Abstract
Background: Shoulder pain is prominent among sedentary employees who make motions of the upper limbs on a regular basis. Rounded shoulder posture (RSP) and hunched shoulder posture (HSP) are the most common clinical postural misalignments. These causes the spine to bend and raise tension on the nerve roots, which has a negative impact on upper-extremity muscular strength and function. Therefore, this study was carried out to investigate the effect of RSP and HSP on the mechanical parameters of the upper body muscles in clinically asymptomatic sedentary workers. Methods: Twenty office workers with RSP, 20 with HSP, and 20 with normal shoulder posture (NSP) were matched for age, BMI, and type of job. Volunteers were split into groups based on photometric shoulder angle measurements. Mechanical properties such as muscle tone, stiffness, and elasticity of the upper trapezius, middle trapezius, posterior deltoid, and pectoralis major were assessed in sedentary postures. Results: The study revealed a significant decrease in muscle tone for the pectoralis major and a significant increase in muscle stiffness for the poster deltoid in both RSP and HSP as compared to NSP. Specifically, muscle tone decreased from 20.1 ± 4.0 to 12.4 ± 3.1 Hz (38.3%), (p ≤ 0.001) in RSP and from 20.1 ± 4.0 to 14.0 ± 4.8 Hz (30.3%), (p ≤ 0.001) in HSP. Muscle stiffness increased from 309.9 ± 70.7 to 348.15 ± 68.7 N/m (11%), (p ≤ 0.001) in RSP and from 309.9 ± 70.7 to 441.7 ± 45.9 N/m (29.8%), (p ≤ 0.001) in HSP. Conclusions: RSP and HSP have an impact on the tone, stiffness, and elasticity of upper body muscles in healthy asymptomatic sedentary workers. These postures, on a regular basis, may affect physical health and decrease workers’ productivity. In addition, it is recommended for sedentary workers to take regular breaks and attend training that could help improve their physical health.
1. Introduction
Excess sedentary behaviour is common and apparently ‘inevitable’ for people who work at a desk for 8 h a day. When a computer is used for a long period in an incorrect posture, the head shifts forward and upward, causing an increase in weight on the neck, which eventually causes a change in the upper body [1,2]. These workers are likely to suffer from lower back, neck, and shoulder aches and other sorts of work-related musculoskeletal injuries. According to EU-OSHA (2019), Musculoskeletal Disorders (MSDs) constitute the most important concern for 60% of workers with a work-related health problem, with 43% including upper limbs and/or shoulders [3]. Faulty postures such as uneven shoulder level are a concern among 36% of adolescents and university students related to shoulder rolling [4,5]. Likewise, over 80% of myofascial pain syndrome patients also have an abnormal rounded shoulder posture (RSP) [6].
The tension in the neck and scapular muscles rises whenever the head moves forward, and the reaction forces in the glenohumeral joint also increase. This can cause MSDs in the upper body, mainly in the shoulders, i.e., rounded shoulder (shoulder forward) and hunched shoulders (shoulder up) [7]. In rounded shoulder posture (RSP), the shoulders appear to be bent forward, caused by scapulae elevation and acromion protraction. These changes may cause disproportion in connected muscles and ultimately cause pain in the head, shoulders, and arms [8].
The shoulders appear lifted up toward the neck and the scapulae are elevated outward in a hunched shoulder posture, which is most commonly observed in computer workers who work in a table-and-chair work environment [9,10,11]. This is caused by the placement of the hands (elbows) during watching (viewing the computer screen) or typing tasks. The recent study conducted on subjects aged 20 to 50 years, revealed that about 73% of workers had right rounded shoulder and 66% had left rounded shoulder [6,12].
There are studies focusing mainly on the head and neck muscles during head postures. However, very few studies have focused on the mechanical effects on muscles due to shoulder postures in sedentary workers. Therefore, the present study focused on investigating the effect of RSPs and HSPs on the mechanical characteristics of the upper body muscles in asymptomatic sedentary workers. The key objective was to assess whether the considered muscles’ tone, stiffness, and elasticity would change during RSPs and HSPs compared to NSPs in the sedentary working population. The outcomes of this study may provide researchers with additional information on shoulder postural alignment. Furthermore, the effect of mechanical parameters on specific muscles during a particular sedentary posture in a specific age group will aid in determining the association between shoulder pain and posture.
2. Methods
2.1. Study Participants
Overall, 60 university staff and students who fulfilled the inclusion requirements were selected. The participants were separated into three groups, normal posture ((NSP), n = 20), RSP (RSP, n = 20), and HSP (HSP, n = 20). The sample size concerning shoulder posture measurements and biomechanical properties was selected based on similar studies [13,14,15,16,17]. All participants were matched for age, height, weight, BMI; the data are presented in Table 1. Only healthy participants without shoulder complaints in the past 6 months were selected for the study. The inclusion criteria of the study are as follows: (1) 25 to 45 years of age, (2) BMI between 18.5 and 25, (3) minimum 35 h of sedentary work, and (4) lack of orthopaedic and neurological comorbidities. Individuals who had undergone surgeries in the upper body region were excluded from the study.

Table 1.
Demographic and clinical characteristics.
To eliminate potential sources of bias, the groups were composed of office employees who performed the same kind of job and in the same kind of workplace. The research was conducted in separate air-conditioned lightroom between 9 a.m. and noon on a workday (Tuesday or Wednesday) between September and November 2021. The protocol was explained to all participants verbally, and they read and signed a consent form. Ethical approval (17 June 2020, No. BE-2-34) was obtained from the regional ethics committee (Lithuanian University of Health Sciences). The Helsinki Declaration of 1964, as well as subsequent revisions, were adhered to.
2.2. Outcome Measures
The outcome measures of this study were (a) stiffness (N/m), the myofascial tissue’s resistance to an external force that has altered its initial shape; (b) tone (Hz), the oscillation frequency of myofascial tissue at its maximum; (c) elasticity after a contraction, the ability to regain its original shape [13].
2.3. Measuring Angle
To determine RSP and HSP, the participants were measured by positioning pointers to the tragus, the seventh cervical vertebra (C7), and the acromion. Two cameras (Canon 600D) (Canon, Tokyo, Japan) were placed 2 m away, one at the acromion level and another at the height of C7. Each volunteer was informed to stand in their natural position and glance at a point highlighted on the screen for a few seconds; the points were marked with markers at C7, tragus, and acromion. When the volunteers were standing in the natural position, photos were taken from side and back view. Moreover, the volunteers were requested to extend their upper body to adjust to normal shoulder position before taking the measurements. Then, the captured images were analysed using the Digimizer tool (version 5.7.2) to measure the angles (Figure 1). The measurements were taken in accordance with the requirements established in the literature [13,16,17]. Rounded shoulder angle: the angle formed by the horizontal line passing through the middle of the humerus and the line from the midpoint of the humerus to the spinous process of C7. Hunched shoulder angle: the angle formed at the intersection of the line between the midpoint of the tragus and the line from the acromion. In the present study, ≤52° was considered as the reference angle for RSP based on Thigpen et al., and ≥45° as the base angle for HSP as per our investigation [16].
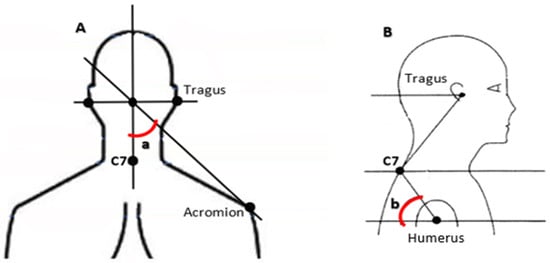
Figure 1.
Marker placement and postural angles. (A) Hunched shoulder posture; (a) hunched shoulder angle; (B) rounded shoulder posture; (b) rounded shoulder angle.
2.4. Procedure
The measurements were taken during the workweek while volunteers were seated and executing their job. The participants were sitting on a chair with their hands on their knees initially and then they were asked to look for a few minutes at a screen placed at eye level and to adopt their standard posture while doing their work [13]. The viscoelastic characteristics were determined in the muscular belly using the Myoton-3 myometer (Myoton AS, Tallin, Estonia). The upper trapezius muscle (UT) was measured first, followed by the middle trapezius muscle (MT), the posterior deltoid muscle (PD), and lastly, the pectoralis major muscle (PM). Due to the better accessibility of the muscle fibres, the measurement point was located in the middle of the muscles.
The probe of the device (3 mm in diameter) was placed perpendicular to the skin’s surface that covered the muscle, and the readings were obtained on the right of the body first, followed by the left side. Eight brief impulses (0.4 N for 15 ms) with a constant automatic preload (0.18 N) were given to trigger the underlying muscle oscillations [18,19]. Then, the induced damped natural oscillations (amplitude of oscillation reduces with time) were recorded by the instrument [8,16,20].
2.5. Data Analysis
The stiffness was obtained by multiplying the highest acceleration of the soft tissue oscillation by the mass of the probe and dividing the result by the maximum displacement of the soft tissue oscillation. With the help of a quick Fourier transform and established methodologies, we calculated the maximum oscillation frequency of soft tissues (Hz) indicative of myofascial stress from the accelerometer data spectrum [13]. The stiffness and tension of the muscles under investigation are inversely related to the values of the two parameters measured. The logarithmic reduction in natural oscillation generated by an impulse was used to calculate elasticity. Muscle flexibility increases when the logarithmic decrement value decreases because mechanical energy is less likely to be wasted when the logarithmic decrement value decreases [21,22].
2.6. Statistical Analysis
Statistical analyses were performed with SPSS (version 28.0, IBM, Armonk, NY, USA). The values of the parameters evaluated were averaged independently for each side of the body based on the results of subsequent measurements. The readings for both sides (i.e., right and left) were averaged again, and then the analysis was conducted separately for the RSP and HSP. First, the effect of mechanical characteristics of muscles in RSP was tested and then on HSP with respect to NSP. The data distribution was analysed using the Shapiro–Wilk test for normality evaluation. Due to the large sample size, the significance of the differences in mean values between the two groups was determined using the parametric independent samples t-test if the data were normally distributed with equal variances. However, if the distribution was not normal and the variance was nonuniform, the nonparametric test (Mann–Whitney U test) was performed. The analyses were carried out by someone uninformed of the group assignment by assuming the significance level as α = 0.05.
3. Results
To our knowledge, this is the first widely available paper where four muscles, the UT, MT, PM, and PD, have been characterized using Myoton-3 during three postures NSP, RSP, and HSP. A few partially relevant outcomes are accessible in the literature for the considered muscles and postures, mainly HSP. In terms of basic features, the groups did not differ; however, those with HSP had a significantly greater HSA (Table 1).
An independent sample t-test was performed to compare the effect of mechanical parameters on muscles in the NSP and RSP groups. The biomechanical characteristics of RSP are shown in Table 2 In terms of muscle tone, the UT, MT, and PM muscles are statistically significant (p < 0.05). For the UT, these are the scores for the NSP (M = 18.6, SD = 4.7) and RSP (M = 14.8, SD = 1.8) groups, t (38) = 3.5, p = 0.002; these are the MT scores for the NSP (M = 13.9, SD = 2.3) and RSP (M = 18.2, SD = 6.0) groups, t (38) = −3.0, p = 0.006; these are the PM scores for the NSP (M = 20.1, SD = 4.0) and RSP (M = 12.4, SD = 3.1) groups, t (38) = 6.9, p ≤ 0.001. Conversely, PD is not statistically significant, p = 0.06. Therefore, the test revealed that the NSP and RSP groups have an effect on muscle tone in the UT, MT, and PM, while they exhibit no effect on the PD muscle.

Table 2.
Mechanical parameters of RSP.
With respect to stiffness, the PM and PD muscles are statistically significant (p < 0.05). The PM scores for the groups are: NSP (M = 235.9, SD = 11.7) and RSP (M = 201.1, SD = 45.8), t (38) = 3.2, p = 0.003. Similarly, the PD scores for the groups are: NSP (M = 309.9, SD = 70.7) and RSP (M = 348.1, SD = 68.7), t (38) = −1.7, p = 0.046. In contrast, UT and MT are not statistically significant, p = 0.248 and p = 0.065. Thus, the findings indicate that the NSP and RSP groups have an effect on PM and PD muscle stiffness, but have no effect on UT and MT muscle stiffness. In terms of elasticity, UT and MT are statistically significant (p < 0.05). UT scores for the NSP group are (M = 1.2, SD = 0.3) and the RSP group are (M = 1.6, SD = 0.2), t (38) = 3.8, p = 0.001. Additionally, the MT scores for the NSP group are (M = 1.7, SD = 0.3) and RSP group are (M = 1.0, SD = 0.008), t (38) = −9.4, p ≤ 0.001. On the other hand, PM and PD are not statistically significant, p = 0.143 and p = 0.302. This shows a difference in elasticity between the NSP and RSP groups, which influences the UT and MT muscles, but not between the PM and PD muscles.
The results of statistical analysis performed to compare the mechanical parameters in the NSP and HSP group are shown in Table 3 MT, PD, and PM muscles are statistically significant (p < 0.05) in muscle tone. MT scores for the NSP group are (M = 13.9, SD = 2.3) and HSP group are (M = 11.2, SD = 3.1), t (38) = 3.0, p = 0.004, PM scores for the NSP group are (M = 20.1, SD = 4.0) and HSP group are (M = 14.0, SD = 4.8), t (38) = 4.3, p ≤ 0.001, and PD scores for the NSP group are (M = 16.0, SD = 2.2) and HSP group are (M = 22.2, SD = 5.0), t (38) = −4.9, p ≤ 0.001, but UT is not statistically significant, p = 0.731. Hence, the test revealed that the NSP and HSP groups do have an effect on the muscle tone of MT, PD, and PM; however, they exhibit no effect on the UT muscles. As for stiffness, all muscles are statistically significant (p < 0.05). The UT scores for the NSP group are (M = 350.4, SD = 72.0) and HSP group are (M = 278.6, SD = 69.6), t (38) = 3.2, p = 0.003 and p < 0.001 for MT, PM, and PD muscles. This shows that the NSP and HSP groups had a significant impact on UT, MT, PM, and PD stiffness. Concerning elasticity, MT and PM are statistically significant (p < 0.05). The MT scores for the NSP group are (M = 1.7, SD = 0.3) and HSP group are (M = 2.0, SD = 0.2), t (38) = −3.4, p = 0.001. In addition, the PM scores for the NSP group are (M = 1.1, SD = 0.6) and RSP group are (M = 1.6, SD = 0.1) t (38) = −3.1, p = 0.005. On the other hand, UT and PD are not statistically significant, p = 0.0993 and p = 0.0.877, respectively. Therefore, the results indicate that the NSP and RSP groups do have an effect on MT and PM, whereas they exhibit no effect on UT and PD muscles.

Table 3.
Mechanical parameters of HSP.
In summary, these results show that among both NSP and RSP participants (Figure 2), the highest elasticity values were recorded in the PM muscle. Simultaneously, the highest tone values were observed in the MT muscle and the highest stiffness values in the PD muscle during RSP. The RSP participants showed considerable variations in the biomechanical characteristics of the muscles studied. Tone and stiffness were statistically significant in the UT and MT muscles, whereas elasticity was significant in the PM and PD muscles. The findings among the NSP and HSP groups show that the values of tone and stiffness are higher in the PD muscle and observed lower values of tone, stiffness, and elasticity in the MT muscle in the HSP group, while the highest tone and stiffness values were recorded in the UT, MT, and PM muscles of the NSP group. Interestingly, elasticity values of the UT and PD had no change in both NSP and HSP.
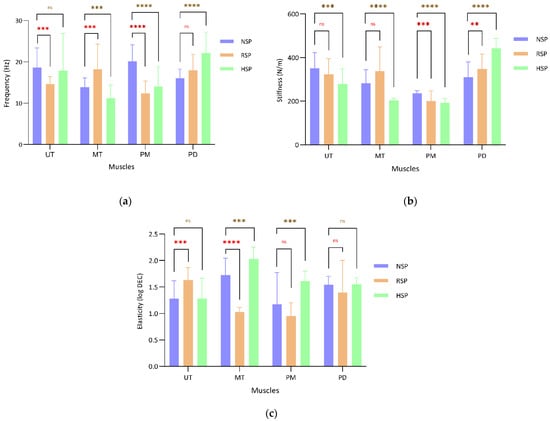
Figure 2.
Mechanical parameters of muscles: (a) tone; (b) stiffness; (c) elasticity of muscles; ns—not significant; ** ≤0.05, *** ≤0.01, and **** ≤0.001—statistically significant.
4. Discussion
The current study is the first to analyse the effects of RSP and HSP with NSP on the mechanical parameters of the upper body muscles in sedentary workers. We assumed that considerable changes in mechanical characteristics might influence the functional impairment of the shoulder and increase the risk of injury when we designed our investigation. Myoton, which is used in this study, has previously been shown to be a reliable screening method for measuring biomechanical and viscoelastic abnormalities [19].
4.1. RSP and the Mechanical Characteristics
RSP can be associated with repetitive overhead activities, backpack carriage, computer and laptop use, and prolonged study hours [23]. This study shows a substantial difference in the mechanical characteristics between the NSP and RSP groups. The tone and elasticity of the UT and MT muscles are statistically significant, whereas stiffness is not significant between the NSP and RSP groups. About a 21% decrement in tone, 7% drop in stiffness, and 33% increase in elasticity of the UT muscle was observed, while a 30% increase in tone, 19% increase in stiffness, and 41% decrease in elasticity of the MT muscles was observed between the NSP and RSP groups. According to a study conducted by Lee et al. on the alteration of muscle contractions in two different sitting postures, there is a substantial difference between the slouched and erect postures [24]. Cools et al. found that when the arm was elevated in a slouched posture and the UT muscle was active for a longer period of time, this could produce pain and continual strain in the cervical and shoulder regions [25].
Interestingly, the results show that the NSP group has much higher muscle tone, stiffness, and elasticity of the UT than the RSP group. The characteristics of the MT muscle, on the other hand, are significantly lower in the NSP group than in the RSP group. In our opinion, this could be because of the variation in shoulder and scapular movements as well as the elbow positioning of each individual in their sitting posture. The primary function of the middle trapezius is to retract the scapula and to maintain the acromiohumeral distance during shoulder elevation due to minimizing of the internal rotation and anterior tilting of the scapula [26]. Guney-Deniz et al.’s findings indicated an increase in the activation levels of middle deltoid and middle trapezius at 0° to 90° of shoulder abduction without scapular retraction [26]. Cheon et al. reported a significant decrease in the middle trapezius muscle activity at 30° extended position and the full range of motion positions as compared to the neutral position (p < 0.05) [27].
The tone and stiffness of the PM muscle is statistically significant, whereas elasticity is not significant between the NSP and RSP groups. In the PM muscle, mechanical characteristics such as tone, stiffness, and elasticity tend to drop by 38%, 14%, and 18% between NSP and RSP. The initial decrease in PM muscle tone that happens while shifting from NSP to RSP indicates that sustaining a seated position demands more tension. According to a study on posture and fitness by Felix, the anterior muscles (pectoralis major and minor) become stiff in the shoulder forward position because they are always shortened [28]. Furthermore, the stiffness of the PD muscle is statistically significant, but there is no difference in tone or elasticity between the NSP and RSP groups. The results show a 12% increase in tone, 12% increase in stiffness, and 6% decrease in elasticity of the PD muscle between the NSP and RSP groups. As mentioned earlier, this immediate increase in stiffness of the PD muscle occurred when shifted from NSP to RSP, indicating that a sitting position requires less stiffness during work. Our earlier study related to muscle activation in various sedentary postures exhibited similar differences in the PD muscle [29]. According to Seo et al., the presence of trauma, and a substantially higher degree of stiffness, increases the preoperative joint range of motion limitations [30,31]. Moreover, sedentary work can cause shoulder instability because the prime movers, such as the deltoids, pectoralis major/minor, latissimus dorsi, and teres major, are not used as often [32].
4.2. HSP and the Mechanical Characteristics
Hunched shoulders are a common symptom of poor posture, especially if people spend a lot of time sitting at a computer, carrying a heavy bag all day, or sitting in the wrong kind of chair, among other things. As per our knowledge, there is no study available related to hunched shoulder posture addressing sedentary workers. In the UT muscle, stiffness was significant, while tone and elasticity were not significant between the NSP and HSP groups. There was a decrease of 20% in stiffness; however, both tone and elasticity were found to be trivial in the UT muscle. A similar conclusion was drawn by Viir et al., who studied the effects on the upper trapezius muscle in various postures and stated that the upright position does not influence the values of elasticity [19]. UT stiffness with and without rotator cuff tendinopathy was studied by Leong et al., and they recommended that monitoring and maintaining UT stiffness is critical for rotator cuff tendinopathy prevention [15]. On the other hand, all mechanical characteristics in the MT muscle were observed to be different between the NSP and HSP groups. The elasticity had a 17% increase, while tone and stiffness showed decrement of 19% and 27%, respectively, in the MT muscle. In MT, stiffness decreased significantly when changed to HSP; this shows the need for posture control during activity or tasks in sedentary workers. Cools et al. concluded that the MT’s tendency to have a lower resting muscular tone contributed to their lack of stiffness changes. The aberrant scapula position and motion are caused by excessive UT activation paired with reduced MT regulation [25]. The rise in muscle tone and fatigue was shown to be mostly dependent on the worker’s physical preparation and length of employment, rather than their age [33].
In the PM muscle, elasticity showed a 45% increase, but both tone and stiffness tended to decrease by 30% and 18%, respectively, between the NSP and HSP groups. The fall in PM muscle tone that happens after changing from an NSP to an HSP demonstrates that sustaining the seated posture requires more effort. Similarly, the decrement in stiffness shows the need for posture control during activity or tasks in sedentary workers. According to Hess [34], muscles such as the pectoralis major and middle trapezius tend to produce more force with the glenohumeral stability constraint, which denotes that the shoulder stability is complex. This clearly demonstrates that PM and MT play a key role in shoulder abduction while performing tasks. In the PD muscle, tone and stiffness increased by 38% and 42%, respectively, while elasticity showed no difference between NSP and HSP. According to Bailey et al., higher stiffness may result in muscle tightness leading to a decreased range of movement of the hand, and lowering muscle stiffness may help improve the shoulder’s range of motion [35].
The function of the middle trapezius is to stabilize and retract the scapula, which can be affected by muscle imbalance. The muscle imbalance is related to RSP and HSP, which can cause disturbance in the length tension relationship of muscles that weakens the stabilizers and retractors. This could be the reason for variation in the mechanical properties in the middle trapezius muscle, whereas the overactive and shortened muscles participating in rounded shoulders are deep upper cervical extensors, which include longissimus capitis, splenius capitis, cervical multifidus, and upper trapezius, and shoulder protractors and elevators, which include pectoralis minor, pectoralis major and levator Scapula [34]. Previous researches have suggested that a weakened postural muscles should be strengthened and shortened muscles should be lengthened in order to improve postural alignment and alleviate rounded shoulder posture and restore the normal muscle balance between opposing muscle groups (agonists and antagonists).This forward posture can cause a lack of space in the lateral and/or anterior area of the subacromial space of the shoulder. Rounded or forward posture can develop for a variety of reasons: poor ergonomics at work, overall weak posture muscles, or repetitive activities that cause increased muscle tone in the front portion of the shoulder or body. Furthermore, it is crucial to note that a direct comparison between the prior research and the current study is difficult to draw because the current study focused on sedentary workers who were divided into groups based on their postural angles.
4.3. Study Limitations
In this study, we grouped the individuals who performed similar work but not random independent participants as samples; therefore, this grouping could introduce a potential bias. The study did not consider the participants with RSP and HSP ailments; perhaps this may affect the mechanical parameters of muscles. Furthermore, only men were included as a part of the study, and in future comparisons, it may well be worth including women as part of a wider group. In addition, a relatively small sample size of the study could contribute to the type II statistical error.
Lastly, while angle measurement is widespread, this is not the only or best way to evaluate postures. As a result, it would be desirable to widen the research to consider classification-based criteria, such as reference points collected from upper body X-rays.
5. Conclusions
In office workers, the biomechanical characteristics of the muscles during RSP and HSP have changed significantly. This study showed that RSP and HSP are more likely to impact the tone, stiffness, and elasticity of the upper body muscles. MT has higher muscle tone in RSP and lower in HSP, and vice versa. In the case of stiffness, for RSP, and HSP, the PD muscle has the highest value, and PM and MT the lowest. PM and UT have the highest logarithmic decrement during RSP and HSP. These postures, held on a regular basis, may affect physical health and decrease workers’ productivity. This shows that the postural changes associated with RSP and HSP could affect sedentary workers’ shoulder kinematics and muscle activity. Furthermore, it is recommended that sedentary workers take regular breaks and attend training that could help improve their physical health, and organizations should track postural changes and alerts by using monitoring devices [36].
Author Contributions
Conceptualization, R.K.R.G. and A.D. (Aurelijus Domeika); methodology, R.K.R.G., A.D. (Aurelijus Domeika), and A.D. (Auksė Domeikienė); investigation, R.K.R.G., A.D. (Aurelijus Domeika), and A.D. (Auksė Domeikienė); Experiments, R.K.R.G. and A.D. (Aurelijus Domeika); formal analysis, R.K.R.G. and A.D. (Aurelijus Domeika); writing—original draft preparation, R.K.R.G.; writing—review and editing, R.K.R.G. and A.D. (Aurelijus Domeika). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Lithuanian University of Health Sciences (No. BE-2-34, 17 June 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available in the article.
Acknowledgments
The authors would like to thank the volunteers who participated in the study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| NSP | Normal shoulder posture |
| RSP | Rounded shoulder posture |
| HSP | Hunched shoulder posture |
| RSA | Rounded shoulder angle |
| HSA | Hunched shoulder angle |
| UT | Upper trapezius |
| MT | Middle trapezius |
| PM | Pectoralis major |
| PD | Posterior deltoid |
| BMI | Body mass index |
References
- Kang, J.-H.; Park, R.-Y.; Lee, S.-J.; Kim, J.-Y.; Yoon, S.-R.; Jung, K.-I. The Effect of The Forward Head Posture on Postural Balance in Long Time Computer Based Worker. Ann. Rehabil. Med. 2012, 36, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Betz, J.J.; Janik, T.J.; Holland, B.; Colloca, C.J.; Haas, J.W. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: Nonrandomized clinical control trial. J. Manip. Physiol. Ther. 2003, 26, 139–151. [Google Scholar] [CrossRef]
- Kok, J.; De Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; Isusi, I. Work-Related MSDs: Prevalence, Costs and Demographics in the EU (European Risk Observatory Executive Summary); Publications Office of the European Union: Bilbao, Spain, 2019; pp. 1–18. [Google Scholar]
- Nguyen, M.T.; Dang, Q.K.; Kim, Y.; Chee, Y. A Measurement System for Rounded Shoulder Posture using a Wearable Stretch Sensor. J. Biomed. Eng. Res. 2018, 39, 10–15. [Google Scholar]
- Soares, F.A.; Andrade, M.M.; De Merletti, R. Automatic Tracking of Innervation Zones Using Image Processing Methods. In Proceedings of the ISSNIP Biosignals and Biorobotics Conference, Vitoria, Brazil, 4–6 January 2010; pp. 214–218. [Google Scholar]
- Mosaad, D.M.; Abdel-Aziem, A.A.; Mohamed, G.I.; Abd-Elaty, E.A.; Mohammed, K.S. Effect of forward head and rounded shoulder posture on hand grip strength in asymptomatic young adults: A cross-sectional study. Bull. Fac. Phys. Ther. 2020, 25, 1–8. [Google Scholar] [CrossRef]
- Tomita, Y.; Suzuki, Y.; Tanaka, Y.; Hasegawa, Y.; Yoshihara, Y.; Okura, K.; Matsuka, Y. Effects of sitting posture and jaw clenching on neck and trunk muscle activities during typing. J. Oral Rehabil. 2021, 48, 568–574. [Google Scholar] [CrossRef]
- Lukasiewicz, A.C.; McClure, P.; Michener, L.; Pratt, N.; Sennett, B.; Ludewig, P. Comparison of 3-Dimensional Scapular Position and Orientation Between Subjects With and Without Shoulder Impingement. J. Orthop. Sports Phys. Ther. 1999, 29, 574–586. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, H.; Shin, W.-S. Characteristics of shoulder pain, muscle tone and isokinetic muscle function according to the scapular position of elite boxers. Phys. Ther. Rehabil. Sci. 2020, 9, 98–104. [Google Scholar] [CrossRef]
- Viir, R.; Virkus, A.; Laiho, K.; Rajaleid, K.; Selart, A.; Mikkelson, M. Trapezius muscle tone and viscoelastic properties in sitting and supine positions. Scand. J. Work Environ. Health Suppl. 2007, 33, 76–80. [Google Scholar]
- Naidoo, N.; Lazarus, L.; Van Tongel, A.; Osman, S.; Satyapal, K. Introduction of the angle of shoulder slope in a South African population. SA Orthop. J. 2017, 16, 40–43. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz. J. Phys. Ther. 2014, 18, 364–371. [Google Scholar] [CrossRef]
- Kocur, P.; Wilski, M.; Goliwąs, M.; Lewandowski, J.; Łochyński, D. Influence of Forward Head Posture on Myotonometric Measurements of Superficial Neck Muscle Tone, Elasticity, and Stiffness in Asymptomatic Individuals With Sedentary Jobs. J. Manip. Physiol. Ther. 2019, 42, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Hibberd, E.E.; Laudner, K.; Berkoff, D.J.; Kucera, K.L.; Yu, B.; Myers, J.B. Comparison of Upper Extremity Physical Characteristics Between Adolescent Competitive Swimmers and Nonoverhead Athletes. J. Athl. Train. 2016, 51, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.T.; Hug, F.; Fu, A. Increased Upper Trapezius Muscle Stiffness in Overhead Athletes with Rotator Cuff Tendinopathy. PLoS ONE 2016, 11, e0155187. [Google Scholar] [CrossRef] [PubMed]
- Thigpen, C.A.; Padua, D.A.; Michener, L.A.; Guskiewicz, K.; Giuliani, C.; Keener, J.D.; Stergiou, N. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. J. Electromyogr. Kinesiol. 2010, 20, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Brink, Y.; Crous, L.C.; Louw, Q.A.; Grimmer, K.; Schreve, K. The association between postural alignment and psychosocial factors to upper quadrant pain in high school students: A prospective study. Man. Ther. 2009, 14, 647–653. [Google Scholar] [CrossRef]
- Kim, T.-W.; An, D.-I.; Lee, H.-Y.; Jeong, H.-Y.; Kim, N.-H.; Sung, Y.-H. Effects of elastic band exercise on subjects with rounded shoulder posture and forward head posture. J. Phys. Ther. Sci. 2016, 28, 1733–1737. [Google Scholar] [CrossRef]
- Viir, R.; Laiho, K.; Kramarenko, J.; Mikkelsson, M. Repeatability of Trapezius Muscle Tone Assessment by a Myometric Method. J. Mech. Med. Biol. 2006, 6, 215–228. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Mullix, J.; Warner, M.; Stokes, M. Testing muscle tone and mechanical properties of rectus femoris and biceps femoris using a novel hand held MyotonPRO device: Relative ratios and reliability. Work Pap. Heal. Sci. Internet. 2012, 2051–6266, 1–8. Available online: https://eprints.soton.ac.uk/345285/1/Testing_muscle_tone_and_mechanical_properties_of_rectus_.pdf (accessed on 6 February 2022).
- Kisilewicz, A.; Janusiak, M.; Szafraniec, R.; Smoter, M.; Ciszek, B.; Madeleine, P.; Fernández-De-Las-Peñas, C.; Kawczyński, A. Changes in Muscle Stiffness of the Trapezius Muscle after Application of Ischemic Compression into Myofascial Trigger Points in Professional Basketball Players. J. Hum. Kinet. 2018, 64, 35–45. [Google Scholar] [CrossRef]
- Singla, D.; Veqar, Z. Association Between Forward Head, Rounded Shoulders, and Increased Thoracic Kyphosis: A Review of the Literature. J. Chiropr. Med. 2017, 16, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.T.; Moon, J.; Lee, S.H.; Cho, K.H.; Im, S.H.; Kim, M.; Min, K. Changes in Activation of Serratus Anterior, Trapezius and Latissimus Dorsi With Slouched Posture. Ann. Rehabil. Med. 2016, 40, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Cools, A.M.; Declercq, G.A.; Cambier, D.C.; Mahieu, N.N.; Witvrouw, E.E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand. J. Med. Sci. Sports 2006, 17, 25–33. [Google Scholar] [CrossRef]
- Guney-Deniz, H.; Harput, G.; Toprak, U.; Duzgun, I. Relationship Between Middle Trapezius Muscle Activation and Acromiohumeral Distance Change During Shoulder Elevation With Scapular Retraction. J. Sport Rehabil. 2019, 28, 266–271. [Google Scholar] [CrossRef]
- Cheon, S.; Park, S. Changes in neck and upper trunk muscle activities according to the angle of movement of the neck in subjects with forward head posture. J. Phys. Ther. Sci. 2017, 29, 191–193. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Felix, D. Posture and Fitness (Part 1): Kyphosis (Rounded Shoulders). Available online: https://www.nifs.org/blog/posture-and-fitness-kyphosis-rounded-shoulders (accessed on 6 February 2022).
- Guduru, R.K.R.; Domeika, A.; Dubosiene, M. Analysis of muscle activation during sedentary positions in different upper extremities in office workers. Turk. J. Physiother. Rehabil. 2021, 32, 31655–31660. [Google Scholar]
- Seo, S.-S.; Choi, J.-S.; An, K.-C.; Kim, J.-H.; Kim, S.-B. The factors affecting stiffness occurring with rotator cuff tear. J. Shoulder Elb. Surg. 2012, 21, 304–309. [Google Scholar] [CrossRef]
- Hellig, T.; Rick, V.; Mertens, A.; Nitsch, V.; Brandl, C. Investigation of observational methods assessing workload of static working postures based on surface electromyography. Work 2019, 62, 185–195. [Google Scholar] [CrossRef]
- Mehrab, M.; de Vos, R.-J.; Kraan, G.A.; Mathijssen, N.M. Injury Incidence and Patterns Among Dutch CrossFit Athletes. Orthop. J. Sports Med. 2017, 5, 2325967117745263. [Google Scholar] [CrossRef]
- Roja, Z.; Kalkis, V.; Vain, A.; Kalkis, H.; Eglite, M. Assessment of skeletal muscle fatigue of road maintenance workers based on heart rate monitoring and myotonometry. J. Occup. Med. Toxicol. 2006, 1, 20. [Google Scholar] [CrossRef]
- Hess, S. Functional stability of the glenohumeral joint. Man. Ther. 2000, 5, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Bailey, L.B.; Shanley, E.; Hawkins, R.; Beattie, P.F.; Fritz, S.; Kwartowitz, D.; Thigpen, C.A. Mechanisms of Shoulder Range of Motion Deficits in Asymptomatic Baseball Players. Am. J. Sports Med. 2015, 43, 2783–2793. [Google Scholar] [CrossRef] [PubMed]
- Guduru, R.K.R.; Domeika, A.; Dubosiene, M.; Kazlauskiene, K. Prediction framework for upper body sedentary working behaviour by using deep learning and machine learning techniques. Soft Comput. 2021, 1–16. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).