent. 2019, 122, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J. Revisiting the Removable Partial Denture. Dent. Clin. N. Am. 2019, 63, 263–278. [Google Scholar] [CrossRef] [PubMed]
- Soltanzadeh, P.; Suprono, M.S.; Kattadiyil, M.T.; Goodacre, C.; Gregorius, W. An In Vitro Investigation of Accuracy and Fit of Conventional and CAD/CAM Removable Partial Denture Frameworks. J. Prosthodont. 2019, 28, 547–555. [Google Scholar] [CrossRef]
- Schweiger, J.; Güth, J.F.; Erdelt, K.J.; Edelhoff, D.; Schubert, O. Internal porosities, retentive force, and survival of cobalt-chromium alloy clasps fabricated by selective laser-sintering. J. Prosthodont. Res. 2020, 64, 210–216. [Google Scholar] [CrossRef]
- Anes, V.; Neves, C.B.; Bostan, V.; Gonçalves, S.; Reis, L. Evaluation of the retentive forces from removable partial denture clasps manufactured by the digital method. Appl. Sci. 2023, 13, 8072. [Google Scholar] [CrossRef]
- Lee, S.J.; Kim, S.W.; Lee, J.J.; Cheong, C.W. Comparison of Intraoral and Extraoral Digital Scanners: Evaluation of Surface Topography and Precision. Dent. J. 2020, 8, 52. [Google Scholar] [CrossRef]
- Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-fabricated removable partial dentures. J. Prosthet. Dent. 2018, 119, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Barraclough, O.; Gray, D.; Ali, Z.; Nattress, B. Modern partial dentures—Part 1: Novel manufacturing techniques. Br. Dent. J. 2021, 230, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Rokaya, D.; Bohara, S.; Srimaneepong, V.; Kongkiatkamon, S.; Khurshid, Z.; Heboyan, A.; Zafar, M.S.; Sapkota, J. Metallic Biomaterials for Medical and Dental Prosthetic Applications. In Functional Biomaterials; Jana, S., Jana, S., Eds.; Springer: Singapore, 2022; pp. 503–522. [Google Scholar]
- Cevik, P.; Schimmel, M.; Yilmaz, B. New generation CAD-CAM materials for implant-supported definitive frameworks fabricated by using subtractive technologies. BioMed Res. Int. 2022, 2022, 3074182. [Google Scholar] [CrossRef] [PubMed]
- Tasaka, A.; Shimizu, T.; Kato, Y.; Okano, H.; Ida, Y.; Yamashita, S. Accuracy of removable partial denture framework fabricated by casting with a 3D printed pattern and selective laser sintering. J. Prosthodont. Res. 2020, 64, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Conceição, P.; Portugal, J.; Neves, C.B. Evaluation of Removable Partial Denture Metal Frameworks Produced by Digital Methods—A Systematic Review. Appl. Sci. 2023, 13, 10824. [Google Scholar] [CrossRef]
- Alabdullah, S.A.; Hannam, A.G.; Wyatt, C.C.; McCullagh, A.P.G.; Aleksejuniene, J.; Mostafa, N.Z. Comparison of digital and conventional methods of fit evaluation of partial removable dental prosthesis frameworks fabricated by selective laser melting. J. Prosthet. Dent. 2022, 127, 478.e1–478.e10. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.F.; Wang, J.C.; Hsu, C.Y.; Peng, P.W. Microstructure, mechanical properties, and retentive forces of cobalt-chromium removable partial denture frameworks fabricated by selective laser melting followed by heat treatment. J. Prosthet. Dent. 2022, 127, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Dikova, T. Chapter 5: Properties of Co-Cr Dental Alloys Fabricated Using Additive Technologies. In Biomaterials in Regenerative Medicine; Dobrzański, L.A., Ed.; InTechOpen: London, UK, 2018; pp. 141–159. [Google Scholar]
- Campbell, S.D.; Cooper, L.; Craddock, H.; Hyde, T.P.; Nattress, B.; Pavitt, S.H.; Seymour, D.W. Removable partial dentures: The clinical need for innovation. J. Prosthet. Dent. 2017, 118, 273–280. [Google Scholar] [CrossRef]
- Negm, E.E.; Aboutaleb, F.A.; Alam-Eldein, A.M. Virtual Evaluation of the Accuracy of Fit and Trueness in Maxillary Poly(etheretherketone) Removable Partial Denture Frameworks Fabricated by Direct and Indirect CAD/CAM Techniques. J. Prosthodont. 2019, 28, 804–810. [Google Scholar] [CrossRef]
- Gentz, F.I.; Brooks, D.I.; Liacouras, P.C.; Petrich, A.; Hamlin, C.M.; Ellert, D.O.; Ye, L. Retentive Forces of Removable Partial Denture Clasp Assemblies Made from Polyaryletherketone and Cobalt-Chromium: A Comparative Study. J. Prosthodont. 2022, 31, 299–304. [Google Scholar] [CrossRef]
- Harb, I.E.; Abdel-Khalek, E.A.; Hegazy, S.A. CAD/CAM Constructed Poly(etheretherketone) (PEEK) Framework of Kennedy Class I Removable Partial Denture: A Clinical Report. J. Prosthodont. 2019, 28, e595–e598. [Google Scholar] [CrossRef] [PubMed]
- Mayinger, F.; Micovic, D.; Schleich, A.; Roos, M.; Eichberger, M.; Stawarczyk, B. Retention force of polyetheretherketone and cobalt-chrome-molybdenum removable dental prosthesis clasps after artificial aging. Clin. Oral Investig. 2021, 25, 3141–3149. [Google Scholar] [CrossRef] [PubMed]
- Zoidis, P.; Papathanasiou, I.; Polyzois, G. The Use of a Modified Poly-Ether-Ether-Ketone (PEEK) as an Alternative Framework Material for Removable Dental Prostheses. A Clinical Report. J. Prosthodont. 2016, 25, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Vaicelyte, A.; Janssen, C.; Le Borgne, M.; Grosgogeat, B. Cobalt–Chromium Dental Alloys: Metal Exposures, Toxicological Risks, CMR Classification, and EU Regulatory Framework. Crystals 2020, 10, 1151. [Google Scholar] [CrossRef]
- Suphangul, S.; Rokaya, D.; Kanchanasobhana, C.; Rungsiyakull, P.; Chaijareenont, P. PEEK Biomaterial in Long-Term Provisional Implant Restorations: A Review. J. Funct. Biomater. 2022, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj Husain, N.; Özcan, M.; Schimmel, M.; Abou-Ayash, S. A digital cast-free clinical workflow for oral rehabilitation with removable partial dentures: A dental technique. J. Prosthet. Dent. 2020, 123, 680–685. [Google Scholar] [CrossRef]
- Oh, K.C.; Yun, B.S.; Kim, J.H. Accuracy of metal 3D printed frameworks for removable partial dentures evaluated by digital superimposition. Dent. Mater. 2022, 38, 309–317. [Google Scholar] [CrossRef]
- Eggbeer, D.; Bibb, R.; Williams, R. The computer-aided design and rapid prototyping fabrication of removable partial denture frameworks. Proc. Inst. Mech. Eng. Part H 2005, 219, 195–202. [Google Scholar] [CrossRef]
- Ye, H.; Ning, J.; Li, M.; Niu, L.; Yang, J.; Sun, Y.; Zhou, Y. Preliminary Clinical Application of Removable Partial Denture Frameworks Fabricated Using Computer-Aided Design and Rapid Prototyping Techniques. Int. J. Prosthodont. 2017, 30, 348–353. [Google Scholar] [CrossRef]
- Keltjens, H.M.; Mulder, J.; Käyser, A.F.; Creugers, N.H. Fit of direct retainers in 9 partial dentures after 8 years of use. J. Oral Rehabil. 1997, 24, 138–142. [Google Scholar] [CrossRef]
- Saad, A.; Abbas, F.; Elgharabawy, S. Clinical evaluation of removable partial denture constructed from 3d printed resin pattern designed using CAD CAM technology. Alex. Dent. J. 2019, 44, 15–21. [Google Scholar] [CrossRef]
- Tasaka, A.; Okano, H.; Shimizu, T.; Kato, Y.; Higuchi, S.; Yamashita, S. Influence of reinforcement bar on accuracy of removable partial denture framework fabricated by casting with a 3D-printed pattern and selective laser sintering. J. Prosthodont. Res. 2021, 65, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Conceição, P.; Franco, M.; Alves, N.; Portugal, J.; Neves, C.B. Fit accuracy of removable partial denture metal frameworks produced by CAD-CAM—A clinical study. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2021, 62, 194–200. [Google Scholar] [CrossRef]
- Guo, F.; Huang, S.; Liu, N.; Hu, M.; Shi, C.; Li, D.; Liu, C. Evaluation of the mechanical properties and fit of 3D-printed polyetheretherketone removable partial dentures. Dent. Mater. J. 2022, 41, 816–823. [Google Scholar] [CrossRef]
- Ye, H.; Li, X.; Wang, G.; Kang, J.; Liu, Y.; Sun, Y.; Zhou, Y. A Novel Computer-Aided Design/Computer- Assisted Manufacture Method for One-Piece Removable Partial Denture and Evaluation of Fit. Int. J. Prosthodont. 2018, 31, 149–151. [Google Scholar] [CrossRef]
- Mohamed, S.; Rasha, H. Digital PEEK framework and patient satisfaction compared to conventional metal framework in removable partial dentures. A clinical trial. Egypt. Dent. J. 2019, 65, 3787–3794. [Google Scholar] [CrossRef][Green Version]
- Conceição, P.; Portugal, J.; Franco, M.; Alves, N.M.; Marques, D.; Neves, C.B. Comparison between digital superimposition and microcomputed tomography methods of fit assessment of removable partial denture frameworks. J. Prosthet. Dent. 2023, in press. [Google Scholar] [CrossRef]
- Lee, J.W.; Park, J.M.; Park, E.J.; Heo, S.J.; Koak, J.Y.; Kim, S.K. Accuracy of a digital removable partial denture fabricated by casting a rapid prototyped pattern: A clinical study. J. Prosthet. Dent. 2017, 118, 468–474. [Google Scholar] [CrossRef]
- ISO 5725-1:2023; Accuracy (Trueness and Precision) of Measurement Methods and Results—Part 1: General Principles and Definitions. International Standard Organization: Geneva, Switzerland, 2023.
- Sampaio-Fernandes, M.A.; Pinto, R.; Sampaio-Fernandes, M.M.; Sampaio-Fernandes, J.C.; Marques, D.; Figueiral, M.H. Accuracy of silicone impressions and stone models using two laboratory scanners: A 3D evaluation. Int. J. Prosthodont. 2022. ahead of print. [Google Scholar] [CrossRef]
- Snosi, A.M.; Lotfy, S.M.; Thabet, Y.G.; Sabet, M.E.; Rizk, F.N. Subtractive versus additive indirect manufacturing techniques of digitally designed partial dentures. J. Adv. Prosthodont. 2021, 13, 327–332. [Google Scholar] [CrossRef]
- Yilmaz, B.; Marques, V.R.; Donmez, M.B.; Cuellar, A.R.; Lu, W.E.; Abou-Ayash, S.; Çakmak, G. Influence of 3D analysis software on measured deviations of CAD-CAM resin crowns from virtual design file: An in-vitro study. J. Dent. 2022, 118, 103933. [Google Scholar] [CrossRef] [PubMed]

| Kennedy Class I | Co-Cr Framework | PEEK Framework | ||
|---|---|---|---|---|
| Loupes | Microscope | Loupes | Microscope | |
| Occlusal rest #44 | A | A | A | A |
| Cingulum rest #33 | A | A | A | A |
| Cingulum rest #43 | A | A | A | A |
| Minor connector #33B | MF | MF | A | A |
| Minor connector #33L | A | A | A | A |
| Minor connector #43 | A | A | A | A |
| Minor connector M #44 | A | A | A | A |
| Minor connector D #44B | A | A | A | A |
| Minor connector D #44L | A | A | A | A |
| Lingual bar | A | A | A | A |
| Kennedy Class III, Modification 1 | Co-Cr Framework | PEEK Framework | ||
|---|---|---|---|---|
| Loupes | Microscope | Loupes | Microscope | |
| Occlusal rest #35 | A | A | A | A |
| Occlusal rest #37 | MF | MF | A | A |
| Occlusal rest #46 | MF | MF | MF | MF |
| Occlusal rest #43 | A | A | A | A |
| Minor connector #35 | A | A | A | A |
| Minor connector #37B | A | A | A | A |
| Minor connector #37L | MF | MF | MF | MF |
| Minor connector #46B | MF | MF | MF | MF |
| Minor connector #46L | A | A | A | A |
| Minor connector #43B | A | A | A | A |
| Minor connector #43L | A | A | A | A |
| Lingual bar | A | A | A | A |
| Kennedy Class I | Co-Cr Framework | |
|---|---|---|
| Loupes | Microscope | |
| Minor connector #33B | MF′ | MF′ |
| Kennedy Class III, Modification 1 | Co-Cr Framework | PEEK Framework | ||
|---|---|---|---|---|
| Loupes | Microscope | Loupes | Microscope | |
| Occlusal rest #37 | MF′ | MF′ | - | - |
| Occlusal rest #46 | MF′ | MF′ | MF′ | MF′ |
| Minor connector #37L | MF′ | MF′ | MF′ | MF′ |
| Minor connector #46B | MF′ | MF′ | MF′ | MF′ |
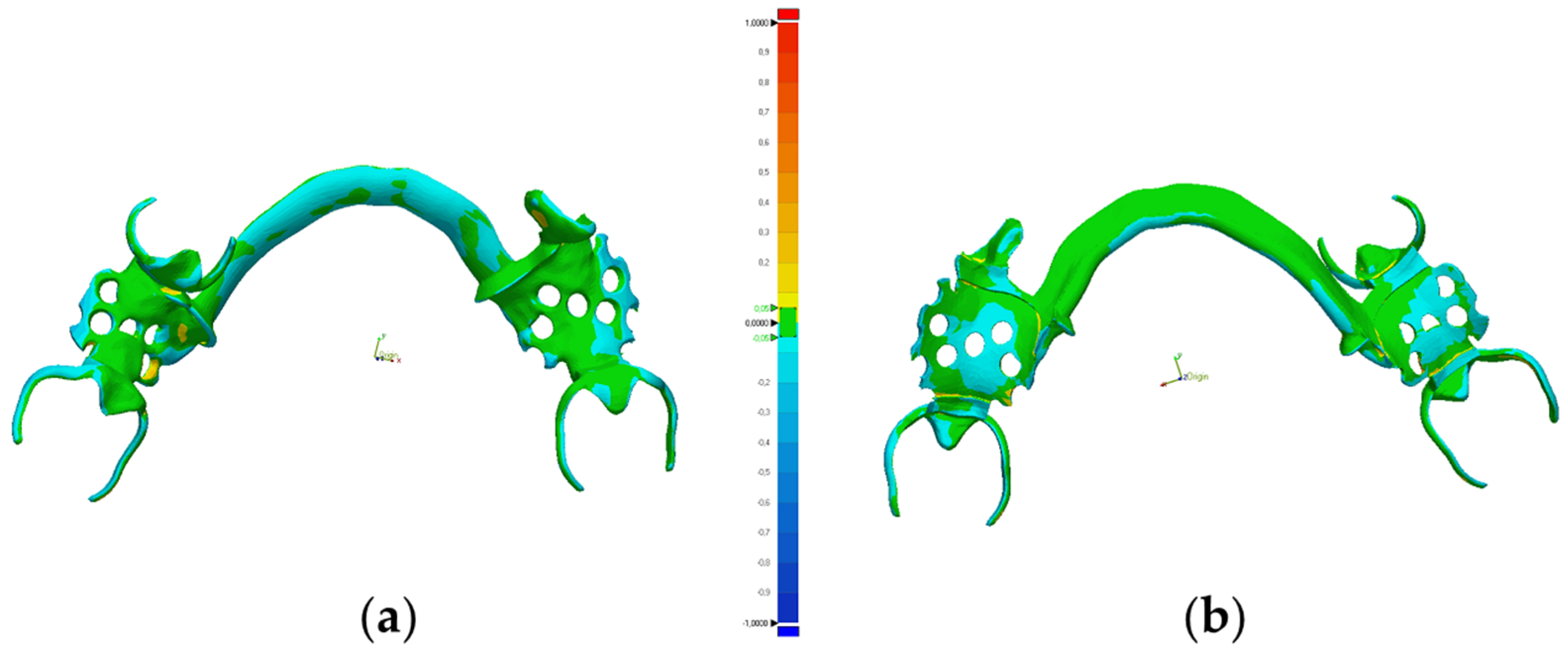
| Co-Cr Framework | PEEK Framework | |
|---|---|---|
| Maximum | 594.5 | 430.1 |
| Minimum | −594.8 | −430.1 |
| Mean | −73.3 | 25.4 |
| Standard Deviation | 128.9 | 64.4 |
| Root Mean Square (RMS) | 148.3 | 69.2 |
| Co-Cr Framework | PEEK Framework | |
|---|---|---|
| Maximum | 454.4 | 302.1 |
| Minimum | −455.4 | −300.9 |
| Mean | −33.3 | −26.9 |
| Standard Deviation | 101.9 | 53.2 |
| Root Mean Square (RMS) | 107.2 | 59.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbosa, L.; Figueiral, M.H.; Neves, C.B.; Malheiro, R.; Sampaio-Fernandes, M.A.; Oliveira, S.J.; Sampaio-Fernandes, M.M. Fit Accuracy of Cobalt–Chromium and Polyether Ether Ketone Prosthetic Frameworks Produced Using Digital Techniques: In Vitro Pilot Study. Appl. Sci. 2024, 14, 118. https://doi.org/10.3390/app14010118
Barbosa L, Figueiral MH, Neves CB, Malheiro R, Sampaio-Fernandes MA, Oliveira SJ, Sampaio-Fernandes MM. Fit Accuracy of Cobalt–Chromium and Polyether Ether Ketone Prosthetic Frameworks Produced Using Digital Techniques: In Vitro Pilot Study. Applied Sciences. 2024; 14(1):118. https://doi.org/10.3390/app14010118
Chicago/Turabian StyleBarbosa, Lara, Maria Helena Figueiral, Cristina Bettencourt Neves, Rodrigo Malheiro, Manuel António Sampaio-Fernandes, Susana João Oliveira, and Maria Margarida Sampaio-Fernandes. 2024. "Fit Accuracy of Cobalt–Chromium and Polyether Ether Ketone Prosthetic Frameworks Produced Using Digital Techniques: In Vitro Pilot Study" Applied Sciences 14, no. 1: 118. https://doi.org/10.3390/app14010118
APA StyleBarbosa, L., Figueiral, M. H., Neves, C. B., Malheiro, R., Sampaio-Fernandes, M. A., Oliveira, S. J., & Sampaio-Fernandes, M. M. (2024). Fit Accuracy of Cobalt–Chromium and Polyether Ether Ketone Prosthetic Frameworks Produced Using Digital Techniques: In Vitro Pilot Study. Applied Sciences, 14(1), 118. https://doi.org/10.3390/app14010118






