Evaluation of the Failure Rate and Clinical Efficacy of Orthodontic Brackets Indirect Bonding with Computer-Aided Transfer Jig System: An In Vivo Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Inclusion and Exclusion Criteria
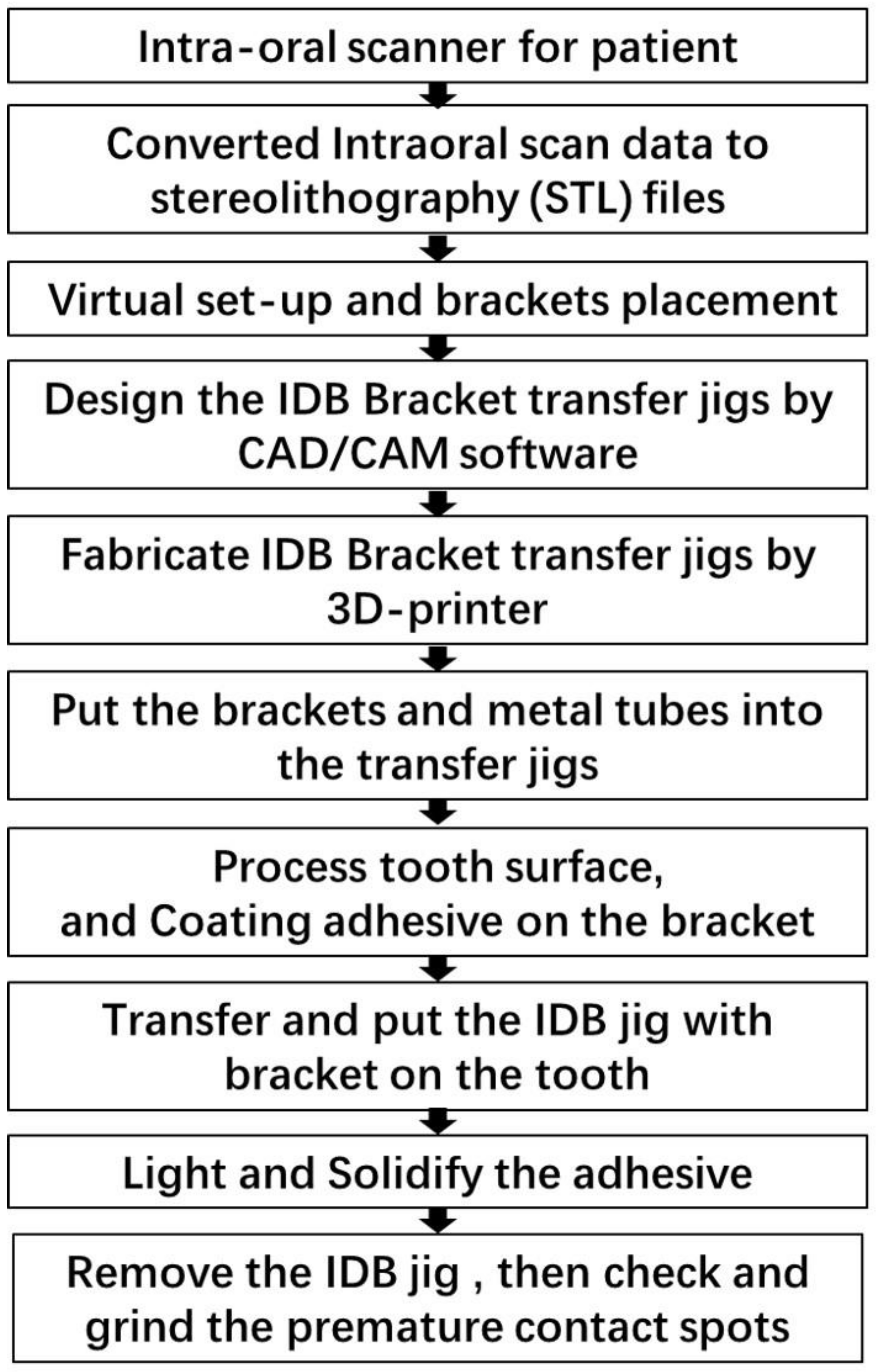
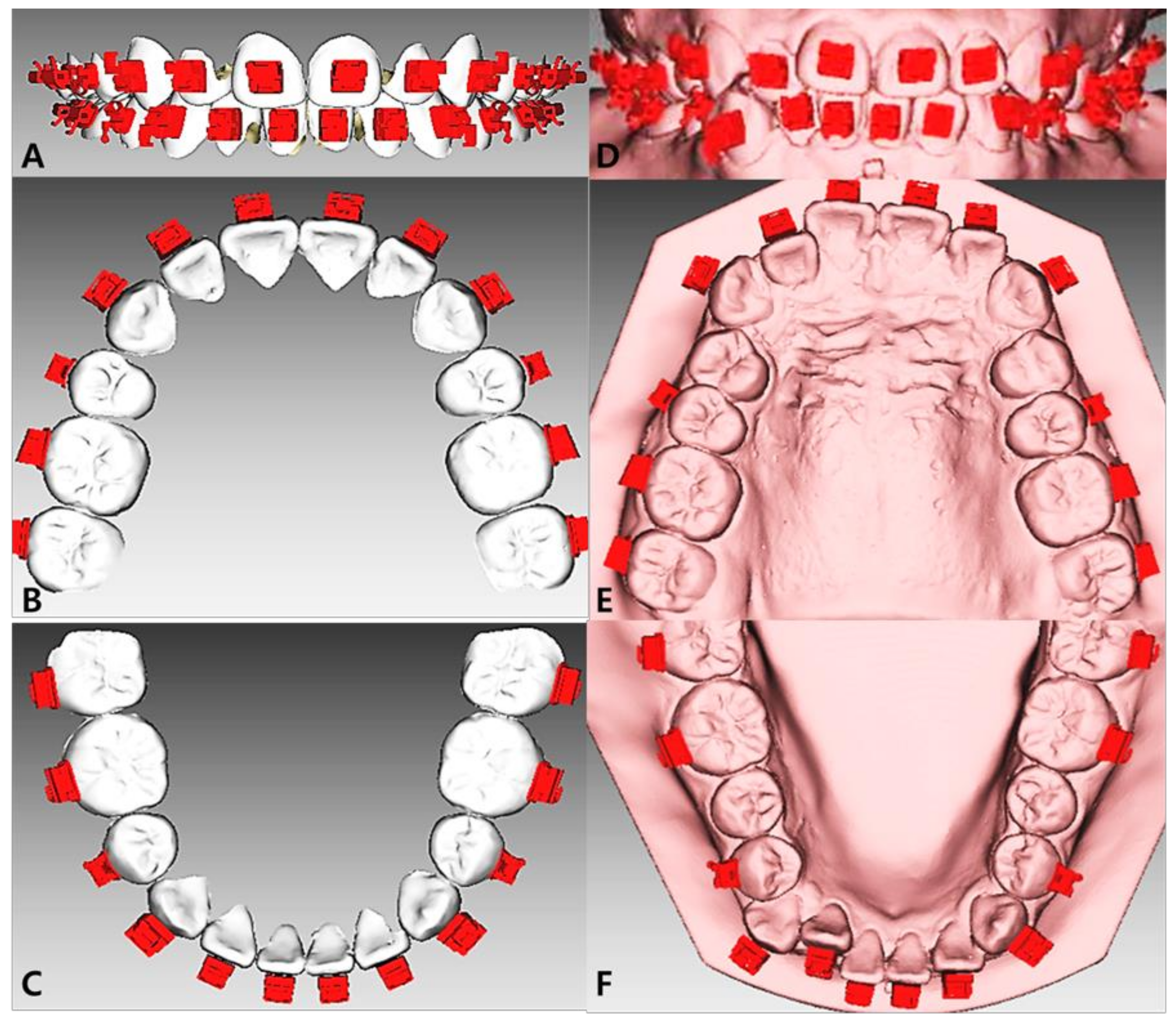
2.3. Study Procedure
2.4. Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
- 1.
- Considering that mandibular teeth, especially mandibular anterior teeth, had a higher bonding failure rate, it is recommended to control the thickness of the resin adhesive as much as possible during the IDB process. For mandibular anterior teeth, the unexpected movement of the surrounding soft tissue must be limited, and contamination of the bonding interface caused by excessive salivation must be controlled. A small archwire was chosen for overcrowded cases to avoid bonding failure due to excessive orthodontic force. Additionally, care should be taken to check and remove premature contact spots. Resin bite blocks can be added when necessary to open the bite;
- 2.
- Considering that the anterior teeth had a higher position error rate, the application of stable and steady occlusal pressure along the long axis of the tooth on the transfer jigs in the IDBS is suggested;
- 3.
- The effects of sex, age, and vertical skeletal pattern warranted careful follow-up of male patients under 20 years of age with hyperdivergent skeletal patterns, provided they followed the treatment instructions. Moreover, patients should be advised to change their dietary habits.
5. Conclusions
- 1.
- Anterior teeth had a higher position error rate. Mandibular anterior teeth had a higher bonding failure rate. IDBS had higher accuracy in the premolars and molars;
- 2.
- Sex, age, and treatment periods are the factors affecting IDBS;
- 3.
- Patients with hyperdivergent skeletal patterns had higher brackets bonding failure rates, while IDBS had higher strength in patients with normodivergent and hypodivergent skeletal patterns.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, J.H.; Choi, J.Y.; Oh, S.H.; Kim, S.H. Three-Dimensional Digital Superimposition of Orthodontic Bracket Position by Using a Computer-Aided Transfer Jig System: An Accuracy Analysis. Sensors 2021, 21, 5911. [Google Scholar] [CrossRef] [PubMed]
- Gange, P. The evolution of bonding in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 147 (Suppl. S4), S56–S63. [Google Scholar] [CrossRef]
- Silverman, E.; Cohen, M.; Gianelly, A.A.; Dietz, V.S. A universal direct bonding system for both metal and plastic brackets. Am. J. Orthod. 1972, 62, 236–244. [Google Scholar] [CrossRef]
- Kanashiro, L.K.; Robles-Ruíz, J.J.; Ciamponi, A.L.; Medeiros, I.S.; Dominguez, G.C.; de Fantini, S.M. Effect of adhesion boosters on indirect bracket bonding. Angle Orthod. 2014, 84, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Panayi, N.C.; Tsolakis, A.I.; Athanasiou, A.E. Digital assessment of direct and virtual indirect bonding of orthodontic brackets: A clinical prospective cross-sectional comparative investigation. Int. Orthod. 2020, 18, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Czolgosz, I.; Cattaneo, P.M.; Cornelis, M.A. Computer-aided indirect bonding versus traditional direct bonding of orthodontic brackets: Bonding time, immediate bonding failures, and cost-minimization. A randomized controlled trial. Eur. J. Orthod. 2021, 43, 144–151. [Google Scholar] [CrossRef]
- Dalessandri, D.; Dalessandri, M.; Bonetti, S.; Visconti, L.; Paganelli, C. Effectiveness of an indirect bonding technique in reducing plaque accumulation around braces. Angle Orthod. 2012, 82, 313–318. [Google Scholar] [CrossRef]
- Sabbagh, H.; Khazaei, Y.; Baumert, U.; Hoffmann, L.; Wichelhaus, A.; Janjic Rankovic, M. Bracket Transfer Accuracy with the Indirect Bonding Technique—A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 2568. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, J.Y.; Kim, S.H.; Kim, S.J.; Lee, K.J.; Nelson, G. Three-dimensional evaluation of the transfer accuracy of a bracket jig fabricated using computer-aided design and manufacturing to the anterior dentition: An in vitro study. Korean J. Orthod. 2021, 51, 375–386. [Google Scholar] [CrossRef]
- Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; Harding, W.J. Factors influencing treatment time in or-thodontic patients. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 230–238. [Google Scholar] [CrossRef]
- Huang, X.H.; Xu, L.; Lin, S. Effects of double transparent pressure diaphragm transfer tray on indirect bonding. Shanghai J. Stomatol. 2016, 25, 734–737. [Google Scholar]
- Menini, A.; Cozzani, M.; Sfondrini, M.; Scribante, A.; Cozzani, P.; Gandini, P. A 15-month evaluation of bond failures of ortho-dontic brackets bonded with direct versus indirect bonding technique: A clinical trial. Prog. Orthod. 2014, 15, 70. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.S.; Abdelsayed, F.A.; Abdelghany, A.H.; Morse, Z.; Aboulfotouh, M.H. For Indirect Orthodontic Attachment Place-ment, adding a Custom Composite Resin Base Is Not Beneficial: A Split-Mouth Randomized Clinical Trial. Int. J. Dent. 2022, 2022, 9059697. [Google Scholar] [CrossRef]
- Benaissa, A.; Merdji, A.; Bendjaballah, M.Z.; Ngan, P.; Mukdadi, O.M. Stress influence on orthodontic system components under simulated treatment loadings. Comput. Methods Programs Biomed. 2020, 195, 105569. [Google Scholar] [CrossRef]
- Knox, J.; Kralj, B.; Hübsch, P.F.; Middleton, J.; Jones, M.L. An evaluation of the influence of orthodontic adhesive on the stresses generated in a bonded bracket finite element model. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 43–53. [Google Scholar] [CrossRef]
- Arici, S.; Caniklioglu, C.M.; Arici, N.; Ozer, M.; Oguz, B. Adhesive thickness effects on the bond strength of a light-cured resin-modified glass ionomer cement. Angle Orthod. 2005, 75, 254–259. [Google Scholar] [PubMed]
- Kulkarni, N.B.; Goyal, S. Comparison of Bracket Failure Rate between Two Different Materials Used to Fabricate Transfer Trays for Indirect Orthodontic Bonding. J. Contemp. Dent. Pract. 2022, 23, 307–312. [Google Scholar]
- Ahangar Atashi, M.H.; Shahamfar, M. Long-term evaluation of clinical performance of direct-bonded brackets: An epidemio-logic survey. J. Contemp. Dent. Pract. 2013, 14, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.; Mheissen, S.; Iqbal, A.; Jafri, A.R.; Alam, M.K. Bracket Failure in Orthodontic Patients: The Incidence and the Influence of Different Factors. BioMed Res. Int. 2022, 2022, 5128870. [Google Scholar] [CrossRef]
- Hitmi, L.; Muller, C.; Mujajic, M.; Attal, J.P. An 18-month clinical study of bond failures with resin-modified glass ionomer cement in orthodontic practice. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 406–415. [Google Scholar] [CrossRef]
- Moninuola, A.E.; Costa, O.O.; Isiekwe, M.C. A review of orthodontic bond failure using a chemical cure adhesive. Odontostomatol. -Trop. Trop. Dent. J. 2010, 33, 35–40. [Google Scholar]
- Feldens, C.A.; Nakamura, E.K.; Tessarollo, F.R.; Closs, L.Q. Desire for orthodontic treatment and associated factors among adolescents in Southern Brazil. Angle Orthod. 2015, 85, 224–232. [Google Scholar] [CrossRef]
- Barbosa, I.V.; Ladewig, V.M.; Almeida-Pedrin, R.R.; Cardoso, M.A.; Santiago, J.F., Jr.; Conti, A.C.C.F. The association between patient’s compliance and age with the bonding failure of orthodontic brackets: A cross-sectional study. Prog. Orthod. 2018, 19, 11. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.S.; Fleming, P.S.; Sharma, P.K.; Battagel, J. Influence of supplemental written information on adolescent anxiety, motivation and compliance in early orthodontic treatment. Angle Orthod. 2010, 80, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Larsson, B.W.; Bergström, K. Adolescents’ perception of the quality of orthodontic treatment. Scand. J. Caring Sci. 2005, 19, 95–101. [Google Scholar] [CrossRef]
- Iliadi, A.; Baumgartner, S.; Athanasiou, A.E.; Eliades, T.; Eliades, G. Effect of intraoral aging on the setting status of resin com-posite and glass ionomer orthodontic adhesives. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 425–433. [Google Scholar] [CrossRef]
- Dudás, C.; Czumbel, L.M.; Kiss, S.; Gede, N.; Hegyi, P.; Mártha, K.; Varga, G. Clinical bracket failure rates between different bonding techniques: A systematic review and meta-analysis. Eur. J. Orthod. 2022, cjac050. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Zeng, Y.; Zhang, Z.; Xu, W.; Xiao, L. Comparison of the transfer accuracy of two digital indirect bonding trays for labial bracket bonding. Angle Orthod. 2021, 91, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.; Cho, Y.; Kim, D.W.; Kim, M.; Kim, Y.J.; Chang, M. Full-arch accuracy of five intraoral scanners: In vivo analysis of trueness and precision. Korean J. Orthod. 2021, 51, 95–104. [Google Scholar] [CrossRef]
- Montasser, M.A. Effect of applying a sustained force during bonding orthodontic brackets on the adhesive layer and on shear bond strength. Eur. J. Orthod. 2011, 33, 402–406. [Google Scholar] [CrossRef]
- Hoffmann, L.; Sabbagh, H.; Wichelhaus, A.; Kessler, A. Bracket transfer accuracy with two different three-dimensional printed transfer trays vs. silicone transfer trays. Angle Orthod. 2022, 92, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Sathyanarayana, H.P.; Premkumar, S.; Manjula, W.S. Assessment of maximum voluntary bite force in adults with normal occlusion and different types of malocclusions. J. Contemp. Dent. Pract. 2012, 13, 534–538. [Google Scholar] [PubMed]
- Cha, B.K.; Kim, C.H.; Baek, S.H. Skeletal sagittal and vertical facial types and electromyographic activity of the masticatory muscle. Angle Orthod. 2007, 77, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Mansour, A.Y.; Drummond, J.L.; Evans, C.A.; Bakhsh, Z. In vitro evaluation of selfetch bonding in orthodontics using cyclic fatigue. Angle Orthod. 2011, 81, 783–787. [Google Scholar] [CrossRef]
- Mansour, A.Y.; Bamashmous, M. Survival analysis of an orthodontic bracket bond subjected to cyclic tensile and shear forces. J. Orthod. Sci. 2018, 7, 1. [Google Scholar] [CrossRef]
- Dos Santos, A.L.; Wambier, L.M.; Wambier, D.S.; Moreira, K.M.; Imparato, J.C.; Chibinski, A.C. Orthodontic bracket bonding techniques and adhesion failures: A systematic review and metaanalysis. J. Clin. Exp. Dent. 2022, 14, e746–e755. [Google Scholar] [CrossRef]
- Inatomi, K.; Saito, H.; Endo, T. Bond strength of indirect bonded brackets in orthodontic adhesives with different viscosities. Dent. Mater. J. 2021, 40, 439–445. [Google Scholar] [CrossRef]
- Pamukcu, H.; Ozsoy, O.P.; Dagalp, R. In vitro and in vivo comparison of orthodontic indirect bonding resins: A prospective study. Niger. J. Clin. Pract. 2018, 21, 614–623. [Google Scholar] [CrossRef]

| Items | Bracket Bonded Teeth | Bonding Failure | Position Error | Total Re-Bonding | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Total | 2531 | 382 | 15.09 | 191 | 7.55 | 573 | 22.64 |
| Maxilla | 1277 | 144 | 37.70 | 97 | 50.78 | 241 | 42.06 |
| Mandible | 1254 | 238 | 62.30 | 94 | 49.21 | 332 | 57.94 |
| Male | 930 | 166 | 17.85 | 97 | 10.43 | 263 | 28.28 |
| Female | 1601 | 216 | 13.49 | 94 | 5.87 | 310 | 19.36 |
| <20 years | 1183 | 217 | 18.34 | 123 | 10.40 | 340 | 28.74 |
| >20 years | 1348 | 165 | 12.24 | 68 | 5.04 | 233 | 17.28 |
| Skeletal Class I | 782 | 114 | 14.58 | 55 | 7.03 | 169 | 21.61 |
| Skeletal Class III | 1093 | 165 | 15.10 | 83 | 7.59 | 248 | 22.69 |
| Skeletal Class III | 656 | 103 | 15.70 | 53 | 8.08 | 156 | 23.78 |
| Hyperdivergency | 779 | 141 | 18.10 | 48 | 6.16 | 189 | 24.26 |
| Normodivergency | 1066 | 149 | 13.98 | 85 | 7.97 | 234 | 21.95 |
| Hypodivergency | 686 | 92 | 13.41 | 58 | 8.45 | 150 | 21.87 |
| Initial stage | 2531 | 170 | 6.72 | 16 | 0.63 | 186 | 7.35 |
| Middle stage | 2531 | 175 | 6.91 | 133 | 5.25 | 308 | 12.17 |
| Late stage | 2531 | 37 | 1.46 | 42 | 1.66 | 79 | 3.12 |
| Incisors and canines | 1275 | 169 | 13.25 | 137 | 10.75 | 306 | 24.00 |
| Premolars | 652 | 94 | 14.42 | 28 | 4.29 | 122 | 18.71 |
| Molars | 707 | 119 | 16.83 | 26 | 3.68 | 145 | 20.51 |
| Items | Bonding Failure | Position Error | Total Re-Bonding | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Site | Total | Site | Total | Site | Total | |||||||||
| Anterior | Premolar | Molar | Anterior | Premolar | Molar | Anterior | Premolar | Molar | ||||||
| Arch | Maxilla | Count | 43 | 45 | 56 | 144 | 75 | 12 | 10 | 97 | 118 | 57 | 66 | 241 |
| Expected count | 63.71 | 35.43 | 44.86 | 144 | 69.58 | 14.22 | 13.20 | 97 | 128.70 | 51.31 | 60.99 | 241 | ||
| Proportion within an arch (%) | 29.86 | 31.25 | 38.89 | 100.00 | 77.32 | 12.37 | 10.31 | 100.00 | 48.96 | 23.65 | 27.39 | 100.00 | ||
| Proportion within site (%) | 25.44 | 47.87 | 47.06 | 37.70 | 54.74 | 42.86 | 38.46 | 50.79 | 38.56 | 46.72 | 45.52 | 42.06 | ||
| The proportion of the total (%) | 11.26 | 11.78 | 14.66 | 37.70 | 39.27 | 6.28 | 5.24 | 50.79 | 20.59 | 9.95 | 11.52 | 42.06 | ||
| Mandible | Count | 126 | 49 | 63 | 238 | 62 | 16 | 16 | 94 | 188 | 65 | 79 | 332 | |
| Expected count | 105.29 | 58.57 | 74.14 | 238 | 67.42 | 13.78 | 12.79 | 94 | 177.29 | 70.69 | 84.01 | 332 | ||
| Proportion within an arch (%) | 52.94 | 20.59 | 26.47 | 100.00 | 65.96 | 17.02 | 17.02 | 100.00 | 56.63 | 19.58 | 23.80 | 100.00 | ||
| Proportion within site (%) | 74.56 | 52.13 | 52.94 | 62.30 | 45.26 | 57.14 | 61.54 | 49.21 | 61.44 | 53.28 | 54.48 | 57.94 | ||
| The proportion of the total (%) | 32.98 | 12.83 | 16.49 | 62.30 | 32.46 | 8.38 | 8.38 | 49.21 | 32.81 | 11.34 | 13.79 | 57.94 | ||
| Total | Count | 169 | 94 | 119 | 382 | 137 | 28 | 26 | 191 | 306 | 122 | 145 | 573 | |
| Expected count | 169 | 94 | 119 | 382 | 137 | 28 | 26 | 191 | 306 | 122 | 145 | 573 | ||
| Proportion within an arch (%) | 44.24 | 24.61 | 31.15 | 100.00 | 71.73 | 14.66 | 13.61 | 100.00 | 53.40 | 21.29 | 25.31 | 100.00 | ||
| Proportion within site (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | ||
| The proportion of the total (%) | 44.24 | 24.61 | 31.15 | 100.00 | 71.73 | 14.66 | 13.61 | 100.00 | 53.40 | 21.29 | 25.31 | 100.00 | ||
| Pearson Chi-Square | 0.000 ** | 0.208 | 0.189 | |||||||||||
| Variables | Bonding Failure | Position Failure | Total Re-Bonding | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | |||||
| Sex | Male | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . |
| Female | −0.28 | −0.51 | −0.05 | 0.0150 * | −0.62 | −0.93 | −0.30 | 0.0001 ** | −0.39 | −0.58 | −0.21 | <0.0001 ** | |
| Age | <20 years | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . |
| >20 years | −0.49 | −0.70 | −0.28 | <0.0001 ** | −0.79 | −1.10 | −0.48 | <0.0001 ** | −0.58 | −0.76 | −0.41 | <0.0001 ** | |
| Skeletal classification | I | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . |
| II | 0.04 | −0.20 | 0.28 | 0.7675 | 0.09 | −0.25 | 0.44 | 0.5988 | 0.05 | −0.14 | 0.25 | 0.5860 | |
| III | 0.18 | −0.09 | 0.45 | 0.2012 | 0.19 | −0.19 | 0.58 | 0.3295 | 0.18 | −0.04 | 0.40 | 0.1119 | |
| Divergency | Hyperdivergency | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | . |
| Normodivergency | −0.33 | −0.58 | −0.08 | 0.0087 ** | 0.01 | −0.37 | 0.40 | 0.9446 | −0.23 | −0.43 | −0.02 | 0.0322 * | |
| Hypodivergency | −0.30 | −0.60 | −0.01 | 0.0439 * | 0.14 | −0.29 | 0.58 | 0.5133 | −0.16 | −0.40 | 0.08 | 0.1882 | |
| Variables | Bonding Failure | Position Failure | Total Re-Bonding | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | Estimate | 95% CI | p-Value | ||||
| Initial stage | 0.000 | . | . | . | 0.000 | . | . | . | 0.000 | . | . | . |
| Middle stage | 0.012 | 0.007 | 0.018 | <0.0001 ** | 0.024 | 0.020 | 0.028 | <0.0001 ** | 0.036 | 0.030 | 0.043 | <0.0001 ** |
| Late stage | −0.015 | −0.021 | −0.009 | <0.0001 ** | 0.006 | 0.002 | 0.010 | 0.0039 ** | −0.009 | −0.016 | −0.002 | 0.0070 ** |
| Incisors and Canine | 0.000 | . | . | . | 0.000 | . | . | . | 0.000 | . | . | . |
| Premolars | 0.000 | −0.009 | 0.008 | 0.9057 | −0.010 | −0.015 | −0.005 | 0.0001 ** | −0.011 | −0.020 | −0.002 | 0.0222 ** |
| Molars | 0.004 | −0.004 | 0.012 | 0.3651 | −0.011 | −0.016 | −0.006 | <0.0001 ** | −0.008 | −0.017 | 0.002 | 0.1058 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bai, J.; Lee, H.-J.; Kim, S.-H. Evaluation of the Failure Rate and Clinical Efficacy of Orthodontic Brackets Indirect Bonding with Computer-Aided Transfer Jig System: An In Vivo Study. Appl. Sci. 2023, 13, 1668. https://doi.org/10.3390/app13031668
Bai J, Lee H-J, Kim S-H. Evaluation of the Failure Rate and Clinical Efficacy of Orthodontic Brackets Indirect Bonding with Computer-Aided Transfer Jig System: An In Vivo Study. Applied Sciences. 2023; 13(3):1668. https://doi.org/10.3390/app13031668
Chicago/Turabian StyleBai, Jin, Hye-Jin Lee, and Seong-Hun Kim. 2023. "Evaluation of the Failure Rate and Clinical Efficacy of Orthodontic Brackets Indirect Bonding with Computer-Aided Transfer Jig System: An In Vivo Study" Applied Sciences 13, no. 3: 1668. https://doi.org/10.3390/app13031668
APA StyleBai, J., Lee, H.-J., & Kim, S.-H. (2023). Evaluation of the Failure Rate and Clinical Efficacy of Orthodontic Brackets Indirect Bonding with Computer-Aided Transfer Jig System: An In Vivo Study. Applied Sciences, 13(3), 1668. https://doi.org/10.3390/app13031668








