Efficacy of Carbamide and Hydrogen Peroxide Tooth Bleaching Techniques in Orthodontic and Restorative Dentistry Patients: A Scoping Review
Abstract
1. Introduction
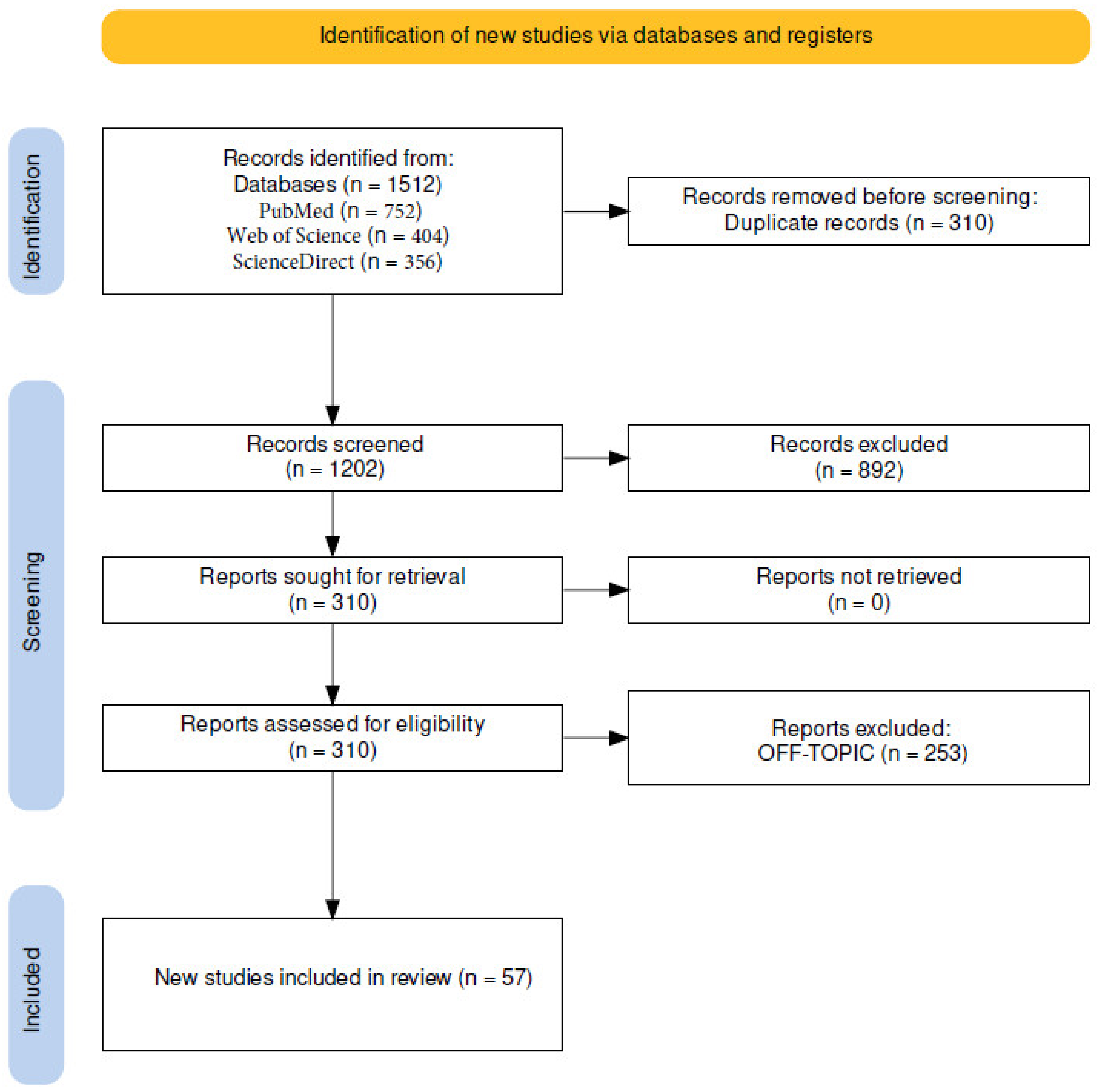
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Inclusion and Exclusion Criteria
2.4. Data Processing
3. Results
4. Discussion
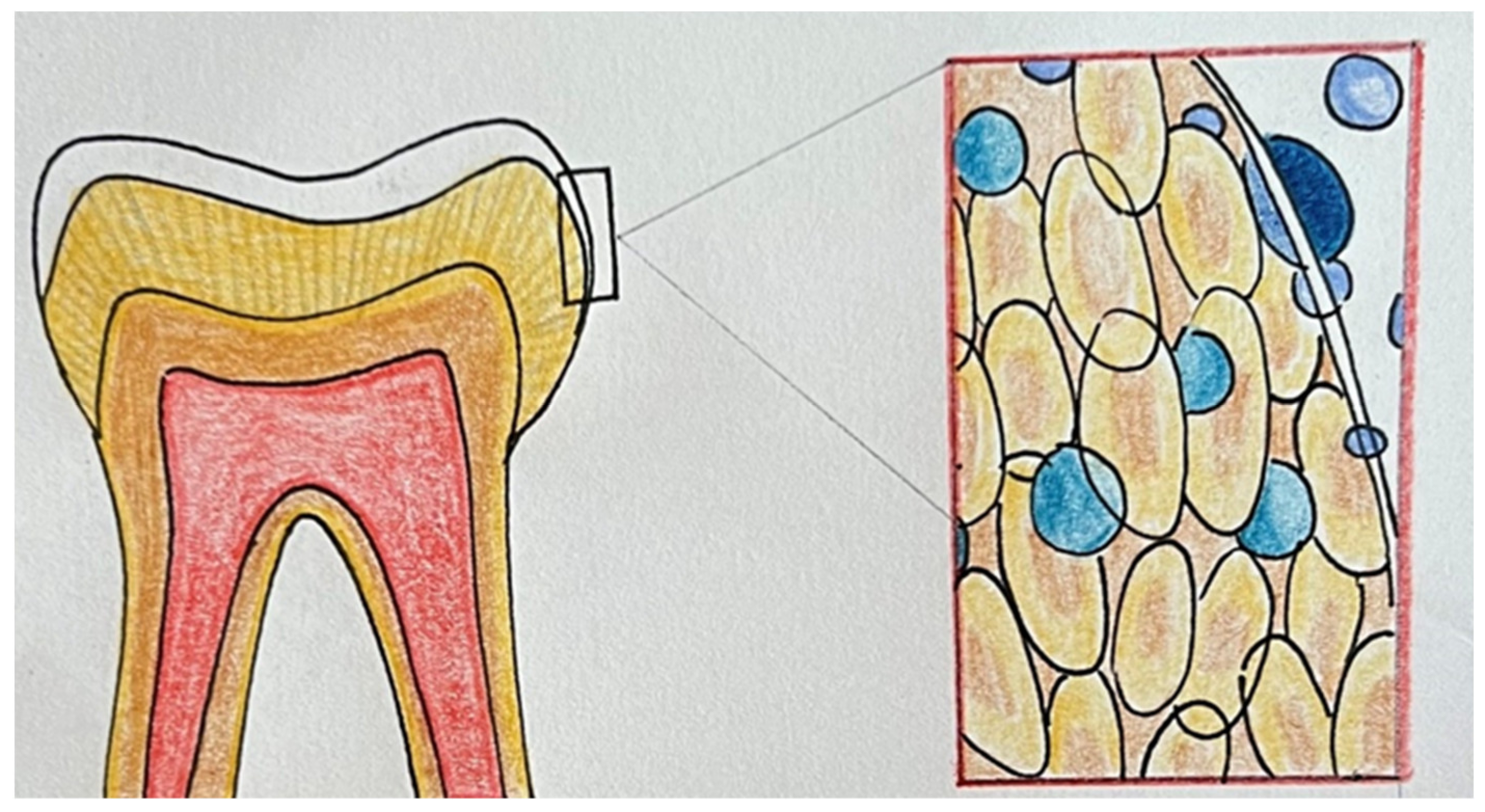
4.1. Bleaching with Carbamide Peroxide
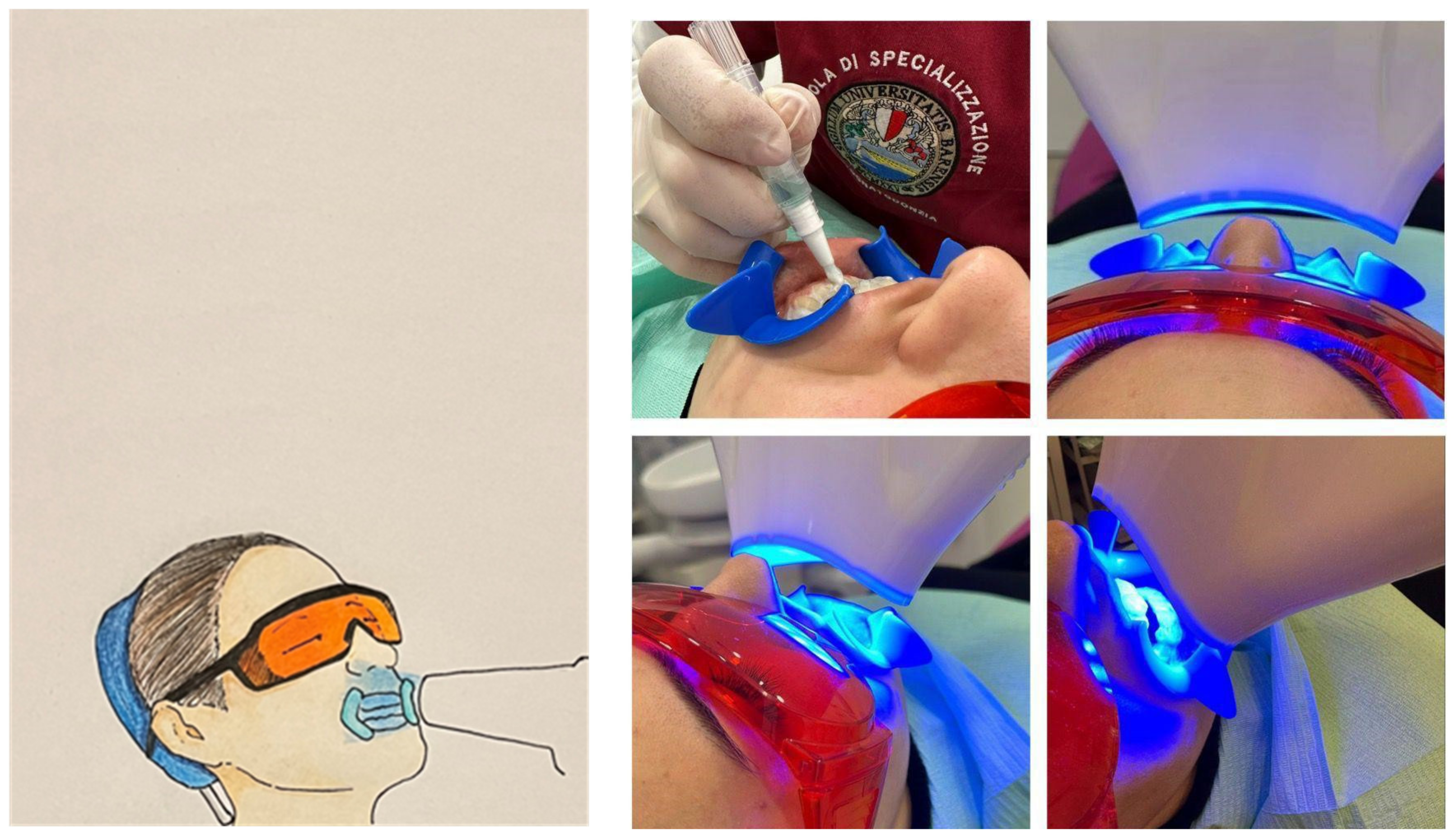
4.2. Bleaching with Hydrogen Peroxide
4.3. Comparison between the Use of Carbamide Peroxide and Hydrogen Peroxide
4.4. Comparison between In-Office and At-Home Dental Bleaching
4.5. Effect of Dental Bleaching in Orthodontic Treatment
4.6. Effects of Dental Bleaching on Composite Restorations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CP | Carbamide peroxide |
| CPP–ACP | Casein phospho-peptide–amorphous calcium phosphate |
| FEA | Finite element analysis |
| HP | Hydrogen peroxide |
| SGU | Shade guide units |
| TiO2 | Nitrogen titanium dioxide |
| TS | Tooth sensitivity |
References
- Isiekwe, G.I.; Sofola, O.O.; Onigbogi, O.O.; Utomi, I.L.; Sanu, O.O.; daCosta, O.O. Dental Esthetics and Oral Health-Related Quality of Life in Young Adults. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 627–636. [Google Scholar] [CrossRef]
- Cantore, S.; Ballini, A.; Farronato, D.; Malcangi, G.; Dipalma, G.; Assandri, F.; Garagiola, U.; Inchingolo, F.; De Vito, D.; Cirulli, N. Evaluation of an Oral Appliance in Patients with Mild to Moderate Obstructive Sleep Apnea Syndrome Intolerant to Continuous Positive Airway Pressure Use: Preliminary Results. Int. J. Immunopathol. Pharmacol. 2016, 29, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Van der Geld, P.; Oosterveld, P.; Van Heck, G.; Kuijpers-Jagtman, A.M. Smile Attractiveness. Self-Perception and Influence on Personality. Angle Orthod. 2007, 77, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Carey, C.M. Tooth Whitening: What We Now Know. J. Evid. Based Dent. Pract. 2014, 14, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, C.; Di Bartolo, I.; Santantonio, M.; Coscia, M.F.; Monno, R.; De Vito, D.; Ruggeri, F.M.; Rizzo, G. Epidemiological and Virological Investigation of a Norovirus Outbreak in a Resort in Puglia, Italy. BMC Infect. Dis. 2007, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- De Vito, D.; Monno, R.; Nuccio, F.; Legretto, M.; Oliva, M.; Coscia, M.F.; Dionisi, A.M.; Calia, C.; Capolongo, C.; Pazzani, C. Diffusion and Persistence of Multidrug Resistant Salmonella Typhimurium Strains Phage Type DT120 in Southern Italy. BioMed Res. Int. 2015, 2015, 265042. [Google Scholar] [CrossRef] [PubMed]
- Halabi, S.; Matsui, N.; Nikaido, T.; Abdo, A.; Burrow, M.F.; Tagami, J. Effect of Two Bleaching Regimens on Enamel Bonding Performance. Dent. Mater. J. 2020, 39, 984–991. [Google Scholar] [CrossRef]
- Coscia, M.F.; Monno, R.; Ballini, A.; Mirgaldi, R.; Dipalma, G.; Pettini, F.; Cristallo, V.; Inchingolo, F.; Foti, C.; de Vito, D. Human Papilloma Virus (HPV) Genotypes Prevalence in a Region of South Italy (Apulia). Ann. Ist. Super Sanita 2015, 51, 248–251. [Google Scholar] [CrossRef]
- Farronato, M.; Boccalari, E.; Del Rosso, E.; Lanteri, V.; Mulder, R.; Maspero, C. A Scoping Review of Respirator Literature and a Survey among Dental Professionals. Int. J. Environ. Res. Public Health 2020, 17, 5968. [Google Scholar] [CrossRef]
- Kwon, S.R.; Wertz, P.W. Review of the Mechanism of Tooth Whitening. J. Esthet. Restor. Dent. 2015, 27, 240–257. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Fama, A.; Cavagnetto, D.; Abate, A.; Farronato, M. Treatment of Dental Dilacerations. J. Biol. Regul. Homeost. Agents 2019, 33, 1623–1627. [Google Scholar]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D Cephalometry on Reduced FOV CBCT: Skeletal Class Assessment through AF-BF on Frankfurt Plane—Validity and Reliability through Comparison with 2D Measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef]
- Pereira, R.; Silveira, J.; Dias, S.; Cardoso, A.; Mata, A.; Marques, D. Bleaching Efficacy and Quality of Life of Different Bleaching Techniques-Randomized Controlled Trial. Clin. Oral Investig. 2022, 26, 7167–7177. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Sutil, E.; da Silva, K.L.; Terra, R.M.O.; Burey, A.; Rezende, M.; Reis, A.; Loguercio, A.D. Effectiveness and Adverse Effects of At-Home Dental Bleaching with 37% versus 10% Carbamide Peroxide: A Randomized, Blind Clinical Trial. J. Esthet. Restor. Dent. 2022, 34, 313–321. [Google Scholar] [CrossRef]
- Tavarez, R.-R.-D.J.; Lima, S.-N.-L.; Malheiros, A.-S.; Menezes, L.-L.; Bandeca, M.-C.; de Miranda, R.C.-M.; Ferreira, M.-C. Assessment of the Aesthetic Impact and Quality of Life of Home Dental Bleaching in Adult Patients. J. Clin. Exp. Dent. 2021, 13, e440–e445. [Google Scholar] [CrossRef]
- Martini, E.C.; Favoreto, M.W.; de Andrade, H.F.; Coppla, F.M.; Loguercio, A.D.; Reis, A. One-Year Follow-up Evaluation of Reservoirs in Bleaching Trays for at-Home Bleaching. J. Esthet. Restor. Dent. 2021, 33, 992–998. [Google Scholar] [CrossRef]
- Silva, L.M.; da Costa Lacerda, Í.A.; Dos Santos, D.B.; Herkrath, F.J.; da Silva, K.L.; Loguercio, A.D.; de Moura Martins, L. Is the At-Home Bleaching Treatment Applied Only on the Lingual Surface as Effective as That on the Buccal Surface? A Randomized Clinical Trial. Clin. Oral Investig. 2022, 26, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
- Estay, J.; Angel, P.; Bersezio, C.; Tonetto, M.; Jorquera, G.; Peña, M.; Fernández, E. The Change of Teeth Color, Whiteness Variations and Its Psychosocial and Self-Perception Effects When Using Low vs. High Concentration Bleaching Gels: A One-Year Follow-Up. BMC Oral Health 2020, 20, 255. [Google Scholar] [CrossRef] [PubMed]
- Tavares, N.R.N.O.; Galvão, A.d.M.; Dietrich, L.; Carvalho, R.F.; Silva, R.S.; Silva, A.L.F.E.; da Silva, G.R. Can Ozone or Violet Light Improve the Color Change or Physicochemical Properties of Hydrogen Peroxide-Bleached Tooth? Braz. Dent. J. 2021, 32, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, D.; Moreira, A.; Cornacchia, T.; Magalhães, C. Evaluation of the Effect of Different Enamel Surface Treatments and Waiting Times on the Staining Prevention after Bleaching. J. Clin. Exp. Dent. 2017, 9, e677–e681. [Google Scholar] [CrossRef]
- Chemin, K.; Rezende, M.; Loguercio, A.D.; Reis, A.; Kossatz, S. Effectiveness of and Dental Sensitivity to At-Home Bleaching With 4% and 10% Hydrogen Peroxide: A Randomized, Triple-Blind Clinical Trial. Oper. Dent. 2018, 43, 232–240. [Google Scholar] [CrossRef]
- Bersezio, C.; Estay, J.; Jorquera, G.; Peña, M.; Araya, C.; Angel, P.; Fernández, E. Effectiveness of Dental Bleaching With 37.5% and 6% Hydrogen Peroxide and Its Effect on Quality of Life. Oper. Dent. 2019, 44, 146–155. [Google Scholar] [CrossRef]
- Barbosa, J.G.; Benetti, F.; de Oliveira Gallinari, M.; Carminatti, M.; da Silva, A.B.D.; Lopes, I.N.I.; Briso, A.L.F.; Cintra, L.T.A. Bleaching Gel Mixed with MI Paste Plus Reduces Penetration of H2O2 and Damage to Pulp Tissue and Maintains Bleaching Effectiveness. Clin. Oral Investig. 2020, 24, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.M.; Ha, A.N.; Kim, J.W.; Kim, S.J. Double-Blind Randomized Study to Evaluate the Safety and Efficacy of Over-the-Counter Tooth-Whitening Agents Containing 2.9% Hydrogen Peroxide. Oper. Dent. 2018, 43, 272–281. [Google Scholar] [CrossRef]
- Del Real García, J.F.; Saldaña-Velasco, F.R.; Sánchez-de la Rosa, S.V.; Ortiz-García, Y.M.; Morales-Velazquez, G.; Gómez-Meda, B.C.; Zúñiga-González, G.M.; Sánchez-Parada, M.G.; Zamora-Perez, A.L. In Vivo Evaluation of the Genotoxicity and Oxidative Damage in Individuals Exposed to 10% Hydrogen Peroxide Whitening Strips. Clin. Oral Investig. 2019, 23, 3033–3046. [Google Scholar] [CrossRef] [PubMed]
- Youssef, S.A.; Cunha, S.R.; Mayer-Santos, E.; Brito, S.A.; de Freitas, P.M.; Ramalho, J.; Morimoto, S.; Gonçalves, F.; Ramalho, K.M. Influence of 35% Hydrogen Peroxide Gel Renewal on Color Change during In-Office Dental Photobleaching with Violet LED: A Split-Mouth Randomized Controlled Clinical Trial. Photodiagnosis Photodyn. Ther. 2021, 36, 102509. [Google Scholar] [CrossRef] [PubMed]
- Martins, I.; Onofre, S.; Franco, N.; Martins, L.M.; Montenegro, A.; Arana-Gordillo, L.A.; Reis, A.; Loguercio, A.D.; da Silva, L.M. Effectiveness of In-Office Hydrogen Peroxide With Two Different Protocols: A Two-Center Randomized Clinical Trial. Oper. Dent. 2018, 43, 353–361. [Google Scholar] [CrossRef]
- Lima, S.N.L.; Ribeiro, I.S.; Grisotto, M.A.; Fernandes, E.S.; Hass, V.; de Jesus Tavarez, R.R.; Pinto, S.C.S.; Lima, D.M.; Loguercio, A.D.; Bandeca, M.C. Evaluation of Several Clinical Parameters after Bleaching with Hydrogen Peroxide at Different Concentrations: A Randomized Clinical Trial. J. Dent. 2018, 68, 91–97. [Google Scholar] [CrossRef]
- Terra, R.; da Silva, K.L.; Vochikovski, L.; Sutil, E.; Rezende, M.; Loguercio, A.D.; Reis, A. Effect of Daily Usage Time of 4% Hydrogen Peroxide on the Efficacy and Bleaching-Induced Tooth Sensitivity: A Single-Blind Randomized Clinical Trial. Oper. Dent. 2021, 46, 395–405. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Prieto, M.V.; Meneses, P.; Angel, P.; Eduardo Fernández, G.; Loguercio, A. One-Year Bleaching Efficacy Using Two HP Products with Different PH: A Double-Blind Randomized Clinical Trial. J. Esthet. Restor. Dent. 2019, 31, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, R.; Rizzante, F.; Rosa, E.R.; Borges, A.; Furuse, A.Y.; Bombonatti, J. Effectiveness of LED/Laser Irradiation on In-Office Dental Bleaching after Three Years. Oper. Dent. 2018, 43, 31–37. [Google Scholar] [CrossRef]
- Bersezio, C.; Pardo, C.; Miranda, S.; Medeiros Maran, B.; Jorquera, G.; Rosa da Silva, A.; Tonetto Rodrigues, M.; Fernández, E. Evaluation of the Effectiveness in Teeth Whitening of a Single Session with 6% Hydrogen Peroxide Laser/LED System. Photodiagnosis Photodyn. Ther. 2021, 36, 102532. [Google Scholar] [CrossRef]
- Angel, P.; Bersezio, C.; Estay, J.; Werner, A.; Retamal, H.; Araya, C.; Martin, J.; Fernández, E. Color Stability, Psychosocial Impact, and Effect on Self-Perception of Esthetics of Tooth Whitening Using Low-Concentration (6%) Hydrogen Peroxide. Quintessence Int. 2018, 49, 557–566. [Google Scholar] [CrossRef]
- Ferraz, N.K.L.; Nogueira, L.C.; Neiva, I.M.; Ferreira, R.C.; Moreira, A.N.; Magalhães, C.S. Longevity, Effectiveness, Safety, and Impact on Quality of Life of Low-Concentration Hydrogen Peroxides in-Office Bleaching: A Randomized Clinical Trial. Clin. Oral Investig. 2019, 23, 2061–2070. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, T.C.; Bortolatto, J.F.; Rizzi, G.; Meloto, B.T.; Dantas, A.A.R.; de Oliveira Junior, O.B. Clinical Performance of 6% Hydrogen Peroxide Containing TiO2N Nanoparticles Activated by LED in Varying Wavelengths-a Randomized Clinical Trial. Lasers Med. Sci. 2022, 37, 2017–2024. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Angel, P.; Bottner, J.; Godoy, I.; Avalos, F.; Fernández, E. Teeth Whitening with 6% Hydrogen Peroxide and Its Impact on Quality of Life: 2 Years of Follow-Up. Odontology 2019, 107, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Celik, E.U. Evaluation of the Efficacy and Color Stability of Two Different At-Home Bleaching Systems on Teeth of Different Shades: A Randomized Controlled Clinical Trial. J. Esthet. Restor. Dent. 2017, 29, 325–338. [Google Scholar] [CrossRef]
- Barcessat, A.R.; Gurgel-Juarez, N.C.; Wetter, N.U. Vital Tooth Bleaching Using Different Techniques: A Clinical Evaluation. Future Dent. J. 2018, 5, S2314718018300831. [Google Scholar] [CrossRef]
- Llena, C.; Collado-González, M.; García-Bernal, D.; Oñate-Sánchez, R.E.; Martínez, C.M.; Moraleda, J.M.; Rodríguez-Lozano, F.J.; Forner, L. Comparison of Diffusion, Cytotoxicity and Tissue Inflammatory Reactions of Four Commercial Bleaching Products against Human Dental Pulp Stem Cells. Sci. Rep. 2019, 9, 7743. [Google Scholar] [CrossRef]
- Peixoto, A.C.; Vaez, S.C.; Pereira, N.A.d.R.; da Silva Santana, C.N.; Soares, K.D.A.; Romão, A.C.T.R.; Ferreira, L.F.; Martins-Filho, P.R.S.; Faria-E-Silva, A.L. High-Concentration Carbamide Peroxide Can Reduce the Sensitivity Caused by in-Office Tooth Bleaching: A Single-Blinded Randomized Controlled Trial. J. Appl. Oral Sci. 2018, 26, e20170573. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Mayer, C.; Rivera, O.; Estay, J.; Vernal, R.; Haidar, Z.S.; Angel, P.; Oliveira, O.B.; Fernández, E. Quality of Life and Stability of Tooth Color Change at Three Months after Dental Bleaching. Qual. Life Res. 2018, 27, 3199–3207. [Google Scholar] [CrossRef]
- Mounika, A.; Mandava, J.; Roopesh, B.; Karri, G. Clinical Evaluation of Color Change and Tooth Sensitivity with In-Office and Home Bleaching Treatments. Indian J. Dent. Res. 2018, 29, 423. [Google Scholar] [CrossRef]
- Chemin, K.; Rezende, M.; Milan, F.M.; Dantas, T.B.; Gomes, K.d.N.; Kossatz, S. Clinical Evaluation of 10% Hydrogen Peroxide on Tooth Sensitivity and Effectiveness in at Home Dental Bleaching. J. Contemp. Dent. Pract. 2018, 19, 1376–1380. [Google Scholar] [CrossRef] [PubMed]
- Maran, B.M.; Vochikovski, L.; de Andrade Hortkoff, D.R.; Stanislawczuk, R.; Loguercio, A.D.; Reis, A. Tooth Sensitivity with a Desensitizing-Containing at-Home Bleaching Gel—A Randomized Triple-Blind Clinical Trial. J. Dent. 2018, 72, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Briso, A.L.F.; Rahal, V.; de Azevedo, F.A.; de Gallinari, M.O.; Gonçalves, R.S.; Frascino, S.M.B.; Santos, P.H.D.; Cintra, L.T.A. Neurosensory Analysis of Tooth Sensitivity during At-Home Dental Bleaching: A Randomized Clinical Trial. J. Appl. Oral Sci. 2018, 26, e20170284. [Google Scholar] [CrossRef]
- Martini, E.C.; Favoreto, M.W.; Coppla, F.M.; Loguercio, A.D.; Reis, A. Evaluation of Reservoirs in Bleaching Trays for At-Home Bleaching: A Split-Mouth Single-Blind Randomized Controlled Equivalence Trial. J. Appl. Oral Sci. 2020, 28, e20200332. [Google Scholar] [CrossRef] [PubMed]
- López Darriba, I.; Novoa, L.; de la Peña, V.A. Efficacy of Different Protocols for At-Home Bleaching: A Randomized Clinical Trial. Am. J. Dent. 2017, 30, 329–334. [Google Scholar]
- Darriba, I.L.; Cabirta Melón, P.; García Sartal, A.; Ríos Sousa, I.; Alonso de la Peña, V. Influence of Treatment Duration on the Efficacy of At-Home Bleaching with Daytime Application: A Randomized Clinical Trial. Clin. Oral Investig. 2019, 23, 3229–3237. [Google Scholar] [CrossRef]
- Vildósola, P.; Vera, F.; Ramírez, J.; Rencoret, J.; Pretel, H.; Oliveira, O.; Tonetto, M.; Martín, J.; Fernández, E. Comparison of Effectiveness and Sensitivity Using Two In-Office Bleaching Protocols for a 6% Hydrogen Peroxide Gel in a Randomized Clinical Trial. Oper. Dent. 2017, 42, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Ermis, R.B.; Uzer Celik, E.; Yildiz, G.; Yazkan, B. Effect of Tooth Discolouration Severity on the Efficacy and Colour Stability of Two Different Trayless At-Home Bleaching Systems. J. Dent. Res. Dent. Clin. Dent. Prospects 2018, 12, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Piknjač, A.; Zlatarić, D.K. Clinical Evaluation of 6-Month Efficacy of 40% in-Office Whitening Treatment. Pesqui. Bras. Odontopediatria Clín. Integr. 2021, 21, e0236. [Google Scholar] [CrossRef]
- Kury, M.; Wada, E.E.; da Silva Palandi, S.; Picolo, M.Z.D.; Giannini, M.; Cavalli, V. Colorimetric Evaluation after In-Office Tooth Bleaching with Violet LED: 6- and 12-Month Follow-Ups of a Randomized Clinical Trial. Clin. Oral Investig. 2022, 26, 837–847. [Google Scholar] [CrossRef]
- Meireles, S.S.; Santos, M.E.; Lustosa, Í.M.C.; Leite, E.L.L. Effects of a Reduced In-office Bleaching Protocol with 37.5% Hydrogen Peroxide on Effectiveness and Tooth Sensitivity: A Double-blind Randomized Clinical Trial. J. Esthet. Restor. Dent. 2021, 33, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Vaez, S.; Correia, A.; Santana, T.; Santana, M.; Peixoto, A.; Leal, P.; Faria-e-Silva, A. Is a Single Preliminary Session of In-Office Bleaching Beneficial for the Effectiveness of At-Home Tooth Bleaching? A Randomized Controlled Clinical Trial. Oper. Dent. 2019, 44, E180–E189. [Google Scholar] [CrossRef]
- Mayer-Santos, E.; Bachiega-Silva, B.; Twiaschor, C.V.; Shimokawa, C.A.K.; Marinho, G.B.; Junior, A.B.; Zanin, F.; Brugnera, A.P.; Ramalho, K.M.; de Freitas, P.M. Blinded, Parallel and Randomized Clinical Evaluation of in-Office Dental Bleaching with Violet LED (405–410 nm). Photodiagnosis Photodyn. Ther. 2022, 38, 102739. [Google Scholar] [CrossRef]
- Piknjač, A.; Soldo, M.; Ileš, D.; Knezović Zlatarić, D. Patients’ Assessments of Tooth Sensitivity Increase One Day Following Different Whitening Treatments. Acta Stomatol. Croat. 2021, 55, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Donassollo, S.H.; Donassollo, T.A.; Coser, S.; Wilde, S.; Uehara, J.L.S.; Chisini, L.A.; Correa, M.B.; Cenci, M.S.; Demarco, F.F. Triple-Blinded Randomized Clinical Trial Comparing Efficacy and Tooth Sensitivity of in-Office and at-Home Bleaching Techniques. J. Appl. Oral Sci. 2021, 29, e20200794. [Google Scholar] [CrossRef] [PubMed]
- Dourado Pinto, A.V.; Carlos, N.R.; do Amaral, F.L.B.; França, F.M.G.; Turssi, C.P.; Basting, R.T. At-Home, in-Office and Combined Dental Bleaching Techniques Using Hydrogen Peroxide: Randomized Clinical Trial Evaluation of Effectiveness, Clinical Parameters and Enamel Mineral Content. Am. J. Dent. 2019, 32, 124–132. [Google Scholar]
- Rodrigues, J.L.; Rocha, P.S.; Pardim, S.L.d.S.; Machado, A.C.V.; Faria-e-Silva, A.L.; Seraidarian, P.I. Association Between In-Office And At-Home Tooth Bleaching: A Single Blind Randomized Clinical Trial. Braz. Dent. J. 2018, 29, 133–139. [Google Scholar] [CrossRef]
- Knezović Zlatarić, D.; Žagar, M.; Illeš, D. A Clinical Study Assessing the Short-term Efficacy of Combined In-office/At-home Whitening Treatment. J. Esthet. Restor. Dent. 2019, 31, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Mailart, M.C.; Sakassegawa, P.A.; Santos, K.C.; Torres, C.R.G.; Palo, R.M.; Borges, A.B. One-year Follow-up Comparing At-home Bleaching Systems Outcomes and the Impact on Patient’s Satisfaction: Randomized Clinical Trial. J. Esthet. Restor. Dent. 2021, 33, 1175–1185. [Google Scholar] [CrossRef] [PubMed]
- Levrini, L.; Paracchini, L.; Bakaj, R.; Diaconu, A.; Cortese, S. Dental Bleaching during Orthodontic Treatment with Aligners. Int. J. Esthet. Dent. 2020, 15, 44–54. [Google Scholar] [PubMed]
- Féliz-Matos, L.; Abreu-Placeres, N.; Hernandez, L.M.; Ruiz-Matuk, C.; Grau-Grullón, P. Evaluation of In-Office Vital Tooth Whitening Combined with Different Concentrations of At-Home Peroxides: A Randomized Double-Blind Clinical Trial. Open Dent. J. 2019, 13, 377–382. [Google Scholar] [CrossRef]
- Pavani, C.C.; Vieira, L.R.; Schott, T.C.; Sundfeld, D.; Pini, N.; Bertoz, A.; Pacheco, R.R.; Sundfeld, R.H. Case Reports of Enamel Microabrasion Associated with At-Home Dental Bleaching After Orthodontic Bracket Removal. Oper. Dent. 2021, 46, 237b–245. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.N.; Dutra, H.; Morais, A.; Sgura, R.; Devito-Moraes, A.G. In-Office Bleaching During Orthodontic Treatment. J. Esthet. Restor. Dent. 2017, 29, 83–92. [Google Scholar] [CrossRef]
- Ahrari, F.; Akbari, M.; Mohammadipour, H.S.; Fallahrastegar, A.; Sekandari, S. The Efficacy and Complications of Several Bleaching Techniques in Patients after Fixed Orthodontic Therapy. A Randomized Clinical Trial. Swiss Dent. J. 2020, 130, 493–501. [Google Scholar]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental Resin Composites: A Review on Materials to Product Realizations. Compos. Part B Eng. 2022, 230, 109495. [Google Scholar] [CrossRef]
- German, M.J. Developments in Resin-Based Composites. Br. Dent. J. 2022, 232, 638–643. [Google Scholar] [CrossRef]
- Yadav, R.D.; Raisingani, D.; Jindal, D.; Mathur, R. A Comparative Analysis of Different Finishing and Polishing Devices on Nanofilled, Microfilled, and Hybrid Composite: A Scanning Electron Microscopy and Profilometric Study. Int. J. Clin. Pediatr. Dent. 2016, 9, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Libonati, A.; Marzo, G.; Klinger, F.G.; Farini, D.; Gallusi, G.; Tecco, S.; Mummolo, S.; De Felici, M.; Campanella, V. Embryotoxicity Assays for Leached Components from Dental Restorative Materials. Reprod. Biol. Endocrinol. 2011, 9, 136. [Google Scholar] [CrossRef] [PubMed]
- Elhoshy, A.Z.; Abouelenein, K.; Elbaz, M.A. Effect of 15% Carbamide Peroxide Bleaching Gel on Color of Class V Resin Composite Restoration. Future Dent. J. 2018, 4, 239–243. [Google Scholar] [CrossRef]
- Mummolo, S.; Mancini, L.; Quinzi, V.; D’Aquino, R.; Marzo, G.; Marchetti, E. Rigenera® Autologous Micrografts in Oral Regeneration: Clinical, Histological, and Radiographical Evaluations. Appl. Sci. 2020, 10, 5084. [Google Scholar] [CrossRef]
- Meireles, S.S.; Santos, I.S.; Bona, A.D.; Demarco, F.F. A Double-Blind Randomized Clinical Trial of Two Carbamide Peroxide Tooth Bleaching Agents: 2-Year Follow-Up. J. Dent. 2010, 38, 956–963. [Google Scholar] [CrossRef] [PubMed]



| Pregnancy and Breastfeeding | If There Is Acute Hypersensitivity, Patient Cannot Take NSAIDS |
|---|---|
| Age < 18 years old | Pulp chamber larger and therefore closer to enamel. Increased incidence of hypersensitivity. |
| Diabetes and xerostomia-inducing drugs | Home bleaching is not recommended because it may decrease salivary flow. In-office bleaching is recommended. |
| Allergies to polymers contained in the mask | Avoid the home one with a mask and opt for the in-office one. |
| PUVA (psoralen and UV radiation) therapy or other types of photochemotherapy | Unable to use UVA lamp to photoactivate bleaching agent. Contact treating physician. |
| Therapy with photoreactive drugs or substance (antibiotics, contraceptives) | Unable to use UVA lamp to photoactivate bleaching agent. Contact treating physician. |
| Immunosuppressive therapies | Contact treating physician. |
| Oncologic patients | Contact the oncologist. |
| Respiratory deficiency | Difficulty in prolonged use of protective barriers and mouth openers, especially in the supine position. |
| Articles screening strategy | KEYWORDS: A: “peroxide”; B: “dental bleaching”; C: “tooth bleaching” |
| Boolean Indicators: (“A” AND “B”); (“A” AND “C”) | |
| Timespan: 2017–2023 | |
| Electronic Database: Pubmed, Web of Science, and ScienceDirect |
| Authors | Type of Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Sutil E. et al., 2022 [15] | Randomized, blind clinical trial | To compare the effects of 10% versus 37% CP on gingival irritation, TS, and bleaching effectiveness. | Eighty patients were chosen based on inclusion and exclusion standards, and randomly divided into two groups (n = 40): 37% CP and 10% CP. | At 1–3 weeks, the 37% CP group demonstrated quicker whitening than the 10% group. Although both groups displayed equal bleaching one month after the conclusion (p = 0.06). |
| Tavarez R.-R.-D.J. et al., 2021 [16] | Clinical study | To assess how at-home bleaching with 10% CP affected patients’ perceptions of their appearance and quality of life. | A total of 107 patients between the ages of 18 and 38 who had at least one anterior tooth in color A2 or darker were chosen. Patients who have undergone any kind of bleaching operations in the past were not eligible. Each patient received a 10% CP at-home bleaching treatment. The patients complied the OHIP-14 and OASIS questionary before and after the treatment. | Although there was a drop in the domain of psychological discomfort and an increase in worries about dental appearance, at-home bleaching with 10% CP had no appreciable effect on patients’ quality of life or aesthetic impression. |
| Martini E.C. et al., 2021 [17] | Clinical study | To assess the color change stability and patient satisfaction following a year of at-home bleaching with 10% CP in trays with or without reservoirs. | Forty-six patients underwent CP bleaching with a bleaching tray with or without reservoirs for three hours each day for 21 days. The color was measured using a spectrophotometer and shade guide units (SGU) one month and one year after bleaching was finished. A 5-point Likert Scale questionnaire was used to gauge patient satisfaction. | The design of the bleaching tray has no impact on the 10% CP’s ability to bleach (Opalescence PF, Ultradent). Regardless of the bleaching tray design, patients were quite pleased with the results of the bleaching. |
| Authors | Type of the Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Estay J. et al., 2020 [19] | Randomized and prospective double-blind clinical trial | To compare the change, stability of color and effects on self-perception with 6% HP gel in an in-office bleaching relative to 37.5% HP gel. | Patients (n = 25) were assessed at 12 months post bleaching treatment: 6% HP chemo-activated alkaline formula gel versus 37.5% HP gel. Color changes were measured using Vita Bleached scale. | The effect of 37.5% HP was significantly better than that of 6% HP in terms of color rebound after 1 year of follow-up. The 6% HP achieved a positive psychosocial impact and enhanced self-perception at follow-up. |
| Tavares N.R.N.O. et al., 2021 [20] | Clinical trial | To evaluate the bleaching effectiveness and the physicochemical effects on enamel of violet light and ozone, associate or not to HP, compared to 35%-hydrogen peroxide. | Patients (n = 15): HP 35%, violet light, ozone, the association between hydrogen peroxide with ozone or violet light. All protocols were performed in two sessions with a 48 h interval. Color (spectrophotometer) and mineral composition (Raman spectroscopy) were measured before and after the bleaching. | Violet light associate with HP was unable to improve the color changes observed for the peroxide alone, in combination with ozone and HP. The ozone therapy improved the bleaching effect in the group that received the association of HP. |
| Monteiro D. et al., 2017 [21] | Clinical trial | To evaluate the effect of surface treatments and waiting time prior to contact with dye on bleached enamel staining susceptibility. | Patients (n: 100): bleached with 35% were in contact with red wine. Color difference was evaluated with a spectrophotometer. Surface treatments and waiting time effects were analyzed with Kruskal–Wallis and Mann–Whitney tests. | Surface treatments and waiting time were not significant to decrease bleached enamel susceptibility to red wine staining. |
| Chemin K. et al., 2018 [22] | Randomized, triple-blind clinical trial | To evaluate the risk for and intensity of TS and color change of at-home dental bleaching with 4% and 10% HP. | Patients (n = 78) into two groups: HP 4%, and HP 10%. At-home bleaching: 30 min twice a day for 2 weeks. The color was assessed by Vita Classical, Vita Bleached-guide and spectrophotometer Vita Easyshade at baseline, at first and second weeks and after one month. TS recorded by a numeric rating scale (0–4) and visual analogue scale (0–10). | Bleaching is effective with 4% and 10% HP concentrations, but 10% HP increased the absolute risk and intensity of TS. |
| Del Real García J.F. et al., 2019 [26] | Clinical trial | To evaluate the impact of 10% hydrogen peroxide whitening strip exposure on the genotoxicity and oxidative damage by means of the buccal micronucleus cytome assay by counting nuclear abnormalities (NAs) in buccal mucosa and attached gingiva cells and by analyzing in whole saliva the molecule 8-hydroxy-2’-deoxyguanosine (8-OHdG). | Patients (n = 113) were divided into: group 1 or control (n = 53), non-whitening strip exposed, and group 2 (n = 60), whitening strip exposed (Crest® 3D Whitestrips® premium plus, 10% hydrogen peroxide). Oral epithelial cells and whole saliva samples were taken at the beginning and 30 days later for group 1 and immediately before bleaching and 15 and 30 days after the end of the bleaching for group 2. | Individuals exposed to 10% hydrogen peroxide whitening strips exhibit NAs increased in oral epithelial cells and 8-OHdG in saliva. Individuals exposed to whitening strips with 10% hydrogen peroxide exhibit increased genotoxic and oxidative damage. |
| Youssef S.A. et al., 2021 [27] | Split-mouth randomized controlled clinical trial | To evaluate the effect of 35% HP gel renewal in association with violet LED (405–410 nm) through a split-mouth randomized controlled clinical trial. | Patients (n = 48) underwent 3 bleaching sessions of 15 min each, with an interval of 7 days between them, using 35% HP combined to violet LED irradiation. Teeth color was measured with VITA Classical scale and the spectrophotometer VITA Easyshade. TS was measured using a Visual Analog Scale before, immediately after each bleaching session, and 14 days and 60 days after the end of the treatment. | There is no need for bleaching gel renewal when following the clinical protocol of 3 sessions of 15 min in a bleaching protocol of 35% HP combined with violet LED. |
| Martins I. et al., 2018 [28] | Multicenter, single-blind, randomized trial | To evaluate the bleaching efficacy and TS of in-office 38% HP applied under different time protocols. | Patients (n = 45) with right superior canines darker than C2 were selected. The 38% HP was applied in two 20 min (2 × 20) applications or one 40 min (1 × 40) application. Color changes were evaluated by using Vita Classical and Vita Bleached guide and Easyshade Spectrophotometer methods at baseline and 30 days after the second session. TS was recorded up to 48 h with a 0–10 Visual Analogue Scale. | The use of a 40 min in-office bleaching agent gel application produced the same whitening degree and TS that the two 20 min bleaching agent applications did. |
| Lima S.N.L. et al., 2018 [29] | Randomized double-blind clinical trial | To compare TS, bleaching efficacy, and cytokine levels after applying in-office bleaching treatments containing 15% and 35% HP. | Patients (n = 25) were randomly assigned to receive HP15% or HP 35% treatment. The bleaching agent was applied in three 15-min applications per session. Two bleaching sessions were separated by a 1-week interval. Gingival crevicular fluid was collected from three jaws sites per patient for the analysis of fluid volume. Flow cytometry was used to analyze gingival crevicular fluid levels of IL-1β, IL-2, IL-4, IL-6, IL-10, tumor necrosis factor, and interferon-gamma. All measurements were obtained before and after bleaching. | Treatment with HP 35% is more effective than HP 15% but generates a greater risk and intensity of TS. No inflammatory changes occurred despite the difference in the HP concentrations. |
| Terra R. et al., 2021 [30] | Single-blind randomized clinical trial | To compare the risk/intensity of TS and color change of a 30 min vs. the recommended 120 min application time of 4% HP for at-home bleaching. | Patients (n = 92) were divided into a group of 30 min vs. the 120 min application for at-home bleaching. Trays with 4% HP were used for 3 weeks. The color was assessed by Vita Classical, Vita Bleached guide 3D-MASTER and spectrophotometer Vita Easy shade at baseline, weekly, and after 1 month. TS was recorded by a numeric rating scale (0–4) and visual analogue scale (0–10). | A 4 week protocol of at-home dental bleaching with 4% HP for 30 min/day whitened teeth similarly to the 120 min/day protocol, with low intensity of TS and high patient satisfaction. |
| Bersezio C. et al., 2019 [23] | Double-blind randomized clinical trial | To evaluate the bleaching efficacy produced by two HP gels with different pHs, at 1 year since treatment. | Patients (n = 28) into two groups and four subgroups. The treatment was assessed during and after the bleaching procedure up to 12 months post-treatment. The color was assessed by two bleaching scales shade guide units and spectrophotometer device. | Bleaching using a neutral (pH = 7.0) in-office gel demonstrated similar stability and rebound effect than an acidic one (pH = 2.0). |
| Mondelli R. et al., 2018 [32] | Randomized, triple-blinded, and split-mouth clinical study | To evaluate effectiveness of a hybrid light source on the color change, stability, and TS in patients submitted to different in-office bleaching techniques. | Patients (n = 20) into four groups: 35% Lase Peroxide Sensy (LPS) + hybrid light; 35% HP+ hybrid light; 35% HP; 25% LPS + hybrid light: 25% HP + hybrid light; and 35% Whiteness HP: 35% HP. For the groups activated with hybrid light, the HP was applied on the enamel surface three consecutive times using a 3 × 2 min protocol (three hybrid light activations for 2 min each, with a 30 s interval for a total of seven minutes and 30 s) for each gel application. For the other groups, HP was applied 3 × 15 min. The color was assessed by a spectrophotometer device. | All techniques and bleaching agents were effective on bleaching during a 36 month evaluation of color stability. The groups activated with HL presented lower TS and required a lower activation time. |
| Bersezio C. et al., 2021 [33] | Clinical trial | To compare the effectiveness and TS of in-office dental bleaching with one versus two applications of 6% (HP) gel with nitrogen titanium dioxide nanoparticles activated by LED/Laser lamp in a single session. | Patients (n = 27) were treated in office with 6% HP with nitrogen titanium dioxide nanoparticles. Group 1 received one application of 72 min and Group 2 received two applications of 36 min. | There were no significant differences in the effectiveness of a single session with one or two applications of 6% HP with nitrogen titanium dioxide nanoparticles between both groups. |
| Angel P. et al., 2018 [34] | Clinical trial | To evaluate the bleaching efficacy and impact on psychosocial and aesthetics self-perception of 6% HP gel compared with a conventional 37.5% HP gel when used as an in-office treatment. | Patients (n = 35) received two sessions of three 12 min applications of treatment with 37.5% HP on one side of the mouth and 6% HP on the other. Color changes were measured objectively using total variation in color and subjectively using the Vita Classical scale. Aesthetic questionnaires were administered to measure self-perception. | Low concentration of HP achieved effective bleaching with good stability at 3 months accompanied by a positive psychosocial impact and enhanced self-perception. However, the traditional 35% concentration was objectively more effective. |
| Ferraz N.K.L. et al., 2019 [35] | Randomized, parallel, and double-blinded clinical trial | To evaluate the impact on the oral health-related quality of life of in-office dental bleaching using low-concentration hydrogen peroxides. | Patients (n = 54) were divided into using 6% or 15% HP in-office bleaching activated via hybrid LED/laser light. Color changes were measured objectively using total variation in color and subjectively using the Vita Classical scale. | Both agents showed bleaching effectiveness but HP 15% presented greater color stability than HP 6%, at the 6 month follow-up. The agents showed low levels of TS, gingival irritation, and did not affect the oral health-related quality of life of the participants. |
| Trevisan T.C. et al., 2022 [36] | Double-blinded clinical trial | To evaluate the clinical performance of dental bleaching performed with 6% HP containing TiO2-N nanoparticles exposed to blue and violet activation lights. | Patients (n = 40) were randomly distributed into four experimental groups (n = 10): 35% HP (PH35)-control; 6% HP (PH6) containing TiO2-N nanoparticles without light activation; PH6 activated with a blue LED (PH6A); and PH6 activated with a violet LED (PH6V). The three bleaching sessions consisted of 3 consecutive 16 min applications of the bleaching agent described for each group. The groups receiving LED activation were exposed to light intermittently every 1 min, with a total exposure time of 8 min in each application. | All groups treated with 6% HP were less likely to cause TS compared to the control group (PH35). The use of PH6 activated by LED violet resulted in an effective and safe clinical protocol for in-office dental bleaching. |
| Bersezio C. et al., 2019 [37] | A split-mouth study | To evaluate color longevity after 2 years of whitening gel (6% HP), blue LED/infrared laser activation system) in comparison to a control 35% concentration. | Patients (n = 31) were treated using 6% or 35% HP gel. The color was measured at baseline and 1 week, 1 month, and 1 and 2 years after treatment using the Easyshade Vita spectrophotometer and the Vita Bleached and Vita Classical Shade Guides. | The positive effect of bleaching on quality of life was maintained in patients treated with a low concentration of the whitening gel. |
| Authors | Type of the Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Celik E.U. 2017 [38] | Randomized controlled clinical trial | Compared the bleaching efficacy of two different at-home bleaching systems (10% CP and 6% HP). | Ninety-two patients were chosen and randomly divided into three groups: negative control, 10% CP, and 6% HP. | Although both bleaching agents were clinically effective, 10% CP was more successful. |
| Peixoto A.C. et al., 2018 [41] | Single-blinded randomized parallel clinical trial | Evaluate TS in patients undergoing in-office tooth bleaching with 37% CP and 35% HP. | Forty patients were randomly assigned to receive two sessions of in-office tooth whitening using either 35% HP or 37% CP. The degree of TS for each patient was assessed before, and up to 24 h after bleaching. | 37% CP resulted in reduced TS. |
| Bersezio C. et al., 2018 [42] | Randomized clinical study | Evaluate the psychosocial impact and aesthetic perceptions of 42 patients undergoing non-vital-tooth bleaching with HP (35%) and CP (37%). | Forty-seven patients were chosen and divided into two groups according to the bleaching agent used: group 1 (35% HP) and group 2 (37% CP). | Both gels were highly effective, and the color change lasts at least three months. |
| Barcessat A.R. et al., 2018 [39] | Clinical trial | Evaluate dental color stability after various bleaching techniques. | Sixty patients were divided into four groups: 35% HP in-office bleaching, in-office application of 3% HP followed by in-office bleaching using 35% HP, 3% HP in-office bleaching, and 10% CP at-home bleaching. | All techniques produced higher bleaching efficacy. |
| Authors | Type of the Study | Aim of Study | Materials | Results |
|---|---|---|---|---|
| Chemin K. et al., 2018 [22] | Randomized clinical trial | Evaluate the effectiveness of home bleaching treatment with 10% HP. | Twenty volunteers. At-home bleaching (30 min twice a day, for 2 weeks). | Follow-up after a mouth, a significant bleaching. |
| Mounika A. et al., 2018 [43] | Randomized clinical trial | Comparison between two techniques: 35% HP + 16% CP. | Thirty patients. At-home bleaching (16% CP) and in-office bleaching (35% HP). | Effective treatment for both procedures and color regression at 3 and 6 months follow-up. |
| Rodrigues J.L. et al., 2018 [60] | Randomized clinical trial | Comparison between two techniques: 38% HP and 10% CP (in-office and at-home bleaching). | Forty patients. In-office bleaching and second session of home bleaching or in-office bleaching. | No difference in bleaching efficacy and TS was found between performing a second session in the study and combining with 1 week of home bleaching. |
| Maran B.M. et al., 2018 [45] | Randomized, triple-blind clinical trial | Comparison between two techniques: 10% CP with desensitizer gel (3% potassium nitrate and 0.2% sodium fluoride) and a 10% CP gel without desensitizer. | Sixty patients. At-home bleaching (3 h a day for 21 days). | No difference in bleaching efficacy and TS. |
| Ermis R.B. et al., 2018 [51] | Randomized clinical trial | Comparison between techniques: 1. 10% CP, 2. bleaching membrane with 10% HP, 3. tray applied bleaching membrane with 10% HP and bleaching pen with 22% CP. | Ninety patients divided into two groups: lighter and darker teeth. The teeth in each group were further divided into three groups (n = 15). | The severity of tooth discoloration and the type of trayless system affected the effectiveness of bleaching, while only the type of trayless system affected color stability. |
| Vildósola P. et al., 2017 [50] | Randomized clinical trial | Comparison between two techniques of in-office bleaching: 6% of HP. | Thirty patients. In-office bleaching in 2 modes: 1 application of 36 min versus 3 applications of 12 min, each for 2 sessions. | No difference about TS. Both reported slight TS. |
| Vaez S. et al., 2019 [55] | Randomized, controlled clinical trial | Comparison between at-home and in-office bleaching 10% CP and 35% HP. | Twenty-six patients in-office bleaching for 45 min with 35% HP and at-home bleaching for 1 h/day with 10% CP. | The combined protocol reduced the time necessary to obtain a good effectiveness with at-home bleaching but increased the risk of TS. |
| Mayer-Santos E. et al., 2022 [56] | Randomized, controlled clinical trial | Comparison between at-home and in-office bleaching with 35% HP. | One-hundred participants divided into 4 groups: G1 35% HP (4 sessions, 1 a week); G2 LED violet (4 sessions, 1 a week); G3 LED violet (4 sessions, 2 a week); G4 hybrid technique (LED violet + 35% HP; 4 sessions, 1 a week). | The hybrid technique showed excellent bleaching with lower TS. |
| Piknjač A. et al., 2021 [52] | Randomized, controlled clinical trial | Comparison between in-office and at-home bleaching: 40% HP, 16% CP, and 10% CP. | Sixty participants divided in 3 groups: 1. 40% HP in-office, 2. home bleaching 16% CP, 3. home bleaching 10% CP. | Same bleaching efficacy but with lower TS of home bleaching with 10% CP compared to home bleaching with 16% CP and in-office bleaching with 40% HP. |
| López Darriba I. et al., 2017 [48] | Randomized clinical trial | Comparison of at-home bleaching techniques: 10% CP and 7.5% HP. | Eighty participants divided into 4 groups: (1) 10% CP/1 h a day; (2) 10% CP/ overnight; (3) 7.5% HP/1 h a day; (4) 7.5% HP/overnight. | The most effective protocol is low concentrations (10% CP) with overnight use. |
| Martini E.C. et al., 2020 [17] | Split-mouth, single-blind, randomized, controlled equivalence trial | Comparison between bleaching with or without reservoirs with 10% CP. | Forty-six patients divided into 2 groups: bleaching trays were made with reservoirs and the other half, without reservoirs. | The presence of reservoirs in a bleaching tray did not improve bleaching or determine TS and gingival irritation. |
| Silva L.M. et al., 2022 [18] | Randomized clinical trial | Comparison of the use of HP in different tooth surfaces. | Twenty-five patients divided into 2 groups: 10% HP once daily for 60 min to the buccal surface (BSB) and 10% HP once daily for 60 min to the lingual surface (LSB). | No significative differences. |
| KnezovićZlatarić D. et al., 2019 [57] | Randomized, controlled trial | Comparison of at-home bleaching techniques: 6% HP and 16% CP. | Thirty participants divided into two groups: 1. 15 received hybrid treatment in-office bleaching (6% HP + 2 weeks at-home bleaching with 16% CP); 2. 15 in a control group. | The hybrid treatment is the most effective. |
| Darriba I. et al., 2019 [49] | Randomized clinical trial | Comparison of different protocols using 10% CP. | Fifty participants divided into 2 groups: (A) with a 14 day treatment and (B) with a 21 day treatment. | Daytime application of at-home bleaching for 3 weeks achieves better bleaching results than 2 weeks, immediately after treatment and 1 and 6 months later. |
| Briso A.L.F. et al., 2018 [46] | Randomized clinical trial | Comparison of power bleaching 10% CP with and without potassium oxalate. | Twenty-five patients. Power bleaching 10% CP with potassium oxalate was utilized and 10% CP without potassium oxalate for 3 weeks. | No difference in TS. |
| Sutil E. et al., 2022 [15] | Randomized, blind clinical trial | Comparison of at-home bleaching techniques: 10% versus 37% CP. | Eighty patients divided into 2 groups. At-home bleaching: 1. 4 h/day for 10% group, 2. 30 min/day for 37% group; both for 3 weeks. | Same results but with less treatment time with 37% CP. |
| Dourado Pinto A.V. et al., 2019 [59] | Randomized clinical trial | Comparison of at-home and in-office bleaching techniques: 10% HP and 40% HP. | Seventy-five patients divided into 3 groups: (a) at-home-bleaching 10% HP for 15 days/1 h a day; (b) office bleaching 40% HP, 3 sessions of 40 min); (c) combined: a session with 40% HP and the other sessions with 10% HP for 15 days. | At-home and combined techniques may cause greater TS than office-technique and lead to a higher gingival irritation. |
| Kury M. et al., 2022 [53] | Randomized clinical trial | Comparison of in-office bleaching techniques CP and HP. | One-hundred patients divided into 5 groups: LED, CP, LED/CP, HP, and LED/HP. | The use of purple LED alone (without bleaching gels) produced perceptible long-term bleaching results. |
| Piknjač A. et al., 2021 [52] | Randomized, controlled clinical Trial | The effectiveness of in-office bleaching with 40% HP. | Twenty participants, 40% HP, 3 applications each 20 min, in one session. | Significant results during 6 months of follow-up. |
| Meireles S.S. et al., 2021 [54] | Randomized, controlled clinical trial | Comparison of in-office bleaching techniques using 37.5% HP. | Forty participants divided into 2 groups: 1. 2 applications (37.5 HP2) 2. 3 applications (37.5 HP3)/8 min for sessions. Three clinical sessions were performed with an interval of 1 week. | No significative differences. |
| Donassollo S.H. et al., 2021 [58] | Randomized, controlled clinical trial | Comparison of at-home and in-office bleaching techniques: 35% HP (in-office) and 10% CP (at-home). | One-hundred-and-thirty volunteers divided into 2 groups: (a) in-office bleaching and a placebo at-home protocol; (b) in-office placebo and at-home bleaching treatment. | The 10% CP produced a superior effect compared with 35% HP and TS were similar for the 2 techniques. |
| Féliz-Matos L. et al., 2019 [64] | Randomized, double-blind clinical trial | Comparison of at-home bleaching techniques: 10%/15%/20% CP and 40%/10% HP. | One-hundred-and-twenty participants divided into four groups of treatment were defined: G1 = CP 10% + HP40% G2 = CP15% + HP40%, G3 = CP20% + HP40%, G4 = HP10% + HP40%. | The result was similar (bleaching and TS). |
| Mailart M.C. et al., 2021 [62] | Randomized clinical trial | One comparison of at-home bleaching techniques: 10% HP and 10% CP. | Sixty participants. Opalescence GO (OGO)-10%HP PT-30 min, White Class-10%HP CT-30 min, Opalescence PF-10%CP CT-2 h, e Opalescence PF-10%CP CT-8 h. | No significant difference. |
| Pereira R. et al., 2022 [13] | Randomized controlled trial | Comparison of at-home bleaching techniques: 6% HP and 16% CP. | Eighty participants. Group A—in-office 6% HP paint-on varnish; group B—at-home 6% HP with adaptable tray; group C—at-home 16% CP with a custom tray. | No significative difference at 6 months of follow-up after treatment. |
| Authors | Type of the Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Ahrari F. et al., 2020 [67] | Randomized clinical trial | To analyze the effectiveness and risks of various whitening techniques in patients with stained teeth who have undergone orthodontic treatment. | Sixty volunteers (31 women, 29 men) aged 14 to 30 years randomly divided in 4 groups: group 1 underwent bleaching at-home, whereas those in groups 2 through 4 underwent bleaching in-office using, respectively, a diode laser, a plasma arc, and no light source. Tooth color was measured at baseline, an hour after the bleaching process was complete, and one week afterwards. A record was kept of the degree of post-treatment problems and TS. | All methods were effective in managing tooth discoloration after orthodontic treatment. Laser-assisted bleaching should be regarded as the finest alternative among in-office procedures because it delivered effective outcomes with the least amount of TS and in the shortest amount of time. |
| Levrini L. et al., 2020 [63] | Finite element analysis, clinical study | To evaluate the teeth whitening performance of trays without reservoirs using clinical research using spectrophotometry and a finite element analysis (FEA). | Three sample areas of gel application on the maxillary central incisors (the incisal edge, the middle part, and the gingival edge) were analyzed. A spectrophotometry was used to ascertain the clinical effectiveness of the bleaching gel as it related to the results of the FEA. The chromatic variation obtained by the bleaching gel on teeth 41 and 32 (control teeth, with reservoirs) was compared with that on teeth 31 and 42 (study teeth, without reservoirs). | Optimal gel distribution is reached when 2 mm3 of gel is applied to the center of the vestibular face of the tooth in the tray. No relevant differences of whitening effectiveness between the teeth with reservoirs and those without. |
| Pavani C.C. et al., 2021 [65] | Case report | To evaluate the improving in esthetics after orthodontic brackets debonding. | One patient undergoing at-home bleaching with 10% HP, fine bur removal of composite, and micro abrasion after orthodontic brackets removal. | The proposed treatment considerably improved the esthetics and successfully removed the grooves created during the removal of the bonding composite, resulting in a smooth enamel surface. |
| Gomes M.N. et al., 2017 [66] | Case report | To evaluate teeth whitening while receiving orthodontic treatment. | Two patients undergoing two or three 40 min sessions while wearing fixed orthodontic braces. | Despite the braces, the teeth were successfully bleached. |
| Authors | Type of the Study | Aim of the Study | Materials | Results |
|---|---|---|---|---|
| Elhoshy A.Z. et al., 2018 [72] | Randomized controlled trial | To evaluate the effect of 15% CP at-home bleaching on nanocomposite and microhybrid resins. | Sixty class V cavities in maxillary premolars. Teeth were divided in 4 groups: Group A (control): 15 specimens, light nanocomposite resin (Filtek Z350 XT) with no post-restoration bleaching procedure (control); Group B (experimental): 15 specimens, light nanocomposite resin (Filtek Z350 XT) with post-restoration bleaching procedure; Group C (control): 15 specimens, restored with microhybrid resin (Filtek Z250 XT) with no post-restoration bleaching procedure; Group D (experimental): 15 specimens, restored with microhybrid resin (Filtek Z250 XT) with post-re- restoration bleaching procedure. | After 2 weeks of bleaching, there was superiority of microhybrid composites for color patterns. No differences in mean opacity and fluorescence values. |
| Meireles S.S. et al., 2010 [74] | Randomized controlled trial | To evaluate color change and TS after 10% CP at-home bleaching in sound and restored teeth. | Forty patients divided in 2 groups. Group A: 20 patients with 6 caries-free maxillary anterior teeth), and Re Group B: 20 patients with at least 1 restoration in the 6 maxillary anterior teeth. | After 2 weeks of bleaching, lower color change in restored teeth. No differences for TS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malcangi, G.; Patano, A.; Inchingolo, A.D.; Ciocia, A.M.; Piras, F.; Latini, G.; Di Pede, C.; Palmieri, G.; Laudadio, C.; Settanni, V.; et al. Efficacy of Carbamide and Hydrogen Peroxide Tooth Bleaching Techniques in Orthodontic and Restorative Dentistry Patients: A Scoping Review. Appl. Sci. 2023, 13, 7089. https://doi.org/10.3390/app13127089
Malcangi G, Patano A, Inchingolo AD, Ciocia AM, Piras F, Latini G, Di Pede C, Palmieri G, Laudadio C, Settanni V, et al. Efficacy of Carbamide and Hydrogen Peroxide Tooth Bleaching Techniques in Orthodontic and Restorative Dentistry Patients: A Scoping Review. Applied Sciences. 2023; 13(12):7089. https://doi.org/10.3390/app13127089
Chicago/Turabian StyleMalcangi, Giuseppina, Assunta Patano, Alessio Danilo Inchingolo, Anna Maria Ciocia, Fabio Piras, Giulia Latini, Chiara Di Pede, Giulia Palmieri, Claudia Laudadio, Vito Settanni, and et al. 2023. "Efficacy of Carbamide and Hydrogen Peroxide Tooth Bleaching Techniques in Orthodontic and Restorative Dentistry Patients: A Scoping Review" Applied Sciences 13, no. 12: 7089. https://doi.org/10.3390/app13127089
APA StyleMalcangi, G., Patano, A., Inchingolo, A. D., Ciocia, A. M., Piras, F., Latini, G., Di Pede, C., Palmieri, G., Laudadio, C., Settanni, V., Garofoli, G., de Ruvo, E., Buongiorno, S., Bordea, I. R., Xhajanka, E., Di Venere, D., Inchingolo, F., Dipalma, G., & Inchingolo, A. M. (2023). Efficacy of Carbamide and Hydrogen Peroxide Tooth Bleaching Techniques in Orthodontic and Restorative Dentistry Patients: A Scoping Review. Applied Sciences, 13(12), 7089. https://doi.org/10.3390/app13127089















