Hand Joint Hypermobility among Dental Students—A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Study Procedure
2.3. Assessment of Outcome Measures
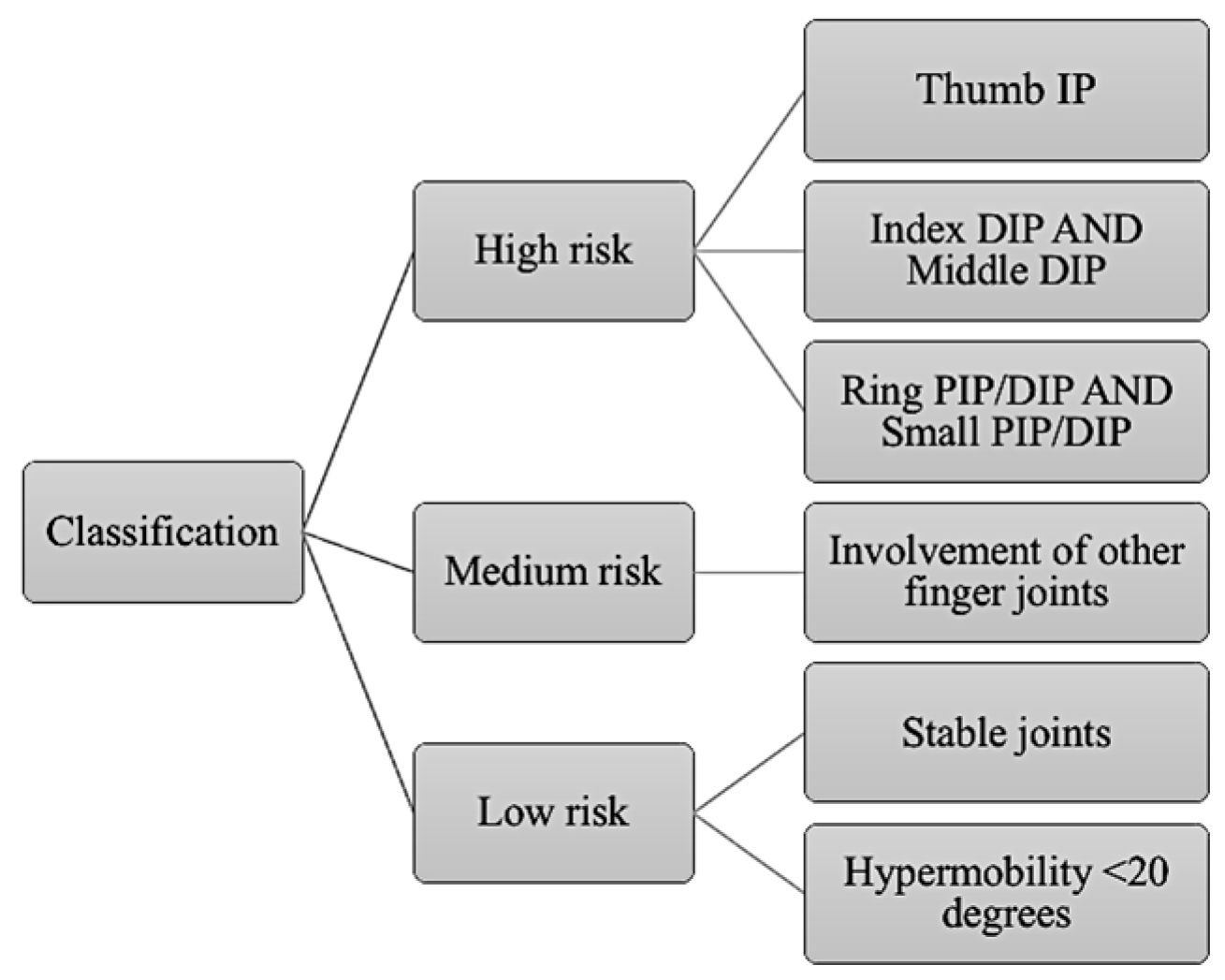
- at high risk, if hyperextension of multiple joints was observed, with particular emphasis on specific fingers used as fulcrum during dental procedures. Specifically, participants were considered at high risk if hypermobility was observed in the thumb IP, in the index DIP and in the middle DIP fingers, or in the ring PIP/DIP and in the small PIP/DIP fingers.
- at medium risk, if the participants’ hypermobility involved joints which are not strictly considered as important for finger rest;
- at low risk, if joints appeared stable with little to no hypermobility (i.e., <20 degrees observed).
2.4. Statistical Analysis
3. Results
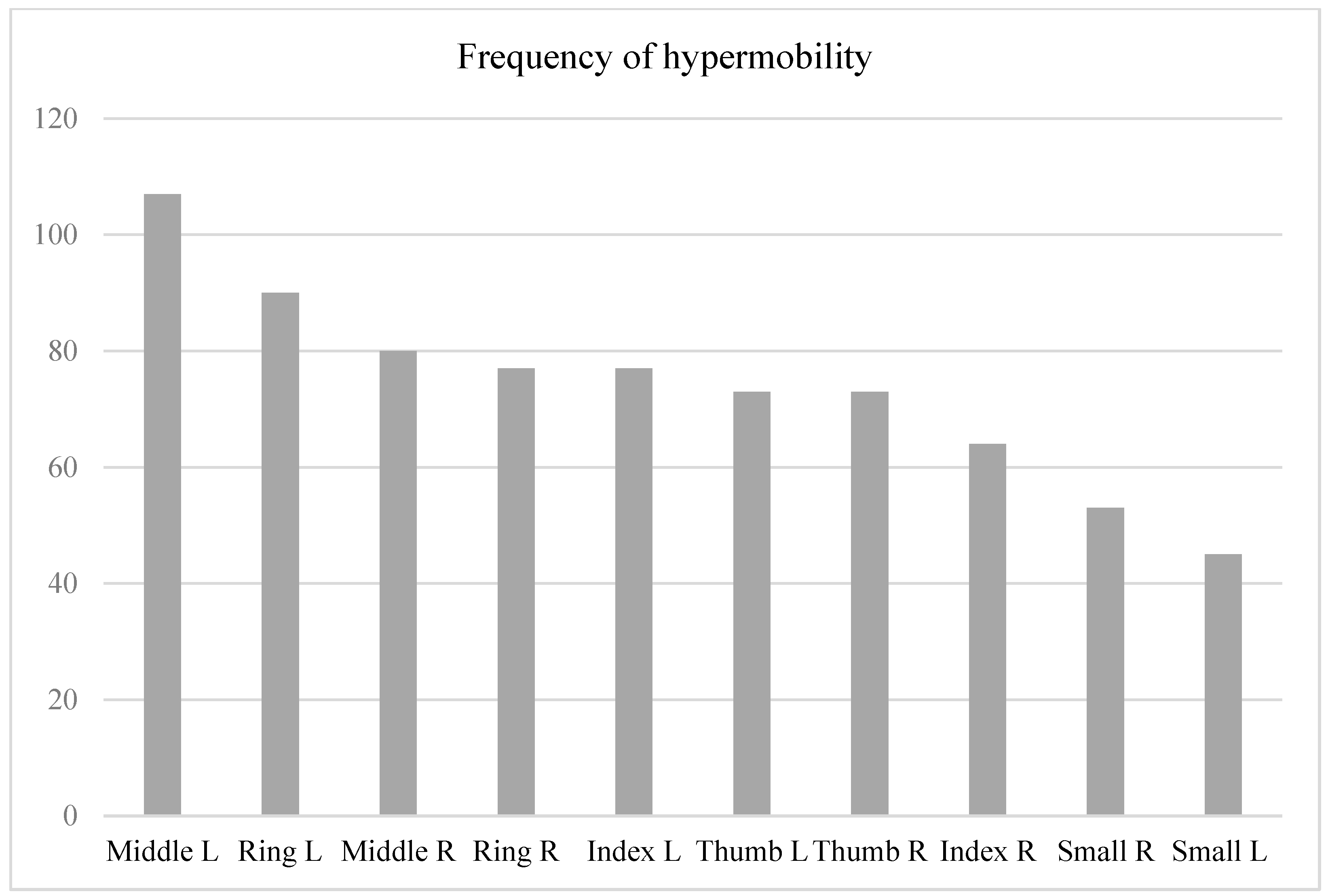
3.1. Aim 1: Prevalence of Hand Joint Hypermobility
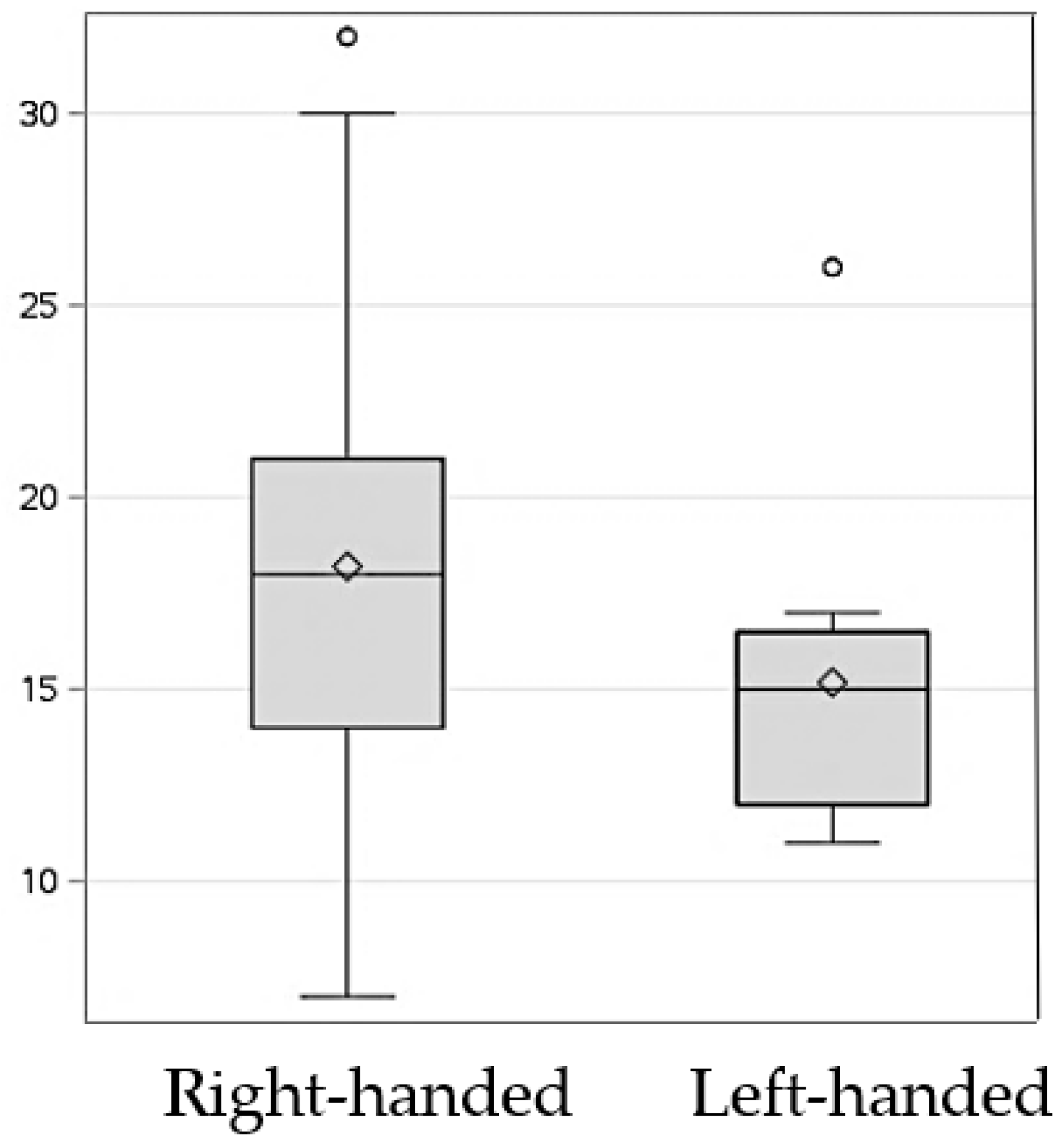
3.2. Aim 2: Correlation between Hypermobility and Muscular Strength
4. Discussion
4.1. High Prevalence of Hand Joint Hypermobility among a Cohort of Dental Students
4.2. Hypermobility Is Associated with Lower Muscle Strength
4.3. Future Directions
4.4. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jensen, A.-M.; Andersen, J.Q.; Quisth, L.; Ramstrand, N. Finger orthoses for management of joint hypermobility disorders: Relative effects on hand function and cognitive load. Prosthet. Orthot. Int. 2020, 45, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Boyle, K.L.; Witt, P.; Riegger-Krugh, C. Intrarater and interrater reliaility of the Brighton and Horan Joint Mobility Index. J. Athl. Train. 2003, 38, 281–285. [Google Scholar] [PubMed]
- Kobayasi, T. Dermal elastic fibres in the inherited hypermobile disorders. J. Dermatol. Sci. 2006, 41, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Szalewska, M.; Lupa, M.; Pochroń, N.; Pudzianowski, S.; Szalewski, L.; Bożyk, A.; Borowicz, J. Prevalence of Joint Hypermobility Syndrome Amongst Dental Students of the Medical University of Lublin. Pol. J. Public Health 2014, 125, 73–76. [Google Scholar] [CrossRef]
- Grahame, R.; Halkim, A.J. Hypermobility. Curr. Opin. Rheumatol. 2008, 20, 106–110. [Google Scholar] [CrossRef]
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A framework for the classification of joint hypermobility and related conditions. Am. J. Med. Genet. Part C Semin. Med Genet. 2017, 174, 148–157. [Google Scholar] [CrossRef]
- Remvig, L.; Jensen, D.V.; Ward, R.C. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: Review of the literature. J. Rheumatol. 2007, 34, 804–809. [Google Scholar]
- Antonio, D.H.; Magalhães, C.S. Survey on joint hypermobility in university students aged 18–25 years old. Adv. Rheumatol. 2018, 58, 3. [Google Scholar] [CrossRef]
- Larsson, L.-G.; Baum, J.; Mudholkar, G.S. Hypermobility: Features and differential incidence between the sexes. Arthritis Rheum. 1987, 30, 1426–1430. [Google Scholar] [CrossRef]
- Kirk, J.A.; Ansell, B.M.; Bywaters, E.G. The hypermobility syndrome: Musculoskeletal complaints associated with generalized joint hypermobility. Ann. Rheum. Dis. 1967, 26, 419–425. [Google Scholar] [CrossRef]
- Ituen, O.A.; Anieto, E.M.; Ferguson, G.; Duysens, J.; Smits-Engelsman, B. Prevalence and Demographic Distribution of Hypermobility in a Random Group of School-Aged Children in Nigeria. Healthcare 2023, 11, 1092. [Google Scholar] [CrossRef] [PubMed]
- Clayton, H.A.; Jones, S.A.H.; Henriques, D.Y.P. Proprioceptive precision is impaired in Ehlers–Danlos syndrome. Springerplus 2015, 4, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.A.; Brems, J.J. The inferior capsular-shift procedure for multidirectional instability of the shoulder. J. Bone Jt. Surg. 1992, 74, 1516–1521. [Google Scholar] [CrossRef]
- Finsterbush, A.; Poground, H. The hypermobility syndrome: Musculoskeeltal complaints in 100 consecutive cases of generalized joint hypermobility. Clin. Orthop. Relat. Res. 1982, 168, 124–127. [Google Scholar] [CrossRef]
- Wolf, J.M.; Cameron, K.L.; Owens, B.D. Impact of Joint Laxity and Hypermobility on the Musculoskeletal System. J. Am. Acad. Orthop. Surg. 2011, 19, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Scollinge, R.; Simmonds, J. Hypermobility, injury rate and rehabilitation in a professional football squad: A preliminary study. Phys. Ther. Sport 2009, 10, 91–96. [Google Scholar] [CrossRef]
- Stewart, D.R.; Burden, S. Does generalised limgamentous laxity increase seasonal incidence of injuries in male first division club rugby players? Br. J. Sports Med. 2004, 38, 457–460. [Google Scholar] [CrossRef]
- Rozen, T.D.; Roth, J.M.; Denenberg, N. Cervical spine joint hypermobility: A possible predisposing factor for new dailty persistent headache. Cephalagia 2006, 26, 1182–1185. [Google Scholar] [CrossRef]
- Soderman, K.; Alfredson, H.; Pietila, T.; Werner, S. Risk factors for leg injures in female soccer players: A propsetive investigation during one out-door season. Knee Surg. Sports Traumatol. Arthrisc. 2001, 9, 313–321. [Google Scholar] [CrossRef]
- Neilson, D.; Martin, V.T. Joint Hypermobility and Headache: Understanding the Glue That Binds the Two Together—Part 1. Headache 2014, 54, 1393–1402. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Klerks, M.; Kirby, A. Beighton Score: A Valid Measure for Generalized Hypermobility in Children. J. Pediatr. 2011, 158, 119–123.e4. [Google Scholar] [CrossRef] [PubMed]
- Jindal, P.; Narayan, A.; Ganesan, S.; MacDermid, J.C. Muscle strength differences in healthy young adults with and without generalized joint hypermobility: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 2016, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Reuter, P.R.; Fichthorn, K.R. Prevalence of generalized joint hypermobility, musculoskeletal injuries, and chronic musculoskeletal pain among American university students. PeerJ 2019, 7, e7625. [Google Scholar] [CrossRef]
- Jansson, A.; Saartok, T.; Werner, S.; Renström, P. General joint laxity in 1845 Swedish school children of different ages: Age- and gender-specific distributions. Acta Paediatr. 2004, 93, 1202–1206. [Google Scholar] [CrossRef] [PubMed]
- Beighton, P.; Horan, F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J. Bone Jt. Surg. 1969, 51, 444–453. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Rogind, H.; Jensen, D.V.; Remvig, L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology 2007, 46, 1835–1841. [Google Scholar] [CrossRef] [PubMed]
- Russek, L.N.; Errico, D.M. Prevalence, injury rate and, symptom frequency in generalized joint laxity and joint hypermobility syndrome in a “healthy” college population. Clin. Rheumatol. 2016, 35, 1029–1039. [Google Scholar] [CrossRef]
- Baeza-Velasco, C.; Gely-Nargeot, M.-C.; Vilarrasa, A.B.; Fenetrier, C.; Bravo, J.F. Association between psychopathological factors and joint hypermobility syndrome in a group of undergraduates from a French university. Int. J. Psychiatry Med. 2011, 41, 187–201. [Google Scholar] [CrossRef]
- Artigues-Cano, I.; Bird, H.A. Hypermobility and Proprioception in the Finger Joints of Flautists. Am. J. Clin. Oncol. 2014, 20, 203–208. [Google Scholar] [CrossRef]
- Leone, V.; Tornese, G.; Zerial, M.; Locatelli, C.; Ciambra, R.; Bensa, M.; Pocecco, M. Joint hypermobility and its relationship to musculoskeletal pain in schoolchildren: A cross-sectional study. Arch. Dis. Child. 2009, 94, 627–632. [Google Scholar] [CrossRef]
- Sperotto, F.; Balzarin, M.; Parolin, M.; Monteforte, N.; Vittadello, F.; Zulian, F. Joint hypermobility, growing pain and obesity are mutually exclusive as causes of musculoskeletal pain in schoolchildren. Clin. Exp. Rheumatol. 2014, 32, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef] [PubMed]
- Samoladas, E.; Barmpagianni, C.; Papadopoulos, D.V.; Gelalis, I.D. Lower back and neck pain among dentistry students: A cross-sectional study in dentistry students in Northern Greece. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Thornton, L.J.; Barr, A.E.; Stuart-Buttle, C.; Gaughan, J.P.; Wilson, E.R.; Jackson, A.D.; Wyszynski, T.C.; Smarkola, C. Perceived musculoskeletal symptoms among dental students in the clinic work environment. Ergonomics 2008, 51, 573–586. [Google Scholar] [CrossRef]
- Freedman, D.M.; Eaton, R.G.; Glickel, S. Long-term results of volar ligament reconstruction for symptomatic basal joint laxity. J. Hand Surg. 2000, 25, 297–304. [Google Scholar] [CrossRef]
- Jónsson, H.; Vatysdóttire, S.T. Hypermobility features in patients with hand osteoarthritis. Osteoarhtitis Cartil. 1995, 3, 1–5. [Google Scholar] [CrossRef]
- Kwon, J.-W.; Lee, W.-J.; Park, S.-B.; Kim, M.J.; Jang, S.H.; Choi, C.K. Generalized Joint Hypermobility in Healthy Female Koreans: Prevalence and Age-Related Differences. Ann. Rehabil. Med. 2013, 37, 832–838. [Google Scholar] [CrossRef]
- Canakci, V.; Orbak, R.; Tezel, A.; Canakci, C.F. Influence of different periodontal curette grips on the outcome of mechanical non-surgical therapy. Int. Dent. J. 2003, 53, 153–158. [Google Scholar] [CrossRef]
- DeCoster, L.C.; Vailas, J.C.; Lindsay, R.H.; Williams, G.R. Prevalence and Features of Joint Hypermobility among Adolescent Athletes. Arch. Pediatr. Adolesc. Med. 1997, 151, 989–992. [Google Scholar] [CrossRef]
- Didia, B.C.; Dapper, D.V.; Boboye, S.B. Joint hypermobility syndrome among undergraduate students. East Afr. Med. J. 2002, 79, 80–81. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sahin, N.; Baskent, A.; Ugurlu, H.; Berker, E. Isokinetic evaluation of knee extensor/flexor muscule strength in patients with hypermobility syndrome. Rheumatol. Int. 2008, 28, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Kumar, B.; Lenert, P. Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. Am. J. Med. 2017, 130, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Rombaut, L.; Malfait, F.; De Wandele, I.; Taes, Y.; Thijs, Y.; De Paepe, A.; Calders, P. Muscle mass, muscle strength, functional performance, and physical impairment in women with the hypermobility type of Ehlers-Danlos syndrome. Arthritis Care Res. 2012, 64, 1584–1592. [Google Scholar] [CrossRef]
- Volpi, E.; Nazemi, R.; Fujita, S. Muscle tissue changes with aging. Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 405–410. [Google Scholar] [CrossRef]
- Wilkinson, D.J.; Piasecki, M.; Atherton, P.J. The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fiber atrophy and muscle fiber loss in humans. Ageing Res. Rev. 2018, 47, 123–132. [Google Scholar] [CrossRef]
- Clinch, J.; Deere, K.; Sayers, A.; Palmer, S.; Riddoch, C.; Tobias, J.H.; Clark, E.M. Epidemiogloy of generalized joint laxity (hypermobility) in fourteen-year-old children from the UK: A population-based evaluation. Arthritis Rheum. 2011, 64, 2819–2827. [Google Scholar] [CrossRef]
- Pasdar, Y.; Darbandi, M.; Mirtaher, E.; Rezaeian, S.; Najafi, F.; Hamzeh, B. Associations between Muscle Strength with Different Measures of Obesity and Lipid Profiles in Men and Women: Results from RaNCD Cohort Study. Clin. Nutr. Res. 2019, 8, 148–158. [Google Scholar] [CrossRef]
- Jeong, S.-M.; Choi, S.; Kim, K.; Kim, S.M.; Kim, S.; Park, S.M. Association among handgrip strength, body mass index and decline in cognitive function among the elderly women. BMC Geriatr. 2018, 18, 225. [Google Scholar] [CrossRef]
- Humphreys, S. The unethical use of BMI in contemporary general practice. Br. J. Gen. Pract. 2010, 60, 696–697. [Google Scholar] [CrossRef]
- To, M.; Alexander, C.M. Are people with joint hypermobility syndrome slow to strengthen? Arch. Phys. Med. Rehabil. 2019, 100, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- Liaghat, B.; Skou, S.T.; Jørgensen, U.; Sondergaard, J.; Søgaard, K.; Juul-Kristensen, B. Heavy shoulder strengthening exercise in people with hypermobility spectrum disorder (HSD) and long-lasting shoulder symptoms: A feasibility study. Pilot Feasibility Stud. 2020, 6, 97. [Google Scholar] [CrossRef] [PubMed]
- Celenay, S.T.; Ozer, K.D. Effects of spinal stabilization exercises in women with benign joint hypermobility syndrome: A randomized controlled trial. Rheumatol. Int. 2017, 37, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Luder, G.; Aeberli, D.; Mebes, C.M.; Haupt-Bertschy, B.; Baeyens, J.-P.; Verra, M.L. Effect of resistance training on muscle properties and function in women with generalized joint hypermobility: A single-blind pragmatic randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2021, 13, 10. [Google Scholar] [CrossRef]
- Desrosiers, J.; Bravo, G.; Hébert, R.; Dutil, É.; Mercier, L. Validation of the Box and Block Test as a measure of dexterity of elderly people: Realibility, validity, and norms studies. Arch. Phys. Med. Rehabil. 1994, 75, 751–755. [Google Scholar] [CrossRef]
- Singh, H.P.; Dias, J.J.; Thompson, J.R. Timed Sollerman hand function test for analysis of hand function in normal volunteers. J. Hand Surg. 2014, 40, 298–309. [Google Scholar] [CrossRef]
- Singh, H.; McKay, M.; Baldwin, J.; Nicholson, L.; Chan, C.; Burns, J.; Hiller, C.E. Beighton scores and cut-offs across the lifespan: Cross-sectional study of an Australian population. Rheumatology 2017, 56, 1857–1864. [Google Scholar] [CrossRef]
- Jelsma, L.D.; Geuze, R.H.; Klerks, M.H.; Niemeijer, A.S.; Smits-Engelsman, B.C. The relationship between joint mobility and motor performance in children with and without the diagnosis of developmental coordination disorder. BMC Pediatr. 2013, 13, 35. [Google Scholar] [CrossRef]

| Outcome | Norm Guidelines | |
|---|---|---|
| Males | Females | |
| Grip Strength | 71 | 45 |
| Lateral Pinch Strength | 19 | 13 |
| 3-Point Pinch Strength | 15 | 11 |
| (a) Right hand | ||||
| 2. | 3. | 4. | 5. | |
| 1. Severity of hypermobility | 0.030 * | 0.071 | 0.007 * | 0.875 |
| 2. Grip strength | 1 | 0.000 * | 0.000 * | 0.574 |
| 3. Lateral pinch | 1 | 0.000 * | 0.671 | |
| 4. Three-point pinch | 1 | 0.155 | ||
| 5. Wrist extension | 1 | |||
| (b) Left hand | ||||
| 2. | 3. | 4. | 5. | |
| 1. Severity of hypermobility | 0.021 * | 0.008 * | 0.015 * | 0.301 |
| 2. Grip strength | 1 | 0.000 * | 0.000 * | 0.602 |
| 3. Lateral pinch | 1 | 0.000 * | 0.860 | |
| 4. Three-point pinch | 1 | 0.795 | ||
| 5. Wrist extension | 1 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sangalli, L.; Alabsy, M.; Lingle, D.; Khazaal, N.; West-Pelak, E.; Mitchell, J.C. Hand Joint Hypermobility among Dental Students—A Cross-Sectional Study. Appl. Sci. 2023, 13, 7158. https://doi.org/10.3390/app13127158
Sangalli L, Alabsy M, Lingle D, Khazaal N, West-Pelak E, Mitchell JC. Hand Joint Hypermobility among Dental Students—A Cross-Sectional Study. Applied Sciences. 2023; 13(12):7158. https://doi.org/10.3390/app13127158
Chicago/Turabian StyleSangalli, Linda, Melisa Alabsy, Dana Lingle, Nada Khazaal, Ella West-Pelak, and John C. Mitchell. 2023. "Hand Joint Hypermobility among Dental Students—A Cross-Sectional Study" Applied Sciences 13, no. 12: 7158. https://doi.org/10.3390/app13127158
APA StyleSangalli, L., Alabsy, M., Lingle, D., Khazaal, N., West-Pelak, E., & Mitchell, J. C. (2023). Hand Joint Hypermobility among Dental Students—A Cross-Sectional Study. Applied Sciences, 13(12), 7158. https://doi.org/10.3390/app13127158







