Abstract
Introduction: The number of migrants living in Europe is growing rapidly. The PROTECT project is a national study conducted among refugees and migrants in the Lazio region, Italy from February 2018 to September 2021 to evaluate their otolaryngological, dental, and ophthalmic health status. This article reports the results of this study with a special focus on otolaryngological conditions and diseases. Materials and methods: A total of 3023 participants were included in the project. Data on the participants’ demographic factors, migration status, and otolaryngological history were collected using a questionnaire. Each patient underwent clinical ear, nose, and throat examination, and the main otolaryngological conditions and diseases were noted. Results: nearly two-thirds of participants were males (68.1%). The mean age was 31.6 ± 13.1. Most of the participants were born in Nigeria, followed by Bangladesh, Pakistan, Somalia, Mali, and Gambia. The prevalence of chronic noise exposure was 5.2%. Unilateral hearing loss was reported by 6.5% of the subjects, and bilateral hearing loss by 3.6%. The most frequent symptoms reported in the questionnaire were snoring (10.4%), nasal obstruction (5.9%), vertigo (5.0%), otalgia (4.5%), and tinnitus (4.2%). At the clinical examination, the most frequent findings were nasal septum deviation (25.2%), ear wax (6.5%), hypertrophic palatine tonsils (5.3%), and tympanic membrane perforation (1.3%). Conclusions: the PROTECT project allowed for the evaluation of otolaryngological, dental, and ophthalmological conditions in over 3000 migrants, giving them the possibility to access specialist care.
1. Introduction
Persons with migrant status living in Europe are increasing rapidly [1]. European countries receive an increasing number of vulnerable people every year, such as minors, unaccompanied foreign minors, disabled people, pregnant women, single parents with minor children, victims of trafficking, people with illnesses or mental disorders, and people who have been tortured, raped, or suffered other forms of psychological, physical, sexual violence [1,2].
Different factors lead to define migrants as vulnerable subjects, including health risks during and after migration, language, socioeconomical barriers, and difficulty in accessing health services in host countries [3]. Many migrants come from war zones and have been victims of persecutory acts in their country of origin [4].
The rates of migration to Europe have increased in recent years with considerable implications for national health systems [5]. The high costs for treatment in private facilities and barriers to accessing free health services are often the main causes of a high incidence of several diseases in migrant patients, including ear, nose, and throat conditions [6,7,8,9,10,11,12]. In fact, the quality of life of these persons is severely impacted by hearing difficulties, breathing issues, and poor oral health, as they could interfere with daily activities such as hearing, eating, and speaking. Furthermore, untreated aural, nasal, or pharyngeal problems could lead to serious risks to the health of older people such as malnutrition, heart disease, pneumonia, oral and pharyngeal cancers, and dementia [13,14,15]. The recent coronavirus disease 19 (COVID-19) pandemic has further worsened access to healthcare especially for vulnerable persons [16,17,18,19,20].
The “Patologie del distRettO TEsta-Collo nei migranti” (PROTECT) project was started in 2018 and led by the Sapienza University of Rome with the aim of protecting the health of vulnerable migrants, with a specific focus on otolaryngological, dental, and ophthalmic conditions through visits performed by otolaryngologists, dentists, and ophthalmologists. The PROTECT project was funded by the Asylum, Migration, and Integration Fund (FAMI) 2014–2020 of the Italian Ministry of the Interior, and cofinanced by the European Union.
In this article, we describe the results obtained in the PROTECT project with a specific focus on otolaryngological conditions and diseases. The results of this project for other conditions were reported elsewhere [21].
2. Materials and Methods
This is a national cross-sectional study (PROTECT project) conducted on the refugee and migrant population present in the Lazio region, Italy, from February 2018 to September 2021. The otolaryngological health of 3023 participants was investigated in a network of 53 reception centres and integration services. Participants were recruited on site through local refugee and migrant services.
The PROTECT project was approved by the Department of Oral and Maxillofacial Sciences, Sapienza, University of Rome (protocol identifying number: 0000839, 02/10/2018). The protocol was in accordance with the 1975 Declaration of Helsinki on medical protocols and ethics, and its later amendments.
2.1. Data Collection
Data were collected through an interviewer-administered questionnaire and a full clinical otolaryngological examination for each patient. The questionnaire investigated demographic factors, migration status, history for otolaryngological diseases, and health-related behaviours. The clinical examination was performed with the help of an otoscope, a nasal speculum, a laryngeal mirror, and a headlight.
Questionnaire administration and otolaryngological examinations were performed by trained otolaryngological specialists of the Department of Sense Organs, Sapienza University of Rome. The visits took place both at the premises of the reception centres distributed in the Lazio region with the use of mobile medical units and in the outpatient services of the Policlinico Umberto I hospital, Rome, Italy.
2.2. Questionnaire Information
The questionnaire was administered individually through an interview. The questionnaire questions are reported in Table 1. The physician filled the form on the basis of the responses received by each patient during the interview.

Table 1.
Individually administered questionnaire to each participant through an operator-administered interview.
2.3. Clinical Examination
The subjects were examined in the premises of the reception centres distributed in the Lazio region and in the outpatient services of the Policlinico Umberto I hospital of Rome, Italy. For each patient, the otolaryngological specialist evaluated the presence of external ear diseases (malformation of the auricle, malformation of the external ear canal, ear wax, external otitis), tympanic membrane perforation, middle otitis, nasal septum deviation or perforation, acute tonsillitis or peritonsillar abscess, and the presence of spontaneous nystagmus. A standard form listing the above conditions was available for each patient, which was filled by the otolaryngological specialist after the visit using a yes/no response.
In the case of patients who had reported hearing loss at questionnaire, a hearing exam with pure tone audiometry and, if indicated, otoacoustic emissions was performed in the Policlinico Umberto I hospital; the response of the patient was considered valid only if the exams confirmed the presence of hearing loss [22,23,24]. Hearing loss was defined as a hearing threshold for two or more frequencies >25 dB HL in one or both ears.
If necessary, on the basis of the health evaluation and clinical history, patients were referred to the otolaryngological department of the Policlinico Umberto I hospital for further diagnostic exams or treatments.
2.4. Statistical Analysis
The forms (questionnaire and clinical examination) filled by the examiner during each visit were collected and entered into a database created using Microsoft Excel (Microsoft, Redmond, WA, USA).
Descriptive statistics, including mean ± SD values and percentages, were calculated for each variable, and used to define the main clinical and demographic characteristics.
Data were evaluated using statistical analysis software (version 20.0, Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA).
3. Results
A total of 3023 participants were examined and interviewed. Their age varied from 0 to 93 years; the mean age was 31.6 ± 13.1, SD = 13,075. Among all the subjects, 2058 were male (68.1%) and 965 were female (31.9%). Data are shown in Table 2.

Table 2.
Demographic characteristics of migrants included in the study.
Most of the participants were born in Nigeria (10.15%, n = 307), followed by Bangladesh (7.51%, n = 227), Pakistan (5.45%, n = 165), Somalia (4.76%, n = 144), Mali (4.03%, n = 122), and Gambia (3.97%, n = 120). The average stay in local refugee and migrant services for patients included in the study was 36.2 days (range 1–91, SD = 21,320).
Figure 1 shows the 20 most common countries of origin of the participants.
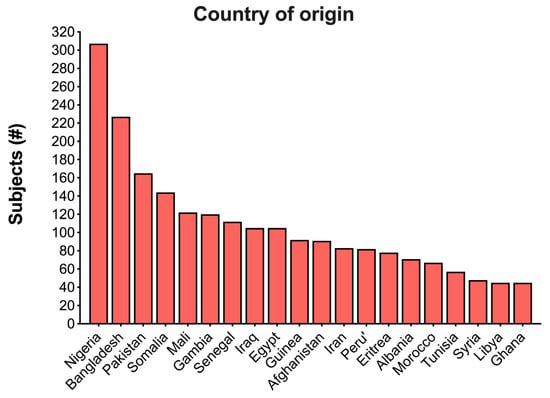
Figure 1.
Distribution of the country of origin of the migrants screened in this project sorted by number of patients. Only the first 20 countries are shown.
The most common otolaryngological issue reported in the questionnaire was snoring, present in 10.38% (n = 314) of the subjects. Other conditions reported by the patients were audiologically confirmed unilateral hearing loss (6.48%, n = 196), nasal obstruction (5.89%, n = 178), chronic noise exposure (5.19%, n = 157), subjective vertigo (4.99%, n = 151), nasal trauma (4.89%, n = 148), familial deafness (4.80%, n = 145), ear pain (4.50%, n = 136), tinnitus (4.17%, n = 126), audiologically confirmed bilateral hearing loss (3.60%, n = 109), ear trauma (3.57%, n = 108), laryngeal trauma (0.89%, n = 27), and dysphonia (0.79%, n = 24). Figure 2 details the otolaryngological conditions and symptoms reported by patients in the questionnaire.
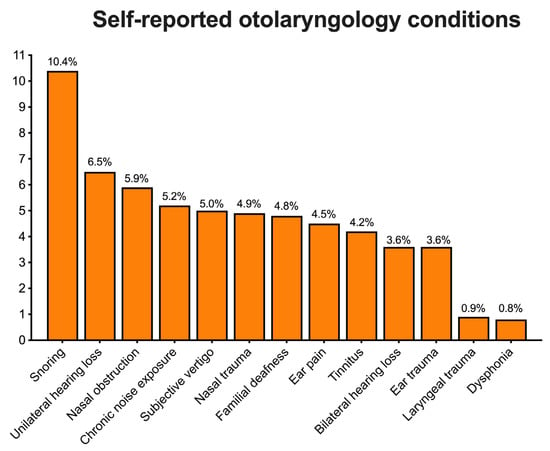
Figure 2.
Histogram of otolaryngological conditions and symptoms reported by patients in the operator-administered questionnaire. Data above each column were rounded to the first decimal.
Otolaryngological examination showed a deviation of the nasal septum in 25.21% (n = 762), ear wax in 6.48% (n = 196), and tonsillar hypertrophy in 5.29% of the patients (n = 160). Other less common pathological findings were tympanic membrane perforation (1.29%, n = 39), external otitis (0.89%, n = 27), and middle ear otitis (0.50%, n = 15). Figure 3 shows the otolaryngological conditions found during the clinical examination.
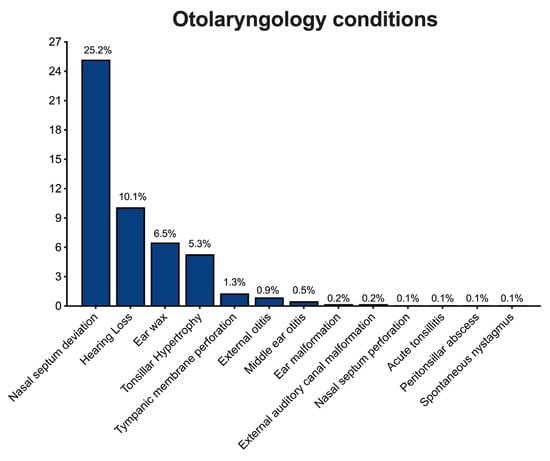
Figure 3.
Histogram of otolaryngological conditions found during the clinical examination. Data above each column were rounded to the first decimal.
4. Discussion
In recent years, the prevalence of aural, nasal, or laryngeal diseases in industrialised countries has decreased due to the large use of preventive measures [25,26]. However, prevention is less diffused in nonindustrialised countries, resulting in a higher incidence of common otolaryngological diseases, as found in the sample of migrants included in this study [6,7,10].
Among aural disorders, hearing loss was the most common condition reported during the screening of the migrants included in the study. In the world, one-third of the population over 65 suffer from disabling hearing impairments [27,28,29]. In Italy, the incidence of hearing loss among the population in the third decade of life, like the mean age of subjects evaluated in this study, is about of 3.2% according to the Italian Society of Occupational Medicine [30]. This number is significantly lower compared to the self-reported hearing loss of patients included in the present study, which involved 6.5% of subjects for unilateral hearing loss and 3.6% for bilateral hearing loss. Differently from the countries of origin of our patients, many factors contributed to the reduction in hearing loss over the last decade in industrialised countries. For example, one of the factors for the pathogenesis of otosclerosis are viral infections [31], and the measles virus shows an important organotropism for the otic capsule [32]. From the 1970s, the introduction of measles vaccination reduced the incidence of otosclerosis [33] and generally of hearing loss [34].
Occupational and environmental noise exposure accounts for the 16% of total hearing loss cases [35,36,37,38,39]. Global governmental bodies that have established regulations to avoid noise exposure include the Occupational Safety and Health Administration, the National Institutes of Occupational Safety and Health, and the European Union (EU) [40]. Unfortunately, these recommendations often are not implemented by the migrants’ countries of origin, as shown by the elevated number of persons in our sample reporting hearing loss or chronic noise exposure in their country of origin.
Research conducted in France and the USA showed that, during screening visits among migrants and homeless individuals, the most frequent symptoms involved the upper and lower respiratory tract, such as a dry or productive cough, rhinorrhea, and dyspnea. Sometimes these symptoms may precede life-threatening diseases such as pulmonary infection or tuberculosis [41,42,43]. Therefore, the possibility of guaranteeing free access to screening the upper airway to all patients is fundamental to identify alterations in nasal airflow (nasal septum deviation or perforation) or chronic infections of the nose, nasopharynx, or oropharynx that could lead to severe infections of the lower airway in the medium and long term.
Quality of life is strongly influenced by the health of the ear, nose and throat. For this reason, it is necessary to render otolaryngological services easily accessible to vulnerable persons and migrants [44]. Projects such as PROTECT aim at improving the quality of life of these patients through the prevention and screening of common conditions, leading to the resolution of the symptoms of an inflammatory/infectious nature or the early interception of more serious conditions such as head and neck neoplasms.
5. Conclusions
The PROTECT project has allowed for the screening of otolaryngological, dental, and ophthalmological conditions in over 3000 migrants, giving them the possibility to access specialist care. Furthermore, for operators of the centers, nurses, and physicians, this project represents an unrepeatable opportunity to offer care to vulnerable persons. The knowledge, prevention, and management of these diseases, which are often painful and disabling in these patients, have led to an improvement in the quality of life of vulnerable migrants included in the PROTECT project.
Author Contributions
Conceptualisation, M.R.; methodology, A.C. and M.R.; validation, A.G. and M.B.; formal analysis, F.Y.R.; investigation, A.M., D.A. and A.M.; resources, A.P. and M.B.; data curation, A.B.; writing—original draft preparation, A.C.; writing—review and editing, M.R.; visualisation, G.P. and L.O.; supervision, A.G. and M.d.V.; project administration, A.P. and L.O.; funding acquisition, A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received external funding from the Asylum, Migration, and Integration Fund (FAMI) 2014–2020 of the Italian Ministry of the Interior, and cofinanced by the European Union according to code PROG-2010.
Institutional Review Board Statement
The “PROTECT” project was approved by the Department of Oral and Maxillofacial Sciences, Sapienza, University of Rome (Protocol identifying number: 0000839 on 2 October 2018). The protocol was in accordance with the 1975 Declaration of Helsinki on medical protocols and ethics and its later amendments.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lebano, A.; Hamed, S.; Bradby, H.; Gil-Salmeron, A.; Dura-Ferrandis, E.; Garces-Ferrer, J.; Azzedine, F.; Riza, E.; Karnaki, P.; Zota, D.; et al. Migrants’ and refugees’ health status and healthcare in Europe: A scoping literature review. BMC Public Health 2020, 20, 1039. [Google Scholar] [CrossRef] [PubMed]
- Zenner, D.; Mendez, A.R.; Schillinger, S.; Val, E.; Wickramage, K. Health and illness in migrants and refugees arriving in Europe: Analysis of the electronic Personal Health Record system. J. Travel Med. 2022, 29, taac035. [Google Scholar] [CrossRef] [PubMed]
- Lauritano, D.; Moreo, G.; Carinci, F.; Campanella, V.; Della Vella, F.; Petruzzi, M. Oral Health Status among Migrants from Middle- and Low-Income Countries to Europe: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12203. [Google Scholar] [CrossRef]
- Pinchi, V.; Focardi, M.; Pradella, F.; Grifoni, R.; Palandri, M.; Norelli, G.A. Day to day issues in the forensic identification practice related to illegal immigration in Italy. J. Forensic Odonto-Stomatol. 2017, 35, 157–165. [Google Scholar]
- Seedat, F.; Hargreaves, S.; Nellums, L.B.; Ouyang, J.; Brown, M.; Friedland, J.S. How effective are approaches to migrant screening for infectious diseases in Europe? A systematic review. Lancet Infect. Dis. 2018, 18, e259–e271. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Marinelli, A.; De-Giorgio, F.; Crescenzi, D.; Vincentiis, M.; Greco, A.; Arcangeli, A.; Ercoli, L. Prevalence of Otolaryngology Diseases in an Urban Homeless Population. Otolaryngol. Head Neck Surg. 2022, 166, 1022–1027. [Google Scholar] [CrossRef] [PubMed]
- Itamura, K.; Hur, K.; Ference, E.; Wrobel, B.; Chambers, T.N. Characterization of Chronic Sinonasal Disease Symptoms in an Urban Homeless Population. Am. J. Rhinol. Allergy 2020, 34, 494–501. [Google Scholar] [CrossRef]
- Lee, S.J.; Thomas, P.; Newnham, H.; Freidin, J.; Smith, C.; Lowthian, J.; Borghmans, F.; Gocentas, R.A.; De Silva, D.; Stafrace, S. Homeless status documentation at a metropolitan hospital emergency department. Emerg. Med. Australas. 2019, 31, 639–645. [Google Scholar] [CrossRef]
- Wadhera, R.K.; Choi, E.; Shen, C.; Yeh, R.W.; Joynt Maddox, K.E. Trends, Causes, and Outcomes of Hospitalizations for Homeless Individuals: A Retrospective Cohort Study. Med. Care 2019, 57, 21–27. [Google Scholar] [CrossRef]
- Westerberg, B.D.; Lango, M.N. Otolaryngology-Related Disorders in Underserved Populations, Otolaryngology Training and Workforce Considerations in North America. Otolaryngol. Clin. North Am. 2018, 51, 685–695. [Google Scholar] [CrossRef]
- Daly, B.; Newton, T.; Batchelor, P.; Jones, K. Oral health care needs and oral health-related quality of life (OHIP-14) in homeless people. Community Dent. Oral Epidemiol. 2010, 38, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Materia, E.; Spadea, T.; Rossi, L.; Cesaroni, G.; Area, M.; Perucci, C.A. Health care inequalities: Hospitalization and socioeconomic position in Rome. Epidemiol. Prev. 1999, 23, 197–206. [Google Scholar] [PubMed]
- Di Stadio, A.; Ralli, M.; Roccamatisi, D.; Scarpa, A.; Della Volpe, A.; Cassandro, C.; Ricci, G.; Greco, A.; Bernitsas, E. Hearing loss and dementia: Radiologic and biomolecular basis of their shared characteristics. A systematic review. Neurol. Sci. 2021, 42, 579–588. [Google Scholar] [CrossRef]
- Pacelli, B.; Zengarini, N.; Broccoli, S.; Caranci, N.; Spadea, T.; Di Girolamo, C.; Cacciani, L.; Petrelli, A.; Ballotari, P.; Cestari, L.; et al. Differences in mortality by immigrant status in Italy. Results of the Italian Network of Longitudinal Metropolitan Studies. Eur. J. Epidemiol. 2016, 31, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Kroening, A.L.H.; Dawson-Hahn, E. Health Considerations for Immigrant and Refugee Children. Adv. Pediatr. 2019, 66, 87–110. [Google Scholar] [CrossRef]
- Ralli, M.; Arcangeli, A.; Ercoli, L. Homelessness and COVID-19: Leaving No One Behind. Ann. Glob. Health 2021, 87, 11. [Google Scholar] [CrossRef]
- Kluge, H.H.P.; Jakab, Z.; Bartovic, J.; D’Anna, V.; Severoni, S. Refugee and migrant health in the COVID-19 response. Lancet 2020, 395, 1237–1239. [Google Scholar] [CrossRef]
- Perri, M.; Dosani, N.; Hwang, S.W. COVID-19 and people experiencing homelessness: Challenges and mitigation strategies. CMAJ 2020, 192, E716–E719. [Google Scholar] [CrossRef]
- Ralli, M.; Cedola, C.; Urbano, S.; Morrone, A.; Ercoli, L. Homeless persons and migrants in precarious housing conditions and COVID-19 pandemic: Peculiarities and prevention strategies. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9765–9767. [Google Scholar] [CrossRef]
- Werner, M.T.; Carey, R.M.; Albergotti, W.G.; Lukens, J.N.; Brody, R.M. Impact of the COVID-19 Pandemic on the Management of Head and Neck Malignancies. Otolaryngol. Head Neck Surg. 2020, 162, 816–817. [Google Scholar] [CrossRef]
- Palaia, G.B.M.; Pranno, N.; Ralli, M.; Bruscolini, A.; Capocci, M.; Gaimari, G.; Macali, F.; Corridore, D.; Cotticelli, L.; Covello, F.; et al. Oral Pathologies in Migrants: The Experience of the “PROTECT” Project in 3023 Patients. Appl. Sci. 2022, 12, 12621. [Google Scholar] [CrossRef]
- Karlsmose, B.; Pedersen, H.B.; Lauritzen, T.; Parving, A. Audiometry in general practice: Validation of a pragmatic pure-tone audiometry method. Scand. Audiol. 1998, 27, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Noorhassim, I.; Kaga, K.; Nishimura, K. Pure-tone audiometry and auditory brainstem responses in noise-induced deafness. Am. J. Otolaryngol. 1996, 17, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Fetoni, A.R.; Garzaro, M.; Ralli, M.; Landolfo, V.; Sensini, M.; Pecorari, G.; Mordente, A.; Paludetti, G.; Giordano, C. The monitoring role of otoacoustic emissions and oxidative stress markers in the protective effects of antioxidant administration in noise-exposed subjects: A pilot study. Med. Sci. Monit. 2009, 15, PR1–PR8. [Google Scholar]
- Global Burden of Disease Cancer, C.; Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [CrossRef]
- Hashim, D.; Genden, E.; Posner, M.; Hashibe, M.; Boffetta, P. Head and neck cancer prevention: From primary prevention to impact of clinicians on reducing burden. Ann. Oncol. 2019, 30, 744–756. [Google Scholar] [CrossRef]
- Syka, J.; Canlon, B. Editorial: Special issue on presbycusis. Hear. Res. 2021, 402, 108115. [Google Scholar] [CrossRef]
- Patel, R.; McKinnon, B.J. Hearing Loss in the Elderly. Clin. Geriatr. Med. 2018, 34, 163–174. [Google Scholar] [CrossRef]
- Osterhammel, D.; Osterhammel, P. High-frequency audiometry. Age and sex variations. Scand. Audiol. 1979, 8, 73–81. [Google Scholar] [CrossRef]
- Riva, M.M.; Cantamessa, F.; Borleri, D.; Mosconi, G. Occupational health and safety of road haulage company employees. Med. Lav. 2018, 109, 180–189. [Google Scholar] [CrossRef]
- McKenna, M.J.; Mills, B.G. Ultrastructural and immunohistochemical evidence of measles virus in active otosclerosis. Acta Otolaryngol. Suppl. 1990, 470, 130–139; discussion 139–140. [Google Scholar] [CrossRef] [PubMed]
- Tatsuo, H.; Ono, N.; Tanaka, K.; Yanagi, Y. SLAM (CDw150) is a cellular receptor for measles virus. Nature 2000, 406, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Arnold, W. Some Remarks on the Histopathology of Otosclerosis. In Otosclerosis and Stapes Surgery; Karger Publishers: Basel, Switzerland, 2007; Volume 65, pp. 25–30. [Google Scholar] [CrossRef]
- McDermott, J.H.; Molina-Ramirez, L.P.; Bruce, I.A.; Mahaveer, A.; Turner, M.; Miele, G.; Body, R.; Mahood, R.; Ulph, F.; MacLeod, R.; et al. Diagnosing and Preventing Hearing Loss in the Genomic Age. Trends Hear. 2019, 23, 2331216519878983. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.I.; Nelson, R.Y.; Concha-Barrientos, M.; Fingerhut, M. The global burden of occupational noise-induced hearing loss. Am. J. Ind. Med. 2005, 48, 446–458. [Google Scholar] [CrossRef]
- Frederiksen, T.W.; Ramlau-Hansen, C.H.; Stokholm, Z.A.; Grynderup, M.B.; Hansen, A.M.; Lund, S.P.; Kristiansen, J.; Vestergaard, J.M.; Bonde, J.P.; Kolstad, H.A. Occupational noise exposure, psychosocial working conditions and the risk of tinnitus. Int. Arch. Occup. Environ. Health 2017, 90, 217–225. [Google Scholar] [CrossRef]
- Zhou, X.; Merzenich, M.M. Environmental noise exposure degrades normal listening processes. Nat. Commun. 2012, 3, 843. [Google Scholar] [CrossRef]
- Agrawal, Y.; Platz, E.A.; Niparko, J.K. Risk factors for hearing loss in US adults: Data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol. Neurotol. 2009, 30, 139–145. [Google Scholar] [CrossRef]
- Rubak, T.; Kock, S.A.; Koefoed-Nielsen, B.; Bonde, J.P.; Kolstad, H.A. The risk of noise-induced hearing loss in the Danish workforce. Noise Health 2006, 8, 80–87. [Google Scholar]
- Sheppard, A.; Ralli, M.; Gilardi, A.; Salvi, R. Occupational Noise: Auditory and Non-Auditory Consequences. Int. J. Environ. Res. Public Health 2020, 17, 8963. [Google Scholar] [CrossRef]
- Hwang, S.W.; Lebow, J.M.; Bierer, M.F.; O’Connell, J.J.; Orav, E.J.; Brennan, T.A. Risk factors for death in homeless adults in Boston. Arch. Intern. Med. 1998, 158, 1454–1460. [Google Scholar] [CrossRef]
- Usatine, R.P.; Gelberg, L.; Smith, M.H.; Lesser, J. Health care for the homeless: A family medicine perspective. Am. Fam. Physician 1994, 49, 139–146. [Google Scholar] [PubMed]
- Ly, T.D.A.; Edouard, S.; Badiaga, S.; Tissot-Dupont, H.; Hoang, V.T.; Pommier de Santi, V.; Brouqui, P.; Raoult, D.; Gautret, P. Epidemiology of respiratory pathogen carriage in the homeless population within two shelters in Marseille, France, 2015–2017: Cross sectional 1-day surveys. Clin. Microbiol. Infect. 2019, 25, 249.e1–249.e6. [Google Scholar] [CrossRef] [PubMed]
- Chaffee, B.W.; Rodrigues, P.H.; Kramer, P.F.; Vitolo, M.R.; Feldens, C.A. Oral health-related quality-of-life scores differ by socioeconomic status and caries experience. Community Dent. Oral. Epidemiol. 2017, 45, 216–224. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).