Featured Application
Apical transportation determined by the endodontic shaping phase can lead to failure of the therapy itself. The use of endodontic instruments with flexible alloys could reduce this problem. The objective of this systematic literature review is to evaluate whether the use of martensitic endodontic instruments can result in less apical transportation compared to austenitic instruments during endodontic therapy. Based on the analysis of the selected articles, it can be concluded that martensitic endodontic instruments result in less apical transportation compared to austenitic instruments during the shaping phase of endodontic treatment.
Abstract
Endodontic shaping can lead to canal and apical anatomical alterations, which may compromise the outcome of root canal treatment. The objective of this systematic literature review is to assess whether the use of martensitic endodontic instruments can result in less apical transportation compared to austenitic instruments during endodontic therapy. A search was conducted on PubMed, Ovid MEDLINE, and the Web of Science. The inclusion criteria were in vitro studies comparing apical transportation using endodontic instruments with austenitic or martensitic alloys. The search of the scientific databases yielded 592 results, of which only 10 were eligible for evaluation after screening. Based on the analysis of the selected articles, it can be concluded that martensitic endodontic instruments result in less apical transportation compared to austenitic instruments during the shaping phase of endodontic treatment. This behavior can be attributed to the increased flexibility of martensitic instruments. Further research is warranted to further explore this topic and provide additional evidence supporting the use of martensitic instruments in clinical practice.
1. Introduction
Shaping the root canal system is essential for achieving clinical success in endodontic treatment [1]. Canal shaping should aim to preserve the canal and apical anatomy as much as possible [2]. Numerous NiTi instruments have been introduced to reduce alterations to and deformations of the canal during endodontic shaping [3,4,5]. However, due to various factors, such as the geometry, alloy, and movement of the instruments, as well as the characteristics of the canal (dentin hardness, canal curvature radius and angle, and complex anatomies) and operator experience, it is still possible to alter this anatomy, leading to consequences such as stripping, canal transportation, or apical transportation [6,7]. Apical transportation refers to the deviation of the physiological apical position from the iatrogenic position, generally located on the outer surface of the curvature, which can compromise the outcome of root canal treatment, and once transportation has occurred, it is impossible to return the canal to its original shape, particularly in curved canals [8,9]. Apical transportation occurs due to the leaning of the rotary instrument in order to return to the original position when subjected to deformation. Consequently, rotary instruments tend to remove more of the dentin on the outermost side of the canal curve. Apical transportation can be classified into three types, depending on the degree [10]:
Type I: minor movement of the position of the foramen, leading to its iatrogenic relocation.
Type II: moderate movement of the physiological position of the foramen, with consequent iatrogenic displacement on the external root surface. In this type of apical transport, a wider communication with the periapical space is achieved. As a result, type II apical transportation can lead to a weak or perforated root.
Type III: severe movement of the physiologic position of the canal, resulting in a significant iatrogenic relocation of the physiologic foramen.
Regarding the treatment of different types of apical transportation, type I transportation is the only type manageable by nonsurgical endodontics. Type II and III require surgical endodontics in order to properly complete the endodontic therapy [11].
Apical transportation may result in inadequately cleaned root canals, root weakening, and improper debridement of the canal in the apical region, and can also lead to the zipping or perforation of the apical foramen [12]. Moreover, it may result in the extrusion of irrigation solution, debris, and filling materials [13,14]. Furthermore, although type I does not require surgical endodontic treatment, it can still make orthograde endodontic therapy more difficult, sometimes making it necessary to use mineral trioxide aggregate (M.T.A.) or new bioceramic materials in order to obtain a correct apical seal [15,16].
In recent decades, there has been a revolution in the production of endodontic instruments with different mechanical characteristics. Technological advancements in the production and treatment of NiTi alloys for use in endodontic files have allowed the development of alloys with different phase transformation behaviors, improving their flexibility, centering ability, fatigue, and torsional resistance [17,18,19,20,21]. Companies have devised various methods for altering the manufacturing process or modifying the physical properties of NiTi instruments, including the use of complex heating–cooling phases to vary the temperature of NiTi alloy’s transition between austenitic and martensitic phases. While austenitic NiTi is strong and hard, the material becomes soft, ductile, and flexible in its martensitic form [22,23,24,25,26]. This has led to the creation of alloys such as M-Wire™ (Dentsply-Tulsa & WDV), R-Phase™ (Kerr), CM-Wire™ (Coltène Whaledent), Blue™ (Dentsply-Tulsa), Gold™ (Dentsply-Tulsa), and Max-Wire™ (FKG), characterized by their ability to transition from the martensitic to austenitic phase at different temperatures. This allows the instruments to operate in the martensitic phase at room temperature and return to the austenitic phase when heated to their phase transition point. The transition temperatures from martensitic to austenitic phases are as follows: 17 °C for R-Phase; 35 °C for Max-Wire; 38 °C for Blue; 50 °C for M-Wire; and 55 °C for CM and Gold [27,28]. This increased flexibility enables instruments with martensitic heat treatments to rotate more centrally within the endodontic canal, following the canal’s anatomy and reducing issues such as canal and apical transportation.
The objective of this systematic literature review is to evaluate whether the use of martensitic endodontic instruments results in less apical transportation compared to the use of austenitic instruments during endodontic therapy.
2. Materials and Methods
2.1. Protocol and Registration
The preferred reporting items of systematic reviews and metanalyses (PRISMA) guidelines were followed for the writing of this systematic review [29]. Before writing this paper, a point-to-point protocol describing the methodology was developed. The review was registered in the CRD York website, PROSPERO (International Prospective Register of Systematic Reviews), organized by the Centre for Reviews and Dissemination (the University of York, National Institute for Health Research, York, UK), with the protocol number CRD42023405277 and the title “Apical Transportation of Different NiTi Alloy Systems: a Systematic Review”.
2.2. Search Strategy
The systematic review was carried out on electronic databases, including Ovid MEDLINE, PubMed, and the Web of Science. No search by hand was performed on other databases. The date parameter for the paper collection was set from January 2013 until April 2023. The following terms and their combinations were searched: (Apical transportation) AND (Instrument alloy), to which Boolean operators were applied. The keywords were selected with the aim of gathering and registering as much relevant data as possible.
The following focus question was developed, according to the population, intervention, comparison, and outcome (PICO) study design:
“Do files with martensitic alloys (I) cause less transportation of the apical foramen (O) than files with austenitic alloys (C) in endodontically treated teeth (P)?”
The review included in vitro studies in which a comparison was performed on the apical transportation of teeth endodontically treated with different endodontic instruments made of different alloys.
2.3. Eligibility Criteria
The full texts of all potentially relevant research papers were obtained, in consideration of the following inclusion criteria:
- In vitro studies comparing apical transportation using endodontic instruments with austenitic or martensitic alloys.
The exclusion criteria that were considered were:
- Research involving teeth with disease.
- Research evaluating canal transportation and not apical transportation.
- Research comparing apical transportation using only one file type.
- Research comparing apical transportation using only one type of alloy.
- Case reports, case series, reviews, and meta-analyses.
- Papers with no full text available.
- Papers written in languages other than English.
2.4. Study Selection and Data Extraction
To reduce bias, two researchers from Messina University (F.P. and A.T.) independently conducted the literature search, and in cases where there were discrepancies in the results, a third senior researcher (G.L.G.) was consulted at each phase (i.e., initial screening, eligibility for final inclusion, data extraction and analysis, and quality assessment). The following variables were defined in this investigation: first author’s last name and year of publication; instrument used; evaluation methods; object of research; conclusions.
2.5. Risk of Bias Assessment
The evaluation of in vitro studies was performed on the basis of a methodological index in which a checklist is used for in vitro studies on dental materials (CONSORT). This checklist of items has the purpose of evaluating how the study was designed, analyzed, and interpreted, and uses 14 domains [30].
2.6. Study Selection
The initial search of the scientific databases yielded 592 results. Duplicate studies and studies published before 1 January 2013 were excluded, resulting in a total of 288 studies. Of these, 8 articles were excluded as they were reviews, meta-analyses, or case reports. After the initial selection, 280 studies underwent a full-text examination. Of these, 34 articles were discarded because they evaluated endodontic instruments made of the same alloy, while 79 were not included as they focused on canal transportation rather than apical transportation. Seven studies were excluded as they evaluated apical transportation using only one endodontic instrument, and 149 studies were discarded because they were not relevant to the objectives of the review. One article was not included in the review because the endodontic instruments analyzed were used with different parameters than those specified by the manufacturer [14]. In total, 10 studies were included in this review [22,31,32,33,34,35,36,37,38,39] (Figure 1). The included papers are listed in Table 1 and Table 2.
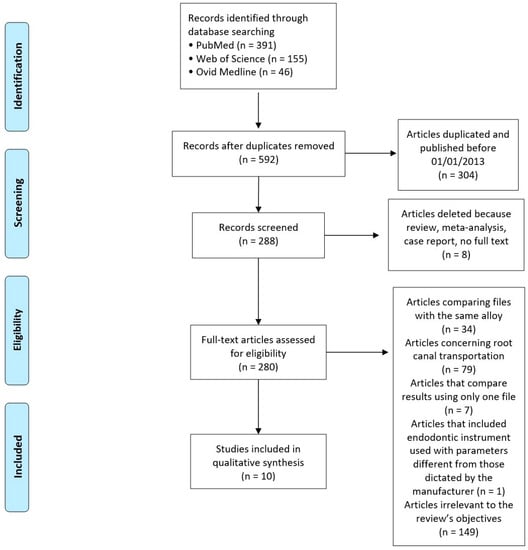
Figure 1.
PRISMA flowchart.

Table 1.
Data extraction from selected studies.

Table 2.
Identification of the included studies.
2.7. Risk of Bias
Table 3 presents the risk of bias in the in vitro studies.

Table 3.
Bias in the in vitro studies.
3. Results and Discussion
Clinically speaking, flexibility is considered to be one of the most important characteristics in choosing one type of endodontic instrument over another instrument [21]. In fact, it is possible to use instruments with different mechanical properties based on the specific characteristics of the root canal anatomy [21]. NiTi instruments have undergone continuous evolution in terms of the different cutting blade designs, flute numbers, variations in helical angles, cross-sectional configurations, and thermomechanical treatments employed.
All of the studies examined in this review were in vitro studies. To evaluate whether endodontic files with martensitic alloy caused less apical transportation compared to those with austenitic alloy, the authors of the included studies utilized various devices and methods, such as Micro CT, photographs and periapical radiographs [22,40]. Micro CT is recognized as the gold standard for the morphological evaluation of the effects of canal shaping. This method is important, as it can be used in in vitro studies to improve the distribution in the study sample, using established morphological parameters to provide a consistent baseline [41]. For example, it is possible to select radicular systems with similar morphologies to eliminate potential anatomical bias that would alter the research results, using established morphological parameters to provide a consistent baseline [42].
The authors of the studies included in this review agree on the results, stating that the use of instruments with martensitic alloys results in less apical transportation during endodontic treatment [22,31,32,34,35,36,37,38].
The NiTi alloys used in endodontic instruments contain approximately 56% by weight of nickel and 44% of titanium, in an equiatomic ratio of 1:1 [41]. In some nickel–titanium alloys, 2% of the nickel is converted to cobalt [43]. Due to the possibility of changing the type of atomic bonds by means of the nickel and titanium included in the alloy, the mechanical properties of NiTi alloy and its crystal structure can change. The alloy can exist in two different microstructural phases—austenite and martensite—with distinct mechanical properties [8]. In the austenitic phase, the alloy is rigid and exhibits shape memory, meaning that when the instrument is bent, it tends to return to its original shape. On the other hand, the martensitic phase is more flexible, and does not have shape memory [21]. The phase transition can occur either through the application of force or through temperature variation.
- Application of force: This results in the transition from the austenitic phase to the martensitic phase. Force is applied when the canal walls compress the rotating instrument, particularly in curved canals [21,44,45].
- Variation in temperature: High temperatures induce the austenitic phase, while low temperatures induce the martensitic phase [21,44,45].
The heat treatments applied to NiTi alloys by companies are aimed at modifying the alloy’s transition temperature, which is the temperature at which the alloy transitions from one phase to another. This allows the creation of instruments with varying percentages of martensite and austenite, resulting in instruments with different levels of flexibility [21,44,45]. The flexibility of the instrument enables it to rotate centrally within the canal, reducing alterations to the endodontic anatomy. When an endodontic instrument passes through a curved canal, it tends to work more on the outer portion of the curve, particularly if the instrument is rigid [45,46,47]. Since it is rare to find a perfectly straight canal in nature, with most canals having varying degrees of curvature, especially in the apical portion, a rigid instrument is more likely to cause apical transportation [22,31,32,34,35,36,37,48,49,50,51,52].
Two the studies included in this systematic review focused on endodontically treated teeth [32,35]. Both studies concluded that the use of martensitic alloys resulted in less apical transportation, even in cases of retreatment.
Two of the articles included in this review did not find any differences in apical transportation when comparing austenitic and martensitic instruments [33,39].
- Saber et al. suggested that the absence of differences in apical transportation could be attributed to the specific characteristics of the iRaCe instruments analyzed, such as their small cross-sectional areas, which increase flexibility and allow for better debris removal, as well as the design of their working parts, which feature alternating cutting edges. This design enables the preparation of curved root canals with larger apical diameters to be achieved with minimal apical transportation compared to when using other rotary NiTi instruments [39,53,54].
- Yilmaz et al. stated that there were no differences in apical transportation among the tested instruments, but attributed this result to the similar behavior of the ProTaper Next and EdgeFile alloys [33]. The results of this study may also be influenced by procedural errors, as the authors prepared the teeth using instruments with different apical diameters (EdgeFile with #40, ProTaper Next with #30, and One Shape with #25). Finally, the authors concluded that the absence of differences in apical transportation could be due to the limited sample size of the study.
The discrepancy in the results obtained from these two studies is likely attributable to various factors, and is not necessarily related to the alloy of the file used. Instead, the differences may be attributed to variations in the design and kinematics of the instruments, as well as the asymmetric or centralized motion and rotation axis of the instruments. Other factors, such as sample size, methodology, and procedural errors, may also contribute to the discrepant findings [55].
Only three of the studies included in this systematic review evaluated the apical transportation occurring during the root canal shaping phases in curved canals [35,36,39]. The apical curvature of the canal is one of the factors with the greatest effect on the occurrence of apical transport. In fact, the risk of transportation is linked to the degree and radius of canal curvature: the more severe the curvature and the smaller the radius of curvature, the more distinct the risk of straightening. Furthermore, it has also been shown that both the radius and the degree of canal curvature have an impact on the stress of the instruments used to prepare these canals [56,57]. For these reasons, future scientific literature should carry out such evaluations on canals with apical curves.
Only one of the studies included in this systematic review of the literature investigated apical transportation using resin blocks and no teeth [36]. In these resin blocks, the canals had precisely defined parameters, including length, taper, curvature, and degree of curvature. All resin blocks were the same, thus representing a sample with repeatable characteristics. This is essential to be able to exclude the bias that can affect the results of studies performed on non-homogeneous samples. In fact, it is possible that the characteristics of root canal anatomy, such as length, curvature and taper, can alter the results of the research. Furthermore, the resin blocks are transparent, making measurements easier for the researcher [36]. The authors concluded that martensitic endodontic instruments determined a lower apical transportation than austenitic instruments during the endodontic shaping phases [36]. However, it must be considered that the dentin and the resin used have different physical characteristics; the compressive resistance and elasticity of resin are lower than dentin [56]. Furthermore, during the shaping phase, the rotation of the tools in the resin blocks generates heat, which may contribute to the softening of the resin material, thus leading to inefficient shaping [58,59].
However, it must be considered that most of the studies included in this systematic review of the literature compare different instruments not only in terms of the type of heat treatment undergone, but also with regard to characteristics such as taper, cross-sectional profile and blade design. Differences in mechanical properties such as flexibility are not only determined by heat treatment, but also by geometric factors such as pitch length, taper or conicity, and cross-sectional shape [60]. All of these characteristics affect clinical performance. For example, non-cutting tips are characterized by a reduction in the tip or the transition angle [61,62]. The literature shows that passive (and therefore non-cutting) tips result in more uniform material removal on the outside and inside of the curve than instruments with active tips [63].
Some of the studies included in this review compared the apical transportation occurring during the shaping phase using instruments with the same design but using different heat treatments [32,34,35]. Two studies analyzed the results obtained after performing shaping using geometrically identical One Shape and One Curve files [32,34]. Both systems use instruments with a clockwise rotation at a constant taper of 0.06. The apical part of the One Curve and One Shape files has a triple-helix cross-sectional design and the middle and coronal parts of the file are designed with an S shape with two blades [64]. One Shape files are made of electropolished austenite 55-NiTi alloy; files in the One Curve system are made with C-wire alloy, which provides shape memory [32,64]. In both studies, the use of the martensitic instrument determined the smallest apical transportation. Kırıcı also evaluated the apical transportation occurring when using two identical reciprocating instruments, but made from different alloys, i.e., Reciproc, made with M-Wire alloy, and Reciproc Blue, made using an innovative heat treatment that gives the instrument a characteristic blue color [35]. This new alloy increased the flexibility and resistance of cyclic fatigue compared to M-Wire [65]. Reciproc Blue was 42.31% more flexible than the Reciproc file [66]. Both instruments have an S-shaped cross-section with two cutting edges and a 0.08 taper, and use reciprocating motion in which the direction of rotation alternates between the counterclockwise and clockwise directions [67,68]. All of the studies included in this systematic review of the literature that analyze the effect of instruments with the same geometric design but with different alloys conclude that instruments with martensitic alloys determine lower apical transportation compared to instruments with austenitic alloys [32,34,35].
Limitations
The main limitation of this article is its reliance on in vitro studies. Although in vitro studies provide valuable insights into the effects of different endodontic instruments, they may not fully reflect the complexities and variations found in clinical settings. Factors such as the presence of surrounding tissues, biological responses, and patient-specific variables cannot be accurately replicated in an in vitro environment. Therefore, the findings of this review should be extrapolated to clinical practice with caution, and further research involving clinical trials is needed to validate the results.
The main limitation of the in vitro studies considered in this review is the high risk of bias. The absence of a blinded investigator and the lack of a methodology involving random sequence generation introduce potential selection bias. Blinding is important in order to minimize the influence of bias in the assessment of outcomes, and random sequence generation is crucial for ensuring the unbiased allocation of interventions. The absence of these key elements in the included studies raises concerns regarding the internal validity of their findings.
Another limitation is the lack of standardization across the studies. Each study evaluated different root canals with varying diameters and curvatures, leading to diverse results. The impossibility of testing both instrument systems in the same root canal hampers direct comparisons and makes it challenging to draw definitive conclusions. The variations in the anatomy of the root canals and the lack of standardization in the experimental conditions introduced potential confounding factors that may have influenced the observed outcomes.
Furthermore, a significant proportion of the literature is focused primarily on evaluating canal transportation rather than apical transportation. Only a few studies have been performed in which apical transportation was specifically investigated, and different types of NiTi alloy compared. This limited availability of studies directly examining apical transportation with the use of different NiTi alloys restricts the depth and breadth of evidence on this specific aspect. Therefore, further research is needed to address these limitations and to provide more comprehensive insights into the effects of different NiTi alloys on apical transportation.
One strong point of this article is its rigorous adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. By following a well-defined protocol and conducting a comprehensive literature search, the authors have ensured transparency and reproducibility in their review process. The inclusion of a registered protocol number further enhances the credibility of the study. Additionally, the involvement of two independent researchers and consultation with a senior researcher for discrepancies adds to the robustness of the study. These methodological aspects increase the reliability of the findings and strengthen the overall quality of this systematic review.
4. Conclusions
The analysis of the obtained results indicates that the use of martensitic endodontic instruments determines lower apical transportation compared to austenitic instruments during the endodontic shaping phases. This behavior is attributable to the greater flexibility of martensitic instruments. The authors therefore recommend the use of martensitic instruments, especially for the shaping phase of complex root canal anatomies.
Author Contributions
Conceptualization, F.P.; methodology, G.L.G.; software, A.T.; formal analysis, F.G.; writing—original draft preparation, F.P.; writing—review and editing, U.B.; supervision, G.L.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arias, A.; Peters, O.A. Present status and future directions: Canal shaping. Int. Endod. J. 2022, 55, 637–655. [Google Scholar] [CrossRef]
- Gonzalez-Rodriguez, M.P.; Ferrer-Luque, C.M. A comparison of Profile, Hero642, and K3 instrumentation systems in teeth using digital imaging analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 97, 112–115. [Google Scholar] [CrossRef]
- Hulsmann, M.; Peters, O.A.; Dummer, P.M.H. Mechanical preparation of root canals: Shaping goals, techniques and means. Endod. Top. 2005, 10, 30–76. [Google Scholar] [CrossRef]
- Burklein, S.; Mathey, D.; Schafer, E. Shaping ability of ProTaper Next and BT-RaCe nickel-titanium instruments in severely curved root canals. Int. Endod. J. 2015, 48, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Burklein, S.; Schafer, E. Critical evaluation of root canal transportation by instrumentation. Endod. Top. 2013, 29, 110–124. [Google Scholar] [CrossRef]
- Ciobanu, I.E.; Rusu, D.; Stratul, S.I.; Didilescu, A.C.; Cristache, C.M. Root Canal Stripping: Malpractice or Common Procedural Accident-An Ethical Dilemma in Endodontics. Case Rep. Dent. 2016, 2016, 4841090. [Google Scholar] [PubMed]
- Peters, O.A.; Peters, C.I.; Basrani, B. Cleaning and shaping the root canal system. In Cohen’s Pathways of the Pulp, 11th ed.; Hargreaves, K.M., Berman, L.H., Eds.; Elsevier: St Louis, MO, USA, 2016. [Google Scholar]
- Peters, O.A.; Laib, A.; Göhring, T.N.; Barbakow, F. Changes in root canal geometry after preparation assessed by high-resolution computed tomography. J. Endod. 2001, 27, 1–6. [Google Scholar] [CrossRef]
- Siqueira, J.F., Jr.; Lopes, H.P. Chemomechanical preparation. In Treatment of Endodontic Infections; Siqueira, J.F., Jr., Ed.; Quintessence Publishing: London, UK, 2011. [Google Scholar]
- Gluskin, A.H.; Peters, C.I.; Wong Ming, R.D.; Ruddle, C.J. Retreatment of non-healing endodontic therapy and management of mishaps. In Text Book of Endodontics, 6th ed.; Ingle, J.I., Bakland, L.K., Baumgartner, C., Eds.; BC Decker: Hamilton, ON, Canada, 2008; pp. 1088–1555. [Google Scholar]
- Hasheminia, S.M.; Farhad, A.; Sheikhi, M.; Soltani, P.; Hendi, S.S.; Ahmadi, M. Cone-beam computed tomographic analysis of canal transportation and centering ability of single-file systems. J. Endod. 2018, 44, 1788–1791. [Google Scholar] [CrossRef]
- Hamze, F.; Honardar, K.; Nazarimoghadam, K. Comparison of two canal preparation techniques using mtwo rotary instruments. Iran Endod. J. 2011, 6, 150–154. [Google Scholar]
- Nevares, G.; de Albuquerque, D.S.; Freire, L.G.; Romeiro, K.; Fogel, H.M.; dos Santos Cunha, R.S. Efficacy of ProTaper next compared with reciproc in removing obturation material from severely curved root canals: A micro-computed tomography study. J. Endod. 2016, 42, 803–808. [Google Scholar] [CrossRef]
- Delai, D.; Jardine, A.P.; Mestieri, L.B.; Boijink, D.; Fontanella, V.R.C.; Grecca, F.S.; Kopper, P.M.P. Efficacy of a thermally treated single file compared with rotary systems in endodontic retreatment of curved canals: A micro-CT study. Clin. Oral Investig. 2019, 23, 1837–1844. [Google Scholar] [CrossRef]
- Casella, G.; Ferlito, S. The use of mineral trioxide aggregate in endodontics. Minerva Stomatol. 2006, 55, 123–143. [Google Scholar]
- Trope, M.; Bunes, A.; Debelian, G. Root filling materials and techniques: Bioceramics a new hope. Endod. Top. 2015, 32, 86–96. [Google Scholar] [CrossRef]
- Hieawy, A.; Haapasalo, M.; Zhou, H.; Wang, Z.J.; Shen, Y. Phase Transformation Behavior and Resistance to Bending and Cyclic Fatigue of ProTaper Gold and ProTaper Universal Instruments. J. Endod. 2015, 41, 1134–1138. [Google Scholar] [CrossRef]
- Govindjee, R.G.; Govindjee, S. Thermal phase transformation in commercial dental files. In Structural Engineering Mechanics and Materials; Report No. USB/SEMM-2015/02; Department of Civil and Environmental Engineering, University of California: Berkeley, CA, USA, 2015. [Google Scholar]
- Silva, E.J.N.L.; Vieira, V.T.L.; Belladonna, F.G.; Zuolo, A.D.S.; Antunes, H.D.S.; Cavalcante, D.M.; Elias, C.N.; De-Deus, G. Cyclic and Torsional Fatigue Resistance of XP-endo Shaper and TRUShape Instruments. J. Endod. 2018, 44, 168–172. [Google Scholar] [CrossRef]
- Gambarini, G.; Grande, N.; Plotino, G.; Somma, F.; Garala, M.; De Luca, M.; Testarelli, L. Fatigue resistance of engine-driven rotary nickel titanium instruments produced by new manufacturing methods. J. Endod. 2008, 34, 1003–1005. [Google Scholar] [CrossRef]
- Shen, Y.; Zhou, H.M.; Zheng, Y.F.; Peng, B.; Haapasalo, M. Current challenges and concepts of the thermomechanical treatment of nickel-titanium instruments. J. Endod. 2013, 39, 163–172. [Google Scholar]
- Zhao, D.; Shen, Y.; Peng, B.; Haapasalo, M. Micro-computed tomography evaluation of the preparation of mesiobuccal root canals in maxillary first molars with Hyflex CM, Twisted Files, and K3 instruments. J. Endod. 2013, 39, 385–388. [Google Scholar] [CrossRef]
- Tabassum, S.; Zafar, K.; Umer, F. Nickel-Titanium Rotary File Systems: What’s New? Eur. Endod. J. 2019, 4, 111–117. [Google Scholar]
- Pedullà, E.; Lo Savio, F.; Boninelli, S.; Plotino, G.; Grande, N.M.; La Rosa, G.; Rapisarda, E. Torsional and Cyclic Fatigue Resistance of a New Nickel-Titanium Instrument Manufactured by Electrical Discharge Machining. J. Endod. 2016, 42, 156–159. [Google Scholar] [CrossRef]
- Pedullà, E.; Lo Savio, F.; Boninelli, S.; Plotino, G.; Grande, N.M.; Rapisarda, E.; La Rosa, G. Influence of cyclic torsional preloading on cyclic fatigue resistance of nickel-titanium instruments. Int. Endod. J. 2015, 48, 1043–1050. [Google Scholar] [CrossRef]
- Pedullà, E.; Lizio, A.; Scibilia, M.; Grande, N.M.; Plotino, G.; Boninelli, S.; Rapisarda, E.; Lo Giudice, G. Cyclic fatigue resistance of two nickel-titanium rotary instruments in interrupted rotation. Int. Endod. J. 2017, 50, 194–201. [Google Scholar]
- Silva, R.V.; Alcalde, M.P.; Horta, M.C.; Rodrigues, C.T.; Silveira, F.F.; Duarte, M.A.; Nunes, E. Root canal shaping of curved canals by Reciproc Blue system and Pro Taper Gold: A micro-computed tomographic study. J. Clin. Exp. Dent. 2021, 13, e112–e118. [Google Scholar] [CrossRef]
- Somma, F. Endodonzia, Principi di Base, Procedure Operative e Tecniche (Sec Edizione) Edito da Edra; Edra: Tuscany, France, 2016. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar]
- Faggion, C.M. Guidelines for Reporting Pre-clinical In Vitro Studies on Dental Materials. J. Évid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef]
- Gomes, I.L.L.; Alves, F.R.F.; Marceliano-Alves, M.F.; Silveira, S.B.; Provenzano, J.C.; Gonçalves, L.S. Canal transportation using Mani GPR or HyFlex NT during the retreatment of curved root canals: A micro-computed tomographic study. Aust. Endod. J. 2021, 47, 73–80. [Google Scholar] [CrossRef]
- Alsofi, L.; Rajkhan, W.; Al-Habib, M.; Ashe, H.; Alnowailaty, Y.; Balto, K. Characterization of the differential efficacy of austenitic vs martensitic NiTi rotary files in non-surgical root canal retreatment: A micro-CT analysis. Front. Biosci. 2021, 26, 465–474. [Google Scholar]
- Yılmaz, F.; Eren, İ.; Eren, H.; Badi, M.A.; Ocak, M.; Çelik, H.H. Evaluation of the Amount of Root Canal Dentin Removed and Apical Transportation Occurrence after Instrumentation with ProTaper Next, OneShape, and EdgeFile Rotary Systems. J. Endod. 2020, 46, 662–667. [Google Scholar] [CrossRef]
- Alghamdi, A.; Alsofi, L.; Balto, K. Effects of a Novel NiTi Thermomechanical Treatment on the Geometric Features of the Prepared Root Canal System. Materials 2020, 13, 5546. [Google Scholar] [CrossRef]
- Kırıcı, D.; Demirbuga, S.; Karataş, E. Micro-computed Tomographic Assessment of the Residual Filling Volume, Apical Transportation, and Crack Formation after Retreatment with Reciproc and Reciproc Blue Systems in Curved Root Canals. J. Endod. 2020, 46, 238–243. [Google Scholar]
- Radwański, M.; Łęski, M.; Pawlicka, H. The influence of the manufacturing process of rotary files on the shaping of L-shaped canals. Dent. Med. Probl. 2018, 55, 389–394. [Google Scholar] [CrossRef]
- Simpsy, G.S.; Sajjan, G.S.; Mudunuri, P.; Chittem, J.; Prasanthi, N.N.; Balaga, P. Shaping ability of reciprocating motion of WaveOne and HyFlex in moderate to severe curved canals: A comparative study with cone beam computed tomography. J. Conserv. Dent. 2016, 19, 578–582. [Google Scholar]
- Gagliardi, J.; Versiani, M.A.; de Sousa-Neto, M.D.; Plazas-Garzon, A.; Basrani, B. Evaluation of the Shaping Characteristics of ProTaper Gold, ProTaper NEXT, and ProTaper Universal in Curved Canals. J. Endod. 2015, 41, 1718–1724. [Google Scholar]
- Saber, S.E.; Nagy, M.M.; Schäfer, E. Comparative evaluation of the shaping ability of ProTaper Next, iRaCe and Hyflex CM rotary NiTi files in severely curved root canals. Int. Endod. J. 2015, 48, 131–136. [Google Scholar] [CrossRef]
- Peters, O.A.; Schonenberger, K.; Laib, A. Effects of four NiTi preparation techniques on root canal geometry assessed by micro computed tomography. Int. Endod. J. 2001, 34, 221–230. [Google Scholar]
- Česaitienė, G.; Venskutonis, T.; Mačiulskienė, V.; Cicėnas, V.; Samaitis, V.; Jasiūnienė, E. Micro-Computed Tomography (Micro-CT) Evaluation of Effects of Different Rotary Glide Path Techniques on Canal Transportation and Centering in Curved Root Canals. Med. Sci. Monit. 2019, 25, 6351–6358. [Google Scholar] [CrossRef]
- Marceliano-Alves, M.F.; Sousa-Neto, M.D.; Fidel, S.R.; Steier, L.; Robinson, J.P.; Pécora, J.D.; Versiani, M.A. Shaping ability of single-file reciprocating and heat-treated multifile rotary systems: A micro-CT study. Int. Endod. J. 2015, 48, 1129–1136. [Google Scholar] [CrossRef]
- Thompson, S.A. An overview of nickel-titanium alloys used in dentistry. Int. Endod. J. 2000, 33, 297–310. [Google Scholar]
- Osaki, R.B.; Bramante, C.M.; Vivan, R.R.; Alcalde, M.P.; Calefi, P.H.S.; Duarte, M.A.H. Influence of temperature on the torsional properties of two thermally treated NiTi rotary instruments. Braz. Dent. J. 2023, 34, 12–18. [Google Scholar] [CrossRef]
- Gavini, G.; Santos, M.D.; Caldeira, C.L.; Machado, M.E.L.; Freire, L.G.; Iglecias, E.F.; Peters, O.A.; Candeiro, G.T.M. Nickel-titanium instruments in endodontics: A concise review of the state of the art. Braz. Oral Res. 2018, 32 (Suppl. 1), e67. [Google Scholar]
- Liu, Y.; Chen, M.; Tang, W.; Liu, C.; Du, M. Comparison of five single-file systems in the preparation of severely curved root canals: An ex vivo study. BMC Oral Health 2022, 22, 649. [Google Scholar] [CrossRef]
- Al-Labed, H.; Layous, K.; Alzoubi, H. The Efficacy of Three Rotary Systems (Reciproc Blue, WaveOne Gold, and AF Blue R3) in Preparing Simulated, Highly Curved Root Canals: An In Vitro Study. Cureus 2022, 14, e30232. [Google Scholar] [CrossRef]
- Dantas, W.C.F.E.; Marceliano-Alves, M.F.V.; Marceliano, E.F.V.; Marques, E.F.; de Carvalho Coutinho, T.M.; Alves, F.R.F.; Martin, A.S.; Pelegrine, R.A.; Lopes, R.T.; Bueno, C.E.D.S. Microtomographic Assessment of the Shaping Ability of the Hyflex CM and XP-endo Shaper Systems in Curved Root Canals. Eur. J. Dent. 2022. ahead of print. [Google Scholar] [CrossRef]
- Scheid, R.C.; Weiss, G. Woelfel’s Dental Anatomy, 8th ed.; Lippincott, Williams & Wilkins: Ambler, PA, USA, 2012. [Google Scholar]
- Verma, P.; Love, R.M. A micro CT study of the mesiobuccal root canal morphology of the maxillary first molar tooth. Int. Endod. J. 2011, 44, 210–217. [Google Scholar] [CrossRef]
- Bolbolian, M.; Ramezani, M.; Valadabadi, M.; Alizadeh, A.; Tofangchiha, M.; Ghonche, M.R.A.; Reda, R.; Zanza, A.; Testarelli, L. Dentin Thickness of the Danger Zone in the Mesial Roots of the Mandibular Molars: A Cone Beam Computed Tomography Analysis. Front. Biosci. 2023, 15, 3. [Google Scholar] [CrossRef]
- Piasecki, L.; Makowka, S.R.; Gambarini, G. Anatomic Two-dimensional and Three-dimensional Models for Cyclic Fatigue Testing of Endodontic Instruments. Iran Endod. J. 2020, 15, 100–105. [Google Scholar]
- Paqué, F.; Musch, U.; Hülsmann, M. Comparison of root canal preparation using RaCe and ProTaper rotary Ni-Ti instruments. Int. Endod. J. 2005, 38, 8–16. [Google Scholar] [CrossRef]
- Pasternak-Júnior, B.; Sousa-Neto, M.D.; Silva, R.G. Canal transportation and centring ability of RaCe rotary instruments. Int. Endod. J. 2009, 42, 499–506. [Google Scholar] [CrossRef]
- Puleio, F.; Lo Giudice, G.; Militi, A.; Bellezza, U.; Lo Giudice, R. Does Low-Taper Root Canal Shaping Decrease the Risk of Root Fracture? A Systematic Review. Dent. J. 2022, 10, 94. [Google Scholar] [CrossRef]
- Ruddle, C. Cleaning and shaping the root canal system. In Pathways of the Pulp, 8th ed.; Cohen, S., Burns, R.C., Eds.; Mosby: St. Louis, MO, USA, 2002; pp. 231–292. [Google Scholar]
- Greene, K.J.; Krell, K.V. Clinical factors associated with ledged canals in maxillary and mandibular molars. Oral Surg. Oral Med. Oral Pathol. 1990, 70, 490–497. [Google Scholar] [CrossRef]
- González Sánchez, J.A.; Duran-Sindreu, F.; de Noé, S.; Mercadé, M.; Roig, M. Centring ability and apical transportation after overinstrumentation with ProTaper Universal and ProFile Vortex instruments. Int. Endod. J. 2012, 45, 542–551. [Google Scholar] [CrossRef]
- Yoo, Y.S.; Cho, Y.B. A comparison of the shaping ability of reciprocating NiTi instruments in simulated curved canals. Restor. Dent. Endod. 2012, 37, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Melo, M.C.; Pereira, E.S.; Viana, A.C.; Fonseca, A.M.; Buono, V.T.; Bahia, M.G. Dimensional characterization and mechanical behaviour of K3 rotary instruments. Int. Endod. J. 2008, 41, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Sabala, C.L.; Roane, J.B.; Southard, L.Z. Instrumentation of curved canals using a modified tipped instrument: A comparison study. J. Endod. 1988, 14, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Powell, S.E.; Wong, P.D.; Simon, J.H.S. A comparison of the effect of modified and non-modified instrument tips on apical canal configuration. Part II. J. Endod. 1988, 14, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Ponce de Leon Del Bello, T.; Wang, N.; Roane, J.B. Crown-down tip design and shaping. J. Endod. 2003, 29, 513–518. [Google Scholar]
- Saricam, E.; Kayaoglu, G. Comparison of OneShape, 2Shape and One Curve endodontic instruments for debris and irrigant extrusion. Dent. Med. Probl. 2020, 57, 255–259. [Google Scholar] [CrossRef] [PubMed]
- De-Deus, G.; Silva, E.J.; Vieira, V.T.; Belladonna, F.G.; Elias, C.N.; Plotino, G.; Grande, N.M. Blue thermomechanical treatment optimizes fatigue resistance and flexibility of the Reciproc files. J. Endod. 2017, 43, 462–466. [Google Scholar] [CrossRef]
- Prados-Privado, M.; Rojo, R.; Ivorra, C.; Prados-Frutos, J.C. Finite element analysis comparing WaveOne, WaveOne Gold, Reciproc and Reciproc Blue responses with bending and torsion tests. J. Mech. Behav. Biomed. Mater. 2019, 90, 165–172. [Google Scholar] [CrossRef]
- Özyürek, T.; Yılmaz, K.; Uslu, G. Shaping Ability of Reciproc, WaveOne GOLD, and HyFlex EDM Single-file Systems in Simulated S-shaped Canals. J. Endod. 2017, 43, 805–809. [Google Scholar] [CrossRef]
- Bürklein, S.; Benten, S.; Schäfer, E. Shaping ability of different single-file systems in severely curved root canals of extracted teeth. Int. Endod. J. 2013, 46, 590–597. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).