Multiple-Criteria Decision-Making for Medical Rescue Operations during Mass Casualty Incidents
Abstract
1. Introduction
- Selection of Hospital Emergency Departments where emergency treatment should be implemented and preparation for specialist treatment in the hospital setting, enabling the most effective medical handling of the incident [10].
- Allocation of medical transport means (Medical Rescue Teams—MRTs) transport those injured in the incident to their assigned ED. A distinction is made between basic and specialized modes of transport. The latter also includes HEMS (Helicopter Emergency Medical Service) air units.
2. Literature Review
- The expected value of survival of the injured in the MCI depends on the post-accident status of the injured person [13,17,41]. In [16], the author conducted research on the change in the probability of survival of the injured over time due to the group of medical segregation to which these persons were assigned. In [16], the author described the survival time of people due to belonging to a segregating group with an appropriate logistic function. In [11], the author took into account the expected value of the casualty’s survival due to the post-accident condition.
- Availability of hospital emergency department (HED) resources and the effectiveness of treatment of individual post-traumatic conditions. In [42,43], an analysis was made of the appointment of specific personnel to treat a specific medical case—the post-accident state of the injured. In [13], the number of operating rooms was taken into account when determining the target HED. In [12], the availability of vacant places of treatment centers, both existing and created temporarily after the MCI, was analyzed.
- The time elapses from the occurrence of the MCI to the moment of medical rescue operations at the scene. In [12], an analysis of the problem of minimizing the total transport time and the waiting of injured persons for medical service during the search and rescue operation was carried out.
- The time that elapses from the moment of the event to the commencement of emergency treatment in the HED. The presented literature analysis shows that the effectiveness of rescue actions in a mass incident is largely determined by the time after which emergency treatment is undertaken [12] in the HED. The quality of the access routes has a great influence on the time of reaching the means of emergency medical transport both to the place of the accident and to the HED. In [44], among others, the number and distribution of event sites and hospitals, as well as the degree of disruption to individual sections of the route, were considered.
- the expected value of the death and
- the expected value of the disability.
- the expected value of the cost of a rescue operation and
- the expected value of the cost of long-term treatment and rehabilitation.
3. Mathematical Description of the Medical Rescue Operations after Mass Casualty Incident
3.1. Characteristics of the Directed Emergency System
3.2. Characteristics of the Mass Casualty Incident
3.3. Characteristics of the Health Condition of People Injured in a Mass Casualty Incident
3.3.1. Severity of the Traumatic State
3.3.2. State of Consciousness
3.3.3. Degree of Basic Life Dysfunctions
3.4. Rules for Qualifying Injured to Medical Priority Groups
- means immediate medical operations upon arrival of emergency services.
- means urgent medical operations with a possible delay.
- means medical operations with a delay of up to several hours.
- means resignation from medical care. This is the priority group of injured people who are not expected to survive the next 24 h.
3.5. Quantities Characterizing Medical Rescue Operations of DES during MCI
4. Formulation of the Optimization Problem
- The MRTB from which the MRT should be allocated.
- the HED to which the injured person should be taken.
- the mode of MRT which should be chosen.
- —objective function due to the -th criterion for evaluating the effectiveness of DES activities for decision variables vector . There are four objective functions of DES effectiveness:
- —the expected value of death,
- —the expected value of disability,
- —the expected value of the cost of carrying out the rescue operation and
- —the expected value of long-term treatment and rehabilitation costs.
- for each injured person, exactly one mode of MRT is taken, and exactly one HED is assigned to treat this person:
- The number of MRTs already assigned to transport service cannot exceed the number of still available MRTs:
- The number of HED beds assigned for injured persons cannot exceed a limit of vacant beds in a certain HED:
- The assignment of the HED and the MRT mode to each person can take exactly one of two values zero or one (binary variable constraint), i.e.,
5. Computer Simulator for Optimal Decision-Making in Medical Rescue Operations
- different multi-criteria optimization methods and their parameters,
- different computing environments (optimization software modules),
- different boundary conditions that describe the MCI and
- scale (size) of the MCI.
- the weighted sum method,
- the weighted global criterion method,
- the hierarchical optimization method and
- the e-constraint method (bounded objective function method).
6. Results and Discussion
- eight people are injured, L = 8,
- injuries encountered are specified in Table 2,
- health condition of injured people is summarized in Table 3,
- the time that elapsed from the moment of occurrence of the incident to the moment of notifying the DES about this incident is (0.2 h = 12 min),
- the optimization problem is solved with the method of the sum of weighted criteria, and the following weight values describing the effectiveness of DES activities are taken: ; it is also noted that the human’s life is the most important factor. Therefore it is assumed that ,
- the logistic function describing the probability of an injured person’s death according to their treatment priority group defined by Equation (35) is set in Table 7. Parameters of the other criteria are intentionally skipped,
- the optimal solution is solved using the LINDO API math software module and
- a more detailed dataset from this example created and used in the CSMRO is available in the open-access repository at the link [56].
- detailed statistical analysis of actual mass incidents to identify the relationship between the various post-accident conditions of the injured and the expected values of death, disability and long-term medical costs;
- dynamic analysis of the current situation at the scene of a mass casualty incident by taking into account the time factor and
- analysis of very large-scale tasks.
7. Conclusions
- significantly shorten the time of decision-making in mass casualty incident handling,
- improve the accuracy of decisions regarding medical care of the injured,
- reduce the stress factor in DES physicians by supporting the decisions made,
- maximize the use of DES forces and resources available at a given moment and
- eliminate information chaos and minimize the risk of making a mistake.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, S.J.; Kim, C.H.; Shin, S.D.; Lee, S.C.; Park, J.O.; Sung, J. Incidence and mortality rates of disasters and mass casualty incidents in Korea: A population-based cross-sectional study, 2000–2009. J. Korean Med. Sci. 2013, 28, 658–666. [Google Scholar] [CrossRef]
- Collins, S.; James, T.; Carter, H.; Symons, C.; Southworth, F.; Foxall, K.; Marczylo, T.; Amlôt, R. Mass casualty decontamination for chemical incidents: Research outcomes and future priorities. Int. J. Environ. Res. Public Health 2021, 18, 3079. [Google Scholar] [CrossRef]
- Holgersson, A.; Björnstig, U. Mass-casualty attacks on public transportation. J. Transp. Secur. 2014, 7, 1–16. [Google Scholar] [CrossRef]
- Rauner, M.S.; Schaffhauser-Linzatti, M.M.; Niessner, H. Resource planning for ambulance services in mass casualty incidents: A DES-based policy model. Health Care Manag. Sci. 2012, 15, 254–269. [Google Scholar] [CrossRef] [PubMed]
- Bazyar, J.; Farrokhi, M.; Khankeh, H. Triage systems in mass casualty incidents and disasters: A review study with a worldwide approach. Open Access Maced J. Med. Sci. 2019, 7, 482–494. [Google Scholar] [CrossRef]
- Iyengar, K.P.; Venkatesan, A.S.; Jain, V.K.; Shashidhara, M.K.; Elbana, H.; Botchu, R. Risks in the management of polytrauma patients: Clinical insights. Orthop. Res. 2023, 15, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Varshney, K.; Mallows, J.; Hamd, M. Disaster triage tags: Is one better than another? Emerg. Med. Australas. 2012, 24, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Challen, K.; Walter, D. Major incident triage: Comparative validation using data from 7th July bombings. Injury 2013, 44, 629–633. [Google Scholar] [CrossRef]
- Postma, I.L.; Weel, H.; Heetveld, M.J.; van der Zande, I.; Bijlsma, T.S.; Bloemers, F.W.; Goslings, J.C. Mass casualty triage after an airplane crash near Amsterdam. Injury 2013, 44, 1061–1067. [Google Scholar] [CrossRef]
- Wilson, D.T.; Hawe, G.I.; Coates, G.; Crouch, R.S. Effective allocation of casualties to hospitals in mass casualty incidents. In Proceedings of the IEEE 3rd International Conference on Emergency Management and Management Sciences (ICEMMS), Beijing, China, 1–8 January 2013. [Google Scholar]
- Dean, M.D.; Nair, S.K. Mass-casualty triage: Distribution of victims to multiple hospitals using the save model. Eur. J. Oper. Res. 2014, 238, 363–373. [Google Scholar] [CrossRef]
- Salman, F.S.; Gül, S. Deployment of field hospitals in mass casualty incidents. Comput. Ind. Eng. 2014, 74, 37–51. [Google Scholar] [CrossRef]
- Cotta, C. Effective patient prioritization in mass casualty incidents using hyperheuristics and the pilot method. OR Spectr. 2011, 33, 699–720. [Google Scholar] [CrossRef]
- Güttinger, D.; Godehardt, E.; Zinnen, A. Online strategies for optimizing medical supply in disaster scenarios. In Proceedings of the IEEE International Conference on Service Operations, Logistics, and Informatics (SOLI), Beijing, China, 10–12 July 2011; pp. 38–44. [Google Scholar]
- Gabdulkhakova, A.; König-Ries, B.; Rizvanov, D. Rational resource allocation in mass casualty incidents–adaptivity and efficiency. In Proceedings of the 9th International ISCRAM Conference, Vancouver, BC, Canada, 22–25 April 2012; pp. 1–5. [Google Scholar]
- Mills, A.F.; Argon, N.T.; Ziya, S. Resource-based patient prioritization in mass-casualty incidents. Manuf. Serv. Oper. Manag. 2013, 15, 361–377. [Google Scholar] [CrossRef]
- Wilson, D.T.; Hawe, G.I.; Coates, G.; Crouch, R.S. A multi-objective combinatorial model of casualty processing in major incident response. Eur. J. Oper. Res. 2013, 230, 643–655. [Google Scholar] [CrossRef]
- Kilic, A.; Dincer, M.C.; Gokce, M.A. Determining optimal treatment rate after a disaster. J. Oper. Res. Soc. 2014, 65, 1053–1067. [Google Scholar] [CrossRef]
- Chu, X.; Zhong, Q. Post-earthquake allocation approach of medical rescue Teams. Nat. Hazards 2015, 79, 1809–1824. [Google Scholar] [CrossRef]
- Chu, X.; Zhong, Q.; Khokhar, S.G. Triage scheduling optimization for mass casualty and disaster response. Asia-Pac. J. Oper. Res. 2015, 32, 1550041. [Google Scholar] [CrossRef]
- Huang, K.; Jiang, Y.; Yuan, Y.; Zhao, L. Modeling multiple humanitarian objectives in emergency response to large-scale disasters. Transp. Res. Part E Logist. Transp. Rev. 2015, 75, 1–17. [Google Scholar] [CrossRef]
- Saisubramanian, S.; Varakantham, P.; Lau, H.C. Risk based optimization for improving emergency medical systems. In Proceedings of the Twenty-Ninth AAAI Conference on Artificial Intelligence, Austin, TX, USA, 25–30 January 2015; pp. 25–30. [Google Scholar]
- Debacker, M.; Van Utterbeeck, F.; Ullrich, C.; Dhondt, E.; Hubloue, I. SIMEDIS: A discrete-event simulation model for testing responses to mass casualty incidents. J. Med. Syst. 2016, 40, 273. [Google Scholar] [CrossRef]
- Luscombe, R.; Kozan, E. Dynamic resource allocation to improve emergency department efficiency in real time. Eur. J. Oper. Res. 2016, 255, 593–603. [Google Scholar] [CrossRef]
- Mills, A.F. A simple yet effective decision support policy for mass-casualty triage. Eur. J. Oper. Res. 2016, 253, 734–745. [Google Scholar] [CrossRef]
- Repoussis, P.P.; Paraskevopoulos, D.C.; Vazacopoulos, A.; Hupert, N. Optimizing emergency preparedness and resource utilization in mass-casualty incidents. Eur. J. Oper. Res. 2016, 255, 531–544. [Google Scholar] [CrossRef]
- Sung, I.; Lee, T. Optimal allocation of emergency medical resources in a mass casualty incident: Patient prioritization by column generation. Eur. J. Oper. Res. 2016, 252, 623–634. [Google Scholar] [CrossRef]
- Wilson, D.T.; Hawe, G.I.; Coates, G.; Crouch, R.S. Online optimization of casualty processing in major incident response: An experimental analysis. Eur. J. Oper. Res. 2016, 252, 334–348. [Google Scholar] [CrossRef]
- Kamali, B.; Bish, D.; Glick, R. Optimal service order for mass-casualty incident response. Eur. J. Oper. Res. 2017, 261, 355–367. [Google Scholar] [CrossRef]
- Niessner, H.; Rauner, M.S.; Gutjahr, W.J. A dynamic simulation-optimization approach for managing mass casualty incidents. Oper. Res. Health Care 2018, 17, 82–100. [Google Scholar] [CrossRef]
- Lee, H.; Lee, T. Multi-agent reinforcement learning algorithm to solve a partially-observable multi-agent problem in disaster response. Eur. J. Oper. Res. 2021, 291, 296–308. [Google Scholar] [CrossRef]
- Wang, C.-N.; Yang, F.-C.; Vo, N.T.M.; Nguyen, V.T.T. Wireless communications for data security: Efficiency assessment of cybersecurity industry—A promising application for uavs. Drones 2022, 6, 363. [Google Scholar] [CrossRef]
- Dang, T.-T.; Nguyen, N.-A.-T.; Nguyen, V.-T.-T.; Dang, L.-T.-H. A two-stage multi-criteria supplier selection model for sustainable automotive supply chain under uncertainty. Axioms 2022, 11, 228. [Google Scholar] [CrossRef]
- Baghaian, A.; Lotfi, M.M.; Rezapour, S. Integrated deployment of local urban relief teams in the first hours after mass casualty incidents. Int. J. Oper. Res. 2022, 22, 4517–4555. [Google Scholar] [CrossRef]
- Olivia, D.; Amrutha, C.; Nayak, A.; Balachandra, M.; Saxena, A. Clinical severity level prediction based optimal medical resource allocation at mass casualty incident. IEEE Access 2022, 10, 88970–88984. [Google Scholar] [CrossRef]
- DuBois, E.; Albert, L.A. Dispatching policies during prolonged mass casualty incidents. J. Oper. Res. Soc. 2022, 73, 2536–2550. [Google Scholar] [CrossRef]
- Chang, K.; Chen, T.; Yang, F.; Chang, T. Simulation optimization for stochastic casualty collection point location and resource allocation problem in a mass casualty incident. Eur. J. Oper. Res. 2023, 309, 1237–1262. [Google Scholar] [CrossRef]
- Chen, M.; Sharma, A.; Bhola, J.; Nguyen, T.V.; Truong, C.V. Multi-agent task planning and resource apportionment in a smart grid. Int. J. Syst. Assur. Eng. Manag. 2022, 13 (Suppl. 1), 444–455. [Google Scholar] [CrossRef]
- Ullah, F.; Khelil, A.; Sheikh, A.A.; Felemban, E.; Bojan, H.M.A. Towards automated self-tagging in emergency health cases. In Proceedings of the IEEE 15th International Conference on e-Health Networking, Applications & Services (Healthcom), Lisbon, Portugal, 9–12 October 2013; pp. 658–663. [Google Scholar]
- Mizumoto, T.; Imazu, S.; Sun, W.; Shibata, N.; Yasumoto, K. Emergency medical support system for visualizing locations and vital signs of patients in mass casualty incident. In Proceedings of the 2012 IEEE International Conference on Pervasive Computing and Communications Workshops (PERCOM Workshops), Lugano, Switzerland, 19–23 March 2012; pp. 740–745. [Google Scholar]
- Wilson, D.T.; Hawe, G.I.; Coates, G.; Crouch, R.S. Modeling uncertain and dynamic casualty health in optimization-based decision support for mass casualty incident response. Int. J. Inf. Syst. Crisis Response Manag. 2013, 5, 32–44. [Google Scholar] [CrossRef]
- Güttinger, D.; Godehardt, E.; Zinnen, A. Optimizing emergency supply for mass events. In Proceedings of the SIMUTools 2011—4th International ICST Conference on Simulation Tools and Techniques, Barcelona, Spain, 21–25 March 2011; pp. 125–133. [Google Scholar]
- Majchrzak, T.A.; Noack, O.; Neuhaus, P.; Ückert, F. Supporting the allocation of traumatized patients with a decision support system. In Using Social and Information Technologies for Disaster and Crisis Management; Murray, J.E., Ed.; IGI Global: Hershey, PA, USA, 2013; Chapter 11; pp. 166–181. [Google Scholar]
- Wilson, D.T.; Hawe, G.I.; Coates, G.; Crouch, R.S. Evaluation of centralised and autonomous routing strategies in major incident response. Saf. Sci. 2014, 70, 80–88. [Google Scholar] [CrossRef]
- Sujan, A. The Glasgow Coma Scale: A breakthrough in the assessment of the level of consciousness. J. Tradit. Med. Clin. Naturop. 2018, 7, 1–2. [Google Scholar] [CrossRef]
- Lowes, A.J.; Cosgrove, J.F. Prehospital organization and management of a mass casualty incident. BJA Educ. 2016, 16, 323–328. [Google Scholar] [CrossRef]
- Tomczyk, Ł.; Kulesza, Z. A method of prioritizing victims of a mass casualty event for managing medical rescue operations. Control Cybern. 2016, 45, 355–370. [Google Scholar]
- Jain, S.; Iverson, L.M. Glasgow Coma Scale; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK513298/ (accessed on 21 June 2022).
- Marler, R.; Arora, J. Survey of multi-objective optimization methods for engineering. Struct. Multidiscip. Optim. 2004, 26, 369–395. [Google Scholar] [CrossRef]
- Gunantara, N. A review of multi-objective optimization: Methods and its applications. Cogent Eng. 2018, 5, 1502242. [Google Scholar] [CrossRef]
- Rahmani, A.; Yousefikhoshbakht, M. An effective branch-and-cut algorithm in order to solve the mixed integer bi-level programming. Int. J. Prod. Manag. Eng. 2017, 5, 1–10. [Google Scholar] [CrossRef]
- LINDO API 14—Powerful Library of Optimization Solvers and Mathematical Programming Tools. Available online: https://www.lindo.com/index.php/products/lindo-api-for-custom-optimization-application (accessed on 22 May 2023).
- IBM ILOG CPLEX Optimization Studio. Available online: https://www.ibm.com/products/ilog-cplex-optimization-studio/cplex-optimizer (accessed on 22 May 2023).
- MATLAB—Mathworks. Available online: https://www.mathworks.com/products/matlab.html (accessed on 22 May 2023).
- Mosek. Available online: https://www.mosek.com/products/mosek/ (accessed on 22 May 2023).
- CSMRO—Dataset—Repository with Dataset Used by the CSMRO. Available online: https://1drv.ms/f/s!AjeUC4hqzRxngStr0YquDdJngnq4?e=ZDXFCG (accessed on 23 June 2023).
| Symbol of the Computational Environment | Name of the Computational Environment | Optimal Solution Method Applied in the Computational Environment |
|---|---|---|
| S1 | LINDO API [52] | int lindo.LSsolveMIP(IntPtr pModel, ref int pnMIPSolStatus) |
| S2 | CPLEX [53] | bool Cplex.Solve() |
| S3 | MATLAB [54] | intlinprog(objective, intcon, A_ineq, b_ineq, A_eq, b_eq, lb, ub, options) |
| S4 | MOSEK [55] | mosek.rescode mosek.Task.optimize() |
| u-th Trauma | Trauma | n-th Degree of Severity |
|---|---|---|
| 1 | flesh wound | 1 |
| 2 | burns up to 10% below 3rd degree | 1 |
| 3 | forearm fracture | 1 |
| 4 | feet fracture | 1 |
| 5 | hand fracture | 1 |
| 6 | spine injury | 2 |
| 7 | hip injury | 2 |
| 8 | shoulder injury | 2 |
| 9 | isolated fracture of the lower leg bones | 3 |
| 10 | traumatic limb amputation | 3 |
| 11 | hypothermia | 3 |
| 12 | head injury | 3 |
| 13 | unstable chest | 3 |
| 14 | shock | 3 |
| 15 | severe skull injury | 4 |
| 16 | brain tissue damage | 4 |
| 17 | extensive crushing | 4 |
| Injured Number l | The Severity of the Traumatic State | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 1, 6 | 2 | 15 | 11 | 1 | 0 | 30 |
| 2 | 15 | 4 | 3 | 1 | 1 | 0 | 34 |
| 3 | 8, 14 | 3 | 9 | 8 | 1 | 0 | 22 |
| 4 | 8 | 2 | 15 | 10 | 0 | 0 | 24 |
| 5 | 11 | 3 | 14 | 10 | 1 | 0 | 46 |
| 6 | 1, 5 | 1 | 15 | 12 | 0 | 1 | 27 |
| 7 | 7 | 2 | 15 | 10 | 0 | 0 | 50 |
| 8 | 11, 12 | 3 | 11 | 8 | 1 | 0 | 57 |
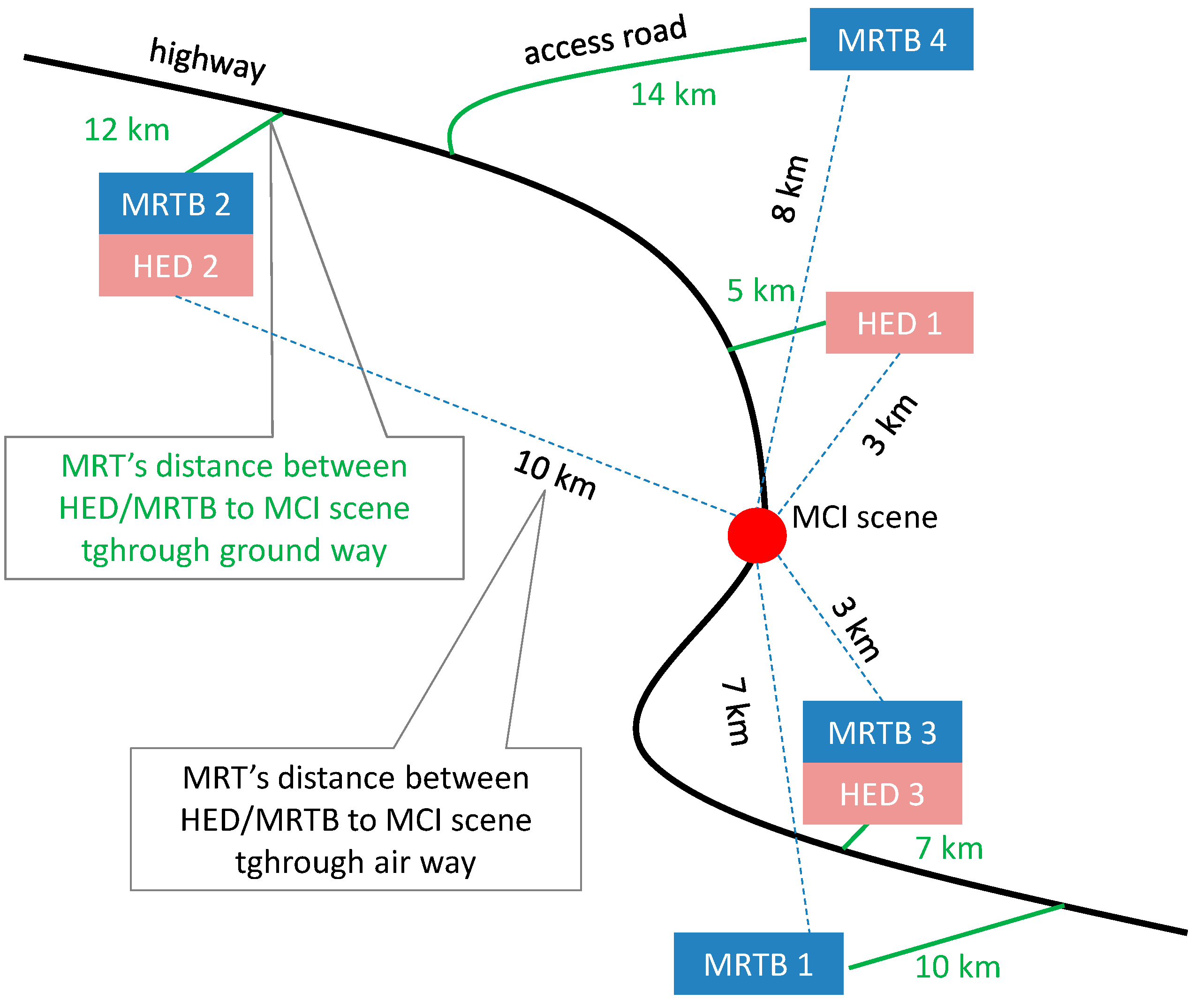
| HED’s Number s | Distance from the HED
to the Scene of the MCI
in Kilometers | Number of Injured People That Can Be Handled by the s-th HED | A Set of Types of Post-Accident Injuries Handled by the s-th HED | |
|---|---|---|---|---|
| for the Ground Type of the MRT () | for the Air Type of the MRT () | |||
| 1 | 5 | 3 | 10 | 1, 7, 8, 9, 10, 11, 12 |
| 2 | 12 | 10 | 10 | 3, 4, 5, 6, 7, 14 |
| 3 | 7 | 3 | 10 | 1, 2, 3, 4, 5, 6, 7, 8, 9, 13, 15 |
| Number of the MRTB b | Distance from the MRTB to the Scene of the MCI in Kilometers | Number of the r-th Mean of the MRT from the b-th MRTB ab,2,r | |
|---|---|---|---|
| for the Ground Type of the MRT () | for the Air Type of the MRT () | ||
| 1 | 10 | 7 | <10,10> |
| 2 | 12 | 10 | <10,10> |
| 3 | 7 | 3 | <10,10> |
| 4 | 14 | 8 | <10,10> |
| Number of the Transport Mode r | Transport Mode | Average Speed Vr of the r-th Transport Mode in Kilometers per Hour |
|---|---|---|
| 1 | air | 60 |
| 2 | ground | 250 |
| Priority Group’s Number g | Logistic Function Parameter | Logistic Function Parameter |
|---|---|---|
| 1 | 30 | 0.25 |
| 2 | 30 | 0.58(3) |
| 3 | 12 | 1.16(6) |
| 4 | 30 | 0.08(3) |
| Injured Person Number l | Priority Group Number g of the l-th Injured Person |
|---|---|
| 1 | 2 |
| 2 | 4 |
| 3 | 1 |
| 4 | 2 |
| 5 | 1 |
| 6 | 3 |
| 7 | 2 |
| 8 | 1 |
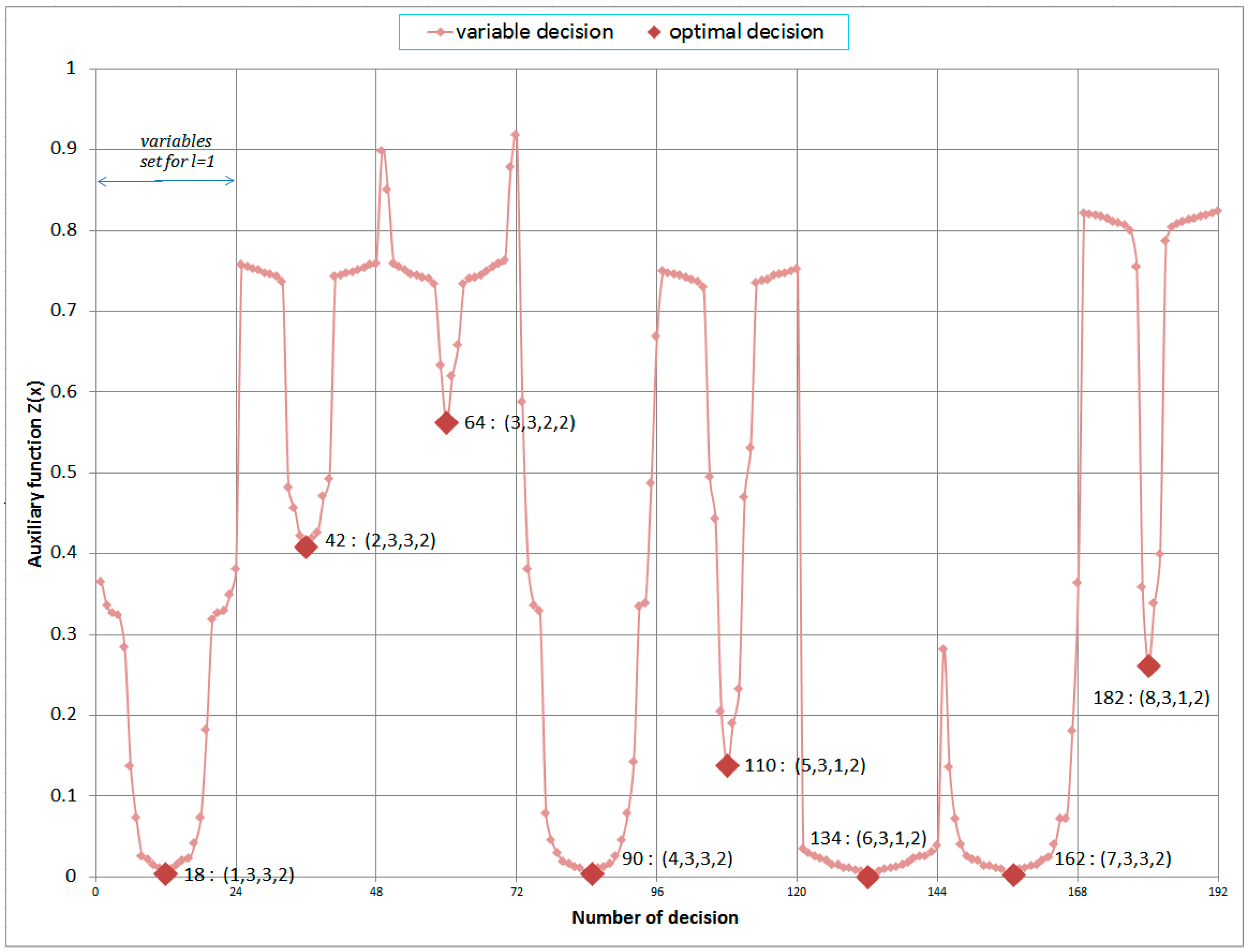
| Number of Non-Zero Decision Variables | Number of the Injured Persons | Number of the MRTB | Number of the HED | Number of the MRT Type | as Defined in Equation (46) | as Defined in Equation (34) |
|---|---|---|---|---|---|---|
| 18 | 1 | 3 | 3 | 2 | 0.00315323 | 0.224 (13 min 44 s) |
| 42 | 2 | 3 | 3 | 2 | 0.40871449 | 0.224 (13 min 44 s) |
| 64 | 3 | 3 | 2 | 2 | 0.56225483 | 0.252 (15 min 12 s) |
| 90 | 4 | 3 | 3 | 2 | 0.00425728 | 0.224 (13 min 44 s) |
| 110 | 5 | 3 | 1 | 2 | 0.13780012 | 0.224 (13 min 44 s) |
| 134 | 6 | 3 | 1 | 2 | 0.00012702 | 0.224 (13 min 44 s) |
| 162 | 7 | 3 | 3 | 2 | 0.00280106 | 0.224 (13 min 44 s) |
| 182 | 8 | 3 | 1 | 2 | 0.26127769 | 0.224 (13 min 44 s) |
| Literature Reference | Optimization Method | Is Multi-Criteria | New Method of Triage or Currently in Practice START | Injured Persons Health Modelling | Complete Service (Injured Assigned to the Certain MRT and ED) |
|---|---|---|---|---|---|
| Rauner et al. [4] | Discrete-event simulation | no | START | no | yes |
| Cotta [13] | Hyperheuristic | no | START | no | no |
| Güttinger et al. [14] | D’Hondt, greedy strategy simulated annealing | no | START | no | yes |
| Wilson et al. [17] | Fixed Job Scheduling Problem Variable Neighborhood Search (VNS) metaheuristics and its deterministic variant Variable Neighborhood Descent (VND) | yes | START | no | yes |
| Dean and Nair [11] | MIP | no | START | no | yes |
| Kilic et al. [18] | Pontryagin’s minimum principle | no | START | no | yes |
| Chu et al. [20] | MIP Flexible job shop scheduling model and a genetic algorithm | no | START | no | yes |
| Repoussis et al. [26] | MIP | no | START | no | yes |
| Sung and Lee [27] | LP, column generation | no | START | no | yes |
| Chang et al. [37] | Rapid-screening algorithm and an adaptive particle global and hyperbox local search | no | START | no | yes |
| The proposed model | MIP | yes | new | yes | yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomczyk, L.; Kulesza, Z. Multiple-Criteria Decision-Making for Medical Rescue Operations during Mass Casualty Incidents. Appl. Sci. 2023, 13, 7467. https://doi.org/10.3390/app13137467
Tomczyk L, Kulesza Z. Multiple-Criteria Decision-Making for Medical Rescue Operations during Mass Casualty Incidents. Applied Sciences. 2023; 13(13):7467. https://doi.org/10.3390/app13137467
Chicago/Turabian StyleTomczyk, Lukasz, and Zbigniew Kulesza. 2023. "Multiple-Criteria Decision-Making for Medical Rescue Operations during Mass Casualty Incidents" Applied Sciences 13, no. 13: 7467. https://doi.org/10.3390/app13137467
APA StyleTomczyk, L., & Kulesza, Z. (2023). Multiple-Criteria Decision-Making for Medical Rescue Operations during Mass Casualty Incidents. Applied Sciences, 13(13), 7467. https://doi.org/10.3390/app13137467






