“Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image
Abstract
:1. Introduction
2. Methods
2.1. Procedures
2.2. Body-Scanning System
2.3. Graphic Processing of 3D Scans
3. Results
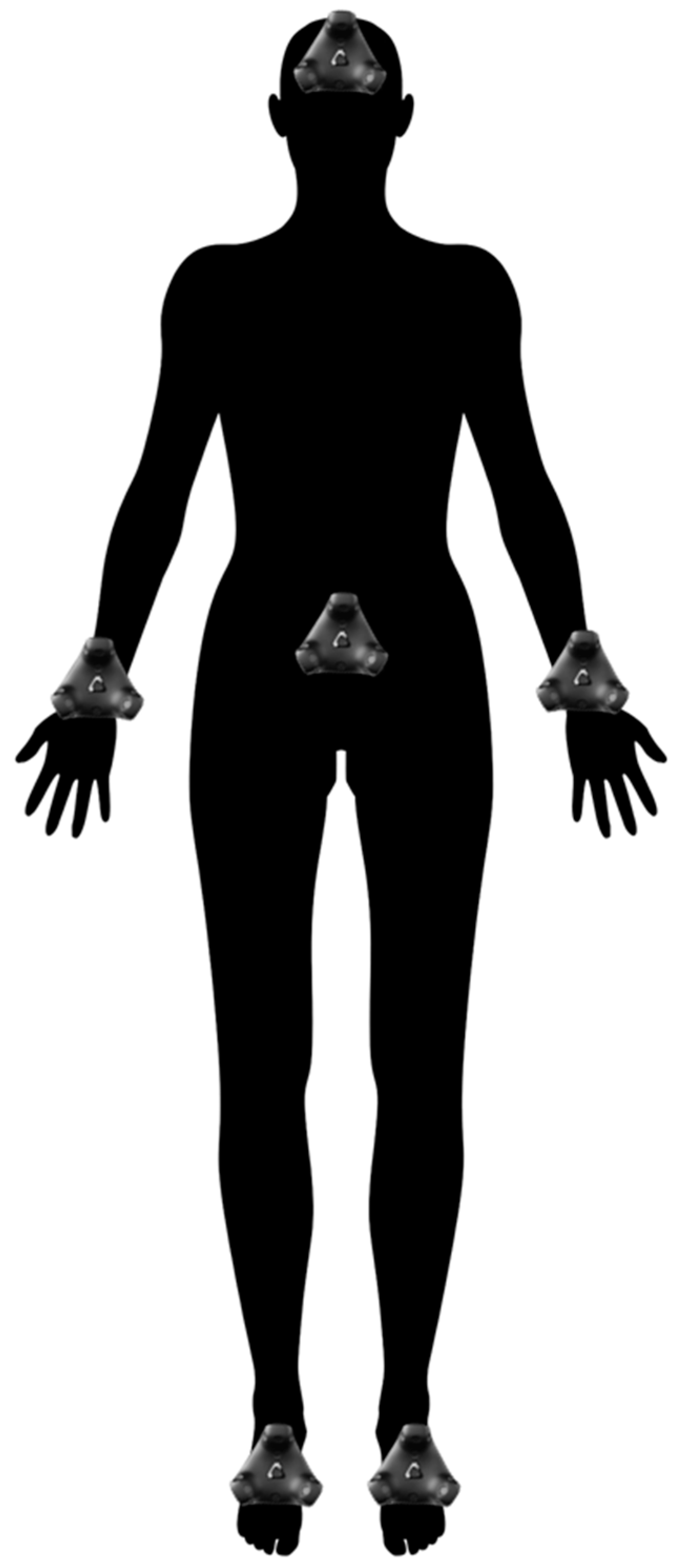
3.1. Technical Setup
3.2. Stimulus-Image Generation
3.3. Experimental Procedures
3.4. VR-Task Analysis
4. Discussion
Future Research Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shindle, M.K.; Khanna, A.J.; Bhatnagar, R.; Sponseller, P.D. Adolescent idiopathic scoliosis: Modern management guidelines. J. Surg. Orthop. Adv. 2006, 15, 43–52. [Google Scholar] [PubMed]
- Misterska, E.; Głowacki, J.; Głowacki, M.; Okręt, A. Long-term effects of conservative treatment of Milwaukee brace on body image and mental health of patients with idiopathic scoliosis. PLoS ONE 2018, 13, e0193447. [Google Scholar] [CrossRef] [PubMed]
- Misterska, E.; Glowacki, J.; Kołban, M. Does rigid spinal orthosis carry more psychosocial implications than the flexible brace in AIS patients? A cross-sectional study. J. Back Musculoskelet Rehabil. 2019, 32, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Misterska, E.; Głowacki, M.; Panek, S.; Ignyś-O′Byrne, A.; Głowacki, J.; Ignyś, I.; Krauss, H.; Piątek, J. Effects of living environment on the postoperative Scoliosis Research Society-24 results in females with adolescent idiopathic scoliosis. Med. Sci. Monit. 2012, 18, CR523–CR531. [Google Scholar] [CrossRef]
- Misterska, E.; Glowacki, M.; Adamczyk, K.; Glowacki, J.; Harasymczuk, J. A longitudinal study of alexithymia in relation to physical activity in adolescent females with scoliosis subjected to cheneau brace treatment: Preliminary report. Spine 2014, 39, E1026–E1034. [Google Scholar] [CrossRef]
- Misterska, E.; Glowacki, M.; Harasymczuk, J. Personality characteristics of females with adolescent idiopathic scoliosis after brace or surgical treatment compared to healthy controls. Med. Sci. Monit. 2010, 16, CR606–CR615. [Google Scholar]
- Misterska, E.; Glowacki, M.; Harasymczuk, J. Brace and deformity-related stress level in females with adolescent idiopathic scoliosis based on the Bad Sobernheim Stress Questionnaires. Med. Sci. Monit. 2011, 17, CR83–CR90. [Google Scholar] [CrossRef]
- Clayson, D.; Luz-Alterman, S.; Cataletto, M.M.; Levine, D.B. Longterm psychological sequelae of surgically versus nonsurgically treated scoliosis. Spine 1987, 12, 983–986. [Google Scholar] [CrossRef]
- Auerbach, J.D.; Lonner, B.S.; Crerand, C.E.; Shah, S.A.; Flynn, J.M.; Bastrom, T.; Penn, P.; Ahn, J.; Toombs, C.; Bharucha, N.; et al. Body image in patients with adolescent idiopathic scoliosis: Validation of the Body Image Disturbance Questionnaire—Scoliosis Version. J. Bone Joint. Surg. Am. 2014, 96, e61. [Google Scholar] [CrossRef]
- Caspi, A.; Amiaz, R.; Davidson, N.; Czerniak, E.; Gur, E.; Kiryati, N.; Harari, D.; Furst, M.; Stein, D. Computerized assessment of body image in anorexia nervosa and bulimia nervosa: Comparison with standardized body image assessment tool. Arch. Womens. Ment. Health 2017, 20, 139–147. [Google Scholar] [CrossRef]
- Toppenberg, H.L.; Ruiter, R.A.C.; Bos, A.E.R. HIV status acknowledgment and stigma reduction in virtual reality: The moderating role of perceivers′ attitudes. J. App. Soc. Psychol. 2019, 49, 203–212. [Google Scholar] [CrossRef]
- Earnshaw, V.A.; Chaudoir, S. From Conceptualizing to Measuring HIV Stigma: A Review of HIV Stigma Mechanism Measures. AIDS Behav. 2009, 13, 1160–1177. [Google Scholar] [CrossRef] [PubMed]
- Mölbert, S.C.; Thaler, A.; Mohler, B.J.; Streuber, S.; Romero, J.; Black, M.J.; Zipfel, S.; Karnath, H.O.; Giel, K.E. Assessing body image in anorexia nervosa using biometric self-avatars in virtual reality: Attitudinal components rather than visual body size estimation are distorted. Psychol. Med. 2017, 26, 1–12. [Google Scholar] [CrossRef]
- Wiggins, C.G.; Shaffrey, C.I.; Abel, M.F.; Menezez, A.H. Paediatric spinal deformities. Neurosurg. Focus 2003, 14, E3. [Google Scholar] [CrossRef]
- Misterska, E.; Głowacki, M.; Harasymczuk, J. Assessment of spinal appearance in female patients with adolescent idiopathic scoliosis treated operatively based on Spinal Appearance Questionnaire. Med. Sci. Monit. 2011, 17, 404–410. [Google Scholar] [CrossRef]
- Erra, U.; Scaniello, G.; Colonnese, V. Exploring the effectiveness of an augmented reality dressing room. Multimed. Tools. Appl. 2018, 77, 25077–25107. [Google Scholar] [CrossRef]
- Perry, B.N.; Armiger, R.S.; Wolde, M.; McFarland, K.A. Clinical Trial of the Virtual Integration Enviroment to Treat Phantom Limb Pain With Upper Extremity Amputation. Front. Neurol. 2018, 9, 770–778. [Google Scholar] [CrossRef]
- Gorski, F.; Bun, P.; Stefanska, K. Use of Virtual Mirror in Design of Individualized Orthopedic Supplies. In Innovations in Mechanical Engineering, Lecture Notes in Mechanical Engineering; Machado, J., Soares, F., Trojanowska, J., Ottaviano, E., Eds.; Springer: Cham, Switzerland, 2022; pp. 388–394. [Google Scholar]
- Robinson, R.; Forget, A.R.; VR Apps. New Technology System Modern Mirror Takes Virtual Try-Ons Next Level, Forbes. 2021. Available online: https://www.forbes.com/sites/roxannerobinson/2021/01/10/forget-ar--vr-apps-new-technology-system-modern-mirror-takes-virtual-try-ons-next-level/ (accessed on 6 November 2022).
- Caserman, P.; Garcia-Agundez, A.; Konrad, R.; Göbel, S.; Steinmetz, R. Real-time body tracking in virtual reality using a Vive tracker. Virtual. Real. 2019, 23, 155–168. [Google Scholar] [CrossRef]
- Piryankova, I.V.; Stefanucci, J.K.; Romero, J.; De La Rosa, S.; Black, M.J.; Mohler, B.J. Can I recognize my body′s weight? The influence of shape and texture on the perception of self. ACM Trans. Appl. Percept. 2014, 11, 1–18. [Google Scholar] [CrossRef]
- Martijn, C.; Vanderlinden, M.; Roefs, A.; Huijding, J. Jansen. Increasing body satisfaction of body concerned women through evaluative conditioning using social stimuli. Health Psychol. 2010, 29, 514–520. [Google Scholar] [CrossRef]
- Aspen, V.; Martijn, C.; Alleva, J.; Nagel, J.; Perret, C.; Purvis, C.; Saekow, J.; Lock, J.; Taylor, C.B. Decreasing body dissatisfaction using a brief conditioning intervention. Behav. Res. Ther. 2015, 69, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Misterska, E.; Głowacki, J.; Okręt, A.; Laurentowska, M.; Głowacki, M. Back and neck pain and function in females with adolescent idiopathic scoliosis: A follow-up at least 23 years after conservative treatment with a Milwaukee brace. PLoS ONE 2017, 12, e0189358. [Google Scholar] [CrossRef] [PubMed]
- Theologis, T.N.; Jefferson, R.J.; Simpson, A.H.; Turner-Smith, A.H.; Fairbank, J.C. Quantifying the cosmetics defect of adolescent idiopathic scoliosis. Spine 1993, 18, 909–912. [Google Scholar] [CrossRef] [PubMed]
- Haher, T.R.; Merola, A.; Zipnick, R.I.; Gorup, J.; Mannor, D.; Orchowski, J. Meta-analysis of surgical outcome in adolescent idiopathic scoliosis: A 35-year English literature review of 11,000 patients. Spine 1995, 14, 1575–1584. [Google Scholar] [CrossRef] [PubMed]
- de Vignemont, F. Body schema and body image—Pros and cons. Neuropsychologia 2010, 48, 669–680. [Google Scholar] [CrossRef]
- Longo, M.R. Implicit and explicit body representations. Eur. Psychol. 2015, 20, 6–15. [Google Scholar] [CrossRef]
- Longo, M.R.; Azañón, E.; Haggard, P. More than skin deep: Body representation beyond primary somatosensory cortex. Neuropsychologia 2010, 48, 655–668. [Google Scholar] [CrossRef]
- Noonan, K.J.; Dolan, L.A.; Jacobson, W.C.; Weinstein, S.L. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J. Pediatr. Orthop. 1997, 17, 712–717. [Google Scholar] [CrossRef]
- Koch, K.D.; Buchanan, R.; Birch, J.G.; Morton, A.A.; Gatchel, R.J.; Browne, R.H. Adolescents undergoing surgery for idiopathic scoliosis: How physical and psychological characteristics relate to patient satisfaction with the cosmetic result. Spine 2001, 26, 2119–2124. [Google Scholar] [CrossRef]
- Farrell, C.; Lee, M.; Shafran, R. Assessment of body size estimation: A review. Eur. Eat. Disord. Rev. 2005, 13, 75–88. [Google Scholar] [CrossRef]
- Gardner, R.M.; Brown, D.L. Body size estimation in anorexia nervosa: A brief review of findings from 2003 through 2013. Psychiatry Res. 2014, 219, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Cash, T.F.; Deagle, E.A. The nature and extent of body-image disturbances in anorexia nervosa and bulimia nervosa: A meta-analysis. Int. J. Eat. Disord. 1997, 22, 107–125. [Google Scholar] [CrossRef]
- Gaudio, S.; Brooks, S.J.; Riva, G. Nonvisual multisensory impairment of body perception in anorexia nervosa: A systematic review of neuropsychological studies. PLoS ONE 2014, 9, e110087. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.M.; Cesa, G.L.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual Reality-Enhanced Cognitive-Behavioral Therapy for Morbid Obesity: A Randomized Controlled Study with 1 Year Follow-Up. Cyberpsychology Behav. Soc. Netw. 2016, 19, 134–140. [Google Scholar] [CrossRef]
- Riva, G. Neuroscience and eating disorders: The allocentric lock hypothesis. Med. Hypotheses 2012, 78, 254–257. [Google Scholar] [CrossRef]
- Riva, G.; Gaudio, S. Allocentric lock in anorexia nervosa: New evidences from neuroimaging studies. Med. Hypotheses 2012, 79, 113–117. [Google Scholar] [CrossRef]
- Teachman, B.A.; Gapinski, K.D.; Brownell, K.D.; Rawlins, M.; Jeyaram, S. Demonstrations of implicit antifat bias: The impact of providing causal information and evoking empathy. Health Psychol. 2003, 22, 65–70. [Google Scholar] [CrossRef]
- Ciao, A.C.; Latner, J.D. Reducing obesity stigma: The effectiveness of cognitive dissonance and social consensus interventions. Obesity 2011, 19, 176. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misterska, E.; Górski, F.; Tomaszewski, M.; Buń, P.; Gapsa, J.; Słysz, A.; Głowacki, M. “Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image. Appl. Sci. 2023, 13, 2374. https://doi.org/10.3390/app13042374
Misterska E, Górski F, Tomaszewski M, Buń P, Gapsa J, Słysz A, Głowacki M. “Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image. Applied Sciences. 2023; 13(4):2374. https://doi.org/10.3390/app13042374
Chicago/Turabian StyleMisterska, Ewa, Filip Górski, Marek Tomaszewski, Pawel Buń, Jakub Gapsa, Anna Słysz, and Maciej Głowacki. 2023. "“Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image" Applied Sciences 13, no. 4: 2374. https://doi.org/10.3390/app13042374
APA StyleMisterska, E., Górski, F., Tomaszewski, M., Buń, P., Gapsa, J., Słysz, A., & Głowacki, M. (2023). “Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image. Applied Sciences, 13(4), 2374. https://doi.org/10.3390/app13042374







