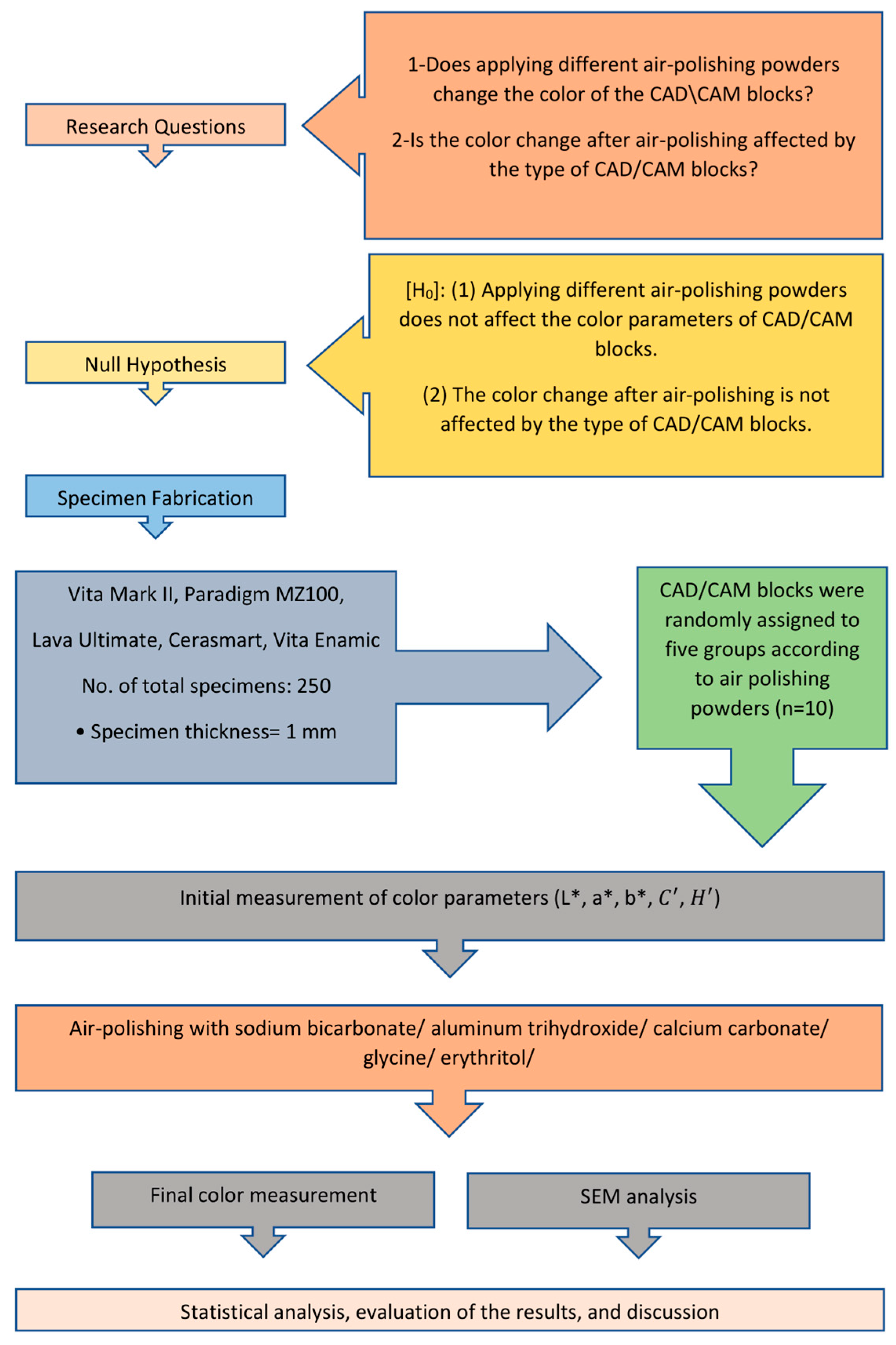
Air-Polishing Powders’ Effect on the Color of CAD/CAM Restorative Materials
Abstract
1. Introduction
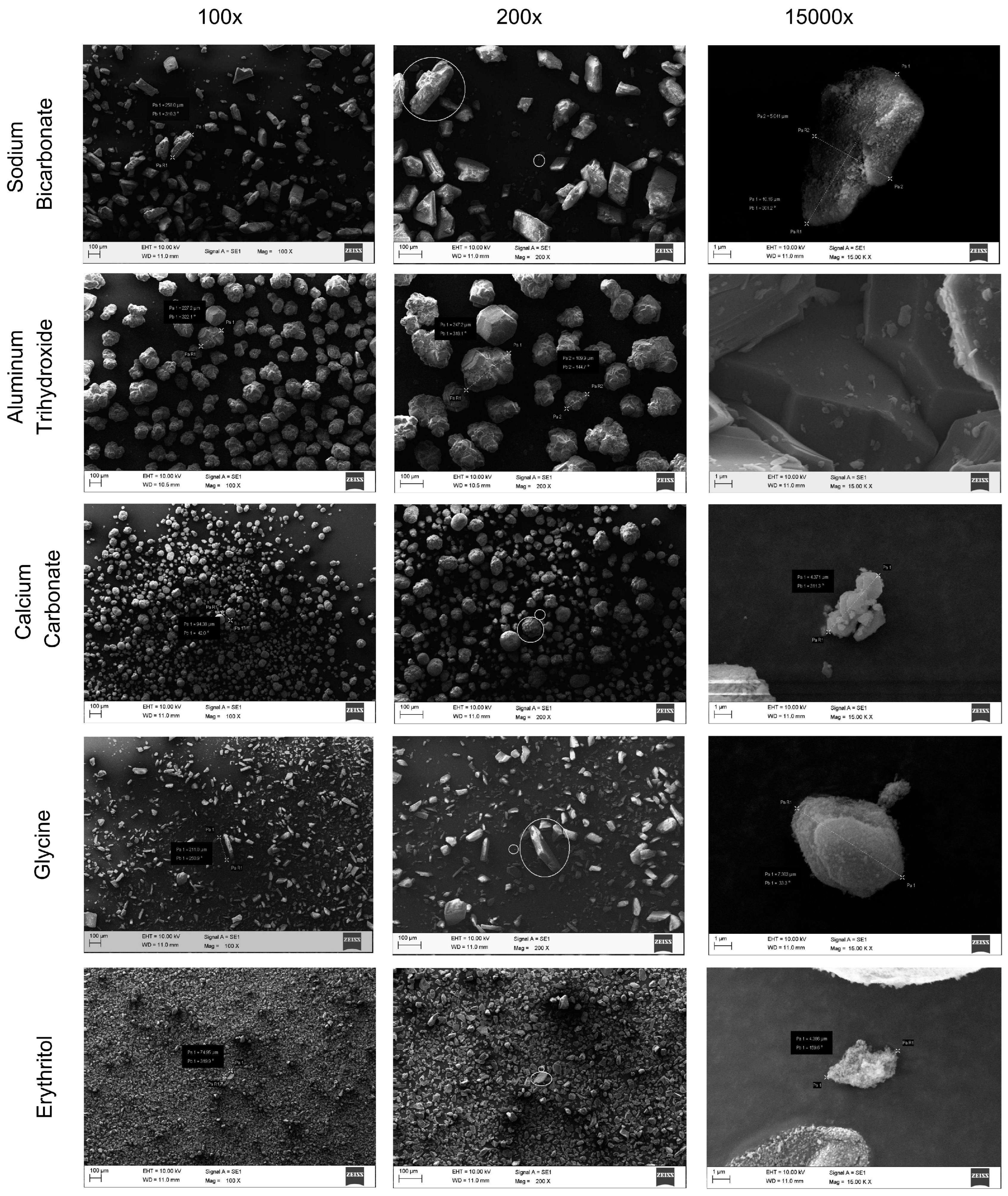
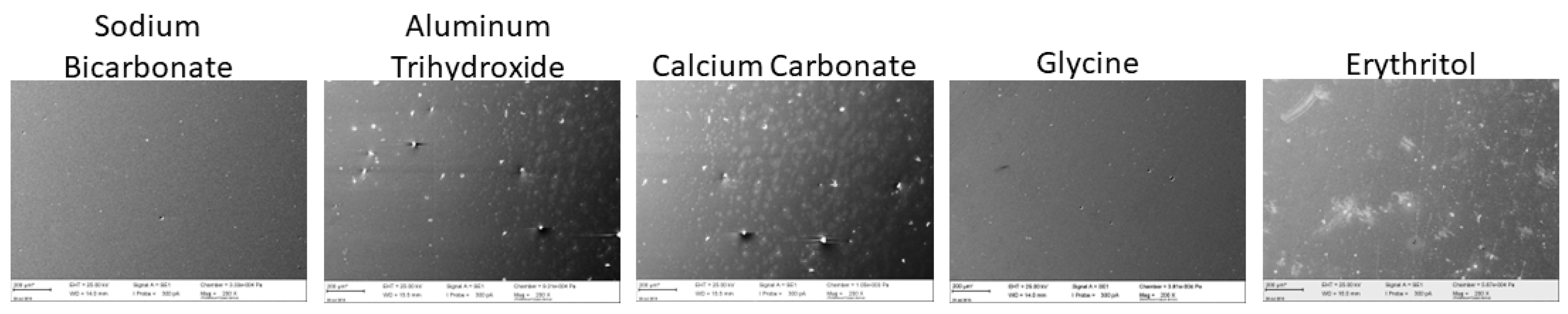
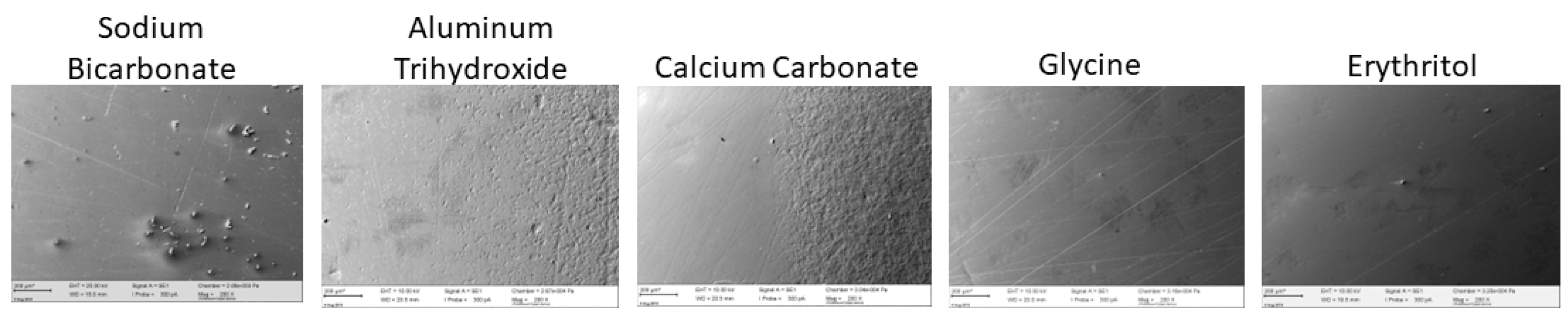
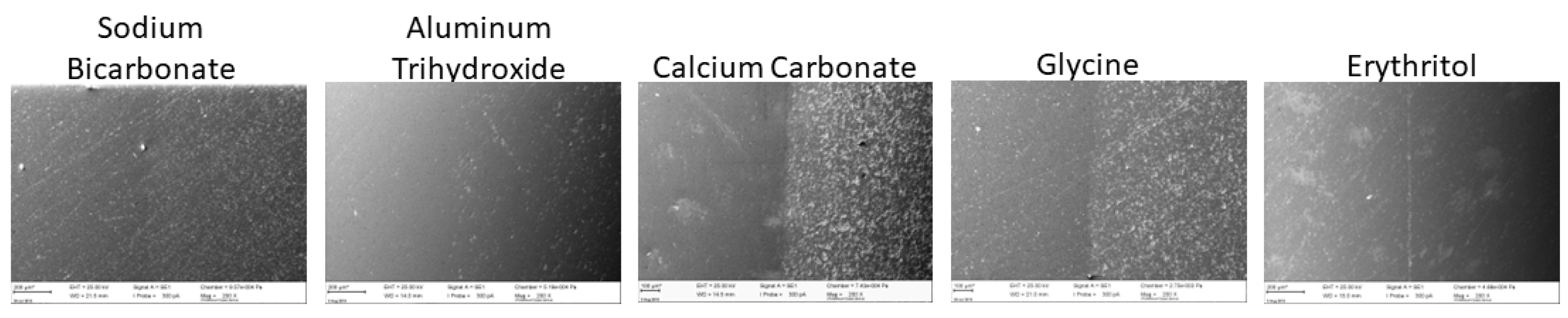
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- Both the type of CAD/CAM restorative material type and the APP had a significant effect on color difference, but their interaction terms were not significant.
- The color changes in all groups were clinically acceptable, but most of the groups presented perceptible color changes.
- Among the APPs, glycine seems the safest to use on restorative materials, but even glycine caused a perceptible color change for MZ.
- Dentists who are uncertain about the specific restorative material should limit prolonged air-polishing or avoid it altogether.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zarone, F.; Russo, S.; Sorrentino, R. From porcelain-fused-to-metal to zirconia: Clinical and experimental considerations. Dent. Mater. 2011, 27, 83–96. [Google Scholar] [CrossRef]
- Bajraktarova-Valjakova, E.; Korunoska-Stevkovska, V.; Kapusevska, B.; Gigovski, N.; Bajraktarova-Misevska, C.; Grozdanov, A. Contemporary dental ceramic materials, a review: Chemical composition, physical and mechanical properties, indications for use. Open Access Maced. J. Med. Sci. 2018, 6, 1742–1755. [Google Scholar] [CrossRef]
- Park, J.S.; Lim, Y.J.; Kim, B.; Kim, M.J.; Kwon, H.B. Clinical evaluation of time efficiency and fit accuracy of lithium disilicate single crowns between conventional and digital impression. Materials 2020, 13, 5467. [Google Scholar] [CrossRef]
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef] [PubMed]
- Ruse, N.D.; Sadoun, M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed]
- Awada, A.; Nathanson, D. Mechanical Properties of Resin-Ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Gracis, S.; Thompson, V.; Ferencz, J.; Silva, N.; Bonfante, E. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Bergamo, E.T.P.; Yamaguchi, S.; Coelho, P.G.; Lopes, A.C.O.; Lee, C.; Bonfante, G.; Benalcázar Jalkh, E.B.; de Araujo-Júnior, E.N.S.; Bonfante, E.A. Survival of Implant-Supported Resin-Matrix Ceramic Crowns: In Silico and Fatigue Analyses. Dent. Mater. 2021, 37, 523–533. [Google Scholar] [CrossRef]
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- Günal-Abduljalil, B.; Ulusoy, M.M. The Effect of Resin Cement Shade and Restorative Material Type and Thickness on the Final Color of Resin-Matrix Ceramics. J. Prosthodont. Res. 2022, 66, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Liebermann, A.; Spintzyk, S.; Reymus, M.; Schweizer, E.; Stawarczyk, B. Nine prophylactic polishing pastes: Impact on discoloration, gloss, and surface properties of a cad/cam resin composite. Clin. Oral Investig. 2019, 23, 327–335. [Google Scholar] [CrossRef]
- Sawai, M.A.; Bhardwaj, A.; Jafri, Z.; Sultan, N.; Daing, A. Tooth polishing: The current status. J. Indian Soc. Periodontol. 2015, 19, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Cobb, C.M.; Daubert, D.M.; Davis, K.; Deming, J.; Flemmig, T.F.; Pattison, A.; Roulet, J.-F.; Stambaugh, R.V. Consensus conference findings on supragingival and subgingival air polishing. Compend. Contin. Educ. Dent. 2017, 38, e1–e4. [Google Scholar] [PubMed]
- Martins, O.; Costa, A.; Silva, D. The efficacy of air polishing devices in supportive periodontal therapy: Clinical, microbiological and patient-centred outcomes. A Systematic Review. Int. J. Dent. Hyg. 2023, 21, 41–58. [Google Scholar] [CrossRef]
- Manresa, C.; Ec, S.; Twigg, J.; Bravo, M. Supportive periodontal therapy (SPT) for maintaining the dentition in adults treated for periodontitis. Cochrane Database Syst. Rev. 2018, 1, 2–3. [Google Scholar] [CrossRef]
- Lu, H.; He, L.; Zhao, Y.; Meng, H. The effect of supragingival glycine air polishing on periodontitis during maintenance therapy: A randomized controlled trial. PeerJ 2018, 2018, e4371. [Google Scholar] [CrossRef]
- Colucci, V.; Dos Santos, C.D.; Do Amaral, F.L.B.; Corona, S.A.M.; Catirse, A.B.C.E.B. Influence of NaHCO3 powder on translucency of microfilled composite resin immersed in different mouthrinses. J. Esthet. Restor. Dent. 2009, 21, 242–248. [Google Scholar] [CrossRef]
- Graumann, S.J.; Sensat, M.L.; Stoltenberg, J.L. Air polishing: A review of current literature. J. Dent. Hyg. 2013, 87, 173–180. [Google Scholar]
- Pelka, M.A.; Altmaier, K.; Petschelt, A.; Lohbauer, U. The effect of air-polishing abrasives on wear of direct restoration materials and sealants. J. Am. Dent. Assoc. 2010, 141, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Janaphan, K.; Hill, R.G.; Gilllam, D.G. In vitro evaluation of the abrasiveness of novel bioactive glass powders (Biominf®) on ivory dentine in air polishing procedures compared to selected reference powders. J. Dent. Maxillofac. Res. 2021, 4, 1–6. [Google Scholar] [CrossRef]
- Karmakar, S.; Kamath, D.G. Subgingival airpolishing: A simple and cost effective medical insurance. J. Pharm. Sci. Res. 2017, 9, 199–201. [Google Scholar]
- Barnes, C.M.; Covey, D.; Watanabe, H.; Simetich, B.; Schulte, J.R.; Chen, H. An in vitro comparison of the effects of various air polishing powders on enamel and selected esthetic restorative materials. J. Clin. Dent. 2014, 25, 76–87. [Google Scholar]
- Johnson, W.W.; Barnes, C.M.; Covey, D.A.; Walker, M.P.; Ross, J.A. The effects of a commercial aluminum airpolishing powder on dental restorative materials. J. Prosthodont. 2004, 13, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Janiszewska-Olszowska, J.; Drozdzik, A.; Tandecka, K.; Grocholewicz, K. Effect of air-polishing on surface roughness of composite dental restorative material-comparison of three different air-polishing powders. BMC Oral Health 2020, 20, 30. [Google Scholar] [CrossRef]
- Barnes, C.M. An In-Depth Look at Air Polishing. Dimens Dent. Hyg. 2010, 8, 32–36. [Google Scholar]
- Németh, K.D.; Haluszka, D.; Seress, L.; Lovász, B.V.; Szalma, J.; Lempel, E. Effect of air-polishing and different post-polishing methods on surface roughness of nanofill and microhybrid resin composites. Polymers 2022, 14, 1643. [Google Scholar] [CrossRef]
- Pelka, M.; Trautmann, S.; Petschelt, A.; Lohbauer, U. Influence of air-polishing devices and abrasives on root dentin-an in vitro confocal laser scanning microscope study. Quintessence Int. 2010, 41, e141–e148. [Google Scholar]
- Ng, E.; Byun, R.; Spahr, A.; Divnic-Resnik, T. The efficacy of air polishing devices in supportive periodontal therapy: A systematic review and meta analysis. Quintessence Int. 2018, 49, 453–467. [Google Scholar]
- Güler, A.U.; Duran, I.; Yücel, A.Ç.; Özkan, P. Effects of air-polishing powders on color stability of composite resins. J. Appl. Oral Sci. 2011, 19, 505–510. [Google Scholar] [CrossRef]
- Mathias, P.; Cunha, T.M.d.S.; Rocha, I.A.R.; Vitória, L.A.; Mathias, C.; Cavalcanti, A.N. Effect of air-polishing on properties of nanocomposite submitted to coffee, red wine and cigarette smoke. Braz J. Oral Sci. 2018, 17, e18021. [Google Scholar] [CrossRef]
- Valian, A.; Ansari, Z.J.; Rezaie, M.M.; Askian, R. Composite surface roughness and color change following airflow usage. BMC Oral Health 2021, 21, 398. [Google Scholar] [CrossRef]
- Eldwakhly, E.; Ahmed, D.R.M.; Soliman, M.; Abbas, M.M.; Badrawy, W. Color and translucency stability of novel restorative CAD/CAM materials. Dent. Med. Probl. 2019, 56, 349–356. [Google Scholar] [CrossRef]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Babina, K.; Polyakova, M.; Sokhova, I.; Doroshina, V.; Arakelyan, M.; Zaytsev, A.; Novozhilova, N. The Effect of ultrasonic scaling and air-powder polishing on the roughness of the enamel, three different nanocomposites, and composite/enamel and composite/cementum interfaces. Nanomaterials 2021, 11, 3072. [Google Scholar] [CrossRef] [PubMed]
- Tada, K.; Kakuta, K.; Ogura, H.; Sato, S. Effect of particle diameter on air polishing of dentin surfaces. Odontology. 2010, 98, 31–36. [Google Scholar] [CrossRef]
- Rayman, A.S.; Dincer, E. Air Polishing. Hygiene 2013, 1, 7–12. [Google Scholar]
- Nelson, S.J.; Ash, M.M. Wheeler’s Dental Anatomy, Physiology and Occlusion, 9th ed.; Saunders/Elsevier: St. Louis, MO, USA, 2010; p. 41. [Google Scholar]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S.; Merete Aass, A.; Aimetti, M.; et al. Treatment of stage I–III Periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47, 4–60. [Google Scholar] [CrossRef]
- Rinke, S.; Bettenhäuser-Hartung, L.; Leha, A.; Rödiger, M.; Schmalz, G.; Ziebolz, D. Retrospective evaluation of extended glass-ceramic ceramic laminate veneers after a mean observational period of 10 years. J. Esthet. Restor. Dent. 2020, 32, 487–495. [Google Scholar] [CrossRef]
- Sampaio, F.B.W.R.; Özcan, M.; Gimenez, T.C.; Moreira, M.S.N.A.; Tedesco, T.K.; Morimoto, S. Effects of manufacturing methods on the survival rate of ceramic and indirect composite restorations : A systematic review and meta-analysis. J. Esthet. Restor. Dent. 2019, 31, 561–571. [Google Scholar] [CrossRef]
- Atkinson, D.R.; Cobb, C.M.; Killoy, W.J. The effect of an air-powder abrasive system on in vitro root surfaces. J. Periodontol. 1984, 55, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; Del Mar Perez, M. Color difference thresholds in dentistry. J. Esthet. Restor. Dent. 2015, 27, S1–S9. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.D.M.; Ghinea, R.; Herrera, L.J.; Ionescu, A.M.; Pomares, H.; Pulgar, R.; Paravina, R.D. Dental Ceramics: A CIEDE2000 acceptability thresholds for lightness, chroma and hue differences. J. Dent. 2011, 39, e37–e44. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Engler, M.L.P.D.; Baumgardt Barbosa Lima, R.; Jesús Suarez, M.; Guy Oliver Salomon, J.P.; Maziero Volpato, C.A. Color stability of a resin nanoceramic after surface treatments, adhesive cementation, and thermal aging. J. Prosthet. Dent. 2022, 127, 498.e1–498.e8. [Google Scholar] [CrossRef]
- Chae, Y. Color appearance shifts depending on surface roughness, illuminants, and physical colors. Sci. Rep. 2022, 12, 1371. [Google Scholar] [CrossRef]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef]
- Şen, N.; Tuncelli, B.; Göller, G. Surface Deterioration of Monolithic CAD/CAM Restorative Materials after Artificial Abrasive Toothbrushing. J. Adv. Prosthodont. 2018, 10, 271–278. [Google Scholar] [CrossRef]


| Material and Manufacturer | Batch | Type | Shade | Composition |
|---|---|---|---|---|
| Vitablocs Mark II (VM); Vita Zahnfabrik | 35360 | Feldspar ceramic | A2 | Fine-particle feldspar ceramic (4 µm). |
| Paradigm MZ 100 (MZ); 3M ESPE | N543696 | Resin composite | A2 | Bis-GMA, TEGDMA. Filler: zirconia–silica particles (0.01 to 3.5 µm), 85% by weight. |
| Lava Ultimate (LU); 3M ESPE | N593972 | Resin nanoceramic | A2 | Bis-EMA, Bis-GMA, TEGDMA, UDMA. Filler: ZrO2 (4–11 nm) and SiO2 (20 nm), aggregated zirconia/silica cluster filler, 80% by weight. |
| Cerasmart (CS); GC Corp. | 1408011 | Flexible hybrid ceramic | A2 | Bis-MEPP, UDMA, Dimethacrylate. Filler: SiO2 (20 nm), barium glass (300 nm), 71% by weight. |
| Vita Enamic (VE); Vita Zahnfabrik | 42821 | Polymer-infiltrated ceramic network | A2 | TEGDMA, UDMA. Filler: feldspar ceramic enriched with aluminum oxide, 86% by weight. |
| Composition | Brand Name | Manufacturer | Mean Particle Size | Mohs No. | Density (g/cm3) | Lot No. |
|---|---|---|---|---|---|---|
| Sodium bicarbonate | Air-Flow Classic | EMS | 65 µm | 2.5 | 2.22 | 1403132 |
| Aluminum trihydroxide | Cavitron Jet-Fresh Powder | Dentsply | 80–325 µm | 4 | 2.42 | 110527 |
| Calcium carbonate | Prophypearls | KAVO | 45–55 µm | 3 | 2.93 | 0265936 |
| Glycine | Air-Flow Soft | EMS | 65 µm | 2 | 1.59 | 1202101 |
| Erythritol | Air-Flow Plus | EMS | 14 µm | <2 | 1.45 | 1302262 |
| V Variation Factor | df | Type III Sum of Squares | Mean Square | F | p | |
|---|---|---|---|---|---|---|
| Corrected model | 24 | ΔE00 | 20.789 | 0.866 | 2.615 | <0.001 ** |
| ΔL* | 80.765 | 3.365 | 4.650 | <0.001 ** | ||
| Δa* | 9.202 | 0.383 | 8.810 | <0.001 ** | ||
| Δb* | 37.621 | 1.568 | 9.190 | <0.001 ** | ||
| 34.267 | 1.428 | 8.299 | <0.001 ** | |||
| 8.909 | 0.371 | 8.916 | <0.001 ** | |||
| Intercept | 1 | ΔE00 | 167.265 | 167.265 | 505.055 | <0.001 ** |
| ΔL* | 5.791 | 5.791 | 8.002 | 0.005 ** | ||
| Δa* | 18.857 | 18.857 | 433.297 | <0.001 ** | ||
| Δb* | 1.246 | 1.246 | 7.306 | 0.007 ** | ||
| 0.476 | 0.476 | 2.767 | 0.098 | |||
| 23.409 | 23.409 | 562.262 | <0.001 ** | |||
| CAD/CAM block | 4 | ΔE00 | 8.220 | 2.055 | 6.205 | <0.001 ** |
| ΔL* | 61.143 | 15.286 | 21.121 | <0.001 ** | ||
| Δa* | 3.144 | 0.786 | 18.063 | <0.001 ** | ||
| Δb* | 34.060 | 8.515 | 49.923 | <0.001 ** | ||
| 0.476 | 0.098 | 43.939 | <0.001 ** | |||
| 3.205 | 0.801 | 19.243 | <0.001 ** | |||
| Air-polishing powder | 4 | ΔE00 | 7.292 | 1.823 | 5.505 | <0.001 ** |
| ΔL* | 6.946 | 1.737 | 2.399 | 0.051 | ||
| Δa* | 4.977 | 1.244 | 28.589 | <0.001 ** | ||
| Δb* | 1.231 | 0.308 | 1.805 | 0.129 | ||
| 1.419 | 0.355 | 2.062 | 0.087 | |||
| 4.593 | 1.148 | 27.578 | <0.001 ** | |||
| CAD/CAM block × air-polishing powder | 16 | ΔE00 | 5.276 | 0.330 | 0.996 | 0.462 |
| ΔL* | 12.676 | 0.792 | 1.095 | 0.361 | ||
| Δa* | 1.081 | 0.068 | 1.552 | 0.084 | ||
| Δb* | 2.330 | 0.146 | 0.854 | 0.623 | ||
| 2.610 | 0.163 | 0.948 | 0.515 | |||
| 1.112 | 0.069 | 1.669 | 0.054 |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | −0.28 ± 0.48 | 0.08 ± 0.39 | −0.07 ± 0.23 | −0.11 ± 0.42 | 1.02 ± 2.36 | 0.090 | |
| B MZ | −0.66 ± 0.82 | −0.94 ± 1.04 | −1.19 ± 0.47 | −0.78 ± 0.62 | −0.57 ± 0.80 | 0.411 | |
| C LU | 0.01 ± 0.56 | 0.23 ± 1.02 | −0.13 ± 0.57 | −0.16 ± 0.40 | −0.02 ± 0.27 | 0.654 | |
| D CS | −0.66 ± 0.82 | −0.56 ± 0.87 | −1.14 ± 0.69 | −0.14 ± 0.65 | −0.43 ± 0.94 | 0.096 | |
| E VE | 0.52 ± 0.43 | 0.51 ± 0.35 | 0.58 ± 0.75 | 0.45 ± 0.43 | 0.63 ± 1.65 | 0.992 | |
| b p | 0.001 ** | 0.001 ** | <0.001 ** | <0.001 ** | 0.066 | ||
| c Post Hoc | B, D < E | B < A, C, E | B, D < A, C, E | B < A, E | − | ||
| D < E |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | −0.34 ± 0.15 | −0.59 ± 0.34 | −0.41 ± 0.15 | −0.24 ± 0.10 | −0.32 ± 0.09 | 0.002 ** | 1, 4, 5 > 2 |
| B MZ | −0.13 ± 0.10 | −0.49 ± 0.16 | −0.49 ± 0.10 | −0.27 ± 0.16 | −0.16 ± 0.09 | <0.001 ** | 1, 4, 5 > 2, 3 |
| C LU | −0.11 ± 0.08 | −0.24 ± 0.15 | −0.52 ± 0.26 | −0.15 ± 0.10 | −0.18 ± 0.29 | <0.001 ** | 1, 2, 4, 5 > 3 |
| D CS | −0.25 ± 0.13 | −0.58 ± 0.22 | −0.55 ± 0.18 | −0.19 ± 0.09 | −0.28 ± 0.11 | <0.001 ** | 1, 4, 5 > 2, 3 |
| E VE | 0.16 ± 0.12 | −0.28 ± 0.26 | −0.30 ± 0.57 | 0.00 ± 0.10 | 0.05 ± 0.31 | 0.007 ** | 1 > 2, 3 |
| b p | <0.001 ** | 0.002 ** | 0.370 | <0.001 ** | 0.003 ** | ||
| c Post Hoc | A, B, C, D < E | A, D < C, E | − | A, B, C, D < E | A, D < E | ||
| A < B, C |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | −0.05 ± 0.18 | 0.15 ± 0.20 | 0.05 ± 0.20 | 0.06 ± 0.15 | 0.12 ± 0.31 | 0.305 | - |
| B MZ | −0.74 ± 0.35 | 0.14 ± 0.43 | −0.62 ± 0.25 | −0.63 ± 0.22 | −0.69 ± 0.34 | 0.495 | - |
| C LU | −0.20 ± 0.32 | 0.23 ± 1.02 | 0.02 ± 0.37 | −0.32 ± 0.23 | −0.08 ± 0.27 | 0.030 * | 4 < 2 |
| D CS | −0.30 ± 0.27 | −0.02 ± 0.77 | −0.47 ± 0.39 | −0.12 ± 0.28 | −0.05 ± 0.53 | 0.204 | - |
| E VE | 0.48 ± 0.34 | 0.42 ± 0.36 | 0.58 ± 0.55 | 0.44 ± 0.37 | 0.59 ± 1.08 | 0.957 | - |
| b p | <0.001 ** | 0.001 ** | <0.001 ** | <0.001 ** | 0.001 ** | ||
| c Post Hoc | B < A, C, D < E | B < A, C, E | B, D < A, C < E | B < A, D, E A, C, D < E C < A | B < A, E |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | −0.04 ± 0.18 | 0.18 ± 0.20 | 0.07 ± 0.19 | 0.06 ± 0.15 | 0.13 ± 0.31 | 0.217 | |
| B MZ | −0.71 ± 0.35 | −0.41 ± 0.34 | −0.52 ± 0.24 | −0.58 ± 0.21 | −0.65 ± 0.33 | 0.216 | |
| C LU | −0.18 ± 0.31 | 0.17 ± 0.42 | 0.10 ± 0.34 | −0.30 ± 0.22 | −0.05 ± 0.31 | 0.014 * | 4 < 2 |
| D CS | −0.29 ± 0.26 | 0.02 ± 0.77 | −0.43 ± 0.38 | −0.11 ± 0.28 | −0.03 ± 0.53 | 0.208 | |
| E VE | 0.50 ± 0.35 | 0.40 ± 0.37 | 0.57 ± 0.56 | 0.44 ± 0.37 | 0.59 ± 1.10 | 0.951 | |
| b p | 0.001 ** | 0.001 ** | <0.001 ** | <0.001 ** | 0.066 | ||
| c Post Hoc | B < A, C, D < E | B < A, C, E | D, B < A, C < E | A, B, C, D < E B < A, D C < A | B < A, E |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | 0.34 ± 0.15 | 0.59 ± 0.33 | 0.41 ± 0.15 | 0.24 ± 0.10 | 0.32 ± 0.08 | 0.002 ** | 1, 2, 3 < 5 |
| B MZ | 0.26 ± 0.11 | 0.57 ± 0.17 | 0.60 ± 0.12 | 0.37 ± 0.18 | 0.27 ± 0.09 | <0.001 ** | 1, 2, 3 < 4, 5 |
| C LU | 0.14 ± 0.12 | 0.22 ± 0.16 | 0.52 ± 0.29 | 0.19 ± 0.12 | 0.18 ± 0.25 | 0.001 ** | 1, 2, 3, 5 < 4 |
| D CS | 0.27 ± 0.14 | 0.58 ± 0.22 | 0.59 ± 0.21 | 0.20 ± 0.09 | 0.28 ± 0.11 | <0.001 ** | 1, 2, 3 < 4, 5 |
| E VE | −0.13 ± 0.11 | 0.31 ± 0.25 | 0.34 ± 0.55 | 0.04 ± 0.08 | 0.00 ± 0.23 | 0.003 ** | 2 < 4, 5 |
| b p | 0.001 ** | 0.001 ** | <0.001 ** | <0.001 ** | 0.066 | ||
| c Post Hoc | E < A, B, C, D | C < A, B, D | - | E < A, B, C, D | E < A, B, D | ||
| C < A | C, D < B |
| 1 Sodium Bicarbonate | 2 Aluminum Trihydroxide | 3 Calcium Carbonate | 4 Glycine | 5 Erythritol | b p | c Post Hoc | |
|---|---|---|---|---|---|---|---|
| A VM | −0.62 ± 0.23 | 0.90 ± 0.44 | 0.62 ± 0.21 | 0.44 ± 0.24 | 1.14 ± 1.75 | 0.352 | - |
| B MZ | 1.03 ± 0.33 | 1.34 ± 0.45 | 1.32 ± 0.38 | 0.99 ± 0.41 | 0.93 ± 0.42 | 0.072 | - |
| C LU | 0.49 ± 0.22 | 0.79 ± 0.43 | 0.87 ± 0.35 | 0.45 ± 0.24 | 0.37 ± 0.39 | 0.004 ** | 5 < 2, 3 |
| D CS | −0.66 ± 0.82 | 1.19 ± 0.34 | 1.26 ± 0.56 | 0.48 ± 0.36 | 0.83 ± 0.46 | 0.002 ** | 4 < 2, 3 |
| E VE | 0.58 ± 0.33 | 0.71 ± 0.25 | 1.03 ± 0.58 | 0.46 ± 0.39 | 0.85 ± 1.36 | 0.423 | - |
| b p | 0.005 ** | 0.003 ** | 0.005 ** | 0.002 ** | 0.570 | ||
| c Post Hoc | C, E < B | C, E < B | A < B, D | A, C, D, E < B | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turunç Oğuzman, R.; Yüzbaşıoğlu, E. Air-Polishing Powders’ Effect on the Color of CAD/CAM Restorative Materials. Appl. Sci. 2023, 13, 11573. https://doi.org/10.3390/app132011573
Turunç Oğuzman R, Yüzbaşıoğlu E. Air-Polishing Powders’ Effect on the Color of CAD/CAM Restorative Materials. Applied Sciences. 2023; 13(20):11573. https://doi.org/10.3390/app132011573
Chicago/Turabian StyleTurunç Oğuzman, Rana, and Emir Yüzbaşıoğlu. 2023. "Air-Polishing Powders’ Effect on the Color of CAD/CAM Restorative Materials" Applied Sciences 13, no. 20: 11573. https://doi.org/10.3390/app132011573
APA StyleTurunç Oğuzman, R., & Yüzbaşıoğlu, E. (2023). Air-Polishing Powders’ Effect on the Color of CAD/CAM Restorative Materials. Applied Sciences, 13(20), 11573. https://doi.org/10.3390/app132011573






