Abstract
This case report describes an 18-year-old female patient with a skeletal class I pattern, mandibular asymmetry, a molar class III on the right side, a molar class II on the left side, and an anterior open bite (AOB). Treatment of AOB is often difficult for orthodontists and a multidisciplinary approach is sometimes required to rehabilitate the correct function and posture of the tongue. In this case the AOB was treated using the Nuvola® OP System: a treatment system that combines orthodontic aligners and a myofunctional elastodontic device called Freedom. An upper molar intrusion with miniscrews was performed during the first phase of the treatment programme, and then the aligner treatment began. The Nuvola® OP System ’s aligners are characterized by lingual pins that guide the tongue to the palatal spot position and take advantage of tongue function. The patient was instructed to wear the Freedom device for 30 min a day and to clench every 3 s with closed lips while wearing the aligners. These exercises improve the fitting of the aligners, improve the tongue’s posture, and take advantage of the masticatory forces to resolve the malocclusion. The patient was successfully treated, thus demonstrating that the Nuvola® OP System is a valid alternative for the treatment of AOB.
1. Introduction
An anterior open bite (AOB) has a multifactorial aetiology and is caused by unfavourable growth patterns, finger sucking habits, enlarged lymphatic tissue, and genetics, among the other factors [1,2,3]. An AOB can impair several functions like speech, swallowing, chewing, and aesthetics [4], thus deteriorating social interactions and quality of life in general [5,6]. In some cases, the aetiology can be identified in incorrect habits like oral respiration or non-nutritive sucking, whose severity and impact on the malocclusion depend on duration, frequency, and severity, as well as the age of the patient [7]. There are several treatment options for reducing the aetiological factors that sustain an AOB [4,6,8,9] and for limiting the excessive vertical growth of the facial skeletal components [5,7,10].
From an orthodontic point of view, an AOB can be solved by controlling the molar eruption and through the orthodontic extrusion of the anterior teeth in growing patients [11,12]. In adult patients, orthodontic camouflage or orthognathic surgery is usually required. Of course, the treatment choice depends on the aetiology, i.e., whether the patient has a skeletal open bite pattern or not, and on the co-existence of combined local factors, such as bad habits [7,13].
The introduction of skeletal anchorage simplified the correction of an AOB [14] through the orthodontic intrusion of posterior teeth with titanium mini-plates or monocortical bone screws [7,14,15]. Skeletal anchorage promotes the intrusion of molars in their bone support and promotes the counterclockwise rotation of the jaw with the consequent closure of the bite [16].
On the other hand, the demand for orthodontic treatment with invisible appliances is constantly increasing, and therefore innovations in clear aligner therapy, which allows the resolution of even complex malocclusions, are important. Regarding the AOB, there are some case reports that have shown the successful treatment of patients with this malocclusion using different methods and appliances [17]. In some cases, clear aligners were also used [16], and some authors have shown that they are successful in controlling the vertical dimension in patients with open bite even when associated with a combination of incisor extrusion and molar intrusion, promoting the counterclockwise rotation of the jaw [18] and improving facial aesthetics [16]. According to this evidence, clear aligners can be successfully used in anterior open bite cases where the aetiology is represented by intruded anterior teeth [19,20]. In the presence of these characteristics, the combination of clear aligners with myofunctional appliances could be beneficial in AOB cases. Indeed, a study showed that clenching exercises may be effective in improving dental contacts, and this could also improve the fit of the aligners, although this has not yet been demonstrated. Moreover, myofunctional appliances showed some positive effects in tongue and labial muscle rehabilitation [5].
Therefore, taking into account this background, the aim of this article was to present a clinical case showing an AOB treated with a combination of clear aligners and a myofunctional appliance (Nuvola® OP System) and to discuss the indications and the clinical results of such a hybrid approach.
2. Case Description and Results
2.1. Diagnosis and Etiology
A young adult female, aged 18 years, visited the Orthodontic Clinic, University of L’Aquila in December 2018; her chief complaint was regarding a lack of tooth overlap and the non-coincidence of the upper and lower midlines. Although aware of her malocclusion, the patient reported that she had not undergone any orthodontic treatment previously, because she had always been recommended traditional orthodontic treatments with a fixed multibracket appliance, which was not acceptable to her. The patient had asked for a completely invisible appliance, without metal brackets, and had also refused the use of lingual brackets.
The patient’s medical history was collected, and a complete clinical examination was performed.
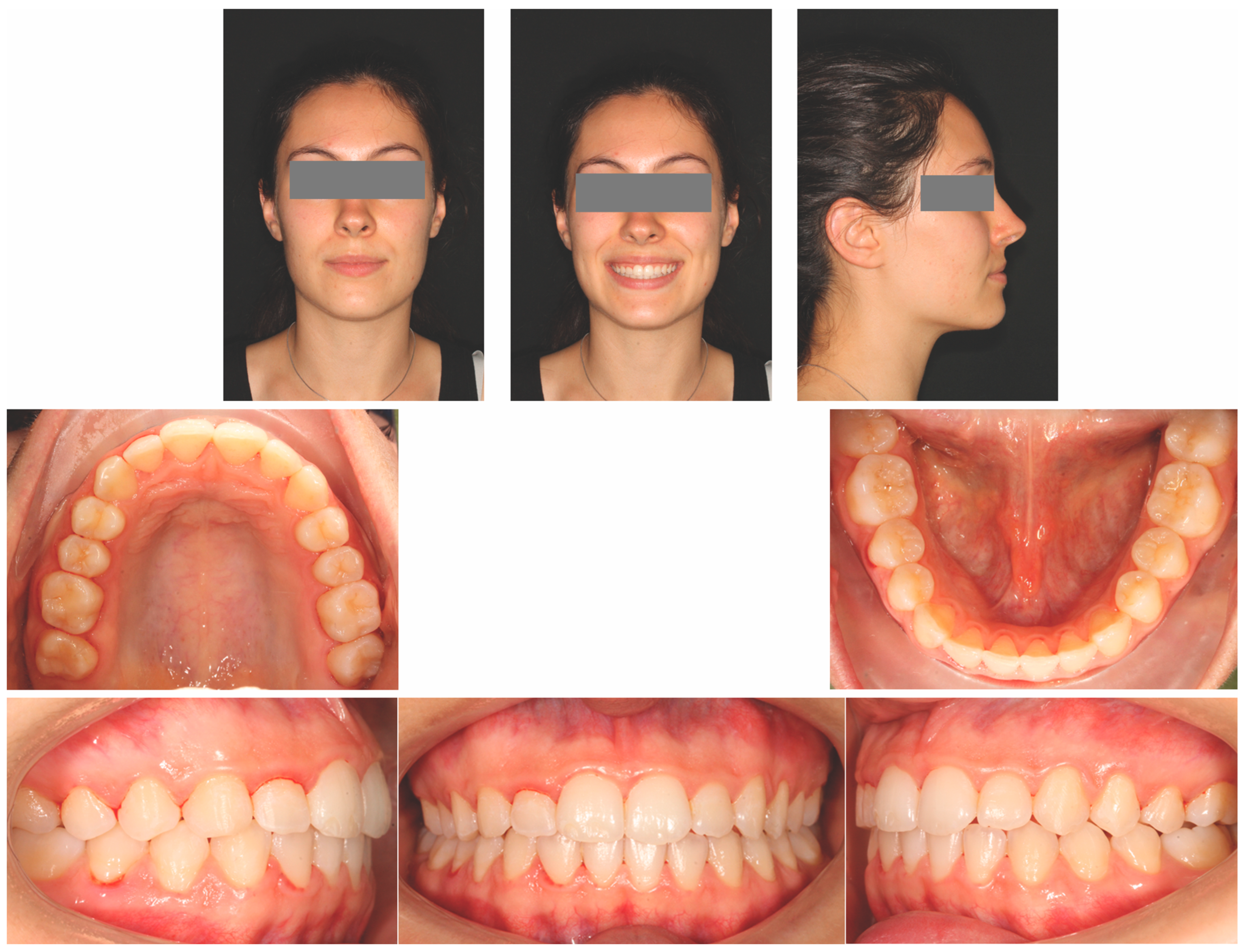
The extra-oral evaluation showed that the profile appeared harmonic although slightly convex. A slight skeletal laterodeviation of the chin was detectable; nevertheless, the anamnesis and the clinical examination revealed sound and healthy temporomandibular joints. The smile analysis showed a wide dental exposure from molar to molar with a slightly increased gingival display, non-coincidence of the dental midlines, and an anterior open bite of 3 millimetres. The upper midline was centred on the facial midline, while the lower midline was shifted to the left by 1.5 millimetres (Figure 1).

Figure 1.
Pre-treatment facial and intraoral photographs.
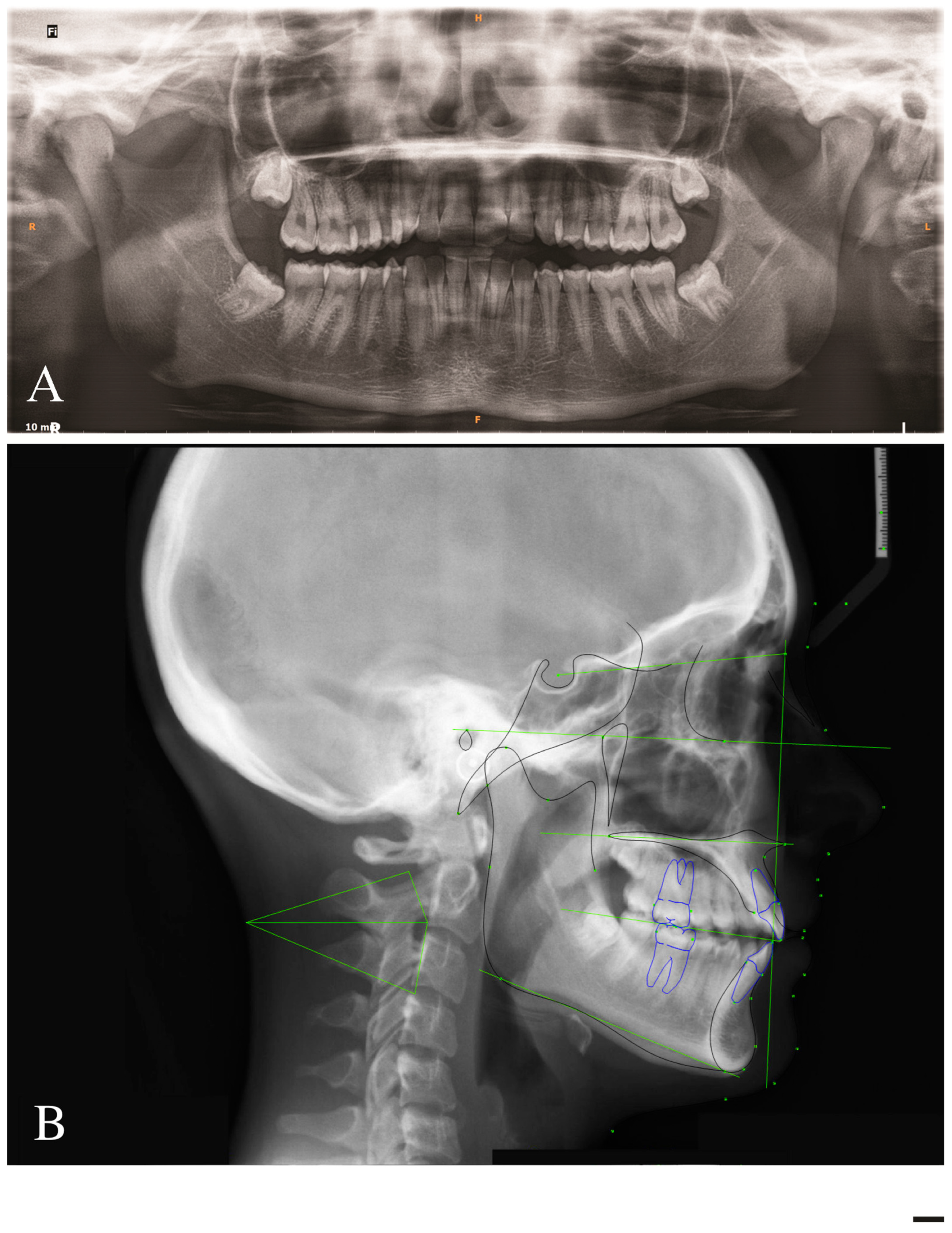
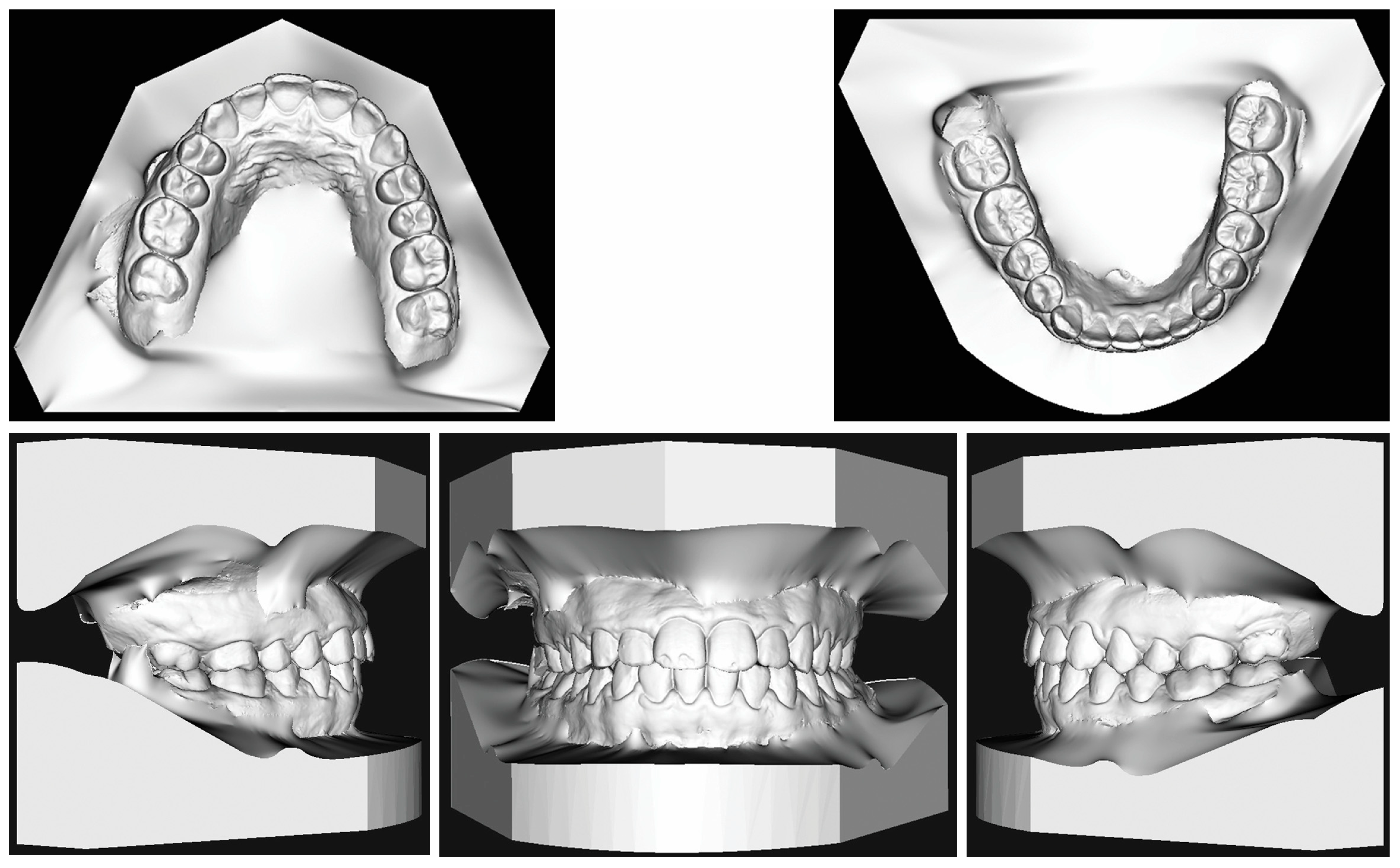
The intraoral analysis showed the presence of all permanent teeth except for the third maxillary and mandibular molars. The patient had a molar and canine class III relationship on the right side and a molar and canine class II relationship on the left side, due to the mandibular laterodeviation. There were 2.2 millimetres of crowding in the upper arch and 1.2 millimetres of crowding in the lower arch; the upper anterior segment was the most crowded, and the pre-treatment cephalometric analysis performed with cephalometric software (Dolphin Imaging System, version 11.9, Canoga Park, Calif) showed a skeletal class I, with an ANB of −0.2° and a WITS of −2.0 mm (Figure 2) (Table 1). Vertical parameters showed a normodivergent pattern. Dental measurements showed a more forward inclination of the upper (U1-Palatal Plane = 117.2°) and lower incisors (IMPA = 96.9°).
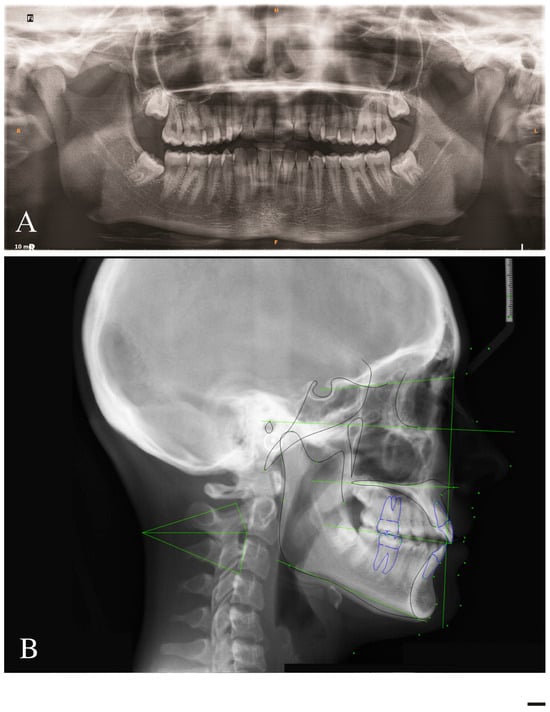
Figure 2.
(A): Pre-treatment panoramic. (B): Pre-treatment lateral radiograph.

Table 1.
Cephalometric analysis.
In conclusion, it could be stated that the patient’s AOB was a dental open bite. In addition, the lower third molars were impacted and mesio-inclinated.
2.2. Treatment Objectives
Following the diagnosis of a dental open bite with asymmetrical molar and canine sagittal relationship and a dental midlines shift, the treatment objectives were to: (1) align and level the dental arches; (2) resolve the AOB; (3) alleviate the gummy smile; (4) obtain acceptable midline coincidence; (5) provide harmonious dental intercuspation.
An AOB can be corrected either by the extrusion of anterior teeth or by the intrusion of posterior teeth to allow the jaw to rotate counterclockwise. In this case, since excessive gingival exposure was already present, the extrusion of the anterior teeth had to be limited to avoid any worsening of the gummy smile. The orthodontic mechanics were aimed mainly at levelling the upper jaw by selective intrusion of the posterior teeth; this solution prevents the extrusion of the upper incisors and allows for the rotation of the mandible in a counterclockwise direction. In this case, this movement had to be well controlled to avoid a more forward inclination of the lower incisors and inversion of the bite, which could have resulted from the mandibular counterclockwise rotation.
2.3. Treatment Alternatives
To achieve all the aforementioned treatment objectives, several treatment options were presented to the patient:
- (1)
- Orthognathic surgery was presented as the ideal treatment option to improve the profile aesthetics, to correct the mandibular laterodeviation, and to resolve the gummy smile.
- (2)
- Alternatively, skeletal maxillary expansion was proposed through surgically-assisted or miniscrew-assisted rapid palatal expansion—with an explanation of the pros and cons of both procedures, as well as the difference in scientific evidence supporting both options—followed by fixed appliance treatment with asymmetric elastics, with the purpose of correcting the mandibular laterodeviation, at least from a dentoalveolar point of view.
- (3)
- To correct the patient’s malocclusion while embracing the patient’s request to have an aesthetic treatment, a lingual fixed appliance was proposed.
- (4)
- The last treatment option proposed to the patient was orthodontic therapy with clear aligners and elastodontic devices (Nuvola® OP System), combined with miniscrews and a transpalatal arch (TPA) to allow controlled intrusion of the posterior molars.
Since the patient refused any orthognathic surgery, palatal expansion with miniscrew-supported devices, and lingual fixed appliances, the latter treatment option was chosen. The Nuvola® OP System involves a combination of clear aligners and myofunctional devices as a complete system to properly reconfigure the dental physiology as well as the occlusal planes.
Anatomical reinforcements and pins are inserted into the aligners and should allow the transmission of axial forces to dental groups, with the purpose of helping the expansion of the dental arch, even in asymmetric arches.
The aligners also have two lingual pins placed on both sides of the retro-incisive papilla, which are designed to generate proprioceptive stimulation of the tongue according to the principles of myofunctional therapy. The patient must use the myofunctional appliance (Freedom) for 30 min a day, performing 3-s-long clenches, alternated with 3 s of relaxation.
The extraction of the lower third molars was proposed to the patient, who refused, despite being informed about the possible sequelae, because she was afraid of surgical procedures. It was then decided to regularly monitor the conditions of the lower third molars.
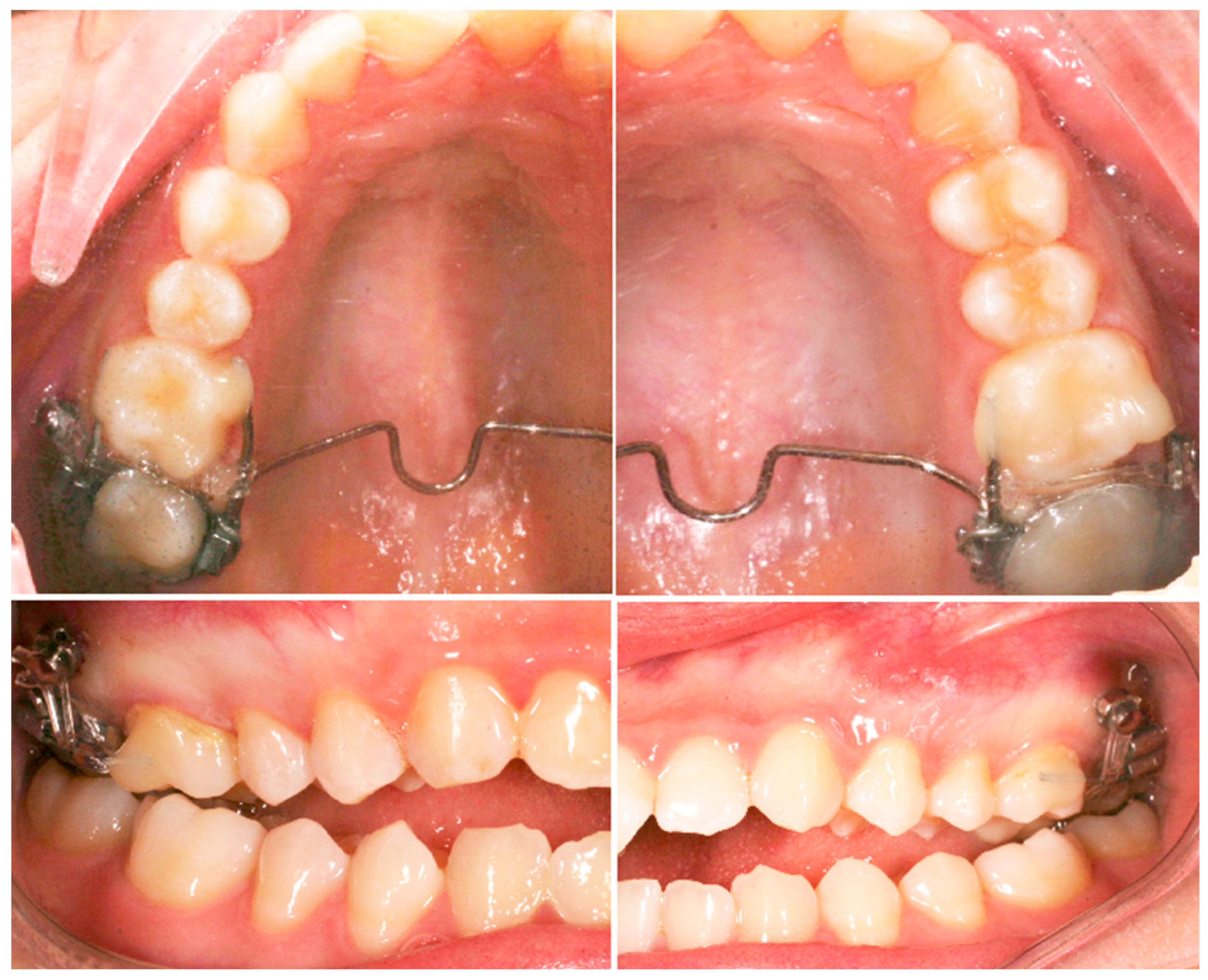
2.4. Treatment Progress
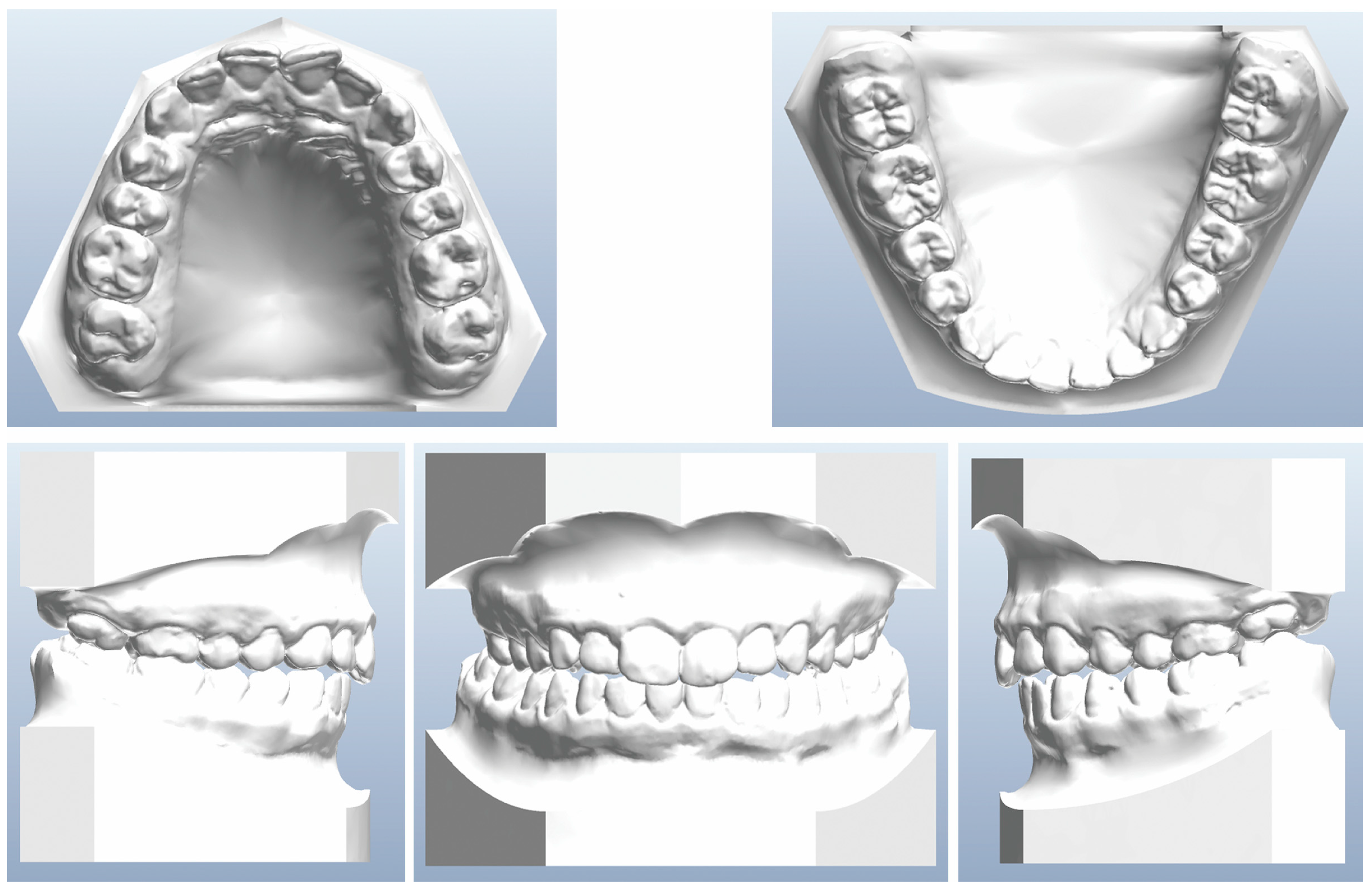
Before beginning the use of clear aligners, intrusion of the posterior teeth with skeletal anchorage was planned. Two miniscrews were inserted in the left and right sides of the upper arch between the first and second molars; this area was chosen because the cortical bone has an adequate thickness that does not require predrilling [21] even though it is not considered a safe zone for miniscrew insertion [22]. After insertion of the miniscrews, a TPA with a distal loop and molar bands for the upper second molars were placed, along with palatal and vestibular segmented 0.019 × 0.025 stainless steel wires connecting the first and second molars on each side (Figure 3). The intrusion force was applied by an elastomeric chain tied from the sectional arch to the miniscrew. At the end of the intrusion phase of the upper molars, new orthodontic records were collected, along with digital impressions of the dental arches taken with an intraoral scanner, to plan the treatment phase with clear aligners (Figure 4).
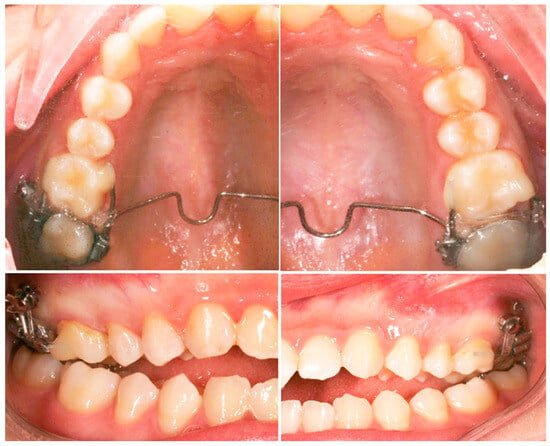
Figure 3.
Intraoral photographs of the first treatment phase with TPA.
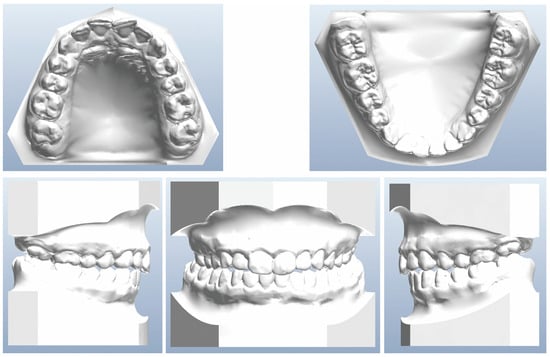
Figure 4.
Dental casts before clear aligner treatment.
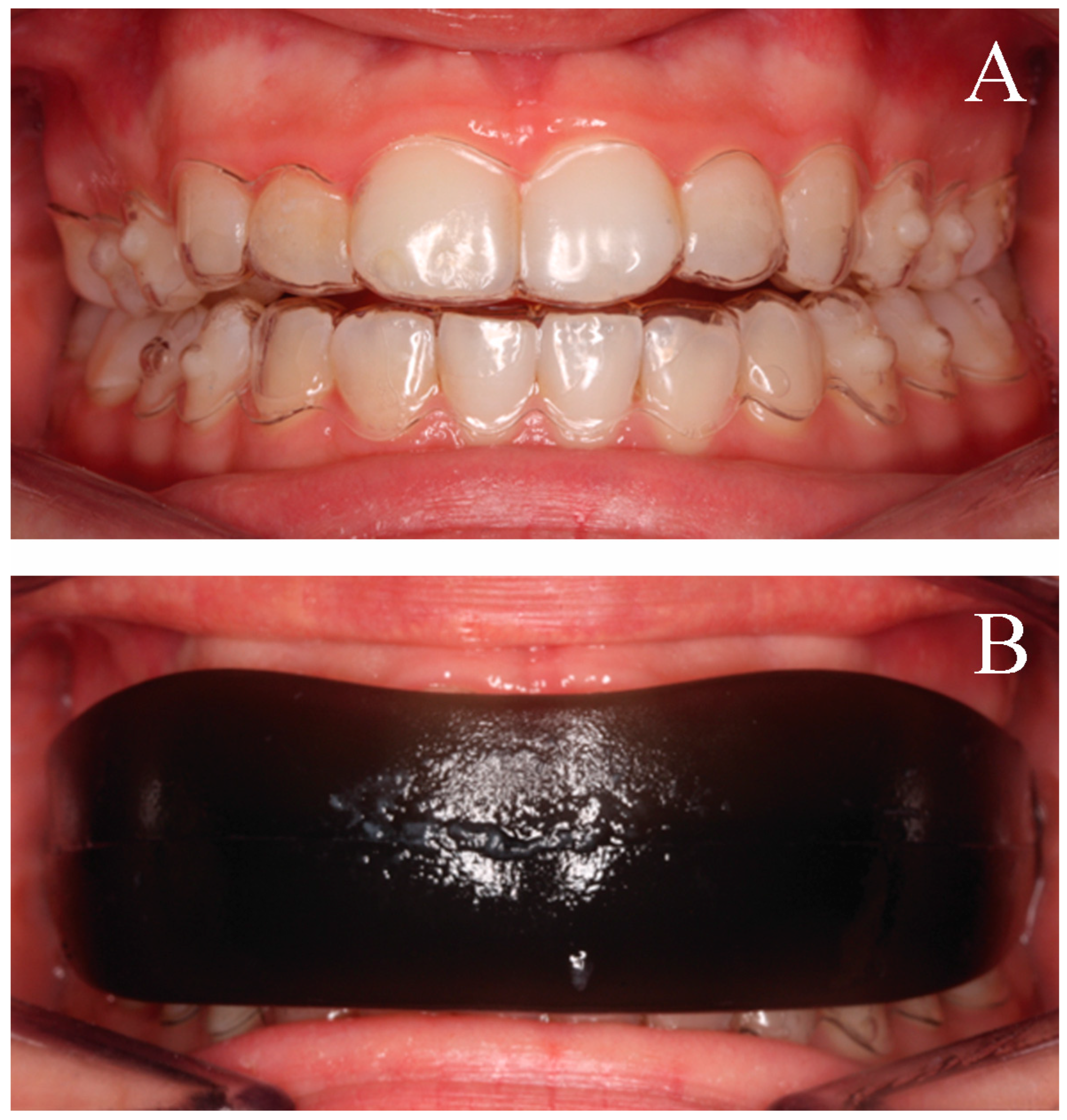
The first phase of therapy involved 18 aligners in the upper and lower arch. The patient was instructed to wear the aligners for at least 22 h a day and to change the set of clear aligners every 15 days. Inter-proximal reduction (IPR) of 0.10 mm was performed between the upper and lower incisors before the third and the sixth aligner. The patient was also given the myofunctional Freedom device to be used daily while wearing the aligners, performing 3-s-long clenching exercises with closed lips for a total of 30 min per day (Figure 5). At the end of the first phase of 18 aligners, a better molar relationship was achieved, the upper incisors were slightly extruded, and the overbite improved.
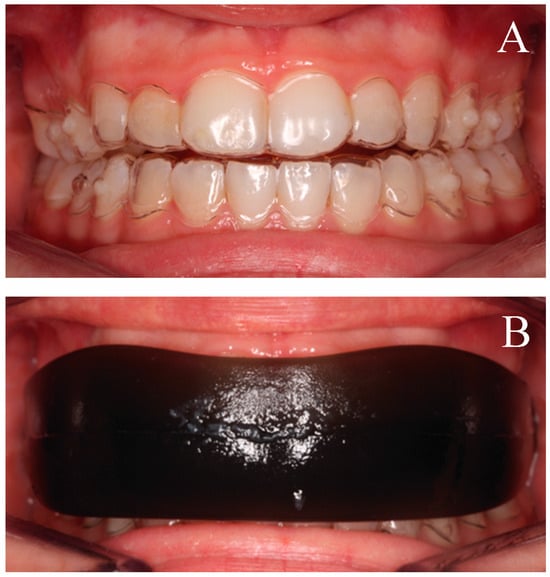
Figure 5.
(A) Intraoral photographs with clear aligners; (B) Intraoral photographs with Freedom appliance and clear aligners on.
New digital impressions were taken and a set of six refinement aligners for the upper and lower arches was planned for the correction of the remaining crowding. The last treatment phase involved the use of class III elastics on the left side and vertical intercuspation elastics on the right side to optimize the molar and canine relationships and to correct the dental midlines (Figure 6). Once the sagittal relationship was fully corrected, intercuspation elastics were used on both sides to improve occlusal settling at the level of the canines and first premolars: silicone moulds were used to place composite buttons on the buccal face of the crowns of the upper cuspid, lower cuspid, and lower first bicuspid, and elastics were used full-time for 3 weeks without aligners.

Figure 6.
Intraoral photographs of the finishing phase with interclass elastics.
Removable orthodontic upper and lower essix retainers were given to the patient at the end of treatment, and she was instructed to use them overnight every night.
2.5. Treatment Results
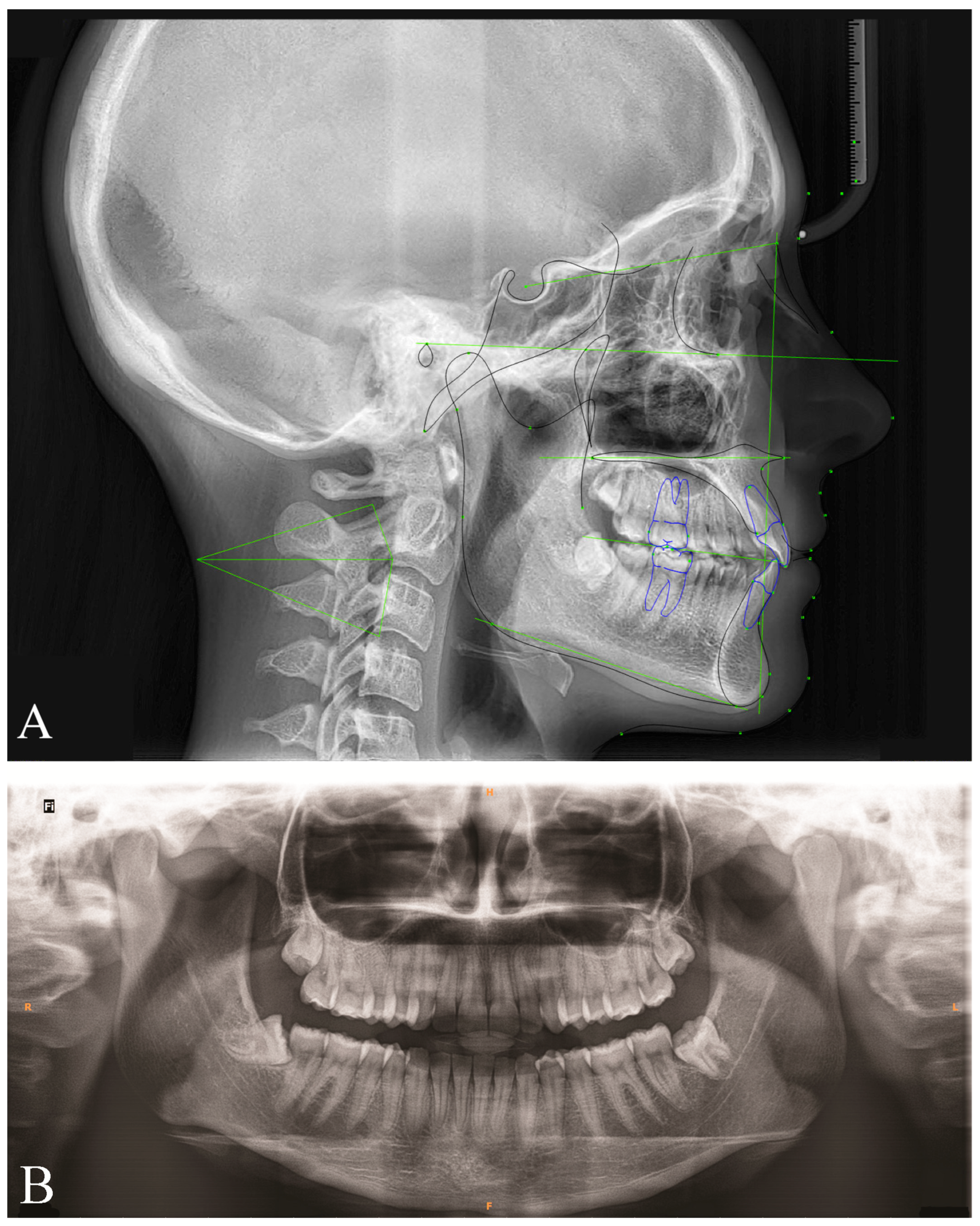
At the end of treatment, the AOB and the crowding were completely resolved, while the gingival exposure was stable (Figure 7 and Figure 8). Analysis of the pre- and post-treatment tracing superimposition showed that miniscrews were effective at achieving the intrusion of the upper second molars, while aligners provided one additional millimetre of first molar intrusion [23] which led to an improvement of overbite of a further two millimetres. Overall, these changes resulted in a significant mandibular counterclockwise rotation that led to the correction of the AOB, without impacting the exposure of the upper incisors. Moreover, the post-treatment cephalometric analysis showed an improvement of the upper and lower incisors’ inclination: U1-Palatal plane = 112.4° and IMPA = 94.7° (Figure 9) (Table 1). The midline discrepancy was also corrected. The whole treatment lasted 17 months. In the first 4 months, only a palatal arch and miniscrews were used, while treatment with the Nuvola® OP System lasted the remaining 13 months. At the end of the treatment programme, the patient showed a correct intercuspidation, normal overjet and overbite, and she was pleased with the entire treatment and the final result. At the 15-month clinical follow-up, the treatment result was stable, and the midline coincidence was maintained (Figure 10).

Figure 7.
Post-treatment facial and intraoral photographs.
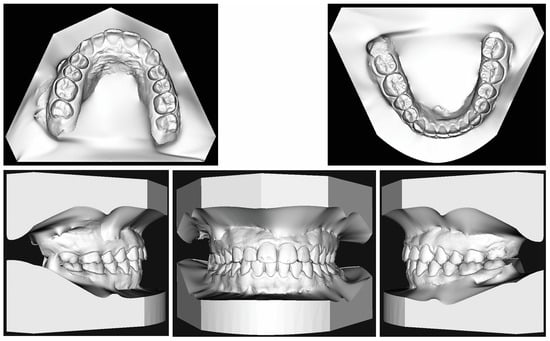
Figure 8.
Post-treatment dental casts.
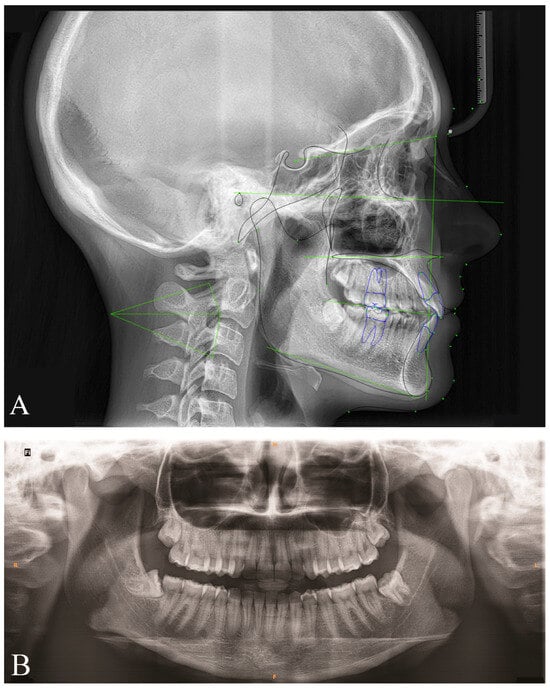
Figure 9.
(A): Post-treatment lateral radiograph. (B): Post-treatment panoramic.

Figure 10.
15-month follow up intraoral photographs.
3. Discussion
Patients with dentofacial malocclusions are disadvantaged in society due to low self-confidence associated with physiological problems [24]. An open bite compromises the social behaviour of the individual in multiple ways, thus influencing the quality of life [6,7]. Consequently, the concern for aesthetics motivates patients with an AOB to seek an orthodontic treatment that is effective while being invisible. Knowledge of the main complaints and expectations of the patient, as well as adequate diagnostic examinations, is important when deciding the ideal treatment plan and achieving a satisfactory result [25]. In the present case, clear aligner treatment was chosen to provide a more comfortable and aesthetic treatment [26], but also because the patient’s compliance and attitude towards orthodontic treatment were excellent. Indeed, different studies have revealed that treatment with clear aligners is well supported by patients because of its minimum aesthetic impact [27,28] and that this technique is even preferred over lingual fixed appliances because the latter causes oral dysfunctions like tongue injuries [28]. Despite their advantage in terms of comfort, clear aligners are not as effective as braces in creating adequate occlusal contacts and controlling root torque [29], even if clinical outcomes are usually comparable to the planning of the digital setup in regard to torque movements of the anterior teeth [30]. However, even though clear aligners can be a successful alternative to fixed appliances to treat patients with mild to moderate malocclusion [31], more complex movements are less predictable, especially vertical movements [32]. For these reasons, in the present case report clear aligners were combined with different auxiliary appliances (TPA, miniscrews, myofunctional appliances, vertical elastics) to predictably obtain molar intrusion and AOB correction. During treatment, IPR was performed to gain space in both dental arches, taking care to perform the exact amount of IPR planned [33]. This treatment option was presented as a compromise treatment compared to orthognathic surgery. However, there is currently no consensus on whether surgical or non-surgical treatment is the most stable approach to treat AOB in adult patients. Of course, the stability of the orthodontic treatment is influenced by aetiological factors and their persistence over time [34]. Because of the frequency of relapse [35], it is essential to evaluate, beyond immediate post-treatment results, the achievement of long-term stability [36]. Many authors have shown that after a few years there is a return to the original configuration both at the molar level and at the level of the upper and lower incisors, of varying degrees [25]. AOB treatment through molar intrusion using skeletal anchorage in adult patients can be considered quite unstable, since a relapse of up to 30% can be observed for both molars [37]. Therefore, more efficient methods of retention should be kept in the long-term follow-up [37]. For AOB cases, tongue rehabilitation is very important, because tongue thrusting is always associated—even though it is not always an aetiological factor—with this kind of malocclusion [38,39] and the stability of the orthodontic result is dependent on the persistence or not of aetiological factors [6].
Regarding the use of the elastodontic device, Uchida et al. investigated the impact that daily clenching had on occlusal contacts and found that voluntary clenching is an effective training exercise to intensify the vertical effects on posterior teeth and to improve the occlusal contact area and the occlusal sagittal balance in normal subjects [39]. In particular, they demonstrated that clenching exercises on soft bite blocks with the protocol presented in this case report (3-s isometric contractions over 30 min per day) are able to increase the amount of tooth contacts even after only 8 weeks. Similarly, it was shown that training in adults with hard chewing gum influenced the functional capacity of the masticatory muscles and increased muscle strength, particularly in those with weak muscles [40], such as hyperdivergent patients with AOB [41]. In summary, the existing evidence and the present case report—with all its limitations—seem to support the idea that muscle rebalancing and training are important for treatment outcomes and for treatment stability. Increasing muscular tone and the amount of occlusal contact could prevent teeth extrusion and thus bite re-opening. Moreover, the orofacial myofunctional therapy seems able to create a new neuromuscular pattern and to resolve the incorrect functional and resting postures of the tongue, by improving its muscular proprioception, mobility, and strength [42]. In this way, it is possible to intervene in the aetiological factors and to increase the predictability and stability of the orthodontic treatment.
4. Conclusions
The present case report showed how the simultaneous action of clear aligners and a myofunctional appliance (Nuvola® OP System), together with miniscrews, led to a satisfactory resolution of AOB. The treatment results were stable at the 15-month follow-up. Even if the use of myofunctional appliances is not common in adult patients, the synergic action of these devices resulted in significant molar intrusion and mandibular autorotation, the rehabilitation of tongue function, and an increase in the tone of the elevator muscles. In conclusion, the present case report suggests that the combined use of a myofunctional appliance with clear aligners should be considered for the treatment of adult patients with similar malocclusions. Further clinical trials are recommended in order to investigate the benefits that this kind of approach can provide and to what extent those benefits would balance the limitations, such as the additional costs and the increased compliance required.
Author Contributions
M.T. Treated the patient, defined the protocol, and revised the manuscript; M.I.P. treated the patient and collected the data; R.E. collected the data and drafted the manuscript; E.S. revised the manuscript; D.C. revised the manuscript and supervised the study. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written consent was obtained from the patient.
Data Availability Statement
The additional data are available by contacting the corresponding author after reasonable request.
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Beane, R.A.; Reimann, G.; Phillips, C.; Tulloch, C. A cephalometric comparison of black open-bite subjects and black normal. Angle Orthod. 2003, 73, 294–300. [Google Scholar] [CrossRef]
- Cangialosi, T. Skeletal morphologic features of anterior open bite. Am. J. Orthod. 1984, 85, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Asiry, M.A.; AlShahrani, I. Prevalence of malocclusion among school children of Southern Saudi Arabia. J. Orthod. Sci. 2019, 8, 2. [Google Scholar] [CrossRef]
- Lentini-Oliveira, D.A.; Carvalho, F.R.; Rodrigues, C.G.; Ye, Q.; Hu, R.; Minami-Sugaya, H.; Carvalho, L.B.; Prado, L.B.; Prado, G.F. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst. Rev. 2014, 2014, CD005515. [Google Scholar] [CrossRef] [PubMed]
- Cozza, P.; Baccetti, T.; Franchi, L.; Mucedero, M.; Polimeni, A. Sucking habits and facial hyperdivergency as risk factors for anterior open bite in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 517–519. [Google Scholar] [CrossRef] [PubMed]
- Xun, C.; Zeng, X.; Wang, X. Microscrew anchorage in skeletal anterior open-bite treatment. Angle Orthod. 2007, 77, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Rizzatto, S.; Allgayer, S.; Menezes, L.; Lima, E. Tratamento da deformidade maxilar decorrente de hábitos deletérios: Relato de caso. Rev. Clin. Ortod. Dent. Press. 2011, 10, 106–115. [Google Scholar]
- Cozza, P.; Baccetti, T.; Franchi, L.; Mucedero, M. Comparison of 2 early treatment protocols for open-bite malocclusions. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 743–747. [Google Scholar] [CrossRef]
- Bianchi, J.; Pinto, A.d.S.; Ignácio, J.; Obelenis Ryan, D.P.; Gonçalves, J.R. Effect of temporomandibular joint articular disc repositioning on anterior open-bite malocclusion: An orthodontic-surgical approach. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 848–858. [Google Scholar] [CrossRef]
- Buschang, P.H.; Sankey, W.; English, J.P. Early treatment of hyperdivergent open-bite malocclusions. Semin. Orthod. 2002, 8, 130–140. [Google Scholar] [CrossRef]
- Bueno Medeiros, R.; Cardoso de Araújo, L.F.; Mucha, J.N.; Trindade Motta, A. Stability of open-bite treatment in adult patients: A systematic review. J. World Fed. Orthod. 2012, 1, 97–101. [Google Scholar] [CrossRef]
- Sherwood, K.H.; Burch, J.G.; Thompson, W.J. Closing anterior open bites by intruding molars with titanium miniplate anchorage. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Erverdi, N.; Usumez, S.; Solak, A. New generation open-bite treatment with zygomatic anchorage. Angle Orthod. 2006, 76, 519–526. [Google Scholar] [CrossRef]
- Park, H.S.; Kwon, O.W.; Sung, J.H. Nonextraction treatment of an open bite with microscrew implant anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 391–402. [Google Scholar] [CrossRef]
- Alsafadi, A.S.; Alabdullah, M.M.; Saltaji, H.; Abdo, A.; Youssef, M. Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: A systematic review. Prog. Orthod. 2016, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Giancotti, A.; Garino, F.; Mampieri, G. Use of clear aligners in open bite cases: An unexpected treatment option. J. Orthod. 2017, 44, 114–125. [Google Scholar] [CrossRef]
- Harris, K.; Ojima, K.; Dan, C.; Upadhyay, M.; Alshehri, A.; Kuo, C.-L.; Mu, J.; Uribe, F.; Nanda, R. Evaluation of open bite closure using clear aligners: A retrospective study. Prog. Orthod. 2020, 21, 23. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofacial Res. 2020, 23, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.R. Treatment of a twice-relapsed anterior open bite using temporary anchorage devices, myofunctional therapy, and fixed passive self-ligating appliances. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 832–842. [Google Scholar] [CrossRef] [PubMed]
- Tepedino, M.; Cattaneo, P.M.; Niu, X.; Cornelis, M.A. Interradicular sites and cortical bone thickness for miniscrew insertion: A systematic review with meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 783–798.e20. [Google Scholar] [CrossRef]
- Tepedino, M.; Cornelis, M.A.; Chimenti, C.; Cattaneo, P.M. Correlation between tooth size-arch length discrepancy and interradicular distances measured on CBCT and panoramic radiograph: An evaluation for miniscrew insertion. Dent. Press J. Orthod. 2018, 23, 39.e1–39.e13. [Google Scholar] [CrossRef] [PubMed]
- d’Apuzzo, F.; Perillo, L.; Carrico, C.K.; Castroflorio, T.; Grassia, V.; Lindauer, S.J.; Shroff, B. Clear aligner treatment: Different perspectives between orthodontists and general dentists. Prog Orthod. 2019, 20, 10. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Jorge, J.; Motta, T.; Marques, L.S.; Paiva, S.M.; Ramos-Jorge, M.L. Association between anterior open bite and impact on quality of life of preschool children. Braz. Oral Res. 2015, 29, 1–7. [Google Scholar] [CrossRef]
- Baek, M.S.; Choi, Y.J.; Yu, H.S.; Lee, K.J.; Kwak, J.; Park, Y.C. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 396.e1–396.e9. [Google Scholar] [CrossRef]
- Azaripour, A.; Weusmann, J.; Mahmoodi, B.; Peppas, D.; Gerhold-Ay, A.; Van Noorden, C.J.F.; Willershausen, B. Braces versus Invisalign®: Gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral Health 2015, 15, 69. [Google Scholar] [CrossRef]
- Verena Nedwed, R.-R.M. Motivation, Acceptance and Problems of Invisalign® Patients. J. Orofac. Orthop. 2005, 66, 162–173. [Google Scholar] [CrossRef]
- Shalish, M.; Cooper-kazaz, R.; Ivgi, I.; Canetti, L.; Tsur, B.; Bachar, E.; Chaushu, S. Adult patients’ a djustability to o rthodontic a ppliances. Part I: A comparison between Labial, Lingual, and InvisalignTM. Eur. J. Orthod. 2012, 34, 724–730. [Google Scholar] [CrossRef]
- Ke, Y.; Zhu, Y.; Zhu, M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Tepedino, M.; Paoloni, V.; Cozza, P.; Chimenti, C. Movement of anterior teeth using clear aligners: A three-dimensional, retrospective evaluation. Prog. Orthod. 2018, 19, 9. [Google Scholar] [CrossRef]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical effectiveness of clear aligner treatment compared to fixed appliance treatment: An overview of systematic reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- De Felice, M.E.; Nucci, L.; Fiori, A.; Flores-Mir, C.; Perillo, L.; Grassia, V. Accuracy of interproximal enamel reduction during clear aligner treatment. J. Oral. Biol. Craniofacial Res. 2019, 21, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; Takano-Yamamoto, T. Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Zuroff, J.P.; Chen, S.H.; Shapiro, P.A.; Little, R.M.; Joondeph, D.R.; Huang, G.J. Orthodontic treatment of anterior open-bite malocclusion: Stability 10 years postretention. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 302.e1–302.e8. [Google Scholar] [CrossRef]
- Ngan, P.; Fields, H.W. Open bite: A review of etiology and management. Am. Acad. Pediatr. Dent. 1997, 19, 91–98. [Google Scholar]
- González Espinosa, D.; de Oliveira Moreira, P.E.; da Sousa, A.S.; Flores-Mir, C.; Normando, D. Stability of anterior open bite treatment with molar intrusion using skeletal anchorage: A systematic review and meta-analysis. Prog. Orthod. 2020, 21, 2–14. [Google Scholar] [CrossRef]
- Dixit, U.; Shetty, R. Comparison of soft-tissue, dental, and skeletal characteristics in children with and without tongue thrusting habit. Contemp. Clin. Dent. 2013, 4, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Uchida, M.; Yamaguchi, K.; Nagano, S.; Ichida, T. Daily clenching exercise, enhances the occlusal contact. Soc. Jpn. Orthod. 2005, 64, 29–37. [Google Scholar]
- Kiliaridis, S.; Tzakis, M.G.; Carlsson, G.E. Effects of fatigue and chewing training on maximal bite force and endurance. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 372–378. [Google Scholar] [CrossRef]
- Bakke, M.; Michler, L.; Han, K.; Möller, E. Clinical significance of isometric bite force versus electrical activity in temporal and masseter muscles. Eur. J. Oral. Sci. 1989, 97, 539–551. [Google Scholar] [CrossRef]
- Mozzanica, F.; Pizzorni, N.; Scarponi, L.; Crimi, G.; Schindler, A. Impact of Oral Myofunctional Therapy on Orofacial Myofunctional Status and Tongue Strength in Patients with Tongue Thrust. Folia Phoniatr. Logop. 2021, 73, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E.; Manders, E.; Goeleven, A.; Fieuws, S.; Willems, G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).