Abstract
Background: The Roussouly classification, based on the functional parameter sacral slope (SS), describes the normal sagittal balance in adults and has proved useful for surgery. Reference values in children should be defined, since they are an important treatment target of conservative treatment. Moreover, during growth, there are few correlations between sagittal parameters, and we hypothesize that a new classification based on the anatomical parameter pelvic incidence (PI) could also be useful. We performed a cross-sectional study to identify the reference values for the Roussouly classification during growth and to develop a new classification based on PI in children. Methods: Correlations between sagittal parameters and age were searched in 222 healthy subjects at the first consultation (6–18 years old). A new classification, based on PI, and comprising three types, is defined and compared to the Roussouly classification. Results: With age, correlations among sagittal balance parameters increase, as well as SS and PI, but with different cut-offs. The distribution of Roussouly types do not correspond to that in adulthood; thus, we defined new reference cut-offs. We defined a PI-based classification in three types, not overlapping Roussouly’s. We found a uniform and balanced distribution of cases among the nine possible combinations. Conclusions: In children, we need to use new thresholds for the Roussouly types. The new classification based on PI is correlated with the Roussouly classification, but it is also clearly different. Future studies will determine its validity.
1. Introduction
Standing posture requires good spinopelvic balance, obtained through a balanced pelvic and spinal shape [1,2]. Sagittal profile spinal parameters play a crucial role in determining disability, health-related quality of life and therapeutic options [3,4]. From a surgical point of view, restoring spinopelvic balance is fundamental to maximize functional outcomes, reduce pain, and avoid complications [5]. The pelvic and spinal parameters showed high correlations in healthy populations [6,7] and significant individual variability [8]. The normative values of spinopelvic parameters in adolescents and children have been reported in healthy subjects [9,10,11] and patients with spinal deformities [12,13,14,15], showing higher variability than in adults [9].
With the practical aims of planning surgery and reducing failures, Roussouly suggested four categories in healthy adults. Roussouly classification is based on the Sacral Slope (SS), the pelvic parameter best correlating with spinal sagittal curves [16]. This approach offers an easier and practical way to classify subjects before surgery, as shown by the number of studies based on the Roussouly classification and new classifications proposed with the same purposes [17]. Contrarily, there are almost no studies in the field of conservative interventions, where current sagittal classification seems less valuable.
Bracing is effective in controlling scoliosis evolution [18]. Scoliosis bracing aims to correct the frontal plane, while keeping the best possible sagittal balance [19]. Nevertheless, the sagittal plane constitutes a significant clinical problem with a frequent flat back induction [5,20], and possible in-brace unbalance [21]. The immediate effects of bracing pose the same problems as surgery to the sagittal balance because it fixes the trunk and spine in a specific position for long durations. Nevertheless, bracing action aims at improving spinal balance at the end of growth. Moreover, children have different sagittal balance compensation mechanisms than adults because their spine and joints are less rigid, and their bodies constantly change toward adulthood. For this reason, we hypothesize that a classification of sagittal balance based on a reliable, anatomical parameter, such as Pelvic Incidence, could be more helpful in bracing children.
The present study aims to (1) assess if the distribution of the Roussouly types differ in children from adults; (2) if so, identify the correct boundaries of Roussouly types in normal children of different age and sex; (3) provide a new classification to the sagittal balance of the growing spine, similar to the Roussouly, but based on the anatomical parameter PI instead of the positional SS; (4) compare the two classifications. The overall aim is to give researchers and clinicians in the field of conservative interventions a better understanding of sagittal balance in children.
2. Materials and Methods
2.1. Study Characteristics
We performed a cross-sectional study embedded in a prospective clinical cohort of a tertiary referral institute specializing in spinal disorders during growth. We obtained the local ethical committee approval, verbal consent from children that took part in the study and written informed consent from participants’ parents. The researchers and the Institute did not receive any funding for this project. No compensation was provided to the participants.
2.2. Participants
We recruited a cohort of healthy subjects using the following inclusion criteria: age between 6 and 18 years, first consultation at our Institute, availability of frontal (PA) and sagittal (LL) radiographs, and no signs of spine pathologies as evaluated by an expert in the field. Exclusion criteria were: previous treatment for any spinal disorder, scoliosis angle exceeding 9° Cobb, Scheuermann’s disease, thoracic kyphosis above 49° Cobb, spondylolisthesis or any other spine disease, back pain, neuromuscular disease, or syndrome. Participants had spinal radiographs requested by their general practitioner before referral to our Institute. A careful clinical and radiographical evaluation by a specialist with extensive experience in spinal deformities allowed their classification as healthy subjects according to the previous inclusion and exclusion criteria. Since we were interested in defining the classifications by age and sex, and since we did not know before the study the numerosity of the sample and the possible distribution of the two variables, we post-hoc divided patients into subgroups to keep a minimum of around 20 patients per group.
2.3. Measurements
A group of expert specialists measured the sagittal spine and pelvic parameters. They included thoracic kyphosis between the lower plate of T12 and the upper plate of T1 (TK-T1) or T4 (TK-T4), lumbar lordosis between T12 and the lower plate of L5 (LL-L5) or the upper plate of S1 (LL-S1), lumbosacral angle (LSA), spino-sacral angle (SSA), spino-pelvic angle (SPA) and the pelvic parameters PI, SS and Pelvic Tilt (PT). We performed all measurements after patients’ clinical information concealment.
To check the reliability of measurements, we randomly extracted the radiographs of 20 patients to be re-measured by two senior physicians and one junior physician, with the latter repeating the measurements one week apart in a different randomized order. We considered test–retest reliability excellent if the value was above 0.8, good between 0.6 and 0.79, moderate between 0.4 and 0.59, and insufficient below 0.4. The intra-rater repeatability of radiograph measurements was excellent, with the inter-rater being excellent (59.3% of parameters) or good (29.6%), with only LSA moderate.
2.4. Identification of the Two Classifications in Children
The Roussouly classification includes four types of sagittal spinal alignment in healthy adults with a uniform distribution: type 1 and 2 have SS < 35° and a prevalence of 28% (5% and 23%, respectively), type 4 has SS > 45° (25%) and type 3 between these boundaries (47%) [16]. According to these principles in the adult classification, we first verified if the Roussouly types in children had the same distribution. Due to the pelvis change during growth, we expected the distribution to differ in children. If our hypothesis had proven true, we planned to identify the new boundaries for the Roussouly types in children of different ages and sex, keeping the same distribution in quartiles as adults.
Using the same principles based on quartiles, we defined the new classification as having three types with progressively growing PI: types A and C include the lowest and highest quartiles; type B consists of the two intermediate ones (50% of the population).
2.5. Data Analysis and Statistics
We checked the data distribution with histograms. We used Pearson’s correlation coefficient to assess the correlation between sagittal parameters and examined the evolution of all pelvic parameters with age. Finally, we compared the distribution of types in the two classifications. In theory, well-balanced patients should have Roussouly types 1–2 (low SS) corresponding to the new classification type A (low PI), with 3 and 4 corresponding to B (medium) and C (large), respectively.
3. Results
3.1. Clinico-Demographical Characteristics
Out of 25,292 children in our clinical files (31 July 2017), we identified 222 participants (Figure 1).
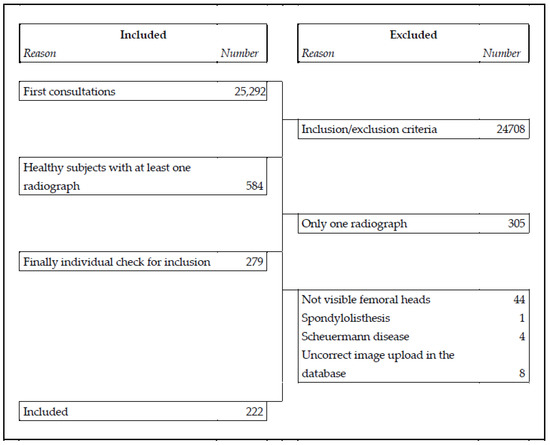
Figure 1.
Flow chart of the procedure used to identify the study group of normal healthy individuals from the prospective database.
We divided the patients into four age groups, and we found some statistically, but not clinically, significant differences between the sexes and among age groups (Table 1).

Table 1.
Characteristics of the study population according to gender and age groups.
3.2. Correlation Analyses
The percentage of correlations above 0.4 among the sagittal parameters was 22.2% in the whole sample, with no difference between sexes; this number significantly increased after age 14, reaching 50% (Table 2).

Table 2.
Correlation coefficients for pelvic and spinal sagittal balance in the total population and in the oldest (age 15–18) and youngest (age < 10) groups. Pearson’s coefficients higher than 0.4 are highlighted.
The correlations with age were all statistically significant but below 0.4. Looking at the age groups, SS increased with a statistically significant difference after age 14; this was also true for PI, but the difference was evident earlier, after age 10 (Figure 2).
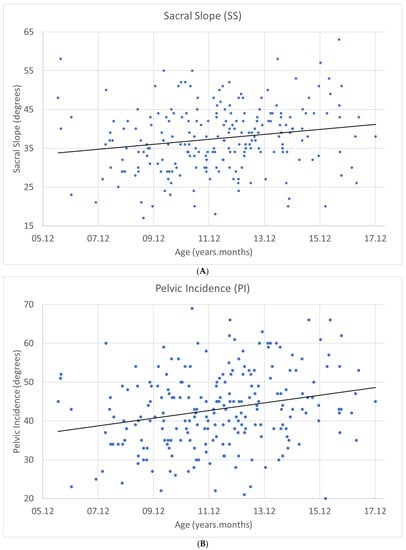
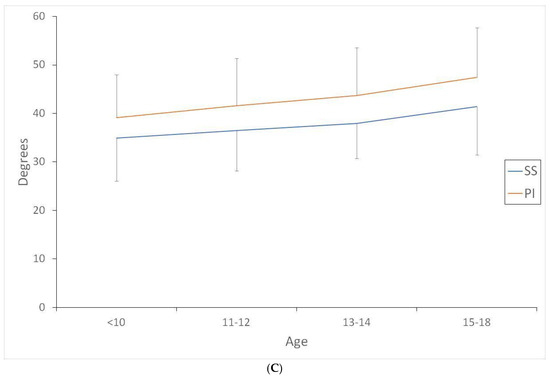
Figure 2.
Variation with the age of (A) Sacral Slope (SS) and (B) Pelvic Incidence (PI), and (C) differences between age groups. While correlations for SS and PI with age were low (0.182 and 0.236, respectively), the differences between age groups appeared statistically significant for SS after age 14 and for PI after age 10.
3.3. Age-Related Effect on SS vs. PI
The adult Roussouly types 1–2 (37%) prevalence was higher than type 4 (15%) in the total population. This difference was more significant below age 10 (type 1–2: 36% and type 4: 10%, respectively) and decreased with growth: after age 15, types 1–2 and 4 had a prevalence of 28.5% and 32%, respectively. We did not find differences between sexes within the age groups. We defined the cut-offs for the Roussouly during growth and the new PI-based classifications according to the results in Table 3.

Table 3.
Sacral slope (SS) and pelvic incidence (PI) variations with age.
The values of the Roussouly classification correspond to the adult values after age 12, whilst those of the new classification continue to grow until at least age 14 (Table 4).

Table 4.
Newly defined limits in the Roussouly classification of sacral slope (SS) to distinguish the different types in different age groups during growth. Limits of pelvic incidence (PI) for the new classification in different age groups during growth. Distribution of the Roussouly classification and the new classification types in the different groups.
3.4. Correlations between the Roussouly SS-Based Classification and the New PI-Based One
We did not find overlap between the two classifications, but there was a balanced distribution of cases among the nine possible combinations (Table 5).

Table 5.
Correlations between the growing age Roussouly classification and the new classification among the different groups. Theoretically, the corresponding types between the two classifications should be A with 1–2, B with 3 and C with 4, respectively. The last line reports the “correct” corresponding types. With growth the two classifications become closer.
4. Discussion
This paper aimed to describe a healthy children cohort and test the Roussouly classification in children. With age, we found a different distribution of the Roussouly types with the need for growing SS and PI thresholds. We found lower correlations between sagittal balance parameters than previously published [8,9,12,22], but these correlations improve with age. Finally, we suggested a new classification based on PI anatomical thresholds as possibly more valuable during growth.
In the present cohort of children, SS and PI continuously increased (Figure 2). This result agrees with several studies showing that the sagittal profile of the spine changes from childhood to adolescence and adulthood [23,24,25]. The wide variability in the sagittal parameters can explain the very low correlation between age and SS/PI, albeit statistically significant. Given the cross-sectional design of this study, we could not observe and combine serial data to identify the age variations. As expected, we coherently found a considerable variation in the distribution of Roussouly types, favouring types 1–2 in younger-aged participants, confirming the need to define new thresholds for the Roussouly classification during growth.
Our findings and previous findings are worth noting [8,9,12,22], in that the youngest have the lowest correlations among sagittal balance parameters. Our explanatory hypothesis correlates with the gradually reducing body elasticity and corresponding increasing rigidity with growth [26]. The younger subjects have more sagittal compensations than adults available at the lower limb (such as genu recurvatum or foot pronation). Conversely, adult rigidity makes the sagittal spinal balance more regional, increasing the internal spinopelvic correlations. This hypothesis could contradict the correlation of spinal parameters higher with functional SS than anatomical PI, which we found in agreement with the literature. However, spinal parameters are all functional, and the spine continuously adjusts its position, with the pelvis synchronously adapting (SS), but within the range determined by its anatomy (PI). Since we measure the instantaneous sagittal balance of single-shot radiography, the position prevails on anatomy, in terms of instantaneous correlations. It has been well established that the long-term conservative treatment should plan results to achieve a functional adult spine [26]. The planning of such approaches requires a careful evaluation of the sagittal plane, aiming to preserve the balance or attempt to improve it, while taking advantage of growth. We expect that increased knowledge of growth effects on the sagittal parameters and the desired normative profile according to age and bone maturity would allow a better and more personalized treatment.
The revised values for the Roussouly classification must be applied in individuals under age 12, while, interestingly, from age 13, the values reach those of adulthood. The new classification provides more accurate data in children, with one more subgroup between ages 12 and 14; interestingly, only the type A threshold does not change after age 12. It is possible that the values in the group aged 15–18 years, in the new classification, could be maintained in adulthood; a specific study could verify this hypothesis. Interestingly, we did not find differences in pelvis parameters between sexes within the age groups. This was not expected, due to the known time lapse between female and male pubertal growth spurt. This result could lay the groundwork for future studies.
We examined the distribution of participants in the two classifications; there was no overlap between the two, and the distribution of cases was uniform and balanced among the nine possibilities. This result could confirm that the variability is probably due to positional factors that influence the Roussouly classification but not the new classification. Another possible explanation includes measurement error for both classifications, even though we found excellent intra- and good inter-operator reliability.
The main limitation of this study is the cross-sectional design, which does not allow observation of changes in each subject over time to determine spinal maturation fully. Nevertheless, it is unethical to prescribe serial radiographs with radiation exposure to define normative data and growth evolution in healthy children. A cross-sectional design is the only option, in line with Roussouly’s approach for his classification [16]. Another limitation is the relatively small sample size, though the sample size is comparable to other similar studies [11,21,23]. Again, this resulted from the difficulty in collecting radiographs from healthy subjects. In light of the current results, we suggest referring to PI in children to reduce the variability due to using a positional parameter, such as SS.
5. Conclusions
During growth, the classical Roussouly classification developed in adults needs an adaptation, and new thresholds (such as those described in the present study) should be used. We also propose a new classification based on the anatomical parameter PI, instead of the positional parameter SS. The new classification is correlated with the Roussouly classification but could be more useful in children when correlations between sagittal parameters are weaker and positional factors may play a central role. Further studies are needed to confirm its validity.
Author Contributions
S.N. conceived the research design; S.N., F.Z., C.C. and S.D. provided a substantial contribution to the acquisition of data and data interpretation. All authors have participated in drafting the manuscript, S.N. revised it critically. All authors have read and agreed to the published version of the manuscript.
Funding
Internal funding for research purposes were directly provided by Italian Scientific Spine Institute (ISICO). The APC was waived by the Editors of the Special Issues.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the local Institutional Review Board.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting reported results can be downloaded on zenodo.org or obtained from the corresponding authors on reasonable request.
Acknowledgments
We wish to thank Alessandro Laurini for his contribution in data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Berthonnaud, E.; Dimnet, J.; Roussouly, P.; Labelle, H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. Clin. Spine Surg. 2005, 18, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Duval-Beaupère, G. Threshold values for supine and standing cobb angles and rib hump measurements: Prognostic factors for scoliosis. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform Soc. Eur. Sect. Cerv. Spine Res Soc. 1996, 5, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009, 34, E599–E606. [Google Scholar] [CrossRef]
- Schwab, F.J.; Smith, V.A.; Biserni, M.; Gamez, L.; Farcy, J.-P.C.; Pagala, M. Adult scoliosis: A quantitative radio-graphic and clinical analysis. Spine 2002, 27, 387–392. [Google Scholar] [CrossRef]
- Cheung, J.P.Y. The importance of sagittal balance in adult scoliosis surgery. Ann. Transl. Med. 2020, 8, 35. [Google Scholar] [CrossRef]
- Deinlein, D.; Bhandarkar, A.; Vernon, P.; McGwin, G.; Wall, K.; Reece, B.; McKay, J.; Theiss, S. Correlation of pelvic and spinal parameters in adult deformity patients with neutral sagittal balance. Spine Deform. 2013, 1, 458–463. [Google Scholar] [CrossRef]
- Wei, X.; Gengwu, L.; Chao, C.; Yifan, L.; Shang, S.; Ruixi, H.; Yunhan, J.; Xiaodong, Z.; Zhikun, L. Correlations between the sagittal plane parameters of the spine and pelvis and lumbar disc degeneration. J. Orthop. Surg. Res. 2018, 13, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Mac-Thiong, J.-M.; Roussouly, P.; Berthonnaud, E.; Guigui, P. Sagittal parameters of global spinal balance: Normative values from a prospective cohort of seven hundred nine caucasian asymptomatic adults. Spine 2010, 35, E1193–E1198. [Google Scholar] [CrossRef]
- Mac-Thiong, J.-M.; Berthonnaud, E.; Dimar, J.R.; Betz, R.R.; Labelle, H. Sagittal alignment of the spine and pelvis during growth. Spine 2004, 29, 1642–1647. [Google Scholar] [CrossRef]
- Vaz, G.; Roussouly, P.; Berthonnaud, E.; Dimnet, J. Sagittal morphology and equilibrium of pelvis and spine. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform Soc. Eur. Sect. Cerv. Spine Res. Soc. 2002, 11, 80–87. [Google Scholar] [CrossRef] [Green Version]
- Vedantam, R.; Lenke, L.G.; Keeney, J.A.; Bridwell, K.H. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine 1998, 23, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.-M.; Labelle, H.; Charlebois, M.; Huot, M.-P.; de Guise, J.A. Sagittal Plane Analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 2003, 28, 1404–1409. [Google Scholar] [CrossRef] [PubMed]
- Bourghli, A.; Aunoble, S.; Reebye, O.; Le Huec, J.C. Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur. Spine J. 2011, 20 (Suppl. 5), 663–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clément, J.-L.; Geoffray, A.; Yagoubi, F.; Chau, E.; Solla, F.; Oborocianu, I.; Rampal, V. Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform Soc. Eur. Sect. Cerv. Spine Res. Soc. 2013, 22, 2414–2420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legaye, J.; Duval-Beaupère, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform Soc. Eur. Sect. Cerv. Spine Res. Soc. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the Normal Variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Passias, P.G.; Bortz, C.; Pierce, K.E.; Passfall, L.; Kummer, N.A.; Krol, O.; Lafage, R.; Diebo, B.G.; Lafage, V.; Ames, C.P.; et al. Comparing and contrasting the clinical utility of sagittal spine alignment classification frameworks: Roussouly versus srs-schwab. Spine 2021, 47, 455–462. [Google Scholar] [CrossRef]
- Dolan, L.A.; Wright, J.G.; Weinstein, S.L. Effects of bracing in adolescents with idiopathic scoliosis. N. Engl. J. Med. 2014, 13, 370. [Google Scholar]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar]
- de Jonge, T.; Dubousset, J.F.; Illés, T. Sagittal plane correction in idiopathic scoliosis. Spine 2002, 27, 754–760. [Google Scholar] [CrossRef]
- Vergari, C.; Courtois, I.; Ebermeyer, E.; Pietton, R.; Bouloussa, H.; Vialle, R.; Skalli, W. Head to pelvis alignment of adolescent idi-opathic scoliosis patients both in and out of brace. Eur. Spine J. 2019, 28, 1286–1295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gutman, G.; Labelle, H.; Barchi, S.; Roussouly, P.; Berthonnaud, É.; Mac-Thiong, J.-M. Normal sagittal parameters of global spinal balance in children and adolescents: A prospective study of 646 asymptomatic subjects. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2016, 25, 3650–3657. [Google Scholar] [CrossRef] [PubMed]
- Schlösser, T.P.C.; Vincken, K.L.; Rogers, K.; Castelein, R.M.; Shah, S.A. Natural sagittal spino-pelvic alignment in boys and girls before, at and after the adolescent growth spurt. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2015, 24, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.-M.; Labelle, H.; Roussouly, P. Pediatric sagittal alignment. Eur. Spine J. Off Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2011, 20 (Suppl. 5), 586–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cil, A.; Yazici, M.; Uzumcugil, A.; Kandemir, U.; Alanay, A.; Alanay, Y.; Acaroglu, E.; Surat, A. The evolution of sagittal segmental alignment of the spine during childhood. Spine 2005, 30, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Shields, M.; Tremblay, M.S.; LaViolette, M.; Craig, C.L.; Janssen, I.; Connor, I.; Gorber, S.C. Fitness of canadian adults: Results from the 2007–2009 canadian health measures survey. Health Rep. 2010, 21, 21–35. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).